RS7-Acid Base Balance
Diunggah oleh
Gabriella ChafrinaDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
RS7-Acid Base Balance
Diunggah oleh
Gabriella ChafrinaHak Cipta:
Format Tersedia
REGULATION OF ACID BASE BALANCE| Tutorial B-1 RS
130110110177|Gabriella Chafrina| 13/12/13
Hydrogen Ion Concentration Is Precisely Regulated
Precise H
+
regulation is essential because the activities of almost all enzyme systems in the body are influenced
by H
+
concentration. Therefore, changes in hydrogen concentration alter virtually all cell and body functions.
Normal concentration of H+ is 0.00004 mEq/L (3.5 million times smaller than concentration of sodium in
extracellular fluid 142 mEq/L)
Acids and BasesTheir Definitions and Meanings
- Hydrogen ion: single free proton released from a hydrogen atom
- Acid: Molecules containing hydrogen atoms that can release hydrogen ions in solutions. Example:
hydrochloric acid (HCl), which ionizes in water to form hydrogen ions (H
+
) and chloride ions (Cl
)
- Base: Ion or a molecule that can accept an H
+
. Examples: HCO
3
is a base because it can combine with H
+
to form H
2
CO
3
. The proteins in the body also function as bases, because some of the amino acids that make
up proteins have net negative charges that readily accept H
+
- The terms base and alkali are often used synonymously. Alkali: molecule formed by the combination of one
or more of the alkaline (sodium, potassium, lithium, and so etc) with a highly basic ion such as a hydroxyl
ion (OH
). The base portion of these molecules reacts quickly with H
+
to remove it from solution
- Strong and Weak Acids and Bases
Strong acid: one that rapidly dissociates and releases especially large amounts of H+ in solution. Example:
HCl
Weak acids: have less tendency to dissociate their ions and release H
+
with less vigor. Example: H
2
CO
3
Strong base: one that reacts rapidly and strongly with H
+
and reacts with H
+
to form water. Example:
OH
-
Weak base: binds with H
+
much more weakly than does OH
. Example: HCO
3
-
Normal Value of Hydrogen Ion Concentration and pH of Body Fluids
- Blood H+ concentration: 0.00004 mEq/L (40 nEq/L). Normal variations: 3 to 5 nEq/L. Extreme conditions
(without causing death): 10 nEq/L to as high as 160 nEq/L
Because concentration ion hydrogen are in very small numbers, it is customary to express H
+
concentration on
a logarithm scale, using pH units:
Therefore, the normal pH = log [0.00000004] = 7.4
- pH normal of arterial blood: 7.4
- pH normal venous blood and interstitial fluid: 7.35 because of the extra amounts of carbon dioxide (CO
2
)
- acidosis < 7.4 (tolerated 0.05) < alkalosis
- 6.8 < person can live more than a few hours < 8.0
- pH in every tissue and fluid is different
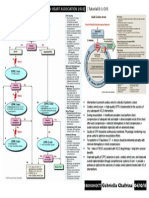
Defenses Against Changes in Hydrogen Ion Concentration: Buffers, Lungs, and Kidneys
There are 3 primary systems that regulate the H
+
concentration in body fluids to prevent acidosis/alkalosis:
(1) Chemical acid-base buffer systems of the body fluids, which immediately combine with acid or base to
prevent excessive changes in H
+
concentration react within a fraction of a second to minimize these
changes. Buffer systems do not eliminate H
+
from or add them to the body but only keep them tied up until
balance can be reestablished.
(2) Respiratory center, which regulates the removal of CO
2
(indirectly H
2
CO
3
) from the extracellular fluid.
Second line of defense, acts within a few minutes
(3) Kidneys, which can excrete either acid or alkaline urine. Relatively slow to respond compared with others,
(over a period of hours to several days) but the most powerful of the acid-base regulatory systems
OBJECTIVE: keep pH to balance either added by strong acid or base
REGULATION OF ACID BASE BALANCE| Tutorial B-1 RS
130110110177|Gabriella Chafrina| 13/12/13
Buffering of Hydrogen Ions in the Body Fluids
- Buffer: any substance that can reversibly bind H
+
- General form:
- When the H
+
concentration increases, the reaction is forced to the right and more H
+
binds to the buffer. .
Conversely, when the H
+
concentration decreases, the reaction shifts toward the left, and H
+
is released
from the buffer
- IMPORTANCE: low concentration of H
+
in the body fluids and the relatively large amounts of acids
produced by the body each day
Bicarbonate Buffer System
- Consists of a water solution that contains two ingredients: (1) a weak acid, H
2
CO
3
and (2) a bicarbonate
salt, such as NaHCO
3
.
- H
2
CO
3
is formed in the body by the reaction:
Exceedingly small amounts of H
2
CO
3
are formed unless the enzyme carbonic anhydrase is present
Carbonic anhydrase abundant in the walls of the lung alveoli (CO
2
is released) and in the epithelial
cells of the renal tubules (CO
2
reacts with H
2
O to form H
2
CO
3
)
- H
2
CO
3
ionizes weakly:
- Bicarbonate salt (commonly NaHCO
3
) in the extracellular fluid
- NaHCO
3
ionizes almost completely:
- System formed: Because of the weak dissociation of H
2
CO
3
, the H
+
concentration is extremely small
- When a strong acid (ex: HCl) is added to the bicarbonate buffer solution, H
+
released from the acid is
increased (buffered by HCO
3
-
): result more H
2
CO
3
formed CO
2
and
H
2
O. Excess CO2 greatly stimulates respiration, which eliminates the CO
2
from the extracellular fluid
- When a strong base (ex: NaOH) is added to the bicarbonate buffer solution:
OH
(from the NaOH) + H
2
CO
3
form additional HCO
3
-
& concentration of H
2
CO
3
(because reacts with
NaOH), causing CO
2
to combine with H
2
O to replace the H
2
CO
3
- CO
2
levels in the blood inhibits respiration and the rate of CO
2
expiration
- HCO
3
that occurs is compensated for by renal excretion of HCO
3
-
Acid base disturbances
Metabolic acid-base disorders: a primary change in extracellular fluid bicarbonate concentration
- a primary decrease in bicarbonate concentration: metabolic acidosis
- a primary increase in bicarbonate concentration: metabolic alkalosis
- increase in PCO
2
: respiratory acidosis
- decrease in PCO
2
: respiratory alkalosis
Phosphate Buffer System
- Not important as an extracellular fluid buffer, but plays a major role in buffering renal tubular fluid and
intracellular fluids.
- The main elements of the phosphate buffer system are H
2
PO
4
and HPO
4
2-
- When a strong acid (ex: HCl) is added: (hydrogen accepted by the
base HPO
4
2-
and converted to H
2
PO
4
) Strong acid (HCl) is replaced by an additional amount of a weak
acid, NaH
2
PO
4
& pH minimized
- When a strong base (ex: NaOH) is added to the buffer system: (the
OH
is buffered by the H
2
PO
4
to form additional amounts of HPO
4
2-
+ H
2
O a strong base (NaOH) is
traded for a weak base, NaH
2
PO
4
, causing only a slight increase in pH
REGULATION OF ACID BASE BALANCE| Tutorial B-1 RS
130110110177|Gabriella Chafrina| 13/12/13
The phosphate buffer system has a pK of 6.8, which is not far from the normal pH of 7.4 in the body fluids
allows the system to operate near its maximum buffering power. However, its concentration in the extracellular
fluid is low, only about 8 per cent of the concentration of the bicarbonate buffer. The phosphate buffer is
especially important in the tubular fluids of the kidneys, for:
(1) Phosphate usually becomes greatly concentrated in tubules, thereby buffering power of phosphate system
(2) The tubular fluid usually has a considerably lower pH than the extracellular fluid does, bringing the
operating range of the buffer closer to the pK (6.8) of the system.
Proteins: Important Intracellular Buffers
- Approximately 60 to 70 per cent of the total chemical buffering of the body fluids is inside the cells, and
most of this results from the intracellular proteins
- This diffusion of the elements of the bicarbonate buffer system causes the pH in intracellular fluid to change
when there are changes in extracellular pH. For this reason, the buffer systems within the cells help prevent
changes in the pH of extracellular fluid but may take several hours to become maximally effective.
- The slowness with which H
+
and HCO
3
move through the cell membranes often delays for several hours
the maximum ability of the intracellular proteins to buffer extracellular acid-base abnormalities
- Example: Hemoglobin, the reaction:
Respiratory Regulation of Acid-Base Balance
- CO
2
is formed continually in the body by intracellular metabolic
processes diffuses from the cells into the interstitial fluids and blood
flowing blood transports it to the lungs diffuses into the alveoli
pulmonary ventilation transferred to the atmosphere
- Metabolic formation of CO
2
pCO
2
extracellular balancing:
pulmonary ventilation
- The higher the alveolar ventilation, the lower pCO
2
, and conversely.
Increasing alveolar ventilation to about 2x normal raises the pH of
extracellular fluid by about 0.23 Conversely a decrease in alveolar
ventilation to reduces the pH by 0.45
- Feedback control of H
+
concentration by the respiratory system:
- Respiratory control cannot return the H+ concentration all the way back
to normal when a disturbance outside the respiratory system has altered
pH. Ordinarily, the respiratory mechanism for controlling H+
concentration has an effectiveness between 50 and 75%, corresponding
to a feedback gain of 1 to 3. That is, if the H+ concentration is suddenly
by adding acid to the extracellular fluid and pH falls from 7.4 to 7.0,
the respiratory system can return the pH to a value of about 7.2 to 7.3.
This response occurs within 3 to 12 minutes.
- Respiratory regulation of acid-base balance is a physiologic type of buffer system because it acts rapidly
and keeps the H+ concentration from changing too much until the slowly responding kidneys can eliminate
the imbalance. In general, the overall buffering power of the respiratory system is one to two times as great
as the buffering power of all other chemical buffers in the extracellular fluid combined. That is, one to two
times as much acid or base can normally be buffered by this mechanism as by the chemical buffers.
- Impairment of lung function can cause respiratory acidosis. Ex: emphysema ability of lungs to
eliminate CO
2
REGULATION OF ACID BASE BALANCE| Tutorial B-1 RS
130110110177|Gabriella Chafrina| 13/12/13
Renal Control of Acid-Base Balance
- The kidneys control acid-base balance by excreting either an acidic or a basic urine
Mechanism:
- Large numbers of HCO
3
are filtered continuously into the tubules, and if they are excreted into the urine,
this removes base from the blood
- Large numbers of H
+
are also secreted into the tubular lumen by the tubular epithelial cells, thus removing
acid from the blood
- See net loss. If there is lot base gone pH decrease, if more acid gone pH increase
Thus, the kidneys regulate extracellular fluid H
+
concentration through three fundamental mechanisms: (1)
secretion of H+, (2) reabsorption of filtered HCO
3
-
, and (3) production of new HCO
3
-
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Pathogenesis of LeprosyDokumen13 halamanPathogenesis of LeprosyNurul AinBelum ada peringkat
- Foreign Body EarDokumen34 halamanForeign Body EarGabriella ChafrinaBelum ada peringkat
- Soal Mde Tropmed 2007Dokumen4 halamanSoal Mde Tropmed 2007Gabriella ChafrinaBelum ada peringkat
- Lab PharmacologyDokumen2 halamanLab PharmacologyGabriella ChafrinaBelum ada peringkat
- ECG Arrhythmia GraphsDokumen3 halamanECG Arrhythmia GraphsGabriella ChafrinaBelum ada peringkat
- Cvs4-Clinical Aspects of Serum Cholesterol LevelDokumen2 halamanCvs4-Clinical Aspects of Serum Cholesterol LevelGabriella ChafrinaBelum ada peringkat
- TM3-Diagnosis and DD of MalariaDokumen3 halamanTM3-Diagnosis and DD of MalariaGabriella ChafrinaBelum ada peringkat
- Rs4 Phop CRPDokumen2 halamanRs4 Phop CRPGabriella ChafrinaBelum ada peringkat
- GUS4 Antihypertensive DrugsDokumen7 halamanGUS4 Antihypertensive DrugsGabriella ChafrinaBelum ada peringkat
- RS7 InfluenzaDokumen6 halamanRS7 InfluenzaGabriella ChafrinaBelum ada peringkat
- Rs6-Cervical Lymph NodeDokumen6 halamanRs6-Cervical Lymph NodeGabriella ChafrinaBelum ada peringkat
- RS5 PiDokumen9 halamanRS5 PiGabriella ChafrinaBelum ada peringkat
- Rs6 Extrapulmonary TuberculosisDokumen4 halamanRs6 Extrapulmonary TuberculosisGabriella ChafrinaBelum ada peringkat
- Rs6 Pleural TuberculosisDokumen5 halamanRs6 Pleural TuberculosisGabriella ChafrinaBelum ada peringkat
- RS5-Defense Mech of LungDokumen3 halamanRS5-Defense Mech of LungGabriella ChafrinaBelum ada peringkat
- RS3 PiDokumen5 halamanRS3 PiGabriella ChafrinaBelum ada peringkat
- Rs4-Gas Exchange and TransportDokumen5 halamanRs4-Gas Exchange and TransportGabriella ChafrinaBelum ada peringkat
- Lab PharmacologyDokumen2 halamanLab PharmacologyGabriella ChafrinaBelum ada peringkat
- Group A Β-Hemolytic Streptococcus: - Tutorial B-1 RSDokumen2 halamanGroup A Β-Hemolytic Streptococcus: - Tutorial B-1 RSGabriella ChafrinaBelum ada peringkat
- CVS6 Page InterpretationDokumen2 halamanCVS6 Page InterpretationGabriella ChafrinaBelum ada peringkat
- GUS6 Macroscopic HematuriaDokumen3 halamanGUS6 Macroscopic HematuriaGabriella ChafrinaBelum ada peringkat
- RS1 ManagementDokumen3 halamanRS1 ManagementGabriella ChafrinaBelum ada peringkat
- Deep Vein Thrombosis (DVT) : - Tutorial D-1 CVSDokumen1 halamanDeep Vein Thrombosis (DVT) : - Tutorial D-1 CVSGabriella ChafrinaBelum ada peringkat
- CVS5-Conduction of Cardiac Action PotentialsDokumen1 halamanCVS5-Conduction of Cardiac Action PotentialsGabriella ChafrinaBelum ada peringkat
- Advance Life Support (American Heart Association 2010) : - Tutorial D-1 CVSDokumen1 halamanAdvance Life Support (American Heart Association 2010) : - Tutorial D-1 CVSGabriella ChafrinaBelum ada peringkat
- CVS6 Heart SoundsDokumen3 halamanCVS6 Heart SoundsGabriella ChafrinaBelum ada peringkat
- Iccu (Tachycardia) : - Tutorial D-1 CVSDokumen2 halamanIccu (Tachycardia) : - Tutorial D-1 CVSGabriella ChafrinaBelum ada peringkat
- Iccu (Tachycardia) : - Tutorial D-1 CVSDokumen2 halamanIccu (Tachycardia) : - Tutorial D-1 CVSGabriella ChafrinaBelum ada peringkat
- Advance Life Support (Resuscitation Council (Uk) 2000) : - Tutorial D-1 CVSDokumen1 halamanAdvance Life Support (Resuscitation Council (Uk) 2000) : - Tutorial D-1 CVSGabriella ChafrinaBelum ada peringkat
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Chapter 2 Protein SeparationDokumen83 halamanChapter 2 Protein SeparationZul Adli SaribinBelum ada peringkat
- BF3 Equilibrium WaterDokumen2 halamanBF3 Equilibrium Watersandypu080% (1)
- Applications of Neutralization TitrationsDokumen22 halamanApplications of Neutralization TitrationsNora BuanBelum ada peringkat
- DistillationDokumen89 halamanDistillationjokish33% (3)
- Crystal Structure Notes: 1. Explain The Following Terms BrieflyDokumen12 halamanCrystal Structure Notes: 1. Explain The Following Terms BrieflyNitesh ShahBelum ada peringkat
- Lab Report: Shahjalal University of Science & Technology, SylhetDokumen5 halamanLab Report: Shahjalal University of Science & Technology, SylhetMd Afif AbrarBelum ada peringkat
- Astm-C 240 PDFDokumen4 halamanAstm-C 240 PDFIvan AlanizBelum ada peringkat
- Quantitative Analytical Chemistry and Its Importance of Pharmaceutical Field1Dokumen9 halamanQuantitative Analytical Chemistry and Its Importance of Pharmaceutical Field1cyper zoonBelum ada peringkat
- Determination of The PH Value of Water Using A PH MeterDokumen7 halamanDetermination of The PH Value of Water Using A PH MeterRome Dionisio Komicho100% (1)
- Standardization of NaohDokumen3 halamanStandardization of NaohsadyaBelum ada peringkat
- Nitric Acid Concentration PDFDokumen2 halamanNitric Acid Concentration PDFmahdiar100% (1)
- Analytical Chemistry: Volumetric Analysis)Dokumen21 halamanAnalytical Chemistry: Volumetric Analysis)Bryar HusenBelum ada peringkat
- Lec8 Chrom3 HPLCDokumen14 halamanLec8 Chrom3 HPLCAnonymous Jlq5r8W1Belum ada peringkat
- Lab ReportDokumen4 halamanLab ReportIhzaz NaeemBelum ada peringkat
- The Impact of Trimethoprim and Norsulfazol On The Metabolic Profile of The S.Aureus (04-02981)Dokumen51 halamanThe Impact of Trimethoprim and Norsulfazol On The Metabolic Profile of The S.Aureus (04-02981)Hernan Matias LedesmaBelum ada peringkat
- Spectrophotometric Determination of Zinc in Pharmaceutical Medication Samples Using 8-Hydroxyquinoline ReagentDokumen8 halamanSpectrophotometric Determination of Zinc in Pharmaceutical Medication Samples Using 8-Hydroxyquinoline Reagentmaha hussinBelum ada peringkat
- Baeocystin in Psilocybe Semilanceata: It"3 - L 4 (LDokumen2 halamanBaeocystin in Psilocybe Semilanceata: It"3 - L 4 (LpiniedduBelum ada peringkat
- 3.4 Calculate The Concentration Set 1 QP MsDokumen4 halaman3.4 Calculate The Concentration Set 1 QP Msbipin jainBelum ada peringkat
- Star Education Academy: Short Questions TestDokumen2 halamanStar Education Academy: Short Questions TestMohammad AshfaqBelum ada peringkat
- CHAPTER - 2 - Acids, Bases and SaltsDokumen2 halamanCHAPTER - 2 - Acids, Bases and Saltsshuchi guptaBelum ada peringkat
- Ge 2009Dokumen3 halamanGe 2009RICHARD MACIENTE SILVINO DA SILVABelum ada peringkat
- Chapter 16Dokumen42 halamanChapter 16Sigmund PohanBelum ada peringkat
- 2022 HSC ChemistryDokumen40 halaman2022 HSC ChemistryioshuofhsueiBelum ada peringkat
- Acid Base Note Chem1aa3Dokumen102 halamanAcid Base Note Chem1aa3violet.pandas37Belum ada peringkat
- AN789 Fast Extraction of VMA 5-HIAA and HVA From Synthetic UrineDokumen4 halamanAN789 Fast Extraction of VMA 5-HIAA and HVA From Synthetic UrineDarshana JuvekarBelum ada peringkat
- Development and Validation of HPLC Method For The PDFDokumen9 halamanDevelopment and Validation of HPLC Method For The PDFAlejandro Muñoz LazoBelum ada peringkat
- Chem Lab Report 1 EqulibriumDokumen4 halamanChem Lab Report 1 EqulibriumГюнель ГусейноваBelum ada peringkat
- Company Profile Indotech 2020Dokumen20 halamanCompany Profile Indotech 2020sabrina saraswatiBelum ada peringkat
- Unit 11 Packet PDFDokumen25 halamanUnit 11 Packet PDFMaxim HristozovBelum ada peringkat
- Evaluation of Critical Consumable Items.Dokumen6 halamanEvaluation of Critical Consumable Items.Abhinav Kumar100% (1)