Laboratory Exams
Diunggah oleh
zerpthederpHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Laboratory Exams
Diunggah oleh
zerpthederpHak Cipta:
Format Tersedia
LABORATORY EXAMS
CHEST X-RAY
J une 22, 2014
No previous film provided for comparison.
There is haziness in the right lower lung field with air bronchograms.
Homogenous meniscal densities are seen in both lower lung fields obscuring the
hemidiaphragms and costophrenic angles. A band of homogenous density is also seen outlining
the periphery of the left hemithorax. The mediastinum is widened with lobular outline. There is
increased perihilar and paracardiac haziness in the intercostal space. The rest of the osseous
and soft tissue structures are unremarkable.
Impression:
1) BILATERAL PNEUMONIA WITH CONSOLIDATION ON THE RIGHT LOWER LUNG
FIELD
2) BILATERAL PLEURAL EFFUSION
3) MEDIASTINAL MASS. SUGGEST CLINICAL AND CT SCAN CORRELATION
4) LEFT CTT IN PLACE
J une 30, 2014
There is an area devoid of lung markings with air fluid leviel in the left superior mediastinum.
The mediastinal width has decreased in size. Homogenous meniscal densities are seen in the
right mid and both lower lung fields obscuring the hemidiaphragms and costophrenic angles.
The trachea is midline. A CTT is seen in the let with its tip at the level of the 10
th
posterior rib.
The rest of the osseious and soft tissue structures are unremarkable.
Impression:
1) BILARERAL PLEURAL EFFUSION
2) MEDIASTINAL MASS WITH INTERVAL DECREASE IN SIZE
3) LOCULATED PNEUMOHYDROTHORAX
4) FOLLOW-UP STUDY IS SUGGESTED.
August 25, 2014
Shows homogenous densities in the right lower lung field with blunting of the right costophrenic
angle. The right thoracotomy tube is again seen with its tip still directed caudally. The rest of the
findings are unchanged.
Impression:
1) BILATERAL PLEURAL EFFUSSION
2) MEDIASTIANL MASS --- UNCHANGED SINCE 8/25/14
3) PNEUMONIA, LEFT
4) LOCULATED PNEUMOHYDROTHORAX IN THE LEFT APICAL REGION IS STILL
CONSIDERED
URINALYSIS REPORT
MACROSCOPIC 09/12/14 SIGNIFICANCE
COLOR DARK YELLOW
APPEARANCE SLIGHTLY CLOUDY
GLUCOSE NEGATIVE
PROTEIN NEGATIVE
pH 7.0
SPECIFIC GRAVITY 1.010
BILIRUBIN NEGATIVE
UROBILINOGEN + = 2 mg/dL
KETONE NEGATIVE
NITRITE NEGATIVE
LEUKOCYTES TRACE
BLOOD NEGATIVE
URINE FLOWCTOMETRY
PUS CELLS 22.5 /uL
RED CELLS 2.0 /uL
EPITHELIAL CELLS 10.1 /uL
BACTERIA 6.1 /uL
CAST 0.13 /uL
COMPLETE BLOOD COUNT
LABORATORY
EXAM
09/13/14 09/14/14 09/17/14 09/18/14 09/19/14 09/20/14 UNIT RANGE
WBC 0.78 0.72 4.07 3.70 7.04 11.34 x10^9/L 4.10-
10.9
Neutrophils 15 13 28 30 12 11 % 47.0-
80.0
Lymphocytes 76 79 62 54 74 76 % 13.0-
40.0
Monocytes 9 7 6 10 12 11 % 2.00-
11.0
Eosinophils 0 0 0 1 0 0 % 0.00-
5.00
Basophils 0 1 4 3 1 0 % 0.00-
2.00
HEMOGLOBIN 12.2 12.5 18.7 15.6 17.0 17.3 g/Dl 12.0-
16.0
HEMATOCRIT 36.4 35.3 52.9 44.1 51.0 52.0 % 36.0-
46.0
RBC 4.6 4.6 6.8 5.6 6.5 6.7 10^12/L 4.50-
5.90
MCV 79.1 79.1 77.9 76.8 78.5 77.6 fL 80.0-
100.0
MCH 26.6 26.6 27.8 27.9 26.2 25.8 Pg 26.0-
34.0
MCHC 34 34 36 36 33.3 33.2 g/L 31.0-
36.0
RCDW 11.2 11.2 12.9 12.7 12.5 12.5 % 11.6-
14.8
PLATELET
COUNT
48 32 3 62 38 39 x10^9/L 140.0-
440.0
MEAN
PLATELET
VOLUME
4.05 5.12 ---- 5.08 4.74 10.23 fL 0.00-
100.0
CBC SIGNIFICANCE
TEST INCREASED DECREASED
WBC Lekocytosis; Infection,
inflammation, Leukemia, or
myeloproliferative disorders
Leukopenia may be caused
by a lymphoma or other
cancer that spread to the
bone marrow
Neutrophils Neutrophilia; inflammation or
certain leukemias
Neutropenia;
immunodeficiency, bone
marrow damage caused by
chemotherapy and radiation
therapy or cancer that
spreads to the bone marrow
Lymphocytes Lymphocytosis; may be due to
lymphocytic leukemia
Lymphocytopenia; bone
marrow damage caused by
chemotherapy and radiation
therapy; corticosteroids
Monocytes May be due to monocytic or
myelomonocytic leukemia
(acute or chronic)
Repeated low counts can
indicate bone marrow damage
or failure
Eosinophils Numbers are normally low in
the blood. One or an
occasional low number is
usually not medically
significant
May be due to leukemia
Basophils Numbers are normally low in
the blood. One or an
occasional low number is
usually not medically
significant
May be due to leukemia
RBC Anemia; May be due to bone
marrow disorder or damage
HEMATOCRIT Usually mirrors RBC results Usually mirrors RBC results;
most common cause is
dehydration
HEMOGLOBIN Usually mirrors RBC results Usually mirrors RBC results
MCV Macrocytic; may be cause by
vitamin B12 or folate deficincy
Microcytic; may cause by iron
deficiency anemia or
thalassemias
MCH Mirrors MCV results;
macrocytic RBCs are large so
tend to have a higher MCH.
Mirrors MCV results; small red
cells would have a lower
value.
MCHC Increased MCHC values
(hyperchromia) are seen in
conditions where the
hemoglobin is more
concentrated inside the red
cells, such as autoimmune
hemolytic anemia, in burn
patients, and hereditary
spherocytosis, a rare
congenital disorder.
May be low when MCV is low;
decreased MCHC values
(hypochromia) are seen in
conditions such as iron
deficiency anemia and
thalassemia
RCDW Indicates mixed population of
small and large RBCs;
immature RBCs tend to be
larger. For example, in iron
deficiency anemia or
pernicious anemia, there is
high variation (anisocytosis) in
RBC size (along with variation
in shape poikilocytosis),
causing an increase in the
RCDW.
Low value indicates uniformity
in size of RBCs
PLATELET COUNT Thrombocytotsis; may be due
to cancer
Thrombocytopenia; may be
due to leukemia,
chemotherapy or radiation
therapy
MEAN PLATELET VOLUME Indicates a high number of
larger, younger platelets in the
blood; this may be due to the
bone marrow producing and
releasing platelets rapidly into
circulation
Indicates average size of
platelets is small; older
platelets are generally smaller
than younger ones and a low
MPV may mean that a
condition is affecting the
production of platelets by the
bone marrow
SERUM LABORATORY EXAMS
EXAMINATION RESULT UNIT NORMAL
VALUE
SIGNIFICANCE
09/11/14
CREATININE
(SERUM)
0.56 mg/dL 0.60-1.50
SGPT 89.00 U/L 12-78
09/18/14
POTASSIUM
(SERUM)
3.20 mmol/L 3.4-5.2
ALBUMIN
(SERUM)
23.34 g/L 35.0-50.0
09/19/14
CREATININE
(SERUM)
0.77 mg/Dl 0.60-1.50
SGPT 228.0 U/L 12-78
IDEAL LABORATORY AND DIAGNOSTIC EXAMS FOR ALL
How is acute lymphocytic leukemia diagnosed?
Certain signs and symptoms can suggest that a person might have acute lymphocytic leukemia,
but tests are needed to confirm the diagnosis.
Medical history and physical exam
If you have signs and symptoms that suggest you might have leukemia, the doctor will want to
get a thorough medical history, including how long you have had symptoms and if you have any
history of exposure to risk factors.
During the physical exam, the doctor will probably focus on any enlarged lymph nodes, areas of
bleeding or bruising, or possible signs of infection. The eyes, mouth, and skin will be looked at
carefully, and a thorough nervous system exam may be done. Your abdomen will be felt for
signs of an enlarged spleen or liver.
Your doctor may also order tests of your blood cell counts. If the results suggest leukemia, the
doctor may refer you to a hematologist, a doctor who specializes in treating blood disorders
(including blood cancers like leukemia). This doctor may run one or more of the tests described
below.
Tests used to diagnose and classify ALL
If your doctor thinks you have leukemia, he or she will need to check samples of cells from your
blood and bone marrow to be sure of the diagnosis. Other tissue and cell samples may also be
taken to help guide treatment.
Blood tests
Blood samples for ALL tests are generally taken from a vein in the arm.
Complete blood count (CBC) and blood cell exam (peripheral blood smear):The complete
blood count (CBC) measures the numbers of red blood cells, white blood cells, and platelets.
This test is often done along with a differential (or diff) which looks at the numbers of the
different types of white blood cells. These tests are often the first ones done on patients with a
suspected blood problem.
For the peripheral smear, a drop of blood is smeared across a slide and then looked at under a
microscope to see how the cells look. Changes in the numbers and the appearance of the cells
often help diagnose leukemia.
Most patients with ALL have too many immature white cells in their blood, and not enough red
blood cells or platelets. Many of the white blood cells will be lymphoblasts (blasts), which are
immature lymphocytes not normally found in the bloodstream. Lymphoblasts do not function like
normal, mature white blood cells.
Even though these findings may suggest leukemia, the disease usually is not diagnosed without
looking at a sample of bone marrow cells.
Blood chemistry and coagulation tests: Blood chemistry tests measure the amounts of
certain chemicals in the blood, but they are not used to diagnose leukemia. In patients already
known to have ALL, these tests can help detect liver or kidney problems caused by spreading
leukemia cells or the side effects of certain chemotherapy drugs. These tests also help
determine if treatment is needed to correct low or high blood levels of certain minerals.
Blood coagulation tests may also be done to make sure the blood is clotting properly.
Bone marrow tests
Bone marrow aspiration and biopsy: Bone marrow samples are obtained by bone marrow
aspiration and biopsy tests usually done at the same time. The samples are usually taken
from the back of the pelvic (hip) bone, although in some cases they may be taken from the
sternum (breastbone) or other bones.
In bone marrow aspiration, you lie on a table (either on your side or on your belly). After
cleaning the skin over the hip, the doctor numbs the skin and the surface of the bone by
injecting a local anesthetic, which may cause a brief stinging or burning sensation. A thin, hollow
needle is then inserted into the bone and a syringe is used to suck out a small amount of liquid
bone marrow. Even with the anesthetic, most patients still have some brief pain when the
marrow is removed.
A bone marrow biopsy is usually done just after the aspiration. A small piece of bone and
marrow is removed with a slightly larger needle that is twisted as it is pushed down into the
bone. With local anesthetic, most patients just feel some pressure and tugging from the biopsy,
but a few may feel a brief pain. Once the biopsy is done, pressure will be applied to the site to
help prevent bleeding.
These bone marrow tests are used to help diagnose leukemia. They may also be done again
later to tell if the leukemia is responding to treatment.
Routine exams under a microscope: The bone marrow is looked at under a microscope by a
pathologist (a doctor specializing in lab tests) and may be reviewed by the patients
hematologist/oncologist (a doctor specializing in cancer and blood diseases).
The doctors will look at the size, shape, and other traits of the white blood cells in the samples
to classify them into specific types.
A key factor is whether the cells appear mature (look like normal blood cells), or immature
(lacking features of normal blood cells). The most immature cells are called lymphoblasts (or
blasts for short).
Determining what percentage of cells in the bone marrow are blasts is particularly important. A
diagnosis of ALL generally requires that at least 20% to 30% of the cells in the bone marrow are
blasts. Under normal circumstances, blasts are never more than 5% of bone marrow cells.
Sometimes just counting and looking at the cells doesnt provide a definite diagnosis, and other
lab tests are needed.
Cytochemistry: In cytochemistry tests, cells are put on a slide and exposed to chemical stains
(dyes) that react only with some types of leukemia cells. These stains cause color changes that
can be seen under a microscope, which can help the doctor determine what types of cells are
present. For instance, one stain can help distinguish ALL from acute myeloid leukemia (AML).
The stain causes the granules of most AML cells to appear as black spots under the
microscope, but it does not cause ALL cells to change colors.
Flow cytometry and immunohistochemistry: Flow cytometry tests look for certain
substances on the surface of cells that help identify what types of cells they are. A sample of
cells is treated with special antibodies (man-made versions of immune system proteins) that
stick to the cells only if these substances are present on their surfaces. The cells are then
passed in front of a laser beam. If the cells now have antibodies attached to them, the laser will
cause them to give off light, which can be measured and analyzed by a computer. Groups of
cells can be separated and counted by these methods.
In immunohistochemistry tests, cells from the blood or bone marrow samples are also treated
with special antibodies. But instead of using a laser and computer, the sample is treated so that
certain types of cells change color when seen under a microscope.
These tests are used for immunophenotyping classifying leukemia cells according to the
substances (antigens) on their surfaces and so it is very helpful in determining the exact type of
leukemia. Different types of lymphocytes have different antigens on their surfaces. These
antigens also change as each cell matures. Each patients leukemia cells all have the same
antigens because they are all derived from the same cell. Lab testing for antigens is a very
sensitive way to diagnose ALL. Because cells from different subtypes of ALL have different sets
of antigens, this is sometimes helpful in ALL classification, although it is not needed in most
cases.
These tests also can be used to look at the cells from lymph nodes, blood samples, and even
other body fluids (like spinal fluid).
Cytogenetics: For this test, chromosomes (long strands of DNA) from leukemia cells are
looked at under a microscope to detect any changes. Normal human cells contain 23 pairs of
chromosomes, each of which is a certain size and stains a certain way. In some cases of
leukemia, the cells have chromosome changes that can be seen under a microscope.
For instance, 2 chromosomes may swap some of their DNA, so that part of one chromosome
becomes attached to part of a different chromosome. This change, called a translocation, can
usually be seen under a microscope. Recognizing these changes can help identify certain types
of ALL and may be important in determining the outlook for the patient.
Most of the chromosome changes in adult ALL are translocations. The most common one is a
translocation between chromosomes 9 and 22 [often written t(9;22)], which results in a
shortened chromosome 22 (called the Philadelphia chromosome). About 1 out of 4 adults with
ALL have this abnormality in their leukemia cells.
Information about this and other translocations may be useful in predicting a persons response
to treatment. For this reason, most doctors will test all patients with ALL for genetic changes in
the leukemia cells.
Cytogenetic testing usually takes about 2 to 3 weeks because the leukemia cells must grow in
lab dishes for a couple of weeks before their chromosomes can be seen under the microscope.
It is often used for bone marrow samples, but it can also be used with blood samples. An
advantage of cytogenetic testing is that it looks at all of the chromosomes, and the doctor
doesnt have to know in advance what changes to test for.
Not all chromosome changes can be seen under a microscope. Other lab tests can often help
find these changes.
Fluorescent in situ hybridization (FISH): This is another type of chromosome test. It uses
special fluorescent dyes that only attach to specific genes or parts of particular chromosomes.
FISH can find most chromosome changes (such as translocations) that are visible under a
microscope in standard cytogenetic tests, as well as some changes too small to be seen with
usual cytogenetic testing.
FISH can be used on regular blood or bone marrow samples. It can also be used to look at cells
from other tissues, like lymph node samples. It is very accurate and can usually provide results
within a couple of days. But because FISH only tests for certain gene changes (and doesnt look
at the chromosomes overall), it is best for looking for the changes that are important based on
the kind of leukemia a person has.
Polymerase chain reaction (PCR): This is a very sensitive DNA test that can also find certain
gene changes too small to be seen with a microscope, even if very few leukemia cells are
present in a sample. Like FISH, it is used to find particular gene changes and not to look at the
chromosomes overall. It is often used to look for the gene made by the Philadelphia
chromosome.
If the leukemia cells have a particular gene (or chromosome) change, PCR can be used after
treatment to try to find small numbers of leukemia cells that may not be visible with a
microscope.
Lumbar puncture (spinal tap)
This test looks for leukemia cells in the cerebrospinal fluid (CSF), the liquid that surrounds the
brain and spinal cord. ALL can spread to the area around the brain and spinal cord. To check
for this spread, doctors remove a sample of CSF for testing.
The patient may lay on their side or sit up for this test. The doctor first numbs an area in the
lower part of the back over the spine. A small, hollow needle is then placed between the bones
of the spine and into the area around the spinal cord to withdraw some of the fluid.
A lumbar puncture can also be used to put chemotherapy drugs into the CSF to try to prevent or
treat the spread of leukemia to the spinal cord and brain.
Lymph node biopsy
Removing a lymph node or part of a lymph node is often an important procedure when
diagnosing lymphomas, but is only rarely needed with leukemia because the diagnosis can be
made looking at blood and bone marrow.
In this procedure, a surgeon cuts through the skin to remove all or part of a lymph node. If the
node is near the skin surface, this is a simple operation that can often be done with local
anesthesia, but if the node is inside the chest or abdomen, general anesthesia is used to keep
the patient asleep during the biopsy.
When the entire lymph node is removed, it is called an excisional lymph node biopsy. If only part
of the lymph node is removed, it is called an incisional lymph node biopsy.
Imaging tests
Imaging tests use x-rays, sound waves, magnetic fields, or radioactive particles to produce
pictures of the inside of the body. Because leukemia does not usually form tumors, imaging
tests arent as useful as they are for other types of cancer.
Imaging tests might be done in people with ALL, but they are done more often to look for
infections or other problems, rather than for the leukemia itself. In some cases they may be
done to help determine the extent of the disease, if it is thought it may have spread beyond the
bone marrow and blood.
X-rays
Chest x-rays may be done if the doctor suspects a lung infection. They may also be done to
look for enlarged lymph nodes in the chest.
Computed tomography (CT) scan
The CT scan is a type of x-ray test that produces detailed, cross-sectional images of your body.
Unlike a regular x-ray, CT scans can show the detail in soft tissues (such as internal organs).
This test can help tell if any lymph nodes or organs in your body are enlarged. It isnt usually
needed to diagnose ALL, but it may be done if your doctor suspects leukemia cells are growing
in an organ, like your spleen.
Instead of taking one picture, like a regular x-ray, a CT scanner takes many pictures as it rotates
around you. A computer then combines these pictures into detailed images of the part of your
body being studied.
Before the scan, you may be asked to drink a contrast solution and/or get an intravenous (IV)
injection of a contrast dye that helps better outline abnormal areas in the body. You may need
an IV line for injecting the contrast dye. The IV injection of contrast dye can cause a feeling of
flushing or warmth in the face or elsewhere. Some people are allergic and get hives or, rarely,
more serious reactions like trouble breathing and low blood pressure. Be sure to tell the doctor if
you have any allergies or have ever had a reaction to any contrast material used for x-rays.
A CT scanner has been described as a large donut, with a narrow table in the middle opening.
You will need to lie still on the table while the scan is being done. CT scans take longer than
regular x-rays, and you might feel a bit confined by the ring while the pictures are being taken.
In some cases, a CT can be used to guide a biopsy needle precisely into a suspected
abnormality, such as an abscess. For this procedure, called a CT-guided needle biopsy, you
stay on the CT scanning table while a radiologist moves a biopsy needle through the skin and
toward the mass. CT scans are repeated until the needle is within the mass. A biopsy sample is
then removed to be looked at under a microscope.
Sometimes a test that combines the CT scan with a PET (positron emission tomography) scan
(PET/CT scan) is done. For a PET scan, a form of radioactive sugar (known
as fluorodeoxyglucose or FDG) is injected into the blood. The amount of radioactivity used is
low. Because cancer cells in the body grow rapidly, they absorb large amounts of the sugar. A
special camera can then create a picture of areas of radioactivity in the body. The PET/CT scan
lets the doctor compare areas of higher radioactivity on the PET scan with the more detailed
appearance of that area on the CT. This is not often needed for patients with ALL.
Magnetic resonance imaging (MRI) scan
Like CT scans, MRI scans provide detailed images of soft tissues in the body. But MRI scans
use radio waves and strong magnets instead of x-rays. The energy from the radio waves is
absorbed by the body and then released in a pattern formed by the type of body tissue and by
certain diseases. A computer translates the pattern into a very detailed image of parts of the
body. A contrast material called gadolinium is often injected into a vein before the scan to better
see details. This contrast material is different from the one used for CT scans.
MRI scans are very helpful in looking at the brain and spinal cord.
MRI scans take longer than CT scans often up to an hour. You may have to lie inside a
narrow tube, which is confining and can be distressing to some people. Newer, more open MRI
machines may be another option. The MRI machine makes loud buzzing and clicking noises
that you may find disturbing. Some places provide headphones or earplugs to help block this
noise out.
Ultrasound
Ultrasound uses sound waves and their echoes to produce a picture of internal organs or
masses. For this test, a small, microphone-like instrument called a transducer is placed on the
skin (which is first lubricated with gel). The transducer emits sound waves and picks up the
echoes as they bounce off the organs. A computer converts the echoes into an image that is
displayed on a computer screen.
Ultrasound can be used to look at lymph nodes near the surface of the body or to look for
enlarged organs inside your abdomen such as the kidneys, liver, and spleen.
This is an easy test to have, and it uses no radiation. For most ultrasounds, you simply lie on a
table, and a technician moves the transducer over the part of your body being looked at.
Gallium scan and bone scan
These tests are not often done for ALL, but they may be useful if you have bone pain that might
be caused by either an infection or cancer in the bones.
For these tests, the doctor or nurse injects a slightly radioactive chemical, which collects in
areas of cancer or infection in the body, into the bloodstream,. These areas can then be seen
with a special type of camera. The images from these scans are seen as hot spots in the body,
but they dont provide much detail. If an area lights up on the scan, other imaging tests such as
x-rays, CTs, or MRIs may be done to get a more detailed look at the area. If leukemia is a
possibility, a biopsy of the area may be needed to confirm this.
Source: cancerorg.com
Anda mungkin juga menyukai
- CYSTOCLYSISDokumen1 halamanCYSTOCLYSISzerpthederpBelum ada peringkat
- Rheumatic Heart DiseaseDokumen5 halamanRheumatic Heart DiseasezerpthederpBelum ada peringkat
- Grand Case Study 2Dokumen2 halamanGrand Case Study 2zerpthederpBelum ada peringkat
- Psychiatric Nursing Bullets (Nle & Nclex)Dokumen21 halamanPsychiatric Nursing Bullets (Nle & Nclex)Richard Ines Valino100% (24)
- Requirements For Perpetual Succour Hospital PGNTDokumen1 halamanRequirements For Perpetual Succour Hospital PGNTzerpthederpBelum ada peringkat
- Session 4: Main SymptomsDokumen86 halamanSession 4: Main SymptomszerpthederpBelum ada peringkat
- Drug StudyDokumen3 halamanDrug Studyudntnid2knwme100% (4)
- Feature StoriesDokumen1 halamanFeature StorieszerpthederpBelum ada peringkat
- Case Study of A Patient With Ischemic CardiomyopathyDokumen33 halamanCase Study of A Patient With Ischemic Cardiomyopathyromeo rivera80% (5)
- Drusadg Study For Paracetamol Omeprazole and Vitamin B ComplexDokumen3 halamanDrusadg Study For Paracetamol Omeprazole and Vitamin B ComplexzerpthederpBelum ada peringkat
- Compilation OF Case Studies: Perpetual Succour Hospital Gorordo Ave., Lahug, Cebu City Nursing Service DepartmentDokumen1 halamanCompilation OF Case Studies: Perpetual Succour Hospital Gorordo Ave., Lahug, Cebu City Nursing Service DepartmentzerpthederpBelum ada peringkat
- Grand Cassade Study 1Dokumen15 halamanGrand Cassade Study 1zerpthederpBelum ada peringkat
- Foetal CirculationDokumen8 halamanFoetal CirculationMujahid_Dean_8976Belum ada peringkat
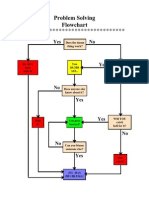
- Problem Solving Flowchart: Yes NoDokumen1 halamanProblem Solving Flowchart: Yes NozerpthederpBelum ada peringkat
- When in Rome PDFDokumen120 halamanWhen in Rome PDFzerpthederpBelum ada peringkat
- Identifying Our Own ProblemsDokumen8 halamanIdentifying Our Own ProblemszerpthederpBelum ada peringkat
- CokeDokumen3 halamanCokezerpthederpBelum ada peringkat
- Community Needs AssessmentDokumen13 halamanCommunity Needs Assessmentzerpthederp0% (1)
- 12 Literary Compositions That Have Influenced The WorldDokumen3 halaman12 Literary Compositions That Have Influenced The Worldzerpthederp100% (6)
- Welcome AddressDokumen1 halamanWelcome AddresszerpthederpBelum ada peringkat
- Bohol SUPREME STUDENT GOV'T Liquidation ReportDokumen1 halamanBohol SUPREME STUDENT GOV'T Liquidation ReportzerpthederpBelum ada peringkat
- NMAT ID Form-1111302389Dokumen1 halamanNMAT ID Form-1111302389zerpthederpBelum ada peringkat
- UlcerDokumen3 halamanUlcerAjay SathyanBelum ada peringkat
- UBCN Nursing Event SponsorshipDokumen3 halamanUBCN Nursing Event SponsorshipzerpthederpBelum ada peringkat
- TOPICDokumen1 halamanTOPICzerpthederpBelum ada peringkat
- UBCN Nursing Staff Event SponsorshipDokumen2 halamanUBCN Nursing Staff Event SponsorshipzerpthederpBelum ada peringkat
- CIM Application Form 1Dokumen1 halamanCIM Application Form 1Kara AguilarBelum ada peringkat
- Dengue Fever Case StudyDokumen24 halamanDengue Fever Case Studymaemaeyee95% (22)
- Session 4: Main SymptomsDokumen86 halamanSession 4: Main SymptomszerpthederpBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Loan PredictionDokumen3 halamanLoan PredictionShreyansh JainBelum ada peringkat
- Problem Set 1 CirclesDokumen2 halamanProblem Set 1 Circlesapi-339611548100% (1)
- TRL External CommunicationDokumen3 halamanTRL External CommunicationAyushGargBelum ada peringkat
- MC0081Dokumen385 halamanMC0081Purushottam KumarBelum ada peringkat
- Catalogo Carbones Helwig GDE-006Dokumen17 halamanCatalogo Carbones Helwig GDE-006Sergio HernandezBelum ada peringkat
- WCS1400 / WCS1400S: FeaturesDokumen7 halamanWCS1400 / WCS1400S: FeaturesbahrowiadiBelum ada peringkat
- Science8 Q2 Module3 (Week6)Dokumen30 halamanScience8 Q2 Module3 (Week6)Mary Grace Lemon100% (1)
- Hargreaves 2007Dokumen15 halamanHargreaves 2007Sam GonçalvesBelum ada peringkat
- Ductile deformation finite strain analysisDokumen27 halamanDuctile deformation finite strain analysisJorgeBarriosMurielBelum ada peringkat
- Is 14416 1996Dokumen20 halamanIs 14416 1996kaustavBelum ada peringkat
- Eng Grammar Book 8Dokumen77 halamanEng Grammar Book 8ЖАНСАЯ Сейдахмет50% (2)
- Manuscript 123Dokumen46 halamanManuscript 123Datuzuharto Sultan100% (1)
- Hospital Managemen T System: Oose LAB FileDokumen62 halamanHospital Managemen T System: Oose LAB FileAASHBelum ada peringkat
- 9 CE AmplifierDokumen5 halaman9 CE AmplifierAnsh PratapBelum ada peringkat
- Fiziks: Basic Properties and Tools of ThermodynamicsDokumen28 halamanFiziks: Basic Properties and Tools of ThermodynamicsSURAJ PRATAP SINGHBelum ada peringkat
- Formulas For Thermodynamics 1Dokumen2 halamanFormulas For Thermodynamics 1Stefani Ann CabalzaBelum ada peringkat
- Testing of Semifinished Products of Thermoplastics Bases - Indications Directive DVS 2201-1Dokumen4 halamanTesting of Semifinished Products of Thermoplastics Bases - Indications Directive DVS 2201-1OscarBelum ada peringkat
- Unit 6 - Quantitative Analysis NotesDokumen53 halamanUnit 6 - Quantitative Analysis Notesapi-182809945Belum ada peringkat
- QAP - LT Panel PDFDokumen8 halamanQAP - LT Panel PDFAkshay Ajay100% (2)
- Daikin RXS-K - Technical DataDokumen21 halamanDaikin RXS-K - Technical DataPrestoneKBelum ada peringkat
- Composition, Thermal and Rheological Behaviour of Selected Greek HoneysDokumen13 halamanComposition, Thermal and Rheological Behaviour of Selected Greek HoneyssyazaqilahBelum ada peringkat
- Signal Circuit LessonDokumen1 halamanSignal Circuit Lessonapi-208557858Belum ada peringkat
- Wound ScaleDokumen4 halamanWound ScaleHumam SyriaBelum ada peringkat
- Chapter 1: Introduction: 1.1 Background TheoryDokumen36 halamanChapter 1: Introduction: 1.1 Background TheoryBe-fit Be-strongBelum ada peringkat
- Methodology of Event StudiesDokumen4 halamanMethodology of Event Studieshaichellam5577Belum ada peringkat
- CSEC-Chemistry-p2 May-June 2012 PDFDokumen20 halamanCSEC-Chemistry-p2 May-June 2012 PDFdela250% (4)
- Final Project Regenerative BrakingDokumen6 halamanFinal Project Regenerative Brakingdims irifiyinBelum ada peringkat
- Woodward MFR 13Dokumen91 halamanWoodward MFR 13OryaBelum ada peringkat
- AC axial compact fan technical specificationsDokumen5 halamanAC axial compact fan technical specificationsdhanasekhar27Belum ada peringkat
- Er DiagramsDokumen20 halamanEr DiagramsMatthew BloomfieldBelum ada peringkat