Patient Safety
Diunggah oleh
Jesse M. MassieDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Patient Safety
Diunggah oleh
Jesse M. MassieHak Cipta:
Format Tersedia
Patient Safety: Mindful, Meaningful, and
Fulfilling
STEVEN C. WINOKUR, M.D., AND
KAY J. BEAUREGARD, R. N.
S U MMA R Y Five years after the landmark report of the Institute of Med-
icine To Err Is Human (Kohn, Corrigan, and Donaldson 2000), many are
asking, "Is U.S. healthcare safer?" A number of articles addressing this
question have been written, interviews with nationally recognized patient
safety leaders have been published, and governing boards of many health-
care organizations are examining reports of care provided by their institu-
tions. Robert M. Wachter, writing in the November 2004 issue of Health
Affairs, concludes that, "At this point, I would give our efforts an overall
grade of C-H, with striking areas of progress tempered by clear opportunities
for improvement."
We describe in this article the pursuit of a culture of safety at William
Beaumont H ospital in Royal Oak, Michigan. Our experience has offered us
the opportunity to ponder a number of key questions: H ow does leadership
guide an organization toward a culture of safety? Does culture truly drive
behavior, or is it really the reverse? H ow can a culture of safety be measured
or observed? What levels of resources and commitment are required for
success? Is safety all about systems and processes, or are core values also
involved? What role does the patient play in ensuring safe care? We attempt
to offer guidance, and share lessons learned, for each of these important
questions.
Steven C. Winokur, M.D., is medical di rector of quality i mprovement and chief
patient safety officer and Kay J. Beauregard, R.N., is admi ni strati ve director for
quality, safety, and accreditation at Wi l l i am Beaumont Hospi tal in Royal Oak,
Mi chi gan.
S T E V E N C . W I N O K U R A N D K A Y ) . B E A U R E C A R D I 7
Patient safety cannot he
separated from employee,
visitor, and caregiver
safety.
Steve,
Our industry and our hospital cannot afford
not responding to this study /To Err Is
Human] and making the necessary invest-
ments to assure patient safety. While Beau-
mont Hospital practices many ofthe
recommendations already, w e still make mis-
takes that cost us millions in dollars and
tragedies in human terms. If! had to make
one investment in 2000 it w ould b e in physi-
cian order entry! Thanks for the material b ut I
have a copy o/To Err Is Human on my desk.
Ken
This note was written to Steven
Winokur, M.D., on December 27 of J999
by Kenneth Matzick, executive vice presi-
dent and chief operating officer of Beau-
mont Hospital in Royal Oak, Michigan.
He wrote in response to a note from Dr.
Winokur one week prior, which provided
him the executive summary
ofthe Institute of Medicine
(IOM) report To Err Is
Human (Kohn, Corrigan,
and Donaldson 2000). Dr.
Winokur had written, "I
would appreciate your thoughts on this,
as many of these recommendations
would require significant commitment
and resources."
At the beginning of 1 999, Beaumont
began a comprehensive one-year review
of its quality management program. A
strong infrastructure of multidisciplinary
peer review and administrative and per-
sonnel support for numerous quality
improvement teams, database manage-
ment, and concerned leadership had been
in place for at least two decades. Acco-
lades were accumulating, such as reviews
received "with commendation" from the
Joint Commission on Accreditation of
Healthcare Organizations (JCAHO),
inclusion in the top-ioo-hospitals lists
and US New s and World Report rankings,
and independent survey best-hospital rat-
ings for the southeast Michigan region.
Yet it was clear to our leadership that a
great deal of work remained to be done to
achieve the level of performance excel-
lence that we feel our patients deserve.
Perhaps what made us somewhat unique
in our ability to respond to the IOM
report was that we were ready to assume
the challenges it presented to all of health-
care: how many hospital executives had a
copy of To Err Is Human on their desk in
December 1 999?
Although we had already pursued and
accomplished many ofthe IOM recom-
mendations, we had not actively nor for-
mally used the term patient safety to
describe our quality management or per-
formance improvement activities. There-
fore, our initial efforts were to define
patient safety; communicate to and edu-
cate our entire organization about patient
safety; and develop an effective, high-
profile infrastructure supported by
updated and yet-to-be-developed patient
safety policies. One of our very first steps
was a presentation to our Board of Direc-
tors about the IOM report in early
2000what it meant and where we
stood. In rapid sequence came our Patient
Safety Vision, a Corporate Performance
Improvement and Patient Safety Plan, the
Corporate Patient Safety Council and
Patient Safety Cabinet, and the appoint-
ment of a Chief Patient Safety Officer at
each of our two hospital divisions.
THE ESSENCE OF PATIENT SAFETY
what is patient safety all about, and how
can an organization be transformed
toward its pursuit?
l 8 F R O N T I E R S O F H E A L T H S E R V I C E S M A N A G E M E N T 2 2 . ' 1
Human factors, high-reliability orga-
nization, error, injury, disclosure,
empowerment, communication, team-
work, hierarchy, just culture, nonpuni-
tive culture, nurse-to-patient ratios, duty
hours, work shifts, mindfulness, legibil-
ity, computerized order entry, IHI,
NPSF, ISMP. ECRI, JCAHO, CMS,
AHRQ, NQF,' the Leapfrog Group, sim-
ulation, learning organization, standard-
ization, simplification. Six Sigma, lean
thinking, fiow, throughput, handoffs.
Internal Bleeding,'' "The Bell Curve,"' pay
for performance, compensation, litiga-
tion, risk management, organizational
ethics, mission, apology, latent errors,
active errors, Swiss cheese, sentinel
events, incident reports, Codman award,
Eisenberg award. Quest for Quality
award, and on and on; With all of these
terms, do we really understand the
essence of patient safety? At Beaumont,
we believe that we do.
The words of former U.S. Secretary of
the Treasury Paul H. O'Neill, in his
remarks to the National Academy of Pub-
lic Administration's Strategic Human
Resources Conference at the University
of Maryland in September 2002, refiect
our sentiments eloquently;
In a truly great organization, every person
can answer "yes" to the following three
questions:
First, "[A]re you treated with dignity
and respect every day by everyone?"
Second, "Do you have the tools to
make a contribution to your organization
that gives meaning to your life?"
And third, "Does someone recognize
the contributions you make?"
We must strive toward that ideal in
public service. When government employ-
ees can answer "yes" to these questions.
they are in a position to achieve their
potential on the job, and in their lives.
Let me give you an example of how I
have approached the first question, of
treating people with dignity and respect.
When I became the CEO of Alcoa, my first
priority was to improve safety for all our
55,000 employees. Not just improve itI
wanted to make it perfect. I didn't have a
profit calculation in mind1 just knew it
was the right thing to do. Workplace safety
is a key element of treating people with
dignity and respect.
At its very core, patient safety is about
dignity and respect and cannot be sepa-
rated from employee, visitor, and care-
giver safety. Safety is safety. Period.
Consider the "straightforward" issue
of handwriting legibility. If we were to
view legible handwriting as indicative of
our dignity and respect toward others,
would hospitals be able to tackle this
problem today, rather than waiting for
technologies to mature and allow for uni-
versal electronic health records? In other
words, if we considered that an illegible
order to another caregiver is one that
could compromise his or her ability to
properly treat a patient on our behalf,
that we have placed both the caregiver
and patient at risk, could we correct this
problem now? We believe that the
answer is yes.
Leadership at AM Levels
At Beaumont Hospital, we have actively
engaged leaders, managers, and care-
givers at all levels ofthe organization to
join in the pursuit of safety in all areas.
In many cases, leadership for the pursuit
of safety has emerged simply by encour-
aging and empowering our staff. Our
leadership for safety does not just come
m
H
C
m
S T E V E N C . W I N O K U R A N D K A Y J . B E A U R E G A R D I 9
Will y o u kno w a
culture of safety when
you see it?
from the chief executive officer (CEO)
and other executives; it truly comes from
many managers and frontline staff as
well. We have provided tools and oppor-
tunities that allow every person in our
organization the chance to make a contri-
bution that is meaningful to them and
results in a safer environment for all.
Resources and Education
Ofcourse, resources and expertise are
also required to ensure a safe environ-
ment. The desire to create a culture of
safety is not in itself sufficient. Here
again we have witnessed an incredible
amount of activity. Beaumont University
is our hospital's center for edu-
cational programs, which is
intended to support leadership
and management development
as well as staff education. Our
chief learning officer worked closely with
the authors to develop basic performance
improvement and patient safety educa-
tional programs in 2000. As our organi-
zation has evolved toward a culture of
safety, we are seeing educational pro-
grams about safety arise from a variety of
interested departments, teams, and
impassioned individuals. Self-learning is
in abundance, with well more than a core
nucleus of our staff as well as several
physicians showing interest in state-of-
the-art methods such as Six Sigma and
human factors engineering. Similarly,
safety is prominent in all budgetary and
resource allocation decisions.
CULTURE OF SAFETY
Will you know a culture of safety when
you see it? Will you sense something
markedly different about the environment
and the interactions ofthe people? Does
culture change all at once, or gradually?
Observable Behaviors
Our experience indicates that a culture of
safety is demonstrated by observable
behaviors. It can be heard, seen, and intu-
ited day in and day out. We confirm a cul-
ture of safety by observing behaviors such
as the following:
Physicians compassionately disclosing
and discussing errors with patients
Managers genuinely thanking staff for
reporting errors
Nurses routinely repeating back verbal
medication orders
Educators training teams using a
human simulator
Patient transporters checking identifi-
cation wristbands before taking a
patient to a scheduled exam
Receptionists and clerks asking each
patient to affirmatively state his or her
name rather than accepting a passive
nod of agreement
- Staff using standardized communica-
tion techniques when a patient is
handed off from one care setting to
another
Staff ascertaining that the oxygen in
the portable tank is adequate for a
round trip to an ancillary department,
using checklists and guides developed
by our clinical engineers
These are merely a few ofthe behav-
iors that we see throughout our large,
complex organization each and every
day; they are telltale signs of our safety
culture.
Behaviors of administrative- and man-
agement-level staff such as the following
also affirm Beaumont's culture of safety:
Our multidisciplinary root cause
analysis teams seek patient and family
2 0 F R O N T I E R S O FH E A L T H S E R V I C E S M A N A G E M E N T 2 2 : 1
input to ensure full understanding of
errors that have occurred.
Our established patient care commit-
tees discuss patient safety at each and
every meeting.
Our financial leaders support a dedi-
cated budget source for immediate
remediation of safety issues.
Human factors analysis is routinely
applied to equipment design and
process improvement.
Ad hoc groups throughout our organi-
zation emergeseemingly on their
ownto discuss patient safety oppor-
tunities and solve problems.
One current example of our multidisci-
plinary, state-of the-art approach to real-
world patient safety opportunities
involves analysis of best practice in
telemetry monitoring. We are taking steps
to optimize communication between our
central telemetry monitors and our
nurses at the bedside. We are also
engaged in human factors research
whereby our clinical engineers measure
responsiveness of technicians following
8- and 12-hour shifts through the use of
simulation and gaming techniques. When
completed, our research may well result
in improved telemetry monitoring prod-
ucts, as well as improved processes within
our hospital.
ORGANIZATIONAL COMMITMENT
Our organizational leadership demon-
strates that patient safety is a top priority
by communicating this to employees and
medical staff at all levels. They actively
recruit staff and physicians for participa-
tion on patient safety committees and
provide staff, physicians, and manage-
ment the opportunity to enroll in a com-
prehensive series of educational classes
and seminars about the science and prac-
tice of safety. Department manager and
supervisor meetings serve as great oppor-
tunities to communicate about ongoing
patient safety initiatives, increase their
visibility, and establish management's
expectations of staff.
Hardwired for Safety
A great many initiatives and programs
are in place up and down the organiza-
tion to fully institutionalize the culture
of safety at Beaumont. Full involvement
of our physicians, nurses, staff, and
patients and their families is integral to
the success of our program. Stakehold-
ers are actively involved through educa-
tion, including shared feedback from
surveys, hotlines and process owner
reports, involvement in patient safety
work groups, and a supportive environ-
ment for those interested in their own
professional grovi^h in this field. Medical
chiefs routinely dedicate agenda time to
patient safety at medical staff depart-
ment meetings. Appointed patient safety
leaders visit every clinical department
and ambulatory site at least annually to
conduct executive rounds. Managers are
expected to discuss patient safety at staff
meetings and as part of in-service train-
ing. Patient safety educational tool kits
with sample agendas, video vignettes,
and case studies have been made avail-
able to all managers.
Readily Available Documents and
Literature
All medical staff and hospital employees
can readily access an abundance of
patient safety information through the
internal web site that contains resources
such as our Patient Safety Vision, our
Corporate Performance Improvement
H
C
m
S T E V E N C,W I N O K U R AND K A Y j . B E A U R E C A R D 21
and Patient Safety Plan, many relevant
patient safety pohcies, and a long list of
internal patient safety expert contacts
and external reference web sites. Our
intranet allows for simplified enrollment
for numerous patient safety courses, as
well as access to printed course materi-
als. Frequent articles pertaining to
patient safety are published in the
employee, physician, and management
newsletters. If one has any doubt as to
the maturity of our evolving safety cul-
ture, just imagine reading about such
topics as situation awareness in our hos-
pital newsletters.
INFRASTRUCTURE
The culture of safety is diffused through-
out all sites and integrated through the
system through a variety of pathways.
. , - Failure mode and effects
Encourasine patient safety , ^ j . ,
** ** '^ ' ' analyses are studied by
Storytelling is effective in
promoting candid group
dis cus s ion.
groups with broad repre-
sentation from a variety of
disciplines and hospital
units. Intensive assess-
ments or sentinel event recommenda-
tions are shared across the organization
so that the lessons learned may be
applied in all departments with similar
risk environments. Variance reports from
all organizational settings, both inpatient
and ambulatory, are aggregated and ana-
lyzed in one centralized patient safety
database.
At the onset of our organizationwide
education plan, all administrators, man-
agers, and medical staff leaders attended
a three-hour patient safety overview
course offered through Beaumont Uni-
versity. Subsequently, new managers are
expected to take this course as a core lead-
ership requirement. New employees are
introduced to patient safety goals at their
initial orientation. Similarly, newly
appointed physicians are introduced to
our patient safety program at the time of
their acceptance to the medical staff.
These educational programs and require-
ments ensure a consistent level of patient
safety education for all caregivers
throughout the organization. Our
brochure "First, Do No Harm: A Guide to
Patient Safety for Beaumont Employees"
is provided to all employees to facilitate
learning and discussion of patient safety
(Exhibit I, pages 29-30).
REPORTING AND FEEDBACK
Potential safety concerns are identified
through various data collection sources:
executive patient safety rounds; patient,
employee, and medical staff surveys; risk
management cases; root cause analyses;
variance/sentinel event reports; anony-
mous employee or patient reports via an
internal hotline (i-SAFE); and informal
communications at manager meetings,
among other avenues.
A supportive environment for error
reporting is demonstrated by the way that
we respond when errors are reported.
Process owners (designated recipients of
variance reports) send thank you notes to
individuals who submit reports. An
excerpt from a recent note sent by our
medical equipment process owner illus-
trates this nicely.
Vicki,
Glad to hear n o on e w as hurt. I ' ll look f or-
w ard to s eein g the varian ce. Y ou are probably
already aw are, but let me take the opportu-
n ity to rein f orce the n on pun itive n ature of
varian ces an d the dedication Beaumon t
exhibits to quality. Som,e of our bes t quality
w ork has res ulted f rom in comin g varian ce
2 2 F R O N T I E R S O F H E A L T H S E R V I C E S M A N A G E M E N T 2 2 : 1
reports. We'll look forward to working together
on root causes and potential quality improve-
ments.
Regards,
Steve
Recognition programs, such as WOW
cards (redeemable for Si.oo at our gift
shop, coffee shop, and cafeteria), are
given to staff who enthusiastically partici-
pate in patient safety rounds. Beaumont's
Corrective Action Policy recognizes the
inevitability of human error and the need
for managers to avoid inappropriate puni-
tive responses to errors. The human
resources department provides education
and support to managers to ensure that
this policy is carried out as intended. A
customized checklist is used to make cer-
tain that evaluation of employee errors is
performed from a process-focused per-
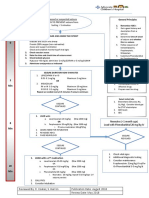
spective (Figure i).
Support services are available to all
employees and medical staff who may
need assistance to overcome feelings of
grief, frustration, anger, embarrassment,
guilt, or loss of confidence that may occur
as a result of clinical error. Encouraging
patient safety storytelling is effective in
promoting candid group discussions.
Staff who see a supportive environment
and learn about genuine process
improvement as a result oftheir reports
continue to report and encourage others
to do so as well.
Measurement of patient safety
progress is accomplished through a vari-
ety of mechanisms. Direct feedback to
senior leadership is encouraged, from
frontline care providers, support staff,
and patients themselves. Employee and
FI GURE 1. Checklistfor Evaluating staff Errors
Objective Review: When reviewing a situation to determine if action should be taken, recog-
nize that human error may occur. Review the procedures, processes, and equipment
involved in the error to determine if the error is process or procedure related. It is important
to remove personal emotions and biases from consideration and use sound, logical thinking
when determining the course of action to take.
What is your process or procedure?
How was staffing that day?
- Were there any unusual circumstances or events that happened that day?
Was the employee performing within the scope of his or her position?
Does the employee have the necessary tools and equipment to effectively perform his or
her job?
Did the employee make a mistake?
Have the procedures and/or protocols been clearly communicated?
What does the employee's performance history or work record look like?
How frequently does the employee make errors?
What was the impact ofthe error?
What is the error rate of this procedure?
m
H
C
S T E V E N C . W I N O K U R A N D K A Y J . B E A U R E G A R D 2 3
A just culture had
become a way of life at
our hospital.
physician surveys assess patient safety
culture, teamwork and communication,
willingness to reports errors, adequacy of
education, and leadership responsiveness
to identified patient safety risks. Areas for
improvement are prioritized
and championed by key lead-
ers in the organization.
Progress is tracked through
the hospital's performance
improvement steering committee, com-
posed of senior hospital and medical staff
leaders. Well-defined patient safety met-
rics are reported monthly to the CEO and
board of directors.
ANALYSI S OF DATA
Analyses of data from variance reports,
process owner reports, patient safety
rounds, sentinel event reports, i-SAFE
hotline calls, patient safety surveys, risk
management cases, and patient feedback
are used to prioritize patient safety initia-
tives.
An innovative approach to analyzing
key processes is illustrated by our variance
reporting methodology. At the onset ofthe
reengineering of our variance reporting
process, common process issues were
identified by an analysis of historical hos-
pital variance report data. Once the key
processes of interestpatient falls, med-
ication events, equipment events, and so
forthwere determined, a process owner
was recruited for each key process. A
management engineer, administrator, and
physician champion were identified to
support each process owner, thus develop-
ing process owner teams. A standardized
method allows all process owners to
assess, track, and analyze the data in a
similar fashion. The analysis strives to
identify root cause process issues that
may include the following:
Patient identification
Staffing levels
Availability of information
Physical environment
Patient assessment
Equipment-related processes
Orientation and training of staff
Communication among caregivers
Data from all process owner reports
are aggregated each calendar quarter so
that both individual processes and the
overall organizational process can be ana-
lyzed and serve as teaching aides.
TI PPI NG POI NT
An error occurred at Beaumont. Correc-
tive (disciplinary) action was being consid-
ered for several staff members who had
been involved in the error. During the
case review session, the incident was
determined to have resulted from a sys-
tem failure and not from an individual
performance issue. Over a long period of
time, safety practices in the failed system
had eroded, and the procedures that
resulted from that erosion became accept-
able in the hospital culture. Written proce-
dures had not been followed for some
timeemployee "work-arounds" pre-
vailed. Nothing bad had happened until
this incident. The employees involved in
this event were "good, conscientious,
long-term" employees. Were they at fault?
Or was our culture at the time the real
basis for this event?
Our analysis: If these employees were
at fault, then the educator who trained
them was at fault; their peers who vali-
dated the process by acting in the same
manner each day were at fault; and their
manager, their director, their administra-
tor, and the people writing this article
were all at fault for allowing this process
2 4 F R O N T I E R S O F H E A L T H S E R V I C E S M A N A G E M E N T 2 2 : 1
to break down. These good, conscientious,
long-term employees were part of a faulty
process and part of a culture that did not
adequately emphasize safety.
The use of corrective action to disci-
pline these employees was determined to
be unnecessary. This decision proved to
be an excellent educational case study, as
staff witnessed firsthand the leadership's
commitment to sound patient safety prin-
ciples. The grapevine is not to be underes-
timated. As a resuh of this case, the
informal communication network worked
at a rapid pace. Nearly all management
staff, and many employees, quickly
learned that there was a new approach to
patient safety; a just culture had become a
way of life at our hospital.
PUTTING THE "PATIENT" IN
PATIENT SAFETY
Organizations that proactively teach
patients how to be partners in safety have
a win-win situation. However, it is essen-
tial to create a culture of patient safety
within the organization prior to assuming
that staff will embrace patients as partners
in care. Staff must be equipped with the
appropriate skills and practice in a sup-
portive culture before they will readily
accept the concept of including the patient
as a partner in care. Beaumont's strate-
gies to "put the patient in patient safety"
include the following:
Design of all patient educational mate-
rials with an emphasis on patient
safety
Patient interviews by senior leadership
during executive safety rounds
Inclusion of patient safety topics in
community education classes
Encouragement for employees to seek
new opportunities to involve patients
Fundamental to our efforts to involve
our patients and their family members is
our "Partners in Safety" brochure (Exhibit
2 , pages 31-32 ). This brochure is provided
to every inpatient and every surgical
patient and is made readily available in all
ambulatory settings. We also actively seek
opportunities to involve patients and their
families in several key processes of care,
such as the following:
The patient identification process
The handoff/transfer process
The surgical site-marking process
The prevention of infant abduction
The medication administration
process
Infection control
The success of these strategies has
been measured through specific ques-
tions on the Patient Safety Department
Assessment tool completed by manage-
ment staff We are pursuing several addi-
tional strategies to further involve the
patient in safety. These include a patient
orientation video and online educational
tools and reference web sites.
GENUINE CHANGE
oft he many examples of genuine change
toward patient safety that we have seen, a
few highlights are featured here.
Patient Identification
Improvement of our patient identification
process was one of our most important
initial goals. Numerous interventions and
process changes were made to allow us to
come as close to perfection as possible in
this critically important step. We stan-
dardized our approach to patient identifi-
cation across the organization, including
standardization ofthe wristbands, adding
m
S T E V E N C. W I N O K U R AND K AY J . B E A U R E C A R D 2 5
Waiting for ne w
te chnologie s and not
addre ssingflaw s in
curre ntly w ritte n
me dication orde rs is not
acce ptable in our culture .
forcing functions'* and point-of-care
reminders, and working with vendors and
suppliers to improve some ofthe related
patient identification products. Bar code
technologies were introduced to meet
selected needs. A consistent role for the
patient is included as part ofthe multi-
check system.
The impact of these process changes
has been dramatic, as evidenced by the
data from Beaumont's variance report
database, which shows that the number
of incidents related to patient identifica-
tion has fallen sharply. We have cele-
brated this success with our employees
through internal recognition programs.
Medication Safety
Our medication safety processes have
been similarly strengthened. Fundamen-
tal to achieving optimal outcomes for our
patients is providing medications in a
safe manner. Opportuni-
ties for improvement are
learned from internal data
sources as well as ongoing
review of recommenda-
tions from outside experts
such as the Institute for
Safe Medication Practices
and JCAHO's Sentinel
Event Alerts. The comprehensive Medica-
tion Process Safety Plan, with 28 short-
term and 19 long-term action items, was
developed. A targeted intervention,
known as "Make It Complete," is directed
at improvement ofthe written medica-
tion order.
Writing a medication order clearly
and completely is a critical first step in a
genuinely safe medication process.
Although we are pursuing technologies
such as computerized physician order
entry for medications, waiting for these
new technologies and not addressing
flaws in currently written medication
orders is not acceptable in our culture.
Therefore, specific guidelines for writing
medication orders were approved, and an
educational campaign ensued. Medica-
tions would not be dispensed by the
pharmacy or administered by the nurse
until the order was "complete" according
to these guidelines. "Make It Complete"
resulted in measured improvement in
prescriber identification, order legibility,
and avoidance of prohibited abbrevia-
tions.
Information Transfer During Patient
Handoffs
Another example of Beaumont's
improvement efforts is information
transfer during the patient handoff
process, which is prioritized as a current
hospitalwide improvement goal. A hand-
off is defined as the transfer of responsi-
bility for a patient from one staff member
to another or from one unit to another.
Expectations at the time of transfer of
care include the following:
It is verified that that patient is appro-
priately prepared for a procedure in an
ancillary department.
Oxygen and other necessities are avail-
able during transport and upon
interim designation.
Receiving staff are provided clinical
information when and where they
need it (not buried in computer
screens or in an unfamiliar portion of
the paper record).
Ancillary staff communicate key infor-
mation back to unit staff (e.g., any
unexpected reactions, the need for
rapid assessment upon return to the
unit).
2 6 F R O N T I E R S O F H E A L T H S E R V I C E S M A N A G E M E N T 2 2 : 1
FI GURE 2. Safety Rounds Sample Agenda
"First, Do No Harm" brochure
"Partners in Safety" brochure
Sentinel event process changes
Site and sidedness process
Patient handoff process
Clinical alarms
Medication safety
Review of physical environment for hazards
Principles of patient safety
Near-miss and error reporting process
Patient identification
Final verification process
Hand hygiene
Chemotherapy administration
Infant/child security
A person-to-person verbal exchange of
information takes place.
Patients participate in the process.
Use of these improvement strategies is
clearly visible, and they are currently
being evaluated by our organization.
SUSTAINING THE EFFORT
Patient safety rounds are regularly held in
all ambulatory and inpatient clinical
departments (see Figure 2 for a sample
agenda). Rounds are attended by the chief
patient safety officer, the hospital safety
officer, an infection control practitioner,
the environmental safety coordinator, a
clinical engineer, selected management
engineers, a human factors specialist,
departmental leadership, and available
unit/department staff.
Goals of patient safety rounds include
advancement of our safety culture and
continued identification of areas of risk so
that risk reduction strategies may be put
in place. Fire safety, environmental safety
or hazardous chemical risks, equipment
safety, employee health and safety, and
infection control procedures are all
assessed during these rounds. Patient
safety rounds provide the opportunity for
visible, active participation by hospital and
medical staff leaders and provide a forum
for staff to discuss their concerns directly
with leadership.
CONCLUSION
For each hospital to tackle patient safety
efforts on its own is itself a genuine bar-
rier to safe systems. We suggest partici-
pating in collaborative efforts and sharing
best practices with other organizations.
Such collaboration is important to the
success of patient safety efforts of large,
complex systems and can be critical for
smaller hospitals that do not have execu-
tive and leadership staff dedicated solely
or even partially to patient safety roles.
For Beaumont, our observations dur-
ing patient safety rounds are perhaps the
most telling signs of our evolution
toward a culture of safety. Departments
now welcome the opportunity to show-
case the improvements in safety that they
have made. Department managers and
staff are the drivers ofthe conversation
during our visits. Observable patient
safety behaviors have permeated our
organization. We believe that our appeal
to core values of dignity and respect has
motivated our staff to modify these
behaviors, thus moving us toward a safe
culture.
m
S T E V E N C . W I N O K U R AN D K A Y J . B E A U R E C A R D 2 J
NOTES
1. Institute for Healthcare Improvement
(IHI); National Patient Safety Founda-
tion (NPSF); Institute for Safe Medica-
tion Practices (ISMP); FCRl (formerly
the Emergency Care Research Institute);
Joint Commission on Accreditation of
Healthcare Organizations (JCAHO);
Centers for Medicare & Medicaid Ser-
vices (CMS); Agency for Healthcare
Research and Quality (AHRQ); National
Quaiity Forum (NQF)
2 . See Wachter and Shojana (2 004).
3 . See Gawande (2 004).
4. Forcing functions are steps in a process
that must be completed in order for the
next step to occur. For example, you
must have your foot on the brake to
move the transmission in your car from
park to reverse; in an airplane bathroom,
you must lock the door to turn on the
light. Forcing functions are very impor-
tant for safety system design.
REFERENCES
Gawande, A. 2 004. "The Bell Curve." [Online arti-
cle created 12 /6/04; retrieved 5/4/05.] New
Yorker, http://www.newyorker.com/fact/content
/?04i2 o6fa_fact.
Kohn, L. T, }. M. Corrigan, and M. S. Donaldson
(eds.). 2 000. To Err Is Human: Building a Safer
Health System. Washington, DC: National Acad-
emies Press.
O'Neill, P. H. 2 002 . "Treasury Secretary Paul H.
O'Neill Remarks to the National Academy of
Public Administration Strategic Human
Resources Conference University of Maryland."
[Online article; retrieved 4/2 7/05.] September
10. http://www.treas.gov/press/releases
Wachter, R. M. 2 004. "The End ofthe Beginning:
Patient Safety Five Years After To Err Is
Human'." [Online article created ri/3 0/04;
retrieved 5/4/05.] Health Affairs Web Exclusive.
November 3 0. http://content.healthafFairs.org
/cgi/reprint/hlthaiT.W4.554vi?maxtoshow=&
HITS-io&hits-io&RESULTFORMAT=&
authori=wachter&fulltext=to+err&andorex
&stored_search-&F IRSTIN D EX=o&
resourcetype=i&journalcode =healthafT.
Wachter, R. M., and K. Shojana. 2 004. Internal
Bleeding: The Truth Behind America's Terrifying
Epidemic of Medical Mistakes. New York: Rugged
Land. LLC.
2 8 F R O N T I E R S O F H E A L T H S E R V I C E S M A N A G E M E N T 2 2 : i
I
I-I
)-<
o
PQ
nj
cx
en
O
X
C
o
CQ
m
X
X
a "
11
till
or. ?:
c ^
til
i i
c
rt
3
c
rt
I
-5
f
i
r
s
t
c
t
i
rt
S
I
X
V
"rt
c
E
\--f
c
E'
g
rt"
1
1
=;
S
1
s
_ i-
rt
^*;
" ^
1
3
~?
)^
g
a
t
i
<
=
l
i
s
s
i
o
n
t
1
"a
rt
1
2
i
- -a s ^
II
c c = -=
= = 5 0
i: H S
5
II
s '^
-:;
^ s
b 5
11 i. 2 1
Cf .5 3
o = ^
^ - -q -^
S 1^ -S ^ ^ i
^p- s ^ u h
SI
ex _ .ii c .s
m
H
m
S T E V E N C . W I N O K U R A N D K A Y j . B E A U R E C A R D 2 9
>
CO
t/3
O
X
4 - '
c
o
s
CQ
S
rt
H
CD
X
X
2 =
B. e
O IP
c
a.
ic
e
-a
rt
c
o
'
s *
1 ^ ^
E - - S " S.
I I
5 E
- p 51 C
"= rt 3
71 - - - * .E e
rt = _g 3
iil
-a . I
^ 1
.J, ij
E rt i
- -j2 ^ i
0) g
. - ^ 7 5
H - ^ =f^-g
S = ~ -E
- -3
-.r, i . . rt
C fe 1-
Z: a.-5
I
III
i
^ rt ^
"i"^ -s
& - . : : :
?: s M ^
3
1
111 i
, q j . s _
. 6 . ac
- i; s i
' -a M o o .2
J 3 i-^ 3 = c
i^ i - S rt S ^
"I I 1= rt . ^ 1
I e I i 11 i
Q-.g^ ^ c 2 =p -^
ts
11
il
I!
i
c
g-i
1 i _
g E 'S^
-a _o ^
"S - - S
1
i
* s
3 l ^
w f^ 11
ill
i 2 ^
'a, .3; =
-C rt rr
^
3 0 F R O N T I E R S O F H E A L T H S E R V I C E S M A N A G E M E N T 2 2 : i
c
I-I
3
u
O
03
in
O
X
ill
o
re
PQ
PM
ffi
X
X
q -9- C
Ji-a; - =
.
"
n
g
rt
i n
c
a
r
e
b
e
a
l
t
a
k
i
i
r
s
e
s
.
3
C
m
c
a.
rt
"u
c
h
n
i
i
s
t
s
,
1
u
rt
^.
1
.S" ui U
0 "3 o 3
fv 0 -1 " ^
rt C ^ -
c/1 O i-T ^
i
f
e
t
y
:
e
a
u
r
r
a
t
i
e
r
:
a
l
r
o
iA CQ CL. =
. -s -s J
-d
c
n
:
t
i
v
e
C rt
rt CL
J
CH ^5 < "O H -Q " .
c
- 1
rt " ^
y qj
y
o
"1
rt
d
t
o
r
1
8
_c:
c
?^
h
a
t
e
1
u
&.
"3
l
e
d
i
c
i
p
l
e
x
E
n
a
n
y
c
o
U l
3
1 3
,0 P
U2 >- ,
rt dj
^ ^
c
^ i
* " * uf
(J U
> X
s
p
r
c
o
u
e
n
t
.
r
e
g
i
c
a
r
a
u
r
u 0 CQ
m
H
m
S T E V E N C. W I N O K U R A N D K A Y | . B E A U R E C A R D 3 I
.Si.
o
a.
o
X
c
o
CQ
CD
I
X
rt
3
o
r
i
f
u
o
-a
O
n
u
r
s
e
i
\
l
y
o
u
r
^ 5
3
l
u
t
y
o
- a
^
3
O
> .
u
L U
i
o
n
s
d
e
c
i
s
i
CO
B
e
a
p
a
r
t
o
f
a
r
e
o
u
y
o
u
r
:
a
b
o
u
t
l
e
s
c
i
o
n
s
- i
^ ^
a
l
t
e
s
a
d
i
c
E
^
l
o
s
i
s
,
E
m
e
n
t
CD
09
a
b
o
u
t
y
o
u
r
t
i
r
e
r
i
g
CT"
E
c
i
n
g
d
o
t
S
o
u
r
>-
-a
CD
C
' ^
CO
^
CD
>
^
y
o
u
r
m
e
a
b
o
u
t
c
o
S
h
a
r
e
a
l
l
i
n
f
o
r
m
;
e
c
t
Cu
rt
y
o
u
i
l
u
r
g
e
r
t
a
v
i
n
g
s
y
o
u
'
r
e
I
"
CO
1
* -
t
r
e
. ^
n
e
e
d
s
w
p
e
c
i
a
l
c'
c
o
n
d
i
t
i
o
n
a
n
d
a
~ rt l
E
l
J.J 3 - -
:
h
e
a
i
t
h
y
o
b
o
u
t
^ > "^
c o "
;
e
o
n
t
o
r
a
t
e
d
i
i
1
f
r
e
e
t
OJJ "_l J-
^. OJ
,_ Oj u-
3 ^ S
3 >
.:= rt
b
o
u
t
l
u
r
s
e
.
rt ^
r- !-
C "
U.
rt
I-. ^
.3 -a
'^ P
A
s
k
f
r
o
t
1-1
3
i
b
o
u
t
V
O
e
c
a
i
l
s
;
i
-o
y
o
u
r
c
a
r
e
g
i
v
e
r
s
.
B
e
s
u
r
e
'
t
o
p
r
o
v
i
o
o
g
r
a
m
s
>
2
rt
u
d
^ 3
C
1
n
e
s
s
e
s
a
h
a
s
i
l
l
m
e
d
i
c
a
l
h
i
s
t
o
r
y
J
1
c
1
n
e
s
s
c
a
:
rt
f
b
s
i
t
e
s
_g
rt
C
0
f
o
r
m
a
.B
3
I
t
o
m
s
y
o
>
l
a
.
o
p
e
r
a
t
i
o
n
s
,
a
s
w
-c
i -
n
o
t
V
p
:
e
r
s
d
:
e
w
o
r
k
rt
J=
"rt
JZ
o
s
u
p
c
rt
d
P
>^
o
v
e
s
.
Q
h
e
s
y
w
e
a
r
g
l
h
o
t
o
u
t
n
d
s
o
r
i
u
l
e
d
t
h
e
i
y
o
n
e
w
v
e
w
a
s
i
"
5
O
1
t
h
a
t
y
l
a
t
i
o
r
c
E
rt
d
1>
j ^
I
..<
L
i
e
s
t
i
o
n
s
o-
Ti
3
O
l
'
l
e
a
s
e
t
e
l
l
u
s
i
r
'
rt
_C
C
?
--3
C
u!
i2
p
U
i
u
c
h
a
s
\
c
a
r
e
,
:
k-
3
c
o
n
c
e
r
n
s
a
b
o
u
t
t
o
u
s
e
h
o
w
1
_5
Q
s
u
r
e
y
i
-a
r
f
o
r
m
t
u
a.
3
O
c
a
t
i
o
n
s
n
e
d
i
t
/
h
a
t
r
1
as
g
c
a
r
e
a
i
-
y
o
u
r
--^
l
e
n
t
n
c
1 -H
e
q
u
l
o
n
e
.
oo
t
e
s
t
I
S
g
o
i
n
g
t
o
\
s
o
m
e
t
h
i
n
g
i
s
b
e
i
n
g
a
n
e
t
a
k
i
CO
)
s
p
i
t
a
o
>
j
u
l
e
a
> .
U l
u
rt
I
3
o
M
a
k
e
s
u
r
e
t
h
a
t
y
l
E
l
]
5
OJ
-
q
u
e
s
n
o
i
v
e
.
A
s
i
<
B
m
a
t
i
o
n
t
h
a
t
y
o
u
i
r
r
y
a
l
i
:
c
a
r
e
t
h
e
o
e
i
t
t
e
m
cy
> i
CD
;
e
d
.
' 4 . '
^\
m
a
n
y
t
i
m
e
s
a
s
v
(
rt
IU
:^ 2
rt --
3 1
H
i
n
t
;
s
u
p
p
i
E -
-
! ' E
d)
e
.
03
u
r
e
r
e
CO
y
o
u
Q
m
e
m
b
e
r
a
m
i
l
y
OJj
I
f
p
o
s
s
i
h
i
e
,
b
r
i
n
c
o
.
a
t
i
i
c
I
s
i
n
f
o
r
e
r
d
r
u
g
c
o
-a
1
t
o
i
n
t
u
%
L -
rt
h
e
a
l
t
CL,
X
e
e
l
3
h
e
i
p
y
o
'
S
V
c
a
n
_(=
f
r
i
e
n
d
w
i
t
h
y
o
u
"oJj
Ul
rt
Ul
t
t
o
y
o
i
1
p
o
r
t
a
n
1
-
r
v
o
u
r
.'
e
n
t
e
JZ
it
---
I
v
e
s
w
t
h
e
i
b
e
r
d
h
e
i
p
n
m
o
r
e
c
o
n
i
f
o
r
t
a
b
l
>.
crt
3
O
i
rt
n
u
r
s
e
s
.
a
n
d
d
o
c
t
o
r
s
t
l
y
o
u
r
7 1.'
I
b
a
d
e
t
B
rt
.Is
o
r
t
h
e
"^
-^
l
.
o
c
c
o
i
n
s
t
r
u
c
t
i
a
v
c
o
r
rt
E
3
O
C
C
3
O
2
n t
r
p
r
o
b
l
i
t-j
o
a
e
r
g
t
e
s
,
s
a
rt
aJ
B
-r-i
rt
3
rt
Q-
; ^
t
i
o
n
s
i
r
e
d
i
c
a
w
i
t
h
m
v
e
h
a
d
rt
c
r^
"-*
u
t
w
r
i
i
L
v
e
y
o
^ ~
>
"O
rt
rt
T3
b
i
r
t
3
O
o
n
e
o
f
t
o
c
a
l
i
a
Y
o
u
'
r
e
a
l
s
o
w
e
l
c
i
e
n
c
i
n
g
.
r
x
p
e
r
i
r
e
n
t
l
y
e
a
r
e
c
u
r
p
JZ
H
>^
o
u
r
s
t
a
i
n
g
y
3
e
k
e
d
(
-C
u
9
at
c
u
s
t
o
m
e
r
h
o
t
l
i
n
i
ri
2
h
F
e
e
l
f
r
i
o
n
s
.
r
q
u
e
s
t
e
e
x
p
e
c
rt
O
U
a
r
e
o
r3
u
-0
I
p
U
S
i
5b
c
d
i
c
a
t
i
o
i
l
y
a
m
e
^
:
c
a
r
e
.
^ :3
w
i
l
l
O
>.
:5
2
4
8
-
5
5
1
-
2
2
7
3
i
p
r
o
'
r
o
y
)
r~
2
4
8
-
9
6
4
-
8
8
0
8
i
_:
^ ,
o
l
u
s
u
a
l
1
U i
f
F
e
r
e
n
t
l
o
o
k
s
d
i
c
k
s
-C
3
C
t
o
r
c
-a
Uf
p
3
u.
l
u
r
e
y
(
q j
^ r-
1J r~
r\ C
Qj r^
i
r
n
a
m
i
n
o
r
t
r
e
C
S
y
o
t
l
i
c
a
t
i
o
rt ^
u. C
0 >.
~o 5
r
i
s
t
b
a
s
t
e
r
i
n
g
> 'E
u. -
3 E
O T3
>. rt
3 2 F R O N T I E R S O F H E A L T H S E R V I C E S M A N A G E M E N T 2 2 : 1
Anda mungkin juga menyukai
- Identifying Child Abuse Fatalities During Infancy: Clinical ReportDokumen11 halamanIdentifying Child Abuse Fatalities During Infancy: Clinical ReportJesse M. MassieBelum ada peringkat
- Oral and Dental Aspects of Child Abuse and Neglect: Clinical ReportDokumen10 halamanOral and Dental Aspects of Child Abuse and Neglect: Clinical ReportJesse M. MassieBelum ada peringkat
- Effective Discipline To Raise Healthy Children: Policy StatementDokumen12 halamanEffective Discipline To Raise Healthy Children: Policy StatementJesse M. MassieBelum ada peringkat
- Jpeds Aom 208Dokumen3 halamanJpeds Aom 208Jesse M. MassieBelum ada peringkat
- i-PASS OBSERVATION TOOLDokumen1 halamani-PASS OBSERVATION TOOLJesse M. MassieBelum ada peringkat
- Ongoing Pediatric Health Care For The Child Who Has Been MaltreatedDokumen18 halamanOngoing Pediatric Health Care For The Child Who Has Been MaltreatedJesse M. MassieBelum ada peringkat
- IJMEDokumen7 halamanIJMEJesse M. MassieBelum ada peringkat
- What Is Child Abuse and Neglect? Recognizing The Signs and SymptomsDokumen8 halamanWhat Is Child Abuse and Neglect? Recognizing The Signs and SymptomsJesse M. MassieBelum ada peringkat
- Making The Most of Mentors: A Guide For MenteesDokumen5 halamanMaking The Most of Mentors: A Guide For MenteesJesse M. MassieBelum ada peringkat
- Cbig Cross-ReportingDokumen25 halamanCbig Cross-ReportingJesse M. MassieBelum ada peringkat
- Preventing Adverse Childhood Experiences (Aces) :: Leveraging The Best Available EvidenceDokumen40 halamanPreventing Adverse Childhood Experiences (Aces) :: Leveraging The Best Available EvidenceJesse M. MassieBelum ada peringkat
- dBA PROTECT YOUR HEARINGDokumen4 halamandBA PROTECT YOUR HEARINGJesse M. MassieBelum ada peringkat
- Suidi Oklahoma ProviderDokumen28 halamanSuidi Oklahoma ProviderJesse M. MassieBelum ada peringkat
- Status EpileticusDokumen2 halamanStatus EpileticusJesse M. MassieBelum ada peringkat
- Male Victims of Intimate Partner Violence: Did You Know?Dokumen3 halamanMale Victims of Intimate Partner Violence: Did You Know?Jesse M. MassieBelum ada peringkat
- Noisey PlanetDokumen1 halamanNoisey PlanetJesse M. MassieBelum ada peringkat
- Minority YouthDokumen28 halamanMinority YouthJesse M. MassieBelum ada peringkat
- COVID Positive/PUI: PAPR Prioritization MatrixDokumen1 halamanCOVID Positive/PUI: PAPR Prioritization MatrixJesse M. MassieBelum ada peringkat
- Kinshipguardianship PDFDokumen139 halamanKinshipguardianship PDFJesse M. MassieBelum ada peringkat
- Intimate Partner Violence, Sexual Violence, Stalking: Before The Age of 18Dokumen1 halamanIntimate Partner Violence, Sexual Violence, Stalking: Before The Age of 18Jesse M. MassieBelum ada peringkat
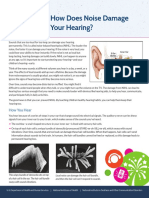
- How Does Noise Damage Your Hearing?Dokumen2 halamanHow Does Noise Damage Your Hearing?Jesse M. MassieBelum ada peringkat
- Domestic Violence Oklahoma 2017Dokumen44 halamanDomestic Violence Oklahoma 2017Jesse M. MassieBelum ada peringkat
- CDC Capacity BuildingDokumen16 halamanCDC Capacity BuildingJesse M. MassieBelum ada peringkat
- How Loud Is Too LoudDokumen2 halamanHow Loud Is Too LoudJesse M. MassieBelum ada peringkat
- Aap Food Insecurity Toolkit For ProvidersDokumen39 halamanAap Food Insecurity Toolkit For ProvidersJesse M. MassieBelum ada peringkat
- In Drinking Water: Sources of LEADDokumen1 halamanIn Drinking Water: Sources of LEADJesse M. MassieBelum ada peringkat
- Advancing Health Equity: A Practitioner'S Guide ForDokumen132 halamanAdvancing Health Equity: A Practitioner'S Guide ForJesse M. MassieBelum ada peringkat
- Fireworks ShowDokumen2 halamanFireworks ShowJesse M. MassieBelum ada peringkat
- Cbig Child Abuse and Neglect Fatalities 2017Dokumen8 halamanCbig Child Abuse and Neglect Fatalities 2017Jesse M. MassieBelum ada peringkat
- Essentials For Childhood:: Steps To Create Safe, Stable, Nurturing Relationships and EnvironmentsDokumen1 halamanEssentials For Childhood:: Steps To Create Safe, Stable, Nurturing Relationships and EnvironmentsJesse M. MassieBelum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- List of 2 Years AffiliationDokumen15 halamanList of 2 Years AffiliationAahad AmeenBelum ada peringkat
- CV of DoctorDokumen1 halamanCV of DoctorBobby Jatt0% (1)
- HEALTHDokumen28 halamanHEALTHKristine SaulerBelum ada peringkat
- NYS Office of Professional Conduct Opens Investigation of Controversial Psychiatrist Kelly Brogan (11/24/20) + My Complaint Re: Her License (3/22/20)Dokumen5 halamanNYS Office of Professional Conduct Opens Investigation of Controversial Psychiatrist Kelly Brogan (11/24/20) + My Complaint Re: Her License (3/22/20)Peter M. Heimlich100% (1)
- HIS-district LaboratoryDokumen6 halamanHIS-district LaboratoryEricka GenoveBelum ada peringkat
- BSN Curriculum 20 21 English 1Dokumen3 halamanBSN Curriculum 20 21 English 1ROSE DIVINAGRACIABelum ada peringkat
- Resume PDFDokumen1 halamanResume PDFapi-353271874Belum ada peringkat
- James Sloan Takes Firm Stand On Issues Important To Tennessee House of Representatives District 63Dokumen4 halamanJames Sloan Takes Firm Stand On Issues Important To Tennessee House of Representatives District 63PR.comBelum ada peringkat
- Experts Validation TableDokumen20 halamanExperts Validation TableDeepti KukretiBelum ada peringkat
- Continuing Competency Log PrintDokumen2 halamanContinuing Competency Log PrintBobBelum ada peringkat
- Clinical Applications of Nursing DiagnosisDokumen768 halamanClinical Applications of Nursing DiagnosisAyaz Ahmed Brohi100% (1)
- 6450a6d07795498d Derma360reportDokumen12 halaman6450a6d07795498d Derma360reportNeelam PahujaBelum ada peringkat
- Medical - Strips (Medical Grade vs. "Hospital Grade")Dokumen22 halamanMedical - Strips (Medical Grade vs. "Hospital Grade")Nirav DesaiBelum ada peringkat
- Pharma DirectoryDokumen1.899 halamanPharma DirectoryVandana Tyagi100% (2)
- Changes in Hospital Competitive StrategyDokumen23 halamanChanges in Hospital Competitive Strategyanantomi100% (1)
- Panic Disorder: GuidelineDokumen3 halamanPanic Disorder: Guidelineputri weniBelum ada peringkat
- (Medical Radiology) Lluís Donoso-Bach, Giles W. L. Boland - Quality and Safety in Imaging-Springer International Publishing (2018)Dokumen187 halaman(Medical Radiology) Lluís Donoso-Bach, Giles W. L. Boland - Quality and Safety in Imaging-Springer International Publishing (2018)Piotr JankowskiBelum ada peringkat
- Project Seminar Hospice FedoraDokumen3 halamanProject Seminar Hospice FedoralalithaBelum ada peringkat
- ��تجميعات الفارما�Dokumen4 halaman��تجميعات الفارما�Turky TurkyBelum ada peringkat
- You Are Dangerous To Your Health CRAWFORDDokumen18 halamanYou Are Dangerous To Your Health CRAWFORDGonzalo PaezBelum ada peringkat
- Pola Penggunaan Obat Antihipertensi Pada Pasien Hipertensi: Teti Sutriati Tuloli, Nur Rasdianah, Faradilasandi TahalaDokumen9 halamanPola Penggunaan Obat Antihipertensi Pada Pasien Hipertensi: Teti Sutriati Tuloli, Nur Rasdianah, Faradilasandi TahalaSifa ShopingBelum ada peringkat
- Healthcare & Life Sciences ReviewDokumen47 halamanHealthcare & Life Sciences Reviewmercadia59970% (1)
- Food Handler Training CoursesDokumen2 halamanFood Handler Training CoursesSai Ram ChanduriBelum ada peringkat
- Cv. Dr. Saldy YusufDokumen6 halamanCv. Dr. Saldy YusufMuhammad FaturrahmanBelum ada peringkat
- Physical Education and Health 12Dokumen2 halamanPhysical Education and Health 12Jenia Alexis CapaBelum ada peringkat
- Dental Claim FormDokumen2 halamanDental Claim Formmiranda criggerBelum ada peringkat
- Francois Gremy (Autosaved)Dokumen7 halamanFrancois Gremy (Autosaved)Donya GholamiBelum ada peringkat
- Dental Officer Information - e (1989)Dokumen10 halamanDental Officer Information - e (1989)Marian GarciaBelum ada peringkat
- Policies Under NMHC Act 2017Dokumen2 halamanPolicies Under NMHC Act 2017SAKSHI SHRIPAL SHAH 1833474Belum ada peringkat
- James Belgira Tamayo, RMT, MD James Belgira Tamayo, RMT, MDDokumen1 halamanJames Belgira Tamayo, RMT, MD James Belgira Tamayo, RMT, MDfilchibuffBelum ada peringkat