BMC Cancer
Diunggah oleh
Jose Antonio VenacostaDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
BMC Cancer
Diunggah oleh
Jose Antonio VenacostaHak Cipta:
Format Tersedia
BioMed Central
Page 1 of 6
(page number not for citation purposes)
BMC Cancer
Open Access
Research article
Docetaxel plus cisplatin is effective for patients with metastatic
breast cancer resistant to previous anthracycline treatment: a
phase II clinical trial
Se Hoon Park
1
, Eun Kyung Cho
1
, Soo-Mee Bang
1
, Dong Bok Shin*
1
,
Jae Hoon Lee
1
and Young Don Lee
2
Address:
1
Division of Hematology and Oncology, Internal Medicine, Gachon Medical School Gil Medical Center, Incheon 405760, Korea and
2
Department of Breast Surgery, Gachon Medical School Gil Medical Center, Incheon 405760, Korea
Email: Se Hoon Park - hematoma@ghil.com; Eun Kyung Cho - ekcho@ghil.com; Soo-Mee Bang - smbang@ghil.com;
Dong Bok Shin* - dbs@ghil.com; Jae Hoon Lee - jhlee@ghil.com; Young Don Lee - peacemk@ghil.com
* Corresponding author
Abstract
Background: Patients with metastatic breast cancer (MBC) are frequently exposed to high
cumulative doses of anthracyclines and are at risk of resistance and cardiotoxicity. This phase II trial
evaluated the efficacy and toxicity of docetaxel plus cisplatin, as salvage chemotherapy in patients
with MBC resistant to prior anthracyclines.
Methods: Patients with MBC that had progressed after at least one prior chemotherapy regimen
containing anthracyclines received docetaxel 75 mg/m
2
followed by cisplatin 60 mg/m
2
every 3
weeks for a maximum of 6 cycles or until disease progression.
Results: Between Jan 2000 and May 2002, 24 patients with tumors primary resistant and 15 with
secondary resistant disease were accrued. All 39 patients were evaluable for safety and 36 for
efficacy. The objective response rate was 31% (95% CI, 1645%) with 3 complete responses. The
median time to disease progression was 7 months, and the median overall survival was 23 months
(median follow-up of 41 months). Neutropenia was the most frequently observed severe
hematologic toxicity (39% of patients), whereas asthenia and nausea were the most common non-
hematologic toxicities. No treatment-related death was observed.
Conclusion: In conclusion, we found docetaxel plus cisplatin to be an active and safe
chemotherapy regimen for patients with MBC resistant to anthracyclines.
Background
In the management of breast cancer, anthracycline-based
chemotherapy regimens remain standard adjuvant or
first-line palliative treatment. Furthermore, some patients
cannot be treated with anthracyclines due to impaired car-
diac function. It is thus important to identify active, well-
tolerated, not anthracycline cross-resistant, salvage regi-
mens [1].
Taxanes (docetaxel and paclitaxel) are currently the most
extensively studied new chemotherapeutic agents for met-
astatic breast cancer (MBC). Single-agent docetaxel has
Published: 22 February 2005
BMC Cancer 2005, 5:21 doi:10.1186/1471-2407-5-21
Received: 30 June 2004
Accepted: 22 February 2005
This article is available from: http://www.biomedcentral.com/1471-2407/5/21
2005 Park et al; licensee BioMed Central Ltd.
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0),
which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
BMC Cancer 2005, 5:21 http://www.biomedcentral.com/1471-2407/5/21
Page 2 of 6
(page number not for citation purposes)
demonstrated significant survival advantages over other
recognized regimens in 2 large randomized trials in
patients with anthracycline-pretreated MBC [2,3]. Phase II
data suggest that docetaxel is the most active agent yet
available for the treatment of MBC [4]. Docetaxel also has
some activity in paclitaxel-resistant MBC [5].
Cisplatin monotherapy has shown response rate of 9% in
salvage settings, and 50% as first-line therapy [6]. Because
docetaxel and cisplatin are both active and have different
mechanisms of action, this combination may provide
additive effect against MBC. Although docetaxel and cispl-
atin were not actively synergistic in preclinical studies
[7,8], this combination chemotherapy has been widely
used for treatment of a variety of tumor types [9-13]. Prior
phase I studies showed the feasibility of this combination
and its activity on different tumors [14]. Considering the
single-agent activity of both drugs, their different mecha-
nism of action and distinct toxicity profile, we designed
this phase II study, in which the combination was evalu-
ated as a salvage therapy in patients with anthracycline-
resistant MBC.
Methods
Eligibility
Eligible patients had measurable or assessable histologi-
cally confirmed breast cancer that had progressed after at
least one prior chemotherapy regimen containing anthra-
cyclines. All patients had Eastern Cooperative Oncology
Group performance status of 2 or lower and adequate
bone marrow, hepatic, and renal function, defined as
white blood cells 4000/L, absolute neutrophil count
1500/L, platelets 100,000/L, total bilirubin 2.0 mg/
dL, transaminases 3 times the upper normal limit, and
serum creatinine 1.5 mg/dL. Concurrent radiation or
hormonal therapy was not allowed; however, patients
with clinically stable metastases of the brain or other sites
who had completed radiation therapy were permitted.
Patients were eligible regardless of the nature of prior ther-
apy, including high-dose therapy with stem cell support
and prior exposure to paclitaxel. Any prior antitumor
treatment had been completed at least 1 month before
entering this study. Patients were excluded if they had
severe comorbid illness, symptomatic peripheral neurop-
athy of any origin, or a history of anaphylaxis of any type.
All patients were provided a thorough explanation of the
study, and they signed informed consent prior to enroll-
ment into the study.
Definition of anthracycline-resistance
Patients were classified as primary and secondary anthra-
cycline-resistant. Primary anthracycline-resistance was
defined as relapse during or within 12 months after
anthracycline-based adjuvant therapy, or disease progres-
sion with no intervening response during anthracycline-
containing chemotherapy for MBC. Secondary resistance
was defined as relapse more than 12 months after receiv-
ing adjuvant anthracycline chemotherapy, or disease pro-
gression at some time after a documented clinical
response to anthracycline-based chemotherapy for MBC.
Pretreatment and follow-up evaluation
Pretreatment evaluation included a complete medical his-
tory and physical examination, a computed tomographic
(CT) scan of the chest and abdomen, magnetic resonance
imaging (MRI) of the brain, and a bone scintigraphy to
assess the extent of disease. Follow-up consisted of physi-
cal examination, monitoring of toxic effects, a complete
blood count, liver function tests, chest radiography, and
CT scan as clinically indicated.
Tumor response and toxicity were recorded in accordance
with the World Health Organization (WHO) criteria.
Responses were assessed every 2 cycles of chemotherapy,
and patients were evaluated before each new treatment
cycle for toxicities.
Treatment plan
The treatment consisted of docetaxel (Taxotere
, Aventis,
Bridgewater, NJ) 75 mg/m
2
given by a 1-hour intravenous
infusion immediately followed by cisplatin 60 mg/m
2
in
a 2-hour infusion. Cycles were repeated every 3 weeks if
the patient's blood count had returned to normal and
non-hematologic toxicities had resolved. Dosage of subse-
quent cycles was adjusted according to the observed toxic-
ities that developed during the preceding cycle. The
treatment continued for a maximum of 6 cycles or until
disease progression. All patients received standard sup-
portive care regimen consisting of adequate hydration,
dexamethasone, and antiemetic therapy according to the
guidelines of the American Society of Clinical Oncology
[15].
Statistics
The primary end points of the trial were the efficacy of the
therapy, which were measured as objective response rate
and time to progression, with a secondary end point of
toxicity. All patients who received at least 2 cycles of treat-
ment or who progressed after the first cycle were consid-
ered assessable for response. The study was conducted
using a single-stage, phase II trial design [16]. Based on
the results from previous phase II trials reporting response
rates of about 30% in patients with anthracycline-resistant
MBC, we selected a 50% target response probability and a
30% null response probability, with type I and type II
error set at 10%. The number of patients required was 39.
Statistical calculations were performed using SPSS soft-
ware, version 11.5 (SPSS, Inc, Chicago, IL). Comparisons
were performed using chi-square test and survival curves
BMC Cancer 2005, 5:21 http://www.biomedcentral.com/1471-2407/5/21
Page 3 of 6
(page number not for citation purposes)
were generated using Kaplan-Meier method. Results were
considered significant at the P = .05.
Results
Patients characteristics
Between Jan 2000 and May 2002, 24 patients with tumors
primary resistant and 15 with secondary resistant disease
were accrued. Among 39 patients assessable for safety, 3
were not evaluable for response due to early discontinua-
tion of treatment.
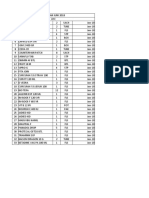
Baseline characteristics of the eligible patients are listed in
Table 1. Median age was 51 years (range, 4164) and
median performance status was 1. Thirty-three patients
(85%) had visceral metastases as the dominant site of dis-
ease. All patients had received prior anthracycline-based
chemotherapy with a median number of prior chemo-
therapeutic regimens of 2 (range, 13). Three patients
(8%) had exposed to paclitaxel in their previous chemo-
therapy regimen.
Efficacy
According to the "intent-to-treat" analysis, the objective
response rate was 31% (95% confidence interval [CI], 16
45%). There were 3 complete responses, 12 partial
responses and 15 patients had stable disease. The three
patients who obtained a complete response had non-vis-
ceral metastatic pattern (neck lymph nodes and/or soft tis-
sue lesions). Most patients who achieved a response did
so at the end of the third cycle (median time to response,
2.2 months; 95% CI, 2.12.4 months).
At a median follow-up of 40.5 months (95% CI, 36.4
44.6 months), the median time to progression was 6.6
months (95% CI, 3.99.4 months) and the median over-
all survival was 22.9 months (95% CI, 17.228.5
months). The time to progression in responders were 16.7
months (P < 0.0001). The Kaplan-Meier method was used
to estimate overall survival and time to progression, as
shown in Figure 1. At the time of present analyses, 21
patients (54%) died.
We observed no significant differences in overall response
rate or survival between primary and secondary anthracy-
cline-resistant groups. The overall survival and time to
progression were higher in patients with objective
response (P < 0.0001 and P = 0.05, respectively).
Toxicity
Patients received a median of 6 cycles (range, 16) of
docetaxel plus cisplatin. Relative dose intensities were
84% (95% CI, 7396%) and 86% (95% CI, 7597%) for
docetaxel and cisplatin, respectively. Twenty-four patients
(62%) completed 6 cycles of chemotherapy as planned;
Nine patients had progression of disease while receiving
treatment and 6 patients discontinued treatment because
of toxicity. Treatment delay was occurred in 54 cycles
(29%).
Toxicity was evaluable in all 39 patients and 189 chemo-
therapy cycles. Even if the most frequent hematological
toxicity was neutropenia (grade 3/4 in 22% of treatment
cycles), only 12 episodes of non-fatal febrile neutropenia
Table 1: Patient characteristics
No. %
Patients
Treated 39 100.0
Evaluable for response 36 92.3
Age
Median (years) 51.3
Range 41.2 64.1
ECOG performance status
0 3 7.7
1 27 69.2
2 9 23.1
Site(s) of metastatic lesion(s)*
Lung 27 69.2
Liver 9 23.1
Lymph node 15 38.5
Soft tissue 3 7.7
Bone 24 61.5
Brain 3 7.7
Response to prior anthracyclines
Primary resistant 24 61.5
Secondary resistant 15 38.5
Interval from the cessation of last chemotherapy
Median (months) 4.1
Range 1.0 11.2
No. of prior chemotherapy regimens
Hormonal therapy (total) 20 51.3
1 9 23.1
2 21 53.8
3 or more 9 23.1
Characteristics of prior chemotherapy
CMF 24
CAF 15
FEC 9
VE 21
High-dose therapy with stem cell rescue 6
AT 3
* Because patients could have metastases at multiple sites, the total
numbers of metastases are greater than the number of patients.
CMF, cyclophosphamide 600 mg/m
2
, methotrexate 40 mg/m
2
, 5-
fluorouracil 600 mg/m
2
, days 1 & 8, every 4 weeks; CAF,
cyclophosphamide 500 mg/m
2
, doxorubicin 50 mg/m
2
, 5-fluorouracil
500 mg/m
2
, every 3 weeks; FEC, 5-fluorouracil 600 mg/m
2
, epirubicin
60 mg/m
2
, cyclophosphamide 600 mg/m
2
, every 4 weeks; VE,
vinorelbine 25 mg/m
2
, days 1 & 8, epirubicin 60 mg/m
2
day 1, every 3
weeks; AT, doxorubicin 50 mg/m
2
, paclitaxel 175 mg/m
2
, every 3
weeks.
BMC Cancer 2005, 5:21 http://www.biomedcentral.com/1471-2407/5/21
Page 4 of 6
(page number not for citation purposes)
were observed. The most commonly encountered non-
hematologic toxicities were asthenia and nausea. Other
toxicities are reported per patient and per cycle in Table 2.
Six patients had severe toxicity precluding further treat-
ment. No treatment-related deaths were observed.
Discussion
Single-agent docetaxel has been considered a standard
treatment for patients with anthracycline-pretreated MBC
for several years. Docetaxel monotherapy often demon-
strated response rates of 50% or more in this setting
[17,18]. Ahn et al. also reported, in a similar patient pop-
ulation, 36% response rate and 69 weeks median survival
with docetaxel 75 mg/m
2
every 3 weeks[19].
Platinum-based combinations also have significant activ-
ity in previously treated as well as previously untreated
patients. In several small clinical trials testing the cispla-
tin-based regimens, response rates of 50%-83% were
reported [20]. The North Central Cancer Treatment Group
(NCCTG) evaluated carboplatin combined with paclitaxel
as first-line chemotherapy for MBC [21]. The overall
response rate was 62% and the median time to progres-
sion was 7.3 months. Clearly, platinum-based combina-
tions are very active against MBC, but the relative degree
of toxicity compared with other agents limited their use in
routine clinical practice. Recently, synergism between
platinum and trastuzumab, a novel monoclonal antibody
directed against the protein product of the HER2/neu
oncogene, awaked interest in the use of cisplatin for breast
cancer [6,22].
There are relatively few completed clinical studies involv-
ing platinum-based combination chemotherapy for
anthracycline-resistant MBC. Spielmann et al. evaluated
docetaxel 75 mg/m
2
plus cisplatin 80 mg/m
2
every 3
weeks in 38 patients with anthracycline-resistant MBC,
giving an objective response rate of 36% [23]. Japanese
investigators performed a phase II study of docetaxel 60
mg/m
2
and cisplatin 80 mg/m
2
in patients with anthracy-
cline-pretreated MBC [24]. They reported an overall
response rate of 64%. In a phase II study of docetaxel and
carboplatin, overall response rate of 61% was achieved in
patients with chemotherapy-pretreated MBC [25].
Gelmon et al. combined biweekly paclitaxel with cisplatin
and achieved a response rate of 85% with few septic
events [26].
We classified "anthracycline-resistant" into primary and
secondary. Ando et al. suggested that the status of anthra-
cycline-resistance is important for the prediction of
response to second-line treatment with docetaxel [27].
However, we could not observe significant difference in
the efficacy of docetaxel plus cisplatin between primary
and secondary resistant groups. The different outcomes
might be due to the current situation that there have been
no standard criteria defining anthracycline-resistance and
often intermingled with "anthracycline-pretreated" or
"anthracycline-refractory."
This study demonstrated that a combination of docetaxel
plus cisplatin in a 3-week cycle was an effective and well-
tolerated regimen for patients with anthracycline-resistant
MBC. In this study, the use of docetaxel plus cisplatin
resulted in an overall response rate of 31% and the
median time to progression was 7 months. Significant
improvements in the actuarial survival rate and time to
progression were observed in the group of patients who
achieved objective responses. The main toxicities, gas-
trointestinal, hematological and asthenia, were managea-
ble with dose adjustment and supportive care. Dose
intensities of more than 80% were delivered and 61% of
patients completed 6 cycles of chemotherapy, which is
considered acceptable and expected. We used the planned
dose of cisplatin 60 mg/m
2
every 3 weeks, rather than 75
mg/m
2
cited in a phase I study [14], because we believed
that tolerability of treatment is indispensable in the sal-
vage setting in the management of solid tumors.
With the increasing use of anthracycline-based chemo-
therapy as adjuvant treatment, as well as first-line chemo-
therapy against MBC, patients are frequently exposed to
high cumulative doses of anthracyclines and are therefore
Estimated curves of overall survival and time to progression Figure 1
Estimated curves of overall survival and time to pro-
gression. At a median follow-up of 40.5 months (95% CI,
36.444.6 months), the median time to progression was 6.6
months (95% CI, 3.99.4 months) and the median overall
survival was 22.9 months (95% CI, 17.228.5 months).
BMC Cancer 2005, 5:21 http://www.biomedcentral.com/1471-2407/5/21
Page 5 of 6
(page number not for citation purposes)
at risk of resistance and cardiotoxicity [28]. This combina-
tion of docetaxel with cisplatin may be particularly useful
in patients previously treated with anthracyclines (but
nave to either docetaxel or cisplatin). In addition, for
patients who have already had cardiac failure and have
not received chemotherapy with taxanes as an adjuvant or
as first-line treatment, use of docetaxel plus cisplatin is
considered a better option. More recently, reports that
trastuzumab has a powerful synergistic interaction with
docetaxel and with cisplatin [29], have prompted evalua-
tion of the combination of trastuzumab with docetaxel
and/or platinum in the treatment of MBC [30,31].
Conclusion
In summary, the combination of docetaxel plus cisplatin
is active and safe in patients with anthracycline-resistant
MBC. The activity observed in anthracycline-resistant and
heavily-pretreated patients suggests relative non-cross-
resistance with other drug combinations. Therefore, we
hope that this study could result in a prospective trial to
determine whether this activity translates into actual
improvement in survival and quality of life in patients
with anthracycline-resistant MBC.
Competing interests
The author(s) declare that they have no competing
interests.
Authors' contributions
SHP collected the data, performed the statistical analysis
and drafted the manuscript. EKC, SB, JHL, YDL followed
the patients. DBS designed the study, followed the
patients and helped with the manuscript. All authors read
and approved the final manuscript.
References
1. O'Shaughnessy J, Twelves C, Aapro M: Treatment for anthracy-
cline-pretreated metastatic breast cancer. Oncologist 2002,
7(Suppl 6):4-12.
2. Nabholtz JM, Senn HJ, Bezwoda WR, Melnychuk D, Deschenes L,
Douma J, Vandenberg TA, Rapoport B, Rosso R, Trillet-Lenoir V,
Drbal J, Molino A, Nortier JW, Richel DJ, Nagykalnai T, Siedlecki P,
Wilking N, Genot JY, Hupperets PS, Pannuti F, Skarlos D, Tomiak EM,
Murawsky M, Alakl M, Aapro M, 304 Study Group: Prospective ran-
domized trial of docetaxel versus mitomycin plus vinblastine
in patients with metastatic breast cancer progressing
despite previous anthracycline-containing chemotherapy. J
Clin Oncol 1999, 17(5):1413-1424.
3. Sjostrom J, Blomqvist C, Mouridsen H, Pluzanska A, Ottosson-Lonn
S, Bengtsson NO, Ostenstad B, Mjaaland I, Palm-Sjovall M, Wist E,
Valvere V, Anderson H, Bergh J: Docetaxel compared with
sequential methotrexate and 5-fluorouracil in patients with
advanced breast cancer after anthracycline failure: a ran-
domised phase III study with crossover on progression by the
Scandinavian Breast Group. Eur J Cancer 1999, 35(8):1194-1201.
4. Crown J: A review of the efficacy and safety of docetaxel as
monotherapy in metastatic breast cancer. Semin Oncol 1999,
26(1 Suppl 3):5-9.
5. Valero V, Jones SE, Von Hoff DD, Booser DJ, Mennel RG, Ravdin PM,
Holmes FA, Rahman Z, Schottstaedt MW, Erban JK, Esparza-Guerra
L, Earhart RH, Hortobagyi GN, Burris HA 3rd: A phase II study of
docetaxel in patients with paclitaxel-resistant metastatic
breast cancer. J Clin Oncol 1998, 16(10):3362-3368.
6. Crown J: The platinum agents: a role in breast cancer
treatment? Semin Oncol 2001, 28(1 Suppl 3):28-37.
7. Bissery MC, Nohynek G, Sanderink GJ, Lavelle F: Docetaxel (Tax-
otere): a review of preclinical and clinical experience. Part I:
Preclinical experience. Anticancer Drugs 1995, 6(3):339-355. 363
368
8. Aoe K, Kiura K, Ueoka H, Tabata M, Matsumura T, Chikamori M,
Matsushita A, Kohara H, Harada M: Effect of docetaxel with cis-
platin or vinorelbine on lung cancer cell lines. Anticancer Res
1999, 19(1A):291-299.
9. Schoffski Schoffski P, Catimel G, Planting AS, Droz JP, Verweij J, Schr-
ijvers D, Gras L, Schrijvers A, Wanders J, Hanauske AR: Docetaxel
and cisplatin: an active regimen in patients with locally
advanced, recurrent or metastatic squamous cell carcinoma
of the head and neck. Results of a phase II study of the
EORTC Early Clinical Studies Group. Ann Oncol 1999,
10(1):119-122.
10. Le Chevalier T, Berille J, Zalcberg JR, Millward MJ, Monnier A, Douil-
lard JY, McKeage MJ, James R, Soulas F, Loret C, Bougon N, Bizzari JP:
Overview of docetaxel (Taxotere)/cisplatin combination in
non-small cell lung cancer. Semin Oncol 1999, 26(3 Suppl
11):13-18.
Table 2: Toxicity of chemotherapy*
Grade 1,2 Grade 3,4
/ 39 pts / 189 cycles / 39 pts / 189 cycles
Febrile neutropenia 12 (31%) 12 (22%)
Neutropenia 18 (46%) 28 (15%) 15 (39%) 42 (22%)
Thrombocytopenia 18 (46%) 24 (13%) 6 (15%) 9 (5%)
Nausea/vomiting 27 (69%) 42 (22%) 24 (62%) 42 (22%)
Oral mucositis 4 (10%) 5 (3%) 3 (8%) 3 (2%)
Asthenia 12 (31%) 12 (22%) 15 (39%) 24 (13%)
Peripheral neuropathy 6 (15%) 7 (4%) 6 (15%) 9 (5%)
Hearing impairment 3 (8%) 3 (2%)
Renal insufficiency 1 (3%) 1 (1%)
* Others: abdominal pain(1), skin rash(1), fatigue(6)
Publish with BioMed Central and every
scientist can read your work free of charge
"BioMed Central will be the most significant development for
disseminating the results of biomedical research in our lifetime."
Sir Paul Nurse, Cancer Research UK
Your research papers will be:
available free of charge to the entire biomedical community
peer reviewed and published immediately upon acceptance
cited in PubMed and archived on PubMed Central
yours you keep the copyright
Submit your manuscript here:
http://www.biomedcentral.com/info/publishing_adv.asp
BioMedcentral
BMC Cancer 2005, 5:21 http://www.biomedcentral.com/1471-2407/5/21
Page 6 of 6
(page number not for citation purposes)
11. Roth AD, Maibach R, Martinelli G, Fazio N, Aapro MS, Pagani O,
Morant R, Borner MM, Herrmann R, Honegger H, Cavalli F, Alberto
P, Castiglione M, Goldhirsch A: Docetaxel (Taxotere)-cisplatin
(TC): an effective drug combination in gastric carcinoma.
Swiss Group for Clinical Cancer Research (SAKK), and the
European Institute of Oncology (EIO). Ann Oncol 2000,
11(3):301-306.
12. PA , Paul J, Birt A, Junor EJ, Reed NS, Symonds RP, Atkinson R, Gra-
ham J, Crawford SM, Coleman R, Thomas H, Davis J, Eggleton SP,
Kaye SB: Docetaxel and cisplatin in combination as first-line
chemotherapy for advanced epithelial ovarian cancer. Scot-
tish Gynaecological Cancer Trials Group. J Clin Oncol 1999,
17(7):2069-2080.
13. Dimopoulos MA, Bakoyannis C, Georgoulias V, Papadimitriou C,
Moulopoulos LA, Deliveliotis C, Karayannis A, Varkarakis I, Aravanti-
nos G, Zervas A, Pantazopoulos D, Fountzilas G, Bamias A, Kyriakakis
Z, Anagnostopoulos A, Giannopoulos A, Kosmidis P: Docetaxel
and cisplatin combination chemotherapy in advanced carci-
noma of the urothelium: a multicenter phase II study of the
Hellenic Cooperative Oncology Group. Ann Oncol 1999,
10(11):1385-1388.
14. Pronk LC, Schellens JH, Planting AS, van den Bent MJ, Hilkens PH, van
der Burg ME, de Boer-Dennert M, Ma J, Blanc C, Harteveld M, Bruno
R, Stoter G, Verweij J: Phase I and pharmacologic study of
docetaxel and cisplatin in patients with advanced solid
tumors. J Clin Oncol 1997, 15(3):1071-1079.
15. Gralla RJ, Osoba D, Kris MG, Kirkbride P, Hesketh PJ, Chinnery LW,
Clark-Snow R, Gill DP, Groshen S, Grunberg S, Koeller JM, Morrow
GR, Perez EA, Silber JH, Pfister DG: Recommendations for the
use of antiemetics: evidence-based, clinical practice guide-
lines. American Society of Clinical Oncology. J Clin Oncol 1999,
17(9):2971-2994.
16. Fleming TR: One-sample multiple testing procedure for phase
II clinical trials. Biometrics 1982, 38(1):143-151.
17. Ravdim PM, Burris HA 3rd, Cook G, Eisenberg P, Kane M, Bierman
WA, Mortimer J, Genevois E, Bellet RE: Phase II trial of docetaxel
in advanced anthracycline-resistant or anthracenedione-
resistant breast cancer. J Clin Oncol 1995, 13(12):2879-2885.
18. Valero V, Holmes FA, Walters RS, Theriault RL, Esparza L, Fraschini
G, Fonseca GA, Bellet RE, Buzdar AU, Hortobagyi GN: Phase II trial
of docetaxel: a new, highly effective antineoplastic agent in
the management of patients with anthracycline-resistant
metastatic breast cancer. J Clin Oncol 1995, 13(12):2886-2894.
19. Ahn JB, Shim KY, Park JO, Chung HC, Yoo NC, Chung HC, Kim JH,
Choi JH, Kim HS, Kim HC, Kim WK, Roh JK: The Efficacy and
Safety of Docetaxel in Patients with Anthracycline-pre-
treated Metastatic Breast Cancer: A Multicenter Phase II
Study. J Korean Cancer Assoc 2000, 32(2):235-243.
20. Sledge GW Jr, Roth BJ: Cisplatin in the management of breast
cancer. Semin Oncol 1989, 16(4 suppl 6):110-115.
21. Perez EA, Hillman DW, Stella PJ, Krook JE, Hartmann LC, Fitch TR,
Hatfield AK, Mailliard JA, Nair S, Kardinal CG, Ingle JN: A phase II
study of paclitaxel plus carboplatin as first-line chemother-
apy for women with metastatic breast carcinoma. Cancer
2000, 88(1):124-131.
22. Naruse I, Fukumoto H, Saijo N, Nishio K: Enhanced anti-tumor
effect of trastuzumab in combination with cisplatin. Jpn J Can-
cer Res 2002, 93(5):574-581.
23. Spielmann M, Llombart A, Zelek L, Sverdlin R, Rixe O, Le Cesne A:
Docetaxel-cisplatin combination (DC) chemotherapy in
patients with anthracycline-resistant advanced breast
cancer. Ann Oncol 1999, 10(12):1457-1460.
24. Kariya S, Ogawa Y, Nishioka A, Yoshida S: Docetaxel-cisplatin
combined chemotherapy in Japanese patients with anthracy-
cline-pretreated advanced breast cancer. Oncol Rep 2002,
9(6):1345-1349.
25. Mavroudis D, Alexopoulos A, Malamos N, Ardavanis A, Kandylis C,
Stavrinidis E, Kouroussis Ch, Agelaki S, Androulakis N, Bozionelou V,
Georgoulias V: Salvage treatment of metastatic breast cancer
with docetaxel and carboplatin. A multicenter phase II trial.
Oncology 2003, 64(3):207-212.
26. Gelmon KA, O'Reilly SE, Tolcher AW, Campbell C, Bryce C, Ragaz J,
Coppin C, Plenderleith IH, Ayers D, McDermott B, Nakashima L,
Healey D, Onetto N: Phase I/II trial of biweekly paclitaxel and
cisplatin in the treatment of metastatic breast cancer. J Clin
Oncol 1996, 14(4):1185-1191.
27. Ando M, Watanabe T, Nagata K, Narabayashi M, Adachi I, Katsumata
N: Efficacy of docetaxel 60 mg/m
2
in patients with metastatic
breast cancer according to the status of anthracycline
resistance. J Clin Oncol 2001, 19(2):336-342.
28. Wood WC, Budman DR, Korzun AH, Cooper MR, Younger J, Hart
RD, Moore A, Ellerton JA, Norton L, Ferree CR, Ballow AC, Frei E,
Henderson IC: Dose and dose intensity of adjuvant chemo-
therapy for stage II, node-positive breast carcinoma. N Engl J
Med 1994, 330(18):1253-1259.
29. Slamon DJ, Leyland-Jones B, Shak S, Fuchs H, Paton V, Bajamonde A,
Fleming T, Eiermann W, Wolter J, Pegram M, Baselga J, Norton L:
Use of chemotherapy plus a monoclonal antibody against
HER2 for metastatic breast cancer that overexpresses
HER2. N Engl J Med 2001, 344(11):783-792.
30. Brufsky AM, Cleary D, Fuchs C, Lebish J, Baar J, Evans T, Lembersky
B, Belani CP: First-line chemotherapy for metastatic breast
cancer (MBC) with docetaxel (T), carboplatin (C), and traz-
tuzumab (H) (TCH): A phase II trial. Proc Am Soc Clin Oncol 2003,
22:18. (abstr 71)
31. Crown J, Pegram M: Platinum-taxane combinations in meta-
static breast cancer: an evolving role in the era of molecu-
larly targeted therapy. Breast Cancer Res Treat 2003, 79(Suppl
1):S11-S18.
Pre-publication history
The pre-publication history for this paper can be accessed
here:
http://www.biomedcentral.com/1471-2407/5/21/prepub
Anda mungkin juga menyukai
- Patient Experience in The Treatment of Metastatic Castration-Resistant Prostate Cancer: State of The ScienceDokumen11 halamanPatient Experience in The Treatment of Metastatic Castration-Resistant Prostate Cancer: State of The ScienceLuis ReyBelum ada peringkat
- Neoadjuvant Paclitaxel For Operable Breast Cancer: Multicenter Phase II Trial With Clinical OutcomesDokumen6 halamanNeoadjuvant Paclitaxel For Operable Breast Cancer: Multicenter Phase II Trial With Clinical OutcomesSubhash SugathanBelum ada peringkat
- MeduloblastomaDokumen7 halamanMeduloblastomasilvia erfanBelum ada peringkat
- 2015 EN Clinical Trial of DC Combined With Chemo Against Metastatic Prostate CancerDokumen14 halaman2015 EN Clinical Trial of DC Combined With Chemo Against Metastatic Prostate CancerKhaliElYamaniBelum ada peringkat
- Clinical Benefit in Patients With Advanced Solid Tumors Treated With Modified Citrus Pectin: A Prospective Pilot StudyDokumen8 halamanClinical Benefit in Patients With Advanced Solid Tumors Treated With Modified Citrus Pectin: A Prospective Pilot Studyyafit_armon5854Belum ada peringkat
- MrnaDokumen14 halamanMrnaapi-675909478Belum ada peringkat
- Cancer - 2022 - Paz Ares - RESILIENT Part 1 A Phase 2 Dose Exploration and Dose Expansion Study of Second Line LiposomalDokumen11 halamanCancer - 2022 - Paz Ares - RESILIENT Part 1 A Phase 2 Dose Exploration and Dose Expansion Study of Second Line LiposomalYulia DjatiwardaniBelum ada peringkat
- 166440996249740030Dokumen10 halaman166440996249740030111Belum ada peringkat
- Pembrolizumab For EarlyDokumen74 halamanPembrolizumab For EarlyKishoreChandraKoradaBelum ada peringkat
- Background: Nivolumab For Recurrent Squamous-Cell Carcinoma of The Head and NeckDokumen10 halamanBackground: Nivolumab For Recurrent Squamous-Cell Carcinoma of The Head and NeckjoitBelum ada peringkat
- Long-Term Survival in Patients With Non-Small Cell Lung CancerDokumen7 halamanLong-Term Survival in Patients With Non-Small Cell Lung CancerMrBuu2012Belum ada peringkat
- Eligibility Criteria: Previous Sectionnext SectionDokumen6 halamanEligibility Criteria: Previous Sectionnext Sectionbettzy21Belum ada peringkat
- FDA Approval Summary - Atezolizumab and Durvalumab in Combination With Platinum-Based Chemotherapy in Extensive Stage Small Cell Lung CancerDokumen6 halamanFDA Approval Summary - Atezolizumab and Durvalumab in Combination With Platinum-Based Chemotherapy in Extensive Stage Small Cell Lung CancerasdffdsaBelum ada peringkat
- 1 s2.0 S1083879111002916 MainDokumen8 halaman1 s2.0 S1083879111002916 MainNunungTriwahyuniBelum ada peringkat
- Metronomic Chemotherapy in Low - and Middle-Income Country Is A New Concept in Pediatric OncologyDokumen4 halamanMetronomic Chemotherapy in Low - and Middle-Income Country Is A New Concept in Pediatric OncologyInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- PIIS0923753419310762Dokumen7 halamanPIIS0923753419310762Kamila MuyasarahBelum ada peringkat
- Bradley J Monk First Line Pembrolizumab ChemotherapyDokumen9 halamanBradley J Monk First Line Pembrolizumab ChemotherapyRaúl DíazBelum ada peringkat
- Reuter 2010Dokumen8 halamanReuter 2010Hector Javier BurgosBelum ada peringkat
- Efficacy, Safety, and Health-Related Quality of Life With Camrelizumab Plus Pemetrexed and Carboplatin As First-Line Treatment For Advanced Nonsquamous NSCLC With Brain MetastasesDokumen11 halamanEfficacy, Safety, and Health-Related Quality of Life With Camrelizumab Plus Pemetrexed and Carboplatin As First-Line Treatment For Advanced Nonsquamous NSCLC With Brain MetastasesJOSE DIAZBelum ada peringkat
- Car T LymphomaDokumen14 halamanCar T LymphomaMuneer KhalamBelum ada peringkat
- Concurrent Radiotherapy and Weekly Paclitaxel For Locally Advanced Squmous Cell Carcinoma of Uterine Cervix-Treated Patients at Rural Centre in IndiaDokumen5 halamanConcurrent Radiotherapy and Weekly Paclitaxel For Locally Advanced Squmous Cell Carcinoma of Uterine Cervix-Treated Patients at Rural Centre in IndiaIjsrnet EditorialBelum ada peringkat
- (583950958) Journal Leucopenia Treatment Effiicacy NPCDokumen8 halaman(583950958) Journal Leucopenia Treatment Effiicacy NPCDaniel HoseaBelum ada peringkat
- 2018 - Breast and Ovarian Cancer - BMC Cancer - BauersfeldDokumen10 halaman2018 - Breast and Ovarian Cancer - BMC Cancer - BauersfeldHouda BouachaBelum ada peringkat
- Clinical Impact of External Radiotherapy in Non-Metastatic Esophageal Cancer According To Histopathological SubtypeDokumen12 halamanClinical Impact of External Radiotherapy in Non-Metastatic Esophageal Cancer According To Histopathological SubtypesilviailieBelum ada peringkat
- Novel Immunotherapeutics in B-Cell Precursor ALLDokumen23 halamanNovel Immunotherapeutics in B-Cell Precursor ALLqcywh2000Belum ada peringkat
- Analysis of Compliance, Toxicity and Survival WeeklyDokumen11 halamanAnalysis of Compliance, Toxicity and Survival Weeklydanu20Belum ada peringkat
- Post-Remission Therapy For Acute Myeloid Leukemia: Department of Internal Medicine III, University Hospital Ulm, GermanyDokumen8 halamanPost-Remission Therapy For Acute Myeloid Leukemia: Department of Internal Medicine III, University Hospital Ulm, GermanyMini Bekti NingsihBelum ada peringkat
- Adoptive Transfer of Natural Killer Cells in Combination With Chemotherapy Improves Outcomes of Patients With Locally Advanced Colon Carcinoma.Dokumen15 halamanAdoptive Transfer of Natural Killer Cells in Combination With Chemotherapy Improves Outcomes of Patients With Locally Advanced Colon Carcinoma.Andrew ChenBelum ada peringkat
- NPCDokumen8 halamanNPCArsy Mira PertiwiBelum ada peringkat
- International Seminars in Surgical OncologyDokumen8 halamanInternational Seminars in Surgical OncologyAhmad ShafiqBelum ada peringkat
- Review Article Prostate ImmunotherapyDokumen24 halamanReview Article Prostate ImmunotherapyMohammed AlabdullahBelum ada peringkat
- Keynote 355Dokumen10 halamanKeynote 355Rocio SolervicensBelum ada peringkat
- Tyrosine Kinase Inhibitor PDFDokumen10 halamanTyrosine Kinase Inhibitor PDFsury listinBelum ada peringkat
- Capecitabine Monotherapy For Recurrent and Metastatic Nasopharyngeal CancerDokumen6 halamanCapecitabine Monotherapy For Recurrent and Metastatic Nasopharyngeal Cancertrifamonika23Belum ada peringkat
- DC Vaksin For GBM-Jurnal RevisiDokumen8 halamanDC Vaksin For GBM-Jurnal Revisiallyssa rahmadittaBelum ada peringkat
- Kim 2005Dokumen5 halamanKim 2005cristina_zaharia865440Belum ada peringkat
- Heymach-2022-Design and Rationale For A Phase1Dokumen5 halamanHeymach-2022-Design and Rationale For A Phase1Luca BertolacciniBelum ada peringkat
- Jurnal EBCR 2-1Dokumen7 halamanJurnal EBCR 2-1Aidil Fittriani AyuBelum ada peringkat
- Breast Specimen Handling and Reporting in The Postneoadjuvant Setting Challenges and AdvancesDokumen13 halamanBreast Specimen Handling and Reporting in The Postneoadjuvant Setting Challenges and AdvancesKarlaMaldonadoMonsalveBelum ada peringkat
- Prognostic Predictive Markers Prognostic Predictive Prognostic PredictiveDokumen5 halamanPrognostic Predictive Markers Prognostic Predictive Prognostic Predictivepre_singh2136Belum ada peringkat
- A Phase II Study Evaluating The Efficacy and Safety of AMG 102 (Rilotumumab) in Patients With Recurrent GlioblastomaDokumen10 halamanA Phase II Study Evaluating The Efficacy and Safety of AMG 102 (Rilotumumab) in Patients With Recurrent GlioblastomaSubhash SugathanBelum ada peringkat
- P ('t':'3', 'I':'176969959') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Dokumen8 halamanP ('t':'3', 'I':'176969959') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Cecep Saeful HudaBelum ada peringkat
- 1 s2.0 S0923753419363677 MainDokumen6 halaman1 s2.0 S0923753419363677 MainSamantha AdrianneBelum ada peringkat
- 8424365Dokumen8 halaman8424365Melody CyyBelum ada peringkat
- mdm230 PDFDokumen3 halamanmdm230 PDFDanus RamadanusBelum ada peringkat
- Prognostic Factors For Survival of Patients With Glioblastoma: Recursive Partitioning AnalysisDokumen9 halamanPrognostic Factors For Survival of Patients With Glioblastoma: Recursive Partitioning AnalysisSungjae AnBelum ada peringkat
- 2018 - Novel Drug Treatments of Progressive RadioiodineRefractory Differentiated Thyroid Cancer-Endocrinol Metab Clin N AmDokumen16 halaman2018 - Novel Drug Treatments of Progressive RadioiodineRefractory Differentiated Thyroid Cancer-Endocrinol Metab Clin N AmDr Eduardo Henrique - EndocrinologistaBelum ada peringkat
- Zhang 2021Dokumen10 halamanZhang 2021barti koksBelum ada peringkat
- Navari 2013Dokumen9 halamanNavari 2013ghinwa jaberBelum ada peringkat
- EVIDoa 2200015Dokumen11 halamanEVIDoa 2200015Gustavo BraccoBelum ada peringkat
- AsdasdDokumen10 halamanAsdasdAdhi PratamaBelum ada peringkat
- 551 PDFDokumen5 halaman551 PDFfaidgustisyarifBelum ada peringkat
- Radioimmunotherapy With Tositumomab and Iodine-131 Tositumomab For Non-Hodgkin's LymphomaDokumen8 halamanRadioimmunotherapy With Tositumomab and Iodine-131 Tositumomab For Non-Hodgkin's LymphomaVera MirandaBelum ada peringkat
- Annotated BibDokumen16 halamanAnnotated Bibapi-542958465Belum ada peringkat
- MyelomaDokumen25 halamanMyelomasquallBelum ada peringkat
- Liau Et Al. - 2018 - First Results On Survival From A Large Phase 3 Clinical Trial of An Autologous Dendritic Cell Vaccine in Newly DiagDokumen9 halamanLiau Et Al. - 2018 - First Results On Survival From A Large Phase 3 Clinical Trial of An Autologous Dendritic Cell Vaccine in Newly DiagJoeyOrpillaBelum ada peringkat
- RT en Pancreas Horowitz 2021Dokumen2 halamanRT en Pancreas Horowitz 2021Carlos N. Rojas PuyolBelum ada peringkat
- Sylvester 2018Dokumen3 halamanSylvester 2018DavorIvanićBelum ada peringkat
- Pharmaceutics 14 01630Dokumen27 halamanPharmaceutics 14 01630H. MD Ebr100% (1)
- AACR 2017 Proceedings: Abstracts 1-3062Dari EverandAACR 2017 Proceedings: Abstracts 1-3062Belum ada peringkat
- Zearalenone and Its MetabolitesDokumen12 halamanZearalenone and Its MetabolitesJose Antonio VenacostaBelum ada peringkat
- Metodo Fleming para CovidDokumen28 halamanMetodo Fleming para CovidJose Antonio VenacostaBelum ada peringkat
- FY2020 FOIA Log EcohealtDokumen13 halamanFY2020 FOIA Log EcohealtJose Antonio VenacostaBelum ada peringkat
- Molecules With Potential For Cancer Therapy in The Developing World-Dibenzyl TrisulfideDokumen6 halamanMolecules With Potential For Cancer Therapy in The Developing World-Dibenzyl TrisulfideJose Antonio VenacostaBelum ada peringkat
- Principles and Practice of Phytotherapy 2013 Calculos BiliaresDokumen8 halamanPrinciples and Practice of Phytotherapy 2013 Calculos BiliaresJose Antonio VenacostaBelum ada peringkat
- Frying OilsDokumen10 halamanFrying OilsSuryadi XuBelum ada peringkat
- Posture Statement of Admiral Kurt W. Tidd Commander, United States Southern CommandDokumen36 halamanPosture Statement of Admiral Kurt W. Tidd Commander, United States Southern CommandJose Antonio VenacostaBelum ada peringkat
- Citrus Peel As A Source of Functional Ingredient-A ReviewDokumen8 halamanCitrus Peel As A Source of Functional Ingredient-A ReviewJose Antonio VenacostaBelum ada peringkat
- Occurrence of Hormonally Active Compounds in Food A ReviewDokumen27 halamanOccurrence of Hormonally Active Compounds in Food A ReviewJose Antonio VenacostaBelum ada peringkat
- Non-IgE-mediated Gastrointestinal Food AllergyDokumen11 halamanNon-IgE-mediated Gastrointestinal Food AllergyJose Antonio VenacostaBelum ada peringkat
- Herbal Medicine For The Management of PCOS With Corroborative Clinical FindingsDokumen19 halamanHerbal Medicine For The Management of PCOS With Corroborative Clinical FindingsJose Antonio VenacostaBelum ada peringkat
- The Mediterranean Diet - Health, Science and SocietyDokumen7 halamanThe Mediterranean Diet - Health, Science and SocietyJose Antonio VenacostaBelum ada peringkat
- Indice de Micro Rnas y CancerDokumen26 halamanIndice de Micro Rnas y CancerJose Antonio VenacostaBelum ada peringkat
- Classifications de Carcinogenos Alpha Betica OrderDokumen35 halamanClassifications de Carcinogenos Alpha Betica OrderJose Antonio VenacostaBelum ada peringkat
- Dr. Oz The Good Life 2014-05-06.bakDokumen170 halamanDr. Oz The Good Life 2014-05-06.bakHani K Hussen100% (1)
- Williams Textbook of Endocrinology 14Th Edition Shlomo Melmed MBCHB Macp All ChapterDokumen67 halamanWilliams Textbook of Endocrinology 14Th Edition Shlomo Melmed MBCHB Macp All Chapterchristina.brown369100% (19)
- Entrepreneurial MotivationDokumen11 halamanEntrepreneurial Motivationsagar0989% (9)
- Training Regulations Bread and Pastry Production NC Ii Productiontraining RegulationsDokumen25 halamanTraining Regulations Bread and Pastry Production NC Ii Productiontraining Regulationskaye maleBelum ada peringkat
- Minutes of Meeting On Perioperative NursingDokumen5 halamanMinutes of Meeting On Perioperative NursingJeezreelBelum ada peringkat
- Soal Speaking 11Dokumen9 halamanSoal Speaking 11Naila SaidahBelum ada peringkat
- Ezra MOV WORK WEEK PLAN 1 NEWDokumen6 halamanEzra MOV WORK WEEK PLAN 1 NEWezra britanicoBelum ada peringkat
- Axis III GMCDokumen4 halamanAxis III GMCFasya GhaffarBelum ada peringkat
- Marketing Management Department Unilab Sales Management Procedure (Sales Management Procedure)Dokumen36 halamanMarketing Management Department Unilab Sales Management Procedure (Sales Management Procedure)Jan AcostaBelum ada peringkat
- Detailed Work ExperienceDokumen10 halamanDetailed Work ExperienceFrancis OcwichBelum ada peringkat
- Kardex: Date Ordere D Additional Orders Date Ordered Additional OrdersDokumen14 halamanKardex: Date Ordere D Additional Orders Date Ordered Additional OrdersLRBBelum ada peringkat
- Metanoia: Reflect - Reform - RenewDokumen39 halamanMetanoia: Reflect - Reform - RenewLJ ZamoraBelum ada peringkat
- Microbiological Assay of VitaminsDokumen3 halamanMicrobiological Assay of Vitaminsशिवराज शैटि100% (1)
- Clinical Teaching ProgrammeDokumen11 halamanClinical Teaching ProgrammeKrini TandelBelum ada peringkat
- Smoking With JJ ResearchDokumen17 halamanSmoking With JJ ResearchKittiwin VongsakulBelum ada peringkat
- The Trauma of War in The Poem Dulce Et Decorum EstDokumen1 halamanThe Trauma of War in The Poem Dulce Et Decorum EstRahiem PottingerBelum ada peringkat
- MediCover Graduate StandardDokumen28 halamanMediCover Graduate StandardNhung LuuBelum ada peringkat
- Eldorado Tool & Manufacturing Company LTD Job DescriptionDokumen1 halamanEldorado Tool & Manufacturing Company LTD Job DescriptionEthan StoneBelum ada peringkat
- Professional Behaviors Assessment FinalDokumen31 halamanProfessional Behaviors Assessment Finalapi-623335773Belum ada peringkat
- The Toronto Empathy QuestionnaireDokumen1 halamanThe Toronto Empathy QuestionnaireEleena100% (1)
- Intervention Plan Sy 2022 2023 TemplateDokumen2 halamanIntervention Plan Sy 2022 2023 TemplateJared Ram JuezanBelum ada peringkat
- Asuhan Keperawatan Keluarga - Pengkajian Keluarga - : Ns. Annisa Wuri Kartika,. S.Kep.,M.KepDokumen46 halamanAsuhan Keperawatan Keluarga - Pengkajian Keluarga - : Ns. Annisa Wuri Kartika,. S.Kep.,M.KepAbidah Rahmi HilmyBelum ada peringkat
- Heart PDFDokumen48 halamanHeart PDFdr.chetan2385Belum ada peringkat
- Summative No - 1 - EntrepDokumen3 halamanSummative No - 1 - EntrepMariepet Acantilado Cristuta-AgustinesBelum ada peringkat
- Barang Ed DekatDokumen12 halamanBarang Ed DekatAkhmad “Billy Rafi” HambaliBelum ada peringkat
- Truearth Healthy FoodsDokumen11 halamanTruearth Healthy FoodsBitan RoyBelum ada peringkat
- Tieng Anh 7 HK1Dokumen13 halamanTieng Anh 7 HK1Tran Tu UyenBelum ada peringkat
- Google Forms Survey Sample H.S.B SBA 2023Dokumen8 halamanGoogle Forms Survey Sample H.S.B SBA 2023Brianna ChuramanBelum ada peringkat
- Agen Anti-Infective 2 Jul 2009Dokumen34 halamanAgen Anti-Infective 2 Jul 2009Anonymous SDqQcmgBelum ada peringkat
- PSPA3714 Tutor Activities ANSWERS Chapter 6 2021Dokumen5 halamanPSPA3714 Tutor Activities ANSWERS Chapter 6 2021Kamogelo MakhuraBelum ada peringkat