Health Insurance
Diunggah oleh
darthvader0050 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
272 tayangan64 halaman123
Hak Cipta
© © All Rights Reserved
Format Tersedia
DOCX, PDF, TXT atau baca online dari Scribd
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen Ini123
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai DOCX, PDF, TXT atau baca online dari Scribd
0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
272 tayangan64 halamanHealth Insurance
Diunggah oleh
darthvader005123
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai DOCX, PDF, TXT atau baca online dari Scribd
Anda di halaman 1dari 64
1
CHAPTER 1 INTRODUCTION TO INSURANCE
1.1 Meaning
Insurance is the equitable transfer of the risk of a loss, from one entity to
another in exchange for payment. It is a form of risk management primarily
used to hedge against the risk of a contingent, uncertain loss.
An insurer, or insurance carrier, is a company selling the insurance; the
insured, or policyholder, is the person or entity buying the insurance policy.
The amount to be charged for a certain amount of insurance coverage is
called the premium. Risk management, the practice of appraising and
controlling risk, has evolved as a discrete field of study and practice.
The transaction involves the insured assuming a guaranteed and known
relatively small loss in the form of payment to the insurer in exchange for
the insurer's promise to compensate (indemnify) the insured in the case of a
financial (personal) loss. The insured receives a contract, called the
insurance policy, which details the conditions and circumstances under
which the insured will be financially compensated.
2
How Insurance Works:
An insurer, or insurance carrier, is a company selling the insurance; the
insured, or policyholder, is the person or entity buying the insurance policy.
The amount to be charged for a certain amount of insurance coverage is
called the premium. The insurance company has to deal with the Risk
Management, the practice of appraising and controlling risk.
The transaction involves the insured assuming a guaranteed and known
relatively small loss in the form of payment to the insurer in exchange for
the insurer's promise to compensate (indemnify) the insured in the case of a
financial (personal) loss. The insured receives a contract, called the
insurance policy, which details the conditions and circumstances under
which the insured will be financially compensated.
3
1.2 History of insurance in India
The business of life insurance in India in its existing form started in India in
the year 1818 with the establishment of the Oriental Life Insurance
Company in Kolkatta.
Some of the important milestones in the Life Insurance Business in India
are:
1912: The Indian Assurance Companies Act enacted as the first statue
to regulate the Life Insurance business.
1928: The Indian Companies Act enacted to enable the government to
collect statistical information about Life Insurance.
1938: Earlier legislation consolidated and amended to by the
Insurance Act with the object of protecting the interest of the insuring
public.
1956: 245 Indian and Foreign Insurers and provident societies taken
over by the Central Government and Nationalized. LIC formed by an
Act of Parliament viz. LIC Act, 1956 with a capital contribution of
Rs.5 crore from the Government of India. The General Insurance
Business in India, on the other hand, can trace its roots to the Triton
Insurance Company Ltd., the first General Insurance Company
established in the year 1850 in Kolkatta by the British.
4
Some of the important milestones in the General Insurance Business in India
are:
1907: The Indian Mercantile Insurance Ltd., set up, the first company
to transact all classes of general insurance business.
1957: General Insurance Council, a wing of the Insurance Association
of India, frames a code of conduct for ensuring fair conduct and sound
business
practices.
1968: The Insurance Act amended to regulate investments and set
minimum solvency margins and the Tariff Advisory Committee set
up.
1972: The General Insurance Business (Nationalization) Act, 1972
nationalized the general insurance business in India with effect from
1st January 1973. 107 insurers amalgamated and grouped into four
companies viz. the National Insurance Company Ltd., the New India
Assurance Company Ltd., the Oriental Insurance Company Ltd., and
the United India Insurance Company Ltd. GIC incorporated as a
company. The funds generated by LIC and Public Sector General
Insurers are invested in the avenues that benefit the society. They
solely acted as public undertaking insurers and catered the life cover
and general risk cover of the public till the enactment of Insurance
Regulatory and Development Authority (IRDA) Act, 1999.
5
1.3 Development of Insurance as Industry:
The concept of insurance is almost as old as human society and over the
years, insurance industry matured into the form that we know today. In
ancient civilization, if someone's home burned down or met with any
disaster, the other members of the community would help together to rebuild
it. Everyone felt morally bound to help in case their home was the next to
burn. Similarly, humans have been managing risk for many years and in the
primitive times the insurance in such economies was agreements of mutual
aid. This type of insurance has survived to the present day in some countries
where a modern money economy with its financial instruments is not
widespread.
Early methods of transferring or distributing risk were practiced by Chinese
and Babylonian traders as long ago as the 3rd and 2nd millennia BC,
respectively. Chinese merchants travelling treacherous river rapids would
redistribute their wares across many vessels to limit the loss due to any
single vessel's capsizing.
The first written account of an insurance policy is found in the Code of
Hammurabi, in the 18th century BC, and was designed to forfeit debts owed
due to catastrophe. The Babylonians developed a system which was
practiced by early Mediterranean sailing merchants. If a merchant received a
loan to fund his shipment, he would pay the lender an additional sum in
exchange for the lender's guarantee to cancel the loan should the shipment
be stolen or lost at sea. Sailing merchants and caravans used this insurance
to protect themselves from the risks of pirates and treacherous natural
terrain. And early health insurance by organized guilds in ancient Greek and
6
Roman civilizations aided surviving members or helped to pay funeral
expenses.
Achaemenian monarchs of Ancient Persia were the first to insure their
people and made it official by registering the insuring process in
governmental notary offices. The insurance tradition was performed each
year where different ethnic groups presented gifts to the monarch. The
presents were assessed by the confidants of the court and this assessment
was registered in special offices. The purpose of registering was that
whenever the person who presented the gift registered by the court was in
trouble, the monarch and the court would help him.
A thousand years later, the inhabitants of Rhodes invented the concept of the
general average. Merchants whose goods were being shipped together would
pay a proportionally divided premium which would be used to reimburse
any merchant whose goods were deliberately jettisoned in order to lighten
the ship and save it from total loss.
Separate insurance contracts (i.e., insurance policies not bundled with loans
or other kinds of contracts) were invented in Genoa in the 14th century, as
were insurance pools backed by pledges of landed estates. These new
insurance contracts allowed insurance to be separated from investment, a
separation of roles that first proved useful in marine insurance. Insurance
became far more sophisticated in post-Renaissance Europe, and specialized
varieties developed.
The first insurance company in the United States underwrote fire insurance
and was formed in Charles Town (modern-day Charleston), South Carolina,
7
in 1732. Benjamin Franklin helped to popularize and make standard the
practice of insurance, particularly against fire in the form of perpetual
insurance.
In India, insurance has a deep-rooted history. It finds mention in the writings
of Manu ( Manusmrithi ), Yagnavalkya ( Dharmasastra ) and Kautilya (
Arthasastra ). The writings talk in terms of pooling of resources that could
be re-distributed in times of calamities such as fire, floods, epidemics and
famine. Insurance in India has evolved over time heavily drawing from other
countries, England in particular.
In the last century, the insurance industry adapted to changing lifestyle and
growth, introducing products such as automobile and health insurance. And
more recently, changing governmental regulations across the world have
impacted the regulations by which the insurance sector operates, enabling
other industries, including the banking industry, to offer similar insurance
products.
8
1.4 Functions of insurance
Provide protection: The primary function of insurance is to provide
protection against future risk, accidents and uncertainty. Insurance
cannot check the happening of the risk, but can certainly provide for
the losses of risk. Insurance is actually a protection against economic
loss, by sharing the risk with others.
Collective bearing of risk: Insurance is an instrument to share the
financial loss of few among many others. Insurance is a mean by
which few losses are shared among larger number of people.
All the insured contribute the premiums towards a fund and out of
which the persons exposed to a particular risk is paid.
Assessment of risk: Insurance determines the probable volume of
risk by evaluating various factors that give rise to risk. Risk is the
basis for determining the premium rate also.
Provide certainty: Insurance is a device, which helps to change from
uncertainty to certainty. Insurance is device whereby the uncertain
risks may be made more certain.
Small capital to cover larger risk: Insurance relieves the
businessmen from security investments, by paying small amount of
premium against larger risks and uncertainty.
Contributes towards the development of industries: Insurance
provides development opportunity to those larger industries having
more risks in their setting up. Even the financial institutions may be
prepared to give credit to sick industrial units which have insured their
assets including plant and machinery.
9
Means of savings and investment: Insurance serves as savings and
investment, insurance is a compulsory way of savings and it restricts
the unnecessary expenses by the insured's For the purpose of availing
income-tax exemptions also, people invest in insurance.
Source of Earning Foreign Exchange: Insurance is an international
business. The country can earn foreign exchange by way of issue of
marine insurance policies and various other ways.
Risk free trade: Insurance promotes exports insurance, which makes
the foreign trade risk free with the help of different types of policies
under marine insurance cover.
10
1.5 The Benefits of Insurance
What advantages does society gain from an insurance system's operation?
How do these benefits compare with the resources used? One of the greatest
benefits with which an insurance system rewards society is stability in
families. Insurance prevents families from experiencing the great hardships
caused by unexpected losses of property or the premature death of the family
income provider. Insurance allows families to continue their activities in a
much more normal fashion after a loss than would be the case if no
insurance existed.
Insurance is also very useful to businesses. Insurance aids the planning
process because the planner knows a property loss will not mean financial
ruin, and the future of a business cannot be destroyed by a fire or the death
of a key person.
Insurance facilitates credit transactions because creditors are more willing to
lend money if the debtor's death does not make collection of the loan
difficult or impossible. Likewise, lenders are more willing to make property
or real estate loans if they know a disaster cannot destroy the financial
security standing behind their loan.
An economist would give insurance system high marks because it functions
as an antimonopoly device. That is, if no insurance system were available,
only the largest businesses could sustain losses and remain in operation.
Without insurance, there would be a tendency toward monopoly in many
industries. For example, one of the nation's largest chains of grocery stores
could probably lose one of its stores in a fire and remain in business,
11
whereas a mom and pop grocery would probably have to close permanently
if an uninsured fire were to destroy its only store. Smaller chains of stores
could not sustain uninsured losses as well as the larger chains. Insurance
allows the smaller operators to pool their exposure to loss and thus remain
competitors in an industry.
Financiers recognize that insurance availability has a tendency to lower a
firm's cost of capital because both creditors and investors would charge
much more for the use of their money if it were subjected to the risks
associated with natural disasters in addition to business risks. In addition,
without insurance, firms would have to hold more money in relatively
nonproductive near cash reserves to protect themselves against the rainy day.
Insurance companies, and the organizations they support, contribute directly
to society's welfare in many ways relating to loss prevention and medical
research. Insurance companies are very important financial intermediaries.
Annually, life insurance companies collect billions of dollars in people's
savings and reinvest these amounts in the economy. Property insurers also
maintain billions of dollars in their reserve accounts that are invested in our
private enterprise economy. Insurers provide a useful service to savers by
evaluating and selecting sound investments. They also provide a service to
business firms and governmental units at the local, state, and federal levels,
In general, business and government borrowers do not find it practical to use
the small savings streams of individuals, but they can effectively use the
river of funds made available by insurance companies.
Benefits Health insurance is a type of insurance that helps the availability of
health insurance funds if participants develop health problems or illnesses.
12
All the needs of seeing a doctor, stay (care) in hospitals, drug costs in the
hospital until the operation, all that can be covered by insurance companies.
Generally these types of treatment or programs that are available are the
benefits of ambulatory (outpatient), benefit of inpatient care (inpatient),
labor benefits and dental benefits.
In general, the benefits of ambulatory (outpatient) are covered by insurance
companies is as consulting fees or general practitioner and specialists,
prescription medication costs, costs of preventive measures, the cost of
assistive devices required by doctors, and others. In the outpatient benefits
have maximum limits use of funds each year. While hospitalization benefits
that can be enjoyed by participants of health insurance is like the hospital
costs, lab fees, delivery fees, the cost of emergency service (emergency).
The benefits of preventive dental care, basic dental care, dental care
complex, and the installation of dentures.
Third-care benefits, namely outpatient, maternity and dental benefits are an
additional option that we can take the following basic program, which
benefits of hospitalization. So, we are not allowed to just take advantage of
outpatient care, childbirth or dental work alone without following the basic
program of hospitalization benefits.
The amount of premium to be paid and the amount of value in health
insurance is dependent on the health insurance program that we choose.
Various insurance companies have the types of programs and premiums vary
by the details of benefits also varies. Typically, insurance companies limit
the amount of the total cost that can be used per year.
13
How Insurance Benefits Society and the Economy
Providing Security: There is always a fear of sudden loss. There may
be a fire in factory, storm in the sea or loss of life .In all these cases it
becomes difficult to bear the loss. Insurance provides a cover against
any sudden loss.
Spreading Risk: The basic principal of insurance is to spread risk
among a large number of peoples. A large number of persons get the
insurance policies and pay premier to the insurer .whenever a loss
occurs, it is compensated out of fund to the insurer
Source for collecting funds: The premium is received regularly in
installments .Large funds are collected by way of premium. It helps in
collecting saving from a large number of persons. The funds can be
gainfully employed in industrial development of a country.
Encourage savings: Insurance does not only protect the risks but it
provides the investment channel too. Life insurance provides a mode
of investment. In case of fixed time policies, the insured gets lump
sum amount after the maturity of the policies.
Improving consumer and worker safety: Insurance makes
businesses and individuals more aware of the risks they face and
provides motivation to prevent losses. For example, insurers provide
premium discounts to safe drivers and to businesses that implement
effective worker safety programs.
14
Protecting consumer transactions: Most consumers have to borrow
money to buy homes and cars; lenders require insurance in order to
secure the loans they make for these purchases. Without insurance,
few people could obtain an auto loan or home mortgage.
Protecting business transactions: Without insurance, most businesses
would find that they could not operate. Insurance enables businesses
of all sizes and types to manage the risks that are an inherent part of
any business operation (e.g., signing contracts, financing and
expanding operations, manufacturing and distributing products,
providing services, hiring employees).
Providing recovery from catastrophes: Hurricanes, winter storms,
fires, and other disasters can cause tremendous, sudden loss to many
people all at once. Insurance coverage enables businesses to replace
inventories and rebuild buildings, and allows homeowners to repair
and rebuild homes and replace property.
15
CHAPTER 2 OVERVIEW OF INSURANCE IDUSTRY
2.1 Overview of Insurance
With largest number of life insurance policies in force in the world,
Insurance happens to be a mega opportunity in India. It's a business growing
at the rate of 15-20 per cent annually and presently is of the order of Rs 450
billion. Together with banking services, it adds about 7 per cent to the
country's GDP. Gross premium collection is nearly 2 per cent of GDP and
funds available with LIC for investments are 8 per cent of GDP.
Yet, nearly 80 per cent of Indian population is without life insurance cover
while health insurance and non-life insurance continues to be below
international standards. And this part of the population is also subject to
weak social security and pension systems with hardly any old age income
security. This it is an indicator that growth potential for the insurance sector
is immense.
A well-developed and evolved insurance sector is needed for economic
development as it provides long term funds for infrastructure development
and at the same time strengthens the risk taking ability. It is estimated that
over the next ten years India would require investments of the order of one
trillion US dollar. The Insurance sector, to some extent, can enable
investments in infrastructure development to sustain economic growth of the
country. Insurance is a federal subject in India. There are two legislations
that govern the sector- The Insurance Act- 1938 and the IRDA Act- 1999.
16
In India, insurance is generally considered as a tax-saving device instead of
its other implied long term financial benefits. Indian people are prone to
investing in properties and gold followed by bank deposits. They selectively
invest in shares also but the percentage is very small. Even to this day, Life
Insurance Corporation of India dominates Indian insurance sector. With the
entry of private sector players backed by foreign expertise, Indian insurance
market has become more vibrant.
Insurance Sector Reforms
In 1993, Malhotra Committee- headed by former Finance Secretary and RBI
Governor R.N. Malhotra- was formed to evaluate the Indian insurance
industry and recommend its future direction. The Malhotra committee was
set up with the objective of complementing the reforms initiated in the
financial sector. The reforms were aimed at creating a more efficient and
competitive financial system suitable for the requirements of the economy
keeping in mind the structural changes currently underway and recognizing
that insurance is an important part of the overall financial system where it
was necessary to address the need for similar reforms. In 1994, the
committee submitted the report and some of the key recommendations
included:
i) Structure
Government should take over the holdings of GIC and its subsidiaries so that
these subsidiaries can act as independent corporations. All the insurance
companies should be given greater freedom to operate.
17
ii) Competition
Private Companies with a minimum paid up capital of Rs.1bn should be
allowed to enter the sector. No Company should deal in both Life and
General Insurance through a single entity. Foreign companies may be
allowed to enter the industry in collaboration with the domestic companies.
Postal Life Insurance should be allowed to operate in the rural market. Only
one State Level Life Insurance Company should be allowed to operate in
each state.
iii) Regulatory Body
The Insurance Act should be changed. An Insurance Regulatory body should
be set up. Controller of Insurance- a part of the Finance Ministry- should be
made independent
iv) Investments
Mandatory Investments of LIC Life Fund in government securities to be
reduced from 75% to 50%. GIC and its subsidiaries are not to hold more
than 5% in any company (there current holdings to be brought down to this
level over a period of time)
v) Customer Service
LIC should pay interest on delays in payments beyond 30 days. Insurance
companies must be encouraged to set up unit linked pension plans.
Computerization of operations and updating of technology to be carried out
in the insurance industry
18
The committee emphasized that in order to improve the customer services
and increase the coverage of insurance policies, industry should be opened
up to competition. But at the same time, the committee felt the need to
exercise caution as any failure on the part of new players could ruin the
public confidence in the industry.
The committee felt the need to provide greater autonomy to insurance
companies in order to improve their performance and enable them to act as
independent companies with economic motives. For this purpose, it had
proposed setting up an independent regulatory body- The Insurance
Regulatory and Development Authority.
Reforms in the Insurance sector were initiated with the passage of the IRDA
Bill in Parliament in December 1999. The IRDA since its incorporation as a
statutory body in April 2000 has fastidiously stuck to its schedule of framing
regulations and registering the private sector insurance companies. Since
being set up as an independent statutory body the IRDA has put in a
framework of globally compatible regulations. The other decision taken
simultaneously to provide the supporting systems to the insurance sector and
in particular the life insurance companies was the launch of the IRDA online
service for issue and renewal of licenses to agents. The approval of
institutions for imparting training to agents has also ensured that the
insurance companies would have a trained workforce of insurance agents in
place to sell their products.
19
Present Scenario
The Government of India liberalized the insurance sector in March 2000
with the passage of the Insurance Regulatory and Development Authority
(IRDA) Bill, lifting all entry restrictions for private players and allowing
foreign players to enter the market with some limits on direct foreign
ownership. Under the current guidelines, there is a 26 percent equity cap for
foreign partners in an insurance company. There is a proposal to increase
this limit to 49 percent.
The opening up of the sector is likely to lead to greater spread and deepening
of insurance in India and this may also include restructuring and revitalizing
of the public sector companies. In the private sector 12 life insurance and 8
general insurance companies have been registered. A host of private
Insurance companies operating in both life and non-life segments have
started selling their insurance policies since 2001.
Non-Life Insurance Market
In December 2000, the GIC subsidiaries were restructured as independent
insurance companies. At the same time, GIC was converted into a national
re-insurer. In July 2002, Parliament passed a bill, de-linking the four
subsidiaries from GIC.
Presently there are 12 general insurance companies with 4 public sector
companies and 8 private insurers. Although the public sector companies still
dominate the general insurance business, the private players are slowly
gaining a foothold. According to estimates, private insurance companies
have a 10 percent share of the market, up from 4 percent in 2001. In the first
20
half of 2002, the private companies booked premiums worth Rs 6.34 billion.
Most of the new entrants reported losses in the first year of their operation in
2001.
Insurance, like project finance, is extended by a consortium. Normally one
insurer takes the lead, shouldering about 40-50 per cent of the risk and
receiving a proportionate percentage of the premium. The other companies
share the remaining risk and premium. The policies are renewed usually on
an annual basis through the invitation of bids.
Of late, with IPP projects fizzling out, the insurance companies are turning
once again to old hands such as NTPC, NHPC and BSES for business.
Re-insurance business
The balance risk is re-insured with other insurers. In effect, therefore, re-
insurance is insurer's insurance. It forms the backbone of the insurance
business. It helps to provide a better spread of risk in the international
market, allows primary insurers to accept risks beyond their capacity settle
accumulated losses arising from catastrophic events and still maintain their
financial stability.
Life Insurance Market
The Life Insurance market in India is an underdeveloped market that was
only tapped by the state owned LIC till the entry of private insurers. The
penetration of life insurance products was 19 percent of the total 400 million
of the insurable population. The state owned LIC sold insurance as a tax
instrument, not as a product giving protection. Most customers were under-
21
insured with no flexibility or transparency in the products. With the entry of
the private insurers the rules of the game have changed.
The growing popularity of the private insurers shows in other ways. They
are coining money in new niches that they have introduced. The state owned
companies still dominate segments like endowments and money back
policies. But in the annuity or pension products business, the private insurers
have already wrested over 33 percent of the market. And in the popular unit-
linked insurance schemes they have a virtual monopoly, with over 90
percent of the customers.
With an annual growth rate of 15-20% and the largest number of life
insurance policies in force, the potential of the Indian insurance industry is
huge. Total value of the Indian insurance market (2004-05) is estimated at
Rs. 450 billion (US$10 billion). According to government sources, the
insurance and banking services' contribution to the country's gross domestic
product (GDP) is 7% out of which the gross premium collection forms a
significant part. The funds available with the state-owned Life Insurance
Corporation (LIC) for investments are 8% of GDP.
The year 1999 saw a revolution in the Indian insurance sector, as major
structural changes took place with the ending of government monopoly and
the passage of the Insurance Regulatory and Development Authority (IRDA)
Bill, lifting all entry restrictions for private players and allowing foreign
players to enter the market with some limits on direct foreign ownership.
Though the focus of this market research report is on the potential growth on
the Indian Insurance Sector, it also talks about the market size, market
22
segmentation, and key developments in the market after 1999. The report
gives an instant overview of the Indian non-life insurance market, and
covers fire, marine, and other non-life insurance. The data is supplied in both
graphical and tabular format for ease of interpretation and analysis. This
report also provides company profiles of the major private insurance
companies.
Just like other forms of insurance, for your car and your home, health
insurance helps relieve the burden of unexpected events: you put away a
little in case you need a lot later. You and your family's health should be of
the highest priority.
Every year, the cost of healthcare increases dramatically. Simple same-day
surgeries, required tests and emergency attention can add up to thousands of
dollars or more.
The overall benefits of health insurance are obvious. You won't be avoiding
the doctor because it costs too much. The hospital bills won't be piling upon
your desk waiting for attention. Your health insurance will provide the help
and care you demand. Also, if you drive a car, health insurance will work
cooperatively with your auto insurance in case of an accident.
There are many health insurance companies available, offering
various types of plans. We are capable to get you the best plan and
coverage to suit your needs.
Using this comprehensive tutorial, you can find out about different
types of health insurance, choosing a policy, and much more.
23
2.2 Innovations in insurance
Several insurance folk who, between them, have more than a hundred years
experience of the sector, were kind enough to provide a considerable amount
of feedback regarding this article. Rather than revise the original I thought it
would be helpful if I summarised what they had to say as a postscript.
There were ten key points which I have put in alphabetical order: you will
have your own view of their relative importance.
1. Actuaries influence
2. Branding
3. Complex distribution
4. Customer engagement
5. Execution
6. Fast follower
7. Knowing V/s doing
8. Mixed message
9. Performance message
10. Pricing
24
1. Actuaries influence. Only a numpty could claim that we could have an
insurance industry without actuarial science at its heart. But do actuaries
dominant the industry to its detriment? Does the professions particular
group think stifle non-analytic thinking? Perhaps the actuarial exams
should encourage different ways of looking at the same issue in much the
same way as the Accountancy training involves current cost, historic cost
and replacement cost accounting?
2. Branding. Organisations with strong brands seem to tune in intuitively to
emotional intelligence, the value of intangible assets, and business renewal
(updating the core brand proposition in response to changing market
conditions). In the insurance sector branding is weak and too often confused
with name recognition. This marketing-naive mindset will inevitably see
innovation as a low business priority.
3. Complex distribution. Ignore how we got here but the fact is that today
our distribution models are so complex that they discourage innovation
because of the perceived free-rider risk.
4. Customer engagement. Once upon a time the market capitalisations of
Unilever and Procter & Gamble comfortably exceeded those of the
supermarkets. Not anymore. Retailers are bathed daily in large amounts of
data that are transformed, with varying degrees of success, in to information
and insight. Retailers are plugged in to their consumers behaviour and
theyve the service cultures to match. That is valuable. Insurers have nothing
like this degree of engagement with their consumers. This, in turn,
25
encourages slow learning and discourages innovation because it cant be
done fast enough or confidently enough.
5. Execution. We can view innovation as Insight + Execution. Not only
does the insurance sector underperform when it comes to the Insight
element, but the Execution skills may be seen as a handicap also, because in
the insurance sector execution is focused on compliance and getting it right
first time, whereas retailers, for example, can execute quickly and well
enough and act on the results.
6. Fast follower. This strategy has a respectable history in the insurance
sector and is not career threatening. Being innovative, on the other hand, can
easily be seen as sticking-ones-neck-out and asking for trouble.
7. Knowing vs Doing. Theres an irony here. The industry (along with
Government) is assigning a good deal of time and resource to making
consumers more financially capable in the belief that there is a big gap
between what consumers actually know about finance and what we need to
know. In fact the important gap is not between not-knowing and knowing; it
is between knowing and doing. And the same is true when it comes to
innovation in the insurance sector. The industry knows what to do. It knows
that shareholders, customers, employees and the wider community would
benefit if it became more innovative. But it chooses not to. There are higher
priorities. There are habits to change. The costs and pain are immediate. The
benefits are deferred.
26
8. Mixed messages. There are mixed messages not only between the
industry and its customers but also within the industry itself. We sell
promises. With some products the consumer can be confident that he or she
can collect on that promise pretty much a hundred percent of the time. But
not with all products. Mixed message number 1. In financial services, we
implicitly criticise consumers for being financially feckless yet at the same
time put more effort in to selling products that promote fecklessness (e.g.
credit cards, loans, overdrafts) and less effort in to those that reward the
behaviours we say are good (e.g. savings, pensions, or protection). Mixed
message number 2. This lack of clarity doesnt encourage innovation.
9. Performance measurement. You wake up tomorrow to find that you are
the CEO of an insurance company. Consider what you will find in your in
tray. Consider your corporate business agenda and priorities. Consider your
corporate culture. Consider the performance measures that will drive the
company regarding business-as-usual items such as advertising, capital
adequacy, claims management, compliance, customer service, employee
engagement, improved Governance, investor relations, and reducing
operational risk. Where is innovation going to add most value? How
confident can you be that the benefits of developing innovation as a
corporate competence will outweigh the direct costs, opportunity costs, and
risks?
27
10. Pricing. In our marketing we over focus on price and then complain
when consumers do. We complain too about commoditisation when
aggregators and our promotion campaigns encourage it. We also seem to
feel that our industry is significantly different to other industries and that (a)
what applies to them does not apply to us and that (b) innovation is an
example of this. But who are we kidding?
28
CHAPTER 3 HEALTH INSURANCE
3.1 Health insurance
Health insurance is insurance against the risk of incurring medical
expenses among individuals. By estimating the overall risk of health care
and health system expenses among a targeted group, an insurer can develop
a routine finance structure, such as a monthly premium or payroll tax, to
ensure that money is available to pay for the health care benefits specified in
the insurance agreement. The benefit is administered by a central
organization such as a government agency, private business, or not-for-profit
entity. The term health insurance (popularly known as Medical Insurance or
Mediclaim) is a type of insurance that covers your medical expenses.The
concept of health insurance is new in India but its awareness is growing fast.
Health insurance comes in handy in case of severe emergencies. Life is
unpredictable, insurance can make it safe and secure from bearing huge
financial loss. A health insurance policy is a contract between an insurance
company and an individual. Sometimes it is associated with covering
disability and custodial needs. The contract is renewable annually.
Health insurance is available to both individual and groups. However,
premium for individual policy is costlier than that of the group policy. An
individual is the owner of his personal policy. Whereas in group plans, the
sponsor is the owner of the policy and the registered members are covered
by the policy. You can take advantage of group health insurance to
overcome the shortage of your individual insurance. People with no policy
or are uninsurable due to one or the other reason can take good advantage of
the group plans and be covered.
29
However, before buying a health insurance policy, plan your requirements
carefully. It will save you from buying a policy which might not be
appropriate for you and can also be expensive.
A health insurance policy is:
1) a contract between an insurance provider (e.g. an insurance company or a
government) and an individual or his/her sponsor (e.g. an employer or a
community organization). The contract can be renewable (e.g. annually,
monthly) or lifelong in the case of private insurance, or be mandatory for all
citizens in the case of national plans. The type and amount of health care
costs that will be covered by the health insurance provider are specified in
writing, in a member contract or "Evidence of Coverage" booklet for private
insurance, or in a national health policy for public insurance.
2) Insurance coverage is provided by an employer-sponsored self-funded
ERISA plan. The company generally advertises that they have one of the big
insurance companies. However, in an ERISA case, that insurance company
"doesn't engage in the act of insurance", they just administer it. Therefore
ERISA plans are not subject to state laws. ERISA plans are governed by
federal law under the jurisdiction of the US Department of Labor (USDOL).
The specific benefits or coverage details are found in the Summary Plan
Description (SPD). An appeal must go through the insurance company, then
to the Employer's Plan Fiduciary. If still required, the Fiduciarys decision
can be brought to the USDOL to review for ERISA compliance, and then
file a lawsuit in federal court.
30
The individual insured person's obligations may take several forms:
Premium: The amount the policy-holder or his sponsor (e.g. an
employer) pays to the health plan to purchase health coverage.
Deductible: The amount that the insured must pay out-of-pocket
before the health insurer pays its share. For example, policy-holders
might have to pay a $500 deductible per year, before any of their
health care is covered by the health insurer. It may take several
doctor's visits or prescription refills before the insured person reaches
the deductible and the insurance company starts to pay for care
however, most policies do not apply co-pays for doctor's visits or
prescriptions against your deductible.
Co-payment: The amount that the insured person must pay out of
pocket before the health insurer pays for a particular visit or service.
For example, an insured person might pay a $45 co-payment for a
doctor's visit, or to obtain a prescription. A co-payment must be paid
each time a particular service is obtained.
Coinsurance: Instead of, or in addition to, paying a fixed amount up
front (a co-payment), the co-insurance is a percentage of the total cost
that insured person may also pay. For example, the member might
have to pay 20% of the cost of a surgery over and above a co-
payment, while the insurance company pays the other 80%. If there is
an upper limit on coinsurance, the policy-holder could end up owing
very little, or a great deal, depending on the actual costs of the
services they obtain.
31
Exclusions: Not all services are covered. The insured are generally
expected to pay the full cost of non-covered services out of their own
pockets.
Coverage limits: Some health insurance policies only pay for health
care up to a certain dollar amount. The insured person may be
expected to pay any charges in excess of the health plan's maximum
payment for a specific service. In addition, some insurance company
schemes have annual or lifetime coverage maxima. In these cases, the
health plan will stop payment when they reach the benefit maximum,
and the policy-holder must pay all remaining costs.
Out-of-pocket maxima: Similar to coverage limits, except that in this
case, the insured person's payment obligation ends when they reach
the out-of-pocket maximum, and health insurance pays all further
covered costs. Out-of-pocket maxima can be limited to a specific
benefit category (such as prescription drugs) or can apply to all
coverage provided during a specific benefit year.
Capitation: An amount paid by an insurer to a health care provider, for
which the provider agrees to treat all members of the insurer.
In-Network Provider: (U.S. term) A health care provider on a list of
providers preselected by the insurer. The insurer will offer discounted
coinsurance or co-payments, or additional benefits, to a plan member
to see an in-network provider. Generally, providers in network are
providers who have a contract with the insurer to accept rates further
discounted from the "usual and customary" charges the insurer pays to
out-of-network providers.
32
Prior Authorization: A certification or authorization that an insurer
provides prior to medical service occurring. Obtaining an
authorization means that the insurer is obligated to pay for the service,
assuming it matches what was authorized. Many smaller, routine
services do not require authorization.
Explanation of Benefits: A document that may be sent by an insurer to
a patient explaining what was covered for a medical service, and how
payment amount and patient responsibility amount were determined.
33
3.2 Benefits of health plans
The utility of your cover depends not only on its features, but also how well
you are able to utilise them. Read on to understand such benefits.
1. Daily hospital cash allowance
All health policies take care of the cost of hospitalisation. However, what
about the expenses incurred on, say, food or refreshments? Or, the money
spent by your family while commuting between hospital and home? After
all, even these add up to a substantial amount. Well, the solution lies within
your policy in the form of Daily Hospital Cash Allowance. Check if your
policy offers this pre-fixed, per-day cash hand-outs.
"This sum is handed over without the insured having to produce any bill to
support the claim, no questions asked," says Sanjay Datta, head,
underwriting & claims, ICICI Lombard.
2. Convalescence benefit
Hospitalisation costs apart, some companies also take care of the insured's
recovery expenses. Also termed as recuperating benefit, this feature
promises a lump sum in case of a prolonged stay at the hospital. "The
duration of prolonged stay usually varies between 7 and 10 days among
policies.
This benefit is usually provided to ensure supplementary costs due to the
stay in hospital, such as a loss of income for the number of days in hospital,"
says Antony Jacob, CEO, Apollo Munich. "Associated costs, such as
compassionate visits by family members, are also covered to some extent."
34
In case of some policies, the post-hospitalisation stage could be treated as
the recuperating period. You need to be aware of the eligible benefit amount
and period, which are usually pre-defined.
3. Alternative treatment
The recent Insurance Regulatory and Development Authority (Irda) draft
guidelines may nudge all companies into covering non-allopathic forms of
treatment, like Ayurveda, Unani and Homeopathy, but some of them do so
even today. For instance, New India Assurance undertakes to reimburse 25%
of such expenses, provided the treatment is taken at a government hospital.
The proposed norms seek to let insurers to pay for these expenses even if the
treatment has been availed at any institute that is either recognised by the
government, accredited by Quality Council of India/National Accreditation
Board on Health or any other suitable institution.
4. Treatment taken at home
The general impression of health insurance covers is that their scope is
restricted to hospitalisation or day-care procedures. However, many policies
widen their coverage ambit to include domiciliary treatment, too. That is,
treatment undergone at home as per doctor's advice. Primarily, this would be
because the patient is unable to visit a hospital. "Here, the insured may be
asked to submit bills from the doctor's clinic.
The pay-out is percentage or value-based," says Datta. The amount and the
number of days for which the benefit period is payable is capped in terms of
percentage of the sum insured or absolute amount. For instance, your policy
35
wordings could make it clear that the benefit is restricted to 10% of the sum
insured or Rs 25,000, whichever is lower.
5. Other Benefits
Doctor services
Hospital services, including inpatient serviceswhen you have to
stay overnight in the hospitaland outpatient services, such as minor
surgery in a surgery center
Many laboratory tests
Diagnostic services, like X-rays and mammograms
Preventive and routine care, like vaccinations and regular checkups
Mental health care for some serious problems
Emergency and urgent careeven if you are outside your health
plan's service area
Rehabilitation therapy, such as physical, occupational and speech
therapy
Some home health or nursing home care after a hospital stay
36
3.3 Disadvantages of health insurance
1. Increased Costs and Labor
In keeping up with the stringent provisions of HIPAA the businesses that
manage your healthcare have to bear increased expenditure on computers
and software for adhering with all the privacy requirements. The paperwork
also increases significantly to comply with the Act due to provisions of
portability etc. Furthermore the businesses have to keep readjusting their
policies according to amendments in the Act and may also have to hire
people and provide adequate training to work within the purview of HIPAA.
2. Misinterpretations and Restrictions:
The elaborate privacy rules of HIPAA can often come in the way during
emergency situations as such private information can be dispensed only to
certain entities and that too for a short period. Furthermore any
misinterpretation of the provisions may impede or slow down the passing of
information. For example, healthcare companies might find it difficult to get
information about a person from hospitals. Fear of the law can also affect
research work carried out by doctors.
3. Electronic Format:
HIPAA urges widespread use of electronic formats to store, process and
share information. Such systems must huge spending and considerable
maintenance costs then. Also since such medium is susceptible to attacks,
the security measures have to be constantly updated to keep the data safe
against unauthorized access, corruption and stealing.
37
4. Cost:
Health insurance can be very costly even for those that have a health
insurance plan through their employers. This cost can sometimes be so
expensive that the person may struggle to make payments. This is
problematic for those that have a low income or are self-employed. Families
may also have a great deal of difficulty affording coverage for the entire
family because of the cost. In addition, even if someone is able to afford
health insurance, they may not be able to afford the co-pays. Some health
insurance plans have high co-pays that can be costly to a person with an
average or low income level. In the end, the total cost has to be carefully
weighed by the person considering health insurance.
5. Medical Coverage:
Actual medical coverage can also be a disadvantage to some people with
health insurance. The medical coverage may not be enough to sufficiently
cover the cost of tests, surgeries and procedures that need to be done. This
can leave the person paying high bills for medical services and may even
cause some people to refuse medical care that they need. This can lead to an
exacerbation of illness or even death, which can end up costing the person,
the person's family, taxpayers and even the government more money.
38
6. Pre-Existing Exclusion:
If a person enrolls in a new group health insurance plan, they may be asked
if they have any pre-existing conditions. According to
Healthinsuranceinfo.net, which is provided through the Georgetown
University Health Policy Institute, some people that have a pre-existing
illness have to undergo a waiting period if changing employers. In addition,
after enrolling in a new group health insurance plan, if a claim is made
during the first year, the insurance company has the right to "look back" to
see if this was due to a pre-existing condition. If it was, the insurance
company may refuse to pay for any charges related to this "pre-existing
condition." This may be in effect for up to 18 months and can be quite
expensive for someone with a serious illness.
39
CHAPTER 4 INTRODUCTION OF IFFCO TOKIO
COMPANY
4.1 Iffco Tokio General Insurance
Profile
Iff-Tokio General Insurance (ITGI) was incorporated on 4th December 2000
with a vision of being industry leader by building customer satisfaction
through fairness, transparency, and quick response. It is a joint venture
between the Indian Farmers Fertilizer Co-operative (IFFCO) and its
associates and Tokio Marine and Nichido Fire Group, the largest listed
insurance group in Japan.
IFFCO Tokio General Insurance has Pan India presence with 65 'Strategic
Business Units' and a wide network of over 120 Lateral Spread Centres and
255 Bima Kendras. It offers a wide range of uniquely customized policies
covering a wide range of customers, from farmers to some of India's largest
automobile manufacturers. From a modest Rs 213 Crores of GWP (Gross
Written Premium) in 2001-02 it has achieved an impressive Rs 2248.16
Crores in 2011-12, thereby becoming one of India's leading private players.
IFFCO Tokio General Insurance has got the Technical Support for
underwriting and reinsurance from Tokio Marine and on Risk Management
from Tokio Risk Consulting (TRC). It is the first company in India to
underwrite mega policies for a fertilizer and an automobile company. This
comprehensive policy is based on international rates and optimizes the
premium outflow for clients even as it offers a one-stop, all-risk cover. Other
than the conventional products, it has been able to come out with niche
40
products like Credit Insurance, Fine Arts Insurance, P & I Insurance, Errors
& Omissions Policy for the IT Sector etc. At the same time it has steadfastly
carried out its rural centric initiatives by launching products like Sankat
Haran Bima Yojana, Mausam Bima Yojana, Mahila Suraksha Bima Yojana
and Janata Bima Yojana for the masses. It's pioneering work using
technology like RFID(Radio Frequency Identification Device) and NDVI
(Normalised Difference Vegetation Index) have made it possible to offer
Cattle and Weather insurance to the rural population at large.
It is also the only insurance company in the country to have a 100%-owned
distribution channel to service its retail customers called IFFCO-TOKIO
Insurance Services Ltd (ITIS). It finds special mention in the 'Capgemini
World Insurance Report- 2009' as an innovative distribution channel. Today,
ITIS has a highly motivated workforce of over 1500 employees in over 350
towns.
As a customer focused company, it conducts bi-annual customer satisfaction
surveys through independent agencies to gauge its operational efficiencies.
This is backed by a robust IT infrastructure, which has enabled, among other
things, speedy settlement of claims.
Subsidiaries
IFFCO-Tokio Insurance Services Limited (ITIS) is a wholly owned
subsidiary and a retail marketing arm of ITGI. It was incorporated on 1st
August 2003. Developing of retail and personal lines has been the major
focus of the company along with spreading into Tier II & III towns and
developing co-operative initiatives for ITGI.
41
At present, ITIS has more than 120 Lateral Spread Centres (LSC) and 255
Bima Kendras (BK) with an employee base of over 1500. Through these two
models, ITGI has extended its network to Tier II & III towns. Bima Kendras
are manned by one or two persons and are usually located in Cooperative
societies which act as the nodal point for sales and service.
IFFCO-Tokio Insurance Services imparts intensive training to its staff by
virtue of its unique online training system as well as classroom training. The
online training system - Gurukul is an interactive training tool which can be
accessed by any employee over internet. It has over 200 modules which
imparts training on insurance products, processes as well as soft skills.
ITIS aspires to become an effective Corporate Agent and gradually diversify
into life and financial products to become a one stop shop for all financial
products.
42
4.2 Micro Insurance by the Iffco-Tokio
The focus of Micro insurance is on the low income segment ignored by
mainstream commercial & social insurance schemes. It may be described as
a "back to basics" campaign. It is characterised by low premium and low
coverage limits. Each policy generates a "micro" financial transaction.
However, the risks are not "micro" to the households which experience
them. Low Income people are exposed to numerous perils. They live in
continuous uncertainty about whether and when a loss might occur. Poverty
and vulnerability reinforce each other in a viciously escalating downward
spiral.
Developing countries lack an effective social protection mechanism to
systematically reach the vast majority of the population which is engaged in
the informal economy. By offering cost-effective risk-hedging instruments,
micro insurance strives to provide some coverage to the excluded. It is thus
integral to any poverty reduction strategy.
By linking multiple small units into larger structures, micro insurance pools
the risk and creates networks that enable better governance. This gives easy
access to reinsurance and helps to generate data which can help in product
design and development.
India will merit a special mention in the history of microinsurance. It
became the first country to have a special regulation on the subject. IRDA
made it mandatory for all formal insurance companies to extend their
activities to rural & social sectors. As former IRDA Chairmnn, Mr C.S. Rao
43
put it succinctly, "IRDA made serving the poor compulsory for insurers in
India."
Iffco Tokio's micro-insurance initiatives are driven by the vision of its parent
company IFFCO which seeks to improve the quality of life of the Indian
farmer. Rather than merely downscaling existing products, it has leveraged
IFFCO's experience of the rural market to craft a product basket designed
specifically for the agricultural sector.
Some of the products are : -
Janta Bima Yojna- This is a comprehensive customized policy offering a
personal accident cover to the insured and his spouse on a floater basis and a
fire & allied perils and burglary cover to the building(house) and its
contents. Three options of Sum insured ( ranging from Rs. 12,500 to Rs
30,000 for the property section and Rs. 15,000 TO Rs .50,000 for the
personal accident section and premium payable ( ranging from Rs 100 to Rs
250), are offered. The policy can be taken on an individual or group basis.
Jan Swasthya Bima Yojna- This group health policy covers hospitalization
expenses, in case hospitalization is necessitated following an accident or
disease. The Sum insured ranges from Rs. 15000 to Rs. 30000 in multiples
of Rs. 5000.
Jan Kalyan Bima This provides comprehensive protection against loss or
damage to the property insured by Fire and allied perils and burglary &
house breaking. It also covers risks of Personal accident and 10 Critical
illnesses. The sum assured is Rs 50,000
44
Jan Suraksha Bima- This is a Personal accident policy for Self Help
Groups providing coverage against death, permanent total disablement,
permanent partial disablement and temporary total disablement resulting out
of an accident.
Mahila Suraksha Bima Yojna- The coverage is same as that of Jan
Suraksha Bima Yojna and is meant for women Self Help Groups only.
Pashudhan Bima Yojna- is a cattle insurance policy applicable to
indigenous, cross breeds and exotic breeds of cattle, covering the death of
the animal due to accident, disease, surgical operations , strike , riot and civil
commotion (SRCC), terrorism and earthquake.
Barish bima Yojna (BBY) - This is an Index based Weather Insurance
Product for Kharif (monsoon) crops like Jowar, paddy, soyabean, cotton etc.
which provides cover for financial losses arising due to deficient or excess
rainfall. The cover is operative during the monsoon months i.e. July to
September/ June to September/ July to October. The maximum Sum Insured
under the micro version of this policy is Rs. 30000/-.
Mausam Bima Yojna (MBY) - The policy provides cover for Rabi crops
like Wheat, Mustard, Potato etc. against financial losses arising due to
adverse weather perils- Temperature, Humidity and Unseasonal Rainfall
during the Rabi season. The maximum Sum Insured under the micro version
of this policy is Rs. 30000/-.
45
Micro insurance is still in its infancy. Problems include high transaction
costs, inappropriate distribution systems, product design issues especially
related to the irregular cash flows of the low income market and lack of data
to interpret the vulnerabilities of the poor. The challenge is to promote an
insurance culture in the low income group and simultaneously develop an
appropriate business model that creates a profitable & sustainable market at
the "bottom of the pyramid." This will help to realise the immense potential
of the vast, underserved market of low income households.
46
4.3 The IFFCO Tokio Edge:
The business model for this segment thrives on technological and channel
innovations to overcome the challenges, and achieve sustainable profitable
growth.
Optimizing IT for touching India's Hinterland:
Radio Frequency Tagging (RFID):
Animal identification is a critical challenge while deciding the claims
for livestock insurance. Instead of depending on the traditional use of
the metallic and plastic tags, which result in high moral hazard,
IFFCO Tokio has innovatively used the latest RFID tagging for
animal identification and fair and fast claim settlement.
This method involves the use of a transponder and transreceiver for
accurate animal identification, which eliminates of the chances of
fraudulent claims. So far more than 10000 animals have been insured
by this method.
Use of automated weather stations:
In the weather insurance business, the conventional use of weather
data obtained from rain gauges or observatories had problems of
delays and manual interference. To combat this, IFFCO Tokio has
started using data from automated weather stations (AWS), that
,besides providing timely and accurate data to the insurer, also
provides daily data and short term weather forecasts to the associated
47
farmers. It facilitates faster claim settlement , and better client
interface by providing Agro-advisory services.
Insurance bundled with fertilizer purchase
To solve the challenges of accessibility, awareness and distribution;
IFFCO and IFFCO Tokio came up with the unique idea of providing a
Personal accident insurance cover bundled with the purchase of
fertilizers from IFFCO or IPL.
To keep the procedure simple the sales receipt itself acts as the policy
document and can be produced for settlement of claims under the
policy.
Counting on the reach of the promoter (IFFCO) Our parent company IFFCO
is the world's largest fertilizer cooperative with nation-wide network of
about 40000 cooperative societies. We have sought to leverage its brand
value, client database and distribution channel to penetrate the rural and
social segment. Most of our one man offices called Bima Kendras are in the
premises of a cooperative
48
4.4 Specialty Insurance
IFFCO-TOKIO provides a wide variety of policies that are customized to
your needs.
For your convenience, we have grouped them. To access information on any
of the policies, simply click on the link you want.
Credit Insurance Policy
Multi Modal transport (MTO) Insurance Policy
Marine Hull & Machinery Insurance Policy
Jeweller's Block Insurance Policy
Barish Bima Yojna (Weather Insurance) Policy
Sagar Bandhu Bima Policy Insurance Policy
Aviation Insurance Policy
Errors and Omissions (Technology) Insurance Policy
Fine Art Insurance Policy Private Collectors
Fine Art Insurance Policy Art Dealers & Gallery Owners
49
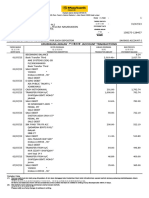
CHAPTER 5 HEALTH INSURANCE IN IFFCO TOKIO
Health Insurance Policies Provided by Iffco tokio
Source: By Researcher
Policies
Individual
Medishield
Insurance
Policy
Swasthya
Kavach (Family
Health
Insurance)
Policy
Swasthya
Kavach (Family
Health
Insurance)
Policy
Critical illness
policy
50
5.1 Individual Medishield Insurance Policy
What does the policy cover?
In the unfortunate event of you or your family members meeting with an
illness or accident resulting in hospitalisation, our Health Insurance gives
you a cash free hospitalisation in more than 3000 hospitals across India. Our
Health Insurance also reimburses the expenses during Pre - Hospitalisation
and Post - Hospitalisation stages of treatment.
Pre-Hospitalisation:
Medical expense incurred 60 days prior to the hospitalization is
reimbursed.
Hospitalisation:
All expenses including the following reimbursed:
Room and board, doctors' fee, intensive care unit charges,
nursing expenses, surgical fees, operating theatre
expenses, anesthesia and oxygen administration expenses,
Room, boarding & nursing expenses for normal room/ICU
limited to 1% /2.5% of basic sum insured per day respectively.
Post-Hospitalisation:
Once discharged from hospital, the policy shall pay for medical
expenses related to the hospitalisation, for a period of 60 days
after discharge.
51
Hospital Daily Allowance:
In addition to hospital expenses, a daily hospital allowance will
be paid for the period of hospitalisation.
Emergency Assistance Service:
In the event of an emergency, assistance services like medical
consultation, evaluation and referral, emergency medical
evacuation, care for minor children etc are provided.
Local Ambulance Service:
In the event of an emergency, cover is provided for expenses
incurred on ambulance services to the nearest hospital where
Emergency Health facilities are available.
General Health Check-up:
You will be reimbursed the expenses incurred for general health
examination (once in a block of 4 claims free years)
Cumulative bonus:
You will be provided with a 5% extra sum insured for every
claims free year subject to a maximum of 50% of capital sum
insured.
52
Benefits under Section - 80D:
Premium upto Rs. 35,000 is eligible for deductions under
Section 80D of Income Tax Act, 1961. However there are sub-
limits within this over-all limit. Premium upto Rs 15,000 is
eligible for tax deduction for self, spouse and dependant
children. Additionally, premium upto Rs 20,000 is eligible for
tax relief or parents health cover if they are senior citizens
(otherwise Rs 15,000 is eligible)
ITGI's Medishield policy ensures comprehensive coverage by offering value
added features, at a nominal increase in premium, like:
Critical illness extension:
You will be covered for 10 named critical illness for double the
basic cover sum insured at 40% of the basic cover premium
53
What does the policy not cover?
Diseases, which have been in existence at the inception of the policy
Illness that commenced during the first 30 days of inception of the
first policy.
Cataracts, Benign Prostatic Hypertrophy, Hysterectomy for
Menorrhagia or Fibromyoma, Hernia, Hydrocele, Fistula in anus,
Piles, Sinusitis and related disorders, in the first year of insurance.
However, on renewal, these exclusions shall not apply. For a complete
list of exclusions, refer to the policy.
Medishield (Individual Plan) covers
Hospitalisation
Pre-hospitalisation
Post - Hospitalisation.
Emergency Assistance Service
Local Ambulance Service.
Family discount is available (5% for 2 people, 10% for 3 or more
people).
Benefits / rates given in the leaflet are indicative Maximum
Entry Age: 5- 55 years (medical reports required above 45 years of
age)
Rates inclusive of service tax.
54
5.2 Swasthya Kavach (Family Health Insurance) Policy
What does the policy cover?
In the unfortunate event of you or your family members meeting with an
illness or accident resulting in hospitalisation, our Swasthya Kavach (Family
Health) Policy gives protection cover for you and your family for any injury
or disease related contingencies like hospitalization, medical expenses,
surgical expenses, organ transplantation, etc. The Policy also offers unique
Critical Illness Coverage (Optional) for the family and is available under two
variants- Base plan and Wider Plan and covers the following:
Pre-Hospitalisation:
Medical expenses incurred 30 days prior to the hospitalization
are reimbursed.
Hospitalisation:
All expenses including the following reimbursed:
Room and board, doctors' fee, intensive care unit charges,
nursing expenses, surgical fees, operating theatre expenses,
anesthesia and oxygen administration expenses. Room expenses
for normal room/ICU limited to 1% /2% of sum insured per day
for Base Plan and 1.5%/2.5% of basic sum insured for Wider
Plan respectively. There are also restrictions on other hospital
expenses in accordance with the room rent under the Base Plan.
55
Post-Hospitalisation:
Once discharged from hospital, the policy shall pay for medical
expenses related to the hospitalisation, for a period of 30 days
after discharge subject to specified limits under Base Plan and
60 days after discharge under wider plan.
Day care surgeries:
The policy covers 121 defined day care surgeries that requires
less than 24 hours hospitalisation and ordinarily fall outside the
scope of most health insurance policies.
Hospital Daily Allowance:
In addition to hospital expenses, a daily allowance will be paid
for the period of hospitalisation.
Emergency Assistance Service:
In the event of an emergency, assistance services like medical
consultation, evaluation and referral, emergency medical
evacuation, care for minor children etc are provided.
Local Ambulance Service:
In the event of an emergency, cover is provided for expenses
incurred on ambulance services to the nearest hospital where
Emergency Health facilities are available.
56
General Health Check-up:
You will be reimbursed the expenses incurred for general health
examination (once in a block of 4 claims free years)
Applicable only under Wider Plan
Cumulative bonus :
You will be provided with a 5% extra sum insured for every
claims free year subject to a maximum of 50% of capital sum
insured- Applicable only under Wider Plan
Benefits under Section - 80D:
Premium upto Rs. 15,000 is eligible for self, spouse and
dependant children with deductions under Section 80D of
Income Tax Act, 1961.
ITGIs Swasthya Kavach Policy ensures comprehensive coverage by
offering value added features, at a nominal increase in premium, like:
Critical illness extension for family:
You will be covered for 10 named critical illness for double the
basic cover sum insured. 10 Critical Illness include: Paralytic
Stroke, Cancer, Renal Failure, Coronary Artery Disease, Major
Injuries, End Stage Liver Disease, Major Burns, Coma, Major
Organ Transplant and Multiple Sclerosis
57
What does the policy not cover?
Diseases, which have been in existence at the inception of the policy
Illness that commenced during the first 30 days of inception of the
first policy.
During the first year of the Policy, the expenses on treatment of
diseases such as Tonsillitis/ Adenoids, Gastric or Duodenal Ulcer, any
type of Cyst/ Nodules/ Polyps, any type of Breast lumps.
During the first two continuous years of the insurance with us, the
expenses on treatment of diseases such as Cataract, Benign Prostatic
Hypertrophy, Hysterectomy for Menorrhagia or Fibromyoma, Hernia,
Hydrocele, Fistula in anus, Piles, Sinusitis, Choletithiasis and
Cholecystectomy, Inter- vertebral Disc Prolapse (other than caused by
an accident), Osteoarthritis, Varicose Veins / Varicose Ulcers etc.
Naturopathy, acupuncture, magnetic treatment, alternative medicines,
etc
Under the Base Plan, during the first two continuous years of the
Policy, the expenses on treatment of diseases such as Renal Failure,
Heart Diseases, any type of Carcinoma/Sarcoma/Blood Cancer.
58
5.3 Group Personal Accident Insurance policy
FFCO TOKIO'S GROUP PERSONAL ACCIDENT POLICY accident
policy is available to provide for payment of compensation in the event of
members of your group:
Sustaining injury, disablement (permanent total, permanent partial and
temporary total) or death arising out of accident
Exclusions
Self injury, suicide, venereal disease or insanity
Influence of intoxicating liquor or drugs
Death due to pregnancy or childbirth
Breach of law with criminal intent
War and nuclear group of perils
On duty with armed forces
We Must Note
That group policies can be given to firm, company, association and
clubs on named as well as unnamed basis where all members must be
included
That group discount is allowed on size of group at inception of the
policy
Additions and deletions can be done during currency of policy for
people joining and leaving
The cover is normally available on 24 hour coverage basis
59
We can offer you discount if you restrict the cover to your employees
for on duty cover only or for off- duty cover only
Other benefits like expenses for ambu1ance charges, damage to
clothes, loss of employment, expenses for carriage of dead body are
admissible- following an accident subject to a limit
Education fund for dependent child is admissible in case death or
permanent total disablement
Documents required for settlement of claims
Claim form
Doctors report, bills in case of temporary/permanent disablement
Police report/post mortem report in case of accidental death
Leave certificate from employer in case of temporary disablement
60
5.4 Critical illness policy
At a time of increasing cost of living, the expenses for medical treatment
have gone up substantially. Particularly if any person contracts a major
disease (critical illness), then he/she has to spend a huge sum of money for
treatment, which most people can ill afford.
Although you cannot prevent the occurrence of serious ailments and
accidents, you can take steps to ensure that the same does not result in
financial ruin for you and your family. ITGI's Critical Illness Insurance
Policy provides just the right kind of cover for such situations at a very
affordable price.
A complete protector
The standard medical cover available in the market is perceived to be rather
expensive for the common man. Normal hospitalization while also involving
a financial strain, can even then be sustained by an average person. but
treatment for critical illness, while saving the person's life could cripple him
financially. By paying a fraction of the normal premium required to be paid
for a full fledged medical cover, complete protection can be taken through
this Policy when it is needed the most. The ailments which are covered
under this Policy are cancer, renal failure, coronary artery diseases requiring
bypass surgery, major organ transplant, paralytic cerebral stroke as well as
accidental injuries resulting in loss of limbs.
61
Benefits Available
Our Policy covers the following heads of expenses, which are normally
incurred in the event of a critical illness treatment:
Room rent and boarding expenses.
Nursing expenses.
Surgeon, anesthetist and medical practitioner/consultant's fees.
Cost of anesthesia, blood, oxygen, operation theatre, surgical
appliances, medicines & drugs, diagnostic materials and X-ray,
dialysis, chemotherapy, radiotherapy, pacemaker, artificial limbs etc.
and similar expenses
When will the Policy not pay?
Some of the important exclusions under the Policy are as follows:
Treatment pertaining to pre-existing diseases.
Any medical treatment due to a disease during the first 120 days of
commencement of insurance cover.
Any expense for treatment related to Human T-Cell Lymphotropic
Viruses Type II (HTLV-III) or Lymphadinopathy Associated Viruses
(LAV) or their mutant derivatives or variations, any syndrome or
condition of a similar kind referred to as AIDS
Treatment for ailments arising out of drug addiction or alcoholism.
Any attempted self injury or suicide
War, nuclear and terrorism risks
62
What extra benefits can be covered?
At an extra premium, you can cover the following items under your Critical
Illness Insurance Policy:
Education cover
Ambulance charges
Cost of travel
Cost of supporting items
Boarding and lodging expenses
Who can apply for this Policy?
This Policy can be issued to various categories of groups as under:
Employers covering their employees including dependants of the
employees
Pre-identified segment/group where the premium is paid by the
State/Central Government.
Members of registered service clubs.
Holders of credit cards or other financial cards.
Holders of deposit or certificate of Banks/NBFCs.
Shareholders of public limited companies, cooperative societies etc.
Students/teachers of educational institutions.
63
CONCLUSION
In the end we can say that health is important factor in our life. Due to
the changing environment human health is badly affecting, so need for
health cover is increasing day by day. Iffco Tokio general Insurance
Company provides various health policies to its customers according to their
varied needs. Hence due to ever increasing medical expenses need for health
insurance is increasing and going to increase in future.
64
WIBLIOGRAPHY
1) www.iffcotokio.co.in
2) www.irda.gov.in
Anda mungkin juga menyukai
- MotivationDokumen148 halamanMotivationdarthvader005Belum ada peringkat
- PrideDokumen1 halamanPridedarthvader005Belum ada peringkat
- Sample MethodologyDokumen7 halamanSample MethodologyNiall KelleherBelum ada peringkat
- IM 4th SemDokumen20 halamanIM 4th Semdarthvader005Belum ada peringkat
- Edited MicrofinanceDokumen59 halamanEdited Microfinancedarthvader005Belum ada peringkat
- Internet BankingDokumen55 halamanInternet Bankingdarthvader005Belum ada peringkat
- Indian Foreign Exc MKTDokumen13 halamanIndian Foreign Exc MKTdinesh_haiBelum ada peringkat
- K.G.Joshi College of Arts & N.G.Bedekar College of Commerce Certificate of Project WorkDokumen2 halamanK.G.Joshi College of Arts & N.G.Bedekar College of Commerce Certificate of Project Workdarthvader005Belum ada peringkat
- Employee Motivation Study Anglo French Textiles MBA ProjectDokumen1 halamanEmployee Motivation Study Anglo French Textiles MBA Projectsauravv7Belum ada peringkat
- A Project Report On Marketing Techniques of Ing Vysya Life Insurance HyderabadDokumen46 halamanA Project Report On Marketing Techniques of Ing Vysya Life Insurance HyderabadSumitJaiswalBelum ada peringkat
- SSC CGL 2013 Preliminary Exam Question PaperDokumen16 halamanSSC CGL 2013 Preliminary Exam Question PaperSai Bhargav VeerabathiniBelum ada peringkat
- RM 4th SemDokumen26 halamanRM 4th Semdarthvader005Belum ada peringkat
- Euro Currency MarketDokumen42 halamanEuro Currency Marketdarthvader005Belum ada peringkat
- Organisational BehaviourDokumen31 halamanOrganisational Behaviourdarthvader005Belum ada peringkat
- Student - Declaration: Bilin.E.B, East West College of ManagementDokumen4 halamanStudent - Declaration: Bilin.E.B, East West College of Managementdarthvader005Belum ada peringkat
- M&M's BPR Project Transforms BusinessDokumen18 halamanM&M's BPR Project Transforms Businessdarthvader005Belum ada peringkat
- New Microsoft Word DocumentDokumen7 halamanNew Microsoft Word Documentdarthvader005Belum ada peringkat
- Diablo 2 On Windows 7Dokumen1 halamanDiablo 2 On Windows 7darthvader005Belum ada peringkat
- Brief OverviewDokumen5 halamanBrief Overviewdarthvader005Belum ada peringkat
- MNC Eco NotesDokumen63 halamanMNC Eco Notesdarthvader005Belum ada peringkat
- Customer Service in LicDokumen62 halamanCustomer Service in Licdarthvader005Belum ada peringkat
- Arena BrochureDokumen10 halamanArena Brochuredarthvader005Belum ada peringkat
- Insurance ProjectDokumen47 halamanInsurance Projectdarthvader005Belum ada peringkat
- Indian Insurance IndustryDokumen51 halamanIndian Insurance Industrydarthvader005Belum ada peringkat
- A Project Report On Marketing Techniques of Ing Vysya Life Insurance HyderabadDokumen46 halamanA Project Report On Marketing Techniques of Ing Vysya Life Insurance HyderabadSumitJaiswalBelum ada peringkat
- HDFC Bank PDFDokumen73 halamanHDFC Bank PDFpriyadarshini100% (1)
- WT/DS135/R Interim Review SummaryDokumen72 halamanWT/DS135/R Interim Review Summarysrikanth_bhairiBelum ada peringkat
- New Microsoft Office Word DocumentDokumen46 halamanNew Microsoft Office Word Documentdarthvader005Belum ada peringkat
- HRM Recruitment Selection Processes at InfosysDokumen1 halamanHRM Recruitment Selection Processes at Infosysdarthvader005Belum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Reviewing The Ambit of Control' Apropos To The Objective of Mandatory Bids': An Analysis Under The Takeover RegulationsDokumen32 halamanReviewing The Ambit of Control' Apropos To The Objective of Mandatory Bids': An Analysis Under The Takeover Regulationsyarramsetty geethanjaliBelum ada peringkat
- DP World's Journey from Local to Global Port OperatorDokumen20 halamanDP World's Journey from Local to Global Port OperatorlucasBelum ada peringkat
- Transaction Details PayPalDokumen1 halamanTransaction Details PayPalChristine Eunice RaymondeBelum ada peringkat
- Debt Vs EquityDokumen10 halamanDebt Vs EquityKedar ParabBelum ada peringkat
- We Like Project 2019Dokumen59 halamanWe Like Project 2019Yash TrivediBelum ada peringkat
- Tutoring Business Plan ExampleDokumen23 halamanTutoring Business Plan Example24 Alvarez, Daniela Joy G.Belum ada peringkat
- Taxation II Bar Questions 2006 - 2014Dokumen42 halamanTaxation II Bar Questions 2006 - 2014Ismael NogoyBelum ada peringkat
- 300 - PEI - Jun 2019 - DigiDokumen24 halaman300 - PEI - Jun 2019 - Digimick ryanBelum ada peringkat
- Chapter Consignment For B Com Ist YrDokumen5 halamanChapter Consignment For B Com Ist YrhanumanthaiahgowdaBelum ada peringkat
- Corporate Mission: To Maximize The Value Shareholder's WealthDokumen14 halamanCorporate Mission: To Maximize The Value Shareholder's WealthCamille GrandeBelum ada peringkat
- Cost Sheet of AmulDokumen7 halamanCost Sheet of AmulKhushi DaveBelum ada peringkat
- New Heritage Doll Company Case StudyDokumen10 halamanNew Heritage Doll Company Case StudyRAJATH JBelum ada peringkat
- Stephanie Calamba and Allan Brillantes SolutionDokumen6 halamanStephanie Calamba and Allan Brillantes SolutionGerald RamiloBelum ada peringkat
- ABM - Specialized Subject: Fundamentals of Accountancy, Business and Management 1Dokumen14 halamanABM - Specialized Subject: Fundamentals of Accountancy, Business and Management 1Jupiter Whiteside100% (6)
- Financial model assumptions and key statements for opening a tea cafe in IndiaDokumen3 halamanFinancial model assumptions and key statements for opening a tea cafe in IndiaYASHASVI SHARMABelum ada peringkat
- CASH FLOW STATEMENT ANALYSISDokumen32 halamanCASH FLOW STATEMENT ANALYSISPranav MishraBelum ada peringkat
- Pertemuan 6 - Financial AnalysisDokumen35 halamanPertemuan 6 - Financial Analysisdyah ayu kusuma wardhaniBelum ada peringkat
- 101 Bir FormDokumen3 halaman101 Bir Formmijareschabelita2Belum ada peringkat
- M2U SA 128457 Jul 2023Dokumen5 halamanM2U SA 128457 Jul 2023syafiqah.mohdali38Belum ada peringkat
- A Project Report On Kotak InsuranceDokumen82 halamanA Project Report On Kotak Insurancevarun_bawa251915Belum ada peringkat
- Assessment of Effectiveness of Internal Control in Government MinistriesDokumen11 halamanAssessment of Effectiveness of Internal Control in Government MinistriesRonnie Balleras Pagal100% (1)
- CV - Ad - WebDokumen19 halamanCV - Ad - Webapi-277535292Belum ada peringkat
- Project Proposal: Ato Aniley WubieDokumen26 halamanProject Proposal: Ato Aniley Wubiedawit100% (2)
- ICAI professionals competency mappingDokumen3 halamanICAI professionals competency mappingसिद्धार्थ शुक्लाBelum ada peringkat
- Detailed StatementDokumen2 halamanDetailed Statementnisha.yusuf.infBelum ada peringkat
- A-IDEA Business Incubation TemplateDokumen6 halamanA-IDEA Business Incubation TemplatevasantsunerkarBelum ada peringkat
- Model Portfolio: DBS Group Research - EquityDokumen12 halamanModel Portfolio: DBS Group Research - EquityFunk33qBelum ada peringkat
- 2016 April ResumeDokumen2 halaman2016 April Resumeapi-308709576Belum ada peringkat
- Reliance General Insurance Company LimitedDokumen7 halamanReliance General Insurance Company LimitedJash TodiBelum ada peringkat
- CASH AND CASH EQUIVALENTS AUDITDokumen5 halamanCASH AND CASH EQUIVALENTS AUDITyna kyleneBelum ada peringkat