Anatomy
Diunggah oleh
Tiiffanyy Faiith PadillaHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Anatomy
Diunggah oleh
Tiiffanyy Faiith PadillaHak Cipta:
Format Tersedia
REVIEW OF ANATOMY & PHYSIOLOGY OF THE
RENAL SYSTEM
It consists of the two kidneys, two ureters, the
urinary bladder, and the urethra.
PURPOSE: Formation of urine (is the main
function of the kidney) to eliminate the potentially toxic
waste products from the blood.
OTHER FUNCTIONS:
Regulates the blood volume, composition, and
pressure by the excretion or conservation of water.
Regulates the electrolyte balance of the blood
by the excretion or conservation of minerals.
Regulates acid-base balance of the blood by
the excretion or conservation of ions such as hydrogen
or bicarbonate.
Regulation all of the tissue fluids.
Production of erythropoietin, which
stimulates erythrocyte (red blood cells) production in
the bone marrow.
KIDNEYS
Are cushioned by surrounding adipose tissue,
which is in turn covered by a fibrous connective
membrane called the renal fascia.
HILUS is on the medial side, which is an
indentation where the renal artery enters and the renal
vein and ureter emerge.
Renal artery is a branch of the abdominal
aorta.
Renal vein returns blood to the inferior vena
cava.
Ureter carries urine from the kidney to the
urinary bladder.
In frontal section, there are three distinct areas of
the kidney the renal cortex, the renal medulla, and the
renal pelvis.
RENAL CORTEX is the outermost area that
contains the parts of the nephrons called renal corpuscles
and convoluted tubules.
RENAL MEDULLA is the middle area which
contains LOOPS OF HENLE and collecting tubules. It
also consists of wedge-shaped pieces called renal pyramids
with the apex or papilla pointing medially.
RENAL PELVIS is the innermost area, which is a
cavity. CALYCES are funnel-shaped extensions of the
renal pelvis that enclose the papillae of the renal pyramids.
NEPHRON is the structural and functional unit of
the kidney, with approximately one million nephrons in
each kidney.
The two major parts of a nephron are the renal
corpuscle and the renal tubule.
RENAL CORPUSCLE consists of a
GLOMERULUS surrounded by a BOWMANS
CAPSULE.
Glomerulus is a capillary network that arises from
the afferent arteriole and empties into the efferent
arteriole (with a smaller diameter to maintain high blood
pressure).
The Bowmans capsule is the expanded end of a
renal tubule, and it encloses the glomerulus. The inner
layer has pores and is highly permeable, while the outer
layer has no pores and is not permeable. The space in
between contains the RENAL FILTRATE.
RENAL TUBULE consists of the proximal
convoluted tubule, the loop of Henle, and the distal
convoluted tubule.
The distal convoluted tubule empty into a
collecting tubule, which then unite to form a papillary duct
that empties the urine into a calyx of the renal pelvis.
All parts of the renal tubule are surrounded by
the peritubular capillaries, which arise from the efferent
arteriole and receive the materials reabsorbed by the renal
tubules.
BLOOD FLOW:
Abdominal aorta ---> Renal artery which branches extensively
into smaller arteries ---> Afferent arterioles ---> Glomerulus ---
> Efferent arterioles ---> Peritubular capillaries ---> Smaller
veins in the kidneys ---> Renal vein ---> Inferior vena cava
FORMATION OF URINE
The formation of urine involves three processes glomerular
filtration in the renal corpuscles, tubular reabsorption, and
tubular secretion.
GLOMERULAR FILTRATION
FILTRATION is the process by which blood
pressure forces plasma and dissolved materials out of
capillaries.
Is the process by which blood pressure forces
plasma, dissolved substances, and small proteins out of the
glomeruli and into the Bowmans capsules. The fluid is
then called RENAL FILTRATE.
The blood pressure in the glomeruli is relatively
high at around 55mmHg. While the pressure in the
Bowmans capsule is low, and its inner layer is permeable,
so that approximately 20-25% of the blood that enters
glomeruli becomes a renal filtrate.
The larger proteins and blood cells are too large to
be forced out of the glomeruli so they remain in the blood.
While waste products such as urea and ammonia are
dissolved in plasma, so they pass to the renal filtrate.
The glomerular filtration rate (GFR) is the
amount of renal filtrate formed by the kidneys in one
minute, with an average of 100-125 mL/min.
The GFR changes if the rate of the blood flow
through the kidney changes.
If blood flow increases, the GFR increases, more
filtrate is formed, and urinary output increases.
If blood flow decreases, less filtrate is formed, and
urinary output decreases.
TUBULAR REABSORPTION
Is the recovery of the useful materials from the
renal filtrate and their return to the blood in the
peritubular capillaries. Approximately 99% of the renal
filtrate formed is reabsorbed.
The MECHANISMS OF REABSORPTION are
active transport, osmosis, diffusion, facilitated diffusion,
and pinocytosis.
ACTIVE TRANSPORT requires energy in the
form of ATP (adenosine triphosphate) for the cells of the
renal tubule to transport useful materials such as glucose,
amino acids, vitamins, and positive ions back to the blood.
OSMOSIS is the movement of solvent
molecules through a SELECTIVELY PERMEABLE
MEMBRANE into a region of higher solute
concentration. The reabsorption of water by
osmosis follows the reabsorption of minerals,
especially sodium. The conservation of water is very
important to maintain normal blood volume and
blood pressure.*
DIFFUSION describes the spread of particles
through random motion from regions of higher
concentration to regions of lower concentration.
FACILITATED DIFFUSION is the spontaneous
passage of molecules or ions across a biological membrane
passing through specific transmembrane integral proteins.
PINOCYTOSIS is the process by which small
proteins become attached to the membrane of the tubule
cells are engulfed and digested. Normally, all proteins in
the filtrate are reabsorbed and none are found in urine.
TUBULAR SECRETION
Is the process in which substances are actively
secreted from the blood in the peritubular capillaries into
the filtrate in the renal tubules.
Waste products such as ammonia and creatinine,
excess water-soluble vitamins, and the metabolic products
of medications may be secreted into the filtrate to be
eliminated in urine.
EFFECTS OF HORMONES IN THE KIDNEYS
ALDOSTERONE (Adrenal Cortex)
Promotes reabsorption of sodium ions from the
filtrate to the blood and excretion of potassium ions into
the filtrate. Water is reabsorbed following the
reabsorption of sodium.
ANTIDIURETIC HORMONE (Posterior Pituitary Gland)
Promotes reabsorption of water from the filtrate
to the blood.
ATRIAL NATRIURETIC HORMONE (Atria Of The Heart)
Decreases reabsorption of sodium ions, which
remain in the filtrate. More sodium and water are
eliminated in the urine.
PARATHYROID HORMONE (Parathyroid Glands)
Promotes reabsorption of calcium ions from the
filtrate to the blood and excretion of phosphate ions into
the filtrate.
OTHER FUNCTIONS OF THE KIDNEYS
ACID-BASE BALANCE. The kidneys are the
organs most responsible for maintaining the normal pH
range of blood and tissue fluid. They have the greatest
ability to compensate for or correct the pH changes that
are part of normal body metabolism or the result of
disease.
SECRETION OF RENIN. When blood pressure
decreases, the juxtaglomerular cells in the walls of the
afferent arterioles secrete the enzyme renin. RENIN then
initiates the renin-angiotensin-aldosterone mechanism --->
Formation of Angiotensin II ---> Vasoconstriction &
Increase secretion of aldosterone
---> Increase BP.
VITAMIN D CONVERSION. Vitamin D is
converted into its most active form, CALCITRIOL. It is
efficient in the absorption of calcium and phosphate from
food in the small intestine.
SECRECTION OF ERYTHROPOIETIN. It
stimulates the red bone marrow to increase the rate of
RBC production. Thus, increasing the oxygen-carrying
capacity of the blood.
URETERS
The smooth muscle in the wall of the ureter
contracts in peristaltic waves to propel urine toward the
urinary bladder. It is compresses when the bladder is fills
and expands.
URINARY BLADDER
It functions for temporary storage of urine.
In women, the bladder is inferior to the uterus.
While in men, it is superior to the prostate gland.
URETHRA
It carries urine from the bladder to the exterior.
Within its wall, near the bladder, is an
involuntary, internal urethral sphincter. The external
urethral sphincter on the other hand, is under voluntary
control and is made of skeletal muscles.
In women it is 1.0-1.5 inches long, while in men it
is 7-8 inches long.
---------------------
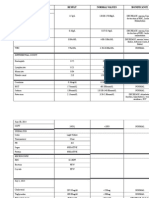
URINALYSIS
Used to establish baseline information, confirm or
establish a diagnosis, or determine if further testing needs
to be done.
URINE CULTURE
Is done to determine the number of bacteria
present in the urine and to identify the organism causing
the infection in the urine.
NOTE: The urine should be collected before
antibiotic treatment is begun to avoid affecting results. The
midstream clean-catch system is used to obtain voided
specimens.
A bacterial count of 100,000 or more per milliliter
of urine indicates urinary tract infection.
The urine is cultured to grow and identify the
kind of bacteria present. Often a sensitivity test is also
ordered to determine what kind of antibiotic will be most
effective in eradicating the offending bacteria.
RESIDUAL URINE
This study looks at the amount of urine left in the
bladder after voiding.
REFERENCE VALUE: < 50 mL
The patient is catheterized immediately after
voiding. If a large amount of urine is present, a urinary
catheter may be left in place.
Increased residual volume may be noted with
urethral strictures and sphincter impairment.
QUANTITATIVE TEST FOR PROTEIN
It requires a 12 or 24-hour collection.
Persistent proteinuria is usually seen with
glomerular renal disease.
REFERENCE VALUE: <150 mg/24 hours
CREATININE CLEARANCE
It measures the amount of creatinine cleared from
the blood in a specified period by comparing the amount of
creatinine in the blood with the amount of
creatinine in the urine.
REFERENCE VALUE: 85-135 mL/min
A minimum creatinine clearance of 10 mL per
minute is needed to live without dialysis.
It is an excellent indicator of renal function.
URINE CYTOLOGY
It is a microscopic examination of urine to detect
atypical epithelial cells shed from the surface of the
urinary tract.
It is used as screening for people with high risk for
the development of cancer within the urinary system.
URINE BLADDER CANCER MARKERS (
BLADDER TUMOR ANTIGEN ) BTA
It is a protein that is produced by the bladder
tumor cells.
REFERENCE VALUE: BTA < 14 units/mL
KIDNEY FUNCTION TESTS (SERUM
CREATININE)(4)
Creatinine is a waste product from muscle
metabolism and is released into the blood stream at a
steady rate.
REFERENCE VALUE: 0.6-1.5 mg/dL
A serum creatinine level above 1.5 mg/dL means
there is kidney dysfunction. The higher the creatinine
level, the more impaired the kidney function.
CYSTATIN C
It is a proteinase inhibitor.
It is a small molecule that is produced by all cells
with chromosomes and genetic material at their center,
and is produced at a constant rate and filtered
out of the blood by the glomerulus and
reabsorbed by the tubular epithelial cells.
It is a sensitive marker that reflects the
glomerular filtration rate independent of body weight and
height.
REFERENCE VALUE: 0.53-0.95 mg/dL
BLOOD UREA NITROGEN
Urea is a waste product of protein metabolism.
It is not as sensitive an indicator of kidney
function as the creatinine level. This is because it is readily
affected by increased protein intake, dehydration,
and other factors.
REFERENCE VALUE: 8-20 mg/dL
URIC ACID
It is an end product of purine metabolism and the
breakdown of body proteins. It is not as diagnostic as
creatinine because many factors can cause an
elevated uric acid level.-7
REFERENCE VALUE: 2-7 mg/dL
BUN TO CREATININE RATIO
It evaluates hydration status.
REFERENCE VALUE: About 10:1
An elevated ratio is seen with hypovolemia. A
normal ratio with an elevated BUN and creatinine is seen
with intrinsic renal disease.
BLOOD CHEMISTRIES or ELECTROLYTES
SODIUM
It is an extracellular electrolyte regulating blood
volume.
REFERENCE VALUE: 135-145 mEq/L-8
Some values usually remain within normal ranges
until late stages of renal failure.
POTASSIUM
Kidneys are responsible for excreting potassium.
In renal diseases, it is one of the first electrolyte to become
abnormal.
REFERENCE VALUE: 3.5-5.0 mEq/L-10
> 6 mEq/L can lead to muscle weakness and
cardiac arrhythmias.
CALCIUM
It is the main mineral in bone and aids in muscle
contraction, neurotransmission, and blood clotting.
REFERENCE VALUE: 4.5-5.5 mEq/L
PHOSPHORUS
Phosphorus balance is inversely related to calcium
balance.
In renal disease, phosphorus levels are elevated.
REFERENCE VALUE: 2.8-4.5 mg/dL
MAGNESIUM
Is found in the bone and intracellularly. It is
excreted by the kidney.
REFERENCE VALUE: 1.3-2.1 mEq/L
Chronic renal disease causes magnesium
elevations.
Symptoms of elevated magnesium levels include
lethargy, nausea and vomiting, and slurred speech.
BICARBONATE
Most patients in renal failure have metabolic
acidosis and low serum bicarbonate levels.
REFERENCE VALUE: 22-28 mEq/L
SERUM ALBUMIN
Low levels may be seen in nephrotic syndrome.
REFERENCE VALUE: 3.5-5.0 g/dL
---------------------
RENAL ULTRASOUND OR ULTRASONOGRAPHY
Uses high-frequency sound waves to visualize the
kidneys, ureters, and bladder.
It helps diagnose congenital disorders of the
kidney, renal abscesses, kidney stones, and tumors.
Identifies enlargement of the kidneys, and changes
of renal structures.
NO SPECIAL PREPARATIONS OR
AFTERCARE, and also NO KNOWN
COMPLICATIONS.
BLADDER ULTRASOUND
Scans the bladder for residual urine volume,
bladder wall thickness, bladder calculi, tumors, and
diverticula.
KIDNEY-URETER-BLADDER X-RAY STUDY
Is also known as a FLAT PLATE OF THE
ABDOMEN14
Is a radiological procedure that examines the size,
shape, and position of the kidneys, ureters, and bladder.
It helps discover renal calculi, kidney size, or
masses in the kidney.
COMPUTED TOMOGRAPHY ( CT SCAN )
It is radiological procedure where in the computer
constructs images of the area scanned from a series of
tomograms or cross-sectional slices and displays them on a
screen.
The CT scan of the abdomen and pelvis may be
done to discover tumors, metastatic cancers, renal cysts, or
abscesses. The scan may also be used for tumor staging or
identifying masses.
NURSING CONSIDERATIONS:
NPO for 4 hours before the procedure.
Instruct to avoid movements during the
procedure.
If contrasts are given prior to the procedure,
check for allergies to the dye or iodine.
MAGNETIC RESONANCE IMAGING ( MRI )
It is a radiological procedure where computer-
generated films are produced by the interaction of radio
waves and magnetic fields. It is used to visualize the
kidneys, bladder, prostate, testes, and retroperitoneum.
NURSING CONSIDERATIONS:
MRI is contraindicated in any patient with
metallic objects in the body, surgical clips, or pacemakers.
Patient preparation includes removal of any metal
objects, jewelry, or clothing with metal clips.
Assess for any history of claustrophobia, and
sedate when necessary.
Check also for allergies since contrast media
might also be administered.
INTRAVENOUS PYELOGRAM ( IVP )
It is a common radiological procedure in which x-
ray examination visualizes the renal tissue, calyces,
pelvises, ureters, and the bladder after the intravenous
injection of contrast media or dye. It provides a rough
estimate of renal function.
During the test a radiopaque dye is injected into a
large vein. Then dye is cleared from the blood by the
kidneys.
Because the x-rays cannot penetrate the dye, the
dye outlines the renal structures. Radiographs are taken at
frequent intervals to see the dye filling the renal pelvis and
going down the ureters into the bladder.
The dye outlines the renal system and identifies
abnormal size or shape of kidneys, polycystic kidney
disease, tumors, and renovascular hypertension.
BEFORE PROCEDURE:
Assess patient for allergies to iodine or
contrast media prior to the test. The patient should be
warned about a warm, flushing sensation up the arm
and sometimes all over the body when the dye is
injected. A strange taste may occur as well.
NPO for 8 hours prior to the test.
Enemas will possibly be given the evening
before the test to empty the colon.
On rare occasions, it can cause acute renal
failure because the dye is highly concentrated and it
can obstruct renal tubules. IVP is not recommended
for patients with renal insufficiency or failure.
AFTER PROCEDURE:
Instruct to drink large amount of water.
Monitor urine output.
RENAL ANGIOGRAPHY or ARTERIOGRAM
It is a radiological procedure purposed to visualize
renal blood vessels.
The femoral artery is pierced with a needle, and a
catheter is threaded up through the femoral and iliac
arteries into the aorta and the renal artery.
A contrast agent is injected to make the renal
arterial supply visible on x-ray examination.
The test helps the physician see blood flow to the
kidneys to determine the cause and treatment of kidney
disease.
It is useful if renal insufficiency is caused by renal
vascular disease.
The test reveals hypervascular tumors, renal
cysts, renal artery stenosis, renal artery aneurysms,
pyelonephritis, obstructions, renal infarction, and
evaluates renal trauma.
BEFORE THE PROCEDURE:
Check for allergies to iodine or contrast
media.
NPO for 4 to 8 hours prior to the test.
An enema or cathartic may be given the
evening prior to the test.
AFTER THE PROCEDURE:
Put patient on bed rest for up to 12 hours.
Check distal pulses in leg every 30-60 minutes.
Instruct not to bend the leg, and the head of
the bed is not raised more than 45 degrees.
Monitor vital signs, dressing, and pulses in the
affected extremity frequently.
POSSIBLE COMPLICATIONS: Blood vessel
injury, embolus or clot formation, and allergic reaction.
NEPHROTOMOGRAM
It is a radiological procedure in which a series of
x-rays are taken from different angles to create a three-
dimensional image of the kidney, and uses intravenous
contrast media.
It is useful in the identification of renal cysts,
tumors, areas of non-perfusion, and renal fractures or
lacerations following renal trauma.
PREPARE PATIENT AS IN IVP.
RENAL SCAN
It is a nuclear scan that works on the principle
that when radioactive substances called radioisotopes are
injected into the blood stream, it can be detected by a
special camera called a gamma camera similar to an x-ray
machine.
It measures kidney function, renal blood flow,
glomerular filtration rate, tubular function, and excretion
of urine, as well as, outlines the kidneys size and shape.
It is mainly used for the diagnosis of renovascular
hypertension.
ADVANTAGE: The ability to determine kidney
function without exposure to contrast agents and the
ability to obtain quantitative information that may not be
obtainable by other procedures. The level of radiation is
low.
NO SPECIAL PREPARATION is usually
necessary. Drink two glasses of water prior to the test.
RENAL BIOPSY
Involves obtaining a renal tissue for laboratory
analysis. It is indicated when microscopic examination of
kidney tissue is needed to diagnose or treat a renal
disorder.
It is used to diagnose benign and malignant
masses, causes of renal failure, renal transplant tissue, or
lupus.
PERCUTANEOUS RENAL BIOPSY is done with
a needle through the skin. While OPEN RENAL BIOPSY
is done through a surgical incision.11-12
BEFORE THE PROCEDURE:
A CT Scan or Ultrasound is done first to
locate the kidney for biopsy.(1)
The patient is NPO for 6 to 8 hours.
A mild sedative is administered.
The patient should not take anticoagulants
before the biopsy because of the risk of bleeding.
A complete blood cell count and coagulation
studies are performed prior to the biopsy.(2)
For a percutaneous biopsy, a local anesthetic
is used.
DURING THE PROCEDURE:
The patient is placed in a prone position,
usually with a sandbag under the abdomen, and the
biopsy is taken through the flank area.
Instruct the patient to take a deep breath in
and hold it while the needle is being inserted.
AFTER THE PROCEDURE
Following the biopsy, the patient may be kept
in prone position.
Observe closely for bleeding, because the
kidney is highly vascular.
A bandage is applied, and the patient is
maintained on bed rest for 24 hours or more.
Urine is inspected for blood with each voiding
and compared to the previous voiding for 24 hours.
Grossly bloody urine, falling blood pressure,
and rising pulse are signs of bleeding, and are
reported immediately.
No heavy lifting for 2 weeks when the patient
goes home.
POSSIBLE COMPLICATIONS: Gross
hematuria, Pain, Infection, Hypotension, Pneumothorax &
Hemorrhage.13
CYSTOSCOPY & PYELOGRAM (C & P)
CYSTOSCOPY is a minor surgical procedure
that involves a rigid or fiberoptic instrument (cystoscope)
inserted into the bladder through the urethra. While
PYELOGRAM involves the insertion of a urethral
catheter into the pelvis of the kidney. Radiopaque dye is
injected through the catheter and radiographs are taken.
A light end of the instrument allows a physician to
visualize the interior of the bladder.
CYSTOGRAM
It is an x-ray of the bladder and lower urinary
tract.
A contrast media or a radioisotope is instilled into
the bladder via a catheter or cystoscope.
The test is done to evaluate the filling and
emptying of the bladder, and the purpose is to visualize the
bladder and evaluate vesicoureteral reflux.
It determines incomplete bladder emptying,
distention, or reflux, as well as, obstruction to urine flow.
NO MEDICATION, FASTING, OR SPECIAL
DIETS ARE NECESSARY. The patient is prepared
accordingly for either catheter or cystoscope insertion.
After the scan, there may be slight dysuria and
pink urine for 1-2 days. Bright red urine, fever, or
persistent discomfort should be reported to the physician.
---------------------
SKIN
The nurse inspects the skin for color, texture,
edema, or swelling. A patient with chronic renal failure
may have a yellow or gray cast skin.
The presence of crystals on the skin is called
uremic frost (4) and is a late sign of waste products
building up in the blood (uremia). (5)
When the wastes are not filtered by the kidneys,
they can come out through the skin look like a coating of
frost.
VITAL SIGNS
If renal disease is suspected, blood pressure
should be assessed and documented while the patient is
lying, sitting, and standing.
An increase in blood pressure is commonly seen
with renal disease.
ORTHOSTATIC HYPOTENSION or
POSTURAL HYPOTENSION, a drop in blood pressure
accompanied by a rise in pulse rate as the patient rises to
sitting or standing position. This is could indicate fluid
deficit.
A rapid respiratory rate indicates fluid retention
in the lungs.
LUNG SOUNDS
If the patient retains more fluid than the heart can
effectively pump, fluid may be retained in the lungs.
This is manifested as CRACKLES, which are
popping sounds heard on inspiration and sometimes on
expiration when the chest is auscultated. WHEEZES may
also be present.
EDEMA
Fluid retention may be manifested as edema
(excess fluid in tissues).
The nurse assesses and documents the degree and
location of edema. Edema may be generalized in renal
failure. The nurse also looks edema in the area around the
eyes (periorbital edema).
DAILY WEIGHTS
Weight is the single best indicator of fluid balance
in the body. Patients with renal disease often have fluid
imbalances.
The patient should be weighed at the same time
each day, in the same or similar clothing, and with the
same scale.
The nurse is careful not just to document the
weight, but also to look at trends in weight gain or loss. If
the patients weight is STEADILY INCREASING, fluid
retention is suspected and should be reported. A patient
undergoing diuresis is expected to have decreasing
weights.
INTAKE AND OUTPUT
All patients with renal disease should have careful
measurement of intake and output with each voiding. As
with daily weights, the nurse notes trends in retention or
loss of fluid and reports significant changes to the
physician.
-----------------
URINARY INCONTINENCE
Is used to refer to the involuntary leakage of
urine.
Is often underdiagnosed because many patients
are too embarrassed to talk about the problem. Most
patients do not seek treatment until the problem
profoundly affects quality of life.
STRESS INCONTINENCE (1)
Is the involuntary loss of less than 50 mL of
urine associated with increasing abdominal pressure
during coughing, sneezing, laughing, or other physical
activities.
Is commonly seen in women following
childbirth and after menopause. In men, stress
incontinence is associated with prostatectomy and
radiation.
URGE INCONTINENCE
Is the involuntary loss of urine associated with
an abrupt and strong desire to void. The patient
typically complains of being unable to make it to the
bathroom in time.
It is the most common type of urinary
incontinence in older adults.(2)
Patients with STRESS OR URGE
INCONTINENCE can be taught KEGELS
EXERCISES to increase perineal muscle tone.
FUNCTIONAL INCONTINENCE
It is the inability to reach the toilet because of
environmental barriers, physical limitations, loss of
memory, or disorientation.
People with functional incontinence are often
dependent on other and have no other urinary
problems.
OVERFLOW INCONTINENCE
Is the involuntary loss of urine associated with
overdistention of the bladder. It occurs with acute or
chronic urinary distention with dribbling of urine.
The bladder is unable to empty normally despite
frequent urine loss.
Spinal cord injuries or an enlarged prostate may
cause this type of incontinence.
TOTAL INCONTINENCE
Is a continuous and unpredictable loss or
urine. It usually results from surgery, trauma, or a
malformation of the ureter.
A bladder training has been tried and proven
ineffective. Often the patient with total incontinence is
neurologically impaired. (3)
URINARY RETENTION
Is the inability to empty the bladder completely
during attempts to void.
There are TWO TYPES OF URINARY
RETENTION
ACUTE URINARY RETENTION
There is sudden onset of retention and no
urine output.
CAUSE: Use of anesthesia, medications, or
local trauma to the urinary structures.
COMPLICATIONS: Extreme pain, bladder
distention, and the possibility of bladder rupture or
acute renal failure.
2. CHRONIC URINARY RETENTION
There is a slower onset of retention of urine
and only some urine is being expelled.
CAUSE: Enlarged prostate gland, diabetes,
pregnancy, a medication effect, strictures, or other
causes of obstruction of the urinary tract.
HOW TO ASSESS FOR URINARY RETENTION?
Determine the urine output
BLADDER SCAN assess the volume of urine
in the bladder. It helps guide the need for
catheterization, thereby reducing unnecessary
catheterizations, and associated risks.
A residual volume of 150-200 mL of urine
indicates the need for treatment of urinary retention.
Palpate the lower abdomen
(6) bladder scan/fbc
URINARY CATHETERS
INDWELLING URINARY CATHETER ( Foley
Catheters )
This is inserted into hospitalized patients for
various justifiable reasons, such as shock, heart failure, or
urinary tract obstruction.
Catheters should be avoided if possible because of
the high risk of urinary tract infections. URINARY
INCONTINENCE is not justification for insertion of a
catheter.
URINARY CATHETERS result in infection of the
urinary tract up to 44% of patients within 72 hours, and
up to 90% of patients who have indwelling catheters for 17
days develop significant bacterial infection.
Bacteria enters the bladder mainly in one of two
ways with an indwelling catheter:
(1) through the outlet at the end of the drainage bag
contaminating the urine, and
(2) around the catheter up the urethra and into the bladder.
It has been demonstrated that the incidence of
infection is decreased when intermittent straight
catheterization is used instead of indwelling urinary
catheters.
INTERMITTENT CATHETERIZATION
For patients who are unable to void, the best
intervention is intermittent catheterization.
It reduces the risk of infection as long as the
bladder is not allowed to overfill. A full bladder stretches
the muscle fibers, which in turn reduces circulation the
bladder and increases the risk of infection.
SUPRAPUBIC CATHETER (7)
Is an indwelling catheter that is inserted through
an incision in the lower abdomen directly into the bladder.
URINARY TRACT INFECTION
It refers to invasion of the urinary tract by
bacteria.
In hospital settings, it is the second most common
nosocomial infection.
There are TWO TYPES OF URINARY TRACT
INFECTION:
LOWER URINARY TRACT INFECTION
- Includes URETHRITIS, PROSTATITIS, and
CYSTITIS.
2. UPPER URINARY TRACT INFECTION
- Includes PYELONEPHRITIS and URETERITIS.
Are almost always caused by an ascending
infection, starting at the external urinary meatus and
progressing toward the bladder and kidneys.
The majority of UTIs are caused by the bacterium
Escherichia coli, which is commonly found in stool.
RISK FACTORS:
STASIS OF THE URINE IN THE BLADDER.
It can be caused from obstruction such as
a clamped catheter or simply from not voiding
frequently enough
Urine overdistends the bladder.
---> Decrease of blood supply to the wall of the
bladder keeps WBCs from fighting contamination
that may have entered the bladder.
---> The standing urine then serves as a culture
medium for bacterial growth.
---> Incomplete emptying of the bladder prevents
flushing out of the bacteria and allows bacteria to
ascend to higher structures.
CONTAMINATION in the perineal and
urethral areas can be from fecal soiling, from sexual
intercourse in which bacteria are massaged into the
urinary meatus, or from the infection in the area.
INSTRUMENTATION or having instruments
or tubes inserted into the urinary meatus. The most
common cause is URINARY CATHETERIZATION.
Within 48 hours of catheter insertion, bacterial
colonization begins.
REFLUX OF URINE
PREVIOUS UTIs are thought to provide
reservoir of persistent bacteria that cause reinfection.
WOMEN are more susceptible than men due
to the short length of the female urethra and close
proximation to anus and vagina.
OLDER ADULTS due to diminished immune
response, diabetes, and neurogenic bladder. In older
men, it is due to enlargement of prostate. While in
older women, the decline in estrogen can contribute to
the risk of UTI.
SIGNS & SYMPTOMS: Urinary urgency,
frequency, dysuria, incontinence, nocturia, hematuria,
flank pain, cloudy urine with casts, foul-smelling urine,
fever, chills, costovertebral tenderness. Urine is positive
for nitrites.
DIAGNOSTIC TESTS: Urinalysis, culture is
greater than 100,000 bacteria, elevated WBCs, elevated
sedimentation rate, increased neutrophils.
COMPLICATIONS: Pyelonephritis, Urosepsis,
Renal failure.
TYPES OF UTI:
URETHRITIS is the inflammation of the
urethra that may be due to a chemical irritant,
bacterial infection, trauma, or exposure to a sexually
transmitted disease.
PROSTATITIS is the inflammation or
infection of the prostate gland.
CYSTITIS is inflammation and infection of
the bladder wall. It can be caused by bacteria, viruses,
fungi, or parasites.(9)
PYELONEPHRITIS is infection of the renal
pelvis, tubules, and interstitial tissue of one or both
kidneys. (11)
RISK FACTORS: Urological surgery,
lymphatic infection, urinary stasis, decreased
immunity.
Begins with colonization and infection of
the lower urinary tract by means of the infection
of the ascending urethral route Begins in the
renal medulla and spreads to the adjacent cortex
URETERITIS is the inflammation or
infection of the ureters. (10)
(9)
THERAPEUTIC INTERVENTIONS: Antibiotic
therapy sensitive to organism cultured from urine.
MEDICATIONS FOR URINARY TRACT INFECTION:
Cinoxacin (Cinobac) Urinary antiseptic
Methenamine (Mandelamine) Urinary antiseptic,
Anti-infective
Trimethoprim-Sulfamethoxazole (Bactrim, Septra)
Sulfonamides
Sulfisoxazole (Gantrisin) Sulfonamide
Ciprofloxacin (Xipro) Fluoroquinolone
Astreonam (Azactam) Antibiotic
Phenazopyridine (Pyridium) Urinary analgesic
HEALTH TEACHING
Void frequently At least every 3-4 hours while
awake.
Drink up to 3,000 mL of fluid a day if there are no
fluid restrictions from the physician. Preferably drink
water.
Drink one glass of cranberry juice (10 0z) per day.
Take showers, avoid bath tubs.
Wipe perineum from the front to the back after
toileting.
Urinate after sexual intercourse.
Avoid bubble bath and bath salts, perfumed
feminine hygiene products, synthetic underwear, and
constricting clothing such as tight jeans.
Take prescribed medication for UTIs until it is all
gone.
If UTI is associated with another source of
infection such as vaginitis or prostatitis, ensure that both
infections are treated.
UROLOGICAL OBSTRUCTIONS
It refers to an interference with the flow of urine
at any location along the urinary system.
CAUSES: Urethral strictures, renal calculi,
tumors in the urinary system
PATHOPHYSIOLOGY:
UROLOGICAL OBSTRUCTIONS --- Urine does not
drain normally from the kidney ---
Local compression --- Decompensation of the area ---
Moving up of the pressure along the continuum of the
renal system ---
Reflux of urine --- Dilation and thinning of renal tubules -
-- Atrophy of renal tissues ---
Renal blood flow is compromised --- Destruction of renal
tissues
URETHRAL STRICTURES
Is the narrowing of the lumen of the urethra
caused by a scarred tissue.
CAUSES: STDs such as gonorrhea and
chlamydia, TRAUMA from insertion of catheters and
surgical instruments and straddle injuries, congenital
abnormalities.
More common in elderly men.
POSSIBLE COMPLICATION: Urinary Tract
Infection
MEDICAL TREATMENT:
Mechanical dilation of the urethra, URETHROPLASTY
(surgical repair of the urethra) (12)
RENAL CALCULI
It refers to the hard, generally small stones that
form somewhere in the renal structures.
The stones are masses of crystals and protein that
form when the urine becomes supersaturated with a salt
capable of forming solid crystals.
NOTE: The symptoms occur when the stones
become impacted in the urinary tract. Stones less than 5
mm are readily passed in the urine.
NEPHROLITHIASIS is the condition where
stones are found in the kidneys.(13)
CAUSES: Familial history, chronic dehydration,
infection, dietary factors, immobility
PATHOPHYSIOLOGY:
Urinary salts are concentrated enough to settle out --->
Formation of a nucleus which the salts collect and deposit ( e.g.
pus, dead tissue, crystals ) Stones usually grow in the papillae
or in the renal tubules, calyces, and renal pelvis,
as well as in the ureter or bladder.
COMMON URINARY SALTS: (14)
Calcium oxalate
Calcium phosphate
Magnesium ammonia
Uric acid
Cystine
Triamterene stones ( recently discovered stones -
Potassium-sparing diuretics)
MEDICATIONS AFFECTING STONE
FORMATION
Acetazolamide
Adrenocorticosteroids -
Allopurinol
Antacids
Aspirin
Chemotherapeutic agents
Hydrochlorothiazide
Furosemide
Vitamin C
Vitamin D
SIGNS & SYMPTOMS: Excruciating flank pain
and renal colic, hematuria, dysuria, frequency, urgency,
enuresis, costovertebral tenderness
OTHER SIGNS & SYMPTOMS: Nausea,
vomiting, diarrhea
DIAGNOSTIC TESTS: Urinalysis, Crystals and
urine pH, 24-hour renal creatinine clearance, BUN,
Creatinine, KUB ( reveals most calculi ), Retrograde
pyelography, Ultrasound
NURSING INTERVENTIONS:
Intravenous fluids are administered.
Monitor and strain urine output.
Administer pain medications as prescribed.
Dietary modification depending on the
composition of the renal stones.
PHARMACOLOGIC TREATMENT: Calcium
stones may be treated with Thiazide Diuretics and
Allopurinol.
MEDICAL TREATMENT:
CHEMOLYSIS
Involves stone dissolution using infusions
of chemicals to dissolve stone.
LITHOTRIPSY THERAPY (15)
Is the use of sound, laser, or dry shock-
wave energies to break the stone into small
fragments.
SURGICAL MANAGEMENT:
PERCUTANEOUS NEPHROLITHOTOMY
Is performed with a scope that is inserted
through the skin into the kidney to aid breaking
up the stone and to irrigate the renal pelvis.
A PERCUTANEOUS NEPHROSTOMY
TUBE is sometimes left in place at first to prevent
the stone fragments from passing through the
urinary system.
NEPHROLITHOTOMY
Is the surgical incision into the kidney to
remove the stone.
PYELOLITHOTOMY
It is the removal of stones lodged in the
renal pelvis.
COMPLICATIONS: Shock, Sepsis,
Hydronephrosis, Hydroureter, Renal Failure
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- SRS PostOp Care (Add Pic)Dokumen24 halamanSRS PostOp Care (Add Pic)m1au123100% (3)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- FITTP and Red Flags TabulationDokumen4 halamanFITTP and Red Flags Tabulationalyssa marie salcedo100% (2)
- Computed Tomography Radiation Safety Issues in OntarioDokumen71 halamanComputed Tomography Radiation Safety Issues in Ontariopebbles18950% (2)
- Brain Tumor New 1Dokumen6 halamanBrain Tumor New 1Tiiffanyy Faiith PadillaBelum ada peringkat
- Assessment Stab WoundsDokumen6 halamanAssessment Stab WoundsTiiffanyy Faiith PadillaBelum ada peringkat
- Laboratory Findings: Result Normal Values SignificanceDokumen3 halamanLaboratory Findings: Result Normal Values SignificanceTiiffanyy Faiith PadillaBelum ada peringkat
- Fluid and ElectrolyteDokumen11 halamanFluid and ElectrolyteTiiffanyy Faiith PadillaBelum ada peringkat
- RBC DisordersDokumen70 halamanRBC DisordersNdor Baribolo100% (1)
- Rawla 2018 Efficacy and Safety of Megestrol inDokumen6 halamanRawla 2018 Efficacy and Safety of Megestrol inAbdallah H. KamelBelum ada peringkat
- First Aid Principles and PracticeDokumen51 halamanFirst Aid Principles and PracticeGiselle KhrystineBelum ada peringkat
- Etiqa PDFDokumen39 halamanEtiqa PDFClifford LedesmaBelum ada peringkat
- FCE Use ESOL 3Dokumen2 halamanFCE Use ESOL 3Fran PasteriBelum ada peringkat
- Anti Allergy: NO Produk Komposisi Kemasan HNA Hna + PPN KETDokumen6 halamanAnti Allergy: NO Produk Komposisi Kemasan HNA Hna + PPN KETMuhammad Asri,S.Kep,NsBelum ada peringkat
- Factors Associated With Iron Deficiency Anemia Among Women of Childbearing Age in Yaqshid DistrictDokumen82 halamanFactors Associated With Iron Deficiency Anemia Among Women of Childbearing Age in Yaqshid DistrictMohamed Omar HassanBelum ada peringkat
- Equine Dental BrochureDokumen2 halamanEquine Dental BrochurevetthamilBelum ada peringkat
- Interaksi Obat Dengan Nutrisi EnteralDokumen5 halamanInteraksi Obat Dengan Nutrisi EnteralRijantono Franciscus MariaBelum ada peringkat
- Bühler Heim 2018 General Introduction To The Psychotherapy of Pierre JanetDokumen18 halamanBühler Heim 2018 General Introduction To The Psychotherapy of Pierre JanetsammyBelum ada peringkat
- Acute Flaccid ParalysisDokumen4 halamanAcute Flaccid ParalysisZharah RuzBelum ada peringkat
- Daftar PustakaDokumen4 halamanDaftar PustakaAnisa OktavianiBelum ada peringkat
- Hepatitis C in PregDokumen4 halamanHepatitis C in PregYwagar YwagarBelum ada peringkat
- Effectiveness of The Motor Relearning ApproachDokumen5 halamanEffectiveness of The Motor Relearning ApproachZahid MehmoodBelum ada peringkat
- Educ763 Chart AlignmentDokumen6 halamanEduc763 Chart Alignmentapi-297105278Belum ada peringkat
- Skin Graft and Flap: Ibnu F Hantoro Diponegoro University Faculty of MedicineDokumen11 halamanSkin Graft and Flap: Ibnu F Hantoro Diponegoro University Faculty of MedicineLuqman AlwiBelum ada peringkat
- Ecart MedsDokumen5 halamanEcart Medsしゃいな ふかみBelum ada peringkat
- ActinobacillosisDokumen17 halamanActinobacillosisKhalid Gul100% (1)
- Problem and Its ScopeDokumen49 halamanProblem and Its ScopeAnnaly DelcastilloBelum ada peringkat
- Basic Life Support in Infants and ChildrenDokumen9 halamanBasic Life Support in Infants and ChildrenMelissa Espinoza PeñaBelum ada peringkat
- PRO Post Natal AssessmentDokumen9 halamanPRO Post Natal AssessmentMali KanuBelum ada peringkat
- Industrial Pharmacy Practice Notes-1Dokumen4 halamanIndustrial Pharmacy Practice Notes-1Gerald Limo Arap ChebiiBelum ada peringkat
- The Effects of Estrogens and ProgesteroneDokumen7 halamanThe Effects of Estrogens and ProgesteroneTinke WinkeBelum ada peringkat
- Wisner Et Al - Antipsychotic Treatment During PregnancyDokumen8 halamanWisner Et Al - Antipsychotic Treatment During PregnancymirasaqqafBelum ada peringkat
- Jurnal Nausea and VomitingDokumen15 halamanJurnal Nausea and VomitingRisa KarmeylithaBelum ada peringkat
- Drug Study of Antidiabetic DrugsDokumen6 halamanDrug Study of Antidiabetic DrugsLorina Lynne ApelacioBelum ada peringkat
- UAS Kritis 1 (T4) - Monitoring Fungsi Pernapasan - Bu HY (A11)Dokumen108 halamanUAS Kritis 1 (T4) - Monitoring Fungsi Pernapasan - Bu HY (A11)rifqifuadiBelum ada peringkat