Resident Tutorial 57-Part 1
Diunggah oleh
Surat TanprawateHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Resident Tutorial 57-Part 1
Diunggah oleh
Surat TanprawateHak Cipta:
Format Tersedia
Resident tutorial57
Surat Tanprawate, MD, FRCPT
Division of Neurology, Chiangmai University
Neurology you should know
1. Symptomatology approach
2. Disease based learning
3. Skills learning-
1. History taking, Physical exam
2. Thinking skills: summarisation, problem lists,
discussion
Symptomatology approach
Cognitive function and behavioural change
Level of consciousness: coma, delirium
Content of conscious: dementia, other higher cognitive
disorder (dysphasia, acalculia etc)
Neuropsychiatric problems
Cranial nerve function
visual loss, diplopia, dysarthria, hearing loss, vertigo,
dysphagia
Symptomatology approach
Motor system
weakness
movement disorder
gait disorder
ataxia
Sensory system
numbness
pain, and headache
Autonomic function
bowel bladder involvement,
dysautonomia
Episodic disorder
transient loss of
consciousness
episodic neurological signs/
symptoms
Cognitive dysfunction
- coma
A middle aged woman
She presented with sudden alteration of consciousness
PE: conscious: coma
pupils: 3 mm SRTL
no motor response
vertical eye movement
dolls eye-negative
case
case
The question of alter level of
conscious state
Coma mimicker: lock-in syndrome
Localize lesion
Caused of coma state
Evaluated brain death
Arousal and awareness, the two components of consciousness in coma,
vegetative state, minimally conscious state, and locked-in syndrome.
Lancet Neurol 2004; 3: 53746
11
Alteration of consciousness
Level of consciousness
Stupor and coma
Content of
consciousness
Behavioural state
Structural
Non-structural
-Metabolic
-Toxic
Symmetrical Asymmetrical
C P O M R
(1)
(2)
(3)
Localise lesion and identify
the cause
Behavioral state Denition Lesion Comment
Locked-in
syndrome
Alert and aware,
quadriplegic with lower CN
palsy
Bilateral anterior
pontine
Similar state:severe
polyneuropathy
MG, NM blocking
agent
Persistent
vegetative state
Absent cognitive function
but retain vegetative
component
Extensive cortical grey
and subcortical white
matter with relative
preservation of brain
stem
Synonyms include
apallic syndrome,
coma vigil, cerebral
cortical death
Abulia Severe apathy, patient
neither speak nor moves
spontaneously
Bilateral frontal medial Severe case
resemble akinetic
mutism, but patient is
alert and aware
Catatonia Mute, and mark decrease
motor activity
Usually psychiatric May be mimicked by
frontal lobe
dysfunction and drug
Pseudocoma Feigned coma
Behavioural state that may mimic coma
Locked in
syndrome
Localisation of the structural
lesions
C: state of consciousness
P: pupillary size and response to light
O: ocular movement, nystagmus, and ocular reex
M: motor response
R: respiratory pattern
Hippus Greek hippos meaning horse
Hippus, also known as pupillary athetosis, is
spasmodic, rhythmic, but irregular dilating and
contracting pupillary movements between the
sphincter and dilator muscles
Unilateral/bilateral miosis,
retained light reaction
Bilateral unresponsive large pupils
Pupils remain xed in mid-position
Bilateral xed mid-position pupils
Hypothalamic/
diencephalon
Upper midbrain
Central midbrain
Lower brainstem/
medulla
Rostro-caudal brainstem compression secondary to
an expanding supratentorial process
O: Ocular movement
Resting position
Eye deviation
Spontaneous eye movement: nystagmus, ocular
bobbing, ocular dipping
Reex ocular movement: VOR, OCR
J of Neurol and Psychi 1988;51:725-727
mnemonic used to remember the FAST direction of
nystagmus is COWS
COWS: Cold Opposite, Warm Same.
Cold water = FAST phase of nystagmus to the side
Opposite from the cold water lled ear
Warm water = FAST phase of nystagmus to the
Same side as the warm water lled ear
M: Motor response
Resting position
Eyes and head are deviated to the one side opposite
hemiparesis
Decerebrate and decorticate
Adventitious movements
Tonic clonic
myoclonus
Purposeful movement
Posture in coma
Decerebrate rigidity
bilateral upper and
lower limb extensor
posture, usually the
consequence of
bilateral mid-brain
lesions
Decerebrate cat
Decorticate posture
bilateral exion of the
upper limbs and
extension of the lower
limbs, usually the
consequence of an
diencephalic
lesion(late)
R: Respiratory pattern
Cheyne- stoke respiration
Central neurogenic hyperventilation
Apneustic breathing
Cluster breathing
Ataxic respiration
Localisation from respiratory
patterns
Cheyne Stokes - crescendo-decrescendo
breathing - intact brainstem
Central Neurogenic hyperventilation - lower
midbrain/upper pons
Apneustic - lower pontine lesion
Biot breathing/Ataxic breathing - Medullary lesion
Localisation schematic
Cause of coma/alter mental status
Structural
Non-structural
Exogenous:
drugs
toxin (lead, thallium, cyanide, methanol, CO)
Endogenous
metabolic (Na, glucose, Ca, lactic), hypoxemia,
hypercapnia, hypothyroid
Toxin from organ failure: uraemia, hepatic
encephalopathy
Point of concern
Structure mimic toxic-metabolic
SAH, Sinus vein thrombosis, Chronic
subdural hemorrhage,
Diffuse multifocal disorder; vasculitis,
demyelinating
Toxic-metabolic mimic structural
barbiturate, lead poisoning,
hypoglycaemia, hepatic encephalopathy,
hyponatremia
Non convulsive status epilepticus
Fixed stare, repetitive blinking and chewing or
swallowingsmall myoclonic twisting of face and
extremities
Circumstance
Prolong post ictal state
Acute and uctuating of confusion or stupor
Stupor with myoclonus
Episodic partial complex sign
Acute catatonia
Intoxication
Can occur with sympatholytic (clonidine)
Anti-cholonergics (TCA, phenothiazine, anti-
parkinson, OTC
Cholinergic (organophosphate)
Serotonin syndrome (MAOI)
Anion gap acidosis poisonings (ethylene glycol,
salicylates, toluene, paraldehyde, uremia, DKA)
Cognitive dysfunction
- dementia
The memory
Episodic memory & semantic memory
Long term memory: a wide dispersed networks
The cascade of brain areas through which visual information is rst
processed perceptually and then for the purpose of memory
Amnestic and dementia syndrome
!
Amnestic syndrome
Profound loss of the episodic memory
!
Dementia
Acquired and persistent compromise in multiple
cognitive, domains that are severe enough to
interfere with every day functioning
!
Delirium or acute confusional state(ACS)
Prominent decits or uctuations in attention
processing
Gad
e
Amnesia - Causes and localizations
Amnestic
syndrome
= loss of episodic memory
anterograde loss
variable retrograde loss
Normal or relatively spared:
intelligence
working memory
conditioning
priming
Classic case: HM (Scoville &Milner, 1957)
Bilateral removal of mesial temporal
lobes
@openneurons
A man with short term
memory loss
Gade
Alzheimers disease: Topography of neuropathological
changes
Neurobrillary
tangles
Van Hoesen & Solodkin, Ann.N.Y.Acad.Sci. 1994,747:12-35
Herpes simplex
encephalitis
Clinical symptoms
fever
memory loss
alteration of consciousness
neurological decit
Investigation:
Brain imaging: fronto-temporal
lobe involvement
CSF: increase cell, relatively
normal sugar
Wernicke-Korsakoff syndrome
After 2 days treatment with thiamine
* Confusion
* Eye symptoms
- gaze paralysis
- nystagmus
* Gait ataxia
Neuropathological lesions:
Lesions along the neural axis,
particularly close to the ventricle walls
Victor, Adams & Collins, 1971, 1989
Chronic phase:
Korsakoffs disease
(amnesic syndrome)
Transient Global
Amnesia
Hours to day
Temporary version of amnestic syndrome
Causes
Idiopathic
Associated with CPS, Migraine, TIA of
hippocampus, Drug intoxication, Alcohol
blackout, Minor head injury
Dementia diagnosis: The DSM IV
criteria
!
Cognitive problems
!
Memory +
!
Aphasia, Apraxia, Agnosia, Disturbance of
executive function
!
Impairment in occupational or social functioning
Dementia
Reversibel dementia
- Drug
- Syphilis
- Hypothyroid
- Vitamin deciency
- Organ failure
Irreversible dementia
Stable
Progressive
- Vascular
- Post traumatic
- Post encephalitis
- etc
Neurodegenerative Non-neurodegenerative
- CJD
- ADC
- Vascular
Alzheimers
disease
Non-Alzheimers
disease
- Parkinsons disease dementia
- DLB
- Parkinson plus syndrome
- Genetic (Wilson, Huntington)
Alzheimers disease (AD)
AD is a common neurodegenerative disease characterised
by memory impairment plus one or more additional
cognitive disturbance (dementia)
Gradual decline in 3 key symptom domains
Cognition (MMSE, MOCA, ADAS-Cog)
Behaviour and personality
Activities of daily living (ADL)
Prevalence
Age > 65 years : 10%
Age > 85 years : 30%
Staging and diagnosis of MCI and Alzheimers disease
!" $ %&'( )&*&+(,-*
!" $%&'() *%++ ,-.-/%
!" $%& '()%*(+%,
Pathophysiology
Depletion of acetylcholine (ACh): especially in moderate to severe disease stages
Aim of dementia
management
1. Cure disease
2. Prevent disease or delay onset
3. Slow progression of disease
4. Treat primary symptoms eg memory
5. Treat secondary symptoms eg
depression, hallucinations
!" $ %&'( )&*&+(,-*
!" $%&'() *%++ ,-.-/%
!" $%& '()%*(+%,
Pathophysiology
Depletion of acetylcholine (ACh): especially in moderate to severe disease stages
APP A"
Neuronal
cell death
#-secretase
"-secretase
Ach
deciency
Secretase modulators
Immunotherapy
amyloid binders
anti-inammation
anti-oxidants
neuroprotection
inammation
oxidative stress
excitotoxicity
Acethylcholine
esterase inhibitor
AD modifying and symptomatic strategies
Neurotransmitters deficiency
Acetylcholine esterase inhibitor
(AchEI)
Donepezil(Aricept),
Rivastigmine(Exelon),
Galantamine(Reminyl)
Pharmacologic treatment
Acetylcholine esterase inhibitor (AchEI)
Donepezil(Aricept),
Rivastigmine(Exelon),
Galantamine(Reminyl)
Symptomatic treatment
drug to control psychological
symptoms
Memantine
NMDA receptor antagonist
Beta amyloid
Dysfunction of Glutamate
reuptake pump
Dysfunction of glutamate
synthetase enzyme
NMDA antagonists: slow intracellular Ca
accumulation and delay nerve damage
Memantine
Approved for use of moderate-severe AD
Use in combination with AchE inhibitor
Mild benets in cognition and clinicians global
assessment of change
Not efcacious in mild AD
No effect on survival time
Psychological and Behavioral
symptoms in dementia
BPSD (Behavioral and Psychological
Symptoms of Dementia)
Apathy, agitation, anxiety, irritability,
aberrant motor behavior, dysinhibition,
delusion, hallucination, euphoria
BPSD
Pharmacologic treatment
Other dementia
Vascular dementia
Normal pressure hydrocephalus (NPH)
Hypothyroidism
AID Dementia
Wernicke-Kosakoff amnestic syndrome
Other neurodegenerative dementia (PDD, FTD, DLB)
66
History
Normal pressure
hydrocephalus (NPH)
First described 40
years ago by
neurosurgeon Solomon
Hakim
Treatable syndrome
Dementia
Gait apraxia
Urinary urgency and
incontinence
The New England Journal of Medicine in 1965
10/3/57
67
NPH : clinical condition or syndrome
characterized by
triad of symptoms
Motor disturbances
Incontinence of urine
Mental change
Ventriculomegaly and normal CSF pressure
10/3/57
68
The difference between NPH [normal
pressure hydrocephalus and other treatable
dementias is that this is a surgically treated
dementia.
CSF shunt if the hydrocephalus is communicating
Endoscopic third ventriculostomy if hydrocephalus
is obstructive
10/3/57
69
Diagnosis
Most patients start as possible NPH
Differential diagnosis of symptoms is important,
because theyre among the most common
symptoms of elderly
Gait :peripheral neuropathy, cervical or lumbar stenosis
and myelopathy, parkinsonism, or arthritis
Incontinence:prostate for men or stress incontinence
for women
Dementia : Alzeimer,s disease, frontotemporal
dementia, vascular dementia, or parkinsonism
10/3/57
70
Diagnosis
Starts either with symptom, CT or MRI showing
enlarged ventricle, or both
Symptom triad
Does not need to be present in its entirety
Most experts believe gait impairment is required
If gait is normal, then look for other causes first
Neuroimaging
In the elderly, ventriculomegaly is sometimes hard to
distinguish from normal ageing, and periventricular T2
changes are ubiquitous
10/3/57
71
Diagnostic : CSF- Removal Approach
2 approaches in use in the United States
Large volume lumbar puncture (LP)
Continuous CSF drainage via spinal
catheter
10/3/57
Dementia in hypothyroidism
Patients with the AIDS dementia complex
present with a variable, yet characteristic,
constellation of abnormalities in cognitive,
motor, and behavioral function. Perhaps
the salient aspects of the disorder are the
slowing and loss of precision in both
mentation and motor control . These
patients often lose interest in their work as
well as in their social and recreational
activities. (Price et al., 1988)
HIV-associated Neurocognitive Disorders
(HAND)
HIV-1-Associated Dementia (HIV-D)
AIDS Dementia Complex (ADC)
HIV-associated Cognitive/Motor Complex
HIV-associated Mild Neurocognitive Disorder
Asymptomatic Neurocognitive Impairment
HIV-Associated Mild Cognitive/Motor Disorder
HIV-D
Essential features
disabling cognitive impairment accompanying by
motor dysfunction, and behavioural change
HIV dementia symptoms are more associated
with motor slowing and loss of executive control
than with language and memory disturbance.
Subcortical dementia
Janssen et al. Neurology 1991. 41:778-785
White-matter abnormalities on CT and MRI
Left: CT scan showing ventricular enlargement and white-matter
hypodensity.
Right: FLAIR MRI showing both cortical and central atrophy,
and characteristic conuent signal abnormalities deep within the
white matter.
Operational denition of HIV-D and clinical
features of use for diagnosis
HIV-1 seropositivity
History of acquired and commonly progressive cognitive-behavioural decline,
with apathy, memory loss, and slowed mental processing
Neurological examination: diffuse and symmetrical CNS signs, including slowed
eye and limb movements, apraxia, hyperreexia, hypertonia, and release signs
Neuropsychological assessment: impairment in at least two domains, including
frontal lobe, psychomotor speed, and non-verbal memory
CSF analysis: exclusion of neurosyphilis, TB, and cryptococcal meningitis
CT and MRI: diffuse cerebral atrophy with symmetrical deep white-matter
hyperintensities.
Exclusion criteria: major psychiatric disorder, intoxication or other cause for
dementia; metabolic impairmenteg, hypoxia, sepsis, uraemia; active CNS
opportunistic processes
Janssen RS, et al. Neurology 1991; 41: 77885.
HIV-D CMV encephalitis PML
Features
Memory disturbance,
mental slowing, gait
disturbance
Delirium, seizures,
brainstem sign
Focal neurological signs
Course Several months Days to weeks Weeks to months
MRI
Diffuse atrophy,
symmetrical deep white
matter, diffuse intensities
Normal or
periventriculitis
Scattered, asymmetrical
subcortical white matter
lesions
CSF
Non-diagnostic immune
activation less marked
in patients treated with
HAART
PCR+ for CMV 90%
PCR+ for JC/BK virus
60%
Differentiation of HIV-D from opportunistic infection
Pre- vs Post HAART era
Natural history change from 6 months (mean) to 44 months to death
Altered pattern of neuropsychological decits in such patients, with
tendency for more cortical type
Hypermetabolism location on PET scan
Pre-HAART: basal ganglia
HAART: mesial temporal lobe
CSF biomarker: beta-2 microglobulin and HIV viral load are not
strongly correlated with ADC severity
Navia B, et al. Ann Neurol 1986, 19:517 524.
Dore GJ, et al. AIDS 2003, 17:15391545.
Cysique L, et al. XIVth International AIDS Conference. Spain 2002.
Treatment of HIV-D
Objective: to maximally suppress HIV replication in CNS
PI containing regimen can reverse neurocognitive
decits
Sacktor N et al. J Neurovirol 2000; 6: 84-88
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Post Traumatic Headache Disorder - 2020Dokumen26 halamanPost Traumatic Headache Disorder - 2020Surat TanprawateBelum ada peringkat
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Headache Tutorial - Neuro Essential CMU2020Dokumen66 halamanHeadache Tutorial - Neuro Essential CMU2020Surat Tanprawate100% (4)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Status Epilepticus in Adult PDFDokumen22 halamanStatus Epilepticus in Adult PDFSurat TanprawateBelum ada peringkat
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (894)
- Headache Case Seminar - RCPTDokumen25 halamanHeadache Case Seminar - RCPTSurat TanprawateBelum ada peringkat
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- New Era in Migraine Management - 2019 - HatYaiDokumen77 halamanNew Era in Migraine Management - 2019 - HatYaiSurat Tanprawate100% (3)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Migraine SubtypeDokumen55 halamanMigraine SubtypeSurat Tanprawate100% (1)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Headche:Dizzy Med Stud - 2016Dokumen51 halamanHeadche:Dizzy Med Stud - 2016Surat TanprawateBelum ada peringkat
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Neurological Examination - Pre-Med - 401Dokumen73 halamanNeurological Examination - Pre-Med - 401Surat Tanprawate100% (4)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Neuro-Ophthalmology - Third Year Student - 2018Dokumen126 halamanNeuro-Ophthalmology - Third Year Student - 2018Surat TanprawateBelum ada peringkat
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- Status Epilepticus PathophysiologyDokumen22 halamanStatus Epilepticus PathophysiologySurat TanprawateBelum ada peringkat
- Headache Case Seminar - RCPTDokumen25 halamanHeadache Case Seminar - RCPTSurat TanprawateBelum ada peringkat
- Refractory-Primary-Headache Surat PornchaiDokumen51 halamanRefractory-Primary-Headache Surat PornchaiSurat TanprawateBelum ada peringkat
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Headache in Emergency ConditionDokumen34 halamanHeadache in Emergency ConditionSurat TanprawateBelum ada peringkat
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Neuro Ophthalmology For Med Student - 2016Dokumen120 halamanNeuro Ophthalmology For Med Student - 2016Surat Tanprawate100% (3)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Ambulatory Conference: Approach To Parkinson's DiseaseDokumen37 halamanAmbulatory Conference: Approach To Parkinson's DiseaseSurat Tanprawate100% (1)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Physical Exam For DiagnosisDokumen61 halamanPhysical Exam For DiagnosisSurat Tanprawate100% (2)
- Physical Exam For DiagnosisDokumen61 halamanPhysical Exam For DiagnosisSurat Tanprawate100% (2)
- DPP-4 Inhibitor and The BrainDokumen19 halamanDPP-4 Inhibitor and The BrainSurat TanprawateBelum ada peringkat
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Basic Movement Disorder ApproachDokumen96 halamanBasic Movement Disorder ApproachSurat Tanprawate100% (18)
- Acute Migraine Management, Chiangmai 2015Dokumen60 halamanAcute Migraine Management, Chiangmai 2015Surat Tanprawate100% (1)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- MS and NMO Update From ECTRIMS - Boston 2014 PDFDokumen43 halamanMS and NMO Update From ECTRIMS - Boston 2014 PDFSurat TanprawateBelum ada peringkat
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- Channelopathy of CNSDokumen55 halamanChannelopathy of CNSSurat TanprawateBelum ada peringkat
- Role AEDs in Migraine PreventionDokumen61 halamanRole AEDs in Migraine PreventionSurat TanprawateBelum ada peringkat
- Neuro OphthalmologyDokumen114 halamanNeuro OphthalmologySurat TanprawateBelum ada peringkat
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- MS and NMO Update From ECTRIMS - Boston 2014 PDFDokumen43 halamanMS and NMO Update From ECTRIMS - Boston 2014 PDFSurat TanprawateBelum ada peringkat
- WN - jun14.BB M CohenDokumen12 halamanWN - jun14.BB M CohenSurat TanprawateBelum ada peringkat
- PD SubtypeDokumen11 halamanPD SubtypeSurat TanprawateBelum ada peringkat
- Headache You Should Know - SuratDokumen33 halamanHeadache You Should Know - SuratSurat Tanprawate100% (2)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Occam's Razor and Hickam's DictumDokumen6 halamanOccam's Razor and Hickam's DictumSurat TanprawateBelum ada peringkat
- Broncho DilatorsDokumen53 halamanBroncho DilatorsDocRNBelum ada peringkat
- Progress in Retinal and Eye Research: Contents Lists Available atDokumen40 halamanProgress in Retinal and Eye Research: Contents Lists Available atSalsa BillaBelum ada peringkat
- Biosure RGDokumen2 halamanBiosure RGJuan Martinez Del AngelBelum ada peringkat
- Toxic Responses of the Skin: Skin Functions and DiseasesDokumen6 halamanToxic Responses of the Skin: Skin Functions and DiseasesM. JoyceBelum ada peringkat
- CH 142: Sepsis and Septic Shock ANSWERSDokumen2 halamanCH 142: Sepsis and Septic Shock ANSWERSTop VidsBelum ada peringkat
- Template For Case ReportDokumen2 halamanTemplate For Case ReportevanBelum ada peringkat
- Clinical Practice Guidelines For Rest OrthosisDokumen8 halamanClinical Practice Guidelines For Rest OrthosisJavier HonoldBelum ada peringkat
- How Food Handlers Can Spread IllnessDokumen2 halamanHow Food Handlers Can Spread IllnessSavitri Maharani BudimanBelum ada peringkat
- Scientists transform spinach leaf into beating human heart tissueDokumen4 halamanScientists transform spinach leaf into beating human heart tissueSkye M. PetersBelum ada peringkat
- Group 1 Case Study Chapter 24Dokumen10 halamanGroup 1 Case Study Chapter 24Doneva Lyn MedinaBelum ada peringkat
- Fundamentals of Rheumatoid Arthritis and Various Homoeopathic Trials in Patients of Rheumatoid Arthritis: An UpdateDokumen6 halamanFundamentals of Rheumatoid Arthritis and Various Homoeopathic Trials in Patients of Rheumatoid Arthritis: An UpdateHomoeopathic PulseBelum ada peringkat
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Study DesignDokumen130 halamanStudy Designephremtigabie7Belum ada peringkat
- Vaccine Research StatusDokumen112 halamanVaccine Research StatusJunko Tsukuda100% (1)
- Baby SensesDokumen2 halamanBaby SensesCamille LiqueBelum ada peringkat
- A Case of Patient AI, Who Came in Due To Sore ThroatDokumen16 halamanA Case of Patient AI, Who Came in Due To Sore ThroatLovelle LopezBelum ada peringkat
- Carbetocin For The Prevention of Postpartum HemorrhageDokumen8 halamanCarbetocin For The Prevention of Postpartum HemorrhageLeslie GuzmanBelum ada peringkat
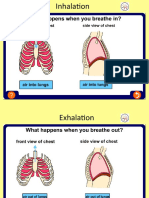
- Asthma Inhale and ExhaleDokumen14 halamanAsthma Inhale and ExhaleNguyen Nhu VinhBelum ada peringkat
- MBBS - General Medicine Reg Id: KMC - 142105 RX ID: 406824261Dokumen1 halamanMBBS - General Medicine Reg Id: KMC - 142105 RX ID: 406824261Dipam HalderBelum ada peringkat
- He367t R1 RCDokumen2 halamanHe367t R1 RCSedighe VafaieBelum ada peringkat
- Toacs 5Dokumen244 halamanToacs 5Mobin Ur Rehman Khan100% (2)
- J Paediatrics Child Health - 2017 - Halliday - The Fascinating Story of SurfactantDokumen6 halamanJ Paediatrics Child Health - 2017 - Halliday - The Fascinating Story of SurfactantTin TomašićBelum ada peringkat
- Introduction To Epidemiology of Infection Diseases PDFDokumen17 halamanIntroduction To Epidemiology of Infection Diseases PDFRovaidKhanBelum ada peringkat
- Chapter 1 - Orientation To PharmacologyDokumen4 halamanChapter 1 - Orientation To Pharmacologydlneisha61Belum ada peringkat
- AGada TantraDokumen3 halamanAGada TantraGuru Prasad100% (1)
- Brain injury patterns in hypoxiaDokumen7 halamanBrain injury patterns in hypoxiaDr.Deepak S MD,MRCPCHBelum ada peringkat
- General Concepts in PharmacotherapyDokumen40 halamanGeneral Concepts in PharmacotherapyBindira MaharjanBelum ada peringkat
- Ozone - A Wide Spectrum Healer by Gary Null PHDDokumen20 halamanOzone - A Wide Spectrum Healer by Gary Null PHDangelakimba100% (4)
- 2013 Pankaj R BodadeDokumen8 halaman2013 Pankaj R BodadeGeorge StoicaBelum ada peringkat
- Food Classes: FAT Water Vitamins, Minerals, & Roughage ProteinDokumen25 halamanFood Classes: FAT Water Vitamins, Minerals, & Roughage Proteinuminoriah80% (5)
- Nicola Zammitt, - Alastair O'Brien - Essentials of Kumar & Clark's Clinical Medicine-Elsevier (2017) PDFDokumen927 halamanNicola Zammitt, - Alastair O'Brien - Essentials of Kumar & Clark's Clinical Medicine-Elsevier (2017) PDFJamie Baczewski100% (8)