Abramson CH 3
Diunggah oleh
bencleeseJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Abramson CH 3
Diunggah oleh
bencleeseHak Cipta:
Format Tersedia
P1: OSO/UKS P2: OSO/UKS QC: OSO/UKS T1: OSO
MCGH209-c03 9-780-7817-XXXX-X MCGH209-Abramson-v1 August 18, 2011 11:11
............................................................................................................................................................................
CHAPTER 3 Dosimetry and Dose Reduction Techniques
Jonathon Leipsic / Brett Heilbron
Radiation Bioeffects
Predicting Risk at a Low Radiation Dose
Patient Dose Exposure Calculations
Comparison of Cardiac CT to Other Imaging Tests
Comparison of Cardiac CT to Catheter Angiography
Growth in Medical Imaging
Making Sense Out of the Stochastic Risks of Medical Ionizing Radiation: Which Organs Are at Risk?
Cardiac CT Dose Reduction Tools
Retrospective Gating
ECG-Gated Tube Current Modulation
Sequential Scanning
Practical Tips for Using Prospective Triggering
High-Pitch Mode
Iterative Reconstruction
Tube Voltage
Tube Current Optimization
Scan Range
Shielding
Patient Preparation
A report on medical exposure to ionizing radiation in the
United States population estimated that the collective ra-
diation dose increased 700% between 1980 and 2006.
1
Computed tomography (CT) had an annual growth rate of
>10% per year and accounted for approximately 50% of
the total collective dose in 2006. The majority of these
CT-related dosesapproximately 65% of the collective CT
doseresulted from CT examinations of the chest, ab-
domen, and pelvis.
1
Continuing developments in CT gantry technology in-
cluding sliprings, multisegmenteddetector arrays, andsub-
second gantry rotation have resulted in significant improve-
ments in image acquisition time, thereby enabling coronary
CTangiography.
2
In2006, cardiac CTwas estimatedtohave
resultedin1.5%of the collective CTdose, but withsignificant
further improvements in scanner technology and greater
adoption of cardiac CT in clinical practice, this number will
almost certainly continue to increase. As such, identifying
and implementing strategies for minimizing radiation ex-
posure associated with this emerging technology is a vital
priority.
Cardiac CT provides excellent cross-sectional anatom-
ical detail of the coronary arteries, the heart, and the sur-
rounding structures. It is unique in its ability to noninva-
sively detect coronary artery atherosclerosis
3,4
and assess
for stenosis.
5
This exceptional anatomical detail and spatial
109
P1: OSO/UKS P2: OSO/UKS QC: OSO/UKS T1: OSO
MCGH209-c03 9-780-7817-XXXX-X MCGH209-Abramson-v1 August 18, 2011 11:11
110 Section I Technology, Technique and Dosimetry
resolution has, however, come at a significant radiation
price. Depending on scanner-specific factors and the spe-
cific acquisition protocol, cardiac CT studies may deliver
doses in excess of 20mSv (millisievert). The PROTECTION
I (Prospective Multicenter Study on Radiation Dose Esti-
mates of Cardiac CT Angiography) study surveyed 50 in-
ternational sites performing coronary CT angiography, and
measured an effective median dose of 11 mSv.
6
Raff et al.
reported both pre- and postradiation reduction strategy im-
plementationdata from12 centers inMichigan. The median
dose prior to initiation of best practice measures was 22
mSv, witha subsequent decrease inradiationdose to 10mSv
following implementation of optimal imaging protocols.
7
Similar to all medical imaging tests that utilize ionizing
radiation, cardiac CT must be performed with recognition
of the overlying principal of ALARA (as low as reasonably
achievable). CT physicians must be aware of their patients
exposure, and should ensure that all dose reduction tech-
niques are in place to strike an appropriate balance between
image quality andpatient dose. Inthis chapter, the history of
radiation dose in cardiac CT will be reviewed; the rationale
for radiation dose concern will be discussed; and, finally, a
review of the current and newly developed dose-reduction
strategies for cardiac CT will be detailed.
RADIATION BIOEFFECTS
Mechanism for Damage
Radiation has the propensity to damage tissue via ioniza-
tion of atoms. Ionizing radiation contains enough energy to
remove tightly bound electrons from their orbits, causing
the atomto become charged or ionized. Cellular interaction
may result in DNA injury directly from a radiation hit or
indirectly via free radical formation.
There are continuous repair mechanisms in place to re-
store the damage. Different cell types demonstrate a range
of sensitivities with rapidly dividing cells more susceptible
to radiation injury. The end result of radiation effects at the
cellular level range from the absence of cellular damage to
cell death in highly sensitive tissues. In the intermediate
range, cellular damage may occur, but successful repair al-
lows for normal function. Onthe other hand, incorrect DNA
repair may result in unstable DNA with abnormal cellular
function and rapid mitosis, which represents the mecha-
nism for radiation-induced malignancy.
Deterministic versus Stochastic Effects
Depending on the time and intensity of exposure, the po-
tential bioeffects of radiation fall into two broad categories.
1. Deterministic effects usually correlate to high levels of
exposure over a short period of time and have two key
features:
a. There is a threshold dose below which deterministic
effects will not be present.
b. The severity of the effect increases with the inten-
sity of exposure. These effects occur at identifiable
thresholds for a specific tissue and include skin
burns or erythema, hair loss, and cataract formation;
however, the extent of exposure in medical imaging
typically does not reach this threshold amount and
is therefore less of a factor in clinical imaging.
8
2. Stochastic effects are relevant to medical imaging and
refer to the induction of malignancy or a genetic de-
fect via prolonged low-level exposure to radiation. Un-
like deterministic effects, no threshold level exists, and
some level of exposure poses a risk that is determined
by a multitude of factors that will be reviewed below.
Carcinogenic Hypotheses
There are two hypotheses germane to any discussion on the
carcinogenesis of medical radiation. The linear no-threshold
hypothesis
9
describes an increasing linear relationship be-
tween radiation dose exposure and malignancy risk. This
hypothesis suggests that risk increases in a linear fashion
without a threshold and that it is reasonable to linearly
extrapolate the risk of malignancy induction from higher
doses to the risk from lower dose exposures. As such, if
radiation exposure doubles, so too does the risk for malig-
nancy. The secondhypothesis is the linear-quadratic theory,
10
which states that the risk of malignancy at lower radiation
doses is so low that it is nearly impossible to quantify, but
it increases quadratically with higher dose exposures.
Radiation Bioeffects:
1. Stochastic effects are relevant to medical imaging and
refer to the induction of malignancy from low-level
radiation exposure. There is no threshold, so some
level of exposure poses a risk.
2. The linear no-threshold hypothesis describes a linear
relationship between radiation dose exposure and
malignancy risk. The risk for malignancy induction
from higher doses can be extrapolated to the risk from
exposure to lower doses. If radiation exposure
doubles, so too does the risk for malignancy.
3. The impact from medical imaging radiation exposure
cannot be distinguished from natural background
radiation exposure.
4. The impact from medical imaging radiation exposure
cannot be distinguished from other carcinogenic
factors.
The Data
There is significant debate within the medical and scien-
tific communities regarding the potential consequences of
ionizing radiation exposure. Data in the Food and Drug
P1: OSO/UKS P2: OSO/UKS QC: OSO/UKS T1: OSO
MCGH209-c03 9-780-7817-XXXX-X MCGH209-Abramson-v1 August 18, 2011 11:11
Chapter 3 Dosimetry and Dose Reduction Techniques 111
Administration (FDA) policy paper suggest that a 10-mSv
CT study may be associated with the development of a fatal
cancer in approximately 1 in 2,000 cases.
9
The data for risk
estimates has largely been based on the Life Span Study
of malignancies associated with radiation exposure in sur-
vivors of the atomic bomb explosions in Japan in 1945.
9
There is, however, no consensus regarding whether the
effects on individuals who experience acute high levels of
heterogeneous whole-body irradiation can be extrapolated
to partial-body exposures of a much lower dose of medical
ionizing radiation.
Using the more conservative linear no-threshold hy-
pothesis, the Biological Effects of Ionizing Radiation (BEIR)
VII report from the National Research Council of the Na-
tional Academies reported the age- and gender-averaged
lifetime risk of death froma malignancy attributable to radi-
ation exposure to be 57.9 per 100 individuals of the general
population per 100 mSv of exposure.
9
Extrapolation of the
data, however, is not straightforward, because it was also
stated that statistical limitations make it difficult to evaluate
cancer risk in humans at doses less than 100 mSv. In indi-
viduals who received less than an estimated lifetime dose
of 100 mSv, the relative risk of developing solid tumors was
not statistically different from those not exposed, despite a
large sample size and relatively long follow-up period (1950
2000).
11
PREDICTING RISK AT A LOW
RADIATION DOSE
Predicting the risk of malignancy at low levels of radiation
is extremely difficult for a multitude of reasons. Malignan-
cies secondary to ionizing radiation are not distinguishable
fromcancers that occur randomly or secondary to other car-
cinogenic agents. Another confounding variable is that all
people are exposed to background radiation secondary to
cosmic radiation, radon, and other low-level sources on the
order of approximately 3 mSv per year.
7,11
These dose expo-
sures are random, and the interaction between photons and
cellular molecules would suggest that even such low levels
of background radiation may result in carcinogenic dam-
age. Given these nonmeasurable confounding variables, it
is extremely difficult to distinguish the impact of a single
exposure to medical imaging ionizing radiation from expo-
sure to natural background radiation.
In an effort to increase our understanding of the ef-
fects of radiation exposure, researchers have investigated
the long-termoutcomes associatedwiththe atomic bombex-
plosions of 1945. This extensively studiedcohort of survivors
represents a unique group due to its size, demographic het-
erogeneity in terms of age and gender, and the absence
of an underlying disease process prior to the exposure to
radiation.
A substantial portion of the 25,000 survivors received
less than 50 mSv, a low level of exposure that approximates
the dose range delivered by multiple chest CTexaminations.
The major negative effect reported in this group was an
increased prevalence of cancer compared to a nonexposed
population. Also, the occurrence of solid cancers had in-
creased in proportion to radiation dose. Thus, while lon-
gitudinal follow-up data from the bombing survivors has
provided informative data, it is important to underscore that
it is difficult to extrapolate findings fromthis incident to the
level of exposure associated with cardiac CT (320 mSv).
Moreover, attempts to make direct comparisons have been
highly controversial and lack widespread consensus.
In addition to studies of the atomic bomb survivors, re-
search examining cancer risk among workers in the nuclear
industry has also provided valuable data. In 2007, Cardis
and colleagues reported findings from a 15-country study of
more than 407,000 radiation workers followed for as long
as 20 years. This is the largest cohort to study the cancer
induction effect of low-level radiation exposure, and it pro-
vided accurate dosimetry and a diverse, multiethnic sample.
The average exposure for eachworker was 19mSv, while
90% of workers received a dose of less than 50 mSv. This
low-level exposure is comparable to the radiation dose asso-
ciated with a cardiac CT examination prior to the initiation
of low-dose strategies. Anexcess relative risk for all causes of
mortality of 0.42/Sv (0.00042/mSv) was reported, as well
as a parallel increase in relative risk as the radiation dose
increased ( p <0.02), indicating a doseresponse effect. The
increased risk in all-cause mortality was mainly due to an
increase in mortality from all cancers, rather than a spe-
cific cancer profile. More remains to be learned concerning
other carcinogenic exposures encountered by the cohort,
including tobacco.
Radiation Exposure Data
Atomic Bomb
r
Increased prevalence of cancer from whole-body
atomic bomb exposure.
r
Occurrence of solid tumors increased in proportion to
radiation dose.
r
Difficult to extrapolate high levels of whole-body
exposure to lower levels of partial-body exposure.
Beir VII
r
Average lifetime risk of death from radiation-induced
malignancy per 100 mSv exposure is 57.9 per 100
individuals.
r
There is no increased risk for malignancy if lifetime
exposure is less than 100 mSv.
Nuclear Industry
r
Low-level radiation exposure comparable to medical
imaging radiation exposure.
r
Increased relative mortality risk of 0.42 per Sv or
0.00042 per mSv.
r
Increased mortality from cancer but confounding
variables, such as tobacco use, need to be evaluated.
P1: OSO/UKS P2: OSO/UKS QC: OSO/UKS T1: OSO
MCGH209-c03 9-780-7817-XXXX-X MCGH209-Abramson-v1 August 18, 2011 11:11
112 Section I Technology, Technique and Dosimetry
PATIENT DOSE EXPOSURE
CALCULATIONS
The parameters by whichradiationdose are measureddiffer
betweenmodalities.
1215
The most commonly acceptedterm
in clinical use is exposure. Exposure refers to the amount of
ionizationproduced inair by a photonof irradiationand can
be measured at the body surface with minimal difficulty. A
means of assessing dose exposure in cardiac CT, however,
is termed effective dose. Effective dose provides an estimate
of the whole-body dose that would be required to provide
the same estimated stochastic risk as the partial-body dose
actually delivered by the coronary CT angiogram.
14,15
Effec-
tive dose is a helpful measure because it allows comparison
of the CT dose to the dose delivered during other medical
examinations. The effective dose is calculated by summing
the absorbed doses to individual organs (e.g., breast, esoph-
agus) weighted for their radiation sensitivity.
13
The standard measurement units for effective dose are
the sievert (Sv) and millisievert (mSv). To calculate the effec-
tive dose, one must calculate the absorbeddose toeachorgan
system multiplied by the organ radiation sensitivity. Given
the markedly asymmetric distribution of radiation during
cardiac CT, this calculation is not routinely performed. A
simpler calculation is performed in which scanner manu-
facturers use dose data derived from measurements made
inheadandbody phantoms to determine a weightedCTdose
index (CTDI) for each CT scanner model at all available se-
lections for tube voltage (kVp, peakkilovoltage), tube current
(mA, milliamperes), and rotation time.
12
The selected pitch
value is then incorporated to yield a CT dose index called
the CTDI
vol
. The scan length is then determined from the
topogram, and the appropriate CTDI
vol
is combined with
the scan length to calculate the doselength product (DLP).
These measurable parameters act as reference standards
for typical dose exposure in CT.
The DLP is a measure of the radiation dose delivered
to the patient during the study. An estimated effective dose
for the specified CT scan can subsequently be derived by
multiplying the DLP value by the normalized effective dose
coefficients for the scanned body part (Table 3-1). These nor-
malized effective dose coefficients are determined by the
radiation sensitivity of the body region scanned. In cardiac
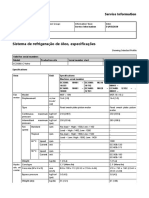
Table 3-1. Coefficients for converting dose-length product
(DLP) to effective dose (E)
Study E/DLP (mSv/mGy cm)
Head 0.0023
..........................................................................................................................................................
Chest 0.017
..........................................................................................................................................................
Abdomen 0.015
..........................................................................................................................................................
Abdomen/Pelvis 0.017
..........................................................................................................................................................
Pelvis 0.019
CT, the accepted standard for effective dose quantification
is 0.017, which when multiplied by the dose length product
in mGy (milligray) cm allows for the calculation of the
effective dose in millisievert.
It should be noted that while 0.017 is the most com-
monly used conversion factor, it is simply the most widely
accepted conversion factor for chest imaging. A formally
accepted conversion factor for cardiac CT is lacking. Many
argue for a higher conversion factor, while a number
of recently published cardiac CT manuscripts, including
PROTECTION I,
6
utilized a lower conversion factor of
0.014. It should be understood that these committee-
determined tissue-weighting factors represent a subjective
balance between cancer incidence, cancer mortality, life
shortening, and hereditary risk. Over time, weighting fac-
tors have been modified and changed, and there is no as-
surance that they will not be modified again in the future
as additional knowledge is gained. Since weighting factors
are calculated based on gender and age averages, they are
applicable to patients of either gender and varying ages, but
the estimated risk of malignancy induction may vary signif-
icantly when applied to an individual patient.
16
While the methods described above are the accepted
means for estimating effective dose in cardiac CT, these are
simply estimates and not direct measures of dose. It is of
great importance to note that all reported radiation doses
for a particular patient are estimates that may be influenced
by numerous assumptions and approximations. To actu-
ally quantify the patients dose exposure, one would need
to make physical measurements with the use of ionization
chambers, lithiumfluoride or calciumfluoride thermolumi-
nescent dosimeters, metal oxide semiconductor field effect
transistors, film, aluminum oxide crystals, or other solid-
state detectors. These are, however, not commonly used in
the calculation of CT-related effective radiation dose.
COMPARISON OF CARDIAC CT TO
OTHER IMAGING TESTS
Effective dose (expressed in sievert) is averaged over age
and gender, and can be utilized to compare procedures that
use ionizing radiation, but should not be employed retro-
spectively to estimate lifetime cancer risk. Individual risk
is best evaluated by determining the mean doses to all ra-
diosensitive tissues of the individual and combining these
with age-, gender-, and organ-specific risk coefficients. As
in cardiac CT, the effective dose is calculated by summing
the absorbed doses to individual organs (e.g., breast, esoph-
agus) weighted for their radiation sensitivity. A list of effec-
tive dose estimates fromother CT imaging tests is included
for comparison purposes (Table 3-2).
There has been much discussion comparing the radia-
tion dose in coronary CT angiography with nuclear myocar-
dial perfusion imaging because these examinations com-
monly are utilized in similar patient populations. Both
P1: OSO/UKS P2: OSO/UKS QC: OSO/UKS T1: OSO
MCGH209-c03 9-780-7817-XXXX-X MCGH209-Abramson-v1 August 18, 2011 11:11
Chapter 3 Dosimetry and Dose Reduction Techniques 113
Table 3-2. Adult effective doses for various CT
procedures (Ref. 14)
Average Values reported
effective in literature
Examination dose (mSv) (mSv)
Head 2 0.94.0
..........................................................................................................................................................
Chest 7 4.018.0
..........................................................................................................................................................
Chest for pulmonary
embolism 15 1328
..........................................................................................................................................................
Abdomen 8 3.525
..........................................................................................................................................................
Three-phase liver study 15
..........................................................................................................................................................
Spine 6 1.510
..........................................................................................................................................................
Neck 3
..........................................................................................................................................................
Calcium scoring 3 1.012
..........................................................................................................................................................
Virtual colonography 10 4.013.2
typically target low- to intermediate-risk patients with atypi-
cal chest pain. Unlike cardiac CT, radiation exposure is not
a preferred parameter for radionuclide radiation measure-
ments, which use internally administered radioisotopes ca-
pable of producing both photon and particulate radiation.
Instead, the number of nuclear disintegrations per second,
expressed in megabecquerels (MBq), is used to quantify the
activity of radionuclides. Organ dose estimates are based
on mathematical models of male and female torsos with
standardized organ size, mass, and geometry.
17,18
These ge-
ometric parameters are combined with the activity, half-life,
distribution, and elimination kinetics of the radionuclide to
calculate dose estimates.
1822
The difficulties related to the changing definitions for
the estimation of a radiation dose in nuclear imaging are
similar to the issues incardiac CT. Consistent dose informa-
tionis not always available. For cardiac radionuclide studies,
the radiation dose estimates listed in the package inserts of
radiopharmaceuticals may not reflect up-to-date informa-
tion. For organ doses, there may be variation between the
values listed in package inserts and the values in current
publications, because the package inserts may not reflect
the newest kinetic data. Package inserts that have not been
updated may report anolder dosimetry concept called whole-
body dose, expressed in units of mGy, because the concept
of effective radiation dose was not widely used when many
of the current radiopharmaceuticals were introduced and
studied.
The whole-body dose represents the total energy ab-
sorbed by the body divided by the mass of the standard
reference human body. The numerical values for whole-
body dose are typically 50% of the value of the effective
radiation dose.
17
In addition, the changes in tissue-specific
weighting factors discussed above may not be reflected in
package inserts. Current updated estimates of organ doses
and exposure for different radiopharmaceuticals have been
reported and allow for comparison of estimated effective
dose for cardiac nuclear imaging to other non-nuclear car-
diac tests (Table 3-3).
Table 3-3. Estimated effective radiation doses from various medical imaging tests (Ref. 21)
Representative Range of reported Administered
effective dose effective dose activity
Examination value (mSv) values (mSv) (MBq)
Chest x-ray PA and lateral 0.1 0.050.24 NA
..................................................................................................................................................................................................................................................................................................................................
CT chest 7 418 NA
..................................................................................................................................................................................................................................................................................................................................
CT abdomen 8 425 NA
..................................................................................................................................................................................................................................................................................................................................
Coronary calcium CT 3 112 NA
..................................................................................................................................................................................................................................................................................................................................
64-slice coronary CTA
Without tube current modulation 15 1218 NA
With tube current modulation
21
9 818 NA
..................................................................................................................................................................................................................................................................................................................................
Dual-source coronary CTA
With tube current modulation 13 617 NA
..................................................................................................................................................................................................................................................................................................................................
Prospectively triggered coronary CTA
22
3 24 NA
..................................................................................................................................................................................................................................................................................................................................
Diagnostic invasive coronary angiogram 7 216 NA
..................................................................................................................................................................................................................................................................................................................................
Percutaneous coronary intervention or radiofrequency ablation 15 757 NA
..................................................................................................................................................................................................................................................................................................................................
Myocardial perfusion study
Sestamibi (1-day) stress/rest 9 1100
Thallium stress/rest 41 185
F-18 FDG 14 740
P1: OSO/UKS P2: OSO/UKS QC: OSO/UKS T1: OSO
MCGH209-c03 9-780-7817-XXXX-X MCGH209-Abramson-v1 August 18, 2011 11:11
114 Section I Technology, Technique and Dosimetry
COMPARISON OF CARDIAC CT TO
CATHETER ANGIOGRAPHY
There is a wide range of reported mean dose exposure
in conventional coronary angiography, from 2.3 to 22.7
mSv.
2229
The United Nations Scientific Committee on the
Effects of Atomic Radiation reports a typical dose value of
7 mSv.
29
However, coronary andnoncoronary interventions
with long procedural and fluoroscopic times candeliver ion-
izing radiation doses three to five times greater than this
cited level. The dose exposure relates to a number of factors
including operator experience, equipment, and the com-
plexity of the procedure.
22,24
The potential for radiation-induced skin injury is one
issue relevant to catheterization procedures, but with CT
or radionuclide imaging. Coronary interventions and cer-
tain electrophysiological procedures can be complex with
long fluoroscopy times often in a few projections. Dose
rates of catheterization laboratory x-ray units are relatively
high, and there have been numerous reported cases of skin
injury. Skin injuries represent a deterministic effect with
a known threshold skin dose and time course, with in-
juries that range from transient erythema to necrosis and
malignancy.
29
For the first time, data have been published showing
lower effective patient dose with coronary CT angiography
than with catheter angiography.
30
Dewey et al. published a
median coronary CT angiography dose of 4.2 mSv com-
pared to 8.5 mSv for catheter angiography, while main-
taining excellent diagnostic performance on a 320-slice
platform. The volume of data illustrating a lower effec-
tive dose from CT will continue to grow with the adop-
tion of new dose-reduction techniques and technological
advancements.
31
GROWTH IN MEDICAL IMAGING
In 2006, approximately 377 million diagnostic and in-
terventional radiologic examinations and 18 million nu-
clear medicine examinations were performed in the United
States.
19,29,32
It has been estimated that the equivalent per-
person annual effective dose from medical procedures has
increased six-fold from 0.5 mSv in 1980 to 3.0 mSv in
2006.
29,33
Also, there has been a 15-fold increase in the
number of radiologic and nuclear medicine imaging proce-
dures performed from 1950 to the present. Approximately
70% of all imaging procedures are chest and extremity ra-
diographs, but these studies only account for 12% of the cu-
mulative radiation dose frommedical imaging, whereas the
impact and contribution of CT to population radiation expo-
sure is much higher and continues to grow with expanding
CT applications (Table 3-4).
34
CT examination frequency
increased worldwide from 1 to 3 procedures per 1,000 indi-
viduals in 19771985, to 35 procedures per 1,000 individuals
in 19972007.
The growth in nuclear imaging and its impact on ra-
diation dose exposure has been less well documented. Car-
diac imaging procedures account for approximately 60%
of all nuclear imaging tests performed in the United States
(Table 3-5). The number of nuclear cardiac studies, includ-
ing positron emission tomography, increased from 1% of
the total nuclear tests in 1973, to 57% in 2005, while other
common nuclear tests remained fairly constant.
15
Table 3-4. Estimated number and collective effective doses of various CT procedures in the United States (Ref. 16)
No of CT scans Percentage of total Percentage of collective
Type of exam in millions no. of CT scans dose from CT scans
Head CT 19.0 28.4 8.7
..................................................................................................................................................................................................................................................................................................................................
Chest CT 10.6 15.9 17.0
..................................................................................................................................................................................................................................................................................................................................
Abdominal pelvic CT 21.2 31.7 48.6
..................................................................................................................................................................................................................................................................................................................................
CTA (Non-neuro, noncoronary) 4.3 6.4 12.8
..................................................................................................................................................................................................................................................................................................................................
Spine CT 4.1 6.2 9.5
..................................................................................................................................................................................................................................................................................................................................
Whole-body screening 0.2 0.3 0.4
..................................................................................................................................................................................................................................................................................................................................
Calcium score CT 0.5 0.8 0.2
..................................................................................................................................................................................................................................................................................................................................
Gated cardiac CT 0.3 0.5 1.4
..................................................................................................................................................................................................................................................................................................................................
Virtual colonography 0.2 0.3 0.5
..................................................................................................................................................................................................................................................................................................................................
Miscellaneous 0.7 1.0 0.8
..................................................................................................................................................................................................................................................................................................................................
Interventional procedures 2.3 3.4 0.1
..................................................................................................................................................................................................................................................................................................................................
Total 63.5 100 100
P1: OSO/UKS P2: OSO/UKS QC: OSO/UKS T1: OSO
MCGH209-c03 9-780-7817-XXXX-X MCGH209-Abramson-v1 August 18, 2011 11:11
Chapter 3 Dosimetry and Dose Reduction Techniques 115
Table 3-5. Estimated number and collective effective doses in diagnostic nuclear medicine procedures in the United States
(Ref. 16)
No. of examinations Percentage of total no. Percentage of collective
Type in millions of procedures dose from procedures
Brain 0.11 <1 0.1
..................................................................................................................................................................................................................................................................................................................................
Thyroid study 0.42 <1 0.2
..................................................................................................................................................................................................................................................................................................................................
Lung scan 0.78 4 0.9
..................................................................................................................................................................................................................................................................................................................................
Cardiac study 10.3 57 85.2
..................................................................................................................................................................................................................................................................................................................................
Gastrointestinal tract study 1.27 7 1.6
..................................................................................................................................................................................................................................................................................................................................
Renal study 0.49 3 0.3
..................................................................................................................................................................................................................................................................................................................................
Bone study 3.62 20 9.3
..................................................................................................................................................................................................................................................................................................................................
Study for infection 0.40 2 0.6
..................................................................................................................................................................................................................................................................................................................................
Tumor study 0.96 2 1.8
..................................................................................................................................................................................................................................................................................................................................
Miscellaneous 0.87 5 N/A
..................................................................................................................................................................................................................................................................................................................................
Total 18.6 100 100
MAKING SENSE OUT OF THE
STOCHASTIC RISKS OF MEDICAL
IONIZING RADIATION: WHICH
ORGANS ARE AT RISK?
As discussed earlier, stochastic effects with radiation-
induced carcinogenesis is the primary concern in medical
imagingradiationexposures.
3436
Ionizingradiationcarries
enough energy to overcome the binding energy of the elec-
trons orbiting atoms and molecules, enabling the creation
of ions. In biological material exposed to ionizing radiation,
the most common scenario is the creation of hydroxyl rad-
icals from x-ray interactions with water molecules. These
radicals then interact with adjacent DNA to cause strand
breaks or base damage. X-ray radiation also can ionize DNA
directly. Most radiation-induced damage is rapidly repaired
by various systems within the cell, but DNA double-strand
breaks are more difficult to repair, and resultant gene fu-
sion, translocation, and mutations are all possible, and have
been linked to malignancy induction.
The organs of particular concern in cardiac CT exami-
nations include the lungs, breasts, and esophagus, because
they are located in the field of view and are subjected to the
highest radiation burden. The risk for breast cancer induc-
tion must be considered in the context of a patients overall
risk for breast cancer development. The relative risk of a
coronary CT angiogram with an historical effective dose of
10 mSv is approximately 1.02 compared to other risk factors,
suchas a positive family history witha relative riskof 2.13.6.
Acomparisonto Japanese atomic bombsurvivors
37
pro-
vides another example of the magnitude of risk imparted by
radiation exposure compared with other known risk fac-
tors. The relative risk of developing lung cancer secondary
to tobacco use ranged from 4.9 in individuals who smoked
115 cigarettes per day to 13.3 in individuals who smoked 25
cigarettes per day.
22
On the other hand, the relative risk of
lung cancer associated with an exposure of 1,000 mSv, or
approximately 50100 coronary CT angiograms, was esti-
mated to be 2.2.
It hadbeenestimatedthat the over 70millionCTexami-
nations performed inthe United States in2007 would even-
tually result in approximately 29,000 malignancies and
14,500 malignancy-related deaths.
33,37
In this analysis, the
most likely sites for cancer induction were lung, colon, and
haematological malignancies such as leukemia. The risk of
cancer induction is greatest in younger females, who have
the added burden of possible breast cancer initiation. Due
to a lack of data, however, the discussionof cancer induction
was not placed in the appropriate context, nor was the diag-
nostic power of CTin altering patient management factored
into the data.
An example would be in the assessment of coronary
artery disease. A 50-year-old male patient has an approxi-
mately 52%likelihoodof developingcoronary artery disease.
If the entire U.S. population of 50- to 55-year-old individu-
als (18.8 million people) were screened for coronary artery
disease with coronary CT angiography every five years until
the age of 70, there would be an estimated increase in the
number of fatal malignancies over the screening period to
42,900.
21,36
While this is a staggering number, it must be
considered within the context of the approximately 350,000
annual deaths in the same cohort from coronary artery
disease.
The issue of malignancy induction from ionizing ra-
diation is a complex and much-debated topic. The linear
P1: OSO/UKS P2: OSO/UKS QC: OSO/UKS T1: OSO
MCGH209-c03 9-780-7817-XXXX-X MCGH209-Abramson-v1 August 18, 2011 11:11
116 Section I Technology, Technique and Dosimetry
threshold hypothesis continues to be questioned
36
because
its supporting data are less than robust. Setting the debate
aside, it remains clear that physicians must selectively uti-
lize this modality when deemed medically indicated, and
efforts to minimize dose exposure while maximizing diag-
nostic efficacy are vital.
CARDIAC CT DOSE REDUCTION TOOLS
Rapid advancements in CT technology have occurred with
improved temporal and spatial resolution, as well as re-
duced acquisition time. Sixteen-slice CT was introduced
in 2002 while 64-slice multidetector CT (MDCT) scanners
with gantry rotation times of 330420 ms were launched
in 2004. The advent of the 64 MDCT has greatly improved
the quality and consistency of coronary artery visualization
and assessment. These systems provide a slice collimation
of 0.50.625 mm with data acquisition in a 612 sec breath
hold.
There have been numerous single-center studies illus-
trating the value of this technology in coronary artery as-
sessment and stenosis exclusion,
3743
all of which have
shown high sensitivities and negative predictive values.
The ACCURACY (Assessment by Coronary Computed
Tomographic Angiography of Individuals Undergoing In-
vasive Coronary Angiography) trial was a multicenter large
cohort that validated the data from these single-center
papers.
44
Further technical advances have since been de-
veloped to improve spatial and temporal resolution, includ-
ing dual-source equipment and high-definition scanners.
Larger detectors have also been released to enable data ac-
quisition in a single heart beat.
Factors affecting the quantity of radiation exposure in-
clude the scanner type (number of detectors, dual versus
single source, dual versus single energy, detector material,
gantry speed, filters and scatter), gating (prospective versus
retrospective), tube voltage, tube current, scan range, acqui-
sition time, pitch and overlap, slice thickness, reconstruc-
tion method (iterative reconstruction versus filtered back-
projection), and patient factors (size and age).
The CT physician must take advantage of image ac-
quisition and dose-reduction tools to ensure that protocols
adhere to ALARA. The following section will detail factors
that affect radiationexposure and howthese parameters can
be altered to obtain diagnostic image quality at the lowest
possible radiation dose.
RETROSPECTIVE GATING
The first and still most commonly used technique for coro-
nary CT angiography is retrospectively gated helical acqui-
sition, which provides the greatest flexibility for image re-
construction owing to the low helical pitch and resultant
data acquisition in multiple phases of the cardiac cycle.
Historically, these scans have used a very low helical pitch
(0.20.5, dependent upon the patient heart rate and single
vs. dual tube) to obtain CT attenuation measurements at all
spatial locations inthe heart inall phases of the cardiac cycle.
The raw scan data and a digitized recording of the patients
ECG signal are stored in the scanner database. This data
can then be reconstructed in a selective fashion at multi-
ple points of the cardiac cycle. Data reconstruction at 510%
intervals allows cine imaging for myocardial and valvular
assessment and ejection fraction quantification. The oper-
ator can also review all of the raw data and select the most
motion-free and diagnostic data set for clinical review. In
fact, if the heart rate and pitch factor are set low enough,
there may be sufficient redundancy in the data to drop an
entire heart beat without missing a segment of the heart
upon image reconstruction. In this situation the data is re-
dundant, which enables ECG editing to remove premature
ventricular contractions to improve image quality inspecific
coronary segments.
Due to redundancy, retrospectively gated coronary CT
angiography provides significant flexibility, but this flexibil-
ity comes at a considerable radiation price. In all helically
acquired CT examinations, radiation dose exposure is in-
versely proportional to pitch. A retrospectively gated coro-
nary CT angiogram with a pitch factor of 0.2 delivers five
times the radiation dose than that of a chest CT with a pitch
of 1, assuming that other parameters such as voltage and
current are the same. Given that initial coronary CT an-
giography data acquisition was almost universally acquired
in a retrospective mode, it is not surprising that early data
suggested median doses ranging up to 32 mSv.
45,46
ECG-GATED TUBE CURRENT
MODULATION
Given the temporal resolution limitations of current CT
technology, even with newer-generation equipment, the
data for coronary artery analysis are best obtained at mid- to
end-diastole (for heart rates <6570beats/min[bpm]).
4749
At higher heart rates there may be merit in data reconstruc-
tion at end-systole due to the preservation of the length
of systole and shortening of diastole at higher heart rates.
Aside from elevated heart rates and arrhythmias, the ma-
jority of data acquired will not be used in coronary artery
analysis and are only helpful if functional assessment is re-
quested. As a result, tube current can be modulated with
the full tube current on for a limited portion of diastole
and reduction of the tube current to 20% for the remain-
der of the cardiac cycle (Figure 3-1A,B). Some systems allow
for further tube current reduction to 4% of the maximum
mA.
49
ECG-gated tube current modulation has been shown
to reduce radiationexposure by approximately 3035%with-
out impairing coronary artery diagnostic image quality
4648
(Figure 3-2). The downside of ECGtube current modulation
is image quality degradation from increased noise during
P1: OSO/UKS P2: OSO/UKS QC: OSO/UKS T1: OSO
MCGH209-c03 9-780-7817-XXXX-X MCGH209-Abramson-v1 August 18, 2011 11:11
Chapter 3 Dosimetry and Dose Reduction Techniques 117
A B
Figure 3-1. Retrospective gating with ECG tube current modulation
(A) Axial image in diastole (70% of the R-R interval) at the level of the right coronary ostium displays
significant degradation of image quality due to cardiac motion. (B) A corresponding axial image at the same
level but in systole (35% of the R-R interval) shows significant improvement in image quality despite
increased image noise from the lower tube current. The diagnostic efficacy of this study was salvaged by the
absence of cardiac motion in systole on this retrospectively gated acquisition.
R
e
t
r
o
s
p
e
c
t
i
v
e
g
a
t
i
n
g
P
r
o
s
p
e
c
t
i
v
e
g
a
t
i
n
g
0
mA
Max
R
e
t
r
o
s
p
e
c
t
i
v
e
g
a
t
i
n
g
w
i
t
h
E
C
G
m
o
d
u
l
a
t
i
o
n
0
mA
Max
0
mA
Max
Figure 3-2. Mechanism of data acquisition with retrospective gating, retrospective gating with ECG
tube current modulation, and prospective gating
During retrospective gating, tube current is at its maximum throughout the cardiac cycle allowing for great
flexibility in data reconstruction, but at a higher radiation dose exposure. In retrospective gating with tube
current modulation, the current is at its maximum during mid-diastole (6080% of the R-R interval) and is
reduced by approximately 80% for the remainder of the cardiac cycle, resulting in a 3035% radiation dose
reduction. Note that tube current remains on throughout the acquisition unlike prospective gating. In
prospective gating, tube current is on for a predetermined segment of the R-R interval but off for the
remainder of the cardiac cycle, resulting in a marked reduction in radiation dose, but little to no flexibility in
image reconstruction.
P1: OSO/UKS P2: OSO/UKS QC: OSO/UKS T1: OSO
MCGH209-c03 9-780-7817-XXXX-X MCGH209-Abramson-v1 August 18, 2011 11:11
118 Section I Technology, Technique and Dosimetry
those phases of the cardiac cycle with lower tube current.
The increased noise at lower tube current does not hinder
cardiac function analysis because the ventricular contours
can still be visualized. Interpretation of the coronary arter-
ies in these phases, however is problematic and often not
diagnostic.
If used appropriately in selected patients (i.e., regular
sinus rhythm, low heart rates), ECG-triggered tube current
modulation will result in diagnostic image quality in almost
all cases, while achieving substantial savings in radiation
exposure.
4648
The benefits of ECG dose modulation depend very
muchonheart rate. At higher heart rates, there is less time to
rapidly alter the tube current, which results in less-effective
dose reduction. Additionally, since reconstruction in late
systole canbe helpful at higher heart rates, a longer peakcur-
rent plateau with a shorter duration of tube current reduc-
tionwill improve the likelihoodof successful coronary artery
analysis, but will result in less dose savings. At higher rates
some centers elect to either extend the time of full tube cur-
rent or forego its use altogether, increasing the relative dose.
Improvements have been made, however, in techniques
and algorithms to enable the use of ECG-triggered tube
modulation for higher and irregular heart rates. ECG-
triggered tube current modulation is recommended in the
majority of retrospectively gated examinations.
4648
SEQUENTIAL SCANNING
Another important strategy for dose reduction is the
prospective ECG-triggered sequential scan mode. This was
historically used for calcium scoring CT studies, but has re-
cently been validated and adopted for use in coronary CT
angiography.
5052
With prospective triggering, data are ac-
quired only during the diastolic phases of the cardiac cycle,
resulting in substantial (up to 90%) reduction in patient
dose (Figure 3-3A,B).
The disadvantage of prospective gating is that images
can only be reconstructed during the prespecified phases of
the cardiac cycle, without data available outside this window
(Figures 3-2 and 3-4). In addition, functional analysis is
not possible because the tube is off for the nonspecified
phases of the cardiac cycle. The prescribed window of data
acquisition can be as narrow as that required to reconstruct
one phase (one-half of the gantry rotation time plus the fan
angle), but this significantly limits the flexibility for image
A B
Figure 3-3. Prospectively triggered, 100 kVp
Prospectively gated image acquisition in a 67-year-old male BMI 27.5 kg/m
2
with a tube voltage of 100 kVp
and effective biologic radiation dose of 0.89 mSv. Note the excellent image quality free of motion enabled by
the patients regular and low heart rate of 58 bpm with fewer than three beats of variability. The (A) right
coronary artery has proximal noncalcified plaque with positive remodelling, and (B) the left anterior
descending is free of disease.
P1: OSO/UKS P2: OSO/UKS QC: OSO/UKS T1: OSO
MCGH209-c03 9-780-7817-XXXX-X MCGH209-Abramson-v1 August 18, 2011 11:11
Chapter 3 Dosimetry and Dose Reduction Techniques 119
Prospectively
Gated Axial
64-MDCT
mA
100%
Prospectively
Gated Spiral
128-DSCT
Prospectively
Gated Axial
256/320 MDCT
mA
100%
mA
100%
Figure 3-4. Prospectively triggered coronary CT angiography performed on different platforms
On a 64-slice MDCT system, the study will typically be acquired over four to six heart beats; however, the
larger detector platforms such as 256/320 MDCT or 128 DSCT enable data acquisition over one to two
cardiac cycles. Note the acquisition time in blue corresponding to the minimum tube time on at a phase of
the cardiac cycle chosen prior to the study. The technique relies on the absence of heart rate variability with
consistent R-R intervals to allow triggering acquisition at the appropriate phase of the cardiac cycle.
Regardless of the platform used, this technique is sensitive to arrhythmias and ectopic beats.
reconstruction. Padding or widening the tube on time or ac-
quisition window (Figure 3-5), has been anecdotally shown
to increase the likelihood of a diagnostic study, although
this has not been studied scientifically. The additional tube
on time also comes with added patient dose exposure.
50,51
Prospective triggering takes advantage of the large vol-
ume detector coverage, which ranges from 40 mm (64
0.625 mm) to 160 mm (320 row detector). With prospec-
tive triggering, the table is stationary during image acqui-
sition and then moves to the next position for the subse-
quent acquisition initiated by the next cardiac cycle. There
is minimal overlap between the scans, even with routine
64-detector coverage, resulting in significant dose reduc-
tion. This technique is reliable, but depends on a regular
heart rate and consistent R-R interval. While the dose-
reduction impact from sequential scanning is impressive,
it should be used only in patients with low and stable
heart rates.
5254
Given the potential benefits of prospective
triggering as a dose-reduction technique, efforts should be
made to ensure tight heart rate and rhythm control.
Prospective gatingis currently inclinical use onall avail-
able MDCT and dual-source computed tomography (DSCT)
cardiac-capable platforms, regardless of the number of de-
tector rows. Prospective gating also reduces dose in non
coronary gatedstudies includingpost-CABG(coronary artery
bypass grafting) scans with a 79.5%reduction from31.2-mSv
retrospective gating to 6.4 mSv.
52
In the emergency department, Shuman and colleagues
reported significant dose reduction in triple-rule-out stud-
ies usingprospective triggeringwiththe meaneffective dose
of 31.8 5.1 mSv (retrospective gating) to 9.2 2.2 mSv
(prospective triggering).
53
In that study, 99.5% of coronary
segments imaged with prospective triggering were evalu-
able, and prospectively triggered images were 2.2 (95% CI,
1.14.5) times as likely to receive high image quality scores
as retrospectively gated images ( p <0.05).
A number of studies have also evaluated the diagnostic
accuracy of prospectively triggered coronary CT angiogra-
phy compared to conventional angiography (CA). Scheffel et
al. studied 120 patients, and reported overall patient-based
0 200 400 600 800 1000 Time msec
Minimum
Acquisition
Window
Padding
200 msec msec 200 0 0
Padding Figure 3-5. Padding
This schematic displays the technique called
padding, or greater tube time on, to enable a
greater number of phases of the cardiac cycle to be
acquired to increase the likelihood of success of a
prospectively triggered study. Additional padding
beyond the minimum acquisition window can be
added in intervals of 25 msec, but increases
radiation exposure in a linear fashion.
P1: OSO/UKS P2: OSO/UKS QC: OSO/UKS T1: OSO
MCGH209-c03 9-780-7817-XXXX-X MCGH209-Abramson-v1 August 18, 2011 11:11
120 Section I Technology, Technique and Dosimetry
sensitivity, specificity, PPV, and NPV for the diagnosis
of significant stenoses to be 100%, 93%, 94%, and 100%,
respectively.
55
Stolzman et al. reported an overall sensitiv-
ity, specificity, PPV, and NPV of 98%, 99%, 95%, and
100%, respectively.
56
Dewey et al. evaluated 320-MDCT
before same-day CAand reported per-patient sensitivity and
specificity to be 100% and 94%, respectively, for CT com-
pared with CA.
57
PRACTICAL TIPS FOR USING
PROSPECTIVE TRIGGERING
The following three criteria should be met prior to initiating
prospective ECG triggering: (1) HR (heart rate) <70 bpm,
(2) HR variability <10 bpm, and (3) no need for functional
data assessment. As a result, aggressive heart rate control is
required for effective utilization of this technique. It is rec-
ommended that even when resting heart rates are between
55 and 59 bpm, patients should receive 12.525 mg of oral
metoprolol.
50
The final decision to be made when performing
a prospectively triggered examination is the amount of
padding or additional tube on-time for the study. Available
padding options withcurrent software ranges from0to 200
msec. In patients with stable heart rates with minimal heart
rate variability, a selection of 0 msec or no padding (no ad-
ditional tube on time) is chosen to minimize dose. As the
heart rate variability increases, padding in increments of
25 msec up to a maximum of 200 msec may be selected.
The use of padding increases the examination effective dose
in a linear fashion from 2.15 mSv with 0 msec of padding
to 7.89 mSv with maximum padding of 200 msec.
50,52
If
heart rate variability exceeds 10 bpm, despite beta blockade,
it is advised to revert to retrospective gating rather than the
prospective technique.
HIGH-PITCH MODE
With the introduction of second-generation dual-source CT
systems, a new fast table speed/high pitch scan mode has
been developed.
5860
Achenbach et al. evaluated this scan
mode in 37 consecutive patients with body weight less than
100kg and lowheart rates (<60bpm).
58
Their data reported
an estimated effective radiation dose of 0.94 0.06 mSv
without degradation of image quality. This technique uti-
lizes two large (64-slice) detectors together with a z-flying
focal spot, allowing a simultaneous acquisition of data in
2 128 slices and a very high pitch factor of 3.2 or 3.4 with
scan initiation at 60%of the R-Rinterval. High helical pitch
on the order of 3.23.4 had not been possible with single-
source scanners. With single-source techniques, the spiral
or helical pitch (table movement per rotation divided by the
collimated beam width) is limited to a maximum of 1.5 in
order to ensure gapless coverage in the z-axis.
A dual-source system configuration is one with two
x-ray tubes and two detectors arranged in a 90-degree
angle allowing high temporal resolution and high-pitch
data acquisition
58,59
(Figure 3-6). The temporal resolution
is achieved because only a 90-degree rotation of the sys-
tem is necessary for image reconstruction, unlike conven-
tional systems that require a 180-degree rotation of the x-ray
gantry. In the high-pitch scan mode, the second tube of
the DSCT systemis used to essentially fill the data gaps, en-
abling a helical pitch factor of 3. Initial experiences with this
novel scan technique would suggest that it is quite robust,
with data supporting its usage in >70% of patients.
59,60
Limitations of this technique are similar to prospective
triggering in that functional data is not obtained, and im-
age acquisition is susceptible to artifacts due to ectopy. At
this juncture, use of a high-pitch spiral technique is limited
to heart rates of less than 60 bpm and has been primarily
used in patients weighing <100 kg. Proof-of-concept trials
were initially performed on the 64-DSCT system; however,
the latest 128-detector row DSCT platform is ideal for em-
ploying this technique. Early clinical results show good po-
tential, and the technique represents yet another method of
performing low-dose cardiac CT.
ITERATIVE RECONSTRUCTION
Image reconstruction for CT has traditionally been per-
formed using filtered backprojection (FBP). FBP is fast and
mathematically simple, thus requiring limited computa-
tional power to perform, but the simplicity results in a noise
penalty.
6163
Iterative reconstruction is currently used in
positron emission tomography and was utilized in some
early CT,
61
but until recently was not available inmodernCT
due to its complexity and the computational power required.
Iterative reconstruction, unlike FBP, reconstructs CT data
sets by fully modeling the systemstatistics. The reconstruc-
tion process is iterative in nature to overcome the mathe-
matical complexity introduced by the added modeling.
6164
Iterative reconstruction does not assume that the measured
signal is free of noise due to x-ray photon statistics or
electronic noise, but rather uses more accurate statistical
modeling during the reconstruction process.
63
This enables
improved noise properties in the reconstructed images,
while maintaining spatial resolution and other image qual-
ity parameters. Asubsequent decrease inimage noise allows
for a substantial reduction in the tube current used during
image acquisition.
The first iterative reconstruction algorithm, Adaptive
Statistical Iterative Reconstruction (ASIR) (GE Healthcare,
Milwaukee, WI), became available for clinical use in 2008
on the Discovery GE HDCT (GE Healthcare, Milwaukee,
WI). Reconstructed images with a high proportion of iter-
ative reconstruction in its current form have a distinct ap-
pearance comparedto traditional FBP, witha different noise
P1: OSO/UKS P2: OSO/UKS QC: OSO/UKS T1: OSO
MCGH209-c03 9-780-7817-XXXX-X MCGH209-Abramson-v1 August 18, 2011 11:11
Chapter 3 Dosimetry and Dose Reduction Techniques 121
75 ms
270 ms
Figure 3-6. High helical pitch flash acquisition
The large detector size and dual-source scanner technology enable the use of a high helical pitch (3.2)
acquisition without loss of data.
texture andsmoother borders, whichhas beendescribedas a
plastic appearance. While pure or 100%ASIR is currently
not considered optimal for image reconstruction,
63
signifi-
cant tube current reduction is possible with 40%ASIRwith
a measured noise reduction of approximately 20%. Because
tube current is related to the square of the noise reduc-
tion, 20% noise reduction with 40% ASIR reconstruction
would theoretically permit a tube current reduction of ap-
proximately 3040%, resulting in a proportional decrease
in the effective radiation dose, without altering image noise
(Figures 3-7, 3-8, and 3-9).
It is possible that the lack of familiarity by the inter-
preting physician with the appearance of pure (100%) ASIR
reconstructed images may result in decreased diagnostic
confidence. Alternatively, it is plausible that current itera-
tions of ASIR may result in excessive smoothing and artifi-
cial lowering of image noise, and therefore reconstruction
that combines ASIR and FBP may be optimal. While early
data is being presented on preferred image quality, further
studies are required to explore the diagnostic accuracy of
varying percentages of ASIR reconstruction compared to
quantitative catheter angiography.
62,63
ASIR is additive to other, more traditional, dose-
reduction algorithms.
63
The use of ASIR in combination
with a reduced tube current, tube voltage of 100 kV, and
prospective ECG triggering with minimal padding has en-
abled image acquisition at a median dose of approximately
1 mSv in nonobese patients, while maintaining image qual-
ity and interpretability.
63
Currently, more complex iterative algorithms, such as
model-based iterative reconstruction, are being developed.
These more advanced iterative reconstruction techniques
have the potential to improve image quality significantly,
but are computationally very demanding and are therefore
not yet ready for clinical use.
TUBE VOLTAGE
Image acquisition is typically performed with a tube volt-
age of 120 kV.
65
A number of publications have proposed
and shown equivalent image quality at a lower tube voltage
in patients with BMI <30 kg/m
2
.
66,67
The potential for data
acquisition at a lower tube voltage has exciting implications
for effective dose, because dose is proportional to the square
of the tube voltage.
66
Estimates suggest that reduction of
tube voltage to 100 kV will decrease effective dose by ap-
proximately 3050%.
66
Data indicates that the resultant in-
crease in image noise from tube voltage reduction is offset
by increased contrast resolution.
6668
Increased intravas-
cular contrast resolution occurs with decreased tube voltage
(100 or 80 kV) because iodine resorption is inversely pro-
portional to tube potential due to the higher degree of the
photoelectric effect at lower energies.
68
P1: OSO/UKS P2: OSO/UKS QC: OSO/UKS T1: OSO
MCGH209-c03 9-780-7817-XXXX-X MCGH209-Abramson-v1 August 18, 2011 11:11
122 Section I Technology, Technique and Dosimetry
A
C
B
Figure 3-7. ASIR versus FBP
Curved multiplanar reformats of the left anterior
descending (LAD) artery reconstructed with (A)
100% FBP, (B) 40% ASIR with 60% FBP, and (C)
100% ASIR. Noise was progressively reduced with
an increasing percentage of ASIR with noise
measurements of (A) 48, (B) 39, and (C) 25. The
noise-reduction properties must be balanced with
the overly smoothed appearance of the pure iterative
image (C).
A review of image quality at reduced tube voltage
showed that while there was a statistically significant in-
crease in image noise in the 100 kV group, the signal-to-
noise ratio as a whole was improved.
66
In this subgroup
analysis of the PROTECTIONI study, a reducedtube voltage
of 100 kV was associated with a 53% reduction in radiation
dose compared to a matched cohort imaged at 120 kV. As
above, image quality inthis cohort sufferedfromanincrease
in image noise, although the benefit of increased intravas-
cular contrast attenuation resulted in similar or improved
overall signal-to-noise ratio.
65
A criticism of most dose-reduction techniques is the
lack of randomized trials evaluating the impact on image
quality. Accordingly, the PROTECTION II study prospec-
tively randomized 400 patients with a body weight <90 kg
to either the standard 120 kV or 100 kV scan protocol.
68
Radiation dose was significantly lower in the 100 kV group
with a 31% dose reduction without significant difference in
qualitative or quantitative image assessment (Figure 3-10).
These data are the first to showin a randomized fashion the
comparability of image acquisition at low tube voltage and
incombinationwithother publisheddata, strongly supports
the routine use of lower tube voltage in nonobese patients.
While no patients in the above-mentioned study were im-
aged at 80 kV, there have been other small nonrandomized
studies that have shown diagnostic image quality and dose
reduction of up to 90% when utilizing 80 kV in patients
with BMI <25 kg/m
2
.
66
With growing evidence that low
kV scanning is appropriate in patients with BMI <30, it is
important to propose a BMI-based standardized scan proto-
col toensure consistent utilizationof low-voltage techniques
(Table 3-6).
P1: OSO/UKS P2: OSO/UKS QC: OSO/UKS T1: OSO
MCGH209-c03 9-780-7817-XXXX-X MCGH209-Abramson-v1 August 18, 2011 11:11
Chapter 3 Dosimetry and Dose Reduction Techniques 123
100
0
200 300 400 500 600 700 800
10
20
30
40
FBP ASIR
Figure 3-8. The impact of iterative reconstruction on image
noise at various tube currents
ASIR-reconstructed images (in darker blue) suffer from less
image noise (y-axis) at all tube current levels (x-axis) compared to
FBP. The horizontal lines denote the difference in noise levels
that can be achieved with a lower tube current using iterative
reconstruction.
TUBE CURRENT OPTIMIZATION
The current generation of cardiac-capable CT scanners has
much greater tube power than earlier CT platforms. This
increased tube power has played an important role in the
advancement of coronary CT angiography. Cardiac proto-
cols generally require greater tube current delivered in a
significantly shorter period of time than is routinely used
for other CTapplications. Maximumpower of the x-ray tube
reaches 100kW, andthe radiationdose may exceed100mGy
if actually used to its maximum capacity. This power is use-
ful for rapid cardiac scanning of individuals with high BMI.
However, if protocols are not individually adjusted, it may
result in needlessly high radiation doses.
Radiation dose can be reduced by use of anatomy-
adapted tube-current modulation. Unfortunately, this tech-
nique, which is quite effective in other CT applications, is
not fully compatible with ECG dose modulation. Instead,
manual selectionof tube current for eachcase onanindivid-
ual basis is essential. The tube current is tailored according
to the patients BMI, chest circumference, estimated mus-
cle, and breast mass. Reliance on a standard CT protocol
without adjusting tube current (mA) leads to an excessive
radiation dose in thin patients and potentially poor image
quality in large patients. A 5 cm difference in thoracic di-
ameter corresponds to a factor of two or more in the dose
required to maintain similar image quality.
69
Jung et al.
reported that the use of weight-adapted mA reduced dose
by 17.9% in men and 26.3% in women, while maintaining
image quality.
70
In high-BMI patients, increasing contrast
volume can be used to offset the expected decrease in coro-
nary artery attenuation.
71
In the PROTOCOL study, LaBounty et al. prospec-
tively evaluated 449 patients in multiple centers undergo-
ing 64-detector coronary CT angiography, and compared
patients pre- (n = 247) versus post initiation (n = 202) of a
standardized protocol that incorporated multiple dose-
reduction strategies
72
. In multivariate analysis, a 20% re-
duction in radiation dose was associated with each 100 mA
reduction in tube current.
SCAN RANGE
The scan range, also known as z-axis coverage, refers to the
cranio-caudal distance of image acquisition. This distance
is directly proportional to the radiation exposure. Radiation
dose increases proportional to the scan range. As such, the
scan range should routinely be limited to the minimum
distance necessary in order to answer the clinical question
posed.
The use of a low-dose scout scan can be used to deter-
mine the minimumscanrange required. The scout image is
used to identify the cranial limit at the tracheal bifurcation,
Filtered backprojection ASIR
Figure 3-9. Iterative image reconstruction
Unlike FBP, system optics and statistics are both
incorporated in iterative image reconstruction,
resulting in more efficient image updating and
noise reduction.
P1: OSO/UKS P2: OSO/UKS QC: OSO/UKS T1: OSO
MCGH209-c03 9-780-7817-XXXX-X MCGH209-Abramson-v1 August 18, 2011 11:11
124 Section I Technology, Technique and Dosimetry
A B
Figure 3-10. Prospectively gated, 80 kVp
A 55-year-old female with a BMI of 22 and scan parameters of 400 mA, 80 kVp, 40% ASIR, and prospective
gating with zero padding yielded a total effective dose of 0.49 mSv. The (A) right coronary artery and (B) left
anterior descending artery are shown with curved multiplanar reformats and are without discernible
stenosis or plaque.
or preferably at the mid-level of the right and left pulmonary
artery and the caudal limit belowthe heart. Relying solely on
the use of anatomic landmarks to set up the CT angiogram
is possible, but runs the risk of an inappropriately long scan
length or alternatively the exclusion of necessary structures.
If a coronary artery calcium score CT is obtained prior
to the CT angiogram, then this noncontrast study can be
used to determine the scan range. The cranial and caudal
limits of the scan range are placed with in a safety distance
of 10 mm from the cranial and caudal ends of the heart and
coronary arteries to accommodate differences in diaphrag-
matic excursion during breath holding. As a result, extrane-
ous data can be limited to approximately 20 mm, resulting
in patient dose reduction. Using retrospectively gated heli-
cal acquisitions, a scan length reduction of 1 cm results in
an approximate dose savings of 1 mSv.
6
Therefore, careful
individualization of scan length, in addition to other scan
parameters, is recommended.
SHIELDING
There has been much excitement in the last few years re-
garding the shielding of particular radiosensitive organs. It
makes intuitive sense to shield radiosensitive organs within
(breast, lung) or outside (thyroid, intestine, gonads) the
scan field by using lead- or bismuth-based protective ma-
terial. Theoretically, this should help minimize radiation
exposure. However, studies performed with both phantoms
and patients suggest that shielding may simply result in an
increase in image noise with only a modest reduction in
radiation exposure for chest CT imaging.
71
Based on the
chest CT experience, radiation exposure to organs outside
Table 3-6. Standardized BMI-based protocol
Body mass index Tube voltage Tube current Gating Padding duration
(m/kg
2
) (kV) (mA) method (msec) Scan length
<25 100 275450 PG
Minimize
..................................................................................................................................................................................................................................................................................................................................
2529.9 100 325550 PG
Minimize
..................................................................................................................................................................................................................................................................................................................................
3033.9 120 375625 PG
Minimize
..................................................................................................................................................................................................................................................................................................................................
34 120 500800 PG
Minimize
Prospective triggering or axial scanning. Note is made that the ability to prospectively gate large patients is equipment dependent.
Minimum tube on time should be used when heart rate < 65 bpm and there is minimal heart rate variability.
P1: OSO/UKS P2: OSO/UKS QC: OSO/UKS T1: OSO
MCGH209-c03 9-780-7817-XXXX-X MCGH209-Abramson-v1 August 18, 2011 11:11
Chapter 3 Dosimetry and Dose Reduction Techniques 125
the scan field during cardiac CT would appear to be negligi-
ble, andthe data supporting shielding is limited.
73
Shielding
for cardiac CT is currently not recommended by the SCCT
working group on the acquisition and performance of car-
diac CT.
48
Until more conclusive data are available, shield-
ing should not be utilized as a routine tool to lower radiation
exposure.
PATIENT PREPARATION
Patient heart rate and heart rate variability during breath-
holding are crucial factors in determining whether some
dose reduction tools can be employed. For instance, a low
(i.e., <6065 bpm) and regular heart rate facilitates the
ability to obtain images using prospective triggering or ret-
rospective gating with ECG dose modulation. Such an ap-
proachwill ensure a loweffective radiationdose. Depending
on the scanner platformand software specifications, higher
heart rates and irregular rhythms may require retrospective
gating without the use of ECG-gated tube current modula-
tion. Heart rates >80 bpm, particularly with irregular R-R
intervals suchas atrial arrhythmias, were relative contraindi-
cations for the examination because of a high incidence of
motion artifacts. However, ongoing hardware and software
advancements, such as dual-source CT, wide-detector scan-
ners, and ECG editing, have permitted successful image
acquisition even with high and irregular heart rates.
74
The
data evaluating the diagnostic accuracy of coronary CT an-
giography in these conditions is limited. As a result, the
limitations regarding higher heart rates are equipment de-
pendent, and scan settings have to be adjusted accordingly.
As a rule, the duration of systole remains relatively con-
stant even at higher heart rates. If prospective triggering is
employed, triggering exposure in end-systole may result in
less motion artifact in patients with higher heart rates. Pre-
mature atrial or ventricular complexes are often more diffi-
cult because they may alter the R-R cycle abruptly and ran-
domly without anticipation. Software developments have
been incorporated into clinical practice that enable PVC de-
tection, allowing the scanner to pause following an ectopic
beat and wait for a more appropriate R-R interval. While
these software algorithms are now available, the efficacy of
these techniques is uncertain and imaging patients with
significant ectopy may still produce artifacts.
CONCLUSION
The last decade has seen dramatic advancements in
CT technology, allowing for noninvasive coronary
artery imaging that was previously considered impos-
sible. While CThas become aninvaluable tool for coro-
nary artery evaluation, it may result in a high radiation
dose burden. Fortunately, unique strategies to mini-
mize radiation dose exposure have been pursued by
vendors and clinicians, and dose levels from cardiac
CT are at historically low levels. The expanding fields
of perfusion and plaque imaging, along with newer
technology utilizing dual radiation sources, threaten
to compromise the gains made in radiation dose re-
duction. While these new applications are exciting,
physicians must remain vigilant to ensure that patient
safety is paramount and that imaging is performed in
accordance with the principle of ALARA at all times.
Dose Reduction Tools
Retrospective Gating with ECG Tube Current
Modulation
1. Tube current can be modulated with the full tube
current on for a limited portion of diastole and
reduction of the tube current to 4% for the re-
mainder of the cardiac cycle.
2. ECG-gated tube current modulation can reduce
radiation exposure by approximately 3035%
without impairing coronary artery diagnostic im-
age quality.
3. ECG-triggered tube current modulationis recom-
mended when performing coronary CTangiogra-
phy with retrospective gating.
Sequential Scanning/Prospective Gating
1. Data are acquired only during the diastolic phases
of the cardiac cycle, resulting in substantial (up to
90%) reduction in patient dose.
2. The table is stationary during image acquisition
and then moves to the next position for the sub-
sequent acquisition initiated by the next cardiac
cycle.
3. The following are recommendations for a suc-
cessful prospective ECG triggered examination:
(i) HR <70 bpm, (ii) HR variability <10 bpm,
and (iii) no need for functional data.
P1: OSO/UKS P2: OSO/UKS QC: OSO/UKS T1: OSO
MCGH209-c03 9-780-7817-XXXX-X MCGH209-Abramson-v1 August 18, 2011 11:11
126 Section I Technology, Technique and Dosimetry
High Pitch Mode
1. This technique utilizes two large detectors to-
gether with a z-flying focal spot, allowing a si-
multaneous acquisition of data in 2 128 slices
with a very high pitch factor of 3.2.
2. The second tube of the DSCTsystemis used to es-
sentially fill the data gaps to enable a high helical
pitch factor.
3. The high pitch mode results in significant dose
savings with sub-mSv effective doses reported.
Iterative Reconstruction
1. Unlike FBP, iterative reconstruction fully models
the systemstatistics and does not assume that the
measured signal is free of noise, but rather uses
more accurate statistical modeling during the re-
construction process.
2. Improved noise properties in reconstructed im-
ages allow for tube current reduction during im-
age acquisition, resulting in decreased effective
radiation dose without altering image noise.
3. Iterative reconstruction, in combination with
other dose-reduction techniques, has enabled im-
age acquisitionat a mediandose of approximately
1 mSv in nonobese patients, while maintaining
image quality and interpretability.
Tube Voltage
1. Compared to a standard 120 kVp protocol, tube
voltage reduction to 100 kVp will decrease effec-
tive dose by approximately 3050%.
2. Resultant image noise from tube voltage reduc-
tion is offset by increased contrast resolution.
3. Increased intravascular contrast resolution oc-
curs with decreased tube voltage (100 or 80 kV)
because iodine resorption is inversely propor-
tional to tube potential due to the higher degree
of the photoelectric effect at lower energies.
4. A voltage of 100 kVp should be considered for
coronary CT angiography in patients with BMI
<30 kg/m
2
.
Tube Current
1. Maximum power of the x-ray tube reaches 100
kW, and radiation dose may exceed 100 mGy if
actually used to its maximum capacity.
2. Reliance on a standard CT protocol without ad-
justing tube current (mA) leads to an excessive ra-
diation dose in thin patients and potentially poor
image quality in large patients.
3. Scanprotocols shouldbe tailoredto the individual
patient.
Scan Range
1. Radiation dose increases proportionally to the
cranio-caudal distance (z-axis coverage) of image
acquisition.
2. A scan length reduction of 1 cm results in ap-
proximate dose savings of 1 mSv inretrospectively
gated examinations.
3. Careful individualization of scan length is neces-
sary to ensure that coronary CT angiography is
performed in accordance with ALARA.
Patient Preparation
1. Ensuring proper patient preparation is necessary
because poor heart rate control andbreathing arti-
facts can significantly degrade image quality and
impair diagnostic accuracy.
2. Proper heart rate control allows for implementa-
tion of dose-reduction tools that include sequen-
tial scanning and ECG tube current modulation.
REFERENCES
1. Mettler FA, Jr, Thomadsen BR, Bhargavan M, et al. Medical radiation
exposure in the United States in 2006: Preliminary results. Health Phys
2008;95:502-507.
2. Budoff MJ, Achenbach S, Blumenthal RS, et al. Assessment of
coronary artery disease by cardiac computed tomography: a scientific
statement from the American Heart Association Committee on
Cardiovascular Imaging and Intervention, Council on Cardiovascular
Radiology and Intervention, and Committee on Cardiac Imaging,
Council on Clinical Cardiology. Circulation 2006;114(16):1761-1791.
3. Leber AW, Becker A, Knez A, Quantification of obstructive and
nonobstructive coronary lesions by 64-slice computed tomography: A
comparative study with quantitative coronary angiography and
intravascular ultrasound. J Am Coll Cardiol 2005;46(1):147-154.
P1: OSO/UKS P2: OSO/UKS QC: OSO/UKS T1: OSO
MCGH209-c03 9-780-7817-XXXX-X MCGH209-Abramson-v1 August 18, 2011 11:11
Chapter 3 Dosimetry and Dose Reduction Techniques 127
4. Motoyama S, Kondo T, Anno H, et al. Atherosclerotic plaque
characterization by 0.5-mm-slice multislice computed tomographic
imaging. Circ J 2007;71(3):363-366.
5. Cheng V, Gutstein A, Wolak A, et al. Moving beyond binary grading of
coronary arterial stenoses on coronary computed tomographic
angiography: Insights for the imager and referring clinician. J Am Coll
Cardiol Img 2008;1:460-471.
6. Hausleiter J, Meyer T, Hermann F, et al. Estimated radiation dose
associated with cardiac CT angiography JAMA 2009;301(5):500-507.
7. Raff GL, Chinnaiyan KM, Share DA, et al. Radiation dose from cardiac
computed tomography before and after implementation of radiation
dose-reduction techniques. JAMA 2009;301:2340-2348.
8. Blakely EA. Biological effects of cosmic radiation: Deterministic and
stochastic. Health Phys 2000;79(5):496-506.
9. Committee to Assess Health Risks from Exposure to Low Levels of
Ionizing Radiation, Board on Radiation Effects Research, Division on
Earth and Life Studies, National Research Council of the National
Academies. Health Risks from Exposure to Low Levels of Ionizing Radiation:
BEIR VII-Phase 2. Washington, DC: National Academies Press; 2006
10. United Nations Scientific Committee on the Effects of Atomic
Radiation (UNSCEAR). Epidemiological studies of radiation and cancer.
Paper presented at 54th session of UNSCEAR; May 29June 2, 2006;
Vienna, Austria.
11. Cardis E, Vrijheid M, Blettner M, et al. The 15-country collaborative
study of cancer risk among radiation workers in the nuclear industry:
estimates of radiation-related cancer risks. Radiat Res 2007;167:396-416.
12. Huda W. Radiation dosimetry in diagnostic radiology. Am J
Roentgenol 1997;169:1487-1488.
13. Brenner DJ. Effective dose: a flawed concept that could and should be
replaced. Br J Radiol 2008;81:521-525.
14. Mettler F, Huda W, Yoshizumi T, et al. Effective doses in radiology
and diagnostic nuclear medicine: a catalog. Radiology 2008;248:254-263.
15. Martin CJ. Effective dose: How should it be applied to medical
exposures? Br J Radiol 2007;80:639-647.
16. Mettler F, Bhargavan M, Faulkner K, et al. Radiologic and nuclear
medicine studies in the United States and worldwide: Frequency,
radiation dose, and comparison with other radiation sources: 19502007.
Radiology 2009;253;520-531.
17. National Council on Radiation Protection and Measurements.
Ionizing radiation exposure of the population of the United States: 2006.
NCRP Report No. 160. Bethesda, MD: National Council on Radiation
Protection and Measurements, 2009.
18. International Commission on Radiological Protection (ICRP).
Radiation dose to patients from radiopharmaceuticals (Publication 53).
Ann ICRP 1987;18(1-4):1-377.
19. Valentin J. Radiation dose to patients from radiopharmaceuticals
(addendum 2 to ICRP Publication 53): ICRP Publication 80 approved by
the Commission in September 1997. Ann ICRP 1998;28:1-126.
20. Higley B, Smith FW, Smith T, et al. Technetium-99m-1,2-bis
[bis(2-ethoxyethyl) phosphino]ethane: Human biodistribution, dosimetry,
and safety of a new myocardial perfusion imaging agent. J Nucl Med
1993;34:30-38.
21. Gerber T, Carr J, Arai A, et al. Ionizing radiation in cardiac imaging.
Circulation 2009;119:1056-1065.
22. Karppinen J, Parviainen T, Servomaa A, et al. Radiation risk and
exposure of radiologists and patients during coronary angiography and
percutaneous transluminal coronary angioplasty (PTCA). Radiat Prot
Dosim 1995;57:481-485.
23. Leung KC, Martin CJ. Effective doses for coronary angiography. Br J
Radiol 1996;69:426-431.
24. Broadhead DA, Chapple CL, Faulkner K, et al. The impact of
cardiology on the collective effective dose in the North of England. Br J
Radiol 1997;70:492-497.
25. Betsou S, Efstathopoulos EP, Katritsis D, et al. Patient radiation doses
during cardiac catheterization procedures. Br J Radiol 1998;71:634-639.
26. Harrison D, Ricciardello M, Collins L. Evaluation of radiation dose
and risk to the patient from coronary angiography. Aust NZ J Med
1998;28:597-603.
27. Neofotistou V, Karoussou A, Hobotesi H, et al. Patient dosimetry
during interventional cardiology procedures. Radiat Prot Dosim
1998;80:151-154.
28. United Nations Scientific Committee on the Effects of Atomic
Radiation, UNSCEAR 2000 Report to the General Assembly, With
Scientific Annexes. Sources and Effects of Ionizing Radiation, New York:
United Nations; 2000.
29. Koenig TR, Wolff D, Mettler FA, et al. Skin injuries from
fluoroscopically guided procedures: Part 1: Characteristics of radiation
injury. Am J Roentgenol 2001;177:3-11.
30. Dewey M, Zimmermann E, Deissenrieder F. Noninvasive coronary
angiography by 320-row computed tomography with lower radiation
exposure and maintained diagnostic accuracy comparison of results with
cardiac catheterization in a head-to-head pilot investigation. Circulation
1009;120:867-875.
31. Labounty TM, Leipsic J, Mancini GBJ, et al., Effect of a standardized
radiation dose reduction protocol on diagnostic accuracy of coronary
computed tomographic angiography. Am J Cardiol 2010;106(2):
287-292.
32. de Gonzalez B, Mahesh M, Kim, KP et al. Projected cancer risks from
computed tomographic scans performed in the United States in 2007.
Ann Intern Med 2009;169:2071-2077.
33. Zanzonico P, Rothenberg LN, Strauss HW. Radiation exposure of
computed tomography and direct intracoronary angiography: Risk has its
reward. J Am Coll Cardiol 2006;47:1846-1849.
34. Tubiana M, Feinendegen LE, Yang C, et al. The linear no-threshold
relationship is inconsistent with radiation biologic and experimental data.
Radiology 2009;251(1):13-22.
35. Pierce DA, Sharp GB, Mabuchi K. Joint effects of radiation and
smoking on lung cancer risk among atomic bomb survivors. Radiat Res
2003; 159: 511-520.
36. Einstein AJ, Henzlova MJ, Rajagopalan S. Estimating risk of cancer
associated with radiation exposure from 64-slice computed tomography
coronary angiography. JAMA 2007;298:317-323.
37. Leschka S, Alkadhi H, Plass A, et al. Accuracy of MSCT coronary
angiography with 64-slice technology: first experience. Eur Heart J
2005;26:1482-1487.
38. Raff GJ, Gallagher MJ, ONeill WW, et al. Diagnostic accuracy of
noninvasive angiography using 64-slice spiral computed tomography.
J Am Coll Cardiol 2005;46:552-557.
39. Leber AW, Knez A, von Ziegler F, et al. Quantification of obstructive
and nonobstructive coronary lesions by 64-slice computed tomography
(A comparative study with quantitative coronary angiography and
intravascular ultrasound). J Am Coll Cardiol 2005;46:147-154.
40. Mollet NR, Cademartiri F, van Mieghem CA, et al. High-resolution
spiral computed tomography coronary angiography in patients referred
for diagnostic conventional coronary angiography. Circulation
2005;112:2318-2323.
41. Ropers D, Rixe J, Anders K, et al. Usefulness of multidetector row
computed tomography with 64 0.6 mm collimation and 330-ms
rotation for the noninvasive detection of significant coronary artery
stenoses. Am J Cardiol 2006;97:343-348.
P1: OSO/UKS P2: OSO/UKS QC: OSO/UKS T1: OSO
MCGH209-c03 9-780-7817-XXXX-X MCGH209-Abramson-v1 August 18, 2011 11:11
128 Section I Technology, Technique and Dosimetry
42. Fine JJ, Hopkins CB, Ruff N, et al. Comparison of accuracy of
64-slice cardiovascular computed tomography with coronary angiography
in patients with suspected coronary artery disease. Am J Cardiol
2006;97:173-174.
43. Nikolaou K, Knez A, Rist C, et al. Accuracy of 64-MDCT in the
diagnosis of ischemic heart disease. Am J Roentgenol 2006;187:111-117.
44. Budoff MJ, Dowe D, Jollis JG, et al. Diagnostic performance of
64-multidetector row coronary computed tomographic angiography for
evaluation of coronary artery stenosis in individuals without known
coronary artery disease: Results from the prospective multicenter
ACCURACY (Assessment by Coronary Computed Tomographic
Angiography of Individuals Undergoing Invasive Coronary Angiography)
trial. J Am Coll Cardiol 2008;52(21):1724-1732.
45. Hausleiter J, Meyer T. Tips to minimize radiation exposure.
J Cardiovasc Comp Tomogr 2008;2(5):325-327.
46. Hausleiter J, Meyer T, Hadamitzky M, et al. Radiation dose estimates
from cardiac multislice computed tomography in daily practice: Impact
of different scanning protocols on effective dose estimates. Circulation
2006;113:1305-1131.
47. Abbara Chair S, Arbab-Zadeh A. Callister TQ, et al. SCCT Guidelines
for the performance and acquisition of coronary computed tomographic
angiography, J Cardiovasc Comp Tomogr 2009;doi:10.1016/j.jcct.
2009.03.004.
48. Halliburton S, Sola S, Kuzmiak S. Effect of dual-source cardiac
computed tomography on patient radiation dose in a clinical setting:
Comparison to single-source imaging. JCCT 2008;2:392-400.
49. Abada HT, Larchez C, Daoud B, et al. MDCT of the coronary arteries:
Feasibility of low-dose CT with ECG-pulsed tube current modulation to
reduce radiation dose. Am J Roentgenol 2006;186:S387-390.
50. Earls JP. How to use a prospective gated technique for cardiac CT.
JCCT 2009;3:45-51.
51. Earls JP, Berman EL, Urban BA, et al. Prospectively gated transverse
coronary CT angiography versus retrospectively gated helical technique:
Improved image quality and reduced radiation dose. Radiology
2008;246(3):742-753.
52. Earls JP, Schrack EC. Prospectively gated low-dose CCTA: 24 months
experience in more than 2,000 clinical cases. Int J Cardiovasc Img
2009;25:177-187.
53. Shuman WP, Branch KR, May JM, et al. Whole-chest 64-MDCT of
emergency department patients with nonspecific chest pain: Radiation
dose and coronary artery image quality with prospective ECG triggering
versus retrospective ECG gating. Am J Roentgenol 2009;192:1662-1667.
54. Husmann L, Valenta I, Gaemperli O, et al. Feasibility of low-dose
coronary CT angiography: First experience with prospective ECG-gating.
Eur Heart J 2008;29:191-197.
55. Scheffel H, Alkadhi H, Leschka S, et al. Low-dose CT coronary
angiography in the step-and-shoot mode: Diagnostic performance. Heart
2008;94(9):1132-1137.
56. Stolzmann P, Scheffel H, Leschka S, et al. Influence of calcifications
on diagnostic accuracy of coronary CT angiography using prospective
ECG triggering. Am J Roentgenol 2008;191(6):1684-1689.
57. Dewey M, Zimmermann E, Deissenrieder F, et al. Noninvasive
coronary angiography by 320-row computed tomography with lower
radiation exposure and maintained diagnostic accuracy: Comparison of
results with cardiac catheterization in a head-to-head pilot investigation.
Circulation 2009;120(10):867-875.
58. Achenbach S, Marwan M, Ropers D, et al. Coronary computed
tomography angiography with a consistent dose below 1 mSv using
prospectively electrocardiogram-triggered high-pitch spiral acquisition.
Eur Heart J 2010;31(3):340-346.
59. Hausleiter J, Bischoff B, Hein F, et al. Feasibility of dual-source
cardiac CT angiography with high-pitch scan protocols. J Cardiovasc
Comput Tomogr 2009;3(4):236-242.
60. Leschka S, Stolzmann P, Alkadhi H, et al. Diagnostic accuracy of
high-pitch dual-source CT for the assessment of coronary stenoses: First
experience. Eur Radiol 2009;19(12):2896-2903.
61. Hara AK, Paden RG, Silva AC, et al. Iterative reconstruction
technique for reducing body radiation dose at CT: Feasibility study. Am J
Roentgenol 2009;193:764-771.
62. Leipsic J, Labounty TM, Min JK, et al. Adaptive statistical iterative
reconstruction: assessment of image noise and image quality in coronary
CT angiography. AJR Am J Roentgenol 2010;195:649-654.
63. Leipsic J, Labounty TM, Heilbron B, et al. Estimated radiation dose
reduction using adaptive statistical iterative reconstruction in coronary CT
angiography: the ERASIR study. AJR Am J Roentgenol 2010;195:655-660.
64. Bischoff B, Hein F, Meyer T, et al. Impact of a reduced tube voltage
on CT angiography and radiation dose results of the PROTECTION I
study. J Am Coll Cardiol Img 2009;2:940-946.
65. Leschka S, Stolzmann P, Schmid FT, et al. Low kilovoltage cardiac
dual-source CT: Attenuation, noise, and radiation dose. Eur Radiol
2008;18:1809-1817.
66. Rehani MM, Bongartz G, Kalender W, et al. Managing patient dose
in computed tomography. Ann ICRP 2000;30(4):7-45.
67. Hausleiter J, Meyer T, Hein F, et al. Prospective randomized trial on
radiation dose estimates of CT angiography in patients scanned with a
100 kV protocol: The PROTECTION II study. Presented at the American
College of Cardiology Annual Scientific Session. MarchApril 2009,
Orlando, FL.
68. Starck G, Lonn L, Cederblad A, et al. A method to obtain the same
levels of CT image noise for patients of various sizes, to minimize
radiation dose. Br J Radiol 2002;75(890):140-150.
69. Jung B, Mahnken AH, Stargardt A, et al. Individually weight-adapted
examination protocol in retrospectively ECG-gated MSCT of the heart.
Eur Radiol 2003;13(12):2560-2566.
70. Tatsugami F, Husmann L, Herzog BA, et al. Evaluation of a body
mass indexadapted protocol for low-dose 64-MDCT coronary
angiography with prospective ECG triggering. Am J Roentgenol
2009;192(3):635-638.
71. Geleijns J, Salvado Artells M, Veldkamp WJ, et al. Quantitative
assessment of selective in-plane shielding of tissues in computed
tomography through evaluation of absorbed dose and image quality. Eur
Radiol 2006;16:2334-2340.
72. LaBounty TM, Earls JP, Leipsic J, et al. Effect of a standardized
quality-improvement protocol on radiation dose in coronary computed
tomographic angiography. Am J Cardiol 2010;106(11):1663-1667.
73. Donadieu J, Roudier C, Saguintaah M, et al. Estimation of the
radiation dose from thoracic CT scans in a cystic fibrosis population.
Chest. 2007;132:1233-1238.
74. Oncel D, Oncel G, Tastan A. Effectiveness of dual-source CT
coronary angiography for the evaluation of coronary artery disease in
patients with atrial fibrillation: Initial experience. Radiology 2007;
245:703-711.
Anda mungkin juga menyukai
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Nwewsletter Spotlight Fall 2008Dokumen16 halamanNwewsletter Spotlight Fall 2008bencleeseBelum ada peringkat
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Med Terminology in A Flash - CardioDokumen66 halamanMed Terminology in A Flash - CardiobencleeseBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Chapter 7. Pharmacokinetics of Oral AbsorptionDokumen28 halamanChapter 7. Pharmacokinetics of Oral AbsorptionbencleeseBelum ada peringkat
- Harrison's Online ContentsDokumen18 halamanHarrison's Online Contentsbencleese0% (1)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Chapter 3. One-Compartment Open Model Intravenous Bolus AdministrationDokumen23 halamanChapter 3. One-Compartment Open Model Intravenous Bolus AdministrationbencleeseBelum ada peringkat
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Chapter 5. Intravenous InfusionDokumen22 halamanChapter 5. Intravenous InfusionbencleeseBelum ada peringkat
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Chapter 1. Introduction To Medical ResearchDokumen10 halamanChapter 1. Introduction To Medical ResearchbencleeseBelum ada peringkat
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- INFLAMMATORY Breast CancerDokumen20 halamanINFLAMMATORY Breast CancerbencleeseBelum ada peringkat
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Basic & Clinical Biostatistics, 4th EditionDokumen6 halamanBasic & Clinical Biostatistics, 4th EditionbencleeseBelum ada peringkat
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Applied Biopharmaceutics & Pharmacokinetics, 5th EditionDokumen1 halamanApplied Biopharmaceutics & Pharmacokinetics, 5th Editionbencleese14% (7)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Medical InterviewDokumen12 halamanMedical Interviewbencleese100% (1)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The TandemheartDokumen6 halamanThe TandemheartbencleeseBelum ada peringkat
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- Lysosomal Disorders - PedsDokumen38 halamanLysosomal Disorders - PedsbencleeseBelum ada peringkat
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- Chemistry Note Form 5Dokumen9 halamanChemistry Note Form 5SofiyyahOpieBelum ada peringkat
- 2017 Alcon Catalogue NewDokumen131 halaman2017 Alcon Catalogue NewJai BhandariBelum ada peringkat
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Bituminus Material PDFDokumen196 halamanBituminus Material PDFSubramanian BalakrishnanBelum ada peringkat
- HKV-8 Valve Catalog SPLRDokumen128 halamanHKV-8 Valve Catalog SPLRCabrera RodriguezBelum ada peringkat
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Assignments CHSSCDokumen7 halamanAssignments CHSSCphani12_chem5672Belum ada peringkat
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- Flexible Perovskite Solar CellsDokumen31 halamanFlexible Perovskite Solar CellsPEDRO MIGUEL SOLORZANO PICONBelum ada peringkat
- 1 s2.0 S0263876299718186 Main PDFDokumen7 halaman1 s2.0 S0263876299718186 Main PDFLeydi PatiñoBelum ada peringkat
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Chapter Test 2nd Quarter.Dokumen5 halamanChapter Test 2nd Quarter.Roziel MontalbanBelum ada peringkat
- Wasif CVDokumen2 halamanWasif CVTalha BaigBelum ada peringkat
- LAB211 Assignment: Title Background ContextDokumen2 halamanLAB211 Assignment: Title Background ContextDuong Quang Long QP3390Belum ada peringkat
- CFR 2011 Title49 Vol3 SubtitleBDokumen626 halamanCFR 2011 Title49 Vol3 SubtitleBmgmqroBelum ada peringkat
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Corrosion Properties of Copper Nickel Alloys in Chlorinated Sea WaterDokumen14 halamanCorrosion Properties of Copper Nickel Alloys in Chlorinated Sea WaterArunBelum ada peringkat
- MATH 320 Numerical Analysis NotesDokumen70 halamanMATH 320 Numerical Analysis NotesWinnie Mutuku100% (1)
- Sistema de Refrigeração de Óleo, EspecificaçõesDokumen2 halamanSistema de Refrigeração de Óleo, EspecificaçõesAlexandreBelum ada peringkat
- Time Value of Money:: "Money Is An Arm or Leg. You Either Use It or Lose It." - Henry FordDokumen33 halamanTime Value of Money:: "Money Is An Arm or Leg. You Either Use It or Lose It." - Henry FordramunagatiBelum ada peringkat
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- High Performance Liquid Chromatographic Technique and Validation For Determination of Favipiravir in Bulk and Tablet FormulationDokumen7 halamanHigh Performance Liquid Chromatographic Technique and Validation For Determination of Favipiravir in Bulk and Tablet FormulationEditor IJTSRDBelum ada peringkat
- Chapter # 1 ChemDokumen3 halamanChapter # 1 ChemRana Hassan TariqBelum ada peringkat
- Web Application Penetration TestingDokumen11 halamanWeb Application Penetration TestingRohitBelum ada peringkat
- Staircase Preliminary Design Based On NBC and IS CodeDokumen10 halamanStaircase Preliminary Design Based On NBC and IS CodeEducation. HubBelum ada peringkat
- Programming in C - CPU Scheduling - Round RobinDokumen3 halamanProgramming in C - CPU Scheduling - Round RobinGenus SumBelum ada peringkat
- Chapter 3.1 - Igneous RockDokumen64 halamanChapter 3.1 - Igneous Rockalvinllp83Belum ada peringkat
- Cisco Ccna Icnd PPT 2.0 OspfDokumen15 halamanCisco Ccna Icnd PPT 2.0 OspfAMIT RAJ KAUSHIKBelum ada peringkat
- Manual HoneywellDokumen36 halamanManual HoneywellVicente RodriguezBelum ada peringkat
- DeskView Client 6 45 enDokumen166 halamanDeskView Client 6 45 enRazvan22081997Belum ada peringkat
- DC Lecture Slides 1 - Information TheoryDokumen22 halamanDC Lecture Slides 1 - Information TheoryG VenkateshBelum ada peringkat
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Mesh Based Multicast Routing ProtocolDokumen10 halamanMesh Based Multicast Routing ProtocolArul JothiBelum ada peringkat
- Completation Inteligent RevistaDokumen9 halamanCompletation Inteligent RevistaGabriel Castellon HinojosaBelum ada peringkat
- Seafloor Spreading TheoryDokumen16 halamanSeafloor Spreading TheoryMark Anthony Evangelista Cabrieto100% (1)
- Project Robot ArmDokumen62 halamanProject Robot ArmTechs Solutions RobotsBelum ada peringkat
- August 19-23 Lesson PlanDokumen1 halamanAugust 19-23 Lesson Planapi-282162606Belum ada peringkat
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDari EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDPenilaian: 5 dari 5 bintang5/5 (3)