Case ReportMalnutrition
Diunggah oleh
Nofilia Citra CandraJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Case ReportMalnutrition
Diunggah oleh
Nofilia Citra CandraHak Cipta:
Format Tersedia
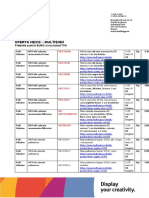
Clinical Exposure
1. Data Pasien
Jenis Kelamin: wanita
Usia : 2 tahun 11 bulan
Berat : 8! "# $in##i : 81 cm
%tatus e"onomi: ren&ah
2. 'namnesis
Keluhan utama
(#antu" lemas &an ti&a" bertena#a &an berat ba&an ti&a"
bertambah.
Keluhan lain
$i&a" a&a
)iwa*at pen*a"it ter&ahulu
$i&a" a&a riwa*at *an# si#ni+"an
)iwa*at pen*a"it "eluar#a
$i&a" a&a riwa*at *an# si#ni+"an
,ainn*a
'na" pertama. Pen&apatan *an# san#at ren&ah sehin##a oran# tua
san#at sulit untu" mencu"upi "ebutuhan +si" ana".
!. Pemeri"saan -isi"
.eart rate : 11/ 01min
Bloo& pressure : 2/13/
)espirator* rate : !/ 01min
4nspection : $hin rib apparent limbs loo"e& small marasmic
apperance
Palpation : ,i5er an& spleen are normal no pain in
ab&omen
Percussion : (o mass no or#ans enlar#ement no pain
'uscultation : ,i5er an& spleen are normal no bruit soun&
normal intestine soun&
timpani soun& on epi#astric
'nthropometr* : B64 : 12378Un&er 79Percentile: Born wei#ht :
!"#
;. Pemeri"saan penun<an# *an# perlu &ila"u"an
,aborator* %tu&ies
$he most help=ul laborator* stu&ies in assessin# malnutrition in a
chil& are hematolo#ical stu&ies an& laborator* stu&ies e5aluatin#
protein status.
o .ematolo#ical stu&ies shoul& inclu&e a CBC count with )BC
in&ices an& a peripheral smear. $his coul& also help exclu&e
anemias =rom nutritional &e+ciencies such as iron =olate an&
5itamin B912 &e+ciencies.
o 6easures o= protein nutritional status inclu&e serum albumin
retinol9bin&in# protein prealbumin trans=errin creatinine
an& BU( le5els. )etinol9bin&in# protein prealbumin an&
trans=errin &eterminations are much better short9term
in&icators o= protein status than albumin. .owe5er in the +el&
a better measure o= lon#9term malnutrition is serum albumin
because o= its lon#er hal=9li=e.
'&&itional &ia#nostic e5aluation
o 4n chil&ren who ha5e a histor* o= a&e>uate =oo& inta"e an&
si#ns1s*mptoms o= malnutrition =ocus on i&enti=*in# the cause
o= malnutrition. Per=orm laborator* stu&ies base& on
in=ormation =rom a complete histor* an& ph*sical examination.
o 4nitial &ia#nostic laborator* stu&ies inclu&e a CBC count
se&imentation rate serum electrol*tes an& urinal*sis an&
culture. %tool specimens shoul& be obtaine& i= the chil& has a
histor* o= abnormal stools or stoolin# patterns or i= the =amil*
uses an unreliable or >uestionable source o= water.
o '&&itional stu&ies ma* =ocus on th*roi& =unctions or sweat
chlori&e tests particularl* i= hei#ht 5elocit* is abnormal.
-urther &ia#nostic stu&ies shoul& be &etermine& as &ictate& b*
the histor* an& ph*sical examination. -or example lab tests
e5aluatin# renal =unction such as phosphorus an& calcium
shoul& be obtaine& in the presence o= renal s*mptoms.
Chil&ren with suspecte& li5er &isease shoul& ha5e tri#l*ceri&e
an& 5itamin le5els obtaine& while ?inc le5els shoul& be
obtaine& in patients with chronic &iarrhea.
Celiac serolo#* is a use=ul screenin# test an& shoul& be consi&ere&
especiall* i= there is a =amil* histor* o= celiac &isease or i= other
autoimmune &iseases such as t*pe 4 &iabetes mellitus are present.
7. )in#"asan
@irl 2 *ears 11 months 8! "# with 81 cm hei#ht. .eart rate
11/ 01min BP 2/13/ )) !/ 01min. 4nspection +n& $hin rib apparent
limbs loo"e& small marasmic apperance. Palpation an& percussion
+n&in# normal. 'uscultation +n&in#s li5er an& spleen are normal no
bruit soun& normal intestine soun& timpani soun& on epi#astric.
3. Dia#nosis
Aor"in# &ia#nosis
6arasmus
DiBerential &ia#nosis
Kwashior"or 6arasmus Kwashior"or
7. Diagnostic reasoning
Dia#nostic reasonin# an& &iBerential &ia#nosis
6arasmus li"el* become the &ia#nosis. Unable to thri5e or
catch9up is a car&inal si#n =or malnutrition especiall* people in rural
area with low income population. Kwashior"or an& 6arasmus
Kwashior"or can be exclu&e& because these &isease si#n is oe&ema
on ab&omen.
8. Patient Reaction
-eelin#s : ,ethar#*
4nsi#ht : .er mother "now that her &au#hter lac" o= nutrition but
she canCt aBor&
=oo& to =ee& her &au#hter
-ear : %he =eels sa& with her &au#hter con&ition
Expectations : %he hope her &au#hter reco5er as =ast as possible
2. Disease )e5iew
Malnutrition is globally the most important risk factor for illness and death,
contributing to more than half of deaths in children worldwide; child
malnutrition was associated with 54% of deaths in children in developing
countries in 200!
"rotein#energy malnutrition $"%M&, 'rst described in the
(20s, is observed most fre)uently in developing countries but has been
described with increasing fre)uency in hospitali*ed and chronically ill children
in the +nited ,tates! -he e.ects of changing environmental conditions in
increasing malnutrition is multifactorial! "oor environmental conditions may
increase insect and proto*oal infections and also contribute to environmental
de'ciencies in micronutrients! /verpopulation, more commonly seen in
developing countries, can reduce food production, leading to inade)uate food
intake or intake of foods of poor nutritional )uality! 0onversely, the e.ects of
malnutrition on individuals can create and maintain poverty, which can
further hamper economic and social development!
Marasmus involves inade)uate intake of protein and calories, whereas a child
with kwashiorkor has fair#to#normal calorie intake with inade)uate protein
intake! 1lthough signi'cant clinical di.erences between kwashiorkor and
marasmus are noted, some studies suggest that marasmus represents an
adaptation to starvation whereas kwashiorkor represents a dysadaptation to
starvation! 2n addition to "%M, children may be a.ected by micronutrient
de'ciencies, which also have a detrimental e.ect on growth and
development! -he most common and clinically signi'cant micronutrient
de'ciencies in children and childbearing women throughout the world include
de'ciencies of iron, iodine, *inc, and vitamin 1 and are estimated to a.ect as
many as two billion people! 1lthough forti'cation programs have helped
diminish de'ciencies of iodine and vitamin 1 in individuals in the +nited
,tates, these de'ciencies remain a signi'cant cause of morbidity in
developing countries, whereas de'ciencies of vitamin 0, 3, and 4 have
improved in recent years! Micronutrient de'ciencies and protein and calorie
de'ciencies must be addressed for optimal growth and development to be
attained in these individuals!
Pathoph*siolo#*
Malnutrition a.ects virtually every organ system! 4ietary protein is
needed to provide amino acids for synthesis of body proteins and other
compounds that have various functional roles! %nergy is essential for all
biochemical and physiologic functions in the body! 5urthermore,
micronutrients are essential in many metabolic functions in the body as
components and cofactors in en*ymatic processes! 2n addition to the
impairment of physical growth and of cognitive and other physiologic
functions, immune response changes occur early in the course of signi'cant
malnutrition in a child! -hese immune response changes correlate with poor
outcomes and mimic the changes observed in children with ac)uired immune
de'ciency syndrome $124,&! 6oss of delayed hypersensitivity, fewer -
lymphocytes, impaired lymphocyte response, impaired phagocytosis
secondary to decreased complement and certain cytokines, and decreased
secretory immunoglobulin 1 $2g1& are some changes that may occur! -hese
immune changes predispose children to severe and chronic infections, most
commonly, infectious diarrhea, which further compromises nutrition causing
anore7ia, decreased nutrient absorption, increased metabolic needs, and
direct nutrient losses!
%arly studies of malnourished children showed changes in the
developing brain, including, a slowed rate of growth of the brain, lower brain
weight, thinner cerebral corte7, decreased number of neurons, insu8cient
myelini*ation, and changes in the dendritic spines! More recently,
neuroimaging studies have found severe alterations in the dendritic spine
apparatus of cortical neurons in infants with severe protein#calorie
malnutrition! -hese changes are similar to those described in patients with
mental retardation of di.erent causes! -here have not been de'nite studies
to show that these changes are causal rather than coincidental!
4
/ther pathologic changes include fatty degeneration of the liver and
heart, atrophy of the small bowel, and decreased intravascular volume
leading to secondary hyperaldosteronism!
4nternational Epi&emiolo#*
-he 9orld :ealth /rgani*ation estimates that by the year 205, the
prevalence of malnutrition will have decreased to ;!<% globally, with =!4
million children younger than 5 years a.ected as measured by low weight for
age! -he overwhelming ma>ority of these children, 2!? million, will live in
developing countries with ;0% of these children in 1sia, particularly the
southcentral region, and 2<% in 1frica! 1n additional <5 million $2(!0%&
children will have stunted length@height secondary to poor nutrition!
0urrently, more than half of young children in ,outh 1sia have "%M,
which is <!5 times the prevalence in the western hemisphere! 2n sub#,aharan
1frica, =0% of children have "%M! 4espite marked improvements globally in
the prevalence of malnutrition, rates of undernutrition and stunting have
continued to rise in 1frica, where rates of undernutrition and stunting have
risen from 24% to 2<!?% and 4;!=% to 4?%, respectively, since ((0, with
the worst increases occurring in the eastern region of 1frica!
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- HISTORY AND PHYSICAL EXAMINATION (Putul)Dokumen2 halamanHISTORY AND PHYSICAL EXAMINATION (Putul)Reshma Francis100% (1)
- Yoga Your Home Practice CompanionDokumen257 halamanYoga Your Home Practice Companionjohncoltrane97% (33)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Case Report ChickenpoxDokumen6 halamanCase Report ChickenpoxNofilia Citra CandraBelum ada peringkat
- AGIL ParadigmDokumen3 halamanAGIL ParadigmNofilia Citra Candra83% (6)
- Clinical Case Report on GERD Diagnosis and TreatmentDokumen7 halamanClinical Case Report on GERD Diagnosis and TreatmentNofilia Citra CandraBelum ada peringkat
- Test Buat UnileverDokumen5 halamanTest Buat UnileverNofilia Citra CandraBelum ada peringkat
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Lester Desjarlais Inquest Parts I and IIDokumen108 halamanLester Desjarlais Inquest Parts I and IIJames Turner100% (1)
- Process Design For 1.70 IFAS STPDokumen18 halamanProcess Design For 1.70 IFAS STPGenesis International0% (1)
- Myastenia Grafis. SuryaDokumen13 halamanMyastenia Grafis. SuryaNofilia Citra CandraBelum ada peringkat
- Ponv Prevention in General Anesthesia Patients - Siap EmailDokumen4 halamanPonv Prevention in General Anesthesia Patients - Siap EmailNofilia Citra CandraBelum ada peringkat
- Arteri LineDokumen13 halamanArteri LineNofilia Citra Candra100% (1)
- Diabetes TBDokumen2 halamanDiabetes TBAuladi Lubis ∑Belum ada peringkat
- Hemodynamic Monitoring I ABP CVP AoDokumen35 halamanHemodynamic Monitoring I ABP CVP AoNofilia Citra CandraBelum ada peringkat
- Myasthenia Gravis: An Overview of Its Anatomy, Pathophysiology, Clinical Presentation, Diagnosis and TreatmentDokumen41 halamanMyasthenia Gravis: An Overview of Its Anatomy, Pathophysiology, Clinical Presentation, Diagnosis and TreatmentNofilia Citra CandraBelum ada peringkat
- Myastenia Grafis. SuryaDokumen13 halamanMyastenia Grafis. SuryaNofilia Citra CandraBelum ada peringkat
- Maxilofacial Trauma: Presenter: - Wisnu Adiputra (07120080072) - Nofilia Citra Candra (07120090066)Dokumen97 halamanMaxilofacial Trauma: Presenter: - Wisnu Adiputra (07120080072) - Nofilia Citra Candra (07120090066)Nofilia Citra CandraBelum ada peringkat
- Icu Enteral Feeding GuidelinesDokumen12 halamanIcu Enteral Feeding GuidelinesNofilia Citra CandraBelum ada peringkat
- Neural Mechanisms Involved in Controlling Eating BehaviourDokumen4 halamanNeural Mechanisms Involved in Controlling Eating BehaviourNofilia Citra CandraBelum ada peringkat
- Bahan Baca LapjagDokumen1 halamanBahan Baca LapjagNofilia Citra CandraBelum ada peringkat
- Cardiomyopathy 2Dokumen84 halamanCardiomyopathy 2O.r. CadzBelum ada peringkat
- Cara Baca Foto ThoraxDokumen23 halamanCara Baca Foto ThoraxNofilia Citra CandraBelum ada peringkat
- Signal Transduction and Regulation Lecture 1 PW Point 2003Dokumen63 halamanSignal Transduction and Regulation Lecture 1 PW Point 2003Nofilia Citra CandraBelum ada peringkat
- NystagmusDokumen14 halamanNystagmusaks008inBelum ada peringkat
- Vascularization and Cortex of The Brain-2011Dokumen34 halamanVascularization and Cortex of The Brain-2011Nofilia Citra CandraBelum ada peringkat
- CSF and Cerebral Blood FlowDokumen58 halamanCSF and Cerebral Blood FlowCindy PrayogoBelum ada peringkat
- Answer For Unilever TestDokumen3 halamanAnswer For Unilever TestNofilia Citra Candra0% (1)
- DR - Anggraini - Development of Gastrointestinal SystemDokumen16 halamanDR - Anggraini - Development of Gastrointestinal SystemNofilia Citra CandraBelum ada peringkat
- Management of Diarrhea: Non-Drug and Drug TherapyDokumen40 halamanManagement of Diarrhea: Non-Drug and Drug TherapyNofilia Citra CandraBelum ada peringkat
- Abdominal PainDokumen51 halamanAbdominal PainNofilia Citra CandraBelum ada peringkat
- Drugs For Osteoarthritis Revise 2010Dokumen65 halamanDrugs For Osteoarthritis Revise 2010Nofilia Citra CandraBelum ada peringkat
- Nerve InjuryDokumen46 halamanNerve InjuryNofilia Citra CandraBelum ada peringkat
- Men in Go EncephalitisDokumen1 halamanMen in Go EncephalitisNofilia Citra CandraBelum ada peringkat
- Complete VaccinationDokumen2 halamanComplete VaccinationNgoo NwosuBelum ada peringkat
- Reiki Tummo Brochure 2013Dokumen2 halamanReiki Tummo Brochure 2013Alicia TerryBelum ada peringkat
- UV-VIS Method for Estimating Fat-Soluble Vitamins in MultivitaminsDokumen6 halamanUV-VIS Method for Estimating Fat-Soluble Vitamins in MultivitaminsTisenda TimiselaBelum ada peringkat
- Week 4-Physical Fitness TestDokumen38 halamanWeek 4-Physical Fitness TestCatherine Sagario OliquinoBelum ada peringkat
- Nursing Assignment SampleDokumen12 halamanNursing Assignment Sampleswetha swethaBelum ada peringkat
- Hahnemann Advance MethodDokumen2 halamanHahnemann Advance MethodRehan AnisBelum ada peringkat
- AMD UpdatedDokumen258 halamanAMD UpdatedmcolossodBelum ada peringkat
- Everett Association of School Administrators (EASA) Administrative HandbookDokumen46 halamanEverett Association of School Administrators (EASA) Administrative HandbookJessica OlsonBelum ada peringkat
- Come Back To Your Senses Use Your Body: Psychologyt LsDokumen1 halamanCome Back To Your Senses Use Your Body: Psychologyt LsMarina Moran100% (1)
- Survival of The Sickest PresentationDokumen24 halamanSurvival of The Sickest Presentationapi-255985788Belum ada peringkat
- GastroparesisDokumen10 halamanGastroparesisapi-437831510Belum ada peringkat
- Journal Club Presentation: DR Waleed AhmadDokumen30 halamanJournal Club Presentation: DR Waleed Ahmadkaram aliBelum ada peringkat
- MANAGEMENT AND PREVENTIONDokumen6 halamanMANAGEMENT AND PREVENTIONIrina BalutaBelum ada peringkat
- Voyeuristic Disorder SymptomsDokumen7 halamanVoyeuristic Disorder SymptomsgoyaBelum ada peringkat
- Heart Failure Lily ModifiedDokumen57 halamanHeart Failure Lily ModifiedSabila FatimahBelum ada peringkat
- Boy Scouts Lipa City Investiture CampDokumen1 halamanBoy Scouts Lipa City Investiture CampAndro Brendo VillapandoBelum ada peringkat
- RNTCP - Wikipedia, The Free EncyclopediaDokumen5 halamanRNTCP - Wikipedia, The Free EncyclopediaakurilBelum ada peringkat
- Oferta Hexis - Multisign: Preturile Sunt in EURO Si Nu Includ TVADokumen9 halamanOferta Hexis - Multisign: Preturile Sunt in EURO Si Nu Includ TVAPoschina CiprianBelum ada peringkat
- Paul B. Bishop, DC, MD, PHD, Jeffrey A. Quon, DC, PHD, FCCSC, Charles G. Fisher, MD, MHSC, FRCSC, Marcel F.S. Dvorak, MD, FRCSCDokumen10 halamanPaul B. Bishop, DC, MD, PHD, Jeffrey A. Quon, DC, PHD, FCCSC, Charles G. Fisher, MD, MHSC, FRCSC, Marcel F.S. Dvorak, MD, FRCSCorlando moraBelum ada peringkat
- Methodology Tapping Methodology of WaterlineDokumen15 halamanMethodology Tapping Methodology of WaterlineBryBelum ada peringkat
- Module 7 Health Insurance Types and ImportanceDokumen10 halamanModule 7 Health Insurance Types and ImportanceKAH' CHISMISSBelum ada peringkat
- Second Trimester Complications 2015Dokumen64 halamanSecond Trimester Complications 2015gibreilBelum ada peringkat
- Stericon Plus BioindicatorDokumen4 halamanStericon Plus Bioindicatorupt labkeswanbaliBelum ada peringkat
- IWA Publishing - Anaerobic Reactors For Sewage Treatment - Design, Construction and Operation - 2020-01-10Dokumen1 halamanIWA Publishing - Anaerobic Reactors For Sewage Treatment - Design, Construction and Operation - 2020-01-10JOHNY ALEJANDRO GARCIA SEPULVEDABelum ada peringkat
- Digestive System PowerpointDokumen33 halamanDigestive System PowerpointThomas41767% (6)
- Stetler Model EBP PosterDokumen1 halamanStetler Model EBP PosterEmily MBelum ada peringkat