M. Folikulitiseefef
Diunggah oleh
Sandy GunawanJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
M. Folikulitiseefef
Diunggah oleh
Sandy GunawanHak Cipta:
Format Tersedia
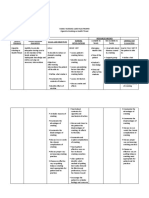
FIGURE 32-32 Infectious folliculitis: Malassezia furfur A 41-year-old Hispanic male with
trunkal rash for 2 months. Multiple, discrete, follicular papulopustules on the chest. Lesional
biopsy showed yeast forms of Malassezia furfur. The lesions resolved after treatment with oral
itraconazole
Infectious Foliculitis
_ Infectious folliculitis begins in the upper portion of
the hair follicle
_ Etiologic agents: Bacteria, fungi, virus, mites
_ Manifestations: Follicular papule, pustule, erosion,
or crust at the follicular infundibulum
_ Infection can extend deeper into the entire length
of the follicle (sycosis).
ETIOLOGY AND EPIDEMIOLOGY
Etiology See Table 32-6.
Predisposing Factors
Shaving hairy regions such as the beard area,
axillae, or legs facilitates follicular infection.
Extraction of hair such as plucking or waxing.
Occlusion of hair-bearing areas facilitates
growth of microbes: clothing, plastic film,
_ Infectious folliculitis begins in the upper portion of
the hair follicle
_ Etiologic agents: Bacteria, fungi, virus, mites
_ Manifestations: Follicular papule, pustule, erosion,
or crust at the follicular infundibulum
_ Infection can extend deeper into the entire length
of the follicle (sycosis).
INFECTIOUS FOLLICULITIS ICD-9 : 704.8 ICD-10 : L73.8 _ _
adhesive plaster, position (sitting occludes
buttocks, lying in bed occludes back), prosthesis,
natural occlusion in intertriginous
sites (axillae, inframammary, anogenital).
Topical climate with high temperature and
relative humidity.
Topical glucocorticoid preparations.
Systemic antibiotic promotes growth of gramnegative
bacteria; diabetes mellitus; immunosuppression.
TABLE 32-6 Classification of Infectious Folliculitis by Etiology
Infectious Agent Organism
Bacterial S. aureus: superficial (Bockhart impetigo); deep (sycosis); may
progress
to furuncle (boil) or carbuncle formation
Pseudomonas aeruginosa (hot-tub) folliculitis; gram-negative folliculitis
Fungal Dermatophytic folliculitis: tinea capitis, tinea barbae, Majocchi
granuloma;
Malassezia folliculitis;
Candida folliculitis
Viral Herpes simplex virus;
Varicella-zoster virus;
Molluscum contagiosum;
Syphilitic Secondary syphilis: alopecia, acneiform
Infestation Demodicidosis
Superficial infection heals without scarring,
but in darkly pigmented individuals, postinflammatory
hypo- and hyperpigmentation.
Extension of infection can progress to abscess
or furuncle formation (Fig. 32-29).
CLINICAL MANIFESTATION
Symptoms S. aureus and dermatophytic folliculitis
can be chronic. Usually nontender or
slightly tender; may be pruritic. Uncommonly,
tender regional lymphadenitis.
Skin Lesions
Papule or pustule confined to
the ostium of the hair follicle,
at times surrounded by an erythematous
halo (Figs. 32-27, 32-
28). Rupture of pustule leads
to superficial erosions or crusts.
Scattered discrete or more frequently
grouped and clustered.
Usually, only a small percentage
of follicles in a region is
infected.
In chronic folliculitis, a full range of lesions is
noted.
Pseudofolliculitis barbae caused by penetration
of the skin by sharp tips of shaved
hairs frequently complicated by S. aureus
secondary infection (see Fig. 32-24).
Distribution Face S. aureus . Gram-negative
folliculitis: resembles or may coexist with acne
vulgaris. Molluscum contagiosum. Demodicidosis
resembles rosacea.
Beard Area S. aureus folliculitis: folliculitis
(sycosis) barbae, most commonly of
shaved beard area Dermatophytic folliculitis:
tinea barbae; papulopustules may coalesce to
deeply infiltrated kerion. Herpes
simplex virus. Molluscum contagiosum.
Demodicidosis resembles
rosacea.
Scalp S. aureus . Dermatophytic.
Neck S. aureus in shaved area and
nape of neck, occipital scalp, especially
in diabetics. Pseudofolliculitis
in shaved area. Keloidal folliculitis
in nape of neck; follicular keloids
to large nodulartumorous keloidal
masses. (see page 986)
Legs Occurs in women who shave
legs. In India, a chronic folliculitis
occurs in young men, lasting for
years. Pustular dermatitis atrophicans
of the legs reported commonly
from West Africa, usually affecting
the shins, sometimes the thighs and
forearms.
Trunk S. aureus in axillae, especially
in those who shave. Pseudomonas
aeruginosa (hot tub) folliculitis
(Fig. 32-30). Malassezia folliculitis.
Candida folliculitis on the back of
hospitalized patients with fever who
lie in supine position.
Buttocks Common site for S. aureus
folliculitis. Dermatophytic.
Variants
S. aureus Folliculitis Can be either
superficial folliculitis (infundibular)
(Fig. 32-27) or deep (sycosis)
(extension beneath infundibulum)
with abscess formation (Figs. 32-28,
32-29). In the shaved beard area,
also known as sycosis vulgaris, or
barbers itch. In severe cases (lupoid
sycosis), the pilosebaceous units may
be destroyed and replaced by fibrous
scar tissue.
Gram-Negative Folliculitis Occurs in individuals
with acne vulgaris treated with oral antibiotics.
Acne typically worsens, having been in
good control. Characterized by small follicular
pustules and/or larger abscesses on the cheeks.
Hot Tub Folliculitis Occurs on the trunk following
immersion in spa water (Fig. 32-30).
Dermatophytic Folliculitis Infection begins
in the perifollicular stratum corneum and
spreads into follicular ostia and hair shafts
(see Section 25). (Fig. 32-31)
Tinea Capitis (see Section 25
In dermatophytic Majocchi granuloma, scattered
papules, pustules and nodules, usually
associated with tinea cruris or tinea corporis.
Malassezia Folliculitis More common in subtropical
and tropical climates. Pruritic, monomorphic
eruption characterized by follicular
papules and pustules on the trunk, most often
on the back (Fig. 32-32), upper arms, and less
often on the neck and face; excoriated papules.
Absence of comedones differentiates it from
acne vulgaris (see Section 25). Synonym : Pityrosporum
folliculitis.
Candida albicans Occurs in sites of occluded
skin such as the back of a hospitalized febrile
patient or under plastic dressing, especially if
topical glucocorticoid preparations are used.
Large follicular pustules (see Section 25).
Herpetic Folliculitis Occurs predominantly in
the beard area (viral sycosis) in men. Characterized
by follicular vesicles and later crusts
(Fig. 32-33).
Molluscum Folliculitis Presents as umbilicated
skin-colored papules in a follicular and perifollicular
distribution over the beard area.
Syphilitic (Luetic) Folliculitis: Secondary
Nonscarring alopecia of the scalp and beard
(alopecia areolaris); moth-eaten appearance.
Synonym : Alopecia syphilitica.
Demodicidosis Clinical presentation: perifollicular
scaling (pityriasis folliculorum or rosacea-
like erythematous follicular papules and
pustules with a background of erythema on the
face. Etiology: Demodex folliculorum .
DIFFERENTIAL DIAGNOSIS
Follicular Inflammatory Disorders Acneiform
disorders (acne vulgaris, rosacea, perioral dermatitis),
HIV-associated eosinophilic folliculitis,
chemical irritants (chloracne), acneiform
adverse cutaneous drug reactions [epidermal
growth factor receptor inhibitors (e.g., erlotinib),
halogens, glucocorticoids, lithium], keloidal folliculitis,
pseudofolliculitis barbae.
Regional Differential Diagnosis Face : acne,
rosacea, perioral dermatitis, keratosis pilaris,
pseudofolliculitis barbae (ingrowing hairs).
Scalp : folliculitis necrotica. Trunk : acne vulgaris,
pustular miliaria, transient acantholytic
disease (Grover disease). Axillae and groins :
hidradenitis suppurativa.
LABORATORY FINDINGS
Direct Microscopy Gram Stain S. aureus:
gram-positive cocci. Also visualizes fungi.
KOH Preparation Dermatophytes: hyphae,
spores. M. furfur : multiple yeast forms; Candida
: mycelial forms.
Culture Bacterial S. aureus, P. aeruginosa ;
gram-negative folliculitis: Proteus, Klebsiella,
Escherichia coli . In cases of chronic relapsing
folliculitis, culture nares and perianal region for
S. aureus carriage.
Fungal Dermatophytes; C. albicans .
Viral Herpes simplex virus (HSV).
Dermatopathology The following features
should be evaluated: Are microorganisms
present? Is the inflammatory infiltrate predominantly
follicular or perifollicular? What region
of the pilosebaceous structure is involved? Is
the inflammatory process acute suppurative
(neutrophilic), chronic lymphocytic, or granulomatous
(foreign-body response to keratin
subsequent to rupture of follicle)? Is any portion
of the pilosebaceous structure destroyed?
DIAGNOSIS
Clinical findings confirmed by laboratory findings.
COURSE AND PROGNOSIS
S. aureus folliculitis can progress to deeper
follicular and perifollicular infection with
abscess (furuncle, carbuncle) or cellulitis.
Infection of multiple contiguous follicles
results in a carbuncle.
Many types of infectious folliculitis tend to
recur or become chronic unless the predisposing
conditions are corrected.
MANAGEMENT
Prophylaxis Correct underlying predisposing
condition . Washing with antibacterial soap or
benzoyl peroxide preparation or isopropyl/ethanol
gel.
Antimicrobial Therapy Bacterial Folliculitis
See Table 24-2.
Gram-negative Folliculitis Associated with
systemic antibiotic therapy of acne vulgaris.
Discontinue current antibiotics. Wash with
benzoyl peroxide. In some cases, ampicillin
(250 mg four times daily) or trimethoprim-sulfamethoxazole
four times daily. Isotretinoin.
Fungal Folliculitis Various topical antifungal
agents. For dermatophytic folliculitis: terbinafine,
250 mg PO for 14 days, or itraconazole,
100 mg twice daily for 14 days. For Candida
folliculitis: fluconazole or itraconazole, 100 mg
twice daily for 14 days.
Herpetic Folliculitis See Herpes Simplex Virus
Infections (Section 27).
Demodicidosis Permethrin cream. Ivermectin,
200 g/kg (usual range, 1218 mg) stat.
Pseudofolliculitis Barbae Rule out secondary
S. aureus infection. Discontinue shaving.
Use beard clipper instead of safety razor.
Destruction of hair follicle: electrolysis; laser
hair removal.
Anda mungkin juga menyukai
- Checklist Suhu Apotek Puskesmas Kelurahan Joglo Ii: BulanDokumen3 halamanChecklist Suhu Apotek Puskesmas Kelurahan Joglo Ii: BulanSandy GunawanBelum ada peringkat
- Dyslipidemia ATP4 GUIDLINESDokumen9 halamanDyslipidemia ATP4 GUIDLINESSandy GunawanBelum ada peringkat
- Diretrizes Européias para DislipidemiaDokumen50 halamanDiretrizes Européias para DislipidemiaEno FilhoBelum ada peringkat
- Hepti Muliyati, Aminuddin Syam, Saifuddin Sirajuddin: Artikel PenelitianDokumen7 halamanHepti Muliyati, Aminuddin Syam, Saifuddin Sirajuddin: Artikel PenelitianHermansyah ChiuBelum ada peringkat
- Daftar Pustaka KeratitisDokumen1 halamanDaftar Pustaka KeratitisSandy GunawanBelum ada peringkat
- ATP III Guideline KolesterolDokumen6 halamanATP III Guideline KolesterolRakasiwi GalihBelum ada peringkat
- JNC 8.pdf - Hypertension GuideDokumen14 halamanJNC 8.pdf - Hypertension GuideFeliDokterBelum ada peringkat
- AdhdDokumen9 halamanAdhdSandy GunawanBelum ada peringkat
- Classification of Topical Corticosteroids (WHO)Dokumen2 halamanClassification of Topical Corticosteroids (WHO)Sandy GunawanBelum ada peringkat
- BB TB Ada HubungaDokumen6 halamanBB TB Ada HubungaSandy GunawanBelum ada peringkat
- Yovita Levina - English Task 201350220Dokumen3 halamanYovita Levina - English Task 201350220Sandy GunawanBelum ada peringkat
- TP Tinggi BadanDokumen1 halamanTP Tinggi BadanSandy GunawanBelum ada peringkat
- AMU95AP User GuideDokumen9 halamanAMU95AP User GuideSandy GunawanBelum ada peringkat
- Daftar Pustaka Ophthalmic Drug ReferencesDokumen1 halamanDaftar Pustaka Ophthalmic Drug ReferencesSandy GunawanBelum ada peringkat
- Dosis Obat Epilepsi Anak DewasaDokumen3 halamanDosis Obat Epilepsi Anak DewasaSandy GunawanBelum ada peringkat
- American College of Rheumatology's Eleven Criteria for Diagnosing LupusDokumen1 halamanAmerican College of Rheumatology's Eleven Criteria for Diagnosing LupusSandy GunawanBelum ada peringkat
- Tumbuh Kembang AnakDokumen10 halamanTumbuh Kembang AnakSandy GunawanBelum ada peringkat
- Antibiotik Florokuinolon Topikal MataDokumen7 halamanAntibiotik Florokuinolon Topikal MataSandy GunawanBelum ada peringkat
- American College of Rheumatology's Eleven Criteria for Diagnosing LupusDokumen1 halamanAmerican College of Rheumatology's Eleven Criteria for Diagnosing LupusSandy GunawanBelum ada peringkat
- WFA Girls 0 13 PercentilesDokumen1 halamanWFA Girls 0 13 PercentilesSandy GunawanBelum ada peringkat
- Pediatric Vital SignsDokumen2 halamanPediatric Vital SignsSandy GunawanBelum ada peringkat
- Renal FunctiionDokumen1 halamanRenal FunctiionSandy GunawanBelum ada peringkat
- Menstrual Blood ProblemsDokumen4 halamanMenstrual Blood ProblemsSandy GunawanBelum ada peringkat
- Class Description: Asa ClassificationDokumen1 halamanClass Description: Asa ClassificationSandy GunawanBelum ada peringkat
- Efek Stroke Pada OtakDokumen2 halamanEfek Stroke Pada OtakSandy GunawanBelum ada peringkat
- DementiaDokumen18 halamanDementiaSandy GunawanBelum ada peringkat
- Efek Stroke Pada OtakDokumen2 halamanEfek Stroke Pada OtakSandy GunawanBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- MisoprostolDokumen3 halamanMisoprostolMichael Aditya LesmanaBelum ada peringkat
- Critical Care-Sepsis Case StudyDokumen25 halamanCritical Care-Sepsis Case Studyapi-378305067Belum ada peringkat
- Assam Tea Gardens Cachar, Burtoll T.E. Commissionerate of Labour, Government of Assam Plantation Association name: TAIBVBDokumen4 halamanAssam Tea Gardens Cachar, Burtoll T.E. Commissionerate of Labour, Government of Assam Plantation Association name: TAIBVBAvijitSinharoyBelum ada peringkat
- Gingival Retraction in Fixed Dental ProsthesisDokumen15 halamanGingival Retraction in Fixed Dental ProsthesisSeena Sam100% (2)
- Dermato CHDokumen10 halamanDermato CHSuthan KaveriBelum ada peringkat
- Family Nursing Care Plan Proper Cigarette Smoking As Health ThreatDokumen2 halamanFamily Nursing Care Plan Proper Cigarette Smoking As Health ThreatWishley Ann PiñedaBelum ada peringkat
- Mind-Body Skills For Regulating The Autonomic Nervous SystemDokumen60 halamanMind-Body Skills For Regulating The Autonomic Nervous Systemnorociel8132100% (4)
- Finishing & CementationDokumen20 halamanFinishing & Cementationiin revient29Belum ada peringkat
- Nursing Ethics: Raymund Christopher R. Dela Peña, RN, RMDokumen23 halamanNursing Ethics: Raymund Christopher R. Dela Peña, RN, RMrnrmmanphd100% (1)
- TylenolDokumen2 halamanTylenolAle_deCastroBelum ada peringkat
- Common TestsDokumen8 halamanCommon Testsapi-84383303Belum ada peringkat
- What Is First Aid? A Simple: Definition 1Dokumen3 halamanWhat Is First Aid? A Simple: Definition 1Robert D.PalbanBelum ada peringkat
- Neuromuscular QuestionsDokumen9 halamanNeuromuscular QuestionsLily JenBelum ada peringkat
- Dialysis Center Software FromDokumen18 halamanDialysis Center Software FromAmit jain100% (1)
- Fulminant Hepatic FailureDokumen53 halamanFulminant Hepatic FailureAR KarthickBelum ada peringkat
- Role of pharmacists beyond drug salesDokumen3 halamanRole of pharmacists beyond drug salesAlrick AsentistaBelum ada peringkat
- Acute PancreatitisDokumen23 halamanAcute PancreatitisGel Torres Galvez50% (2)
- Chatterjee, A., & Coslett, H.B. (Eds.) (2014) - The Roots of Cognitive Neuroscience. Behavioral Neurology and Neuropsychology. Oxford University Press PDFDokumen431 halamanChatterjee, A., & Coslett, H.B. (Eds.) (2014) - The Roots of Cognitive Neuroscience. Behavioral Neurology and Neuropsychology. Oxford University Press PDFReg A. Derah100% (1)
- CT venography reliability vs DSADokumen7 halamanCT venography reliability vs DSAwan hanisaBelum ada peringkat
- Campbell 10 Edition:: Renal Cyst Disease: Indication, Procedure and ResultsDokumen13 halamanCampbell 10 Edition:: Renal Cyst Disease: Indication, Procedure and ResultsAkmal FawziBelum ada peringkat
- Concept Map Epidural AbcessDokumen11 halamanConcept Map Epidural Abcessapi-593859653Belum ada peringkat
- Impaired Skin Integrity Related To Excess Fluids Volume As Evidenced by Swelling of The Lower ExtremitiesDokumen2 halamanImpaired Skin Integrity Related To Excess Fluids Volume As Evidenced by Swelling of The Lower ExtremitiesLevin MenpinBelum ada peringkat
- Nursing Assignments GuideDokumen54 halamanNursing Assignments GuideEya CamillerBelum ada peringkat
- Principles of Practice For Pharmaceutical CareDokumen29 halamanPrinciples of Practice For Pharmaceutical CareNgetwa TzDe TheWirymanBelum ada peringkat
- Spontaneous Regression of Sequestrated Lumbar Disc Herniations - 2014Dokumen6 halamanSpontaneous Regression of Sequestrated Lumbar Disc Herniations - 2014SNBelum ada peringkat
- Family Health Care Gold BrochureDokumen15 halamanFamily Health Care Gold BrochureYASH JAISINGBelum ada peringkat
- Functional Crown Lengthening Surgery Periodontic and Prosthodontic ConsiderationsDokumen5 halamanFunctional Crown Lengthening Surgery Periodontic and Prosthodontic ConsiderationsNajeeb UllahBelum ada peringkat
- Anesth Essays ResDokumen8 halamanAnesth Essays ResFi NoBelum ada peringkat
- Surgical Site Infections and Hand Hygiene Discharge TeachingDokumen36 halamanSurgical Site Infections and Hand Hygiene Discharge TeachingKhzBelum ada peringkat
- Physical Assessment Answer 16 PrintedDokumen3 halamanPhysical Assessment Answer 16 PrintedJune Dumdumaya100% (2)