Diunggah oleh
Ambar RahmanHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Diunggah oleh
Ambar RahmanHak Cipta:
Format Tersedia
Endocrine Journal Advance Publication
Endocrine Journal 2012, 59
METABOLIC syndrome (MetS) is a term applying
to the appearance of several cardiovascular risk fac-
tors such as abdominal obesity, hyperglycemia, dyslip-
idemia, and high blood pressure related to insulin resis-
tance in the same patient [1].
At this moment, several defnitions of MetS exist.
Mostly used are those according to World Health
Organization (WHO), National Cholesterol Education
Program (NCEP) and International Diabetes Federation
(IDF). According to WHO defnition the basic com-
ponent of MetS is diabetes mellitus or glucose intoler-
ance, with at least two of further criteria present: central
obesity [elevated waist/hip ratio (WHR), or body mass
Metabolic syndrome infuencing infarct size and heart failure
in patients with acute coronary syndrome does gender
matter?
Darko Kranjec
1)
and Velimir Altabas
2)
1)
Department of Cardiology, Division of Internal Medicine, Zabok General Hospital, Zabok,Croatia
2)
Department of Endocrinology, Diabetes and Metabolic Diseases, Internal Clinic, University Hospital Centre
Sestre milosrdnice, Zagreb, Croatia
Abstract. Metabolic syndrome (MetS) is occurrence of diabetes mellitus/glucose intolerance, arterial hypertension, central
obesity, dyslipidemia and microalbuminuria in the same patient (defnition by WHO). Presence of metabolic syndrome is
associated with larger myocardial infarction size and complications following acute myocardial infarction. Two hundred
and thirty patients with acute coronary syndromes were analyzed. Those with MetS (n=141) included patients with diabetes
mellitus/glucose intolerance and at least two of the following criteria: hypertension, hypertriglyceridemia/low HDL
cholesterol, android obesity/body mass index (BMI) 30, microalbuminuria. Control group did not meet criteria for MetS.
Presence of heart failure was assigned according to Killip graduation. The MetS group had larger myocardial infarction
size determined by peak creatin-kinase (CK) (14841354 vs. 981890, p = 0.003) and creatin-kinase MB (141117 vs.
9578, p = 0.002). While in non-MetS group males had larger myocardial infarction than females, in MetS group females
had larger myocardial infarction than males. Cardiac failure occurred more in MetS group of patients, again more
emphasized in females. Occurrence of metabolic syndrome in acute coronary syndromes patients predisposes to larger
myocardial infarction size, more on the account of female patients having MetS. MetS, again particularly in females
predisposes to higher chance of having heart failure during acute coronary syndromes. Recognizing the female group with
MetS as of higher risk for large myocardial infarction and heart failure leads us to take special attention on this patients.
Key words: Metabolic syndrome, Acute coronary syndromes, Infarction size, Heart failure, Gender
index (BMI) over 30 kg/m
2
], hypertriglyceridemia, low
HDL cholesterol and elevated blood pressure. Central
obesity is a key component of MetS according to IDF
(with two others needed for diagnosis), and NCEP def-
nition does not include any obligatory feature - for mak-
ing the diagnosis there must be present at least three of
fve earlier mentioned conditions.
Specifc for a WHO defnition is that one of the basic
criteria is also microalbuminuria or elevated albumin/
creatinine ratio [2-5].
In the pathogenesis of MetS, the most important
role plays central abdominal obesity manifested not
necessarily as increased body mass index, but also as
increased waist circumference [6-8]. Central abdomi-
nal obesity is well known risk factor of total [9], but
also cardiovascular morbidity and mortality, particu-
larly regarding increased waist circumference [10].
Regarding BMI there are some data, that higher BMI
in late adolescence increases risk of coronary disease
Advance Publication
doi: 10.1507/endocrj. EJ 12-0131
ORIGINAL
The J apan Endocrine Society
Submitted Apr. 6, 2012; Accepted J ul. 10, 2012 as EJ 12-0131
Released online in J -STAGE as advance publication Aug. 17, 2012
Correspondence to: Velimir Altabas, Department of Endocrinology,
Diabetes and Metabolic Diseases, Internal Clinic, University
Hospital Centre Sestre milosrdnice, Vinogradska 29, Zagreb 10
000, Croatia. E-mail:velimir.altabas@gmail.com
2 Kranjec et al.
Endocrine Journal Advance Publication Endocrine Journal Advance Publication
Data analysis
Data regarded and analyzed in this trial were:
1) Demographic data of patients (age, gender, WHR,
BMI). Regarding age there are some data that
patients with MetS having myocardial infarction are
older [21], while regarding gender women may have
signifcantly higher rate of MetS during ACS than
man, and might be signifcantly older than man hav-
ing ACS [19].
2) Laboratory parameters: peak serum levels of car-
diac enzymes [CK, (CK MB fraction expressed
in IU/mL)], that were checked every 8 h until peak
and descent was documented. Peak serum cardiac
enzymes we used as a surrogate for myocardial
infarction size. Furthermore we analyzed serum tro-
ponin and brain natriuretic peptide (pro-BNP) level
at admittance, glycosylated hemoglobin (HbA1c),
creatinine, overall cholesterol, low-density lipopro-
tein (LDL) and HDL fractions, serum triglycerides,
presence of microalbuminuria, blood glucose level
at admittance, leukocyte count at admittance, fasting
glucose at days 4 and 5.
3) Concomitant diseases and previous medical his-
tory (glucose intolerance, diabetes mellitus, arterial
hypertension, grade of cardiac failure according to
Killip).
4) Previous medical history (anamnesis of previous
myocardial infarction)
Defnition of MetS and its components
MetS was defned according to WHO criteria [5].
1. Diabetes mellitus or glucose intolerance or insulin
resistance with two or more following criteria:
2. Hypertriglyceridemia/or low levels of HDL choles-
terol
3. Arterial hypertension
4. Android type of obesity/or high BMI index
5. Microalbuminuria
Diabetes mellitus was diagnosed by WHO criteria
and glucose intolerance was verifed by oral glucose
tolerance test (OGTT).
Triglycerides, total, HDL and LDL cholesterol were
determined from fasting blood sample. By WHO cri-
teria fasting triglycerides level of 1.7 mmol/L or higher
states hypertriglyceridemia, low HDL levels are below
0.9 mmol/L in males and 1.0 mmol/L in females.
Blood pressure of more than 130/85 mmHg was
measured 3 times in intervals of 10 minutes 3 days in
the row if hypertension is registered for the frst time,
and stroke in middle-aged males [11].
According to literature MetS is a risk factor for
cardiovascular diseases [12-14], by some authors it
is particularly emphasized in the population of mid-
dle-aged males [15], while others fnd that correlation
more strong in older population [16-18]. Differences
in age and in the infuence of MetS on cardiovascu-
lar morbidity and mortality could be caused by, so far
undiscovered geographic factors in particular areas
of world (Finland versus Australia and New Zealand,
respectively).
There are some data about the incidence of MetS in
patients with acute myocardial infarction [19], as well
as that MetS predisposes to higher rate of complica-
tions like cardiac failure, myocardial reinfarction [20,
21], and - according to some authors also to sudden
cardiac death. Some authors state that the presence
of MetS even in nondiabetic patients with myocardial
infarction predisposes to larger myocardial size and a
higher rate of acute renal failure [22].
Objective
The aim of this study is to determine the infarct size
and heart failure incidence in patients suffering from
acute coronary syndrome (ACS), regarding the pres-
ence of MetS. We analyzed infarct size and heart fail-
ure incidence in both groups regarding gender. We
also analyzed the infuence of particular components
of metabolic syndrome on infarct size and heart failure
and compared their infuence with infuence of MetS.
Subjects and Methods
Studied group
In our study, there were included 230 consecu-
tively patients suffering from ACS. All patients were
hospitalized in coronary care unit at University hos-
pital Dubrava, Zagreb, Croatia from J anuary 2006
until January 2007. Patients with subacute myocar-
dial infarction at admittance were not included into
the study. The ethics committee of University hospital
Dubrava approved the study.
To all patients the methods and goals of the study
were explained, and all patients entering the study gave
their written consent. Informations were received at
the time of admittance, and follow-up was obtained
during hospitalization.
Endocrine Journal Advance Publication
3 Metabolic and acute coronary syndrome
Endocrine Journal Advance Publication
63.29), and had signifcant more often low HDL levels
(p=0.007). There was no difference in standard cardiac
medications in both groups.
Baseline metabolic conditions of study population
are shown in Table 1.
All patients with STEMI underwent urgent per-
cutaneous coronary intervention (PCI), while
some patients with NSTEMI and UA [having high
Thrombolysis in Myocardial Infarction-Study group
(TIMI) risk score] underwent urgent or delayed PCI
during hospitalization.
Among 183 patients with myocardial infarction the
MetS group had statistically signifcant larger myo-
cardial infarct size as determined by peak CK-MB
[141117 vs. 9578 IU/mL (t= 3.208, df=176, p=
0.002)] and peak CK levels [1484 1354 vs. 981890
IU/mL (t= 3.022, df= 177, p= 0.003)] (Table 2), which
was particularly emphasized in females having MetS
(Fig. 1). Mean age of patients without MetS was 63.9
years (SD 11.83), while mean age of patients with
MetS was 65.7 years (SD 9.68). Statistical probabil-
ity that these two age averages are equal was 0.239, so
it does not able us to claim them statistically different.
In other words age was not found to have confound-
ing effects for differences in myocardial infarction size
between two groups (Tables 3a and 3b)
While in patients without MetS myocardial infarc-
tion size was signifcantly larger in males than in
females, in MetS group myocardial infarction size was
signifcantly larger in female group, and MetS-female
patients was a group with largest myocardial infarction
size at all (Fig. 1, Tables 3a and 3b).
Mean age of male patients with myocardial infarction
without MetS was 62.19, and of females were 66.17,
while mean age of males with MetS having myocar-
dial infarction was 64.11, of females 69.3. When using
statistical method of analysis of variance (ANOVA)
and analyzing myocardial infarction size (expressed as
peak MB-CK values) in terms of age and gender, we
concluded, that age had no infuence on the myocardial
infarction size difference between genders (p =0.875)
in our group of patients. There is a statistically signif-
icant difference according to MetS (p=0.04), but not
regarding gender (p=0.810), and there is interactive
infuence between MetS and gender (p=0.020) (Tables
3a and 3b).
All patients with MetS having myocardial infarction
had diabetes mellitus/glucose intolerance, so the pres-
ence of diabetes mellitus/glucose intolerance again had
another criterion was positive history of hypertension.
Android type of obesity was determined by WHR
higher than 0.9 in males, or 0.85 in females or BMI
higher than 30 kg/m
2
.
Microalbuminuria was measured by semi quantita-
tive method by CLINITEK bands: signifcant microal-
buminuria appeared when level of albumin is urine was
20 mg/L or more, or when albumin/creatinine ratio was
30 mg/g or more.
Defnition of heart failure
Congestive heart failure was defned by chest radi-
ography, echocardiography, and/or physical fndings
as: ventricular (S3), atrial (S4) gallop, tachyarrhythmia,
pulsus-alternans-rapid rate, dyspnea, fatigue, ascites,
peripheral edema, and liver enlargement, symptoms
of pulmonary edema and by increased serum pro-BNP
level at admittance. Stage of congestive heart failure in
patients based on clinical fndings was graded in one of
four stages according to Killip classifcation. Patients
having stage II or higher by Killip classifcation were
considered as positive in terms of having heart failure.
Increased serum pro-BNP level at admittance was used
as additional tool to diagnose/exclude heart failure.
Statistical analysis
Continuous variables were expressed as mean (M)
and standard deviation (SD). Dichotomous variables
were expressed as percentage. Students t test was
used to compare continuous variables, and Fishers
Exact Test was used to compare dichotomous variables.
Additionally, for testing hypotheses that the group or
cell means of the dependent variable (MB-CK) are
equal, analysis of variance was performed with two
factors (MetS components by gender) and age as cova-
riate. A p value < 0.05 was considered to indicate sta-
tistical signifcance. All statistical analyses were per-
formed with the IBM SPSS Statistics 19 software.
Results
Among 230 patients with ACS 141 (61.3%) met
criteria for MetS according to WHO (similar to data
from literature [19]), while 89 (38.7%) did not have
MetS. MetS was present in 92 of 152 male patients
(60.5%) and in 49 of 78 females (62.8%), so there were
no signifcant differences in gender. 47 of 230 patients
had UA, 91 NSTEMI, and 92 STEMI. Women hav-
ing ACS were older (mean age 68.28) than men (mean
4 Kranjec et al.
Endocrine Journal Advance Publication Endocrine Journal Advance Publication
Table 1 Baseline characteristics of study population
Presence of MetS components Gender N
Sig.
*
Diabetes mellitus/glucose intolerance
No
Male
Female
33
20
0.490
Yes
Male
Female
89
41
Total 183
Low HDL
No
Male
Female
32
6
0.007
Yes
Male
Female
90
55
Elevated triglicerides
No
Male
Female
53
27
1.000
Yes
Male
Female
69
34
Hypertension
No
Male
Female
40
14
0.169
Yes
Male
Female
82
47
Microalbuminuria
No
Male
Female
51
31
0.207
Yes
Male
Female
71
30
High BMI
No
Male
Female
73
39
0.520
Yes
Male
Female
49
22
Elevated WHR
No
Male
Female
30
19
0.286
Yes
Male
Female
92
42
* Fishers Exact Test.
Table 2 Metabolic syndrome, its components, and myocardial infarction size.
Presence of MetS and its components
CK MB-CK
n M SD p***** n M SD p*****
MetS
No 66 981 890
0.003
66 95 78
0.002
Yes 117 1484 1354 117 141 117
Low HDL cholesterol*
No 38 1047 945
n.s.
38 90 87
0.024
Yes 145 1370 1287 145 133 110
Diabetes mellitus/glucose intolerance
No 53 1043 930
0.036
53 99 81
0.020
Yes 130 1409 1320 130 134 114
Hypertension
No 54 1290 1100
n.s.
54 126 100
n.s.
Yes 129 1308 1283 129 123 109
Hypertriglyceridemia**
No 80 1095 935
0.034
80 109 92
n.s.
Yes 103 1464 1399 103 136 116
Microalbuminuria***
No 82 1320 1157
n.s.
82 129 95
n.s.
Yes 101 1289 1290 101 120 115
BMI (kg/m
2
)
30 (normal) 112 1343 1269
n.s.
112 123 103
n.s.
>30 (high) 71 1240 1168 71 126 112
WHR****
Normal 49 1292 1266
n.s.
49 116 105
n.s.
Elevated 134 1307 1220 134 127 107
M = mean peak CK (MB-CK) in IU/mL; SD = standard deviation; * < 0.9 mmol/L in males and < 1.0 mmol/L in females; ** 1.7
mmol/L; *** urine albumin level 20 mg/L, or albumin/creatinine ratio 30 mg/g; **** > 0.9 in males and > 0.85 in females; *****
Students t test.
Endocrine Journal Advance Publication
5 Metabolic and acute coronary syndrome
Endocrine Journal Advance Publication
no confounding effect regarding the difference in myo-
cardial infarction size between males and females.
Group of patients with diabetes mellitus and glucose
intolerance (130 out of 183 patients having myocardial
infarction) had also larger myocardial infarction deter-
mined by peak MB-CK [134114, versus 9981 IU/
mL values (t=2.355, df= 134, p=0.020)] and peak CK
[14091320 versus 1043930 IU/mL (t= 2.120, df=
135, p= 0.036)] than patients without diabetes and glu-
cose intolerance, respectively.
When analyzed all other particular components
of MetS (arterial hypertension, HDL, triglycerides,
microalbuminuria, WHR, BMI), the group of patients
with low HDL had also signifcantly larger myocar-
dial infarction size than group with normal HDL when
size of myocardial infarction was expressed by peak
MB-CK. While using peak-CK as a surrogate for
myocardial infarction size, group of patients with high
triglycerides showed statistically signifcant larger
myocardial infarction than group with normal triglyc-
erides (Table 2).
Since MB-CK is more sensitive and more specifc
Table 3b Myocardial infarction size expressed as mean peak MB-CK according to MetS (ANOVA)
a,b
MB-CK
Hierarchical method
Sum of Squares df Mean Square F Sig
Covariates Age 267.826 1 267.826 .025 .875
MetS 90638.050 1 90638.050 8.431 .004
Gender 632.088 1 623.088 .058 .810
2-way interactions MetS Gender 59361.419 1 59361.419 5.522 .020
Model 150890.4 4 37722.596 3.509 .009
Residual 1913525 178 10750.141
Total 20644416 182 11342.942
a
, MB-CK by MetS, Gender and Age;
b
, Covariates entered frst
Table 3a Myocardial infarction size expressed as mean peak MB-CK according to MetS, age and
gender
MetS Gender n M SD Mean age SD
No
Male
Female
43
23
110.77
64.26
86.84
46.93
62.19
66.17
13.27
11.78
Yes
Male
Female
79
38
130.38
162.84
109.47
128.86
64.11
69.63
9.74
9.14
Total 183 124.20 106.50 65.07 11.04
M = mean peak MB-CK in IU/mL; SD =standard deviation
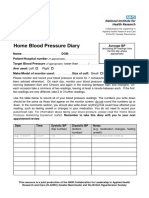
Fig. 1 Myocardial infarction size (expressed in mean peak
MB-CK in IU/mL) according to gender and metabolic
syndrome.
6 Kranjec et al.
Endocrine Journal Advance Publication Endocrine Journal Advance Publication
While in the group without diabetes/glucose intolerance
mean MB-CK value in males was 119.12, in females it
was only 66.25. On the contrary, in the group of diabe-
tes/glucose intolerance the mean CK-MB was 125.08
in males and even 154.66 in females (p=0.22). All
other components of MetS including elevated BMI and
WHR did not show important infuence of gender on
myocardial infarction size (Table 4).
When analyzing all 230 patients with ACS, the pres-
for cardiac muscle, we can conclude that patients with
MetS, diabetes mellitus/glucose intolerance and low
HDL are at risk of having larger myocardial infarction,
because they had statistically signifcantly larger myo-
cardial infarction than their counterpart groups.
When using ANOVA to analyze particular compo-
nents of MetS and their infuence on differences in MI
size according to gender, most of this infuence could
be attributed to diabetes mellitus/glucose intolerance.
Table 4 Infuence of different MetS components on peak MB- CK
Presence of MetS components (a) Gender (b) n
MB-CK
Sig.
M SD
Diabetes mellitus/glucose
intolerance
No
Male
Female
33
20
119.12
66.25
90.14
49.56
p
age
=0.876
p
a
=0.041
p
b
=0.784
p
a
b
=0.022
Total 53 99.17 81.04
Yes
Male
Female
89
41
125.08
154.66
106.67
127.51
Total 130 134.41 113.99
Total
Male 122 123.47 102.13
Female 61 125.67 115.62
Total 183 124.20 106.50
Low HDL
No
Male
Female
32
6
97.06
49.17
92.25
22.18
p
age
=0.877
p
a
=0.025
p
b
=0.757
p
ab
=0.333
Total 38 89.50 86.66
Yes
Male
Female
90
55
132.86
134.02
104.29
118.69
Total 145 133.30 109.57
Elevated triglicerides
No
Male
Female
53
27
115.36
97.04
101.48
69.30
p
age
=0.878
p
a
=0.089
p
b
=0.938
p
ab
=0.287
Total 80 109.18 91.84
Yes
Male
Female
69
34
129.7
148.41
102.93
138.99
Total 103 135.87 115.72
Hypertension
No
Male
Female
40
14
135.7
98.86
103.89
85.46
p
age
=0.879
p
a
=0.851
p
b
=0.909
p
ab
=0.173
Total 54 126.15 100.00
Yes
Male
Female
82
47
117.50
133.66
101.36
122.84
Total 129 123.39 109.48
Microalbuminuria
No
Male
Female
51
31
138.55
112.71
98.17
89.70
p
age
=0.878
p
a
=0.588
p
b
=0.967
p
ab
=0.120
Total 82 128.78 95.33
Yes
Male
Female
71
30
112.63
139.07
104.22
137.73
Total 101 120.49 115.12
High BMI
No
Male
Female
73
39
130.42
109.26
104.05
100.97
p
age
=0.878
p
a
=0.841
p
b
=0.916
p
ab
=0.071
Total 112 123.05 103.03
Yes
Male
Female
49
22
113.10
154.77
99.35
135.50
Total 71 126.01 112.48
Elevated WHR
No
Male
Female
30
19
126.3
99.53
101.20
112.64
p
age
=0.879
p
a
=0.532
p
b
=0.879
p
ab
=0.264
Total 49 115.92 104.45
Yes
Male
Female
92
42
122.54
137.50
102.97
116.33
Total 124 127.23 107.12
M = mean peak CK (MB-CK) in IU/mL; SD = standard deviation; * ANOVA with factors a by b, with age
as covariate; p
a
sig. of factor a, p
b
sig. of factor b, p
ab
sig. of interaction, p
age
sig. of covariate.
Endocrine Journal Advance Publication
7 Metabolic and acute coronary syndrome
Endocrine Journal Advance Publication
When analyzing other components of MetS and their
possible infuence on heart failure, we can see that in
subgroups of patients with microalbuminuria, elevated
WHR and high BMI there is tendency toward having
higher rate of cardiac failure during ACS, although not
statistically signifcant (Table 5).
If we analyze some other laboratory parameters that
might have infuenced myocardial infarction size and
heart failure such as elevated leukocyte count at admit-
tance, elevated blood sugar at admittance and elevated
serum creatinine level we found a correlation between
elevated creatinine at admittance and heart failure
(Table 6a), while there was no correlation with myo-
cardial infarction size (Table 6b).
ence of cardiac failure was also signifcantly higher in
the MetS group. 89 out of 230 patients have devel-
oped heart failure during ACS (grade Killip II or more).
While only 28.1% of patients with heart failure were
from non-MetS group (25 patients), even 71.9% of
patients with heart failure (64 of them) were from the
MetS group (Fig. 2), which was again relatively more
emphasized in females (Fig. 3).
When analyzing according to MetS presence, 71.9%
(64) of patients without MetS did not developed
heart failure, and only 28.1% (25) had, while in MetS
group even 45.4% (64 of 141) developed heart failure
(p=0.012, Odds ratio=2.128) (Table 5). We can con-
clude that MetS increases the chance of having heart
failure during ACS.
Regarding cardiac failure aside from MetS group,
diabetes mellitus/glucose intolerance group had also
statistically signifcant higher cardiac failure by Killip
classifcation than the group without diabetes mellitus/
glucose intolerance. While in patients without diabe-
tes/glucose intolerance only 27.4% had heart failure
and 72.6% did not have, even 43.9% of patients with
diabetes mellitus/glucose intolerance developed heart
failure (p=0.020, Odds ratio=2.078).
Fig. 3 Heart failure occurrence according to gender and
metabolic syndrome
Fig. 2 Heart failure occurrence according to MetS in patients
with ACS
8 Kranjec et al.
Endocrine Journal Advance Publication Endocrine Journal Advance Publication
Table 5 Metabolic syndrome and its components infuencing heart failure.
Presence of MetS and its
components
Presence of heart failure
p*****
Odds
ratio
No Yes
n (%) n (%)
MetS
No 64 (71.9) 25 (28.1)
0.012 2.128
Yes 77 (54.6) 64 (45.4)
Low HDL cholesterol*
No 28 (58.3) 20 (41.7)
n.s. 0.855
Yes 113 (62.1) 69 (37.9)
Diabetes mellitus/
glucose intolerance
No 53 (72.6) 20 (27.4)
0.020 2.078
Yes 88 (56.1) 69 (43.9)
Hypertension
No 40 (60.6) 26 (39.4)
n.s. 0.960
Yes 101 (61.6) 63 (38.4)
Hypertriglyceridemia**
No 62 (60.8) 40 (39.2)
n.s. 0.961
Yes 79 (61.7) 49 (38.3)
Microalbuminuria***
No 69 (65.7) 36 (34.3)
n.s. 1.411
Yes 72 (57.6) 53 (42.4)
BMI (kg/m
2
)
30 94 (63.1) 55(36.9)
n.s. 1.236
>30 55 (58.0) 34 (42.0)
WHR****
Normal 41 (65.1) 22 (34.9)
n.s. 1.249
Elevated 100 (59.9) 67 (40.1)
Total 141 (61.3) 89 (38.7)
* < 0.9 mmol/L in males and < 1.0 mmol/L in females; ** >1.7 mmol/L; *** urine albumin
level >20 mg/L, or albumin/creatinine ratio >30 mg/g; **** > 0.9 in males and > 0.85 in
females; ***** Fishers Exact Test.
Table 6a Blood glucose, leukocyte count, and creatinine at admittance infuencing heart failure.
Laboratory fndings at admittance
Presence of heart failure
p*
Odds
ratio
No Yes
n (%) n (%)
Blood glucose at admittance
11 mmol/L 88 (62.9) 52 (37.1)
n.s. 1.181
>11 mmol/L 53 (58.9) 37 (41.1)
Leukocyte count at admittance
1010
3
/L 112 (64.4) 62 (35.6)
n.s. 1.682
>1010
3
/L 29 (51.8) 27 (48.2)
Creatinine level at admittance
97 mmol/L 96 (66.2) 49 (33.8)
0.050 1.741
>97 mmol/L 45 (52.9) 40 (47.1)
Total 141 (61.3) 89 (38.7)
* Fishers Exact Test.
Table 6b Blood glucose, leukocyte count, creatinine at admittance, and myocardial infarction size.
Laboratory fndings at admittance
CK MB-CK
n M SD p* n M SD p*
Blood glucose at admittance
11 mmol/L 110 1269 1122
n.s.
110 124 101
n.s.
>11 mmol/L 73 1353 1380 73 125 114
Leukocyte count at admittance
1010
3
/L 134 1290 1163
n.s.
134 125 102
n.s.
>1010
3
/L 49 1336 1406 49 121 119
Creatinine level at admittance
97 mmol/L 115 1274 1198
n.s.
115 126 106
n.s.
>97 mmol/L 68 1352 1286 68 121 107
Endocrine Journal Advance Publication
9 Metabolic and acute coronary syndrome
Endocrine Journal Advance Publication
attributed to differences in age and attendant comor-
bidities. Female patients with coronary artery disease
typically are older, and may have a higher prevalence
of risk factors.
Otherwise, gender differences in the size of infarc-
tion and clinical outcome of patients with acute myocar-
dial infarction may be explained in part by the female
status. Several conditions found only in women may
hint at differences in the pathophysiology of ischemic
vascular disease between sexes, including early meno-
pause, gestational diabetes, peripartum vascular dissec-
tion, preeclampsia and eclampsia, polycystic ovarian
syndrome, low-birth-weight children, and hypotha-
lamic hypoestrogenemia. Females also have a higher
prevalence of vascular diseases like Raynauds phe-
nomenon, migraines, and other vasospastic disorders.
There is also evidence that sex hormones play a role
in the pathophysiology of vascular disease. Changes
in estrogen and androgen balance occur during preg-
nancy, during the peripartum period, and with the use
of oral contraceptives or hormone replacement ther-
apy. Additionally, the aging process heralds a marked
reduction in estrogen levels. The predominant source
of estrogen before menopause is estradiol. After meno-
pause, a lower level of estrogen is produced primarily
from the conversion of androgens to estrone in adipose
tissue. These variations have implications for the dif-
ferences in ischemic heart disease between the sexes
and are coincident with the rise in risk for women that
occurs after menopause. Further evidence that may
help to explain variations in coronary artery disease
outcome are gender differences in vascular anatomy.
Women typically have smaller and less compliant con-
duit arteries than men. Age-related stiffening of the
aorta appears more prominent in diabetic women than
men.
Additional evidence for sex-related differences in
arterial size and remodeling comes from data on trans-
plant and transgender patients. These data support the
concept of differences in vascular physiology based on
sex hormone status. There appears to be enlargement
with androgens, consistent with positive remodeling.
The latter may itself be an independent marker of vas-
cular disease [39].
Similar to some previous studies, the incidence of
MetS was high [19, 40] - around 60%. MetS was asso-
ciated with a higher rate of cardiac failure following
ACS, while so far there were data about higher rates of
heart failure following myocardial infarction [21] (in
present studies patients with unstable angina were not
Discussion
MetS is a well known risk factor for CVD [12-14].
Regarding particular components of metabolic syn-
drome there are many trials investigating diabetes mel-
litus and worse outcome following myocardial infarc-
tion [23-25].
There is also evidence that high triglycerides and low
HDL, as well as elevated triglycerides/HDL ratio pre-
dict frst coronary syndrome in men [26], all cause mor-
tality in women with suspected myocardial ischemia
[27], and extensive coronary disease [28]. According
to some authors, hypertriglyceridemia is associated
with cardiovascular disease (CVD) and MetS [29].
Regarding hypertension and ACS, there are some
data, that antecedent hypertension predicts heart fail-
ure in patients with myocardial infarction [30].
Regarding obesity and myocardial infarction some
authors state that BMI is inversely related to mortality
during myocardial infarction (unlike WHR) [31,32],
while others state that central obesity is associated with
larger myocardial necrosis during myocardial infarc-
tion [33]. On long term data are not consistent, while
some authors state that abdominal obesity is an inde-
pendent predictor of all-cause mortality following
myocardial infarction particularly in men [34], others
state BMI has no infuence on survival following myo-
cardial infarction [35].
There are some trials showing that microalbumin-
uria is a predictor of increased risk for complications
following myocardial infarction [36] and that patients
with microalbuminuria have larger myocardial infarc-
tion size-even nondiabetic, hypertensive patients [37].
Others state that microalbuminuria during myocar-
dial infarction is a strong predictor for 1-year mortal-
ity [38].
This is the frst study to our knowledge demonstrat-
ing that females with acute myocardial infarction and
MetS have larger infarct size than males, which is in
opposite to the group without MetS. Although females
with MetS having myocardial infarction were older,
and had more often low HDL levels, statistical analysis
showed that age and low HLD levels had no confound-
ing effect. In the group of patients with myocardial
infarction, but without MetS, females were also older
than males, but males had larger myocardial infarction
than females, so the cause of larger myocardial infarc-
tion in females lies somewhere beyond it.
Much, but not all of this gender disparity can be
10 Kranjec et al.
Endocrine Journal Advance Publication Endocrine Journal Advance Publication
m
2
), normal WHR or no microalbuminuria (Table 5).
Although it is well known that the incidence of MetS
during acute myocardial infarction is high and that it
predisposes to higher rate of complications [21], MetS
is, however still under-recognized and under-treated
[41]. Recognizing MetS in patients during ACS as of
very high risk for larger infarction size and heart failure
rate (especially in females) leads us to take more atten-
tion to this group of patients, during hospitalization as
well on the discharge.
Learning points
Metabolic syndrome infuencing infarct size and
heart failure in patients with acute coronary syndrome
does gender matter?
Patients with MetS have larger myocardial infarc-
tion than patients with no MetS.
In the group of patients with no MetS, males have
larger myocardial infarction size than females.
In the group of patients with MetS, females have
larger myocardial infarction size than males.
Patients with MetS have higher rate of heart failure
during ACS than non - MetS patients, which is par-
ticularly emphasized in females.
Since females with MetS having ACS are a group
of higher risk for having larger myocardial infarc-
tion and heart failure, all females with MetS having
ACS should probably need more intensive surveil-
lance during hospitalization, and probably urgent
coronarography, nevertheless which type of ACS
they have.
Acknowledgements
The authors express their gratitude to Coronary Care
Unit staff of University Hospital Dubrava, Zagreb,
Croatia.
involved). There is also a tendency toward higher per-
centage of cardiac failure in females with MetS having
ACS, not previously described in literature.
To our knowledge, it is also the frst study fac-
ing directly MetS versus its components in the terms
of comparing risk for larger myocardial infarction size
and cardiac failure. In that manner we found that MetS
group had statistically signifcant larger myocardial
infarction in the terms of peak CK and MB-CK than
non-MetS group, which matches with data from litera-
ture [22]. The mechanism predisposing for larger myo-
cardial infarction and cardiac failure in MetS patients
might be advanced atherosclerosis and/or endothelial
dysfunction in this group of patients. Those patients are
more prone to coronary artery disease, which is proba-
bly more severe in patients having at the same time dia-
betes/glucose intolerance, hypertension, dyslipidemia,
obesity, and microalbuminuria (components of MetS).
When analyzing particular components of MetS, dia-
betes mellitus/glucose intolerance group and low HDL
group had larger myocardial infarction size than groups
with no diabetes/glucose intolerance and normal HDL,
respectively. Other components of MetS (hypertension,
increased BMI, microalbuminuria, elevated WHR) did
not appear to be neither predictors of larger myocardial
infarction size, nor cardiac failure when comparing with
groups with no hypertension, normal BMI, no microal-
buminuria and normal WHR in this study. Regarding
high triglyceride levels we can conclude that it might
be of importance in the terms of myocardial infarction
size, but not as high important as MetS, diabetes melli-
tus/glucose intolerance or low HDL.
Regarding heart failure during ACS, again groups
with MetS and diabetes mellitus/glucose intolerance
had higher percentage of heart failure than the control
groups. In the groups of patients with elevated BMI,
elevated WHR and microalbuminuria there is a ten-
dency toward higher rate of cardiac failure when com-
paring with groups with normal BMI (beyond 30 kg/
1. Eckel RH, Grundy SM, Zimmet PZ (2005) The meta-
bolic syndrome. Lancet 365: 1415-1428.
2. World Health Organization (1999) Defnition, diagnosis,
and classifcation of diabetes mellitus and its complica-
tions: report of WHO consultation. Part 1: Diagnosis
and classifcation of diabetes mellitus. WHO.
3. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel
RH, et al. (2005) American Heart Association; National
Heart, Lung and Blood Institute. Diagnosis and man-
agement of the metabolic syndrome: an American
Heart Association/National Heart, and Blood Institute
Scientifc Statement. Circulation 112: 2735-2762.
4. Alberti KG, Zimmet P, Shaw J (2005) IDF Epidemiology
Task Force Consensus Group. The metabolic syn-
References
Endocrine Journal Advance Publication
11 Metabolic and acute coronary syndrome
Endocrine Journal Advance Publication
ological and cardiovascular risk factors at entry. Aust N
Z J Med; 21: 701-709.
19. aliunas R, lapikas R, Babarskiene R, lapikiene B,
Lukiene D, et al. (2008) The prevalence of the met-
abolic syndrome components and their combinations
in men and women with acute ischemic syndromes.
Medicina (Kaunas) 44(7): 521-528.
20. Kranjec D, Pinter , Birti T, abrijan T, Halle J, et al.
(2002) Metabolic Syndrome X-High Factor for Acute
Myocardial Infarction and Its Complications. Coll
Antropol 26(1): 23-29.
21. Zeller M, Steg PG, Ravisy J, Laurent Y, Janin-Manifcat
L, et al. (2005) Prevalence and Impact of Metabolic
Syndrome on Hospital Outcomes in Acute Myocardial
Infarction. Arch Intern Med 165(10): 1192-1198.
22. Clavijo LC, Pinto TL, Kuchulakanti PK, Torguson R,
Chu WW, et al. (2006) Metabolic syndrome in patients
with acute myocardial infarction is associated with
increased infarct size and in- hospital complications.
Cardiovasc Revasc Med 7: 7-11.
23. Abraham WT (2003) Diabetes, hypertension, and renal
insuffciency in post-myocardial infarction cardiovas-
cular risk. Rev Cardiovasc 4 Suppl 3:S30-6.
24. Abbud ZA, Shindler DM, Wilson AC, Kostis JB (1995)
Effect of diabetes mellitus on short-and longterm mor-
tality rates of patients with acute myocardial infarction: a
statewide study Myocardial Infarction Data Acquisition
System Study Group. Am Heart J 130: 51-58.
25. Donahoe SM, Stewart GC, Mc Cabe CH, Mohanavelu
S, Murphy SA, et al. (2007) Diabetes and Mortality
Following Acute Coronary Syndromes. JAMA 298(7):
765-775.
26. Codero A, Andres E, Ordonez B, Leon M, Laclaustra M,
et al. (2009) Usefulness of triglycerides-to-high-density
lipoprotein cholesterol ratio for predicting the frst coro-
nary event in men. Am J Cardiol 104(10): 1393-1397.
27. Bittner V, Johnson BD, Zineh I, Pharm D, Rogers WJ, et
al. (2009) The TG/HDL Cholesterol Ratio Predicts All
Cause Mortality in Women With Suspected Myocardial
Ischemia: a Report from the Womens Ischemia
Syndrome Evaluation (WISE). Am Heart J 157(3): 548-
555.
28. Lemos da Luz P, Favarato D, Rocha-Faria NJ ,
Lemos P, Palandri-Chagas ACP (2008) High Ratio of
Triglycerides to HDL-Cholesterol Predicts Extensive
Coronary Disease. Clinics 63: 427-432.
29. Ascaso J F, Millan J , Mateo-Gallego R, Ruiz A, Suarez-
Tembra M, et al. (2011) Prevalence of metabolic syn-
drome and cardiovascular disease in a hypertriglyceri-
demic population. Eur J Intern Med 22(2): 177-181.
30. Richards AM, Nicholls MG, Troughton RW, Lainchbury
J G, Elliot J , et al. (2002) Antecedent hypertension and
heart failure after myocardial infarction. J Am Coll
Cardiol 39: 1182-1188.
31. Lee SH, Park JS, Kim W, Shin DG, Kim YJ, et al.
drome-a new worldwide defnition. Lancet 366: 1059-
1062.
5. Gerard TC, Seng KG, Gerald FW (2006) Revisiting the
metabolic syndrome. Med J Aust 185(8): 445-448.
6. Ferranini E, Haffner SM, Mitchel BD, Stern MP (1991)
Hyperinsulinemia: the key feature of a cardiovascular
and metabolic syndrome. Diabetologia 34: 416-422.
7. Reaven GM (2005) The insulin resistance syndrome:
defnition and dietary approaches to treatment. Annu
Rev Nutr 25: 391-406.
8. Nilsson G, Hedberg P, J onason T, Lnnberg I, Tenerz ,
et al. (2008) Waist circumference alone predicts insulin
resistance as good as the metabolic syndrome in elderly
women. Eur J Intern Med 19: 520-526.
9. Chen Y, Jiang Y, Mao Y (2007) Hospital admissions
associated with body mass index in Canadian adults. Int
J Obes 31: 962-967.
10. Willis LH, Slentz CA, Houmard J A, J ohnson J L, Duscha
BD, et al. (2007) Minimal versus Umbilical Waist
Circumference measures as Indicators of Cardiovascular
Disease Risk. Obesity (Silver Spring) 15: 753-759.
11. Falkstedt D, Hemmingsson T, Rasmussen F, Lundberg
I (2007) Body mass index in late adolescence and its
association with coronary heart disease and stroke in
middle age among Swedish men. Int J Obes (Lond)
31(5): 777-783.
12. Isomaa B, Almgren P, Tuomi T, Forsen B, Lahti K, et al.
(2001) Cardiovascular morbidity, and mortality associ-
ated with the metabolic syndrome. Diabetes Care 24:
683-689.
13. Ford ES (2004) The metabolic syndrome and mortal-
ity from cardiovascular disease and all-causes: fndings
from the National Health and Nutrition Examination
Survey II Mortality Study. Atherosclerosis 173: 309-
314.
14. Sattar N, Gaw A, Scherbakova O, Ford I, OReilly DS,
et al. (2003) Metabolic syndrome with and without
C-reactive protein as a predictor of coronary heart dis-
ease and diabetes in the West of Scotland coronary pre-
vention study. Circulation 108: 414-419.
15. Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK,
Kumpusalo E, et al. (2002) The metabolic syndrome
and total and cardiovascular disease mortality in mid-
dle-aged men. JAMA 288: 2709-2716.
16. Simons LA, Simons J , Friendlander Y, McCallum J
(2007) Does a diagnosis of the metabolic syndrome pro-
vide additional prediction of cardiovascular disease and
total mortality in the elderly? The Dubbo study. Med J
Aust 186(8): 400-403.
17. Simons LA, McCallum J , Simons J , Powell I, Ruys J ,
et al. (1990) The Dubbo study: an Australian prospec-
tive community study of the health of elderly. Aust N Z
J Med 20: 783-789.
18. Simons LA, McCallum J , Friedlander Y, Simons J ,
Powell I, et al. (1991) Dubbo Study of the elderly: soci-
12 Kranjec et al.
Endocrine Journal Advance Publication
1-month mortality in myocardial infarction. Am Heart J
157(2): 327-333.
37. Lazzeri C, Valente S, Chiostri M, Picariello C, Gensini
GF (2010) Microalbuminuria in hypertensive nondia-
betic patients with ST elevation myocardial infarction.
J Cardiovasc Med (Hagerstown) 11: 748-753.
38. Berton GR, Cordiano R, Palmieri R, Cucchini F, De Toni
R, et al. (2001) Microalbuminuria during acute myocar-
dial infarction; a strong predictor for 1-year mortality.
Eur Heart J 22(16): 1466-1475.
39. Anderson RD, Pepine CJ (2007) Gender Differences in
the Treatment for Acute Myocardial Infarction. Bias or
Biology? Circulation 115:823- 826.
40. Tenerz A, Norhammar A, Silveira A, Hamsten A,
Nilsson G, et al. (2003) Diabetes, insulin resistance,
and the metabolic syndrome in patients with acute myo-
cardial infarction without previously known diabetes.
Diabetes Care 26(10): 2270-2276.
41. Prasad SB, Fahrtash F, Malaiapan Y, Meredith IT,
Cameron J (2010) Obesity and the metabolic syn-
drome in patients with acute myocardial infarction. Int
J Cardiol 144(3): 450-451.
(2008) Impact of body mass index and waist-to-hip
ratio on clinical outcomes in patients with ST-segment
elevation acute myocardial infarction (from the Korean
Acute Myocardial Infarction Registry). Am J Cardiol
102(8): 957-965.
32. Zeller M, Steg PG, Ravisy J, Lorgis L, Laurent Y, et
al. (2008) Relation between Body Mass Index, Waist
Circumference, and Death After Acute Myocardial
infarction. Circulation 118: 465-456.
33. Iglesias-Bolanos P, Olivar-Roldan J, Penalver-Talavera
D, Diaz-Guardiola P, Vega-Pinero B, et al. (2009) Effect
of abdominal obesity on size of myocardial infarction.
Endocrinol Nutr 56(1): 4-8.
34. Kragelund C, Hassager C, Hildebrandt P, Torp-Pedersen
C, Kober L (2005) Impact of obesity on long-term
prognosis following acute myocardial infarction. Int J
Cardiol 98(1): 123-131.
35. Bucholz EM, Rathore SS, Reid KJ, Spertus JA,
Krumholz HM (2010) Association of body mass index
and mortality after acute myocardial infarction. J Am
Coll Cardiol 55(10s1): A125.
36. Schiele F, Menevau N, Chopard R, Genon VD, Oettinger
J , et al. (2009) Prognostic value of microalbuminuria on
Anda mungkin juga menyukai
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- VND ArticleDokumen11 halamanVND ArticleAmbar RahmanBelum ada peringkat
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- P ('t':'3', 'I':'668014889') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Dokumen5 halamanP ('t':'3', 'I':'668014889') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Ambar RahmanBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5795)
- NIH Public Access: Author ManuscriptDokumen12 halamanNIH Public Access: Author ManuscriptAmbar RahmanBelum ada peringkat
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- PatofisDokumen8 halamanPatofisAmbar RahmanBelum ada peringkat
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- 2012 2013 USFA Age Classification RestrictionsDokumen1 halaman2012 2013 USFA Age Classification RestrictionsAmbar RahmanBelum ada peringkat
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- Chest PainDokumen30 halamanChest PainLamya ZamanBelum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Pathway LeukemiaDokumen2 halamanPathway LeukemiaAmbar RahmanBelum ada peringkat
- How To Critically Appraise A PaperDokumen6 halamanHow To Critically Appraise A PaperAmbar RahmanBelum ada peringkat
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Sci9 q1 Mod1 Respiratory and Circulatory Systems Working With Other Organ Systems Version3Dokumen44 halamanSci9 q1 Mod1 Respiratory and Circulatory Systems Working With Other Organ Systems Version3Raniey MayolBelum ada peringkat
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Simpo 14 Sept 19Dokumen71 halamanSimpo 14 Sept 19Henry SBelum ada peringkat
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Ecg MCQSDokumen2 halamanEcg MCQSZafar Iqbal Manj100% (2)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- AcceptedDokumen28 halamanAcceptedChistian LassoBelum ada peringkat
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Angiography 170411210116Dokumen44 halamanAngiography 170411210116Ndikintum MaciasBelum ada peringkat
- NCP Decreased Cardiac OutputDokumen2 halamanNCP Decreased Cardiac OutputYamete KudasaiBelum ada peringkat
- Heart AnatomyDokumen7 halamanHeart AnatomyArjon BalaBelum ada peringkat
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- Vascular MCQ RoundsDokumen8 halamanVascular MCQ RoundsMohamed Elkhodary100% (1)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Pig Heart DissectionDokumen4 halamanPig Heart Dissectiongerardgil82Belum ada peringkat
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Circulatory System (Heart)Dokumen3 halamanThe Circulatory System (Heart)NinaBelum ada peringkat
- Home Blood Pressure DiaryDokumen2 halamanHome Blood Pressure DiaryCherieBelum ada peringkat
- Entresto in Insuficienta CardiacaDokumen2 halamanEntresto in Insuficienta CardiacaRadu AndreiBelum ada peringkat
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- ECG UworldDokumen4 halamanECG UworldBaebee LouBelum ada peringkat
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1091)
- Start CPR Shout For Help/Activate Emergency Response: Give Oxygen Attach Monitor/DefibrillatorDokumen2 halamanStart CPR Shout For Help/Activate Emergency Response: Give Oxygen Attach Monitor/DefibrillatorFelicia ErikaBelum ada peringkat
- Antihypertensive Drugs.Dokumen35 halamanAntihypertensive Drugs.Abdul WahabBelum ada peringkat
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- BLS ExamDokumen5 halamanBLS ExamAhmed - Sawalha67% (6)
- Generic Name Brand Name Drug Class Mechanism of Action StructureDokumen4 halamanGeneric Name Brand Name Drug Class Mechanism of Action StructurenoelkiddoBelum ada peringkat
- Buerger's DiseaseDokumen41 halamanBuerger's DiseaseMay-ann CabreraBelum ada peringkat
- 30 Dec JoBs BY KHALIQ HASSAN - Watermarked PDFDokumen4 halaman30 Dec JoBs BY KHALIQ HASSAN - Watermarked PDFKamran Talpur100% (1)
- SDL DL BrochureDokumen2 halamanSDL DL BrochureNanda Nabilah UbayBelum ada peringkat
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- New York Heart Association (NYHA) Functional Classification in A Patient With Heart DiseaseDokumen2 halamanNew York Heart Association (NYHA) Functional Classification in A Patient With Heart Diseasemanikchopra111Belum ada peringkat
- Research Poster PresentationDokumen1 halamanResearch Poster Presentationapi-328441669Belum ada peringkat
- Masiag National High SchoolDokumen6 halamanMasiag National High SchoolJESSAN DE PEDROBelum ada peringkat
- Sir ClanDokumen109 halamanSir ClanJames AbendanBelum ada peringkat
- Anti-Arrhythmic Effect of Wild Honey AgainstDokumen10 halamanAnti-Arrhythmic Effect of Wild Honey AgainstMelivea Paez HerediaBelum ada peringkat
- A Case of Hypertension in Diabetes This Case Study Aims ToDokumen4 halamanA Case of Hypertension in Diabetes This Case Study Aims Towalit1101 mukrinin100% (1)
- Anesthetic Management For Woman With Single Ventricle Heart After BCPS Who Undergoes Curretage ProcedureDokumen3 halamanAnesthetic Management For Woman With Single Ventricle Heart After BCPS Who Undergoes Curretage ProcedureAnastasia AngelaBelum ada peringkat
- VastarelDokumen20 halamanVastarelKristen FieldsBelum ada peringkat
- Daftar InventarisDokumen47 halamanDaftar InventarisTri NastitiBelum ada peringkat
- 2.cardiac Output 17Dokumen38 halaman2.cardiac Output 17UmerBelum ada peringkat
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)