Posterior Crowns KM
Diunggah oleh
KevalChavdaHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Posterior Crowns KM
Diunggah oleh
KevalChavdaHak Cipta:
Format Tersedia
Dr.
Keyvan Moharamzadeh
Academic Unit of Restorative Dentistry
The University of Sheffield
Posterior Full-Coverage Crowns
Aims
The reasons for crowning a
compromised tooth
Design and biological considerations
Materials
Full coverage crowns: FGC, PFM,
All-ceramic
Tooth preparations
Clinical Stages
The reasons to restore a
compromised tooth
Restoring function (first) and
aesthetics (second)
Restoring structural integrity and
resisting fracture
Integrating with other prosthesis
The Compromised Tooth
Restoring function (first) and
aesthetics (second)
The Compromised Tooth
Restoring structural integrity and
resisting fracture
Endodontically treated
teeth
Weakened tooth due to access
cavity preparation
Loss of Structural integrity
associated with loss of roof of the
pulp chamber
Loss of dentine elasticity
Posterior Teeth
Cuspal protection is required if:
Loss of marginal ridges
Loss of substantial tooth structure
Heavily restored tooth
(Panitvisai P et al., J Endod 1995)
Posterior Teeth
Cuspal protection can be achieved by:
Adhesive restorations
Cusp-coverage cast restorations
Full-coverage restorations
The Compromised Tooth
Restoring function (first) and
aesthetics (second)
Restoring structural integrity and
resisting fracture
Integrating with other prosthesis
Posterior Crowns
Design Considerations
Is the tooth in function?
Appearance
Adjacent Teeth
Periodontal Tissues
Pulp
Retention of the crown to the tooth
Materials
Posterior Crowns
Periodontal Tissues
Plaque control
Periodontal attachment
Alveolar bone levels
Status of periodontal disease
Pulpal death following
crown preparations
Aggressive insult to the tooth,
dentine and odontoblasts
Thermal damage
Local anaesthesia
Dessication
Bacterial contamination
Pulpal death following
crown preparations
10% - Hammerle 2000
19% - Saunders 1999
10% - Valderhaug 1997
6% - Jackson 1992
10% - Kerschbaum 1979 and 1993
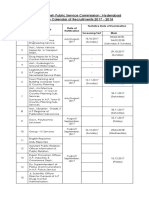
University of Graz
Austria
School of dentistry
Dep. of Prosthodontics
Gerwin Arnetzl
Minimum of 0,7 mm dentine thicknes
is recommended for pulpal protection
Gente 1995, Jde 1986, Robach 1982
0,7mm
Courtesy G. Unterbrink
A shoulder preparation of 1.2 mm
Results in a remaining dentine width of 0.7 mm
only in 50 % of maxillary molars
in all other premolars and molars the
remaining dentine width is less than
0.7mm
A 1.2mm shoulder crown preparation
on a posterior tooth leaves 0.7mm
remaining dentine thickness
Thermal
Chemical
Osmotic
Dessication
Thermal
Chemical
Osmotic
Dessication
Bacterial
Toxins
Posterior Crowns
Materials
Balancing Function
and Aesthetics
Posterior Crowns
Materials
Metal
Metal-Ceramic
Ceramic
Posterior Crowns
Materials
Metal (Full Gold Crown)
Minimal tooth reduction
Least aesthetic (? Not an issue)
Can be adjusted intra-orally (occlusion)
Gold alloy types:
Type I (Soft) was hard enough to stand up to biting forces
but soft enough to burnish against the margins of a cavity
preparation. It was used mostly for one-surface inlays.
Type II (Medium) was less burnishable but hard enough to
stand up in small, multiple surface inlays that did not include
buccal or lingual surfaces.
Type III (hard) The most commonly used type of gold for
all-metal crowns and bridges. A typical type III gold alloy
includes the following metals: Gold 75% Silver 10%
Copper 10% Palladium 3% Zinc 2%
Type IV (Extra hard) was used for partial denture
frameworks but was not used in fixed prosthetics.
Full Gold Crown
Donovan T, 2004: Retrospective clinical
evaluation of 1,314 cast gold restorations
in service from 1 to 52 years.
The survival rates at various time periods were
97% at 9 years, 90.3% at 20 years, 94.9% at
25 years, 98% at 29 years, 96.9% at 39 years,
and 94.1% for restorations in place > 40
years. It appears that properly fabricated cast
gold inlays, onlays, partial veneer crowns, and
full veneer crowns can provide extremely
predictable, long-term restorative service.
Posterior Crowns
Materials
Metal-Ceramic
Metal Core
Extensive buccal tooth reduction
Aesthetics at the cost of tooth tissue
Only the metal component can be
adjusted intra-orally
PFM alloy types:
High-noble alloys have a minimum of 60% noble metals (any
combination of gold, palladium, and silver) and a minimum of 40% by
weight of gold. They usually contain a small amount of tin, indium, or
iron which provides for oxide layer formation. These metals provide a
chemical bond for the porcelain.
Noble alloys (gold, palladium, or silver) contain at least 25% by weight
noble metal. They have relatively high strength, durability, hardness, and
ductility.
Base-metal alloys contain less than 25% noble metal. They are much
harder, stronger and have twice the elasticity of the high-noble and
noblemetal alloys. Castings can be made thinner and still retain the
rigidity needed to support porcelain. They appear to be the ideal metal
for cast-dental restorations and were heavily used for PFM frameworks
due to their low cost and high strength characteristics. Unfortunately,
nickel and beryllium, two of the most commonly used constituents of
base-metal alloys can cause allergic reactions when in intimate contact
with the gingiva.
Ceramic-Fused to metal Crown
PFM crown
Pjetursson et al., 2007. A systematic
review of the survival and complication
rates of all-ceramic and metal-ceramic
reconstructions after an observation
period of at least 3 years. Part I: Single
crowns.
In meta-analysis, the 5-year survival of all-
ceramic crowns was estimated at 93.3% and
95.6% for metal-ceramic crowns.
Posterior Crowns
Materials
All Ceramic
High strength ceramic core
Most aesthetic
Low edge strength
Requires extensive reduction
Intra-oral adjustment not possible
All ceramic Crowns
Wang X et al., 2012. A systematic review of all-
ceramic crowns: clinical fracture rates in
relation to restored tooth type.
All-ceramic crowns demonstrated an acceptable
overall 5-year fracture rate of 4.4%
irrespective of the materials used. Molar
crowns (8.1%) showed a significantly higher 5-
year fracture rate than premolar crowns
(3.0%), and the difference between anterior
(3.0%) and posterior crowns (5.4%) also
achieved significance.
Principles of Tooth
Preparation for crowns
Preservation of tooth structure
Retention
Resistance
Structural durability
Marginal integrity
Posterior Crowns
Retention of the crown
Retention Form: Prevents
dislodgement of the crown in an
axial direction.
Resistance Form: Prevents
dislodgement of the crown due to
rotation from a lateral load.
Tooth Preparation Design
Preparations should be well-defined
and well-finished
Tooth Preparation Design
Preparations should be well-defined and
well-finished
A clear finish line should be visible
Tooth Preparation Design
Preparations should be well-defined and
well-finished
A clear finish line should be visible
Ceramic margins should be a butt-
joint rounded shoulder
Contour to
gingiva
Shoulder
margin
- All Ceramic Crown -
Tooth Preparation Design
Preparations should be well-defined and
well-finished
A clear finish line should be visible
Ceramic margins should be a butt-joint
rounded shoulder
Metal margins should have chamfer
margins
Chamfer margins
Tooth Preparation Design
Preparations should be well-defined and
well-finished
A clear finish line should be visible
Ceramic margins should be a butt-joint
rounded shoulder
Metal margins should have chamfer
margins
All preparation line angles and point
angles are best rounded
Tooth Preparation for All
Ceramic Crown
Minimum occlusal reduction: 1.5mm
>2 mm in
areas of
stress
- All Ceramic Crown -
Occlusal reduction reflects the
morphology of the tooth and the
functional pathways of the occlusion
5 taper
Shoulder
margin
Occlusal
reduction:
>1.5mm
>2 mm in
areas of
stress
Zone of retention
Tooth Preparation for
PFM crown
PFM crown prep
PFM crown prep
Tooth Preparation for Full
Gold Crown
Full Gold Crown Prep
Posterior Crowns
Clinical Stages-Phase I
Pre-op clinical and radiographic
assessment
Further investigations, study models,
diagnostic wax-up
Treatment Planning
Informed consent
Posterior Crowns
Clinical Stages-Phase II
Tooth build up (if necessary) and
Preparation
Impression
Occlusal Record
Temporisation
Fabrication (Lab stage)
Posterior Crowns
Clinical Stages-Phase III
Removal of temporary crown
Try-in of definitive crown
Cementation of definitive crown
Occlusal check
Review
Anda mungkin juga menyukai
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Qi Gong & Meditation - Shaolin Temple UKDokumen5 halamanQi Gong & Meditation - Shaolin Temple UKBhuvnesh TenguriaBelum ada peringkat
- PaintballDokumen44 halamanPaintballGmsnm Usp MpBelum ada peringkat
- Grounds of Divorce Under Hindu Religion or Hindu Law Unit-A: Chapter-IiDokumen42 halamanGrounds of Divorce Under Hindu Religion or Hindu Law Unit-A: Chapter-IiSatyam PathakBelum ada peringkat
- Capacitor BanksDokumen49 halamanCapacitor BanksAmal P RaviBelum ada peringkat
- Monitoring AlkesDokumen41 halamanMonitoring AlkesEndangMiryaningAstutiBelum ada peringkat
- Post Traumatic Stress DisorderDokumen2 halamanPost Traumatic Stress Disorderapi-188978784100% (1)
- Unit 9 Organic Law On Provincial and Local-Level Government (OLPLLG) - SlidesDokumen29 halamanUnit 9 Organic Law On Provincial and Local-Level Government (OLPLLG) - SlidesMark DemBelum ada peringkat
- TDS Shell Spirax s6 Gxme 75w-80Dokumen2 halamanTDS Shell Spirax s6 Gxme 75w-80rstec pyBelum ada peringkat
- Project PlanDokumen55 halamanProject PlanAlfredo SbBelum ada peringkat
- Perioperative Care For CABG PatientsDokumen32 halamanPerioperative Care For CABG PatientsAya EyadBelum ada peringkat
- US Army Medical Course MD0722-100 - Microbiology For The Veterinary SpecialistDokumen114 halamanUS Army Medical Course MD0722-100 - Microbiology For The Veterinary SpecialistGeorges100% (2)
- Ifm Product Innovations PDFDokumen109 halamanIfm Product Innovations PDFJC InquillayBelum ada peringkat
- API 650 10th Edition ErrataDokumen6 halamanAPI 650 10th Edition ErrataJosé Ramón GutierrezBelum ada peringkat
- MelatoninaDokumen32 halamanMelatoninaCodrut GeorgescuBelum ada peringkat
- APPSC Calender Year Final-2017Dokumen3 halamanAPPSC Calender Year Final-2017Krishna MurthyBelum ada peringkat
- Assistive TechnologyDokumen3 halamanAssistive Technologyapi-547693573Belum ada peringkat
- Sedation and Analgesia in Critically Ill Neurologic PatientsDokumen24 halamanSedation and Analgesia in Critically Ill Neurologic PatientsrazaksoedBelum ada peringkat
- English Language Paper 1 - Answer KeyDokumen5 halamanEnglish Language Paper 1 - Answer Keybangtansone1997Belum ada peringkat
- Installation Manual (DH84309201) - 07Dokumen24 halamanInstallation Manual (DH84309201) - 07mquaiottiBelum ada peringkat
- BARCODESDokumen7 halamanBARCODESChitPerRhosBelum ada peringkat
- Capacity Requirement PlanningDokumen17 halamanCapacity Requirement PlanningvamsibuBelum ada peringkat
- Preservation and Collection of Biological EvidenceDokumen4 halamanPreservation and Collection of Biological EvidenceanastasiaBelum ada peringkat
- Drill Site Audit ChecklistDokumen5 halamanDrill Site Audit ChecklistKristian BohorqzBelum ada peringkat
- RCM Design and ImplementationDokumen34 halamanRCM Design and ImplementationRozi YudaBelum ada peringkat
- How To Create Your Cosmetic Product Information FileDokumen12 halamanHow To Create Your Cosmetic Product Information Filewill100% (3)
- Rahu Yantra Kal Sarp Yantra: Our RecommendationsDokumen2 halamanRahu Yantra Kal Sarp Yantra: Our RecommendationsAbhijeet DeshmukkhBelum ada peringkat
- Laughter, It Is Good For YouDokumen2 halamanLaughter, It Is Good For YouClaire B.L.Belum ada peringkat
- Private Standard: Shahram GhanbarichelaresiDokumen2 halamanPrivate Standard: Shahram Ghanbarichelaresiarian tejaratBelum ada peringkat
- SRV SLB222 en - 05062020Dokumen2 halamanSRV SLB222 en - 05062020Nguyen ThuongBelum ada peringkat
- UIP ResumeDokumen1 halamanUIP ResumeannabellauwinezaBelum ada peringkat