Definitions and Classifications: A. Coker and R. Oliver
Diunggah oleh
Anonymous pJfAvl0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
22 tayangan6 halamanpost partum hemorrhage
Judul Asli
PPH-Chap-02
Hak Cipta
© © All Rights Reserved
Format Tersedia
PDF, TXT atau baca online dari Scribd
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen Inipost partum hemorrhage
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PDF, TXT atau baca online dari Scribd
0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
22 tayangan6 halamanDefinitions and Classifications: A. Coker and R. Oliver
Diunggah oleh
Anonymous pJfAvlpost partum hemorrhage
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PDF, TXT atau baca online dari Scribd
Anda di halaman 1dari 6
2
DEFINITIONS AND CLASSIFICATIONS
A. Coker and R. Oliver
INTRODUCTION
Conventionally, the term postpartum hemor-
rhage is applied to pregnancies beyond 20
weeks gestation. Although bleeding at an earlier
gestational age may have a similar etiology and
management to postpartum hemorrhage, these
are usually referred to as spontaneous
miscarriages.
There has been no significant change in the
definitions or classification over the past 50
years; this does not reflect the advances made
in medical and surgical treatment over this
period
1
. A widely used definition currently is
that proposed by the World Health Organiza-
tion (WHO) in 1990 as any blood loss from the
genital tract during delivery above 500 ml
2
.
The average blood loss during a normal
vaginal delivery has been estimated at 500 ml;
however, around 5% of women would lose
greater than 1000 ml during a vaginal birth
36
.
Cesarean deliveries are associated with an aver-
age estimated blood loss of 1000 ml
7
. There is,
therefore, a degree of overlap in the acceptable
range of blood loss for vaginal and Cesarean
deliveries.
PURPOSE OF CLASSIFICATION
Classification of postpartum hemorrhage is
desirable for the following reasons. First, due to
the rapidity of disease progression, there is an
overriding clinical need to determine the most
suitable line of management. The urgency of
intervention depends on the rate of the patients
decline or deterioration.
The second reason for classification is to
assess the prognosis. This may help to deter-
mine the immediate, medium and long-term
clinical outcome. Therefore, a prognostic classi-
fication will guide the degree of aggressiveness
of the intervention, especially as management
may involve more than one clinical specialty.
It will also help to decide on the optimal site
for subsequent care, for example in a high-
dependency unit or intensive care unit, if such
exist in the hospital.
The third reason is to allow effective
communication based on standardization of the
estimate of the degree of hemorrhage, thus stan-
dardizing differing management options. The
initial assessment is usually made by the staff
available on site, and these are often relatively
junior medical or midwifery personnel. They, in
turn, have to assess the severity of bleeding and
summon help or assistance as required. Thus, a
standardized easily applicable working classifi-
cation facilitates effective communication and
obviates inter-observer variation.
CLASSIFICATIONS IN USE
Conventional temporal classification
Traditionally, the classification of postpartum
hemorrhage has been based on the timing of the
onset of bleeding in relation to the delivery.
Hemorrhage within the first 24 h of vaginal
delivery is termed either early or primary
postpartum hemorrhage, whereas bleeding
occurring afterwards, but within 12 weeks of
delivery, is termed late or secondary postpartum
hemorrhage
8
.
Secondary postpartum hemorrhage is less
common than primary postpartum hemorrhage,
affecting 13% of all deliveries. In both cases,
the true blood loss is often underestimated due
to the difficulty with visual quantitation
9,10
.
11
33
Z:\Sapiens Publishing\A5211 - Postpartum Hemorrhage\Make-up\Postpartum Hemorrhage - Voucher Proofs #T.vp
30 August 2006 14:19:07
Color profile: Generic CMYK printer profile
Composite Default screen
Classification based on quantification of
blood loss
Amount of blood lost
Blood loss at delivery is estimated using various
methods. These range from the less modern
methods of counting blood-soaked pieces of
cloth or kangas used by traditional birth
attendants in rural settings, to more modern
techniques such as calculating the blood loss
by subtraction after weighing all swabs using
sensitive weighing scales
11
.
The International Statistical Classification
of Diseases and Related Health Problems,
Tenth Revision, Australian Modification
(ICD-10-AM) describes postpartum hemor-
rhage as a blood loss of 500 ml or more for a
vaginal delivery and 750 ml or more in associa-
tion with Cesarean delivery
12
.
Change in hematocrit
The American College of Obstetricians and
Gynecologists advocates the definitions of either
a 10% change in hematocrit between the ante-
natal and postpartum periods, or a need for
erythrocyte transfusion
13
.
Rapidity of blood loss
In attempts to overcome these inconsistencies,
the classification of postpartum hemorrhage has
also been based on the rapidity of blood loss.
Severe hemorrhage has been classified as blood
loss > 150 ml/min (within 20 min, causing loss
of more than 50% of blood volume) or a sudden
blood loss > 15002000 ml (uterine atony; loss
of 2535% of blood volume)
14
.
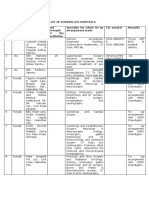
Volume deficit
A form of standardized classification described
by Benedetti considers four classes of hemor-
rhage
15
(Table 1). The class of hemorrhage
reflects the volume deficit, and this is not neces-
sarily the same as the volume of blood loss.
Class 1 The average 60 kg pregnant woman
has a blood volume of 6000 ml at 30 weeks ges-
tation. A volume loss of less than 900 ml in such
a woman will rarely lead to any symptoms and
signs of volume deficit and will not require any
acute treatment.
Class 2 A blood loss of 12001500 ml will
begin to manifest clinical signs, such as a rise in
pulse and respiratory rate. There may also be
recordable blood pressure changes, but not the
classic cold clammy extremities.
Class 3 These are patients in whom the blood
loss is sufficient to cause overt hypotension. The
blood loss is usually around 18002100 ml.
There are signs of tachycardia (120160 bpm),
cold clammy extremities and tachypnea.
Class 4 This is commonly described as massive
obstetric hemorrhage. When the volume loss
exceeds 40%, profound shock ensues and the
blood pressure and pulse are not easily record-
able. Immediate and urgent volume therapy is
necessary, as this quantity of blood loss can
be fatal secondary to circulatory collapse and
cardiac arrest.
Classification based on causative factors
The causes of postpartum hemorrhage can also
form a basis of classification (Table 2).
Causes of primary postpartum hemorrhage
Primary postpartum hemorrhage is traditionally
considered as a disorder of one or more of the
four processes: uterine atony, retained clots or
placental debris, genital lesions or trauma, and
disorders of coagulation. An aide memoire is the
four Ts: tonus, tissue, trauma and thrombin.
Uterine atony alone accounts for 7590% of
cases of postpartum hemorrhage.
12
POSTPARTUM HEMORRHAGE
Hemorrhage
class
Acute blood loss
(ml)
Percentage
lost
1
2
3
4
900
12001500
18002100
2400
15
2025
3035
40
Table 1 Benedettis classification of hemorrhage
15
34
Z:\Sapiens Publishing\A5211 - Postpartum Hemorrhage\Make-up\Postpartum Hemorrhage - Voucher Proofs #T.vp
30 August 2006 14:19:07
Color profile: Generic CMYK printer profile
Composite Default screen
Classification based on clinical signs and
symptoms
Any bleeding that results in or could result
in hemodynamic instability, if untreated,
is considered as postpartum hemorrhage
(Table 3).
PITFALLS OF CURRENT
CLASSIFICATIONS
The drawbacks of a classification based solely
on blood loss or hematocrit include the fact that
this is a retrospective assessment and may not
represent the current clinical situation. To a
certain extent, any classification is of limited use
to a clinician faced with active and continuous
bleeding.
The change in hematocrit depends on the
timing of the test and the amount of fluid
resuscitation previously administered
16
. It could
also be affected by extraneous factors such as
prepartum hemoconcentration, which may exist
in conditions such as pre-eclampsia.
Where the diagnosis is made by a clinical
estimate of blood loss, there is often signifi-
cant underestimation. The WHO definition of
500 ml is increasingly becoming irrelevant, as
13
Definitions and classifications
Causes of primary PPH
Tonus (uterine atony)
Uterine overdistention: multiparity, polyhydramnios, macrosomia
Uterine relaxants: nifedipine, magnesium, beta-mimetics, indomethacin, nitric oxide donors
Rapid or prolonged labor
Oxytoxics to induce labor
Chorioamnionitis
Halogenated anesthetics
Fibroid uterus
Tissue
Impediment to uterine contraction/retraction: multiple fibroids, retained placenta
Placental abnormality: placenta accreta, succenturiate lobe
Prior uterine surgery: myomectomy, classical or lower segment Cesarean section
Obstructed labor
Prolonged third stage of labor
Excessive traction on the cord
Trauma
Vulvovaginal injury
Episiotomy/tears
Macrosomia
Precipitous delivery
Thrombin (coagulopathy)
Acquired during pregnancy: thrombocytopenia of HELLP syndrome, DIC (eclampsia, intrauterine fetal
death, septicemia, placenta abruptio, amniotic fluid embolism), pregnancy-induced hypertension, sepsis
Hereditary: Von Willebrands disease
Anticoagulant therapy: valve replacement, patients on absolute bedrest
Causes of secondary PPH
Uterine infection
Retained placental fragments
Abnormal involution of placental site
Adapted from Wac et al. Female Patient 2005;30:19
Table 2 Classification of postpartum hemorrhage (PPH) according to causative factors
35
Z:\Sapiens Publishing\A5211 - Postpartum Hemorrhage\Make-up\Postpartum Hemorrhage - Voucher Proofs #T.vp
30 August 2006 14:19:07
Color profile: Generic CMYK printer profile
Composite Default screen
most healthy mothers in the developed world
can cope with a blood loss of less than 500 ml
without any hemodynamic compromise.
Classifications based on the need for blood
transfusion alone are also of limited value
as the practice of blood transfusion varies
widely according to local circumstances and
attitudes to transfusion of both patients and
physicians
17
.
The clinical application of such a classifica-
tion may, in addition, be limited because of
inherent individual differences in response
to blood loss. Hemodynamic compensation
depends on the initial hemoglobin levels prior to
onset of bleeding, and these vary among healthy
individuals. For these reasons, reliance on a
classification solely based on the amount of
blood loss and without consideration of clinical
signs and symptoms may lead to inconsistency
with management.
NEED FOR A CLINICAL AND
PROGNOSTIC CLASSIFICATION
Universally, guidelines on the management of
postpartum hemorrhage have reiterated the
importance of accurate estimation of blood loss,
and the clinical condition of the hemorrhaging
patient. This was further emphasized in the
19881990 Confidential Enquiries into Mater-
nal Deaths in the United Kingdom (CEMD)
18
and reiterated in the 19911993 report as a
list of six bullet points, the first being accurate
estimation of blood loss
19
.
The ideal classification of postpartum hem-
orrhage should take into consideration both the
volume loss and the clinical consequences of
such loss. The recorded parameters should be
easily measurable and reproducible. This will
help in providing an accurate and consistent
assessment of loss, which can readily be com-
municated and incorporated into most labor
ward protocols.
PROPOSED CLASSIFICATION
The 500 ml limit as defined by WHO
2
should
be considered as an alert line; the action line is
then reached when the vital functions of the
woman are endangered. In healthy women, this
usually occurs after the blood loss has exceeded
1000 ml.
We propose a classification (Table 4)
wherein the volume loss is assessed in conjunc-
tion with clinical signs and symptoms. We pro-
pose this classification as being mainly useful in
fully equipped hospitals and obstetric units. It is
not being proposed for full implementation in
areas which are resource-poor.
Our adaptation of a previously described
classification
15
will fulfil most of these criteria.
This guideline adopts a practical approach
whereby a perceived loss of 5001000 ml (in
the absence of clinical signs of cardiovascular
instability) prompts basic measures of monitor-
ing and readiness for resuscitation (alert line),
whereas a perceived loss of > 1000 ml or a
smaller loss associated with clinical signs of
shock (hypotension, tachycardia, tachypnea,
oliguria or delayed peripheral capillary fill-
ing) prompts a full protocol of measures to
resuscitate, monitor and arrest bleeding.
14
POSTPARTUM HEMORRHAGE
Blood loss
Blood pressure
(mmHg) % ml Signs and symptoms
1015
1525
2535
3545
5001000
10001500
15002000
20003000
normal
slightly low
7080
5070
palpitations, dizziness, tachycardia
weakness, sweating, tachycardia
restlessness, pallor, oliguria
collapse, air hunger, anuria
Adapted from Bonnar J. Baillieres Best Pract Res Clin Obstet Gynaecol 2000;14:1
Table 3 Symptoms related to blood loss with postpartum hemorrhage
36
Z:\Sapiens Publishing\A5211 - Postpartum Hemorrhage\Make-up\Postpartum Hemorrhage - Voucher Proofs #T.vp
30 August 2006 14:19:08
Color profile: Generic CMYK printer profile
Composite Default screen
References
1. El-Refaey H, Rodeck C. Post partum haemor-
rhage: definitions, medical and surgical manage-
ment. A time for change. Br Med Bull 2003;67:
20517
2. World Health Organization. The Prevention and
Management of Postpartum Haemorrhage. Report
of a Technical Working Group, Geneva, 36
July, 1989. Unpublished document. WHO/
MCH/90.7. Geneva: World Health Organiza-
tion, 1990
3. Pritchard JA, Baldwin RM, Dickey JC, Wiggins
KM. Blood volume changes in pregnancy and
the puerperium. Am J Obstet Gynecol 1962;84:
127182
4. Newton M. Postpartum hemorrhage. Am J
Obstet Gynecol 1966;94:71117
5. De Leeuw NK, Lowenstein L, Tucker EC,
Dayal S. Correlation of red cell loss at delivery
with changes in red cell mass. Am J Obstet
Gynecol 1968;100:1092101
6. Letsky E. The haematological system. In Hytten
F, Chamberlain G, eds. Clinical Physiology in
Obstetrics, 2nd edn. Oxford: Blackwell, 1991:
275
7. Baskett TF, ed. Complications of the third stage
of labour. In Essential Management of Obstetrical
Emergencies, 3rd edn. Bristol, UK: Clinical Press,
1999:196201
8. Alexander J, Thomas P, Sanghera J. Treatments
for secondary postpartum haemorrhage.
Cochrane Database of Systematic Reviews,
2005, Issue 3
9. Gahres EE, Albert SN, Dodek SM. Intrapartum
blood loss measured with Cr 51-tagged erythro-
cytes. Obstet Gynecol 1962;19:45562
10. Newton M, Mosey LM, Egli GE, Gifford WB,
Hull CT. Blood loss during and immediately
after delivery. Obstet Gynecol 1961;17:918
11. Prata N, Mbaruku G, Campbell M. Using the
kanga to measure post partum blood loss. Int J
Gynaecol Obstet 2005;89:4950
12. National Centre for Classification in Health.
Australian Coding Standards. The International
Statistical Classification of Diseases and Related
Health Problems, Tenth Revision, Australian
Modification (ICD-10-AM). Sydney, Australia,
2002
13. American College of Gynecologists and Obstetri-
cians. Quality Assurance in Obstetrics and Gynecol-
ogy. Washington DC: American College of
Obstetricians and Gynecologists, 1989
14. Sobieszczyk S, Breborowicz GH. Management
recommendations for postpartum hemorrhage.
Arch Perinatal Med 2004;10:1
15. Benedetti T. Obstetric haemorrhage. In Gabbe
SG, Niebyl JR, Simpson JL, eds. A Pocket
Companion to Obstetrics, 4th edn. New York:
Churchill Livingstone, 2002:Ch 17
15
Definitions and classifications
Hemorrhage class Estimated blood loss (ml) Blood volume loss (%) Clinical signs and symptoms
0 (normal loss) < 500 < 10 none
ALERT LINE
1 5001000 < 15 minimal
ACTION LINE
2 12001500 2025 urine output
pulse rate
respiratory rate
postural hypotension
narrow pulse pressure
3 18002100 3035 hypotension
tachycardia
cold clammy
tachypnea
4 > 2400 > 40 profound shock
Need observation replacement therapy
Replacement therapy and oxytocics
Urgent active management
Critical active management (50% mortality if not managed actively)
Table 4 Proposed classification. Adapted from Benedetti
15
37
Z:\Sapiens Publishing\A5211 - Postpartum Hemorrhage\Make-up\Postpartum Hemorrhage - Voucher Proofs #T.vp
30 August 2006 14:19:08
Color profile: Generic CMYK printer profile
Composite Default screen
16. Cunningham FG, Gant NF, Leveno KJ, et al.,
eds. Conduct of normal labor and delivery.
In Williams Obstetrics, 21st edn. New York:
McGraw-Hill, 2001:3205
17. Schuurmans N, MacKinnon C, Lane C, Etches
D. Prevention and management of postpartum
haemorrhage. J Soc Obstet Gynaecol Canada
2000;22:27181
18. Hibbard BM. Report on Confidential Enquiries
into Maternal Deaths in the United Kingdom,
19881990. London: Her Majestys Stationery
Office, 1994
19. Anonymous. Report on Confidential Enquiries
into Maternal Deaths in the United Kingdom,
19911993. London: Her Majestys Stationery
Office, 1996
16
POSTPARTUM HEMORRHAGE
38
Z:\Sapiens Publishing\A5211 - Postpartum Hemorrhage\Make-up\Postpartum Hemorrhage - Voucher Proofs #T.vp
30 August 2006 14:19:08
Color profile: Generic CMYK printer profile
Composite Default screen
Anda mungkin juga menyukai
- Medical Slang, Acronyms and Veterinary TermsDokumen26 halamanMedical Slang, Acronyms and Veterinary TermsAneez Abdulsamad100% (1)
- Obstetric Emergencies PDFDokumen15 halamanObstetric Emergencies PDFEdi BackyBelum ada peringkat
- Clinical Surgery Review 2023: For USMLE Step 2 CK and COMLEX-USA Level 2Dari EverandClinical Surgery Review 2023: For USMLE Step 2 CK and COMLEX-USA Level 2Belum ada peringkat
- Overview of Postpartum Hemorrhage - UpToDateDokumen48 halamanOverview of Postpartum Hemorrhage - UpToDatewendy100% (1)
- RCOG Guideline 2011Dokumen24 halamanRCOG Guideline 2011John DoeBelum ada peringkat
- Postpartum HemorrhageDokumen53 halamanPostpartum HemorrhageDr_Soranus100% (2)
- ACOG Practice Bulletin No 183 Postpartum-Hemorrhage-2017Dokumen19 halamanACOG Practice Bulletin No 183 Postpartum-Hemorrhage-2017Leslie GuzmanBelum ada peringkat
- ACOG Practice Bulletin No 183 Postpartum-Hemorrhage-2017Dokumen19 halamanACOG Practice Bulletin No 183 Postpartum-Hemorrhage-2017dinnhanifahBelum ada peringkat
- DHARSHINI (PPH)Dokumen5 halamanDHARSHINI (PPH)Rashvinder Kaur PurbaBelum ada peringkat
- Disseminated Intravascular CoagulationDokumen27 halamanDisseminated Intravascular CoagulationMouhammad DawoudBelum ada peringkat
- Nelson JaundiceDokumen7 halamanNelson JaundiceJesly CharliesBelum ada peringkat
- Emily B. Baglione CRNA, BSN, MS,: Chief OB CRNA, Anesthesia Group of AlbanyDokumen55 halamanEmily B. Baglione CRNA, BSN, MS,: Chief OB CRNA, Anesthesia Group of AlbanyAsyfiyaTami100% (1)
- ACOG Practice Bulletin No 183 Postpartum-Hemorrhage-2017Dokumen19 halamanACOG Practice Bulletin No 183 Postpartum-Hemorrhage-2017Faizah Arifin100% (1)
- Best Practice in Outpatient Hysteroscopy: Green-Top Guideline No. 59Dokumen22 halamanBest Practice in Outpatient Hysteroscopy: Green-Top Guideline No. 59biiicaBelum ada peringkat
- Nursing Care Plan for Mrs. Yolanda Yambut BenavidezDokumen8 halamanNursing Care Plan for Mrs. Yolanda Yambut BenavidezRafi LabBelum ada peringkat
- Seminar On Complication of 3rd Stage PPHDokumen13 halamanSeminar On Complication of 3rd Stage PPHjuhi labana0% (1)
- Postpartum HaemorrhageDokumen44 halamanPostpartum Haemorrhageella_28Belum ada peringkat
- English For NursingDokumen30 halamanEnglish For NursingKiki SeptyantiBelum ada peringkat
- Informatics Quiz 1 NAME: - DATE: - I. Multiple Choice. Choose The Best Answer. Encircle The Letter of The Correct AnswerDokumen2 halamanInformatics Quiz 1 NAME: - DATE: - I. Multiple Choice. Choose The Best Answer. Encircle The Letter of The Correct Answerlouie roderosBelum ada peringkat
- Critical CareDokumen12 halamanCritical CaremiltoncesargomezBelum ada peringkat
- Postpartum Hemorrhage Causes and PreventionDokumen21 halamanPostpartum Hemorrhage Causes and PreventionLillian HerreraBelum ada peringkat
- SDMS ID: P2010/0496-001 2.9/09WACS Title: Management of Postpartum HaemorrhageDokumen11 halamanSDMS ID: P2010/0496-001 2.9/09WACS Title: Management of Postpartum HaemorrhageYwagar YwagarBelum ada peringkat
- Maternal Haemorrhage: Causes, Risks, ManagementDokumen10 halamanMaternal Haemorrhage: Causes, Risks, ManagementWindy MentariiBelum ada peringkat
- Baird 2017Dokumen20 halamanBaird 2017Jhasmyn MartinezBelum ada peringkat
- Causes and Management of Postpartum HemorrhageDokumen6 halamanCauses and Management of Postpartum Hemorrhagemusyawarah melalaBelum ada peringkat
- Obstetrics V13 Obstetric Emergencies Chapter Diagnosis and Management of Shock in Postpartum Hemorrhage 1698108756Dokumen12 halamanObstetrics V13 Obstetric Emergencies Chapter Diagnosis and Management of Shock in Postpartum Hemorrhage 1698108756laucel peñaBelum ada peringkat
- Santoso2005Dokumen11 halamanSantoso2005ayubahriBelum ada peringkat
- Antepartum and Postpartum Hemorrhage: Fitsum AshebirDokumen64 halamanAntepartum and Postpartum Hemorrhage: Fitsum Ashebirzuzuyasi65Belum ada peringkat
- Obstetrics V13 Obstetric Emergencies Chapter Diagnosis and Management of Shock in Postpartum Hemorrhage 1682196492Dokumen14 halamanObstetrics V13 Obstetric Emergencies Chapter Diagnosis and Management of Shock in Postpartum Hemorrhage 1682196492lizzieBelum ada peringkat
- 41 Management of Obstetric HaemorrhageDokumen5 halaman41 Management of Obstetric HaemorrhageParvathy R NairBelum ada peringkat
- Hemorragia Intraparto PDFDokumen12 halamanHemorragia Intraparto PDFana catalinaBelum ada peringkat
- Intrapartum HemorrhageDokumen12 halamanIntrapartum HemorrhageLillian HerreraBelum ada peringkat
- Hemorragia Posparto-AcogDokumen19 halamanHemorragia Posparto-AcogCristian LaraBelum ada peringkat
- Postpartum Hemorrhage (PPH) : Layal Mansour, Med IVDokumen37 halamanPostpartum Hemorrhage (PPH) : Layal Mansour, Med IVlayalmansourBelum ada peringkat
- Understanding Blood Product Replacement for Postpartum HemorrhageDokumen13 halamanUnderstanding Blood Product Replacement for Postpartum HemorrhageEvelyn Yanet Facho BautistaBelum ada peringkat
- Emergencia 0bstétricas PDFDokumen15 halamanEmergencia 0bstétricas PDFgladymarBelum ada peringkat
- New insights for defining and diagnosing postpartum hemorrhageDokumen7 halamanNew insights for defining and diagnosing postpartum hemorrhageRabbi'ahBelum ada peringkat
- Dr. Robert Casanova - Third-Trimester BleedingDokumen13 halamanDr. Robert Casanova - Third-Trimester Bleedingzeek powerBelum ada peringkat
- Post Partum HemorrhageDokumen10 halamanPost Partum HemorrhagedenekeBelum ada peringkat
- Diagnosis and Management of Shock in Postpartum HemorrhageDokumen12 halamanDiagnosis and Management of Shock in Postpartum HemorrhageJeferson CuaranBelum ada peringkat
- Prevention and Management of Postpartum Haemorrhage: Green-Top Guideline No. 52Dokumen24 halamanPrevention and Management of Postpartum Haemorrhage: Green-Top Guideline No. 52naeem19860% (1)
- Obstetric HaemorrhageDokumen4 halamanObstetric Haemorrhageapi-142637023Belum ada peringkat
- Postpartum Hemorrhage: Medical and Minimally Invasive ManagementDokumen33 halamanPostpartum Hemorrhage: Medical and Minimally Invasive ManagementMayrita NamayBelum ada peringkat
- Obstetric EmergenciesDokumen15 halamanObstetric EmergenciesAndi SaputraBelum ada peringkat
- Postpartum Hemorrhage Risks and PreventionDokumen21 halamanPostpartum Hemorrhage Risks and PreventionCintya PradyanthiBelum ada peringkat
- Maternal Haemorrhage: Leading Cause of Preventable Maternal DeathDokumen10 halamanMaternal Haemorrhage: Leading Cause of Preventable Maternal DeathSakena NurzaBelum ada peringkat
- Hemorragia PostpartoDokumen34 halamanHemorragia PostpartoGiiszs AlvarezBelum ada peringkat
- Postpartum Hemorrhage - Medical and Minimally Invasive Management - Uptodate FreeDokumen59 halamanPostpartum Hemorrhage - Medical and Minimally Invasive Management - Uptodate FreecarolinaBelum ada peringkat
- Postpartum Hemorrhage Management The Importance ofDokumen5 halamanPostpartum Hemorrhage Management The Importance ofBhawna JoshiBelum ada peringkat
- Postpartum Hemorrhage Management The Importance of PDFDokumen5 halamanPostpartum Hemorrhage Management The Importance of PDFBhawna JoshiBelum ada peringkat
- Coagulation Management and Transfusion in Massive Postpartum HemorrhageDokumen7 halamanCoagulation Management and Transfusion in Massive Postpartum HemorrhageAlberto LiraBelum ada peringkat
- Nejmra 1513247Dokumen11 halamanNejmra 1513247Franz Huber QueiroloBelum ada peringkat
- B41. Su-Et-Al PPH PDFDokumen21 halamanB41. Su-Et-Al PPH PDFjhon heriansyahBelum ada peringkat
- Hemorragia Obstetrica Masiva - 024635Dokumen13 halamanHemorragia Obstetrica Masiva - 024635Maykel Vivas HueteBelum ada peringkat
- Antepartum Hemorrhage GuideDokumen4 halamanAntepartum Hemorrhage GuideElvisBelum ada peringkat
- Antepartum HemorrhageDokumen12 halamanAntepartum HemorrhageMohammed AbdBelum ada peringkat
- PPH Introduction 1Dokumen95 halamanPPH Introduction 1regine maeBelum ada peringkat
- Post Partum HemorrhageDokumen38 halamanPost Partum Hemorrhageariani putri devantiBelum ada peringkat
- Postpartum HaemorrhageDokumen17 halamanPostpartum HaemorrhageKehem Pelhem FelhemBelum ada peringkat
- Postpartum HaemorrhageDokumen17 halamanPostpartum HaemorrhageKehem Pelhem FelhemBelum ada peringkat
- Nejmra 1513247Dokumen11 halamanNejmra 1513247Jose BoderoBelum ada peringkat
- Third Trimester BleedingDokumen10 halamanThird Trimester BleedingGustavo CaicutoBelum ada peringkat
- Nursing Role in Emergency Delivery in Women WithDokumen11 halamanNursing Role in Emergency Delivery in Women WithFeFo GhBelum ada peringkat
- Narrative Report ContentsDokumen15 halamanNarrative Report ContentsGladie Ann Dela RosaBelum ada peringkat
- Hemophilia and Hemostasis: A Case-Based Approach to ManagementDari EverandHemophilia and Hemostasis: A Case-Based Approach to ManagementAlice D. MaBelum ada peringkat
- HP May06 MassiveDokumen7 halamanHP May06 MassiveAnonymous pJfAvlBelum ada peringkat
- WHO Dengue Guidelines 2013Dokumen160 halamanWHO Dengue Guidelines 2013Jason MirasolBelum ada peringkat
- EScholarship UC Item 8k05n5csDokumen10 halamanEScholarship UC Item 8k05n5csAnonymous pJfAvlBelum ada peringkat
- Eclampsia and Preeclampsia Pharmacological ManagementDokumen4 halamanEclampsia and Preeclampsia Pharmacological ManagementTony HermawanBelum ada peringkat
- Primary Bone TumorsDokumen12 halamanPrimary Bone TumorsAnonymous pJfAvlBelum ada peringkat
- HELLP SyndromeDokumen8 halamanHELLP SyndromeMerlyn RumtheBelum ada peringkat
- HELLP SyndromeDokumen15 halamanHELLP Syndromebrendiux_982383Belum ada peringkat
- Comparative Study Between Tubularized Incised Plate (Snodgrass) Urethroplasty and Reverse FlapDokumen5 halamanComparative Study Between Tubularized Incised Plate (Snodgrass) Urethroplasty and Reverse FlapAnonymous pJfAvlBelum ada peringkat
- Severe Pre-Eclampsia and EclampsiaDokumen15 halamanSevere Pre-Eclampsia and Eclampsiasmansa123Belum ada peringkat
- Antibiotics For Incomplete Abortion (Review) : May W, Gülmezoglu AM, Ba-Thike KDokumen12 halamanAntibiotics For Incomplete Abortion (Review) : May W, Gülmezoglu AM, Ba-Thike KSilvi AnjaniBelum ada peringkat
- PDF 39-41 Bilateral Proliferating Brenner Tumor of The OvaryDokumen3 halamanPDF 39-41 Bilateral Proliferating Brenner Tumor of The OvaryAnonymous pJfAvlBelum ada peringkat
- Obstetrics/Gynecology: Emergency Medical Technician - BasicDokumen77 halamanObstetrics/Gynecology: Emergency Medical Technician - BasicAnonymous pJfAvlBelum ada peringkat
- Cholecystitis Drainage PDFDokumen6 halamanCholecystitis Drainage PDFAnonymous pJfAvlBelum ada peringkat
- Method Biliary DrainageDokumen10 halamanMethod Biliary DrainageAnonymous pJfAvlBelum ada peringkat
- Diagnostic Criteria and Severity Assessment of AcuteDokumen7 halamanDiagnostic Criteria and Severity Assessment of AcutedefinationBelum ada peringkat
- Vitamin CDokumen3 halamanVitamin CAnonymous pJfAvlBelum ada peringkat
- Saving MothersDokumen73 halamanSaving MothersAnonymous pJfAvlBelum ada peringkat
- Antimicrobial CholangitisDokumen9 halamanAntimicrobial CholangitisAnonymous pJfAvlBelum ada peringkat
- Tokyo Guidelines Establish Diagnostic Criteria for Acute Cholangitis and CholecystitisDokumen4 halamanTokyo Guidelines Establish Diagnostic Criteria for Acute Cholangitis and CholecystitisEduardo Martinez AvilaBelum ada peringkat
- Tokyo Guidelines For The Management of Acute Cholangitis and CholecystitisDokumen10 halamanTokyo Guidelines For The Management of Acute Cholangitis and CholecystitisYohan YudhantoBelum ada peringkat
- Biological Indicators in Response To Radiofrequency/Microwave ExposureDokumen10 halamanBiological Indicators in Response To Radiofrequency/Microwave ExposureAnonymous pJfAvlBelum ada peringkat
- Free Radicals and Antioxidants in Human Health PDFDokumen11 halamanFree Radicals and Antioxidants in Human Health PDFRonald DarwinBelum ada peringkat
- Diagnosis Assessment CholecystitisDokumen5 halamanDiagnosis Assessment CholecystitisAnonymous pJfAvlBelum ada peringkat
- Oxygen-Free Radicals Impair Fracture Healing in Rats: A Were ofDokumen3 halamanOxygen-Free Radicals Impair Fracture Healing in Rats: A Were ofAnonymous pJfAvlBelum ada peringkat
- Fracture Healing in The Elderly PatientDokumen14 halamanFracture Healing in The Elderly PatientAnonymous pJfAvlBelum ada peringkat
- Biological Indicators in Response To Radiofrequency/Microwave ExposureDokumen10 halamanBiological Indicators in Response To Radiofrequency/Microwave ExposureAnonymous pJfAvlBelum ada peringkat
- 12 Prasad NagiDokumen6 halaman12 Prasad NagiAnonymous pJfAvlBelum ada peringkat
- Septic Induced AbortionsDokumen4 halamanSeptic Induced AbortionsAnonymous pJfAvlBelum ada peringkat
- Left Ovarian Brenner Tumor: Key-Word: Ovary, NeoplasmsDokumen2 halamanLeft Ovarian Brenner Tumor: Key-Word: Ovary, NeoplasmsAnonymous pJfAvlBelum ada peringkat
- Surgical TechniqueDokumen6 halamanSurgical TechniqueDavid PalomequeBelum ada peringkat
- Nursing Care of Post Anesthesia Patients OutlinedDokumen13 halamanNursing Care of Post Anesthesia Patients OutlinedRhea JessicaBelum ada peringkat
- Newborn Screening: A Blood Test to Check for DisordersDokumen2 halamanNewborn Screening: A Blood Test to Check for DisordersKateLayaogBelum ada peringkat
- Neonatología PolinDokumen601 halamanNeonatología Polinnohemi baezBelum ada peringkat
- Oxford Handbooks Online: Mesopotamian Beginnings For Greek Science?Dokumen14 halamanOxford Handbooks Online: Mesopotamian Beginnings For Greek Science?Ahmed HammadBelum ada peringkat
- RPTDokumen6 halamanRPTparagkulkarni11Belum ada peringkat
- Aswathy P K - Resume NewDokumen3 halamanAswathy P K - Resume NewsherrymattBelum ada peringkat
- Enhanced Recovery ProtocolsDokumen17 halamanEnhanced Recovery ProtocolsHening Tirta KusumawardaniBelum ada peringkat
- SAT SHCO 3RD Edition 20 9 2022Dokumen150 halamanSAT SHCO 3RD Edition 20 9 2022Sumit SardanaBelum ada peringkat
- A New Look at The Safety of Breastfeeding During Pregnancy - KellyMomDokumen11 halamanA New Look at The Safety of Breastfeeding During Pregnancy - KellyMomdoggydogBelum ada peringkat
- Review Article: Impetigo Herpetiformis: Review of Pathogenesis, Complication, and TreatmentDokumen4 halamanReview Article: Impetigo Herpetiformis: Review of Pathogenesis, Complication, and TreatmentRatu TriaBelum ada peringkat
- Establishment of Trauma Center: Dr. Sanjay ShahDokumen34 halamanEstablishment of Trauma Center: Dr. Sanjay ShahDr. Rakshit SolankiBelum ada peringkat
- KC DataDokumen7 halamanKC DataDeepa YadavBelum ada peringkat
- Hospital ResearchDokumen62 halamanHospital ResearchPol vincent olmedillaBelum ada peringkat
- MNEMONICS OBGYN DIFFERENTIALSDokumen3 halamanMNEMONICS OBGYN DIFFERENTIALSak3dave888Belum ada peringkat
- A Study On The Effectiveness of Promotional Strategies With Reference To Hope Hospital".Dokumen85 halamanA Study On The Effectiveness of Promotional Strategies With Reference To Hope Hospital".Satya SriBelum ada peringkat
- Clinical Practice Guideline for Diagnosing and Treating Sudden Hearing LossDokumen45 halamanClinical Practice Guideline for Diagnosing and Treating Sudden Hearing Lossvania fatmaBelum ada peringkat
- LIST OF EMPANELLED HOSPITALSDokumen38 halamanLIST OF EMPANELLED HOSPITALSChandan ChatterjeeBelum ada peringkat
- PostnatalDokumen99 halamanPostnatalPlain GerlBelum ada peringkat
- Soal SisipanDokumen4 halamanSoal SisipanpanysiagianBelum ada peringkat
- ReportsDokumen2 halamanReportssawtulhassanBelum ada peringkat
- CapstoneessayDokumen5 halamanCapstoneessayapi-318193881Belum ada peringkat
- VIS Report FialDokumen16 halamanVIS Report FialAyaz MahmoodBelum ada peringkat
- MAPEH 10 - First Periodical TestDokumen3 halamanMAPEH 10 - First Periodical TestTeacherbhing MitrcBelum ada peringkat