1 s2.0 S1356689X13000751 Main PDF
Diunggah oleh
ubiktrash14920 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
32 tayangan5 halamanPhysiotherapists should be proactive in preparing themselves to participate in innovative models of health care, which are emerging from healthcare workforce reforms in Australia. A targeted literature review was undertaken through EBSCO Host, cochrane, Medline, sportsdiscus, cinahl, Healthsource and Google.com. Themes included the need for standard National action in relation to legislative and regulatory / registration issues, appropriate education, credentialing and supervisory requirements for physiotherapy prescrib
Deskripsi Asli:
Judul Asli
1-s2.0-S1356689X13000751-main.pdf
Hak Cipta
© © All Rights Reserved
Format Tersedia
PDF, TXT atau baca online dari Scribd
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniPhysiotherapists should be proactive in preparing themselves to participate in innovative models of health care, which are emerging from healthcare workforce reforms in Australia. A targeted literature review was undertaken through EBSCO Host, cochrane, Medline, sportsdiscus, cinahl, Healthsource and Google.com. Themes included the need for standard National action in relation to legislative and regulatory / registration issues, appropriate education, credentialing and supervisory requirements for physiotherapy prescrib
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PDF, TXT atau baca online dari Scribd
0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
32 tayangan5 halaman1 s2.0 S1356689X13000751 Main PDF
Diunggah oleh
ubiktrash1492Physiotherapists should be proactive in preparing themselves to participate in innovative models of health care, which are emerging from healthcare workforce reforms in Australia. A targeted literature review was undertaken through EBSCO Host, cochrane, Medline, sportsdiscus, cinahl, Healthsource and Google.com. Themes included the need for standard National action in relation to legislative and regulatory / registration issues, appropriate education, credentialing and supervisory requirements for physiotherapy prescrib
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PDF, TXT atau baca online dari Scribd
Anda di halaman 1dari 5
Professional issue
Non-medical prescribing by physiotherapists: Issues reported in the
current evidence
Joanne H. Morris
a,
*
, Karen Grimmer
b
a
ACT Health Directorate, Canberra 2605, Australia
b
International Centre for Allied Health Evidence, (iCAHE), University of South Australia, Australia
a r t i c l e i n f o
Article history:
Received 8 March 2013
Received in revised form
6 April 2013
Accepted 8 April 2013
MeSH keywords:
Physical therapy modalities
Physical therapy specialty
Drug prescriptions
Drug therapy
Primary health care
Medicine
Extended scope physiotherapy
a b s t r a c t
Physiotherapists should be proactive in preparing themselves to participate in innovative models of
health care, which are emerging from the healthcare workforce reforms in Australia. One challenging
outcome of workforce change is physiotherapy (non-medical) prescribing (NMP), which is part of the
extension of scope of physiotherapy practice. This paper summarises the current evidence base for
Australian physiotherapists seeking to obtain prescribing rights. A targeted literature review was un-
dertaken through EBSCO Host, Cochrane, Medline, SportsDiscus, Cinahl, Healthsource and Google.com
using broad search terms to identify peer-reviewed and grey literature pertaining to NMP by physio-
therapists, nationally and internationally. No critical appraisal was undertaken however literature was
structured into the NHMRC hierarchy of evidence. Themes raised in the included literature were reported
descriptively. There were six relevant peer-reviewed articles, of hierarchy levels III_3 and IV. There was
however, comprehensive and recent grey literature to inform Australian physiotherapy NMP initiatives.
Themes included the need for standard National action in relation to legislative and regulatory/regis-
tration issues, appropriate education, credentialing and supervisory requirements for physiotherapy
prescribing.
Many lessons can be learnt from the literature, including the importance of planned, uniform National
action (rather than piecemeal state-by-state initiatives). Essential elements include appropriate training
and skills-based recognition within the discipline and the broader health team, and the need to overtly
demonstrate effectiveness and safety. Regularly-evaluated service-delivery models which support NMP by
physiotherapists arefurther required, todemonstrate efciency, timeliness, patient centredness andequity.
Crown Copyright 2013 Published by Elsevier Ltd. All rights reserved.
1. Introduction
The last decade has seen rapid international changes to
healthcare environments and workforce (Kersten et al., 2007;
McClellan, et al., 2010; Stanhope et al., 2012). Drivers of change
include increasing prevalence of chronic disease, ageing pop-
ulations, and increasing community expectations of responsiveness
(eg shorter waiting times, quicker assessments). This has led to
innovative models of care described internationally as workforce
redesign (Robertson et al., 2003; Stanhope et al., 2012). Expansion
of scope of practice is one workforce redesign initiative which in-
volves physiotherapists (Robertson et al., 2003).
Increased prevalence of chronic disease brings an increased
demand for medicines. Within an environment promoting
healthcare responsiveness to consumer demand, this can be
addressed by increasing the number of prescribers via Non-Medical
Prescribing (NMP).
This paper considers medicolegal, professional and educational
as well as workforce redesign issues relevant to prescribing by
physiotherapists.
2. Issues surrounding extended scope practice in
physiotherapy
Extended Scope Physiotherapy Practice (ESP) is dened as:
A role that is outside the currently recognised scope of practice
and requires legislative change. Extended scope of practice requires
some method of credentialing following additional training, com-
petency development and signicant clinical experience. Examples
* Corresponding author. Tel.: 61 02 6244 2154; fax: 61 02 6244 3692.
E-mail addresses: jo.morris@act.gov.au (J.H. Morris), Karen.grimmer@
unisa.edu.au (K. Grimmer).
Contents lists available at SciVerse ScienceDirect
Manual Therapy
j ournal homepage: www. el sevi er. com/ mat h
1356-689X/$ e see front matter Crown Copyright 2013 Published by Elsevier Ltd. All rights reserved.
http://dx.doi.org/10.1016/j.math.2013.04.003
Manual Therapy 19 (2014) 82e86
include prescribing, injecting and surgery. This role describes the
breadth of practice.
Australian Health Workforce Advisory Committee, 2006.
2.1. Background of NMP
NMP has been in existence in the UK since 1989 (Drug and
Therapeutic Bulletin, 2006). This largely reects pressures brought
to bear on the UK health workforce, to increase service responsive-
ness. Specically relating to physiotherapy-prescribing in the UK,
activities have occurred under direct instruction from Medical
Practitioners since early1990s, andinjectionpractices since1995via
patient-group directives (PGDs). In 2009, there were approximately
3000 physiotherapy-injectors (Department of Health (UK) 2009).
There is general international support for ESP physiotherapy
roles as a way of making specialist healthcare services more
available to those who need it (Kersten et al., 2007; McClellan et al.,
2010; Lebec, 2010). Kersten et al. (2007) systematically reviewed
literature about ESP physiotherapy roles in the UK, their accept-
ability and effectiveness. This review included 23 data sources that
reported at least one component of ESP physiotherapy roles being
invasive (eg prescribing and injecting). Holdsworth et al. (2008)
specically mentioned prescribing NSAIDs as a component of
extended-scope physiotherapy roles.
However, there is a lack of published evidence relating to the role
and effectiveness of physiotherapists when prescribing or adminis-
tering medication, or injecting. There is more literature relating to
other ESP physiotherapy roles in undertaking traditional medical
tasks egorthopaedic triage or listing for surgery (Kerstenet al., 2007).
A study by Birchall et al. (2008) discussed the efcacy of
injecting hyaluronic acid for the treatment of OA knee pain, with
the injections being provided by physiotherapists, however the
paper did not discuss the ability of the physiotherapists to provide
this treatment more the efcacy of the treatment itself.
For the purposes of this paper, prescribing is dened as:
The information gathering, clinical decision making and commu-
nication steps involved in the initiation, continuation or cessation of
a medication, remedy or treatment for a specic patient
Nissen et al., 2010.
3. Methods
3.1. Aim
This review aimed to identify issues reported in the current
literature (published and unpublished) which should be consid-
ered, before NMP by physiotherapists is introduced in Australia as
part of any workforce reform.
The current evidence-base was established in three ways
a) a targeted literature reviewof electronic databases EBSCOHost,
Cochrane, Medline, SportsDiscus, Cinahl, Healthsource, using
broad search terms of:
Prescr#
Physiother#*
b) identifying grey literature via Google.com and government
internet sites
c) Hand searching reference lists of included peer-reviewed and
grey literature to identify articles not retrieved via primary
database searching.
Included articles were limited to full text, peer-reviewed, and
comprehensive government documents, published between 2002
and 2012. Included articles were classied in the NHMRC hierarchy
(Merlin, et al., 2009), although critical appraisal of methodology
was not undertaken. Literature was extracted on NMP activities
undertaken by physiotherapists, and service delivery issues (i.e.
legislation, registration, training, competencies). Data synthesis
was reported descriptively.
4. Results
Of 237 potentially relevant peer-reviewed articles, six directly
addressed NMP for physiotherapists. Three relevant government
reports were also sourced, and no additional references were
identied by hand-searching (see Fig. 1).
4.1. Overview
Six relevant peer-reviewed articles were found (hierarchy levels
III_3, IV). Three comprehensive, recent grey literature sources were
identied. The evidence suggests that the UK approach to physio-
therapy ESP (including NMP) has lacked a consistent, robust and
National direction (Nissen et al., 2010; McCormick and Downer,
2012; Stanhope et al., 2012). However Nissen et al. (2010) and the
Department of Health (UK) (2009) concur that NMP has the po-
tential to:
Improve patient care without compromising safety
Make it simpler and more efcient for patients to get the
medicines they need
Increase patient choice in safely accessing medications e
including access to care closer to home
Make better use of the skills of health professionals and in-
crease value for money
Contribute to introduction of a more exible team working
Facilitate early discharge from hospital
Prevention of admission to hospital
4.2. Safety
The UK Department of Health (2009) demonstrated in an
adverse events report (January 2005eJune 2006) detailing 60,000
medication incidents in the UK, that none related to Allied Health
Professional (AHP) prescribers. The reports investigating NMP
(Department of Health (UK) 2009; Nissen et al., 2010) highlighted
key requirements to safely introduce NMP:
Credentialing processes
A competency framework
A licensed accrediting body/organisation to regulate registra-
tion processes
It is therefore essential to consider these components in the
context of introducing NMP by Australian physiotherapists.
4.3. Models of prescribing
The UK has trialled several NMP models. Nissen et al. (2010)
completed a scoping report for National Health Workforce
Australia on NMP, based on UK learnings. They presented ideas for
developing a nationally-consistent approach to prescribing by non-
medical health professionals in Australia. Four cumulative tiers
were recommended to underpin introduction of NMP in Australia:
1. Administration: tight model for immediate prescription only
2. Protocol model: allowing scope for supply of a course of
medication (e.g. antibiotics)
J.H. Morris, K. Grimmer / Manual Therapy 19 (2014) 82e86 83
3. Supplementary/collaborative: delegated prescribing author-
ity model with controls on disease state(s) treated and range of
medications available
4. Independent: delegated prescribing authority where a prac-
titioner operates within a collaborative environment without
direct supervision constraints
The cumulative approach described by Nissen et al. (2010) could
be adapted to accommodate the variety of clinical areas and con-
texts within which Australian physiotherapists operate, as well as
individuals prescribing interests. For instance, for the rst tier,
basic formulary could be developed for individual clinical areas,
using clinical experts, which are then adapted to individual
situations.
4.4. Current legislation
There are Australian state-by-state variations in the Medicines,
Poisons and Therapeutics Goods Regulations/Acts, relative to
physiotherapists. In some Australian states, there is capacity within
current legislation to trial limited physiotherapy-prescribing (un-
der standing order or permit arrangements), whilst other states
require legislative changes. Information about state and territory
Medicines and Poisons Acts needs to be accessed by individual state
websites (Appendix 1). The Australian Health Practitioner Regula-
tion Agency (AHPRA) is currently developing a document to collate
this information, thus providing a central resource for physiother-
apists to review the legislation as it applies to them.
4.5. Grey areas of physiotherapy-prescribing
There are continuing legislative grey areas of physiotherapist
involvement with medicines in Australia (Sullivan & Lansbury,
1999; Grimmer et al., 2002; Kumar & Grimmer, 2005). This in-
cludes physiotherapists providing patients with variable advice
regarding NSAIDs and pain medication, or administering NSAIDs
during treatment. In light of NMP initiatives, it is timely to consider
the differences in medicines training in Australian undergraduate
and postgraduate physiotherapy programs, to ensure minimum
educational standards (Sullivan & Lansbury, 1999; Grimmer et al.,
2002; Kumar & Grimmer, 2005; Braund & Haxby Abbott, 2011)
5. Discussion
Proactivity is required to ensure that NMP by Australian phys-
iotherapists has appropriate medicolegal support, formal training
and credentialing, and formal recognition by the health workforce.
Whenever a physiotherapist receives NMP rights, standard evalu-
ations should regularly occur to ensure consistent quality care. The
Institute of Medicine model (Kohn, et al., 2000) denes quality care
in terms of effectiveness, efciency, timeliness, safety, patient
centredness and equity. NMP by physiotherapists should be eval-
uated in these terms to ensure that it is a recognised and sustain-
able element of the future health workforce.
5.1. Regulation
There is a new National registration body for physiotherapists
(Australian Health Practitioner Regulation Agency (AHPRA e http://
www.ahpra.gov.au/)). This may be the most appropriate Australian
body to provide regulatory authority to Australian physiotherapy-
prescribing. This approach would be consistent with the UK experi-
ence, where the regulatory body (the Health Professions Council), is
responsible for the regulatory function of physiotherapist-
prescribers, by a notation in the clinicians registration. It is there-
fore suggestedthat a caveat be includedinthe Australianregistration
processes to accommodate credentialed physiotherapy-prescribers.
5.2. Education and training
Coupled with variable training in undergraduate pharmacology
(Sullivan &Lansbury, 1999; Grimmer et al., 2002; Kumar &Grimmer,
2005; Braund & Haxby Abbott, 2011), currently there are limited
training programs in post-graduate pharmacology available to
Fig. 1. Literature review ow chart.
J.H. Morris, K. Grimmer / Manual Therapy 19 (2014) 82e86 84
physiotherapists wishing to work inESP roles. Adecade-old study by
Sullivan and Lansbury (1999) suggested that inadequate training in
medications potentially resulted in lax practice, particularly related
to obtaining and keeping comprehensive records about patients
medication. These ndings were supported by Grimmer et al. (2002)
who undertook a survey of approximately half of the registered
physiotherapists in South Australia. This survey found notable dif-
ferences in engagement with medicines in day-to-day clinical
practice, as well as variable understanding of dosage, and action of
oral and topical NSAIDs. More recently, Braund and Haxby Abbott
(2011) undertook a study of New Zealand physiotherapists under-
standing of contraindications to recommending NSAIDs, nding that
whilst 70% could demonstrate knowledge relating to gastro-
Intestinal issues, ulcers or bleeding, only 30% had demon-
strated knowledge of respiratory, renal or allergic risks. This
literature highlights that an essential component for introducing
physiotherapy-prescribing is a nationally-recognised and accredited
training program for undergraduate physiotherapists, and formal
avenues for continuing professional development, credentialing and
skill maintenance for physiotherapists working in-scope as well as in
extended scope roles.
5.3. Credentialing
The credentialing and education process must translate to the
clinical environment and model of care within which the
physiotherapy-prescriber works. A credentialing model that in-
cludes supervision from a registered prescriber within an appro-
priate clinical context is essential to ensure that a safe and
effective level of prescribing practice is achieved and recognised.
However, in the current context, where there are no registered
physiotherapy prescribers, there has to be engagement with other
registered prescribers to provide supervision. McCormick and
Downer (2012) identied that a key component for supervision
of NMP students is ensuring that the education and supervision
process and scope of practice of the NMP student is well under-
stood by the medical supervisor. A key consideration to intro-
ducing physiotherapy-prescribing will be education and
consultation with other health professionals to ensure local sup-
port and engagement.
5.4. Use of protocols and guidelines
Atkins (2003) identied through interviews with 11 UK phys-
iotherapists with recognised injecting skills that a more formalised
approach to physiotherapy-prescribing and ESP roles will produce a
more consistent, transferable and recognised workforce.
5.5. Competency
A competency framework that is specic to Australian physio-
therapy knowledge and practice is urgently required, to underpin
roll-out of extended scope of practice. Australian physiotherapists
have the skills and training to assess, diagnose and provide treat-
ment to patients in broad clinical areas, including, but not limited to,
musculoskeletal, cardio-respiratory, neurology, paediatrics, obstet-
rics and gynaecology and aged-care practices. There are credible
workforce, patient access and health outcome drivers to extend
physiotherapy scope of practice in all of these clinical areas, thus
consideration of prescribing needs across these clinical elds is
required. Moreover, many of the urgent drivers for change come
from rural and remote areas, where access to medical practitioners
may be a signicant issue. The practicalities of introducing
physiotherapy-prescribing in metropolitan, regional, rural and
remote settings need to be carefullyconsidered, as the ways inwhich
NMP is introduced and supported may be signicantly different.
6. Conclusion
NMP is an essential component of physiotherapy ESP. With the
right training and supports, it has been shown to be safe overseas,
and it could be practiced similarly by Australian physiotherapists.
However, for this to be a successful and acceptable workforce re-
form initiative in Australia, it requires policy and legislation
changes, promotion of alternative NMP models to suit different
situations, context-relevant training and credentialing, and
informed support from the medical profession. Comprehensive
evaluation criteria should be developed and widely implemented,
to ensure that safe practices and prescribing principles are
demonstrated by physiotherapy-prescribers.
Acknowledgements
Jessica Stanhope, iCAHE, for assisting with searching.
Appendix 1. State and Territory Legislation documents
relating to medicines
Victorian Drugs, Poisons and Controlled Substances Act 1981:
http://www.legislation.vic.gov.au/Domino/Web_Notes/LDMS/
LTObject_Store/LTObjSt7.nsf/DDE300B846EED9C7CA25761600
0A3571/3E94BBFB45B6850ACA257A700000A6DF/$FILE/81-97
19aa099%20authorised.pdf
Controlled Substances Act 1984 e South Australia: http://www.
legislation.sa.gov.au/LZ/C/A/CONTROLLED%20SUBSTANCES%20
ACT%201984/2004.09.29/1984.52.PDF
Health (Drugs and Poisons) Regulation 1996 e Queensland: http://
www.legislation.qld.gov.au/LEGISLTN/CURRENT/H/HealDrAPoR
96.pdf
Poisons Act 1971 e Tasmania: http://www.thelaw.tas.gov.au/
tocview/index.w3p;condall;doc_id81%2B%2B1971 %2BAT%
40EN%2B20100214000000;histon;prompt;rec;termpois
ons%20act
Poisons and Therapeutic Drugs Act 1966 e New South Wales:
http://www.legislation.nsw.gov.au/maintop/view/inforce/act
311966cd0N
Poisons and Therapeutic Goods Regulation 2002 http://www.
legislation.nsw.gov.au/fullhtml/inforce/subordleg6392002
FIRST0N
Northern Territory Poisons & Dangerous Drugs Act: http://www.
austlii.edu.au/au/legis/nt/consol_act/padda296/
Western Australia Poisons Act 1964: http://www.austlii.edu.au/
au/legis/wa/consol_act/pa1964121/
Poisons Regulations 1965
http://www.austlii.edu.au/au/legis/wa/consol_reg/pr1965230/
s40.html
Australian Capital Territory e Medicines, Poisons and Therapeutic
Goods Act 2008: http://www.legislation.act.gov.au/a/2008-26/
current/pdf/2008-26.pdf
Source of support
None.
Competing interests
None declared.
J.H. Morris, K. Grimmer / Manual Therapy 19 (2014) 82e86 85
References
Section 1: Peer-reviewed literature from search
Atkins E. Physiotherapists experience of implementing their injection therapy
skills. Physiotherapy 2003;89:145e57.
Birchall D, Ismail AM, Peat G. Clinical outcomes from a physiotherapist-led intra-
articular hyaluronic acid injection clinic. Musculoskeletal Care 2008;6:135e49.
Braund R, Haxby Abbott J. Recommending NSAIDs and Paracetamol: A Survey of
New Zealand Physiotherapists Knowledge and Behaviours. Physiotherapy
Research International 2011;16:43e9.
Grimmer K, Kumar S, Gilbert A, Milanese S. Non-steroidal anti-inammatory drugs
(NSAIDs): physiotherapists use, knowledge and attitudes. Australian Journal of
Physiotherapy 2002;48:82e92.
Kumar S, Grimmer K. Non-steroidal anti-inammatory drugs (NSAIDs) and Phys-
iotherapy management of musculoskeletal conditions: a professional mine-
eld? Therapeutics and Clinical Risk Management 2005;1:69e76.
Sullivan G, Lansbury G. Physiotherapists knowledge of their clients medication: A
survey of practising physiotherapists in New South Wales, Australia. Physio-
therapy Theory and Practice 1999;15:191e8.
Section 2: Government reports from search
Department of Health (UK). Allied health professions prescribing and medicines
supply mechanisms scoping project report. http://www.dh.gov.uk/en/
Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_
103948; 2009.
Drug and Therapeutic Bulletin. Non-medical prescribing. Drug and Therapeutic
Bulletin 2006;44:33e6.
Nissen L, Kyle G, Stowasser D, Lum E, Jones A, McLean C. Non-medical prescribing.
http://www.ahwo.gov.au/documents/NHWT/Non%20Medical%20Prescribing%
20Final%20Report.pdf; 2010. Accessed May 2012.
Section 3: Background Information
Australian Health Workforce Advisory Committee. The Australian Allied Health
Workforce. North Sydney: AHWAC NAHAC Endorsed National Denitions. An
overview of Workforce Planning Issues, Report 2006.1, http://www.ahwo.gov.
au/documents/Publications/2006/The%20 Australian%20allied%20health%20wo
rkforce.pdf; 2006. Accessed May 2012.
Holdsworth LK, Webster VS, McFadyen AK. The Scottish Physiotherapy Self Referral
Study Group. Physiotherapy 2008;94:236e43.
KerstenP, McPhersonK, Lattimer V, George S, BretonA, Ellis B. Physiotherapyextended
scope of practice ewho is doing what and why? Physiotherapy 2007;93:235e42.
Kohn LT, Corrigan JM, Donaldson MS. To err is human: Building a safer health
system. Institute of Medicine (IOM). http://books.nap.edu/openbook.php?
isbn0309068371; 2000.
Lebec MT. Extended scope physiotherapists in the emergency department: one step
further. Physical Therapy Reviews 2010;15:420e1.
McClellan CM, Cramp F, Powell J, Benger JR. Extended scope physiotherapists in the
emergency department: a literature review. Physical Therapy Reviews 2010;15:
106e11.
McCormick E, Downer F. Students perceptions of learning in practice for NMPs.
Nurse Prescribing 2012;10:85e90.
Merlin T, Weston A, Tooher R. Extending an evidence hierarchy to include topics
other than treatment: revising the Australian levels of evidence. BMC Medical
Research Methodology 2009;9:34e42.
Robertson VJ, Oldmeadow LB, Cromie JE, Grant MJ. Taking charge of change: a new
career structure in physiotherapy. Australian Journal of Physiotherapy 2003;49:
229e31. Accessed May 2012.
Stanhope J, Grimmer-Somers K, Milanese S, Kumar S, Morris J. Extended scope
physiotherapy roles for orthopedic outpatients: an update systematic review of
the literature. Journal of Multidisciplinary Healthcare 2012;5:37e45. http://
www.ahpra.gov.au/. The Australian Health Practitioner Regulation Agency.
Accessed 8.10.12.
J.H. Morris, K. Grimmer / Manual Therapy 19 (2014) 82e86 86
Anda mungkin juga menyukai
- Cholesterol e Book FinalDokumen14 halamanCholesterol e Book Finalubiktrash1492Belum ada peringkat
- Cereal: Important Information If You Have Type 2 DiabetesDokumen1 halamanCereal: Important Information If You Have Type 2 Diabetesubiktrash1492Belum ada peringkat
- Type of Bread: Important Information If You Have Type 2 DiabetesDokumen1 halamanType of Bread: Important Information If You Have Type 2 Diabetesubiktrash1492Belum ada peringkat
- NIH Public Access: A High-Fiber Diet Does Not Protect Against Asymptomatic DiverticulosisDokumen17 halamanNIH Public Access: A High-Fiber Diet Does Not Protect Against Asymptomatic Diverticulosisubiktrash1492Belum ada peringkat
- 10+ Top Medical: Tests To Follow On The LCHF DietDokumen12 halaman10+ Top Medical: Tests To Follow On The LCHF Dietubiktrash1492Belum ada peringkat
- A Time To FastDokumen7 halamanA Time To Fastubiktrash1492Belum ada peringkat
- Physical Inactivity: The Biggest Public Health Problem of The 21st CenturyDokumen3 halamanPhysical Inactivity: The Biggest Public Health Problem of The 21st Centuryubiktrash1492Belum ada peringkat
- Training Endurance Part2Dokumen2 halamanTraining Endurance Part2ubiktrash1492Belum ada peringkat
- Movilidad MadridDokumen9 halamanMovilidad Madridubiktrash1492Belum ada peringkat
- Dive Sites (Dive Spots) : TOYAPAKEH - Nusa PenidaDokumen3 halamanDive Sites (Dive Spots) : TOYAPAKEH - Nusa Penidaubiktrash1492Belum ada peringkat
- Training Endurance Part1Dokumen2 halamanTraining Endurance Part1ubiktrash1492Belum ada peringkat
- Association of Dietary Fatty Acids With Coronary RiskDokumen17 halamanAssociation of Dietary Fatty Acids With Coronary Riskubiktrash1492Belum ada peringkat
- Training Endurance Part1Dokumen2 halamanTraining Endurance Part1ubiktrash1492Belum ada peringkat
- Atlas of Osteopathic TechniquesDokumen80 halamanAtlas of Osteopathic Techniquesubiktrash1492100% (1)
- Home Study Course in Osteopathy Massage and Manual Therapeutics 1900 PDFDokumen150 halamanHome Study Course in Osteopathy Massage and Manual Therapeutics 1900 PDFubiktrash1492100% (1)
- Principles of Osteopathy PDFDokumen188 halamanPrinciples of Osteopathy PDFubiktrash1492Belum ada peringkat
- Manual TherapyDokumen10 halamanManual Therapyubiktrash1492Belum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
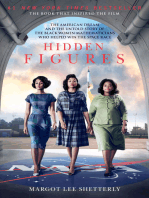
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Ofra Ayalon Healing Trauma With Metaphoric Cards PDFDokumen3 halamanOfra Ayalon Healing Trauma With Metaphoric Cards PDFKrisztina MkBelum ada peringkat
- Personal BoundariesDokumen4 halamanPersonal Boundariesscribdreaderplus75% (4)
- Congenital DiseaseDokumen39 halamanCongenital DiseaseRavi SharmaBelum ada peringkat
- Vertigo MeniereDokumen5 halamanVertigo MeniereHamba AllahBelum ada peringkat
- Myths of DialysisDokumen26 halamanMyths of DialysisSijo Muthukad M100% (1)
- Contrast MediaDokumen94 halamanContrast MediaJustin JoseBelum ada peringkat
- ArenavirusDokumen29 halamanArenavirusRamirez GiovarBelum ada peringkat
- Occupational Health NursingDokumen22 halamanOccupational Health NursingIrene Joy ArellanoBelum ada peringkat
- Aplastic AnemiaDokumen3 halamanAplastic AnemiaFrancis JuneBelum ada peringkat
- Enamel Hypoplasia RestorationDokumen4 halamanEnamel Hypoplasia RestorationzaheerbdsBelum ada peringkat
- Chennai STP Eia ReportDokumen51 halamanChennai STP Eia Reportmahesh warBelum ada peringkat
- Poisoning and Drug OverdoseDokumen95 halamanPoisoning and Drug OverdoseMohammed Younis Shaheen100% (2)
- Helen K. Sneller: Program, 1996Dokumen2 halamanHelen K. Sneller: Program, 1996Siddharth NelsonBelum ada peringkat
- Nota PsikoterapiDokumen4 halamanNota PsikoterapiAraizzs OthmanBelum ada peringkat
- Bladder Irrigation & InstallationDokumen12 halamanBladder Irrigation & InstallationSui NarcanBelum ada peringkat
- Acute PancreatitisDokumen2 halamanAcute PancreatitisHassan Nor Boransing Mangorsi100% (1)
- ATI DRUG TABLES Module4 Respiratory Glucocorticoids InhalationDokumen1 halamanATI DRUG TABLES Module4 Respiratory Glucocorticoids InhalationnoeyeshaveseenBelum ada peringkat
- Paul Holmes, Steve Farnfield - The Routledge Handbook of Attachment - Implications and Interventions-Routledge (2014)Dokumen205 halamanPaul Holmes, Steve Farnfield - The Routledge Handbook of Attachment - Implications and Interventions-Routledge (2014)Pamela Fontánez100% (4)
- Kleihauer TestDokumen3 halamanKleihauer Testteo2211Belum ada peringkat
- ما يقارب 200 سؤال مع الاجابة لاسئلة الهيئة السعودية للتخصصات الصحية لاخصائيي المناعة والامصال وبDokumen34 halamanما يقارب 200 سؤال مع الاجابة لاسئلة الهيئة السعودية للتخصصات الصحية لاخصائيي المناعة والامصال وبMohsen HaleemBelum ada peringkat
- Reflexology and DementiaDokumen8 halamanReflexology and DementiaNatalie Stubbs100% (1)
- (Treatments That Work) Gail Steketee, Randy O. Frost - Compulsive Hoarding and Acquiring - Therapist Guide-Oxford University Press (2006)Dokumen237 halaman(Treatments That Work) Gail Steketee, Randy O. Frost - Compulsive Hoarding and Acquiring - Therapist Guide-Oxford University Press (2006)mdmonzurh1100% (2)
- CRITICAL THINKING CASE STUDY - PharmaDokumen4 halamanCRITICAL THINKING CASE STUDY - PharmaElleBelum ada peringkat
- Endometriosis & AdenomyosisDokumen47 halamanEndometriosis & AdenomyosisAzim Syahmi Abd RazakBelum ada peringkat
- Book Reviews: Trigger Points and Muscle Chains in OsteopathyDokumen4 halamanBook Reviews: Trigger Points and Muscle Chains in OsteopathyConstanza López MillerBelum ada peringkat
- Prophylaxis and Treatment For AspirationDokumen19 halamanProphylaxis and Treatment For Aspirationbalab2311Belum ada peringkat
- West Visayas State University Medical Center E. Lopez St. Jaro Iloilo CityDokumen7 halamanWest Visayas State University Medical Center E. Lopez St. Jaro Iloilo CityRegine Marie EspañaBelum ada peringkat
- CL12Dokumen598 halamanCL12preeti dBelum ada peringkat
- Quarter 1 SUMMATIVE TEST For Beauty CareDokumen4 halamanQuarter 1 SUMMATIVE TEST For Beauty CareVinzMontederamosMalupa-Jimenez100% (2)
- 14 WartsprotocolDokumen9 halaman14 WartsprotocolLakshmi Deepak IBelum ada peringkat