1 s2.0 S2210523914000348 Main PDF
Diunggah oleh
Hernan Dmgz0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
24 tayangan7 halamanRosmarinic acid, a polyphenol, ameliorates hyperglycemia by regulating the key enzymes of carbohydrate metabolism in high fat diet - STZ induced experimental diabetes mellitus. RA exhibits a wide array of benefecial and pharmacological properties including antioxidant, anti-microbial and anti-inflammatory.
Deskripsi Asli:
Judul Asli
1-s2.0-S2210523914000348-main.pdf
Hak Cipta
© © All Rights Reserved
Format Tersedia
PDF, TXT atau baca online dari Scribd
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniRosmarinic acid, a polyphenol, ameliorates hyperglycemia by regulating the key enzymes of carbohydrate metabolism in high fat diet - STZ induced experimental diabetes mellitus. RA exhibits a wide array of benefecial and pharmacological properties including antioxidant, anti-microbial and anti-inflammatory.
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PDF, TXT atau baca online dari Scribd
0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
24 tayangan7 halaman1 s2.0 S2210523914000348 Main PDF
Diunggah oleh
Hernan DmgzRosmarinic acid, a polyphenol, ameliorates hyperglycemia by regulating the key enzymes of carbohydrate metabolism in high fat diet - STZ induced experimental diabetes mellitus. RA exhibits a wide array of benefecial and pharmacological properties including antioxidant, anti-microbial and anti-inflammatory.
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PDF, TXT atau baca online dari Scribd
Anda di halaman 1dari 7
Biomedicine & Preventive Nutrition 4 (2014) 431437
Available online at
ScienceDirect
www.sciencedirect.com
Original article
Rosmarinic acid, a polyphenol, ameliorates hyperglycemia by
regulating the key enzymes of carbohydrate metabolism in high fat
diet STZ induced experimental diabetes mellitus
G. Jayanthy , S. Subramanian
Department of Biochemistry, University of Madras, Guindy Campus, 600025 Chennai, India
a r t i c l e i n f o
Article history:
Received 19 February 2014
Accepted 10 March 2014
Keywords:
Rosmarinic acid
Carbohydrate metabolizing enzymes
Insulin
Glucose
Type 2 diabetes
a b s t r a c t
Rosmarinic acid (RA) is a polyphenolic phytoconstituent found in many herbs of lamiacea species like
rosemary, mint, thyme, basil, oregano. RA exhibits a wide array of benefecial and pharmacological prop-
erties including antioxidant, anti-microbial and anti-inammatory. Oral administration of RA (100 mg/kg
body weight) to high fat diet fed low doses of STZ induced type 2 diabetic rats for 30days established
a signicant (P <0.05) decline in the levels of blood glucose, glycosylated hemoglobin, blood urea, serum
uric acid and creatinine along with increase in plasma insulin level. Diminished activities of hepatospe-
cic pathophysiological enzymes such as aspartate transaminase (AST), alanine transaminase (ALT) and
alkaline phosphatase (ALP) were observed in diabetic rats administered with RA. Further, the altered
activities of key carbohydrate metabolizing enzymes such as hexokinase, pyruvate kinase, glucose-6-
phosphatase, fructose 1,6-bisphosphatase, glucose-6-phosphate dehydrogenase, glycogen synthase and
glycogen phosphorylase (P <0.05) in the liver tissue of diabetic rats were signicantly reverted to near
normal levels upon treatment with RA. Also, RA administration to diabetic rats improved hepatic glyco-
gen content suggesting the anti-hyperglycemic potential of RA in diabetic animals. The obtained results
were compared with metformin, a standard oral hypoglycemic drug. Thus, the present ndings indicate
that RA is nontoxic and it can potentially maintain glycemic control and regulate the key enzymes of
carbohydrate metabolism in experimental diabetic rats.
2014 Elsevier Masson SAS. All rights reserved.
1. Introduction
Diabetes mellitus encompasses a heterogeneous group of
metabolic disorders characterized by altered glucose and lipid
metabolismresulting in persistent hyperglycaemia. The incidence
of diabetes mellitus is increasing globally and is speculated that
about 552 million people would be affected worldwide by the year
2030 [1] of which the developing countries contribute more to
this increase. Hyperglycaemia is often preceded by insulin resis-
tance, which plays a key role in the development of type 2 diabetes
(T2D) since insulin facilitates the uptake of glucose especially in
muscle. Marked dysregulation of glucose and lipid metabolism
and a rise in fasting and postprandial glucose and lipid levels
are the consequences of insulin resistance or deciency of insulin
[2].
Highfat diet inducedinsulinresistance model is the most widely
used experimental model and is shown to impair carbohydrate
Corresponding author. Tel.: +91 9443026668.
E-mail address: subbus2020@yahoo.co.in (S. Subramanian).
metabolism, increase hepatic glucose production and decrease
insulin sensitivity which is the main feature of type 2 diabetes [3].
On the other hand, streptozotocin (STZ) is being currently used to
induce both type 1 and type 2 diabetes mellitus by inducing -
cell death through alkylation of DNA. A high dose of STZ strongly
impairs insulin secretion mimicking type 1 diabetes whereas a low
dose STZ has been shown to induce a mild impairment of insulin
secretionwhichresembles theclinical features similar totype2dia-
betes [4]. Therefore, in the present study a combination of high fat
diet and low dose STZ has been employed to induce experimental
diabetes in rats [57].
Based on the current understanding of the pathophysio-
logy of type 2 diabetes, multiple pharmacological and non-
pharmacological therapies are being recently developed with the
aim of improving glycaemic control and prevention of diabetic
complications. However, most of the synthetic antidiabetic drugs
available in the market fail to maintain glycaemic control for a pro-
longed time and are accompanied by various side effects [8]. Thus,
in the recent days use of functional foods and their bioactive com-
ponents are being considered as a newapproach in the prevention
and management of diabetes and its complications [9].
http://dx.doi.org/10.1016/j.bionut.2014.03.006
2210-5239/ 2014 Elsevier Masson SAS. All rights reserved.
432 G. Jayanthy, S. Subramanian / Biomedicine & Preventive Nutrition 4 (2014) 431437
Fig. 1. Structure of Rosmarinic acid.
Plant based active components have a better complimentary
potential to act against a number of free radical mediated diseases
such as cancer and diabetes. Among those, polyphenols appear to
be appropriate nutraceuticals andsupplementarytreatment option
for various aspects of diabetes mellitus due to their biological
properties. Phenolic acids constitute about one third of the total
polyphenolic component in the diet and is categorized to two main
classes, hydroxybenzoic acidderivatives andhydroxycinnamic acid
derivatives.
Rosmarinic acid ((2R)-2-[[(2E)-3-(3,4-dihydroxyphenyl)-1-
oxo-2-propenyl]]oxy]]-3-(3,4-dihydroxyphenyl)propanoic acid)
(Fig. 1), a natural phenol carboxylic acid, is a secondary metabolite
predominantly found in many lamiaceae herbs used for culinary
purpose such as lemon balm, rosemary, oregano, thyme, pepper
mint, etc. [10]. RA belongs to the family of hydroxyl cinnamic
acids and is an ester of 3,4-dihydroxyphenyllactic acid and caffeic
acid [11]. Apart from RA being a potent antioxidant, it has a large
number of other biological activities such as anti-viral, antibac-
terial and anti-inammatory properties and it could also prevent
-amyloid aggregation [12]. In the absence of systemic reports in
the literature on the role of RA in ameliorating insulin resistance in
high fat-fed condition, the present study is aimed to establish the
hypoglycaemic as well as insulin sensitizing effects of Rosmarinic
acid in high fat diet and low dose STZ induced experimental type
2 diabetes, in rats.
2. Materials and methods
2.1. Chemicals
Rosmarinic acid, streptozotocin, EDTA were procured from
Sigma Chemicals Co., St. Louis, MO, USA, stored at 24
C and pro-
tected from light. All other chemicals used were purchased from
standardcommercial suppliers andwereof analytical gradequality.
2.2. Animals
Male albino Wistar rats weighing 150170g were purchased
fromTamilnaduVeterinary andAnimal Sciences University (TANU-
VAS), Chennai. The rats were housed in polypropylene cages lined
with husk. They were maintained at an ambient temperature of
252
C and 12/12h of light/dark cycle. Animals were fed with
standard commercial rat chow (Hindustan Lever Ltd.) and water
ad libitum and housed under standard environmental conditions
throughout the study. The experiments were strictly conducted
according to the ethical norms approved by the Ministry of Social
Justices and Empowerment, Government of India and Institutional
Animal Ethics Committee Guidelines (IAEC No. 01/01/2013).
2.3. Experimental induction and diet
The rats were divided into two dietary regimens by feeding
either normal or high fat diet (HFD) for the initial period of 2weeks
[7]. After 2weeks of dietary manipulation, the groups of rats fed
with HFD was injected intra-peritoneally (IP) with a low dose of
STZ (35mg/kg b.w.) dissolved in 0.1Mcold citrate buffer (pH 4.5).
One week after STZ injection, the rats were screened for blood glu-
cose level. Rats having fasting blood glucose (FBG) >250mg/dL that
exhibitedrandomhyperglycaemia andglycosuria were selectedfor
the experiment. The rats were allowed to continue to feed on their
respective diets until the end of the experiments.
2.4. Toxicity and dosage xation studies
The acute toxicity of Rosmarinic acid was studied in the control
rats according to OECD guideline 423. Different doses of RA dis-
solved in water were given orally and the animals were observed
continuously for the rst 2hours followed by every hour up to
6hours and daily thereafter for 14days for any signs of morbidity,
mortality and behavioural toxicity. RA was found to be nontoxic up
to 2g/kg b.w.
Gradeddoses of RA(100, 150, 200mg/kgb.w.) was administered
to HFD+STZ induced diabetic rats for various periods of treat-
ment. From the data obtained, the optimum dosage was xed as
100mg/kg b.w. for 30days. The animals were divided into four
groups, comprising a minimum of six animals in each group as
follows:
group 1 control rats fed with normal pellet;
group 2 HFD+STZ (i.p. 35mg/kg b.w.) induced rats;
group 3 RA (administered orally 100mg/kg b.w.) treated dia-
betic rats;
group 4 diabetic rats treated with metformin (200mg/kg
b.w./day) in aqueous solution orally for 30days.
Table 1
Effect of Rosmarinic acid (RA) on the body weight, water intake and food intake in the experimental groups of rats after 30days experimental period.
Groups Body weight (g) Water intake (mL/rat/day) Food intake (g/rat/day)
Initial Final Initial Final Initial Final
Control 173.20 5.54 221.30 10.4 28.56 2.22 32.03 1.63 23.52 1.37 28.70 1.39
Diabetic 165.30 9.59
a
147.30 8.21
a
60.43 4.89
a
72.65 4.50
a
39.24 2.51
a
57.02 4.50
a
Diabetic +RA 170.60 7.44
b
187.10 9.16
b
62.54 3.25
b
37.45 4.19
b
37.40 2.05
b
31.38 1.44
b
Diabetic +Metformin 174.24 5.89
b
196.22 8.35
b
60.22 2.77
b
35.56 2.98
b
39.10 2.38
b
39.13 1.68
b
Values are given as meanS.D. for groups of six rats in each. One-way ANOVA followed by post hoc test LSD. Statistical signicance was compared within the groups as
follows.
a
Denotes signicant difference in comparing with control at P<0.05.
b
Denotes signicant difference in comparing with diabetic at P<0.05.
G. Jayanthy, S. Subramanian / Biomedicine & Preventive Nutrition 4 (2014) 431437 433
At the end of the treatment period, the rats were fasted
overnight, anesthetized and sacriced by cervical decapitation. The
blood was collected with and without anticoagulants for plasma
and serum separation, respectively. The liver tissue was dissected
out, washed in ice-cold saline, and weighed. Tissue was minced
and homogenized (10%, w/v) with 0.1M TrisHCl buffer (pH 7.4)
and centrifuged (3000 g for 10min). The resulting supernatant
was immediately used for various biochemical investigations.
2.5. Oral glucose tolerance test
On the day prior to sacrice, oral glucose tolerance test (OGTT)
test was performed in all the groups. Blood samples were obtained
from the lateral tail vein of rats deprived of food overnight. Suc-
cessive blood sample was taken at 0, 30, 60, 90 and 120minutes
following the administration of 2mg/kg b.w. of glucose solution
[13].
2.6. Determination of glucose, insulin and glycosylated
haemoglobin
Blood glucose determination was done by the method of Sasaki
et al. [14]. Glycosylated haemoglobin in plasma was assayed
with the help of kit procured from SPAN diagnostics Ltd., Surat.
Plasma insulin level was determined using the sensitive rat insulin
radioimmunoassay kit (Linco Research, Inc., St. Charles, MO).
2.7. Determination of urea, uric acid, createnine and urine sugar
Whole blood urea estimation was carried out by the method
described by Natelson et al. [15]. The Serum uric acid and creati-
nine levels was assayed by the methods of Caraway [16] and Brod
and Sirota [17], respectively. Urine sugar was detected using urine
strips.
2.8. Determination of homeostasis model of insulin assessment
As the insulin abnormality cannot be accurately detected by a
single determination of insulin or glucose levels, the insulin resis-
tance was evaluated by homeostasis model assessment of insulin
resistance (HOMA-IR) [18] as follows
HOMA-IR = Fasting insulin level (U/mL)
Fasting blood glugose (mmol/L) /22.5
2.9. Assay of marker enzymes AST, ALT and ALP
Levels of aspartate transaminase (AST), alanine transaminase
(ALT) and alkaline phosphatise (ALP) were assayed by the method
of King [19,20].
2.10. Analysis of carbohydrate metabolising enzymes
The supernatant obtained from the centrifugation of the liver
homogenate was used as enzyme source for the assays of hex-
okinase [21], pyruvate kinase [22], lactate dehydrogenase [23],
glucose-6-phosphatase [24], fructose-1,6-bisphosphatase [25],
glucose-6-phosphate dehydrogenase [26], glycogen synthase [27],
glycogen phosphorylase [28]. Glycogen content in the liver tissue
was assayed by the method of Morales et al. [29].
2.11. Statistical analysis
The results were expressed as meanS.D. of six rats per group
and statistical signicance was evaluated by one-way analysis of
Fig. 2. Effect of Rosmarinic acid on oral glucose tolerance test in the experimental
group of rats. Values are expressed as meanS.D.
variance (ANOVA) using SPSS (version 11.5) program followed by
LSD. Values were considered statistically signicant when P<0.05.
3. Results
3.1. Effect of RA on changes in the body weight, food intake and
water intake
Thechanges inbodyweight, foodandwater intakeof control and
experimental rats are represented in Table 1. Asignicant (P<0.05)
decrease in body weight was observed in diabetic rats as compared
with control rats, whereas there was an elevation in the food and
water intake inthe diabetic rats. Onthe other hand the diabetic rats
treated with RA as well as metformin showed signicant (P<0.05)
increase in body weight and decrease in food and water intake as
compared with diabetic rats.
3.2. Oral glucose tolerance test
OGTT of diabetic rats showed a highly pronounced elevation at
fasting state and at 30, 60, 90 and 120minutes after oral glucose
intake as compared with control rats. The administration of RA as
well as metformintodiabetic rats showeda potential improvement
of elevated values at all points of OGTT curve (Fig. 2).
3.3. Effect of RA on levels of blood glucose, insulin, glycosylated
haemoglobin
Table 2 depicts the levels of blood glucose, plasma insulin and
HbA
1C
in control and experimental groups of rats. There was a
signicant (P<0.05) increase in blood glucose and HbA
1C
during
diabetes, while the plasma insulin level was decreased when com-
pared with the control group of rats. Upon oral administration of
Table 2
Effect of Rosmarinic acid (RA) on the levels of blood glucose, plasma insulin and
glycosylated haemoglobin (HbA
1C
) in the experimental groups of rats after 30days
experimental period.
Groups Blood glucose
(mg/dL)
Insulin
(U/mL)
HbA
1C
(%Hb)
Control 90 5.04 14.82 0.81 7.10 0.19
Diabetic 272 30.7
a
5.02 0.41
a
14.19 0.87
a
Diabetic +RA 102 8.5
b
9.95 0.92
b
8.25 0.42
b
Diabetic +Metformin 88 3.8
b
13.11 0.55
b
7.54 0.25
b
Values are given as meanS.D. for groups of six rats in each. One-way ANOVA
followed by post hoc test LSD was used for statistical analysis.
a
Denotes signicant difference in comparing with control at P<0.05.
b
Denotes signicant difference in comparing with control at P<0.05.
434 G. Jayanthy, S. Subramanian / Biomedicine & Preventive Nutrition 4 (2014) 431437
Table 3
Effect of Rosmarinic acid (RA) on the levels of urea, uric acid, creatinine and urine in the experimental groups of rats after 30days experimental period.
Groups Urea (mg/dL) Uric acid (mg/dL) Creatinine (mg/dL) Urine sugar
Control 29.15 1.63 2.92 0.24 0.65 0.05 Nil
Diabetic 51.54 6.80
a
6.11 0.65
a
2.10 0.46
a
+++
Diabetic +RA 34.75 2.49
b
4.03 0.37
b
0.78 0.08
b
Nil
Diabetic +Metformin 27.63 1.29
b
3.19 0.24
b
0.80 0.08
b
Nil
Values are given as meanS.D. for groups of six rats in each. One-way ANOVA followed by post hoc test LSD was used for statistical analysis.
a
Denotes signicant difference in comparing with control at P<0.05.
b
Denotes signicant difference in comparing with control at P<0.05.
RA and metformin, the levels of blood glucose and HbA
1C
were
decreased with an improvement in plasma insulin level.
3.4. Effect of RA on levels of urea, uric acid, creatinine and urine
sugar
The levels of urea, uric acid, creatinine and urine sugar are illus-
trated in Table 3. The induced diabetic rats also showed signicant
(P<0.05) increase in the urea, uric acid and createnine levels as
compared with control rats and presence of urine sugar. However,
treatment with RA signicantly decreased the levels of urea, uric
acid and creatinine as compared with HFD-STZ induced rats. Urine
sugar present in diabetic rats was found to be drastically reduced
in the rats treated with RA and metformin.
3.5. Effect of RA on insulin resistance
HOMA-IR values of the experimental group of rats are depicted
on Fig. 3. Diabetic rats showed a signicant (P<0.01) elevation of
HOMA-IR and it was decreased signicantly upon administration
of RA and metformin.
3.6. Effect of RA on levels of AST, ALT and ALP
The activities of serum AST, ALT and ALP in control and exper-
imental rats are represented on Fig. 4. The activities of AST, ALT
and ALP were signicantly (P<0.05) increased in HFD-STZ induced
Fig. 3. Effect of Rosmarinic acid on the insulin sensitivity in the experimental group
of rats. Values are expressed as meanS.D.
a*
denotes signicant difference in com-
paring with control at P<0.05.
b*
denotes signicant difference in comparing with
diabetic at P<0.05.
Fig. 4. Effect of Rosmarinic acid on the activities of aspartate transaminase (AST),
alanine transaminase (ALT) and alkaline phosphatase (ALP) on the experimental
groups of rats. Enzyme activity is expressed as: AST and ALT moles of pyru-
vate/h/mg of protein; ALP moles of phenol liberated/min/mg of protein. Results
are expressed as meanS.D.
a*
denotes signicant difference in comparing with
control at P<0.05.
b*
denotes signicant difference in comparing with diabetic at
P <0.05.
diabetic rats. These values were altered signicantly upon treat-
ment with RA as compared to HFD-STZ induced rats.
3.7. Effect of RA on activity of carbohydrate metabolising enzymes
Tables 4 and 5 project the effect of RA supplementation on
the carbohydrate metabolizing enzymes in the liver of control and
experimental group of rats. The activities of hexokinase, pyruvate
kinase and glucose-6-phosphate dehydrogenase were signicantly
(P<0.05) decreased whereas, the activities of lactate dehydro-
genase, glucose-6-phosphatase and fructose-6-phosphatase were
signicantly (P<0.05) increased in diabetic rats when compared to
normal control rats. However, upon treatment with RA to diabetic
rats reversed the activities of these hepatic enzymes to normalcy
similar to metformin treated rats.
Table 4
Effect of Rosmarinic acid (RA) on the levels of hexokinase, pyruvate kinase and lac-
tate dehydrogenase in the experimental groups of rats after 30days experimental
period.
Groups Hexokinase Pyruvate
kinase
Lactate
dehydrogenase
Control 257.23 10.03 214.76 17.61 220.39 14.54
Diabetic 136.54 12.88
a
126.84 17.89
a
478.13 63.73
a
Diabetic +RA 204.93 17.41
b
184.22 19.47
b
305.11 24.10
b
Diabetic +Metformin 221.52 11.51
b
192.02 14.09
b
293.82 17.54
b
Units are expressed as: mol of glucose-6-phosphate formed/h/mg of protein for
hexokinase, mU/mg of protein for pyruvate kinase, mol of pyruvate formed/h/mg
of proteinfor lactatedehydrogenase. Values aregivenas meanS.D. for groups of six
rats in each. One-way ANOVA followed by post hoc test LSD was used for statistical
analysis.
a
Denotes signicant difference in comparing with control at P<0.05.
b
Denotes signicant difference in comparing with control at P<0.05.
G. Jayanthy, S. Subramanian / Biomedicine & Preventive Nutrition 4 (2014) 431437 435
Table 5
Effect of Rosmarinic acid (RA) on the levels of glucose-6-phosphatase, fructose-1, 6-biphosphatase and glucose-6-phosphate dehydrogenase in the experimental groups of
rats after 30days experimental period.
Groups Glucose-6-phosphatase Fructose-1, 6-biphosphatase Glucose-6-phosphate dehydrogenase
Control 1042.27 27.03 463.27 24.73 511.19 21.31
Diabetic 1993.76 177.44
a
821.62 91.37
a
262.54 18.69
a
Diabetic +RA 1242.58 74.80
b
508.11 40.08
b
383.29 24.18
b
Diabetic +Metformin 1151.62 53.08
b
520.53 29.25
b
425.01 20.95
b
Units are expressed as: mol of Pi liberated/h/mg of protein for glucose-6-phosphatase and fructose-1, 6-bisphosphatase and mol of NADPH/min/mg of protein for
glucose-6-phosphate dehydrogenase. Values are given as meanS.D. for groups of six rats in each. One-way ANOVA followed by post hoc test LSD was used for statistical
analysis.
a
Denotes signicant difference in comparing with control at P<0.05.
b
Denotes signicant difference in comparing with control at P<0.05.
3.8. Effect of RA on levels of glycogen and activities of glycogen
synthase and glycogen phosphorylase in liver
Status of glycogen metabolismin the liver of control and exper-
imental group of rats is shown in Table 6. A signicant (P<0.05)
decline inthe glycogencontent, decreasedglycogensynthase activ-
ity, as well as a concomitant increase in the activity of glycogen
phosphorylase was observed in the liver of HFD-STZ induced dia-
betic rats as compared with control rats. Oral treatment with RA
as well as metformin to diabetic rats reinstated the glycogen levels
andthe activities of glycogensynthase andglycogenphosphorylase
were signicantly improved as compared with HFD-STZ induced
rats.
4. Discussion
Type 2 diabetes is one of the most commonchronic andprogres-
sive diseases and is a consequence of number of defects including
impaired insulin secretion by the pancreatic cells, resistance of
peripheral tissues to the effect of insulin and augmented hepatic
glucose production[30]. T2Dposes a major challenge to healthcare
systems around the globe due to its increased incidence and preva-
lence. It also imposes economic burden to the patients as it causes
signicant morbidityandmortalityat escalatingexpenses [31]. Due
to the lopsided features of the conventional therapies for diabetes,
interest on exploring natural remedy is at the peak. Although there
is only meagre biological knowledge on the mode of action in the
treatment of diabetes by plants, their secondary metabolites like
glycosides, avonoids, phenolic acids, etc. are implicatedto possess
antidiabetic effects [32,33]. This study elucidates the antidiabetic
efcacy of RA by evaluating various biological parameters highly
pronounced during diabetes.
Table 6
Effect of Rosmarinic acid(RA) onthelevels of glycogen, glycogensynthaseandglyco-
gen phosphorylase in the experimental groups of rats after 30days of experimental
period.
Groups Glycogen Glycogen
synthase
Glycogen
phosphorylase
Control 62.19 3.76 809.44 32.13 612.39 16.77
Diabetic 25.22 4.10
a
520.17 33.60
a
869.92 60.72
a
Diabetic +RA 46.01 5.58
b
718.82 37.16
b
671.11 34.02
b
Diabetic +Metformin 49.72 3.92
b
738.31 31.52
b
684.78 21.77
b
Units are expressed as: mg/g wet tissue for glycogen, mol of UDP formed/h/mg
proteinfor glycogensynthaseandmol Pi liberated/h/mgproteinfor glycogenphos-
phorylase. Values are given as meanS.D. for groups of six rats in each. One-way
ANOVA followed by post hoc test LSD was used for statistical analysis.
a
Denotes signicant difference in comparing with control at P<0.05.
b
Denotes signicant difference in comparing with control at P<0.05.
As high fat feeding would cause only insulin resistance, which is
a key feature of T2Dbut not overt hyperglycaemia or diabetes, STZ a
well-known diabetogenic agent is used at lowdose in combination
with high fat diet for efcient induction of T2D[8]. This method has
been widely used in recent years for understanding mechanistic
insights in T2D and for therapeutic studies [34,35]. In the present
study, HFD-STZ induced diabetic rats showed signs of weight loss,
polyuria, polydipsia and polyphagia. Loss of body weight denotes
fat and protein catabolismdue to altered glucose homeostasis, and
polyuria denotes osmotic diuresis as a result of hyperglycemia in
HFD-STZ induced rats [36]. Oral administration of RA prevented
the body weight loss, reduced the food and water consumption in
diabetic rats indicating the improved glycaemic control.
OGTT is the most common and more sensitive test measure
for early abnormalities in glucose regulation than fasting plasma
glucose or HbA
1C
[37]. Intriguingly, glucose tolerance of HFD-STZ
induced rats was signicantly reduced and remained high even
after 120min of glucose loading. In contrast, in RA treated dia-
betic rats the blood glucose levels reached a peak and declined to
fasting levels after 120min. Impaired glucose tolerance reects the
hepatic gluconeogenesis and reduced uptake of glucose fromblood
by insulin dependent tissues [38].
Blood glucose control is an important component in delay-
ing or preventing acute or long-term diabetic complications. Oral
administrationof RAto diabetic rats reduces the bloodglucose con-
centrations without causing hypoglycaemic state, probably due to
insulin secretion from surviving beta cells. Though insulin resis-
tance is the initiating pathogenic factor in T2D, -cell failure is
accountable for insulin deciency and impaired glucose tolerance
to overt T2D [39]. In the present study, an observed low level of
plasma insulin in HFD-STZ induced rats denotes perturbations in
-cell function, whereas RA treated rats showed increased plasma
insulin levels, indicating that RA treatment improved -cell func-
tion in diabetic rats. Furthermore, the degree of hyperinsulinemia
and insulin resistance was substantiated from HOMA-IR where
HFD-STZ rats showed signicant higher HOMA-IR values. A pro-
nounced reduction in the HOMA-IR indices of RA treated rats
showed the efcacy of RA in restoring insulin sensitivity. The non-
enzymatic, irreversible covalent bonding of excessive glucose with
Hb in circulation results in the formation of HbA
1C
which is a
critical parameter for assessing long-term glycaemic control and
predicting the incidence of diabetic complications [40]. A signif-
icant increase in level of HbA
1C
indicates poor glycaemic control
in HFD-STZ administered rats. Oral administration of RA decreased
thelevels of HbA
1C
indicatingthat thereis areducednon-enzymatic
glycation of proteins.
Levels of urea, uric acid and creatinine are the key indices in the
hyperglycaemia mediated renal dysfunction [41]. In the present
investigation a signicant elevation in the levels of urea, uric acid
and creatinine was seen in HFD-STZ induced diabetic rats. Oral
treatment with RA reversed the levels to near normalcy denoting
436 G. Jayanthy, S. Subramanian / Biomedicine & Preventive Nutrition 4 (2014) 431437
that it antagonises metabolic complications like diabetic nephropa-
thy.
AST, ALT and ALP serve as the pathophysiological markers for
tissue damage. In this study, signicant increase in the activi-
ties of serum transaminases in HFD-STZ rats elucidates perturbed
homeostasis in high metabolic organs [42]. ALT is a gluconeogenic
enzyme and its increase in diabetic rats is an indicator of impaired
insulin signalling [43]. The activity of ALP is also increased in dia-
betic rats due to an increased oxidative insult of diabetes leading to
hepatic damage [44]. Treatment with RA diminished transminase
activities and restored ALP levels to near normalcy, denoting RA
enhances glucose and insulin metabolismin diabetic rats.
Liver is the primary site of endogenous glucose production
via gluconeogenesis or glycogenolysis, which are the two primary
complementary events balancing the glucose load in our body [45].
Derangement in these two events in concurrence with deprived
pancreatic function and reduced glucose clearance contributes to
a disarray of glucose metabolismleading to elevated systemic glu-
cose [46]. Insulin prevents hyperglycaemia, in part, by suppressing
hepatic gluconeogenesis andglycogenolysis andfacilitatinghepatic
glycogensynthesis. Hexokinase phosphorylates glucose toglucose-
6-phosphate and serves as glucose sensor of insulin producing
pancreatic -cells and regulates glycogen synthesis, hepatic glu-
cose production [47] and their levels are low in both human and
rodent diabetes. The markedly decreased level of insulin observed
in the HFD-STZ induced diabetic animals ultimately leads to the
impairment in the activity of hexokinase, since insulin deciency
is a clinical hallmark of diabetes [48]. However, a modest increase
in the hexokinase activity is seen in diabetic rats administered with
RA.
Pyruvate kinase (PK) is a ubiquitously expressed, rate con-
trolling, key glycolytic enzyme that catalyses the conversion of
phosphoenol pyruvate to pyruvate with the release of ATP. The
decrease in PK levels in diabetic condition alters the glucose
metabolismand ATP production, which might be promptly respon-
sible for the reducedglycolysis andampliedgluconeogenesis [49].
Oral administration of RA to the diabetic rats showed a notable
increase in the PK activity. Lactate dehydrogenase (LDH) is a ter-
minal glycolytic enzyme which facilitates the inter-conversion of
pyruvate to lactate to yield energy under anaerobic conditions [50].
LDH activity is altered by glucose, insulin and NADH. Elevated lev-
els of LDH is observed in experimental diabetic animals which is
attributed to impaired glucose-stimulated insulin secretion [51].
Thus, the normal glucose metabolism and insulin secretion in the
beta cells are perturbed with the increased activity of LDH and it
therefore may be directly responsible for insulin secretory defects
in diabetes. Oral administration of RA as well as metformin to dia-
betic groups of rats showed a signicant reduction in the LDH
activity, probably due to the regulation of NAD
+
/NADHratio by the
oxidation of glucose.
Glucose-6-phosphatase is a crucial gluconeogenic enzyme in
the homeostatic regulation of blood glucose and is critical in
providing glucose to other organs during diabetes, prolonged
fasting or starvation [52]. The activity of glucose-6-phosphatase
is repressed by insulin and its diminished activity leads to
severe metabolic disorders mainly characterised by hypogly-
caemia. Insulin deciency achieved in experimental diabetic rats
enhances glucose-6-phosphatase activity, which in turn increases
the blood glucose levels. Fructose-1, 6-bisphosphatase is another
gluconeogenic enzyme that the dephosphorylation of fructose-1,6-
bisphosphate to fructose-6-phosphate, the second to nal step in
the gluconeogenic pathway and appears as a target for efcient and
safe glycaemic control in diabetes [53]. The activities of glucose-
6-phosphatase and fructose-1, 6-bisphosphatase are increased in
the hepatic tissues of HFD-STZ induced diabetic rats. Activation
of these gluconeogenic enzymes is due to the state of insulin
deciency and availability in surplus of gluconeogenic substrates
[54]. In our study, oral administration of RA diminishes the activi-
ties of glucose-6-phosphatase and fructose-1, 6-bisphosphatase in
HFD-STZ induced diabetic rats. The reduction in the activities of
glucose-6-phosphatase and fructose-1, 6-bisphosphatase can lead
to decreased gluconeogenesis and thereby reducing the endoge-
nous production of glucose.
Glucose-6-phosphate dehydrogenase is the rst and rate-
limiting enzyme in the pentose phosphate pathway, which results
intheproductionof ribose-5-phosphateandNADPH[55]. Theactiv-
ity of glucose-6-phosphate dehydrogenase is foundto be decreased
in diabetic conditions [56]. Oral administration of RA to HFD-STZ
induced diabetic rats signicantly increased the activity of glucose-
6-phosphate dehydrogenase.
Glycogen, a branched polymer of glucose residues synthesized
by the enzyme glycogen synthase, is the primary intracellular
storable form of glucose and its quantity in various tissues is a
direct manifestation of insulin activity [57]. Glycogen synthase,
a crucial and rate-limiting enzyme in tissues non-oxidative glu-
cose disposal, catalyzes the transfer of glucose from UDP-glucose
toglycogeninanimal cells. Glycogenphosphorylase, a rate-limiting
enzyme of glycogenolysis, cleaves (14) linkages to remove glu-
cose molecules from the glycogen. Since there is a decreased
secretion of insulin in HFD-STZ induced diabetic state, there is a
decrease in the glycogen levels, glycogen synthase activity and
responsiveness to insulin signalling are diminished and glyco-
gen phosphorylase activity is signicantly increased [58]. The oral
administration of RAto diabetic rats regulated the activity of glyco-
gen metabolizing enzymes by stimulating the remnant beta cells to
secrete more insulin and there by normalized the altered glycogen
content in skeletal muscle and liver.
5. Conclusion
Collectively, the results of present ndings demonstrate that
RA is nontoxic and exhibits antidiabetic effect during HFD-STZ
induced experimental diabetes in vivo. The results obtained in
this study points to the therapeutic potential of RA, which can
be clinically utilized for various diabetic complications. How-
ever, further studies are in progress to understand the plausible
mechanismby which RA antagonizes hyperglycemia, and provides
insulin secreting/sensitizing activity during HFD-STZ induced T2D
in experimental rats.
Disclosure of interest
The authors declare that they have no conicts of interest con-
cerning this article.
Acknowledgements
The research fellowship (UGC-BSR) of the University
Grants Commission (UGC) (grant number: GCCO/A-2/UGC-
MERITORIOUS/2013/214 dated 10.05.2013), New Delhi, India, to
Mrs. G. Jayanthy is gratefully acknowledged.
References
[1] Whiting DR, Guariguanta L, Weil C, Shaw JE. Diabetes atlas: global estimates
of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract
2011;94:31121.
[2] Saltiel AR, Kahn CR. Insulin signalling and the regulation of glucose and lipid
metabolism. Nature 2001;414:799806.
[3] Henriksen EJ, Teachey MK, Lindborg KA, Diehl CJ, Beneze AN. The high fat-fed
lean Zucker rat: a spontaneous isocaloric model of fat-induced insulin resis-
tance associated with muscleGSK-3 overactivity. Am J Physiol Regul Integr
Comp Physiol 2008;294:181321.
G. Jayanthy, S. Subramanian / Biomedicine & Preventive Nutrition 4 (2014) 431437 437
[4] Szkudelski T. The mechanismof alloxan and streptozotocin action in B cells of
the rat pancreas. Physiol Res 2001;50:53746.
[5] Reed MJ, Meszaros K, Entes LJ. A newrat model of type 2 diabetes: the fat-fed,
streptozotocin-treated rat. Metabolism2000;49(11):13904.
[6] Sahin K, Onderci M, Tuzcu M. Effect of chromium on carbohydrate and
lipid metabolism in a rat model of type 2 diabetes mellitus: the fat-fed,
streptozotocin-treated rat. Metabolism2007;56:123340.
[7] Srinivasan K, Viswanad B, Asrat L, Kaul CL, Ramarao P. Combination of high fat
diet fed and low dose streptozotocin-treated rat: a model for type 2 diabetes
and pharmacological screening. Pharmacol Res 2005;52:31320.
[8] Li PB, Lin WL, Wang YG, Peng W, Cai XY, Su WW. Antidiabetic activities of
oligosaccharides of Ophiopogonis japonicus in experimental type 2 diabetic
rats. IntJ Bio Macromol 2012;51:74955.
[9] Eshak ES, Iso H, Mizoue T, Inoue M, Noda M, Tsugane S. Soft drink, 100%
fruit juice, and vegetable juice intakes and risk of diabetes mellitus. Clin Nutr
2013;32(2):3008.
[10] Clifford MN. Chlorogenic acids and other cinnamates. Nature, occurrence and
dietary burden. J Sci Food Agric 1999;79:36272.
[11] Petersen M, Simmonds MS. Rosmarinic acid. Phytochemistry 2003;62:1215.
[12] Hamaguchi T, Ono K, Murase A, Yamada M. Phenolic compounds prevent
Alzheimers pathology through different effects on the amyloid-beta aggre-
gation pathway. AmJ Pathol 2009;175:255765.
[13] Joy KL, Kuttan R. Antidiabetic activity of Picrorrhiza kurrora extract. J
Ethnopharmacol 1999;167:1438.
[14] Sasaki T, Matsy S, Sonae A. Effect of acetic acid concentration on the colour
reaction in the O-toludiene boric acid method for the blood glucose estimation.
Risnh Kagaku 1972;1:34653.
[15] Natelson S, Scott ML, Beffa C. A rapid method for the estimation of urea in
biologic uids. AmJ Clin Pathol 1951;21(3):27581.
[16] Caraway WT. Determination of uric acid in serumby a carbonate method. Am
J Clin Pathol 1955;25(7):8405.
[17] Brod J, Sirota JH. The renal clearance of endogenous createnine in man. J Clin
Invest 1948;27(5):64554.
[18] Matthews D, Hosker J, Rudenski A, Naylor B, Treacher D, Turner R. Homeostasis
model assessment: insulinresistanceandbetacell functionfromfastingplasma
glucose and insulin concentrations in man. Diabetologia 1985;28:4129.
[19] King J. The transaminases: alanine and aspartate transaminases. In: Van D,
editor. Practical clinical enzymology. London: Nostrand Co.; 1965. p. 36395.
[20] King J. The hydrolases-acid and alkaline phosphatases. In: Van D, editor. Prac-
tical clinical enzymology. London: Nostrand Co.; 1965. p. 199208.
[21] Brandstrup N, Kirk JE, Bruni C. The hexokinase and phosphoglucoisomerase
activities of aortic and pulmonary artery tissue in individuals of various ages. J
Gerontol 1957;12:16671.
[22] Pogson CI, Denton RM. Effect of alloxan diabetes, starvation and refeed-
ing on glycolytic kinase activities in rat epididymal adipose tissue. Nature
1967;216:1567.
[23] King J. A routine method for the estimation of lactic dehydrogenase activity. J
Med Lab Technol 1959;16:26572.
[24] Koide H, Oda T. Pathological occurrence of glucose-6-phosphatase in serumin
liver diseases. Clin ChimActa 1959;4:55461.
[25] Gancedo JM, Gancedo C. Fructose-1, 6-diphosphatase, phosphofructokinase
andglucose-6-phosphate dehydrogenase fromfermenting andnonfermenting
yeasts. Arch Mikrobiol 1971;76:1328.
[26] Ells HA, Kirkman HN. A colorimetric method for assay of erythrocytic glucose-
6-phosphate dehydrogenase. Proc Soc Exp Biol Med 1961;106:6079.
[27] Leloir LF, Goldemberg SH. Glycogen synthetase from rat liver: (Glucose)n+
(UDPG)(Glucose)n+1+UDP. In: Colowick SP, Kalpan NO, editors. Methods in
enzymology. NewYork: Academic Press; 1962. p. 1457.
[28] Cornblath M, Randle PJ, Parmeggiani A, Morgan HE. Regulation of glycogenol-
ysis in muscle. Effects of glucagon and anoxia on lactate production, glycogen
content, and phosphorylase activity in the perfused isolated rat heart. J Biol
Chem1963;238:15927.
[29] Morales MA, Jabbagy AJ, Terenizi HR. Mutations affecting accumulation of
glycogen. Neurospora News 1973;20:245.
[30] Shulman GI. Cellular mechanisms of insulin resistance. J Clin Invest
2000;106:1716.
[31] Shah BR, Hux JE, Laupacis A, Zinman B, van Walraven C. Clinical inertia in
response to inadequate glycemic control: do specialists differ from primary
care physicians? Diabetes Care 2005;28:6006.
[32] Loew D, Kaszkin M. Approaching the problem of bioequivalence of herbal
medicinal products. Phytother Res 2002;16:70511.
[33] Jaiswal D, Rai PK, Watal G. Antidiabetic effect of withania coagulans in experi-
mental rats. Indian J Clin Biochem2009;24:8893.
[34] Epp RA, Susser SE, Morissettee MP, Kehler DS, Jassal DS, Duhamel TA. Exer-
cise training prevents the development of cardiac dysfunction in the low
dose streptozotocin diabetic rats fed a high fat diet. Can J Physiol Pharmacol
2013;91(1):809.
[35] Cao S, Li B, Yi X, Chang B, Zhu B, Lian Z, et al. Effects of exercise on AMPK
signaling and downstream components to PI3K in rat with type 2 diabetes.
PLoS One 2012;7(12):51709.
[36] Subash Babu P, Prabuseenivasan P, Ignacimuthu S. Cinnamaldehyde a poten-
tial antidiabetic agent. Phytomedicine 2007;14:1522.
[37] Ceriello A. Postprandial hyperglycemia and diabetes complications: is it time
to treat? Diabetes 2005;54:17.
[38] Hii CS, Howell SL. Effects of avonoids oninsulinsecretionand45Ca2
+
handling
in rat islets of Langerhans. J Endocrinol 1985;107(1):18.
[39] Abdul-Ghani MA, Tripathy D, DeFronzo RA. Contributions of beta cell dysfunc-
tion and insulin resistance to the pathogenesis of impaired glucose tolerance
and impaired fasting glucose. Diabetes Care 2006;29:11309.
[40] Edelman D, Olsen MK, Dudley TK, Harris AC, Oddone EZ. Utility of
hemoglobinA
1c
in predicting diabetes risk. J Gen Intern Med 2004;19:117580.
[41] Almdal TP, Vilstrup H. Effects of streptozotocin induced diabetes and diet on
nitrogen loss from organs and on the capacity of urea synthesis in rats. Dia-
betologica 1987;30(12):9526.
[42] Egbuonu ACC, Obidoa O, Ezeokonkwo CA, Ejikeme PM, Ezeanyika LUS.
Some biochemical effects of sub-acute oral administration of L-arginine on
monosodiumglutamate-fed Wistar albino rats 1: body weight changes, serum
cholesterol, creatinine, and sodiumion concentrations. Toxicol Environ Chem
2010;92:13317.
[43] Fortson WC, Tedesco FJ, Starnes EC, Shaw CT. Marked elevation of serum
transaminase activity associated with extra hepatic biliary tract disease. J Clin
Gastroenterol 1985;76:5025.
[44] Obrien RM, Granner DK. Regulation of gene expression by insulin. Biochem J
1991;278:0919.
[45] Meyer C, Woerle HJ, Dostou JM, Welle SL, Gerich JE. Abnormal renal, hepatic
and muscle glucose metabolismfollowing glucose ingestion in type 2 diabetes.
Am J Physiol Endocrinol Metab 2004;287:104956.
[46] Wajngot A, Chandramouli V, Schumann WC, Ekberg K, Jones PK, Efendic S, et al.
Quantitative contributions of gluconeogenesis to glucose production during
fasting in type 2 diabetes mellitus. Metabolism2001;50:4752.
[47] Matschinsky FM. Assessing the potential of glucokinase activators in diabetes
therapy. Nat Rev Drug Discov 2009;8:399441.
[48] Postic C, Shiota M, Magnuson MA. Cell-specic roles of glucokinase in glucose
homeostasis. Recent Prog HormRes 2001;56:195217.
[49] Taylor R, Agius L. The biochemistry of diabetes. BiochemJ 1988;250:62540.
[50] Kavanagh KL, Elling RA, Wilson DK. Structure of Toxoplasma gondii LDH1:
active-site differences fromhuman lactate dehydrogenases and the structural
basis for efcient APAD+ use. Biochemistry 2004;43:87989.
[51] Kurosaki E, Nakano R, Momose K, Shimaya A, Suzuki T, Shibasaki M, et al.
Hypoglycemic agent YM440 suppresses hepatic glucose output via gluconeo-
genesis by reducing glucose-6-phosphatase activity in obese Zucker rats. Eur J
Pharmacol 2003;468:1518.
[52] Pilkis SJ, Claus TH. Hepatic gluconeogenesis/glycolysis: regulation and struc-
ture/function relationships of substrate cycle enzymes. Annu Rev Nutr
1991;11:465515.
[53] Massillon D, Barzilai N, Chen W, Hu M, Rossetti L. Glucose regulates in
vivoglucose-6-phosphatase gene expression in the liver of diabetic rats. J Biol
Chem1996;271:98714.
[54] Chen R, Meseck M, McEvoy RC, Woo SL. Glucose-stimulated and self-limiting
insulin production by glucose-6-phosphatase promoter driven insulin expres-
sion in hepatoma cells. Gene Ther 2000;7:18029.
[55] Xu Y, Osborne BW, Stanton RC. Diabetes causes inhibition of glucose-6-
phosphate dehydrogenase via activationof PKA, whichcontributes to oxidative
stress in rat kidney cortex. AmJ Physiol 2005;289:10407.
[56] West IC. Glucose-6-phosphate dehydrogenase: a candidate gene for diabetes.
Diabet Med 2002;19:1724.
[57] Pederson BA, Schroeder JM, Parker G, Smith MW, DePaoli-Roach AA, Roach
PJ. Glucose metabolism in mice lacking muscle glycogen synthase. Diabetes
2005;54:346673.
[58] Parker G, Taylor R, Jones D, McClain D. Hyperglycemia and inhibition of
glycogen synthase in streptozotocin-treated mice: role of O-linked N acetyl-
glucosamine. J Biol Chem2004;279:2063642.
Anda mungkin juga menyukai
- Prediction of Municipal Wastewater Biochemical Oxygen Demand UsingDokumen13 halamanPrediction of Municipal Wastewater Biochemical Oxygen Demand UsingHernan DmgzBelum ada peringkat
- DiazabicyclooctanesDokumen6 halamanDiazabicyclooctanesHernan DmgzBelum ada peringkat
- Novel Techniques To Determine Dilution Ratios of Raw Wastewater andDokumen7 halamanNovel Techniques To Determine Dilution Ratios of Raw Wastewater andHernan DmgzBelum ada peringkat
- 1 s2.0 S0301479718313859 MainDokumen15 halaman1 s2.0 S0301479718313859 MainHernan DmgzBelum ada peringkat
- Kjeldahl Method for Nitrogen DeterminationDokumen12 halamanKjeldahl Method for Nitrogen DeterminationRaj BrothersBelum ada peringkat
- Determination of Seawater Biochemical Oxygen Demand Based On in SituDokumen6 halamanDetermination of Seawater Biochemical Oxygen Demand Based On in SituHernan DmgzBelum ada peringkat
- A Brief Review On Biochemical Oxygen DemandDokumen28 halamanA Brief Review On Biochemical Oxygen DemandHamletStevenCubillosBelum ada peringkat
- Cement and Concrete Research: SciencedirectDokumen12 halamanCement and Concrete Research: SciencedirectHernan DmgzBelum ada peringkat
- Effect of Interfacial Transition Zone On The Transport of Sulfate Ions inDokumen10 halamanEffect of Interfacial Transition Zone On The Transport of Sulfate Ions inHernan DmgzBelum ada peringkat
- Agricultural Water Management: A B C DDokumen7 halamanAgricultural Water Management: A B C DHernan DmgzBelum ada peringkat
- Cement and Concrete Research: SciencedirectDokumen12 halamanCement and Concrete Research: SciencedirectHernan DmgzBelum ada peringkat
- Extract Oil & Grease from Solids Using n-HexaneDokumen13 halamanExtract Oil & Grease from Solids Using n-Hexanel_655851999Belum ada peringkat
- Heavy Metals in Drinking WaterDokumen13 halamanHeavy Metals in Drinking WaterHernan DmgzBelum ada peringkat
- Use of LANDSAT 8 Images For Depth and Water Quality Assessment of El Guajaro Reservoir, ColombiaDokumen8 halamanUse of LANDSAT 8 Images For Depth and Water Quality Assessment of El Guajaro Reservoir, ColombiaHernan DmgzBelum ada peringkat
- Kjedhal MethodeDokumen17 halamanKjedhal MethodeLilis TuslinahBelum ada peringkat
- Determination of Nitrogen SpeciesDokumen14 halamanDetermination of Nitrogen SpeciesHernan DmgzBelum ada peringkat
- Use of LANDSAT 8 Images For Depth and Water Quality Assessment of El Guajaro Reservoir, ColombiaDokumen8 halamanUse of LANDSAT 8 Images For Depth and Water Quality Assessment of El Guajaro Reservoir, ColombiaHernan DmgzBelum ada peringkat
- 3M 6000 Series TDSDokumen5 halaman3M 6000 Series TDSHernan DmgzBelum ada peringkat
- The Fitness For Purpose of AM EURACHEM PDFDokumen70 halamanThe Fitness For Purpose of AM EURACHEM PDFLeila EspinosaBelum ada peringkat
- K, Na y ZN en AlbuminaDokumen6 halamanK, Na y ZN en AlbuminaHernan DmgzBelum ada peringkat
- Metales en Carnes y Comidas de Bebe Por E.a.ADokumen7 halamanMetales en Carnes y Comidas de Bebe Por E.a.AHernan DmgzBelum ada peringkat
- Tendencias de Metales en Quimica AnaliticaDokumen6 halamanTendencias de Metales en Quimica AnaliticaHernan DmgzBelum ada peringkat
- Trace Metal Chemistry in Arid-Zone Field Soils AmendedDokumen5 halamanTrace Metal Chemistry in Arid-Zone Field Soils AmendedHernan DmgzBelum ada peringkat
- Determination of Nitrogen SpeciesDokumen14 halamanDetermination of Nitrogen SpeciesHernan DmgzBelum ada peringkat
- Synthesis and Characterization of New Zeolite Materials Obtained From Fly Ash For Heavy Metals Removal in Advanced Wastewater TreatmentDokumen10 halamanSynthesis and Characterization of New Zeolite Materials Obtained From Fly Ash For Heavy Metals Removal in Advanced Wastewater TreatmentHernan DmgzBelum ada peringkat
- Biological AndNon-biologicalMethods For Silver Nanoparticles SynthesisDokumen10 halamanBiological AndNon-biologicalMethods For Silver Nanoparticles SynthesisHernan DmgzBelum ada peringkat
- Remocion Metales Pesados en Matrices AcuosasDokumen8 halamanRemocion Metales Pesados en Matrices AcuosasHernan DmgzBelum ada peringkat
- Chemical Composition and Antibacterial Activity of Brazilian PropolisDokumen6 halamanChemical Composition and Antibacterial Activity of Brazilian PropolisHernan DmgzBelum ada peringkat
- Waste Water Treatment: Chap 10Dokumen12 halamanWaste Water Treatment: Chap 10Zerihun AlemayehuBelum ada peringkat
- Ok - MetBio BMSResource TUFE283399 24 07 2009 PDFDokumen39 halamanOk - MetBio BMSResource TUFE283399 24 07 2009 PDFHernan DmgzBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Statement of Compulsory Winding Up As On 30 SEPTEMBER, 2008Dokumen4 halamanStatement of Compulsory Winding Up As On 30 SEPTEMBER, 2008abchavhan20Belum ada peringkat
- Hawk Technology Systems v. NCLDokumen6 halamanHawk Technology Systems v. NCLPriorSmartBelum ada peringkat
- Brain, Behavior, and Immunity: Alok Kumar, David J. LoaneDokumen11 halamanBrain, Behavior, and Immunity: Alok Kumar, David J. LoaneRinaldy TejaBelum ada peringkat
- Self Team Assessment Form - Revised 5-2-20Dokumen6 halamanSelf Team Assessment Form - Revised 5-2-20api-630312626Belum ada peringkat
- Exor EPF-1032 DatasheetDokumen2 halamanExor EPF-1032 DatasheetElectromateBelum ada peringkat
- Cisco CMTS Feature GuideDokumen756 halamanCisco CMTS Feature GuideEzequiel Mariano DaoudBelum ada peringkat
- Furnace ITV Color Camera: Series FK-CF-3712Dokumen2 halamanFurnace ITV Color Camera: Series FK-CF-3712Italo Rodrigues100% (1)
- Calibration Motion Control System-Part2 PDFDokumen6 halamanCalibration Motion Control System-Part2 PDFnurhazwaniBelum ada peringkat
- Insize Catalogue 2183,2392Dokumen1 halamanInsize Catalogue 2183,2392calidadcdokepBelum ada peringkat
- Deluxe Force Gauge: Instruction ManualDokumen12 halamanDeluxe Force Gauge: Instruction ManualThomas Ramirez CastilloBelum ada peringkat
- ExpDokumen425 halamanExpVinay KamatBelum ada peringkat
- PWC Global Project Management Report SmallDokumen40 halamanPWC Global Project Management Report SmallDaniel MoraBelum ada peringkat
- Finance at Iim Kashipur: Group 9Dokumen8 halamanFinance at Iim Kashipur: Group 9Rajat SinghBelum ada peringkat
- 2016 Mustang WiringDokumen9 halaman2016 Mustang WiringRuben TeixeiraBelum ada peringkat
- AVANTIZ 2021 LNR125 (B927) EngineDokumen16 halamanAVANTIZ 2021 LNR125 (B927) EngineNg Chor TeckBelum ada peringkat
- Investigatory Project Pesticide From RadishDokumen4 halamanInvestigatory Project Pesticide From Radishmax314100% (1)
- Um 0ah0a 006 EngDokumen1 halamanUm 0ah0a 006 EngGaudencio LingamenBelum ada peringkat
- JSA - 0026 Chipping & Granite cutting and lying Work At PB-19Dokumen2 halamanJSA - 0026 Chipping & Granite cutting and lying Work At PB-19Koneti JanardhanaraoBelum ada peringkat
- Material Safety Data Sheet Lime Kiln Dust: Rev. Date:5/1/2008Dokumen6 halamanMaterial Safety Data Sheet Lime Kiln Dust: Rev. Date:5/1/2008suckrindjink100% (1)
- Abinisio GDE HelpDokumen221 halamanAbinisio GDE HelpvenkatesanmuraliBelum ada peringkat
- Scharlau Chemie: Material Safety Data Sheet - MsdsDokumen4 halamanScharlau Chemie: Material Safety Data Sheet - MsdsTapioriusBelum ada peringkat
- 10 Slides For A Perfect Startup Pitch DeckDokumen6 halaman10 Slides For A Perfect Startup Pitch DeckZakky AzhariBelum ada peringkat
- Radio Theory: Frequency or AmplitudeDokumen11 halamanRadio Theory: Frequency or AmplitudeMoslem GrimaldiBelum ada peringkat
- Cells in The Urine SedimentDokumen3 halamanCells in The Urine SedimentTaufan LutfiBelum ada peringkat
- Daftar PustakaDokumen4 halamanDaftar PustakaRamli UsmanBelum ada peringkat
- Feasibility StudyDokumen47 halamanFeasibility StudyCyril Fragata100% (1)
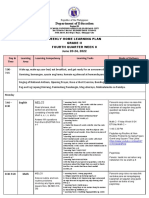
- Department of Education: Weekly Home Learning Plan Grade Ii Fourth Quarter Week 8Dokumen8 halamanDepartment of Education: Weekly Home Learning Plan Grade Ii Fourth Quarter Week 8Evelyn DEL ROSARIOBelum ada peringkat
- Impact of Bap and Iaa in Various Media Concentrations and Growth Analysis of Eucalyptus CamaldulensisDokumen5 halamanImpact of Bap and Iaa in Various Media Concentrations and Growth Analysis of Eucalyptus CamaldulensisInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Test Bank For Core Concepts of Accounting Information Systems 14th by SimkinDokumen36 halamanTest Bank For Core Concepts of Accounting Information Systems 14th by Simkinpufffalcated25x9ld100% (46)
- Basf Masterseal 725hc TdsDokumen2 halamanBasf Masterseal 725hc TdsshashiBelum ada peringkat