Cervical Spine Injury
Diunggah oleh
hesti06taniuchiDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Cervical Spine Injury
Diunggah oleh
hesti06taniuchiHak Cipta:
Format Tersedia
Cervical Spine Injury
Introduction
Flow chart
Immobilisation
Radiology
Clearing c-spine
Proven c-spine injury or c-spine cannot be cleared
Ongoing care
Pressure area care
See also: Radiology guideline- Acute indications
Introduction
Traumatic injuries of the cervical spine are uncommon in children. However in many
circumstances it is prudent to assume there is a cervical spine injury until examination and x-
rays prove otherwise.
It is often challenging to assess and immobilise children when a cervical spine injury is
suspected. Constant reassurance is required to help keep the child still and reduce their
anxiety levels. Depending on the age of the child and their level of anxiety, cooperation may
be reduced. If the child is uncooperative and a thorough examination is not possible, the
collar must stay on and further assessment completed when cooperation has been established.
This document provides a framework for the management of a child with a possible cervical
spine injury at the R.C.H.
Flow Chart
Click to see flow chart
Immobilisation
Patients with suspected or possible cervical spine injury must have their cervical spine
properly immobilised until formal assessment occurs.
Who to immobilise:
The unconscious patient with a history of possible trauma must be immobilised.The
conscious patient with any of the following:
A mechanism of injury that may indicate risk of spinal injury:
o Pedestrian / cyclist hit > 30km/hr.
o Passenger - collision > 60km/hr.
o Fall - more than 3 meters.
o Kicked / fall from a horse.
o Backed over by a car.
o Thrown from vehicle.
o Thrown over handlebars of bike.
o Severe electric shock.
Multiple trauma
Significant injury above clavicles
Trauma & Unexplained hypotension
History of neck trauma
Neck tenderness
Limitations of neck movement due to pain
Neurological deficit
Other major injuries (e.g. fractured limbs, abdominal injury)
How to immobilise the cervical spine:
Fit a once-piece hard collar (see sizing below)
Children <3yo are especially difficult. Rigid cervical collars do not usually fit. They
should be immobilised with parents or staff holding the head and body, or sandbags or
towels in situ and, if cooperative, the head taped to the board.
If uncooperative, avoid rigidly fixing head to trolley or spinal board unless body also
strapped to board as more damage can be done by a child who is thrashing their body
around while their head is strapped to the board.
If the patient's head is attached to the bed, be particularly aware of vomiting and risk
of aspiration - someone must be with the patient at all times.
In the acute phase there is no place for sedation without intubation to aid cervical
spine immobilisation. However analgesia is an important consideration in trauma
patients.
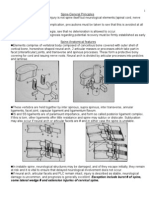
Sizing a One piece Hard collar ("Stiffneck" collar is used at the RCH):
A one piece hard collar is used in the initial stage (image 3)
Measure the distance from the top of the patient's shoulder to the angle of the jaw
with your hand (image 1)
On the "Stiffneck" collar, measure from the bottom of the rigid plastic to the
"measuring post". This should correspond to the above measurement (image 2)
Image 1: Measuring collar
Image 2: Measuring neck
Image 3: Appropriately fitting collar
Patient position, head immobiliser, rolled towels & tapes:
Lie flat on back with staff or parents holding.
If cooperative - consider rolled towels and tape head to spinal board, towels or head
immobiliser (not trolley) to maintain alignment and keep still.
Spinal boards:
Can aid spinal immobilisation in early assessment phase of major trauma but should
be removed as soon as possible. Patients should not leave the emergency department
whilst still on a spinal board.
For patients < 8yo lying on a spinal board, the large occiput causes neck flexion.
These patients should have extra padding under the body but not head (eg. folded
blanket) to keep neck in neutral position.
Spinal boards cause significant patient discomfort and can result in pressure ulcers.
Once a decision is made to immobilise the patient the hard collar should remain on or until
cervical spine is cleared. (see - Clearing the c-spine of injury).
Radiology
Who to x-ray:
X-ray
o Patient has altered conscious state or
o Adequate assessment of neck symptoms not possible due to distracting injury
or intoxication/sedation or
o Neck tenderness or pain or
o Abnormal neurological signs
Do not x-ray
o Patient is alert and has normal conscious state and
o No distracting injury, intoxication or sedation etc. and No neck pain or
tenderness and
o Normal neurological examination
How to x-ray
A doctor or nurse from Emergency or Intensive Care MUST accompany the patient to
radiology for imaging to ensure maintenance of cervical spine immobilisation and
airway management.
The patient must be transferred onto the XR table using a patient-slide keeping the
spine in-line and with the head being held.
The x-rays are taken on the XR table without lifting or moving the patient's head.
The patient is transferred off the table with the same precautions used to move them
on.
The hard collar should remain in place during the cervical spine xray series.
What to x-ray
a. Lateral c-spine (portable) will be taken in ED/ICU for:
o All major trauma patients (along with trauma series - Pelvis on needs only
basis)
o Other patients who need portable x-ray for other reason (e.g. chest x-rays
o This does not exclude an unstable injury.
b. Cervical series will be taken in Radiology (Lat. / AP / Odontoid view (>/=5 yo)):
o If the cervicothoracic junction has not been satisfactorily imaged, a swimmer's
view will be obtained. A single attempt should be made
o Oblique views will only be done if required by the orthopaedic or
neurosurgical unit.
o Flexion and extension views are inappropriate in the acute stage and will not
be performed.
Patients requiring c-spine CT scan:
Must be discussed with the emergency consultant or unit registrar
All intubated patients requiring CT brain should have CT c-spine performed at the
same time
Patients in whom the cranio-cervical or cervico-thoracic junction remain obscured
after a single extra view should not have repeated attempts at plain imaging but have a
CT of the relevant area
Patients with abnormalities on plain c-spine xrays should have a CT of the relevant
area
Note: If imaging is necessary, a full c-spine series or CT scan must still be completed prior to
removal of the collar.
Clearing the c-spine of injury
Who can clear the c-spine?
If the patient is to be discharged from the ED, the Registrar from the following units may
clear the c-spine after discussion with the ED Consultant on duty:
Emergency
Intensive Care
Orthopaedic
Neurosurgery
General Surgery
The Registrar making the decision should be EMST / APLS (or equivalent) trained. If the
patient is an inpatient or potentially an inpatient the c-spine can only be cleared after
consultation with the Neurosurgical or Orthopaedic Consultant, or the Emergency consultant
if the patient is still in the ED.
How to clear the c-spine:
Clearing the c-spine on clinical grounds:
Examine the patient: Collar is removed and, while a senior staff member maintains the head
alignment, the examining doctor checks for the following points in sequential order:
1. Can pain and tenderness be assessed?
2. Are there other distracting injuries? (Another injury in this patient that distracts from
possible spinal injury)
3. Is there midline neck pain?
4. Is there tenderness over the cervical spine?
5. Are there any motor or sensory abnormalities?
6. Is there limitation of active neck movement?
7. Is there limitation to head control?
If these are all absent the collar may be removed.
If any of these are present imaging is warranted
Clearing the c-spine after radiology:
It is imperative that the person making the decision has both examined the patient and viewed
the films.
1. View the films: The examining Doctor must view the films. If there is any doubt about the
'normality' of the films a second opinion should be sought.
2. Re-examine the patient: Collar is removed and, while a senior staff member maintains the
head alignment, the examining doctor checks for the above points in sequential order: (see
above)
If either the films or examination cannot be adequately cleared the cervical collar should
remain insitu. (See - Ongoing care)
Documenting the c-spine clearance:
Spinal clearance (or inability to clear the c-spine) MUST be documented by the examining
doctor in either the 'Major Trauma management record - Medical' or in the patient's history as
soon as a decision is made so all staff are aware and appropriate care provided. If the spine is
not cleared a plan for further assessment of the spine must also be documented, and a two
piece hard collar should be fitted.
It is imperative that this decision is made quickly so that, if cleared, the collar can be
removed.
Proven cervical spine injury or cervical spine cannot be
cleared
Careful neurological examination
Refer patients with isolated bony injury to Orthopaedics
Refer patients with any neurological deficit to Neurosurgery.
Admit all major trauma patients under general surgery.
Imaging of the spine should include plain films plus CT of the affected area, with
MRI for imaging of the spinal cord.
Ongoing Care
Guidelines for timing of fitting long term hard (Aspen) collars:
(a) For patients being discharged:
If imaging is normal and there is ongoing tenderness of the posterior c-spine but the
patient is well enough to be discharged, a two piece Aspen (or Philadelphia) collar
should be applied.
The patient should be brought back to Fracture clinic within 2 weeks for review
(discuss with orthopaedic registrar).
(b) For admitted patients:
By 6 hours, a c-spine injury decision should be made & ideally the one-piece hard
collar is changed to a two piece Aspen (or Philadelphia) collar within 6 hrs if the c-
spine cannot be cleared. The patient must not go any longer than 12 hours in a one-
piece hard collar. If at 12 hours the decision has still not been finalised a two-piece
collar must be fitted regardless; Contact Orthotics department (x5870).
Pressure area care (PAC)
Children <3 years old - greatest area for pressure ulcer is the occiput.
Children >/=3 years old - greatest area for pressure ulcer is sacrum & heels.
Children must be removed from spinal board as soon as possible.
Pressure area care must be considered throughout the resuscitation phase.
Every 2 hours (pressure must be relieved from all bony prominence at least every 2
hours):
Collar must be removed: 2 people, one holding head in alignment the other
removing the collar, cleaning under collar area observing for areas of redness or
breakdown. Clean the collar.
Log roll: Depending on size of patient: 2-4 people to log roll (supporting head,
shoulder and torso, hips and legs)
o Log rolling must be done with the one or two piece hard collar on. Observing
in particular heels, hips, and occiput for pressure areas.
Feet and legs: Passive range of motion and PAC with particular attention to heels.
Orthotics may be required to keep feet in alignment.
Positioning:
Ideal positioning:
Flat on back
Hourly PAC
Bed tilting - (if the head is to be elevated for neurological reasons):
If none of the spine has been cleared the bed should be tilted maintaining body
alignment- trendelenburg tilting.
If everything but the c-spine has been cleared then the bed can be tilted from the hips.
Side to side:
Only once c-spine cleared or fused or at the direction of neurosurgical or orthopaedic
consultant.
No other injuries that contraindicate side to side positioning (e.g. # pelvis).
Consider use of spinal bed.
Air mattresses:
Should not be used for patients that have not had their cervical spine cleared.
May be used once the c-spine has been cleared or spinal fusion has taken place.
If cervical spine cannot be cleared but the mattress is required for pressure area care,
these individual cases must be taken up with the Orthopaedic and/or Neurosurgical
team looking after the patient.
Anda mungkin juga menyukai
- Spinal Immobilization: By: Hatem AlsrourDokumen16 halamanSpinal Immobilization: By: Hatem Alsrourhatem alsrour100% (2)
- Presentation Cervical SpineDokumen48 halamanPresentation Cervical Spinekholoodrezeq8752Belum ada peringkat
- C.1. 0Dokumen8 halamanC.1. 0Bahna LucianBelum ada peringkat
- Summary of Cervical Spine Injury GuidelinesDokumen9 halamanSummary of Cervical Spine Injury GuidelinesAnonymous tN25joEXfLBelum ada peringkat
- Box 7-1 Guidelines For Screening Patients With Suspected Spine InjuryDokumen1 halamanBox 7-1 Guidelines For Screening Patients With Suspected Spine InjuryMarios GhobrialBelum ada peringkat
- TRIAGE - R.P.M. Method for Prioritizing Burn and Spine Injury PatientsDokumen84 halamanTRIAGE - R.P.M. Method for Prioritizing Burn and Spine Injury PatientsArioBelum ada peringkat
- Chapter 6: Spine and Spinal Cord Trauma ObjectivesDokumen23 halamanChapter 6: Spine and Spinal Cord Trauma ObjectivesfadhillahilmayantiBelum ada peringkat
- Practice Guidelines: Cervical Spine ClearanceDokumen2 halamanPractice Guidelines: Cervical Spine ClearanceAnthony AlamBelum ada peringkat
- Spine and Spinal Cord InjuryDokumen52 halamanSpine and Spinal Cord InjuryAdhi WiratmaBelum ada peringkat
- Clearing The Cervical Spine: DR Claudia AY Cheng Senior Medical Officer Department of Anaesthesia and Intensive CareDokumen78 halamanClearing The Cervical Spine: DR Claudia AY Cheng Senior Medical Officer Department of Anaesthesia and Intensive CareVictor ChanBelum ada peringkat
- Fractures of Clavicle 1Dokumen41 halamanFractures of Clavicle 1Noor Al Zahraa AliBelum ada peringkat
- Traction Day 4Dokumen3 halamanTraction Day 4shushmaBelum ada peringkat
- Trauma Clinical Guideline 2017Dokumen7 halamanTrauma Clinical Guideline 2017Paolo ContrerasBelum ada peringkat
- GuideDokumen3 halamanGuideRachelle Danya Dela RosaBelum ada peringkat
- Pediatric Cervical Spinal Motion RestrictionDokumen10 halamanPediatric Cervical Spinal Motion RestrictionRita ValenteBelum ada peringkat
- Indications for Spinal SurgeryDokumen2 halamanIndications for Spinal SurgeryMichael PrayogoBelum ada peringkat
- Cervical TractionDokumen4 halamanCervical TractionGabbii CincoBelum ada peringkat
- Cervical Spine Workshop: Chris Dillon, MD Regions Emergency Medicine Residency ProgramDokumen89 halamanCervical Spine Workshop: Chris Dillon, MD Regions Emergency Medicine Residency ProgramAldi.SiregarBelum ada peringkat
- Spinal cord injury acute careDokumen11 halamanSpinal cord injury acute careKingsley Martinez CastroBelum ada peringkat
- Shoulder Dislocation Background: Shoulder Dislocations Traumatic InjuryDokumen7 halamanShoulder Dislocation Background: Shoulder Dislocations Traumatic Injuryanastasiaanggita_265Belum ada peringkat
- Xrays 123Dokumen13 halamanXrays 123Rasheed OladipupoBelum ada peringkat
- Pediatric Surgery PectusDokumen4 halamanPediatric Surgery Pectustes_syBelum ada peringkat
- Spinal Care Bundle FINAL With Photos Ver 4-1-28!02!12llzllxzlxzlxz ZzkjskdjsdsDokumen27 halamanSpinal Care Bundle FINAL With Photos Ver 4-1-28!02!12llzllxzlxzlxz ZzkjskdjsdsTheo Chairul TheGunnersBelum ada peringkat
- Trauma To The Vertebral Column and Spinal CordDokumen14 halamanTrauma To The Vertebral Column and Spinal CordLory cBelum ada peringkat
- Trauma To The Vertebral Column and Spinal CordDokumen14 halamanTrauma To The Vertebral Column and Spinal CordБека ЭзугбаяBelum ada peringkat
- Trauma To The Vertebral Column and Spinal CordDokumen14 halamanTrauma To The Vertebral Column and Spinal CordEdwardRazvanBelum ada peringkat
- Bilateral Inter-Faceted Dislocation of Cervical Spine: Closed Reduction With Traction Weights - Small and Slow or Lose It All (Neurology)Dokumen10 halamanBilateral Inter-Faceted Dislocation of Cervical Spine: Closed Reduction With Traction Weights - Small and Slow or Lose It All (Neurology)ICBelum ada peringkat
- Trauma To The Vertebral Column and Spinal CordDokumen14 halamanTrauma To The Vertebral Column and Spinal CordSilviu MorteanuBelum ada peringkat
- Fundamentals of Chest RadiologyDokumen119 halamanFundamentals of Chest RadiologyAlexandra DîrțuBelum ada peringkat
- Exception Include Burst # of Spine, Some Lateral Wedge # and Extension Injuries of Cervical SpineDokumen29 halamanException Include Burst # of Spine, Some Lateral Wedge # and Extension Injuries of Cervical Spinebhavesh jain100% (2)
- Shoulder-Acromioclavicular Separation PDFDokumen13 halamanShoulder-Acromioclavicular Separation PDFFebrian ParuraBelum ada peringkat
- Shoulder ComplexxDokumen26 halamanShoulder Complexxbhavesh jainBelum ada peringkat
- Logroll Guideline R CP RNSHDokumen8 halamanLogroll Guideline R CP RNSHAnonymous ENdoGXxsnBelum ada peringkat
- SPINE TRAUMA DIAGNOSIS AND EVALUATIONDokumen96 halamanSPINE TRAUMA DIAGNOSIS AND EVALUATIONSherlockHolmesSezBelum ada peringkat
- Module 9Dokumen7 halamanModule 9Dumahil Cristina AmbosBelum ada peringkat
- Spine InjuriesDokumen58 halamanSpine InjuriesVinwin777Belum ada peringkat
- DDH Treatment - PFDokumen30 halamanDDH Treatment - PFHendra SantosoBelum ada peringkat
- Evaluating and Managing Suspected Spinal InjuriesDokumen26 halamanEvaluating and Managing Suspected Spinal InjuriesAlen NotanubunBelum ada peringkat
- Brachial Plexus InjuryDokumen20 halamanBrachial Plexus InjurySuci PramadianiBelum ada peringkat
- Kuliah Blok Neuroscience-SpineDokumen27 halamanKuliah Blok Neuroscience-SpineCox AbeeBelum ada peringkat
- Svoa Ne 02 020Dokumen10 halamanSvoa Ne 02 020Trina ViskhawatBelum ada peringkat
- 28 C.fracture of SpineDokumen4 halaman28 C.fracture of SpineNoor Hazilla WatyBelum ada peringkat
- Sci Acute ManagementDokumen8 halamanSci Acute ManagementRyan Victor ManaloBelum ada peringkat
- Cervical Spine AnatomyDokumen67 halamanCervical Spine AnatomyAnonymous glhczXqdDBelum ada peringkat
- Dr. Yoyos - Acute Cervical Injury FinalDokumen30 halamanDr. Yoyos - Acute Cervical Injury FinalRsud Malinau Ppk BludBelum ada peringkat
- MRI Shoulder Protocol: Preparation, Positioning and Imaging StepsDokumen27 halamanMRI Shoulder Protocol: Preparation, Positioning and Imaging Stepsدخ D5Belum ada peringkat
- Lecture 3&4Dokumen9 halamanLecture 3&4Irfan NashadBelum ada peringkat
- ResearchDokumen7 halamanResearchJoJoBelum ada peringkat
- C Spine Clearance Ortho 3 Journal ClubDokumen31 halamanC Spine Clearance Ortho 3 Journal ClubMuvenn KannanBelum ada peringkat
- 09 Cervical Spine 2Dokumen12 halaman09 Cervical Spine 2楊畯凱Belum ada peringkat
- Clinical Guidelines for Diagnosis and Management of Developmental Dysplasia of the Hip (DDHDokumen121 halamanClinical Guidelines for Diagnosis and Management of Developmental Dysplasia of the Hip (DDHAnonymous 14fGB26QuBelum ada peringkat
- Emergency Care of Cervical Spine Injuries'Dokumen38 halamanEmergency Care of Cervical Spine Injuries'Khirman BatoolBelum ada peringkat
- CHAPTER 2 Injuries of The PelvisDokumen19 halamanCHAPTER 2 Injuries of The PelvisNabeelBelum ada peringkat
- Birth Brachial Plexus Palsy - Journal ClubDokumen57 halamanBirth Brachial Plexus Palsy - Journal Clubavinashrao39Belum ada peringkat
- Adolescent Health Problems and Nursing CareDokumen40 halamanAdolescent Health Problems and Nursing CaremilayosoresBelum ada peringkat
- Broken Neck GuideDokumen7 halamanBroken Neck GuideSulla FelixBelum ada peringkat
- Dislocations: Diagnosis, Management, and Complications: Marvin H. Meyers, M.D.Dokumen12 halamanDislocations: Diagnosis, Management, and Complications: Marvin H. Meyers, M.D.Unoscientris StupaBelum ada peringkat
- Pathological FractureDokumen92 halamanPathological FractureSeptyAuliaBelum ada peringkat
- Chest X-ray Interpretation for Radiographers, Nurses and Allied Health ProfessionalsDari EverandChest X-ray Interpretation for Radiographers, Nurses and Allied Health ProfessionalsBelum ada peringkat
- Ophthalmic Case Studies: 30 Fundus Photos and Clinical VignettesDokumen16 halamanOphthalmic Case Studies: 30 Fundus Photos and Clinical VignettesVarun100% (1)
- David Icke - Bible ErrorsDokumen36 halamanDavid Icke - Bible ErrorsReb420XXXBelum ada peringkat
- Interferential Therapy - DR ElansuriyanDokumen23 halamanInterferential Therapy - DR Elansuriyanelan suriyanBelum ada peringkat
- Management of TMDDokumen22 halamanManagement of TMDWallisson SoaresBelum ada peringkat
- A3.Fundamentals - 25item With Rationale (PNLE)Dokumen4 halamanA3.Fundamentals - 25item With Rationale (PNLE)Blardy Falking You Benchod BlardyBelum ada peringkat
- Standards of Good Practice For Spinal Interventional ProceduresDokumen20 halamanStandards of Good Practice For Spinal Interventional ProceduresMadyline VictoryaBelum ada peringkat
- Nursing Care Plan for Cholelithiasis Patient Undergoing ECGDokumen2 halamanNursing Care Plan for Cholelithiasis Patient Undergoing ECGJenny Ajoc0% (1)
- Running Head: Ruland'S End of Life Theory AnalysisDokumen11 halamanRunning Head: Ruland'S End of Life Theory AnalysismajoodhBelum ada peringkat
- SIOP22 - EPoster ViewingDokumen1.855 halamanSIOP22 - EPoster ViewingmgBelum ada peringkat
- (P. v. Simonov (Auth.) ) The Emotional Brain PhysiDokumen274 halaman(P. v. Simonov (Auth.) ) The Emotional Brain PhysiludmilaromBelum ada peringkat
- Patient-Controlled Analgesia (PCA) Is An Interactive MethodDokumen10 halamanPatient-Controlled Analgesia (PCA) Is An Interactive Methodrahtu suzi ameliaBelum ada peringkat
- JHH Patient HandbookDokumen32 halamanJHH Patient Handbookkxalxo7637100% (1)
- Pain scale guideDokumen4 halamanPain scale guidethilaga88Belum ada peringkat
- Reiki Level I Manual: A Guide to Healing EnergyDokumen37 halamanReiki Level I Manual: A Guide to Healing EnergyAngelicWildFire100% (3)
- NCP Ruth DeveraDokumen8 halamanNCP Ruth DeveraBESA JERIC FLORESBelum ada peringkat
- NABH Guidelines PDFDokumen71 halamanNABH Guidelines PDFAshish kumarBelum ada peringkat
- Chapter 6 Nervous System & Sense OrgansDokumen7 halamanChapter 6 Nervous System & Sense Organscodethree1033Belum ada peringkat
- Ib Ap Lang - Masculinity TextsDokumen10 halamanIb Ap Lang - Masculinity Textsapi-569001207Belum ada peringkat
- Regis Mani AAOMPT Poster 2008Dokumen1 halamanRegis Mani AAOMPT Poster 2008smokey73Belum ada peringkat
- Spiritual Needs of A Patient With Acute IllnessDokumen3 halamanSpiritual Needs of A Patient With Acute IllnessMarimiel PagulayanBelum ada peringkat
- Analysing - Touching The VoidDokumen3 halamanAnalysing - Touching The VoidArhamBelum ada peringkat
- Fibromyalgia and Chronic Myofascial Pain: A Guide For Relatives and CompanionsDokumen2 halamanFibromyalgia and Chronic Myofascial Pain: A Guide For Relatives and CompanionsAngela Buzea0% (1)
- CubukcuDokumen6 halamanCubukcuElan R.S.Belum ada peringkat
- NURSING CARE PLAN - Myocardial Infarction Assessment Diagnosis Inference Planning Intervention Rationale EvaluationDokumen4 halamanNURSING CARE PLAN - Myocardial Infarction Assessment Diagnosis Inference Planning Intervention Rationale Evaluationsweethoney220% (1)
- Idc NCPDokumen14 halamanIdc NCPEnrique BabierraBelum ada peringkat
- Risk for Fluid and Electrolyte ImbalanceDokumen3 halamanRisk for Fluid and Electrolyte Imbalancerod navales100% (1)
- The Emotion Release Method Lester Levenson StoryDokumen20 halamanThe Emotion Release Method Lester Levenson Storycreat1Belum ada peringkat
- 2 Gray Cook Assessing Movement Part Two TranscriptDokumen4 halaman2 Gray Cook Assessing Movement Part Two TranscriptSeba Millón CampañaBelum ada peringkat
- Diane 35 PM pt3 PDFDokumen11 halamanDiane 35 PM pt3 PDFHum BlumBelum ada peringkat
- Noneconomic Damages WorksheetDokumen4 halamanNoneconomic Damages WorksheetYehonatan WeinbergBelum ada peringkat