Caruso Caffo Raudino Tomasello Nanoparticles and Brain Tumor Treatment
Diunggah oleh
Gabriel Fernández CalvoHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Caruso Caffo Raudino Tomasello Nanoparticles and Brain Tumor Treatment
Diunggah oleh
Gabriel Fernández CalvoHak Cipta:
Format Tersedia
Nzwovznarcrrs
zwn Bnzrw Tton
Tnrzarwa
Gerardo Caruso, M.D.,
Maria Cao Pb.D, M.D.,
Giuseppe Raudino, M.D., and
Francesco Tomasello, M.D.
2012, ASME, 3 Park Avenue, New York, NY 10016, USA (www.asme.org)
All rights reserved. Printed in the United States of America. Except as permitted under
the United States Copyright Act of 1976, no part of this publication may be reproduced
or distributed in any form or by any means, or stored in a database or retrieval system,
without the prior written permission of the publisher.
Co-published by Momentum Press, LLC, 222 E. 46th Street, #203, New York,
NY 10017, USA (www.momentumpress.net)
INFORMATION CONTAINED IN THIS WORK HAS BEEN OBTAINED
BY THE AMERICAN SOCIETY OF MECHANICAL ENGINEERS FROM
SOURCES BELIEVED TO BE RELIABLE. HOWEVER, NEITHER ASME
NOR ITS AUTHORS OR EDITORS GUARANTEE THE ACCURACY
OR COMPLETENESS OF ANY INFORMATION PUBLISHED IN THIS
WORK. NEITHER ASME NOR ITS AUTHORS AND EDITORS SHALL
BE RESPONSIBLE FOR ANY ERRORS, OMISSIONS, OR DAMAGES
ARISING OUT OF THE USE OF THIS INFORMATION. THE WORK IS
PUBLISHED WITH THE UNDERSTANDING THAT ASME AND ITS
AUTHORS AND EDITORS ARE SUPPLYING INFORMATION BUT ARE
NOT ATTEMPTING TO RENDER ENGINEERING OR OTHER PROFES-
SIONAL SERVICES. IF SUCH ENGINEERING OR PROFESSIONAL
SERVICES ARE REQUIRED, THE ASSISTANCE OF AN APPROPRIATE
PROFESSIONAL SHOULD BE SOUGHT.
ASME shall not be responsible for statements or opinions advanced in papers or . . .
printed in its publications (B7.1.3). Statement from the Bylaws.
For authorization to photocopy material for internal or personal use under those
circumstances not falling within the fair use provisions of the Copyright Act, contact
the Copyright Clearance Center (CCC), 222 Rosewood Drive, Danvers, MA 01923,
tel: 978-750-8400, www.copyright.com.
Requests for special permission or bulk reproduction should be addressed to the ASME
Publishing Department, or submitted online at: http://www.asme.org/kb/books/
book-proposal-guidelines/permissions.
ASME Press books are available at special quantity discounts to use as premiums or
for use in corporate training programs. For more information, contact Special Sales at
infocentral@asme.org.
A catalog record is available from the Library of Congress.
(Print) ISBN: 978-0-7918-6003-8
ASME Order No.: 860038
(Electronic) ISBN: 978-1-6065 -408-6 0
Series Editors Preface
Biomedical and Nanomedical Technologies (B&NT)
Tis concise monograph series focuses on the implementation of various
engineering principles in the conception, design, development, analysis and
operation of biomedical, biotechnological and nanotechnology systems and
applications. Te primary objective of the series is to compile the latest re-
search topics in biomedical and nanomedical technologies, specically de-
vices and materials.
Each volume comprises a collection of invited manuscripts, written in
an accessible manner and of a concise and manageable length. Tese timely
collections will provide an invaluable resource for initial enquiries about
technologies, encapsulating the latest developments and applications with
reference sources for further detailed information. Te content and format
have been specically designed to stimulate further advances and applica-
tions of these technologies by reaching out to the non-specialist across a
broad audience.
Contributions to Biomedical and Nanomedical Technologies will inspire
interest in further research and development using these technologies and
encourage other potential applications. Tis will foster the advancement of
biomedical and nanomedical applications, ultimately improving healthcare
delivery.
Editor:
Abmed Al-Jumaily, PbD, Professor of Biomechanical Engineering &
Director of the Institute of Biomedical Technologies, Auckland University
of Technology.
Associate Editors:
Waqar Abmed, PbD, Chair, Nanotechnology and Advanced Manufac-
turing, and Head, Institute of Nanotechnology and Bioengineering, School
of Computing, Engineering & Physical Sciences, University of Central
Lancashire, UK.
Cbristopber H.M. Jenkins, PbD, PE, Professor and Head, Mechanical &
Industrial Engineering Department, Montana State University.
Cowarwas
1. Introduction 1
2. Glioma biology 4
2.1 Invasion and angiogenesis 4
3. Blood-brain barrier 9
3.1 Blood-brain barrier physiology 9
3.2 Blood-brain barrier transport systems 11
4. Nanomedicine and nanotecbnology 14
4.1 Nanoparticle drug delivery 19
4.1.1 Nanoparticle distribution 20
4.1.2 Nanoparticle functionalization 21
4.1.3 Nanoparticle targeting 23
4.2 Nanomedicine and cancer 25
4.3 Nanomedicine and toxicity 30
5. Nanoparticle tecbnologies 33
5.1 Polymeric and polymer-drug conjugate nanoparticles 33
5.2 Micelle nanoparticles 35
5.3 Liposomes 37
5.4 Gold and silver nanoparticles 39
5.5 Metal oxide 41
5.6 Magnetic nanoparticles 42
5.7 Carbon nanotubes 43
5.8 Fullerenes 44
5.9 Peptides nanoparticles 45
5.10 Silica nanoparticles 46
5.11 Quantum dots 48
5.12 Dendrimers 49
6. Nanomedicine applications in brain tumors 51
6.1 Brain tumor drug targeting 55
6.1.1 Systemic approaches 55
6.1.2 Physiological approaches 56
6.1.2.1 Receptor-mediated transcytosis 57
6.1.2.2 Adsorptive-mediated transcytosis 58
6.1.2.3 Eux pump inhibition 60
6.1.2.4 Cell-mediated drug transport 61
6.1.3 Direct CNS approaches 61
6.1.3.1 Intracerebral routes 65
6.1.4 Drug modications and prodrugs 66
7. Experimental studies 69
8. Conclusions 77
References 81
Abstract
Despite progresses in surgery, radiotherapy, and in chemotherapy, an eec-
tive curative treatment of gliomas does not yet exist. Mortality is still close
to 100% and the average survival of patients with GBM is less than 1 year.
Te ecacy of current anti-cancer strategies in brain tumors is limited by
the lack of specic therapies against malignant cells. Besides, the delivery
of the drugs to brain tumors is limited by the presence of the blood brain
barrier. Te oncogenesis of gliomas is characterized by several biological
processes and genetic alterations, involved in the neoplastic transformation.
Te modulation of gene expression to more levels, such as DNA, mRNA,
proteins and transduction signal pathways, may be the most eective mo-
dality to down-regulate or silence some specic gene functions. Gliomas are
characterized by extensive microvascular proliferation and a higher degree
of vasculature. In malignant gliomas targeted therapies ecacy is low. In
this complex eld, it seems to be very important to improve specic selective
drugs delivery systems. Drugs, antisense oligonucleotides, small interference
RNAs, engineered monoclonal antibodies and other therapeutic molecules
may diuse into CNS overcoming the BBB. Nanotechnology could be used
both to improve the treatment ecacy and to reduce the adverse side eects.
Nanotechnology-based approaches to targeted delivery of drugs across the
BBB may potentially be engineered to carry out specic functions as needed.
Moreover, nanoparticles show tumor-specic targeting and long blood cir-
culation time, with consequent low-short-term toxicity. Nanotechnology
deals with structures and devices that are emerging as a new eld of re-
search at the interface of science, engineering and medicine. Nanomedicine,
the application of nanotechnology to healthcare, holds great promise for
revolutionizing medical treatments, imaging, faster diagnosis, drug delivery
and tissue regeneration. Tis technology has enabled the development of
nanoscale device that can be conjugated with several functional molecules
including tumor-specic ligands, antibodies, anticancer drugs, and imag-
ing probes. Nanoparticle systems are, also emerging as potential vectors for
brain delivery, able to overcome the diculties of the classical strategies. By
using nanotechnology it is possible to deliver the drug to the targeted tis-
sue across the BBB, release the drug at the controlled rate, and avoid from
degradation processes. At the same time, it is also necessary to retain the
drug stability and ensure that early degradation of drugs from the nano-
carriers does not take place. Large amounts of small molecules, such as
contrast agents or drugs, can be loaded into NPs via a variety of chemical
methods including encapsulation, adsorption, and covalent linkage. Most
targeting molecules can be added to the surface of NPs to improve targeting
through a concept dened as surface-mediated multivalent anity eects.
viii Nzwovznarcrrs zwn Bnzrw Tton Tnrzarwa
Te future challenges may be the possibility to modify the cell genome and
induce it to a reversion to the wild-type conditions and the enhancing of im-
mune system anti-tumor capacity. Recent advances in molecular, biological
and genetic diagnostic techniques have begun to explore cerebral glioma-
associated biomarkers and their implications for gliomas development and
progression. Realization of targeted therapies depends on expression of the
targeted molecules, which can also provide as specic biomarkers. Te de-
velopment of multifunctional NPs may contribute to the achievement of
targeted therapy in glioma treatment.
1. Introduction
Gliomas are the most common primary brain tumors in adults, with a
worldwide incidence of approximately 7 out of 100,000 individuals per year.
Although brain tumors constitute only a small proportion of overall human
malignancies, they carry high rates of morbidity and mortality. Mortality
is still close to 100% and the average survival of patients with glioblastoma
multiforme (GBM) is less than 1 year when classical treatment is used.
Recent progress in multimodal treatment of this disease has led to only a
slight increase in average survival up to 1518 months. Te eectiveness of
the actual chemotherapeutic approach and multimodal targeted therapies
remains modest in gliomas.
Gliomas are brain tumors with histological, immunohistochemical and
ultra structural features of glial dierentiation. Approximately 50% of pri-
mary brain tumors are gliomas, arising from astrocytes, oligodendrocytes,
or their precursors and ependymal cells. Gliomas are classied from I to
IV according to the World Health Association (WHO) malignancy scale.
Grade I gliomas are benign with a slow proliferation rate and include py-
locitic astrocytoma most common in pediatric age. Grade II gliomas are
characterized by a high degree of cellular dierentiation and grow diusely
into the normal brain parenchyma and are prone to malignant progression.
Tey include astrocytoma, oligodendroglioma and oligoastrocytoma. Grade
III lesions include anaplastic astrocytoma, anaplastic oligoastrocytoma and
anaplastic oligodendroglioma. Tese tumors show a higher cellular density
and a notable presence of atypia and mitotic cells. Grade IV tumors are the
most malignant and also the most frequent gliomas and include glioblas-
toma and gliosarcoma. Tese tumors presented microvascular proliferations
and pseudopalisading necrosis.
Conventional brain tumor treatments include surgery, radiation therapy
and chemotherapy. Surgical treatment is invasive but represents the rst
approach for the vast majority of brain tumors due to diculties arising
in early stage detection. However, after surgical resection, the residual pool
of invasive cells rises to recurrent tumor which, in 96% of cases arise ad-
jacent to the resection margins [1]. Aggressive treatment modalities have
extended the median survival from 4 months to 1 year, but the survival is
often associated with signicant impairment in the quality of life. Radiation
therapy and chemotherapy are non-invasive options often used as adjuvant
therapy, but may also be eective for curing early-stage tumors. In patients
with recurrent GBM, the 6-months progression-free survival is only 21%
after treatment with temozolomide [2]. Adjuvant radiotherapy gives limited
benets and causes debilitation side eects which reduce its ecacy [3]. Te
eectiveness of systemic chemotherapy is limited by toxic eects on healthy
cells, generally resulting in morbidity or mortality of the patient. Moreover,
the presence of the BBB limits the passage of a wide variety of anticancer
2 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
agents. Te high incidence of recurrence and poor prognosis of malignant
gliomas compel the development of more powerful anti-cancer treatments.
Te compromise of the quality of remaining life as well as the limited suc-
cess of current treatment options in shrinking tumors, raise increasing
concerns about the adverse eects of cancer treatment on brain function.
Deterioration in neurological function is accompanied by signicant deteri-
oration in the global quality of life in patients aected by malignant gliomas.
Te advent of molecular studies allows evaluation of the possibility of re-
examination of the biology of gliomas with, a level of precision that prom-
ises interesting advances toward the development of specic and eective
therapies. It is now generally understood that tumor genesis occurs either,
by over-expression of oncogenes, or inactivation of tumor suppressor genes.
Te modulation of gene expression at more levels, such as DNA, mRNA,
proteins and transduction signal pathways, may be the most eective mo-
dality to down-regulate or silence some specic gene functions.
Cerebral gliomas represent an important challenge in modern oncology,
and only in the last years has the development of new multimodal thera-
peutic strategies given the beginning to a new research eld of neuroon-
cology: nanotechnology and nanomedicine. With the advancement in BBB
structure and pathophysiology knowledge, brain delivery and targeting
skills, and brain tumor biology, these new interesting possibilities could
lead to new perspectives in brain tumor treatment. Nanotechnology is an
emerging eld that deals with interactions between molecules, cells and
engineered substances such as molecular fragments, atoms and molecules.
Te impact of nanotechnology in medicine can mainly be seen in diagnostic
methods, drug-release techniques and regenerative medicine. In the recent
past, nanotechnology has garnered much attention due to its potential ap-
plication in cancer, and the National Cancer Institute has constituted an
Alliance of Nanotechnology in Cancer with focus on the development of
novel nanoplatform-based diagnostics, therapeutics and preventive agents.
Nanomedicine could lead to new possibilities to overcome important prob-
lems in malignant brain tumors, such as the non specicity of cancer cells
drug-delivering and targeting, as well as the non complete passage of drugs
through the BBB and into cancer cells avoiding side eects in normal brain
tissue. Nanoparticles are colloidal particles typically synthesized in either
aqueous or organic phases. Due to their small size, nanoparticles can easily
ow through blood capillaries and enter the target cancer cells. Reduction
of toxicity to peripheral organs can also be achieved with these systems
[4]. Nanoparticle-based drug-delivery systems, an antisense approach to
modify gene expression in cancer cell genome, and molecular-based cancer
cell targeting all represent important possibilities in cerebral gliomas treat-
ment. Nanosystems with dierent compositions and biological properties
have been extensively investigated for drug and gene delivery applications
[45]. Te type and the number of linkers within and on the surface of
Iwrnonucrrow 3
nanoparticles and the size of the nanoparticle itself can be modulated to
control the loading/releasing of the encapsulated or covalently linked drug
components or to add surface coating. Moreover, they can improve the e-
cacy of existing imaging and treatment regimens. Te ability to deliver con-
trast or therapeutic agents selectively to tumors at eective concentrations
is a key factor for the ecacy of cancer detection and therapy. Additionally,
encapsulation of drugs within nanoplatforms can provide a signicant ad-
vantage when employing poorly soluble, poorly absorbed or labile agents by
incorporating them in the matrix of the nanoparticle during the formula-
tion/synthetic process.
Tis study presents a review of the recent studies of nanoparticle systems
in cerebral gliomas treatment with a particular emphasis on the develop-
ment of nanocarrier drug delivery systems for brain cancer therapy appli-
cations. Tese technologies include polymeric and polymer-drug conjugate
nanoparticles, micelle nanoparticles, liposomes, metallic and magnetic
nanoparticles, metal oxide, carbon derivates, peptide nanoparticles, inor-
ganic nanopaerticles, quantum dots, and dendrimers.
2. Glioma biology
Genomic DNA aberrations are key genetic events in gliomagenesis.
Recurrent genomic regions of alteration, including net gains and losses,
have been found in gliomas. Whereas some of these regions contain
known oncogenes and tumor suppressor genes, the biologically relevant
genes within other regions remain to be identied. Te phenotypic and
genotypic heterogeneity indicate that no isolated genetic event accounts
for gliomagenesis, but rather the cumulative eects of a number of alter-
ations that operate in a concerted manner. In this pathological process
are included various biological events, such as activation of growth factor
receptor signaling pathways, down-regulation of many apoptotic mecha-
nisms, and imbalance of pro- and anti-angiogenic factors. Several growth
factor receptors, such epidermal growth factor receptor (EGFR), platelet-
derived growth factor receptor (PDRGF), C-Kit, vascular endothelial
growth factor receptor (VEGFR) are over-expressed, amplied and/or
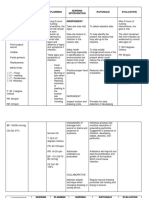
mutated in gliomas (Figure 2-1). In Table 2-1 are summarized the most
common glioma genetic alterations frequently found. In the light of this
novel information, the modulation of gene expression at more levels, such
as DNA, mRNA, proteins and transduction signal pathways, may repre-
sent the most eective modality to down-regulate or silence some specic
genic functions or introduce genes, down-regulated or deleted selectively,
into neoplastic cells.
2.1 Invasion and angiogenesis
Glioma cell invasion consists of an active translocation of glioma cells
through host cellular and extracellular matrix barriers [67]. Cerebral
gliomas show a unique pattern of invasion and with rare exceptions do not
metastasize outside of the brain. How invasive glioma cells survive in the
setting of invasion, evading immune detection, and deferring commitment
to proliferation, remains unknown. Invading glioma cells normally migrate
to distinct anatomical structures. Tese structures include the basement
membrane (BM) of blood vessels, the subependymal space, the glial limi-
tans externa, and parallel and intersecting nerve bre tracts in the white
matter. Glioma cells adhesion to proteins of the surrounding extracellular
matrix (ECM), degradation of ECM components by proteases secretion
by neoplastic cells and migration of glioma cells are fundamental phases in
this process. ECM is composed of proteoglycans, glycoproteins, and colla-
gens and also contains bronectin, laminin, tenascin, hyaluronic acid, and
vitronectin. Critical factors in glioma invasion include the synthesis and
deposition of ECM components by glioma and mesenchymal cells, the re-
lease of ECM-degrading activities for remodeling interstitial spaces, the
presence of adhesion molecules and the eects of cell-matrix inter actions
on the behavior of glioma cells. ECM modication aids the loss of contact
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch02_Bionanoparticles.indd 4 Manila Typesetting Company 08/22/2012 11:43PM
Grroz Broroov 5
inhibition, allowing tumor cells to freely migrate and invade the surround-
ing tissues. Te proteolytic degradation of the BM is mediated by pro-
teases, such as the matrix metalloproteases (MMPs), secreted by tumor
and stromal cells [8]. MMPs play an important role in human brain tumor
invasion, probably due to an imbalance between the production of MMPs
and tissue inhibitor of metalloproteases-1 (TIMP-1) by the tumor cells
[8]. MMP-1 is able to initiate breakdown of the interstitial collagens and to
Figure 2-1 Growth factors signaling pathways in cerebral
gliomas (K-kinase, EGF-epidermal growth factor, PDGF-
plateled derived growth factor, mTOR-mammalian target of
rapamycin, PTEN-tumor suppressor phosphatise and tensin
homolog, PKC-protein kinase C, PI3K phosphatidylinositol-3-
kinase, PLC-phospholipase, Akt-, MEK-1/2-mitogen-activated
protein kinase and extracellular signal-regulated protein kinase-
1/2, kinase, MAPK/ERK-1/2-mitogen-activated protein kinase/
extracellular signal-regulated protein kinase-1/2).
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch02_Bionanoparticles.indd 5 Manila Typesetting Company 08/22/2012 11:43PM
6
N
z
w
o
v
z
n
r
r
c
r
r
s
z
w
n
B
n
z
r
w
T
u
o
n
T
n
r
z
r
r
w
r
Table 2-1 Main genetic alterations in cerebral gliomas.
Gene Chromosome
Molecular
alteration
Molecular alteration
eects
Histotype and
(WHO Grade)
TP53 Cr17p13.1 Mutation Cell cycle control loss,
proliferation
Astrocytoma and oligodendroglioma
(WHO Grade II). Precocious mutation in
secondary GBM
PDGFR-a
PDGF-A
Cr4q11-q12 Amplication/
over-expression
Proliferation/invasion Astrocytoma and oligodendroglioma
(WHO Grade IIIII)
Unknown tumor
suppressor genes
1p, 19q, 4q, 9p
and 11p loss
Loss of
heterozygosity
Proliferation, invasiveness,
angiogenesis
Astrocytoma and oligodendroglioma
(WHO Grade IIIII)
Unknown tumor
suppressor genes
Cr22q Deletion Proliferation Astrocytoma and oligodendroglioma
(WHO Grade II)
Rb 1 Cr13q14.2 Mutations/
deletion
Cell cycle control loss,
proliferation
Astrocytoma and oligodendroglioma
(WHO Grade IIIII)
P16 Cr9p CDKN2/p16
deletion
Cell cycle control loss,
proliferation
Astrocytoma and oligodendroglioma
(WHO Grade IIIII)
PTEN Cr10q23 LOH Regulation Akt/PKB signal-
ing pathway loss; prolif-
eration and tumor growth;
invasiveness, angiogenesis
Astrocytoma and oligodendroglioma
(WHO Grade IIIIV)
BAX Cr19q24 LOH Pro-apoptotic action loss,
proliferation
Astrocytoma and oligodendroglioma
(WHO Grade IIIII)
EGFR (c-erb-2) Cr7p11-p12 Amplication/
over-expression
Cell transformation and
proliferation
De novo GBM
MDM2 Cr12q14.3-q15 Over-expression Cell cycle control loss and
proliferation
De novo GBM
1
2
3
4
5
6
7
8
9
1
0
1
1
1
2
1
3
1
4
1
5
1
6
1
7
1
8
1
9
2
0
2
1
2
2
2
3
2
4
2
5
2
6
2
7
2
8
2
9
3
0
3
1
3
2
3
3
3
4
3
5
3
6
3
7
3
8
3
9
4
0
4
1
4
2
4
3
4
4
A
S
M
E
_
C
h
0
2
_
B
i
o
n
a
n
o
p
a
r
t
i
c
l
e
s
.
i
n
d
d
6
M
a
n
i
l
a
T
y
p
e
s
e
t
t
i
n
g
C
o
m
p
a
n
y
0
8
/
2
2
/
2
0
1
2
1
1
:
4
3
P
M
Grroz Broroov 7
activate the other MMPs which allow glioma cell inltration. Cell adhesion
is the binding of the cells to each other and to the ECM through cell adhe-
sion molecules such as integrins, selectins, cadherins, the immunoglobulin
superfamily and lymphocyte homing receptors. Te extracellular ligands
that anchor these adhesions include laminin, bronectin, vitronectin, and
various collagens. Integrins are heterodimers of a- and b-subunits that reg-
ulate many aspects of the cell behavior including survival, proliferation, mi-
gration and dierentiation. Integrins are expressed on dierent cell types,
including neurons, glial cells, meningeal and endothelial cells. b2 integrins
are specically expressed by leukocytes and they are found on microglia
and on inltrating leukocytes within the CNS. Down-regulated b1 inte-
grin protein levels in vivo probably aect interactions of glioma cells with
ECM components, leading to reduced migration along vascular basement
membranes [9]. Tese data can be interpreted as contributing to the locally
invasive behavior of astrocytic tumors, favoring the regulation of proteases
activation.
Cerebral gliomas are characterized by extensive microvascular prolifera-
tion and a higher degree of vasculature. Angiogenesis, the formation of new
blood vessels from existing microvessels, is a histological indicator of the
degree of malignancy and prognosis. Angiogenesis also includes vessel pen-
etration into avascular regions of the tissue, and is critically dependent on
the correct interactions among endothelial cells, pericytes and surrounding
cells and their association with the ECM and the vascular BM. Cao et al.
[10] demonstrated that, the presence of endothelial glomeruloid-like pro-
liferation in neoplastic vessels, was predictive of active tumor invasiveness
(Figure 2-2). Endothelial cells are guided into avascular areas via macro-
molecules such as VEGF-A, a pro-angiogenic factor and endothelial cell
mitogen. VEGF-A activation causes endothelial cell dierentiation and a
VEGF-A gradient induces stalk cell proliferation along an opening in the
BM in the formation of a new vessel sprout. VEGF also induces expression
Figure 2-2 Presence of marked endothelial glomeruloid-like
proliferations in neoplastic vessels. Tis feature is indicative of
active tumor progression and invasiveness, and of neoplastic
cellular migration.
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch02_Bionanoparticles.indd 7 Manila Typesetting Company 08/22/2012 11:43PM
8 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
of the delta-like ligand, DLL-4, in tip cells that bind to its receptors, as well
as Notch 1 and Notch 4, on adjacent stalk endothelial cells. DLL-4-Notch
signaling functions act as a dampening mechanism in preventing excess an-
giogenesis and promoting orderly development of new vessels. Membrane
type 1-matrix metalloproteinase MT1-MMP on the endothelial cell sur-
face, are also required for the subsequent step in the angiogenesis cascade
of tube formation, by playing a role in endothelial intracellular vacuole and
lumen formation. Te BM is built up of scaolding laminins and essential
components such as collagen IV and collagen XVIII [11]. Part of the nal
stage of angiogenesis is the recruitment of pericytes as their association with
endothelial and vascular smooth muscle cells, is essential for the maturation
of endothelial tubes into blood vessels.
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch02_Bionanoparticles.indd 8 Manila Typesetting Company 08/22/2012 11:43PM
3. Blood-brain barrier
Te brain is a unique organ highly protected by two major barriers, the BBB
which displays the largest surface area and the bloodcerebrospinal uid
barrier (BCSFB). BBB is responsible for several functions, such as main-
tenance of neuronal microenvironment, tissue homeostasis, vasotonous
regulation, brinolysis and coagulation, blood cell activation and migration
during physiological and pathological processes. Tere are several gateways
which oer entry to brain parenchyma, the most important are blood circu-
lation and cerebrospinal uid (CSF) circulation. In the human brain, there
are about 100 billion capillaries in total, providing a combined length of
brain capillary endothelium of approximately 650 km and a total surface
area of approximately 20 m
2
[12]. Despite the rapid development in under-
standing of the molecular structure of components of the BBB, knowledge of
receptor expression at the BBB, advances in medical technology, and break-
throughs in nanotechnology-based approaches, many of the CNS associ-
ated diseases remain under-treated by eective therapies. Since the majority
of drugs and large molecular weight particulate agents such as recombinant
proteins, peptides, monoclonal antibodies, small-interfering RNA (siRNA)
and gene therapeutics do not readily permeate into the brain parenchyma,
one of the most signicant challenges facing CNS drug development, is the
availability of eective brain drug targeting technology.
3.1 Blood-brain barrier pbysiology
Physiologically BBB is made up of three layers such as the inner endothelial
cell layer which forms the wall of the capillary and contains tight junctions,
followed by the presence of a basement membrane upon which pericytes
and astrocytic feet processes lie [13]. Te BBB endothelial cells dier from
endothelial cells in the rest of the body by the absence of fenestrations, more
extensive tight junctions (TJs), and sparse pinocytic vesicular transport.
Endothelial cells TJs limit the paracellular ux of hydrophilic molecules
across the BBB. In addition to brain capillary endothelial cells, extracellular
base membrane, pericytes, astrocytes, and microglia are all integral parts of
the BBB supporting system. Te capillary endothelial cell line the microves-
sels, which are coupled by much more TJ (zonulae occludentes) than found
in peripheral vessels. Te endothelial cells secrete and are surrounded by
a basal lamina (BL), with the end-feet of astrocytic glial cells close on its
opposite side. Astrocytes are the most abundant non-neuron cells and play
many essential roles in the healthy CNS, including biochemical support of
endothelial cells which form the BBB, regulation of blood ow, provision
of nutrients to the nervous tissue, maintenance of extracellular ion bal-
ance, and in the repair and scarring process of the brain and spinal cord
following traumatic injuries. Pericytes are embedded in the BL between en-
dothelial cells and astrocyte cells, making particularly close contact with the
10 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
endothelial cells. Pericytes provide microvasculature structural support and
vasodynamic capacity.
BCSFB function, together with the BBB and the meninges, is the con-
trol of the brain internal environment. It is sited at the choroid plexus epi-
thelium, secreting CSF, which circulates through the ventricles and around
the outside of the brain and spinal cord [14]. Te choroidal epithelium is
a complex organ with many additional functions including neuroendocrine
signaling, neuroimmune and neuroinammatory responses, drug and toxin
metabolism, and transport. On the external surface of the brain the ependy-
mal cells fold over upon themselves to form a double layered structure. Tis
virtual space is known as subarachnoid space and acts in CSF drainage.
Te passage of substances from the blood through the arachnoid membrane
is prevented by tight junctions. Te capillary endothelium in the choroid
plexus is fenestrated, allowing the passage of small molecules. Te arach-
noid membrane is generally impermeable to hydrophilic substances and its
role in the formation of the blood-CSF barrier is largely passive.
TJs are located on the apical region of endothelial cells and are structur-
ally formed by a complex network made of a series of parallel, intercon-
nected, transmembrane and cytoplasmatic strands of proteins [15]. TJs
consist of three integral membrane proteins, namely, claudin, occludin, and
junction adhesion molecules, and a number of cytoplasmic accessory pro-
teins including ZO-1, ZO-2, ZO-3, cingulin. Te high level of integrity of
TJs is reected by the high electrical resistance of the BBB (15002000
cm
2
), which depends on a proper extracellular Ca2+ ion concentration. Te
tightness of the BBB is due to the physical complexity of its junctional struc-
ture and the molecular substructure, in particular, the presence of trans-
membrane proteins claudins 1 and 5 which help to seal the intercellular cleft.
Cytoplasmic proteins link membrane proteins to actin, which is the primary
cytoskeleton protein for the maintenance of structural and functional integ-
rity of the endothelium. In a recent study, treatment of claudin-5 by cyclic
AMP (cAMP) led to enhancement of claudin-5 activity along cell borders,
rapid reduction in transendothelial electrical resistance (TER), and loosen-
ing of the claudin-5-based endothelial barrier against mannitol [16]. Tese
suggest that manipulation of claudin-5, or potentially other TJ proteins may
permit drug transport by altering the function at the BBB but without its
total disruption. Occludin is a phosphoprotein with four transmembrane
domains. Occludin appears to be a regulatory protein that can alter para-
cellular permeability. Occludins and claudins assemble into heteropolymers
and form intramembranous strands.
Adherens junctions (AJs) are located below the TJs in the basal region of
the lateral plasma membrane. Tey are composed of trans-membrane gly-
coproteins (cadherins) linked to the cytoskeleton by cytoplasmatic proteins,
thus providing an additional tightening structure between the adjacent en-
dothelial cells at the BBB. Te cytoplasmic domains of cadherins bind to the
Broon-Bnzrw Bznnrrn 11
submembranal plaque proteins h- or g-catenin, which are linked to the actin
cytoskeleton via a-catenin. In addition to supporting the barrier function,
AJs mediate the adhesion of brain endothelial cells to each other, the initia-
tion of cell polarity and the regulation of paracellular permeability [17].
3.2 Blood-brain barrier transport systems
Tere are dierent mechanisms by which solutes move across membranes
as they enter and leave the brain. Te transport may occur due to diu-
sion, either simple diusion or facilitated transport across aqueous chan-
nels (Figure 3-1). Passive diusion is a concentration gradient dependent
process that allows molecules to move across cellular membranes between
cells (paracellular way) or across cells (transcellular way) down their electro-
chemical gradient without the requirement of metabolic energy. Small
water-soluble molecules simply diuse through the TJs but not to any great
extent. Small lipid soluble substances like alcohol and steroid hormones
penetrate transcellularly by dissolving in their lipid plasma membrane. In
addition to concentration dierences, other factors can aect the diusion
of a drug across the BBB such as lipophilicity and molecular weight. Only
lipid soluble small molecules with a molecular weight of 400 Daltons can
cross the BBB. However, the majority of small molecule drugs have a higher
molecular weight or current water solubility which prevents their simple
diusion across the barrier. In addition, even though some small molecules
such as HIV protease inhibitors exhibit a high degree of lipophilicity, their
CSF and brain concentrations are often undetectable [18]. Tis eect is
Figure 3-1 Molecular transport across the blood-brain barrier.
12 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
believed to be attributed to the functional expression of several ABC mem-
brane associated drug transporters, which can actively export these agents
out of the brain [18]. For almost all other substances, including essential
materials such as glucose and amino acids, transport proteins (carriers), spe-
cic receptor-mediated or vesicular mechanisms (adsorptive transcytosis)
are required to pass the BBB.
Dierent substances are transported through free diusion mecha-
nism either paracellularly or transcellularly. Paracellular diusion is a non-
saturable and noncompetitive movement of compounds between cells. It
occurs to a limited extent at the BBB, due to the TJs. Transcellular diusion
(transcytosis) is a non-saturable and noncompetitive movement across cells
of lipophilic substances. Facilitated diusion is a form of carrier-mediated
endocytosis in which solute molecules bind to specic membrane protein
carriers that trigger a conformational change in the protein. Tis results in a
carrying through of the substance to the other side of the membrane, from
high to low concentration (passive diusion). Tis mechanism contributes
to the transport of various substances including amino acids, nucleoside,
small peptide, monocarboxylates, and glutathione.
Carrier mediated transport (CMT) or carrier mediated inux processes
involve putative proteins that facilitate the movement of poorly permeable
solutes across cellular membranes. Te CMT system is expressed on both
the luminal and abluminal membranes of the brain capillary endothelium
and operates in both directions. CMT systems can be exploited for brain
drug-delivery after reformulating the drug in such a way that the drug as-
sumes a molecular structure mimicking that of the endogenous ligand. If
compounds need to be moved against a concentration gradient, ATP may
provide the energy to facilitate the process. Gabapentin (a g-amino acid) suc-
cessfully crosses the BBB because the structure does mimic that of a a-amino
acid and is recognized by large neutral amino acid transporter [19]. Several
other drugs which have been successfully transported into the brain include
melphalan for brain cancer, laevodopa (L-Dopa) for Parkinsons disease and
a-methyl-DOPA for treatment of high blood pressure. Te uptake of nu-
trients from blood into the brain is facilitated by the solute carrier (SLC)
transporter families. Tese inux carriers are involved in the transport of a
broad range of substrates including glucose, amino acids, nucleosides, fatty
acids, minerals and vitamins in various human tissues, including the brain.
SLCO/SLC21, the organic anion transporting superfamily (OATPs), and
SLC22, the organic cation/anion/zwitterions transporter family, are heavily
involved in the uptake of many diverse substrates [20].
Te active eux transport is responsible for extruding drugs from the
brain and this mechanism is a major obstacle for the accumulation of a wide
range of biologically active molecules in the brain. Te ATP binding cas-
sette (ABC) transporter P-glycoprotein and multidrug resistant protein
(MRP) represent the principle eux mechanism of these agents [21]. Te
Broon-Bnzrw Bznnrrn 13
most abundantly present component of this system is eux P-glycoprotein,
which is a product of the ABCB1gene. Inhibition of P-glycoprotein in pre-
clinical studies has enhanced the penetration of paclitaxel into the brain,
indicating the feasibility of achieving improved drug delivery to the brain by
suppression of P-glycoprotein [22].
Endocytosis and transcytosis allow the internalization, sorting and traf-
cking of many plasma macromolecules. Endocytosis is a process where
molecules from the circulation are internalized in vesicles and are directed
to endosomes or lysosomes within the cell. Endocytosis can be isolated into
bulk-phase (uid phase or pinocytosis) endocytosis and mediated endo-
cytosis (receptor and absorptive mediated). Bulk-phase endocytosis is the
noncompetitive, non-saturable, temperature and energy dependent non-
specic uptake of extracellular uids. Transcytosis refers to the transcellular
movement of molecules.
Receptor mediated endocytosis or clathrin-dependent endocytosis pro-
vides for a highly specic and energy mediated transport enabling eukary-
otic cells to selective uptake macromolecules as specic cargo. Cells have
dierent receptors for the uptake of many dierent types of ligands, includ-
ing hormones, growth factors, enzymes, and plasma proteins. Tis process
occurs at the brain for macromolecular substances, such as transferrin, in-
sulin, leptin, and IGF-I & IGF-II, and is a highly specic type of energy
dependent transport [23].
Adsorptive endocytosis/transcytosis facilitates the transport of large
peptides such as IgG, histone, albumin, native ferritin, horse radish per-
oxidase and dextran. Adsorptive-mediated endocytosis is characterized by
an electrostatic interaction between a positively charged substance and the
negatively charged sites on the brain endothelial cell surface (e.g. glycopro-
tein) [24]. Adsorptive processes largely depend upon electrostatic interac-
tions that allow the positively charged moiety of the substrate to bind to the
negatively charged cell membrane. Receptor mediated transport is mainly
employed in the transport of macromolecules like peptides and proteins
across the BBB, by conjugating the substance with ligands such as lacto-
ferrin, transferrin and insulin. It is an important transport mechanism of
predominant interest in drug delivery.
Cell-mediated transcytosis is a recently identied route of drug transport
across the BBB [25]. Tis transport route relies on immune cells such as
monocytes or macrophages to cross the intact BBB. Unlike the aforemen-
tioned transport pathways which normally permit only solute molecules
with specic properties, cell-mediated transcytosis is unique in that it can
be used for virtually any type of molecule or material as well as particulate
carrier systems.
4. Nanomedicine and nanotecbnology
Nanotechnology is a collective denition referring to every technology and
science which operates on a nanoscale and refers to the scientic principles
and new properties that can be found and mastered when operating in
this range. When we bring materials down to the nanoscale, the properties
change and nanoparticles have other optical, magnetic or electrical prop-
erties than larger particles. Tese properties are and will be utilized in a
wide spectre of areas as in medical applications, information technologies,
energy production and storage, materials, manufacturing, instrumentation,
environmental applications and security. Nanotechnology in biomedical re-
search has emerged as an interdisciplinary science that has quickly found
its own niche in clinical methodologies including imaging, diagnostic and
therapeutic. Te nano-based technology is expected to expand multi-
directionally to provide unmet needs in medicine and has potential to gen-
erate innovations that will bring breakthrough treatments to various human
diseases, including cancer. Nanotechnology is characterized by the manipu-
lation of atoms and molecules leading to the construction of structures in
the nanometer scale size range [2627]. Te National Institute of Health
denes nanomedicine as the application of nanotechnology to diseases treat-
ment, diagnosis, monitoring, and to the control of biological systems. Te
eld of nanomedicine aims to use the properties and physical characteristics
of nanomaterials, which have been extensively investigated as novel intra-
vascular or cellular probes, for both diagnostic and therapeutic purposes.
Te sub-micron size of nanoparticle systems confers considerable advan-
tages as compared to large sized systems including targeted delivery, higher
and deeper tissue penetrability, greater cellular uptake and greater ability to
cross the BBB [28]. NPs consist of molecules with dimensions in the order
of 10
9
nm, of dierent kind and compositions capable of containing drugs
and DNA-RNA fragments and able to regulate their transport and intake
into target tissues and cells. NPs show some peculiar features, such as their
surface to mass ratio, which is higher than that of other particles, their quan-
tum properties, and their capacity to transport other compounds [2930].
Nanomedicine is applied in many elds of biology and medicine, such as
uorescent biological labels, drug and gene delivery, detection of pathogens,
detection of proteins, probing of DNA structure, tissue engineering, tumor
destruction via heating, separation and purication of biological molecules
and cells, MRI contrast enhancement, and phagokinetic studies [31]. NP
drug delivery vehicles have shown the ability to encapsulate a variety of ther-
apeutic agents such as small molecules (hydrophilic and/or hydrophobic),
peptides, protein-based drugs, and nucleic acids (Figure 4-1). By encapsu-
lating these molecules inside a nanocarrier, the solubility and stability of
the drugs can be improved, providing an opportunity to reevaluate potential
drugs previously ignored because of poor pharmacokinetics. Encapsulated
Nzwornrcrwr zwn Nzworrcnworoov 15
molecules can be released from nanocarriers in a controlled manner over
time to maintain a drug concentration within a therapeutic window or the
release can be triggered by some stimulus unique to the delivery site [32].
Te surface of the nanocarrier can be engineered to increase the blood circu-
lation half-life and inuence the bio-distribution, while attachment of tar-
geting ligands to the surface can result in enhanced uptake by target tissues.
Te net result of these properties is to lower the systemic toxicity of the
therapeutic agent, while increasing the concentration of the agent in the area
of interest, resulting in a higher therapeutic index for the therapeutic agent.
In addition to therapeutic drugs, imaging agents can also incorporated into
nanocarriers to improve tumor detection and imaging [33]. Finally, nano-
particles can be engineered to be multifunctional with the ability to target
diseased tissue, carry imaging agents for detection, and deliver multiple
therapeutic agents for combination therapy [34]. Te NPs penetrate easily
in the neoangiogenic vessels interstitium, Fig. 4-2 remaining entrapped in
the tumor, with evident higher retention times of drug into tumor. NPs may
be delivered to specic sites by size-dependent passive targeting or by active
targeting. Passive targeting is directly linked to intrinsic cancer cellular and
micro- environmental features. Active targeting involves the use of peripher-
ally conjugated targeting moieties for enhanced delivery of NP systems. Tis
method has been performed to obtain a high degree of selectivity to specic
tissues and to enhance the uptake of NPs into cancer cells and angiogenic
microcapillaries. With these strategies, NPs drug delivering systems mini-
mize the uptake and the toxic side eects of the anticancer agent by nor-
mal cells and enhance the entry and accumulation of the drug into tumor
cells. NPs behavior within the biological microenvironment, stability, and
extracellular and cellular distribution varies with their chemical makeup,
Figure 4-1 Drug encapsulation in a nanocarrier.
16 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
morphology, and size. When injected intravenously, particles are cleared
rapidly from the circulation, predominantly by the liver and the spleen mac-
rophages [35]. Opsonization, which is surface deposition of blood opsonic
factors such as bronectin, immunoglobulins, and complement proteins,
often aid particle recognition by these macrophages. Size and surface char-
acteristics of nanoparticles both play an important role in blood opsoniza-
tion processes and clearance kinetics. Larger particles (200 nm and above)
are more ecient at activating the human complement system and hence
are cleared faster from the blood by Kuper cells. Te binding of blood
proteins and opsonins to NPs dier considerably in amount and in pattern
depending on surface properties, such as the presence and type of functional
groups and surface charge density [3536]. Indeed, precision surface engi-
neering with synthetic polymers can resolve aggregation and aord control
over nano particle interaction and their fate with biological systems. Tis
strategy suppresses macrophage recognition by an array of complex mecha-
nisms, which collectively achieve reduced protein adsorption and surface
Figure 4-2 Schematic structure of dierent nanocarriers for
drug delivery in brain tumors.
Nzwornrcrwr zwn Nzworrcnworoov 17
opsonization. Here, the eciency of the process is dependent on the poly-
mer type, their surface stability, reactivity, and physics (surface density and
conformation) [35]. Suppression of opsonization favors enhanced passive
retention of NPs at sites and compartments.
Prolonged circulation properties are ideal for slow or controlled release
of therapeutic agents into the blood to treat vascular disorders. Long cir-
culating particles may have application in vascular imaging, or even act as
articial nanoscale red blood cells. Recent advances in synthetic polymer
chemistry aord precise control over the architecture and polydispersity of
polymers, polymer-conjugates, and block copolymers. Some of these novel
materials can form sterically stabilized nanoscale self-assembling structures
with macrophage-evading properties. Molecular signatures related to par-
ticular vascular and lymphatic beds and types of endothelial cells have been
identied, providing landmarks for circulating cells and molecules [37]. Tis
requires assembly of the appropriate targeting ligands on nanocarriers and
long circulating nanosystems. However, the ultimate characteristics such
as ligand density, spacing and conformation are dependent on ligand and
particle properties (curvature and surface reactivity). Tese modications
determine the extent of particle stability and aggregation in vivo, as well as
the eciency of receptor binding and follow up events, such as the mode of
particle internalization and associated signaling processes.
Te macrophages represent a valid pharmaceutical target and there are
numerous opportunities for a focused macrophage-targeted approach [38].
Many pathogenic organisms have developed means of resisting macrophage
destruction following phagocytosis. Passive targeting of nanoparticulate ve-
hicles with encapsulated antimicrobial agents to infected macrophages can
represent a natural strategy for eective microbial killing [39]. Degradation
of the carrier by lysosomal enzymes releases the drug into the phagosome-
lysosome vesicle itself, or into the cytoplasm, either by diusion or by specic
transporters depending on the physicochemical nature of the drug molecule.
Intravenous injection of tuftsin-bearing liposomes to infected animals have
not only resulted in delivery of liposome-encapsulated drugs to the mac-
rophage phagolysosomes, but also in the nonspecic stimulation of liver and
spleen macrophage functions against parasitic, fungal and bacterial infec-
tions [40]. Recently nanocarrier-mediated macrophage suicide (delivery of
macrophage toxins) has proved to be a powerful approach in removing un-
wanted macrophages in gene therapy and other clinically relevant situations.
Numerous polymeric and ceramic nanospheres, nanoemulsions, liposomes,
protein cage architectures, and viral-derived nanoparticles act as powerful
adjuvants, if they are physically or covalently associated with protein antigens
[41]. After endocytic uptake of nanoparticles, macrophages partially degrade
the entrapped antigens and channel peptides into the MHC molecules (class
I or II), for processing and presentation. Tus, there is considerable poten-
tial for nanoparticulate adjuvants for the development of new-generation
18 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
vaccines made either recombinant or from synthetic peptide antigens that
are less or no immunogenic in their own right. Recent advances in cell bi-
ology have provided new information regarding the structure, recognition
properties, and signaling functions of a variety of macrophage/dendritic cells
receptors, particularly those that aect immunogenicity. Harnessing these re-
ceptors as therapeutic targets may prove a better strategy for antigen delivery
and targeting with particulate nanocarriers. Dendritic cell receptors such as
DEC-205 and DECSIGN have been implicated in antigen internalization
and presentation to T cells [42].
A unique attribute of nanoplatform-based delivery systems is their mul-
tifunctionality, characterized by multiple components, which include, imag-
ing agents, therapeutic agents, targeting ligands, and cloaking agents that
avoid interference with the immune system. Nanotheranostic platforms are
powerful tools for imaging and treatment of cancer. Multifunctionality of
these nanovehicles oers a number of advantages over conventional agents.
Tese include targeting to a diseased site thereby minimizing systemic toxic-
ity, the ability to solubilize hydrophobic or labile drugs leading to improved
pharmacokinetics and their potential to image, treat and predict therapeutic
response. Targeted nanoparticle-based treatment technologies with diag-
nostic capabilities are referred to as theranostic agents as they form a class of
agents which can serve diagnostic and therapeutic functions simultaneously.
In the current state of technology, tumor detection and therapy are mostly
performed separately. A more ecient and eective method can be achieved
with theranostic nanoparticles, which would integrate the eorts for detec-
tion, treatment and follow-up monitoring of tumor response, and assist
in the decision-making process for the need for further treatment (Figure
4-3). Recently, Bhojani et al. [43] has developed a modular theranostic
Figure 4-3 Schematic structure of a theranostic nanoparticle
(therapeutic agent-yellow; imaging contrast agent-white).
Nzwornrcrwr zwn Nzworrcnworoov 19
nanoplatform, based on a polyacrylamide (PAA) nanoparticle core, with
encapsulated components for synergistic cancer detection, diagnosis and
treatment. Tis platform combined MRI contrast enhancement, photody-
namic therapy and specic targeting to tumor sites using F3 peptide [44].
F3 peptide, a 31-amino acid fragment of a high mobility group protein, was
shown to home to the vasculature of a number of tumor types by interacting
directly with endothelial cells [4546]. In some human cancers F3 peptide
can interact directly with tumor cells, where it is specically taken up at the
cell surface, then internalized into the cell and transported to the nucleus
[4546]. Te authors have shown that signicant therapeutic benet with
photodynamic therapy was obtained when an F3-targeted polymeric nano-
particle formulation consisting of encapsulated imaging agent (iron oxide)
and photosensitizer (Photofrin) was administered to glioma bearing rats.
Using these multifunctional nanoparticles the authors demonstrated that
nanoparticles could be targeted to intracerebral rat 9L gliomas and detected
using MRI [47]. F3-targeted nanoparticles provided a signicantly increased
survival time over that of nontargeted Photofrin encapsulated nanoparticles
or Photofrin alone [47].
Tissue engineering brings together principles and innovations from en-
gineering and the life sciences for the improvement, repair or replacement
of tissue/organ function. Since its inception, this multidisciplinary eld has
been governed by the generic concept of combining cell, scaold (articial
extracellular matrix) and bioreactor technologies, in the design and fabri-
cation of neo-tissues/organs. Microenvironment of organs and tissues is
composed of parenchymal cells and mesenchymal cells (support cells) im-
mersed in the extracellular matrix. Te objective is to enable the body (cel-
lular components) to heal itself by introducing a tissue engineered scaold
that the body recognizes as part of itself and uses this process to regenerate
neo-native functional tissues [48]. Furthermore the construction of organs
by regenerative therapy has been presented as a promising option to address
this decit. Nanotechnology has the potential to provide instruments that
can accelerate progress in the engineering of organs. Achievement of the
more ambitious goals of regenerative medicine requires control over the un-
derlying nanostructures of the cell and extracellular matrix. Cells, typically
microns in diameter, are composed of numerous nanosized components
that all work together, to create a highly organized, self-regulating machine.
Cell-based therapies, especially those based on stem cells, have generated
considerable excitement in the media and scientic communities, and are
among the most promising and active areas of research in regenerative
medicine [49].
4.1 Nanoparticle drug delivery
Within past few years, rapid developments have been made to use nano-
materials in a wide variety of applications in various elds of medicine such
20 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
as oncology, cardiovascular and orthopedics. Nanomaterials have been used
in specic applications such as tissue engineered scaolds and devices, site
specic drug delivery systems, cancer therapy and clinical bioanalytical di-
agnostics and therapeutics. An area of research where nanotechnology and
nanomedicine applications have been particularly prolic pertains to the de-
livery of diagnostic and therapeutic agents.
Drug delivery can be dened as the process of releasing a bioactive
agent at a specic rate and at a specic site. As current advances in bio-
technology and related areas are aiding the discovery and rational design
of many new classes of drugs, it is crucial to improve specic drug-delivery
methods, to turn these new advances into clinical eectiveness. Several
drugs are limited by their poor solubility, high toxicity, and high dosage,
aggregation due to poor solubility, nonspecic delivery, in vivo degrada-
tion and short circulating half-lives. Targeted drug-delivery systems can
increase patient compliance, extend the product life cycle, provide prod-
uct dierentiation and reduce healthcare costs. Nanotechnology can be
correctly envisioned as the future of drug-delivery technology as it has
the potential to provide useful therapeutic and diagnostic tools in the
near future. NPs oer a suitable means to deliver small molecular weight
drugs as well as macromolecules such as proteins, peptides or genes in the
body using various routes of administration. Te ability of the engineered
NPs to interact with cells and tissues at a molecular level provides them
with a distinct advantage over other polymeric or macromolecular sub-
stances. Drug delivery carriers are macromolecular assemblies that can
incorporate imaging and therapeutic compounds of distinct nature, such
as small chemicals, uorophores and biosensors, peptides and proteins,
oligonucleotides and genes. Tey can be designed to improve the solubil-
ity of these cargo molecules and their bioavailability, and also to control
their circulation, biodistribution in the body, and release rate, together
enhancing their ecacy [5051]. Surface property modications confer
advantageous properties to the particle, such as increased solubility and
biocompatibility which are useful in the crossing of biophysical barriers.
Te use of biodegradable materials in the NPs formulation permits drug
release for prolonged periods. For their small size, NPs can extravasate
through the endothelium in inammatory sites, epithelium, tumors, or
penetrate microcapillaries.
4.1.1 Nanoparticle distribution
Te natural clearance and excretion mechanisms of the human body pro-
vide a framework for the rational design of eective nanoparticles for use
in medical therapies. Once a pharmaceutical agent is introduced into the
circulatory system, it is distributed systemically via the vascular and lym-
phatic systems. Te distribution of a drug in a tissue is correlated with the
relative amount of cardiac output passing through that tissue. Accordingly,
Nzwornrcrwr zwn Nzworrcnworoov 21
tissues and organs with high blood ow (brain, liver, heart, intestines, lungs,
kidneys, and spleen) may be exposed to higher concentrations of a drug,
provided that the drug is able to penetrate into the tissues from the vascu-
lature. Particle size and size distribution determine the in vivo distribution,
biological fate, toxicity, and targeting ability of these delivery systems. In
addition, they can inuence drug loading, drug release, and the stability of
nanoparticles. Generally, nanoparticles have relatively high cell uptake and
are available to a wider range of cellular and intracellular targets due to their
small size and mobility. Very small nanomaterials, on the order of 120 nm,
have long circulatory residence times and slower extravasation from the vas-
culature into interstitial spaces. Tis may cause an altered volume of dis-
tribution when administered intravenously. Smaller particles have a larger
surface area-to-volume ratio and thus most of the drug associated with
small particles would be at or near the particle surface, leading to faster drug
release. Smaller particles also have a greater risk of aggregation during stor-
age, transport and dispersion.
Surface manipulation can control the extent of localization at intersti-
tial sites and limit clearance. As nanomaterials are stealthed via hydrophilic
PEGylation, their circulatory residence times increase. Te zeta potential of
a nanoparticle is commonly used to characterize the surface charge property
of nanoparticles [52]. It reects the electrical potential of the particles and
is inuenced by the composition of the particle and the medium in which
it is dispersed. NPs with a zeta potential above 30 mV have been shown
to be stable in suspension, as the surface charge prevents aggregation of the
particles. Endothelial damage or alteration may modify the distribution
parameters of nanoparticles. Inammation, solid tumors, and deliberate
disruption of endothelial contribute to an increased leakiness that provides
vascular contents greater access to extravascular targets. Te presence of
disturbed, porous vascular beds at the tumor allows for selective targeting
by this passive mechanism. Generally speaking solubility, diusion, and bio-
degradation of the particle matrix inuence the drug release process. It is
evident that the method of incorporation has an eect on the release prole.
If the drug is loaded by the incorporation method, then the system has a
relatively small burst eect and sustained release characteristics. If the nano-
particle is coated by polymer, the release is then controlled by diusion of
the drug from the polymeric membrane. Membrane coating acts as a drug
release barrier and thus drug solubility and diusion in or across the poly-
mer membrane becomes a determining factor in drug release. Furthermore,
the release rate also can be aected by ionic interactions between the drug
and auxiliary ingredients.
4.1.2 Nanoparticle functionalization
NP functionalization represents the rst step towards NP drug delivery
systems. Drug delivery carriers can be functionalized to improve control
22 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
of their circulation and biodistribution in the body at the tissue, cellular,
and sub-cellular level. Tis can be achieved by incorporating immune-
evading moieties and/or anity molecules, that favor adhesion to either
general or specic biological markers, depending on the degree of selectiv-
ity required. In addition, when carriers are targeted to cellular receptors
involved in endocytic transport or coupled to cell penetrating peptides, or
if they are designed to modify the permeability of cellular barriers, they
also provide delivery to a variety of intracellular compartments, such as the
lysosome, cytosol, and nuclei [53]. When administered in vivo, therapeutic
agents are recognized as foreign substances and rapidly cleared from the
body. Clearance of foreign compounds in the body occurs mainly by the
reticuloendothelial system (RES), and other elements of the immune sys-
tem, as well as by renal ltration. For most applications, rapid clearance
is detrimental as it minimizes the chances of the delivered agent to reach
its targets in the body and accumulate there, at amounts amenable to ren-
der signicant ecacy. Tis can be achieved by coating nanoparticles with
hydrophilic polymers/surfactants or formulating nanoparticles with bio-
degradable copolymers with hydrophilic characteristics, e.g., polyethylene
glycol (PEG), polyethylene oxide, polyoxamer, poloxamine, and polysorbate
80. PEG helps form a hydrophilic brush around NP cargoes and/or their
carriers, minimizing interactions with plasma opsonins, the complement,
professional phagocytes, and lymphocytes which provide specic immunity.
As a consequence, certain physiochemical properties of the cargo are al-
tered, allowing the platform to gain solubility and to remain elusive from
immune detection. Tis prolongs the circulation in the bloodstream from
a few hours to days, which favors lengthened medicinal eects and less fre-
quent administrations [54]. Another strategy to minimize drug removal
takes advantage of the natural mechanism by which red blood cells in the
body avoid clearance by elements of the innate immune system. Tis is the
case for CD47, a transmembrane protein that acts like a marker of the self
by binding to its cognate receptor expressed on leukocytes. CD47 inhibits
phagocytosis, in part via regulation of the cytoskeleton and inhibition of en-
gulng structures. Incorporation of CD47 on drug carrier surfaces reduces
attachment to neutrophils and macrophages, therefore prolonging circula-
tion and inhibiting inammation [55]. In addition nanocarriers can also
improve control of the drug ecacy upon release in the case of therapeutic
interventions where the administration is local. Localized implantation of
bioactive agents embedded within porous matrices and/or hydrogels ca-
pable of responding to microenvironment properties can provide controlled
release and eects [56]. Encapsulation within these formulations can also
provide sustained release over prolonged periods of time, as oppose to bulk
delivery of a naked therapeutic, which can apply to the release of encapsu-
lated drugs and also bioactive substances produced by cells encapsulated
within these matrices [56].
Nzwornrcrwr zwn Nzworrcnworoov 23
4.1.3 Nanoparticle targeting
One of the major challenges in drug delivery is to carry the drug at the place
where it is needed and to avoid potential side eects on non diseased organs.
After reaching the targeted tissue, drugs should have the ability to selec-
tively kill diseased cells without aecting normal cells. Tese basic strategies
are also associated with improvements in patient survival and quality of life
by increasing the intracellular concentration of drugs and reducing dose-
limiting toxicities simultaneously. In some cases, general enhanced delivery
throughout the body, rather than specic delivery to particular organs, is
preferred. Tis is the case for genetic conditions that aect multiorgan sys-
tems due to ubiquitous distribution of the molecular markers or functions
aected, such as in many monogenic disorders with both peripheral and
central nervous system components. Targeted drug delivery can be achieved
by active targeting of the drugs, or through passive targeting to the site of
action. Active targeting requires the therapeutic agent to be achieved by con-
jugating the therapeutic agent or carrier system to a tissue or cell-specic
ligand [57]. Te success of drug targeting depends on the selection of the
targeting moiety, which should be abundant, have high anity and specic-
ity of binding to cell surface receptors, and should be well suited to chemi-
cal modication by conjugation. Te active targeting can be achieved by
molecular recognition of the diseased cells by various signature molecules
over-expressed at the diseased site, either via the ligand-receptor, antigen-
antibody interactions or by targeting through aptamers. Te therapeutic
agent can be actively targeted by conjugating the carrier with a cell or tissue-
specic ligand, thereby allowing a preferential accumulation of the drug at
the diseased site. PEGylated gold NPs are decorated with various amounts
of human Tf by Choi et al. [58] to enhance active targeting. Teir results
suggest that targeted NPs can provide greater intracellular delivery of thera-
peutic agents to the cancer cells within solid tumors than their non-targeted
analogs.
Passive targeting exploits the anatomical dierences between normal and
diseased tissues to deliver the drugs to the required site, because the physiol-
ogy of diseased tissues may be altered in a variety of physiological conditions
through the enhanced permeability and retention (EPR) eect [59]. Te
dierence between infection-induced EPR eect and that of cancer is the
duration of the retention period. Te retention in normal tissue, where in-
ammation occurs, is shorter than with cancer because the lymphatic drain-
age system is still operative. Te EPR eect has been greatly exploited for
delivering various therapeutics at the site of action, and many studies po-
tentially support this mechanism of passive targeting. Drugs encapsulated
in nanoparticles or drugs coupled to macromolecules can passively target
tumors through the EPR eect. One of the examples is Doxil, a sterically
stabilized PEGylated liposome that encapsulates doxorubicin. Doxil has
24 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
shown good drug retention in the liposomal formulation. In experimental
studies, such systems showed signicant improvements in tumor size re-
duction working through the EPR mechanism. Recently, Chytil et al. [60]
have exploited the EPR eect for targeting HPMA copolymer-based drug
carriers with covalently bound hydrophobic substituents for targeting solid
tumors. Treatment of mice bearing EL-4 T-cell lymphoma with the above
conjugates resulted in signicant tumor regression. Tese nanoconjugates
also enhanced tumor accumulation, indicating an important role of the EPR
eect in excellent anticancer activity of the conjugate. Since most therapeu-
tics agents do not present intrinsic anity to cells, coupling them to carri-
ers with anity properties provides advantages. Hydrophilic and slightly
positively-charged polymers provide anity to the negatively-charged
plasma membrane of cells [51].
Direct intratumor delivery of anticancer agents using NPs can be used
in the treatment of local cancers such as prostate, head and neck cancers.
Recently, Sahoo et al. [61] have demonstrated that transferrin (Tf ) conju-
gated paclitaxel (Tx)-loaded biodegradable NPs are more eective in dem-
onstrating the antiproliferative eect of the drug than its solution or with
un-conjugated Tx-loaded NPs. NPs are emerging as a promising tool for
the intracellular delivery of practically insoluble drugs and sensitive drugs.
Intracellular targeting refers to the delivery of therapeutic agents to specic
compartments or organelles within the cell, and the delivered cargoes must
gain access to intracellular compartments where their molecular targets are
located. Interventions related to RNA interference or delivery of antisense
oligonucleotides requires transport of these cargoes to the cytosol of the
cell.
Gene therapy is a promising new approach for treating a variety of ge-
netic and acquired diseases. Tese macromolecules are unstable and show
a poor cellular uptake and are rapidly degraded by nucleases. To overcome
these limitations, various chemical modications of oligonucleotides have
been tried. Tese modications have disadvantages such as decreased
mRNA hybridization, elevated cytotoxicity, and increased nonspecic tar-
geting. In order to overcome the disadvantages of viral carriers (high cyto-
toxicity, cost, small transgene size), nonviral carriers have been developed.
Te advantages associated with nonviral carriers include facile large scale
manufacture, low immunogenic response, versatile modications, and the
capacity to carry large inserts. Gene therapies require delivery to the cytosol,
with subsequent transport to the cell nucleus. Te drug can be delivered into
target cells by simple diusion, or it may involve complex cellular machinery.
Te major route of intracellular therapeutic uptake is through endocytosis.
Tis strategy is ideal in the case of delivery of therapeutic agents whose ac-
tion is required at said sub-cellular compartments, such as in the case of
carrier-assisted delivery of enzyme replacement for lysosomal storage dis-
orders. Carriers themselves can also be designed to overcome endosomal
Nzwornrcrwr zwn Nzworrcnworoov 25
membranes, such as in the case of pH-sensitive poly(acid) carriers and
temperature-responsive poly(electrolyte) hydrogels [6263]. Other strate-
gies have been designed to directly overcome the plasmalemma. Tese in-
clude electroporation and ultrasound, where a local electric or ultrasound
pulse is exerted in the immediate post-administration period causing tran-
sient enhancement of the plasmalemma permeability [64], and biolistic
particle delivery systems, where penetration into cells is gained by means
of tungsten or gold particles that are propelled by a gene gun across the
plasma membrane [65]. Amphiphilic and biodegradable cationic copoly-
mers are ecient gene delivery systems, which can condense nucleic acid
and form controlled nanosized complexes. Polyamidoamine (PAMAM) and
poly[2-(dimethylamino) ethyl methacrylate] (PDMAEMA) are low toxic
polymers which have shown great potential as carriers. Polycaprolactone
(PCL) is another promising delivery system. PCL-g-PDMAEMA nano-
particle/DNA complexes could escape from the endosome and release their
payloads eectively in cytoplasm, which may be induced by the enhanced
interaction between the complexes and cell membrane, due to hydropho-
bic modication [66]. Small interfering RNA (siRNA) has attracted much
attention because it enables sequence-specic manipulation of expression
for multiple endogenous genes. Te intracellular release of siRNA from
pluronic/poly(ethylenimine) nanocapsules was achieved by changing the
nanocapsules from a collapsed state to a swollen state using a brief cold
shock treatment [67]. Weber et al. [68] reported an amino-terminated car-
bosilane dendrimer-bound siRNA delivery system. Tese RNase-resistant
carbosilane/siRNA dendriplexes have a high and prolonged gene-silencing
eect, and can be safely used in serum and antibiotics containing medium,
without aecting cell viability and metabolic activity at relatively high den-
drimer concentrations. One of the most common methods used for the
systemic delivery of siRNA involves their electrostatic interaction with cat-
ionic liposomes. Self-assembled liposome-protamine-hyaluronic acid nano-
particles, modied by DSPE-PEG with conjugated ligand have been used
to overcome innate immune responses of siRNA-based therapy. Te devel-
oped nanoparticle formulation has a siRNA encapsulation eciency of 90%
and showed a reduced systemic immunotoxicity [69].
4.2 Nanomedicine and cancer
Cancer, a disease characterized by the uncontrolled growth and spread of
abnormal cells, is still the second most common cause of death in the U.S.
According to the American Cancer Society, about 571,950 Americans are
expected to die in 2011 due to cancer, and that means more than 1,500
deaths per day. Current treatments for various cancers include surgery, ra-
diation, hormone therapy, and chemotherapy. Although these conventional
therapies have improved patients survival, they have also shown several limi-
tations. Te National Cancer Institute (NCI) has identied nanotechnology
26 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
as having the potential to make paradigm-changing impacts on the detec-
tion, treatment, and prevention of cancer. Te growing interest in nanotech-
nology by both academic and industrial investigators has led to increased
development of novel nanotechnology platforms for medical applications,
sharp increases in government funding, and venture capital investment. In
the cancer context, nanotechnology will lead to a new generation of diag-
nostic and therapeutic technologies, creating a range of new solutions for
diagnoses and treatment of neoplastic diseases [45, 26, 7073].
Diagnostic methods are essential for the early detection of diseases to
enable their prompt treatment, minimizing possible damage to the rest of
the organism. Conventional imaging technologies represent static images
of tumors, rather than a continuous visualization of tumor proliferation.
Nanodiagnostics, dened as the use of nanotechnology for clinical diagnos-
tic purposes [74], was developed to meet the demand for increased sensi-
tivity in clinical diagnoses and earlier disease detection. NP-based systems
imaging allows an early detection of tumor, as well as opportunities for
real-time monitoring, thereby increasing both the sensitivity and accuracy
of anticancer therapies. Initial results in nanotechnology-enabled molecular
imaging have been made in all imaging modalities, including optical, nu-
clear, ultrasound, computed tomography, and magnetic resonance imaging
(MRI). MRI contrast agents have made a signicant impact in the use of
MRI for various clinical indications. MRI contrast agents contain paramag-
netic or superparamagnetic metal ions that aect the MRI signal properties
of surrounding tissue. Tese contrast agents are used primarily to increase
the sensitivity of MRI for detecting various pathological processes and also
for characterizing various pathologies. In addition, the contrast agents are
used for depicting normal and abnormal vasculature, or ow-related abnor-
malities and pathophysiologic processes like perfusion. A conglomerate of
numerous nano-sized iron oxide crystals coated with dextran or carboxydex-
tran forms superparamagnetic iron oxide (SPIO) contrast agents [75]. Two
SPIO particle formulations are now clinically available, namely ferumoxides
and ferucarbotran. Both are approved specically for MR imaging of the
liver. After intravenous administration, clinical approved SPIO particles are
cleared from the blood by phagocytosis accomplished by reticuloendothelial
system so that uptake is observed in the normal liver, spleen, bone marrow,
and lymph nodes. After the intracellular uptake, SPIOs are metabolized in
the lysosomes into a soluble, nonsuperparamagnetic form of iron that be-
comes part of the normal iron pool [75]. Following intravenous injection,
SPIO is incorporated into macrophages via endocytosis. Te uptake of
SPIO by phagocytic monocytes and macrophages provides a valuable in-
vivo tool by which MRI can be used to monitor involvement of macrophages
in inammatory processes, such as multiple sclerosis, traumatic nerve injury,
stroke, brain tumors, and vulnerable plaque in carotid artery. Neuwelt et al.
[76] conducted clinical studies with MRI monitoring of macrophages in
Nzwornrcrwr zwn Nzworrcnworoov 27
brain tumours. Te macrophage MRI detection with SPIO of tumor mor-
phology might facilitate the surgical resection or biopsy of brain tumors.
Te main goal of nanotechnology in brain tumor imaging is an accu-
rate and early diagnosis without side toxic eects and the evaluation of the
ecacy of non-invasively treatments [5, 77]. Tese new cellular targeting
based imaging detection methods can reach the specic and selective mo-
lecular recognition only for tumor cells, through the recognition of tumor
specic molecules into ligand-receptor, antibody-antigene interaction, or
other interaction processes between nanoparticle drug-loaded systems and
cancer cells, leading to a diuse and complete delivering of drug into can-
cer cells [78]. Te achievement of higher targeting eciency per NP will
require the nding of more ecient bio-markers for cancer and correspond-
ing targeting moieties. By detecting and analyzing tumor cells and tissues
with nanotechnologies, the internal biological features of cancer during its
occurrence and development can be revealed. Generally speaking, the ap-
plication of nanotechnology in medical diagnostics can be subdivided into
in vitro diagnostic devices and in vivo imaging. Te improvements in the
technologies to characterize cells or cell compartments in vitro (optical and
luminescence microscopy, scanning probe microscopy, electron microscopy
and imaging mass-spectrometry) have been important for the development
of nanomedicine. Te miniaturization and integration of dierent functions
in a single device, based on nanotechnology-derived techniques, have led to
a new generation of devices that are smaller and faster, and give accurate
readings. Tey require much smaller samples, implying less invasive and
traumatic sample extraction methods, and deliver more complete and more
accurate biological data from a single measurement. Te use of these de-
vices in research has become routine, and has improved the understanding
of the molecular basis of disease, as well as helping to identify new therapeu-
tic targets. In vitro diagnostic devices mainly include nanobiosensors and
microarrays. Te nanobiosensors are systems composed by biological and
biomimetic recognition elements. Interaction between the compound of in-
terest and the recognition element produces a variation of physical-chemical
properties (pH, electron transfer, heat, potential, mass, and optical proper-
ties). Prototype sensors have been successfully used to detect nucleic acids,
proteins and ions. Tey can operate in liquid or gas phase, opening up an
enormous variety of downstream applications. Tese detection systems use
inexpensive low-voltage measurement methods and detect binding events
directly [49].
Microarray-based studies have enormous potential in the exploration of
diseases such as cancer, and in the design and development of new drugs.
Microarrays have been widely applied in the study of various pathological
conditions, including inammation, atherosclerosis, breast cancer, colon can-
cer and pulmonary brosis [79]. As a result, functions have been assigned to
previously unannotated genes, and genes have been grouped into functional
28 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
pathways. Several types of microarray have been developed for dierent tar-
get materials, which can be DNA, cDNA, mRNA, protein, small molecules,
tissues, or any other material that can be quantitatively analyzed. A DNA
array consists of a large number of DNA molecules in an orderly arrange-
ment on a solid substrate to form a matrix of sequences in two dimensions.
cDNA microarrays and oligonucleotide microarrays are used for microarray
expression analysis, and to determine the level or volume of expression of a
given gene. Single nucleotide polymorphism microarrays detect mutations
or polymorphisms in a gene sequence [80]. Tis technology is used to test
an individual for disease expression patterns, and to determine whether or
not individuals are susceptible to a disease.
Nanotechnology has produced advances in imaging diagnosis, develop-
ing novel methods and increasing the resolution and sensitivity of existing
techniques. Tese systems include positron-emission tomography (PET),
single-photon-emission CT (SPECT), uorescence reectance imaging,
uorescence-mediated tomography (FMT), ber-optic microscopy, optical
frequency-domain imaging, bioluminescence imaging, laser-scanning confo-
cal microscopy and multiphoton microscopy [81]. Te main benets of mo-
lecular imaging for in vivo diagnosis lie in the early detection of disease and
the monitoring of disease stages, supporting the development of individu-
alized medicine and the real-time assessment of therapeutic and surgical
ecacy. MRI, CT, PET and SPECT are the most widely used and studied
modalities in cancer patients. Overall, nuclear imaging by PET or SPECT
oers greater sensitivity, but is limited by the lack of anatomical context,
whereas MRI provides accurate anatomical detail but no data on cell vi-
ability and shows poor sensitivity [82]. Although none of these modalities
is ideal, MRI is the preferred option for cellular tracking. Detecting proton
relaxations in the presence of a magnetic eld yields tomographic images
with excellent soft tissue contrast, and can locate the cells of interest in the
context of the surrounding milieu (oedema or inammation) without the
use of harmful ionizing radiations. In addition, MRI oers a longer track-
ing window in comparison to PET and SPECT, which are limited by the
decay of the short-lived radioactive isotopes. New contrast agents, used to
increase the sensitivity and contrast of imaging techniques are increasingly
complex and formed by synthetic and biological NPs. NPs possess certain
size-dependent properties, particularly with respect to optical and magnetic
parameters, which can be manipulated to achieve a detectable signal. Te pri-
mary event, in most nanoparticle-based assays is the binding of a nanopar-
ticle label or probe to the target biomolecule that will produce a measurable
signal characteristic of the target biomolecule. A probe that is to function
in a biological system must be water-soluble and stable and have mini-
mal interaction with the surrounding environment. Although remarkable
achievements have been made in nanodiagnostics during recent years, most
of these techniques are still under laboratory investigation. Nida et al. [83]
Nzwornrcrwr zwn Nzworrcnworoov 29
used quantum dots that were attached to epithelial growth factor receptor
and were conjugated with anti-growth antibody, to detect early biomarkers
of cervical cancer. Cross et al. [84] installed a tiny probe on a spring using
nanotechnology, and used it to explore a cell surface and measure its soft-
ness, which was used as a marker to determine whether carcinogenesis had
occurred in the cells. Gao et al. [85] used quantum dots to locate and image
tumors in vivo. Tey coated quantum dots with a layer of polymer NPs and
polyethylene glycol, and attached them to a prostatic gland specic mono-
clonal antibody. Fluoerescent image analysis revealed multi-color uores-
cent images that were sensitive to tumor cells in vivo, as well as information
regarding tumor volume and location. Nasongkla et al. [34] performed a
study on polymer micelle loaded with superparamagnetic iron oxide and
found it promising in the dual-targeting delivery and hypersensitive MR in
cancer cells.
Nanomedicine can improve the targeting ability of chemotherapeutic
agents. Rapaport et al. [86] managed to deliver chemotherapeutic agents
accurately into tumor cells using multifunctional NPs which improved the
targeting ability of chemotherapeutic agents and helped destroy cancer
cells eectively. In a recent study was reported that a polyethylene glycol-
phospholipid nano micelle loaded with adriamycin could selectively accu-
mulate in tumor tissue, and penetrate thick layer of tumor tissue. Integrated
quantum dots and glucose-binding protein antibodies selectively recognize
cancer cells. Tese cells, when irradiated by ultra-violet ray showed green
uorescence. Tis strategy allows the dierentiation of normal cells and
cancer cells. A prolonged ultra-violet irradiation can eliminate the cancer
cells [87]. Recently, Chakravarty et al. [88] coated a carbon nanotube with
a monoclonal antibody against specic targets on lymphoma cells. When
these signed cells were exposed to near infrared light, the carbon nanotube
started to kill these cells by heating them up. A large number of NPs can
serve as carriers of anti-cancer drugs. Drugs incorporated in the nanocarri-
ers, either physically entrapped or chemically tethered, have the potential to
target physiological disorder zones sparing normal cells from collateral con-
sequences. Te pharmacokinetic prole, especially the transportation capa-
bilities, of the drug substances have been greatly modied by incorporation
in a nanodrug delivery system. Tese include enhanced accommodation for
targeting moieties such as chaperones, and alteration in release rates com-
prising of controlled release and site-specic delivery, by use of molecular
engineering techniques. Additionally, encapsulation of the drug substances
in various polymeric and inorganic composites have also been evaluated for
their rationalization of the drug delivery systems. Such encapsulations are
generally made for protecting the biologically active protein and peptide-
based drug compounds from the detrimental eects of biological uids.
In gene therapy, exogenous genes are introduced into cells by properly de-
signed carriers, so as to cure the disease by correcting the abnormal genes.
30 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
Te eciency of liposomes, as non-viral gene delivery vectors, has been in-
creased through surface ligand targeting via monoclonal antibodies, to specic
receptors upregulated on cancer cell surfaces. A biopolymeric gene deliv-
ery nanoparticle has recently been shown to be eective in vivo, in delaying
tumor growth. Tis polymeric nanoparticle-based non-viral gene delivery
vector is a cationic albumin-conjugated pegylated nanoparticle, in which
a plasmid, encoding the proapoptotic Apo2 ligand/tumor necrosis factor-
related apoptosis-inducing ligand (Apo2L/TRAIL), is incorporated. After
intravenous injection of plasmid-loaded nanoparticles, plasmid DNA was
incorporated and inhibited tumor growth [89]. Additionally allied tech-
nologies, such as atomization and pressurization, have come in to play to
facilitate the preparation of nanotechnological carriers. One such comprises
a novel method of atomization, namely electrohydrodynamic atomization
used in an electrospraying method. Pressurization techniques such as high
hydrostatic pressure technology for encapsulation of genes into polymeric
nanomaterials have recently been studied for their ecacy in delivering the
biologically active compounds. Tese novel technologies oer advantages by
eliminating the usage of toxic cationic polymers and chemical tethers, fur-
ther replacing them by simple yet eective hydrogen bonding.
4.3 Nanomedicine and toxicity
Nanotoxicology evaluates the interactions of NPs with biological systems
and the relationship between the physical and chemical properties of NPs
with the induction of toxic biological responses. Currently, a complete evalu-
ation of the size, shape, composition and aggregation-dependent interactions
of NPs with biological systems is lacking, and thus it is unclear whether the
exposure of humans, animals, and plants to engineered nanostructures could
produce harmful biological responses. NPs constitute a part of particulate
matter, and human exposure to NPs has been increased in the past century
because of the industrial revolution. Te same characteristics which make
NPs so attractive in medicine, may contribute to the toxicological prole of
NPs in biological systems. NPs own electronic, optical, and magnetic prop-
erties that are related to their physical dimensions, and their breakdown
could lead to a unique toxic eect that is dicult to predict. NPs surfaces
also, are involved in many catalytic and oxidative processes which may be
potentially cytotoxic. Some NPs contain metals or compounds with known
toxicity, and thus the breakdown of these materials could elicit similar toxic
responses to the components themselves. Many people can be exposed to
nanostructures in a variety of methods such as researchers manufacturing
nanostructures, patients injected with nanostructures, or people using prod-
ucts containing nanostructures. Most of the recent studies in this area have
focused on the absorption of the nanostructures via inhalation or dermal
exposure. In the respiratory system NPs activate dierent transcription fac-
tors with up-regulation of pro-inammatory protein synthesis. Interestingly,
Nzwornrcrwr zwn Nzworrcnworoov 31
various types of NPs can induce dierent inammatory reactions. For ex-
ample, single-walled carbon nanotubes are more toxic in inducing epithe-
lioid granuloma [90]. Mixed carbon NPs and nanotubes are able to induce
platelet aggregation in vitro and accelerate the rate of vascular thrombosis
in rat carotid artery [91]. In CNS, neutral NPs and low concentrations of
anionic NPs have no eect on BBB integrity, whereas high concentrations
of anionic NPs and cationic NPs are toxic for BBB. NPs seem to stimulate
the production of reactive oxygen species and oxidative stress [92]. After
absorption, NPs distribute to various organs, tissues, and cells. Only a few
recent studies have focused on in vivo biodistribution of engineered NPs as
it relates to the nanostructures physical parameters. In studies with quan-
tum dots and single-walled carbon nanotubes, it was discovered that a high
dose of the quantum dots is sequestered in the liver, and the percentage
of these NPs dose sequestered is dependent upon the surface modication
[93]. Although targeted NPs have emerged as one strategy to overcome the
lack of specicity of conventional chemotherapy, there are other potential
risks and challenges associated with this novel strategy. Some cancer cell
types would develop drug resistance, rendering drugs released from the tar-
geted NPs to be ineective. Also the targeted NPs might change the stabil-
ity, solubility, and pharmacokinetic properties of the carried drugs. Te shelf
life, aggregation, leakage, and toxicity of materials used to make NPs are
other limitations for their use. Some materials used to make NPs show low
toxicity, but degrade quickly and do not circulate in tissues long enough for
sustained drug/gene delivery. On the other hand, other materials such as
carbon nanotubes and quantum dots are durable and can persist in the body
for weeks, months, or even years, making them potentially toxic and limiting
their use for repeated treatments. New materials to make targeted NPs such
as silicon/silica (solid, porous, and hollow silicon NPs) have been developed.
However, their use for drug delivery to cancer patients has taken o slowly
due to the potential health risks associated with introducing new materials
in the human body. A systematic quantitative analysis of the pharmacokinet-
ics (absorption, distribution, metabolism, and excretion) of NPs, can lead
to improvements in the design of NPs for diagnostic and therapeutic ap-
plications, a better understanding of nanostructures non-specicity toward
tissues and cell types, and assessments of basic distribution and clearance,
that serve as the basis in determining their toxicity and future investigative
directions. Besides developing new materials and selecting appropriate ma-
terials for each specic treatment, other factors need to be optimally selected
in order to design better targeted NPs. Tese factors include the particles
size, shape, sedimentation, drug encapsulation ecacy, desired drug release
proles, distribution in the body, circulation, and cost. Despite extensive re-
search eorts to develop new targeted NPs, only a few of them are in clinical
use including Abraxane, Doxil, and Myocet
TM
, and are approved by the
FDA. A major contributor to the slow development of eective targeted
32 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
NPs has been the lack of knowledge about the distribution and location of
targeted NPs after either oral administration or injection. Tese important
steps in a nanoplatforms-based drug delivery should be investigated to im-
prove knowledge about systemic ways of administration and their advan-
tages and limits, as well as acute and chronic local and systemic toxic eects.
Most studies have not examined the targeting eciency of NPs in vivo in
real time, and thus precise bio-distribution and subsequently therapeutic
eects are not well-known. Terefore, detecting malignant cells in the body
and monitoring treatment eects on these cells in real time is another chal-
lenge needed to be overcome in the development of ecient targeted NPs.
5. Nanoparticle tecbnologies
Te rst described nanoscale drug delivery systems were lipid vesicles [94].
Te rst application of targeted liposomes was reported in 1980 [95]. Since
then, research has led to important progress in the development of nano-
particles engineered to have multifunctional capabilities, as well as smart
properties such as the ability to respond to the environment, to facilitate
more eective drug delivery strategies. Nanoparticle technologies for nano-
medicine include polymeric NPs, polymer-drug conjugates NPs, micelles,
liposomes, metal complexes, carbon derivates, peptides NPs, silica NPs,
quantum dots and dendrimers. Te diversity of delivery systems allows
nanoparticles to be developed with a diverse array of shapes, size, and com-
ponents which enables them to be tailored for specic applications. However,
the primary consideration when designing any drug delivery system is to
achieve more eective therapies, by controlling the drug concentration in
the therapeutic window, reducing cytotoxic eects, and improving patient
compliance.
5.1 Polymeric and polymer-drug conjugate nanoparticles
Polymeric NPs are synthesized using various methods according to the
needs of the application and type of drugs to be encapsulated. Tese NPs are
extensively used for the nanoencapsulation of various useful bioactive mol-
ecules and medicinal drugs. Polymeric NPs are structured in two dierent
forms, nanospheres and nanocapsules. Tey are, respectively, characterized
by a matrix system in which the drug is dispersed, and a reservoir in which
the drug is conned in a hydrophobic core surrounded by a single polymeric
membrane (core-shell structure). Tese carriers show a higher stability in bi-
ological uids and against the enzymatic metabolism. Teir nanometer-size
promotes eective permeation through cell membranes and stability in the
blood stream. Polymers are being developed to create delivery systems with
excellent drug and protein loading and release properties, a long shelf life,
and little toxicity. Te core matrix of these NPs can be composed of various
biodegradable polymers, such as poly(lactic-coglycolic acid) (PLGA), chito-
san, poly(alkylcyanoacrylate) (PACA), poly(butylcyanoacrylate) (PBCA),
poly(lysine), poly(e-caprolactone) (PCL), and PAsp (polyaspartate). Te
degradation drug release rate of these polymers can be controlled by ad-
justing their molecular mass, and in the case of copolymers, their composi-
tion and microstructure [96]. Polymer NPs have been used as transport
vectors for various peptide CNS delivery after intravenous injection, such
as hexapeptide dalargin, loperamide, tubocurarine and doxorubicin. PLGA
(poly-d,l-lactide-co-glycolide) is one of the most successfully used biode-
gradable nanosystems because it undergoes hydrolysis in the body to pro-
duce the biodegradable metabolite monomers, lactic acid and glycolic acid.
Surface modication of PLGA, drug encapsulation methods and particle
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch05_Bionanoparticles.indd 33 Manila Typesetting Company 08/22/2012 11:44PM
34 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
size, additives added during formulation, molecular weight of drug, and
the ratio of lactide to glycolide moieties have a strong inuence on the re-
lease and eective response of formulated nanomedicines. For those of an
acidic nature, PLGA monomers are blended with alginate, chitosan, pectin,
poly(propylenefumarate) polyvinylacohol, and poly(orthoester). Paclitaxel
promotes the polymerization of tubulin causing cell death by disrupting
the cell division process. Tis drug show neoplastic activity against primary
ovarian carcinoma as well as breast and colon cancers. It is one of the po-
tent anticancer agent but less useful for clinical administration due to its
poor solubility. PLGA intermingled with vitamin E, and tocopheryl poly-
ethylene glycol succinate (TPGS) has been used to encapsulate this drug.
Tis formulation has shown good activity, and a much faster administra-
tion in comparison to traditional formulation. Using some additive with the
PLGA-NPs, 100% drug encapsulation eciency was achieved with full an-
titumor activity [97]. Cisplatin is a valid anticancer drug, but the full thera-
peutic exploitation of cisplatin is limited due to its toxicity in healthy tissues.
Te cisplatin have been encapsulated on PLGAmPEG NPs prepared by
double emulsion methods. PLGAmethoxy(polyethylene glycol) (mPEG)
NPs revealed prolonged drug residence in blood upon intravenous admin-
istration [98]. Tamoxifen prevents proliferation of pre-cancerous cells. Tis
compound competitively binds to estrogen receptors on tumors, producing
a nuclear complex that decreases DNA synthesis and inhibits estrogen ef-
fects. Tamoxifen loaded polyethylene oxide (PEO) modied PCL was pre-
pared by a solvent displacement method. About 90% drug encapsulation
eciency has been achieved when tamoxifen was loaded in the ratio of 10%
by weight of polymer. PEOPCL nanoparticles exhibited a signicantly
increased level of accumulation of the drug within the tumor with time,
as well as extended presence in the systemic circulation [99]. Polyethylene
glycolPCL amphiphilic block copolymeric nanospheres containing taxol
are reported to show promising anticancer activity. It was reported that this
mPEG/PCL diblock copolymeric nanospheres system could be potentially
useful as a novel delivery system for the anticancer drug taxol, having an
outer shell of mPEG and a hydrophobic inner core of PCL [99].
Polymers can also be used to coat other types of nanoparticles.
Polyethylene glycol (PEG) is a hydrophilic polymer that has been used to
coat the surface of NPs, which allows them to avoid clearance by the RES
and cross the BBB [100]. Te mechanism of this phenomenon is thought
to arise from receptor-mediated phagocytosis and passive leakage through
permeable capillaries in tumors [100]. In the 9L gliosarcoma model, PEG
coating of a NP MRI contrast agent increased the amount of MRI signal in-
tensity from the agent [101]. Other hydrophilic polymers, including hydro-
gel (polyacrylamide), dextran, and polysorbate, have been used to coat the
surface of nanoparticles to prolong plasma circulation and improve delivery
across the BBB [100].
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch05_Bionanoparticles.indd 34 Manila Typesetting Company 08/22/2012 11:44PM
Nzwovznrrcrr Trcnworoorrs 35
Polymer-drug conjugates are formed through side-chain grafting of drugs
to polymer chains, allowing them to deliver high doses of chemotherapeutic
drugs. Tese agents bear numerous functional groups that are available for
covalent binding to a variety of biochemically active groups, which direct
them to malignant tumors where they can deliver functional drugs acting
on several tumor targets [102]. Nanoconjugates that carry more than one
functional group provide the capability to simultaneously inhibit several tu-
mor pathways, deliver optimal drug concentrations to the site of treatment,
and reduce adverse eects on healthy tissue. Nanoconjugate polymers are
generally synthesized around a polymer with pendant functional groups like
OH, COOH, or NH2. Nanoconjugates are also smaller in size, less
immunogenic and chemically more stable in plasma. Prolindac (AP5346)
is composed of a HPMA backbone copolymer with platinum grafted to
the side chains through a pH-sensitive chelator designed for drug release
in the tumor environment. Preclinical data demonstrates superior ecacy
of the polymer-drug conjugates, using multiple cancer models including a
M5076 sarcoma platinum-resistant tumor xenograft mice model, multiple
colon xenograft models, L1210 leukemia, and 0157 hybridoma models
[103]. Polyamino acids grafted with drugs on the side chains are another
class of polymerdrug conjugates that have demonstrated high drug load-
ing and ecacy [104]. In the case of polyglutamate-glycine-campthotecin
(CT-2106), degradable linkers have allowed drug loadings ranging from 5%
to 50% [105]. Nanoconjugates can overcome drawbacks of conventional
chemotherapy such as drug resistance and toxicity by specically targeting
tumor cells, activating cancer cell uptake, and bypassing multidrug resis-
tance transporters. Meanwhile, Xyotax, a similar polymerdrug conjugate
(polyglutamate-paclitaxel), is used in several clinical trials including prostate
cancer, metastatic breast cancer, neck cancer, and metastatic colorectal can-
cer. Te clinical data shows an improvement in median survival in Xyotax
patients compared with the control group. One benet of the treatment was
the reduction of multiple side eects including neurotoxicity [106].
5.2 Micelle nanoparticles
Micelles nanoparticles (MNPs) are amphiphilic spherical structures com-
posed of a hydrophobic core and a hydrophilic shell. Te hydrophobic part
is the inner core of the block copolymer which encapsulates the poorly
water-soluble drug, whereas the outer hydrophilic shell or corona of the
block protects the drug from the aqueous environment and stabilizes the
MNPs against recognition in vivo by the RES. Te core can sometimes be
made up of a water-soluble polymer that is rendered hydrophobic by the
chemical conjugation of a water-insoluble drug, and by complexation of the
two oppositely charged polyions. Te polymer always contains a nonionic
water-soluble segment and an ionic segment that can be neutralized by an
oppositely charged surfactant to form a hydrophobic core. Te electrostatic
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch05_Bionanoparticles.indd 35 Manila Typesetting Company 08/22/2012 11:44PM
36 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
interaction between the ionic segment of the block polymer and the surfac-
tant group changes these segments from water-soluble to water-insoluble,
leading to a hydrophobic core in the micelles [107]. MNPs can be engi-
neered by means of ligand coupling, or addition of pH-sensitive moieties,
according to the biological characteristics of the diseased site for active tar-
geting. All these features related to MNPs make them ideal carriers for anti-
cancer drugs and tumor targeting [108]. On reaching the target site, micelles
are internalized into the cells via uid-state endocytosis. To overcome per-
meability problems, amphiphilic copolymers are used to encapsulate poorly
water-soluble anticancer drugs in MNPs. Tese have an inner core made
up of hydrophobic block copolymer in which the drug becomes entrapped,
and an outer shell of hydrophilic block copolymer that reduces the interac-
tions of drugs with the outer aqueous environment, keeping them stable.
Te hydrophilic outer part can be made up of polyethers like PEG, and
poly(ethylene oxide) (PEO). Other hydrophilic shells are made up of poly-
mers such as poly(acryloylmorpholine), poly(trimethylene carbonate), and
poly(vinylpyrrolidone). Genexol-MNP is the rst non-targeted polymeric
micellar formulation approved for cancer therapy. It is currently being evalu-
ated in a clinical phase II trial in the USA for metastatic pancreatic cancer
therapy. Te clinical phase II results showed ~30% of the patients had a
stable disease status and 60% of the patients had an increased survival of
one year [109].
Many recent studies have revealed that polymer-conjugated drugs and
nanoparticles show prolonged circulation in the blood followed by passive
accumulation in tumors, even in the absence of targeting ligands, demon-
strating the existence of a passive retention mechanism. Tumor vasculature
showed a high proportion of proliferative endothelial cells, increased tortu-
osity and aberrant basement membrane formation. Tese features render
tumor blood vessels permeable to macromolecules. Tus, numerous studies
have shown, that the EPR eect causes passive accumulation of macromol-
ecules and NPs in solid tumor, enhancing the therapeutic index while de-
creasing side eects. Active targeting aims to increase the drug delivery to
the target utilizing biologically specic interactions such as antigen-antibody
binding or locally applied signals such as sonication or heating. Active tar-
geting makes use of characteristics shown by the tumor cells, such as over-
expression of cell surface tumor-associated antigens that are at low levels in
normal tissue cells, as well as of the tumor specic antigens and the relatively
more acidic nature of tumor compared to normal tissue. Active targeting de-
creases adverse side eects, because the drug accumulates only in the tumor
sites, and it allows cellular uptake of the drug through endocytosis.
Surfactants are being incorporated into anticancer metal-based drugs.
Te surfactant dodecyl amine reacts with selenious acid to produce a qua-
ternary ammonium salt, which can be conjugated to copper or cobalt ions
to form copper or cobalt cationic complexes. Initial studies demonstrated
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch05_Bionanoparticles.indd 36 Manila Typesetting Company 08/22/2012 11:44PM
Nzwovznrrcrr Trcnworoorrs 37
eectiveness in vitro against ve human monolayer tumor cell lines. Namely
MCF7 (breast carcinoma), HEPG(2) (liver carcinoma), U-251 (glioma),
HCT116 (colon carcinoma), and H-460 (lung carcinoma). Recent evalu-
ation has been undertaken of the potential antitumor activity of NK012,
a 7-ethyl-10-hydroxycamptothecin (SN-38) micellar formulation, and
bevacizumab in human lung cancers [110]. Nude mice bearing PC-14 or
A549 lung adenocarcinoma xenografts show evidence of signicant tumor
growth inhibition compared to saline controls. B-lapachone (b-lap) is a
novel anticancer agent, whose cell-killing eect is activated by the enzyme
NADPH-quinone oxidoreductase 1 (NQO1), a avoprotein overexpressed
in breast, prostate, and lung cancer [111]. In cancer cells where NQO1 is
over-expressed, the agent undergoes futile cycling, resulting in the genera-
tion of reactive oxygen species (ROS). Experimental studies have demon-
strated that growth inhibition occurs in cells over-expressing NQO1, while
cells in which NQO1 is absent are unaected at equivalent concentrations.
Antitumor ecacy was examined in female nude mice bearing subcutaneous
A549 lung tumors and orthotopic Lewis lung carcinoma. Following intrave-
nous administration of b-lap micelles, A549 tumor growth suppression was
evidenced. In the Lewis lung carcinoma model a doubling of survival was
observed (16 days compared to 8 days in controls) [112]. Another target
for molecular cancer therapy is heat shock protein 90 (HSP90), a molecular
chaperone, which under normal conditions is responsible for prevention of
protein aggregation [113]. HSP90 becomes over-expressed under condi-
tions of stress, resulting in tumorigenesis and increased proliferation in a
variety of cancers including lung, prostate, and breast. Tanespimycin, a de-
rivative of the HSP90 inhibitor geldanamycin, has been explored clinically
for chemotherapeutic purposes. Te mechanism of action of tanespimycin
involves the degradation of oncogenic signaling proteins, inducing cell death
via apoptosis. In patients with multiple myeloma, treated with tanespimy-
cin, disease stabilization was observed [114].
5.3 Liposomes
Liposomes (Figure 2-2) are vesicles made up of a lipid bilayer, resembling a
cell membrane. Te lipids form a bilayer based on hydrophobic interactions
in continuous parallel packing, with the hydrophilic head groups positioned
towards the aqueous environment. Tey possess advantages of carrying hy-
drophilic, lipophilic, as well as amphoteric drug molecules, either entrapped
inside it or on its micellar surface. Te brain distribution of long circulating
liposomes can be modulated by conjugation of appropriate targeting vectors.
Examples of brain targeting vectors include monoclonal antibody (mAbto
anti-transferrin receptor, mAb to insulin receptor), cationized proteins (cat-
ionized human serum albumin), endogenous peptides or plasma proteins.
Te basic mechanism by which these liposomes achieve brain concentration
by crossing the BBB is by coupling with brain drug transport vector through
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch05_Bionanoparticles.indd 37 Manila Typesetting Company 08/22/2012 11:44PM
38 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
absorptive-mediated transcytosis, or by receptor-mediated transcytosis.
Hence, by manipulating the liposome structures, they can be constructed
to be temperature or pH sensitive to permit controlled release of their con-
tents. Te dual problems of mediating BBB transport and inhibiting periph-
eral clearance of liposomes were solved by the combined use of PEGylation
technology and chimeric peptide technology [115]. After surface modica-
tion of liposomes with these substances, they behave as a sterically stabi-
lized one, due to enhanced hydrophilicity imparted by polymers hydrophilic
chains, a lower contact angle between particles and phagocytic cells of body,
and due to the lesser interaction between serum opsonins, thereby prevent-
ing opsonisation. Constructed temperature-sensitive liposomes loaded
with doxorubicin in combination with local hyperthermia, show a com-
plete regression of human tumor xenografts in all the mice studied [116].
Te encapsulation of doxorubicin in polyethylene glycol-coated liposomes
(Doxil/Caelyx [PLD]), was developed to enhance the safety and ecacy of
conventional doxorubicin. Te liposomes alter pharmacologic and pharma-
cokinetic parameters of conventional doxorubicin, so that drug delivery to
the tumor is enhanced while toxicity normally associated with conventional
doxorubicin is decreased. In preclinical models, PLD produced remission
and cure against many cancers, including tumors of the breast, lung, ovaries,
prostate, colon, bladder, and pancreas, as well as lymphoma, sarcoma, and
myeloma. PLD appeared to overcome multidrug resistance, possibly as the
result of increased intracellular concentrations and an interaction between
the liposome and P-glycoprotein function [117]. Several phase II studies
showed promising activity of PLD in recurrent ovarian cancer patients with
response rate ranging from 16 to 25% [118].
Bevacizumab is a recombinant humanized monoclonal antibody that in-
hibits VEGF, a growth factor ligand responsible for angiogenesis. Results
from several phase III clinical trials comprising colorectal, non-small cell
lung and breast cancer, demonstrate that bevacizumab results in superior
patient response rates. Bevacizumab can be used as a targeting moiety to
enhance the NPs ecacy. For this reason, bevacizumab-labeled cationic
liposomes have been developed, to improve targeting to several pancre-
atic cancer cell lines including Capane1, HPAFeII, and PANCe1 [119].
Bevacizumab-conjugated liposomes had modest impacts on cell viabil-
ity in vitro, and demonstrated increased cellular uptake by PANCe1 cells
grown in the presence of VEGF. Protein stabilization of liposomes is being
studied to deliver hydrophobic drugs such as docetaxel for cancer therapy.
Docetaxel is encapsulated into the liposome bi-layer and stabilized by albu-
min to prevent rapid drug leakage (ATI-1123). Te results of ATI-1123 ef-
cacy studies in human xenograft mice models for prostate, pancreatic, and
non-small-cell lung cancer showed partial tumor regression in 90% of the
PC3 tumor xenograft model, and improved ecacy in the pancreas model
[120]. Small-interfering RNA fragments have been found to suppress gene
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch05_Bionanoparticles.indd 38 Manila Typesetting Company 08/22/2012 11:44PM
Nzwovznrrcrr Trcnworoorrs 39
expression, with immense silencing eciency and relatively low toxicity.
siRNAs degrade extremely rapidly in physiological environments and are
eliminated almost immediately from circulation upon injection. Liposomes
prove ideal carriers for biological agents such as siRNA because of their
stable aqueous core. Moreover, it is possible to combine RNA-interfering
strategies with traditional chemotherapeutics. One example is the Raf/
MEK/extracellular signal-related kinase (ERK) pathway, which is essential
for cellular proliferation, and found to be aberrant in several cancers [121].
As a result, several inhibitors of key proteins in the cascade have been de-
veloped as potential chemotherapeutics. Recently, it has been demonstrated
that liposomes encapsulating a Mcl1-specic siRNA (siMcl1) and a chemi-
cal MEK inhibitor (PD0325901) showed a valid antitumor ecacy in vitro
and in vivo. Following encapsulation and complexation of PD0325901 and
siMcl1 respectively, the liposomal formulation was administered to KB cells.
Western blot results showed that co-delivery of both agents signicantly re-
duced expression of Mcl1 and pERK1/2 proteins [122]. Antisense therapy
represents a gene silencing strategy that stands to make a profound impact
on cancer therapy. In a phase I study, a liposomal formulation, LErafAON,
that encapsulates the raf antisense oligonucleotide, was administered with
the purpose of acting on c-raf, a protein that bestows cancer cells with resis-
tance to radiation or chemotherapy. In patients with advanced solid tumors
undergoing radiation therapy, the c-raf-1 mRNA was inhibited in three, four
exhibited partial response, four had stable disease, and four showed progres-
sive disease [123]. Recently, the use of bisphosphonates, such as zoledronic
acid, was explored as a treatment strategy, given its ability to inhibit the re-
lease of growth factors essential for cancer cell growth and dierentiation in
bone. Emerging data from several clinical trials serves to highlight a poten-
tial anticancer eect of zoledronic acid, as well as chemotherapeutic synergy
with established drugs [124]. However, zoledronic acid has an extremely
rapid blood clearance and preferential accumulation in bone, necessitat-
ing encapsulation in nanoparticles. Lipo-ZOL is a liposomal formulation
of zoledronic acid that increases circulation times, reduces accumulation in
bone, and increases targeting to tumors [125].
5.4 Gold and silver nanoparticles
Gold nanoparticles (GNPs) (Figure 2-2) exhibit unique physicochemical
properties, including the ability to bind amine and thiol groups, allowing
surface modication and use in biomedical applications. GNPs are used to
prepare nanoshells composed of gold and copper, or gold and silver to func-
tion as contrast agents in MRI, and gold-silica for photothermal ablation of
tumor-cells. Classically GNPs enter into cells with a non-specic receptor
mediated endocytosis mechanism [126]. In vivo GNPs passively accumulate
at tumor sites that have leaky immature vasculature with wider fenestrations
than normal mature blood vessels. Diculties in utilizing the EPR eect for
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch05_Bionanoparticles.indd 39 Manila Typesetting Company 08/22/2012 11:44PM
40 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
tumor drug delivery exist owing to the heterogeneity of tumor vasculature,
particularly at the centre of poorly dierentiated cancers, as well as particle
detection and uptake by the RES. PEGylation represents the most com-
mon method of reducing RES uptake, producing a hydrated barrier caus-
ing steric hindrance to the attachment of phagocytes. GNPs have also been
used for cancer cell imaging and targeting. In various clinical trials the 27-nm
citrate-coated GNPs bound with thiolated PEG and tumor necrosis factor-a
(TNF-a) (CYT-6091) (Aurimmune; CytImmune Sciences, Rockville, MD)
has shown an increase of tumor targeting [127]. An important feature of
GNPs is their capacity to absorb and scatter specic wavelengths of light
across the visible and near-infrared (NIR) spectrum. Te most useful nano-
shells have a silica core diameter of around 120 nm, with a 10 nm layer
of gold shell, and they absorb NIR light (800 nm) and can create intense
heat lethal to cells. An in vivo study demonstrated that 100nm gold nano-
shells maximally accumulated in SK-BR-3 human breast tumors 24 h after
intravenous injection. When a laser tuned to the nanoshell resonance was
applied, average tumor temperatures increased by 9uC in control mice, and
37uC in nanoshell-treated mice, with irreversible tissue damage in the nano-
shell group. All mice in the nanoshell group survived 90 days with no evi-
dence of tumor recurrence [128]. Positive results in vivo, were also obtained
with photothermal ablation therapy in a mouse model for colon carcinoma
after intravenous administration of PEG coated gold nanoshells [78]. Te
GA-GNPs (GNPs stabilized by gum arabic (GA) is used for diagnostic
and therapeutic applications, showing optimal in vitro and in vivo stabil-
ity. Te compound is nontoxic, distributes minimally to non-target organs
in biodistribution studies, and produces contrast on CT imaging [129].
A study group has shown an approach for imaging and targeting cancer
cells using dendrimer entrapped GNPs (G-DENPs). G-DENPs, which
when covalently linked to folic acid and uorescein isothiocyanate mol-
ecules are stable, hydrophilic, biocompatible, and able to specically bind to
cancer cells that over-express high-anity folate receptors. Te folic acid-
conjugated nanoparticles are subsequently endocytosed into lysosomes
of cancer cells, providing a means for targeting and imaging of these cells
[130]. An interesting new therapeutic strategy foresees the connection of
antibodies- nanoshells is able to target cancer cells by interacting with specic
surface antigen expressed only by tumor cells. Te benet of the nanoshell-
mediated approach is that the energy can pass through the healthy tissue
and leave the neighboring cells intact while killing only the tumor cells that
have been targeted by the nanoshells.
Silver nanoparticles (SNPs) are part of the emerging nanotechnology
that have gained increasing interest in the eld of nanomedicine due to their
particular properties and therapeutic potential in treating a large variety of
disease [131132]. Te biological activity of silver has been attributed to
the presence of the Ag+ ion. SNPs inhibit the vascular endothelial growth
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch05_Bionanoparticles.indd 40 Manila Typesetting Company 08/22/2012 11:44PM
Nzwovznrrcrr Trcnworoorrs 41
factor-induced angiogenesis in retinal endothelial cells. Alteration of the
permeability barrier integrity plays a major role in drug-based therapies, as
well as the pathogenesis of cardiovascular diseases, inammation, acute lung
injury syndromes, and carcinogenesis. Recently the molecular mechanism
of SNPs on VEGF-and IL-1b-induced retinal endothelial cell permeability
has been evaluated. Both VEGF and IL-1b increase endothelial cell perme-
ability via an Src dependent pathway. SNPs were found to block VEGF and
IL-1b-induced permeability in retinal endothelial cells from porcine retina,
and this inhibitory eect was dependent on the modulation via Src phos-
phorylation at Y419 [133]. A novel study has demonstrated the antitumor
activity of biologically synthesized SNPs in a Daltons lymphoma ascites tu-
mor system in vitro, by activation of the caspase 3 enzyme which is known
to have a potent inhibitory eect on disease progression in a mouse model,
leading to a potent restorative eect in the treated tumor volume [134].
5.5 Metal oxide
Titanium dioxide (TiO
2
) is a semiconductor, well-known as a ultraviolet
light (UV)-inducible catalyst in the photooxidation of organic substrates
and the deactivation of bacteria, algae, and viruses [135136]. Under UV
excitation, TiO
2
NPs of various sizes and morphologies have been reported
to exhibit cytotoxicity toward some tumors [137138]. One recent example
[137] describes 50 nm rhodamine-labeled TiO
2
/PEG constructs able to be
internalized into rat glioma C6 cells. Te antitumor performance was evalu-
ated in glioma cell spheroids representing a provisional three-dimensional
model valuable for translation to animal xenografted models. Te cytotoxic
eect of the UV-irradiated photocatalyst depended on the concentration
of TiO
2
/PEG and the light exposure time. More than 90% of cells were
killed by a UV dose of 13.5 J cm
2
in the presence of the nanocatalyst at a
concentration of 0.5 mg/mL. Moreover, uorescent images of the photo-
catalyst-treated spheroids co-stained with apoptosis and necrosis markers,
Annexin V-FITC and propidium iodide, reveal the prevalence of induced
apoptotic cell death within rst 6 hours. Functionalization of 5 nm high
crystallinity TiO
2
NPs with a monoclonal antibody recognizing IL13R fos-
tered nanoparticle delivery specically to GBM cells in a manner dependent
upon cellular membrane IL13R expression. Te direct visualization of the
TiO
2
-antibody/receptor interaction and mapping of the IL13R location
and distribution throughout a single A172 brain cancer cell was demon-
strated using synchrotron-based X-ray uorescence microscopy [139140].
It is well established that UV-photoexcitation of bare TiO
2
particles in
aqueous solution results in the formation of various ROS, mainly hydroxyl
(OH), peroxy (HO
2
) radicals, and singlet oxygen (
1
O
2
) [141]. However, in
the case of DA- and DA-antibody-modied TiO
2
particles, ROS arise from
multiple, mechanically distinct redox chemistries, and the principal ROS
produced is the superoxide anion, formed by reaction of photogenerated
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch05_Bionanoparticles.indd 41 Manila Typesetting Company 08/22/2012 11:44PM
42 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
electrons with molecular oxygen [142]. Further in cellulo studies of photo-
induced cytotoxicity toward A172 glioma cells in the presence of selective
ROS quenchers were consistent with these results [139]. Nanostructured
porous TiO
2
has been developed as a biocompatible nano-device for con-
stant chemotherapy drug release into the CNS [141]. A porous titania car-
rier uploaded with low concentrations of a cytostatic platinum complex was
capable of inducing DNA fragmentation, possibly via a strong interaction
between nitrogen atoms in nucleotides, and Lewis acid sites on both the ti-
tania surface, and the platinum complex coordination sphere. Application of
this material directly on to C6 glioma xenografted into Wistar rats resulted
in a signicant decrease in tumor size and growth rate.
5.6 Magnetic nanoparticles
MRI is one of the most frequently-used, non-invasive imaging tools for dis-
ease diagnosis and monitoring, including cancer. Imaging techniques that can
selectively image proliferating cells in vivo, can provide critically important
insights into tumor growth rate, degree of tumor angiogenesis, eectiveness
of treatment, and vigor of normal cells. Contrast agents that are commonly
used in clinical practice for the brain and spinal cord MRI are based on
gadolinium. However, a major problem associated with MRI is its low sen-
sitivity. Utilization of nanotechnology to improve the sensitivity and ecacy
of MRI for cancer detection and imaging is an area that researchers have
focused on in the last several decades. Magnetic NPs, used in biomedical
applications mainly, have an inorganic nanoparticle core and in most cases
are coated by a suitable coating material. Suitable coatings not only increase
the stability and solubility of the nanoformulation, but can also be used to
incorporate a targeting moiety to increase the imaging sensitivity and to do
real-time monitoring. Enhanced proton relaxation is one of the most added-
value properties that make magnetic NPs one of the best contrast agents
for biomedical applications of MRI. Iron oxide and superparamagnetic iron
oxide-(SPIO) NPs exhibit magnetic properties, which are used for MRI
imaging and also provide an opportunity to control particle transport by
external magnets. Superparamagnetic iron oxide contrast agents either form
the core of magnetic NPs that have a polymeric coating, or are more ho-
mogeneously integrated into polymeric NPs [100]. Te signal intensity of
these NPs is related to the size of the particle, its position, its concentration
within a given voxel, data acquisition parameters, the magnetic eld, and
the dosage of the SPIO-NP [75]. SPIO-NP has been used as a bowel con-
trast agent (Lumerin, Gastromark) and for spleen/liver imaging (Endorem,
Feridex). Macrophage-specic uptake of SPIO-NPs increases the contrast
between healthy and diseased tissue because most liver tumors are devoid of
it. Negative enhancement eects of SPIO-NPs on T1/T2-weighted MRI
sequences, allowed increased lesion conspicuousness and increased lesion
detection as compared to non-enhanced imaging. It is well documented
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch05_Bionanoparticles.indd 42 Manila Typesetting Company 08/22/2012 11:44PM
Nzwovznrrcrr Trcnworoorrs 43
that with the help of this technique, liver tumors or metastases as small as
23 mm can be detected. Trough conjugation of iron oxide NPs with
hydrophilic polymer coatings, such as dextran or PEG, it is possible to ob-
tain a sterically preventing opsonisation of NPs in the serum and a reduction
of their uptake by the RES [143]. Recently antibiofouling polymer-coated
magnetic NPs as nanoprobes for MRI have been characterized. SPION
were coated with the protein- or cell-resistant polymer, poly(TMSMA-t-
PEGMA), to generate stable, protein-resistant MRI probes. Te compound
could detect tumors in vivo using MRI, and can be used as a potentially ef-
cient cancer diagnostic probe [101]. MNPs exhibit acute toxicity in vivo,
which has limited their clinical translation. Oxidative stress and interference
with mitochondrial energy production by MNPs can lead to cytotoxicity.
5.7 Carbon nanotubes
Carbon nanotubes (CNs) are essentially cylindrical molecules made of car-
bon atoms. CNs are synthesized by rolling sheets of graphene into hollow
tubes that are single-walled (SWNTs) (0.4- to 2-nm diameter), double-
walled (1- to 3.5-nm diameter), or multi-walled (MWNTs) (2- to 100-nm
diameter). CNs can be synthesized by heating carbon black and graphite in
a controlled ame environment. One of the main advantages of the CN is
its ability to deliver drugs directly to cancer cells. It has also been suggested
that CNs could be used as nanocarriers for delivering drugs into the body
via injectable routes [144]. Drugs can either attach to the outer surface of
the CNs via functional groups, or be loaded inside the CNs. Attachment
of the anticancer drug to the outer surface of the CNs can be through ei-
ther covalent or noncovalent binding, including hydrophobic, stacking,
and electrostatic interactions [145]. Te mechanism by which CNs enter
cells is unclear. Te evaluated processes are the passive diusion of CNs
through the lipid bilayers of the cell membrane, and the attachment of CNs
to the external cell membrane, resulting in its absorption by the cell, using
an energy-dependent process. Generally speaking, small CNs with a length
of up to 400 nm are internalized by a diusion mechanism, while CNs of
400 nm in length are internalized by endocytosis [146]. Functionalization
and alteration of CNs and other graphite nanoplatfom surface chemistry
can reduce or eliminate complement activation, while making the CNs more
biocompatiable [147]. Functionalized SWNTs were conjugated with pacli-
taxel through branched PEG chains via a cleavable ester bond. Te resultant
formulation was more eective in suppressing tumor growth in vivo than
Taxol or paclitaxel-PEG conjugated in a 4T1 breast cancer animal model
[148]. Similar ndings have been obtained when paclitaxel was loaded into
PEGylated SWNTs or MWNTs using HeLa cells and MCF-7 cancer cells
lines [149]. Kam et al. [150] have shown the possibility to direct nanotubes
to specically targeted cancer cells by using coating of nanotube surface
with folic acid. In this way carbon nanotubes bind specically to cancer
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch05_Bionanoparticles.indd 43 Manila Typesetting Company 08/22/2012 11:44PM
44 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
cells that over-express folate receptors, and then allow receptor-mediated
endocytosis of nanotubes. With this approach is possible to introduce genes
directly into tumor cells without any cellular or viral vector by using aero-
sol, systemic delivery or microcellular injection. Another interesting use of
carbon nanotubes, is characterized by their ability to carry short interfer-
ing RNA (siRNA) molecules that exert RNA interference on target gene
expression [151]. Te authors used siRNA-conjugated carbon nanotubes
that specically targeted murine telomerase reverse transcriptase, and show
that delivery of siRNA into tumor cells silences the target gene, inhibits the
proliferation of cancer cells in vitro, and suppresses tumor growth [151].
CNs are also able to absorb light in the near infrared (NIR) region resulting
in heating of the nanotubes [152]. Engineering the structure of MWNTs,
by creating intentional surface defects or dopants, will cause scattering in
the travelling current and also increase the heating of the nanotube. Tis
physical feature of the engineered MWNTs can be employed to thermally
destruct the tumor cells by using MWNTs that have good heat conduct-
ing properties. Although CNs toxicity is not fully understood and toxicity
study results are conicting, it is important to be aware of potential compli-
cations. It has been noted that as the particle size decreases, the surface area
of the particles increases. Tis means that there will be more area available
for chemical interactions to take place, which would enhance the toxicity of
the particles. A novel research report shows that when murine epidermal
cells were exposed to unpuried SWCNTS containing 30% iron, signi-
cant dose-dependent activation of transcription factor AP-1 occurred [153].
Systemic application of CNs can result in oxidative stress in end organs, and
inhalational exposure of CNs can result in acute lung injury, inammation
and brosis [154].
5.8 Fullerenes
Fullerenes are a family of carbon allotropic compounds in form of a hol-
low sphere, ellipsoid or tube. Te most common form is C60. It has also
led to the discovery or synthesis of other fullerene variations, such as C70,
C20 (the smallest member), carbon nanotubes (elongated, tube-structured
fullerene), carbon nano-onions, and nano buds [155]. An important prop-
erty of the C60 molecule is its high symmetry. Fullerenes have the ability
to assume dierent forms and to encage compounds. Te unique physical,
chemical, electrical, and optical properties of fullerenes and their derivatives
have led to their incorporation into new or improved devices and materials,
and to advancements in engineering, industry, and science. However, the dif-
cult processibility of fullerenes has presented a major problem in the hectic
search for medicinal applications. C60 is insoluble in aqueous media and ag-
gregate very easily. Commonly, fullerenes are encapsulated in special carriers
like cyclodextrins, calixarenes, polyvinylpyrrolidone, micelles and liposomes.
A second technique is that of chemical functionalization with amino acid,
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch05_Bionanoparticles.indd 44 Manila Typesetting Company 08/22/2012 11:44PM
Nzwovznrrcrr Trcnworoorrs 45
carboxylic acid, polyhydroxyl group, amphiphilic polymers to increase the
hydrophilicity.
Fullerenes and their derivatives show potential antiviral activity. Te
antiviral activity of fullerene derivatives is based on several biological
properties, including their molecular architecture and antioxidant activity.
Another potential medical application of fullerenes is related to their photo-
excitation. In fact, fullerene can be excited from ground state to
1
C60 by
photo- irradiation. In the presence of molecular oxygen, the fullerene can
decay from its triplet to ground state, transferring its energy to O
2
, gen-
erating a single oxygen
1
O
2
, and is highly cytotoxic. Again, in the presence
of oxygen, the fullerene radical anion can transfer one electron, produc-
ing a superoxide anion radical O
2
and an hydroxyl radical OH [156].
Iwamoto and Yamakoshi [157] introduced a highly water soluble C60-N
vinylpyrrolidine copolymer as agent for photodynamic therapy. Liu et al. [158]
demonstrated the use of a poly-ethylene glycol (PEG)-conjugated fullerene
containing Gd
3+
ions for photodynamic therapy in combination with MRI.
Te authors demonstrate through experimental data, that tumor PDT eect
was signicantly promoted by photosensitizer tumor targetability and MRI
activity. By attaching hydrophilic moieties, fullerenes become water-soluble
and are capable of carrying drugs and genes for cellular delivery. A lipophilic
slow-release drug delivery system which employs fullerene derivatives to en-
hance therapeutic ecacy in tissue culture, was designed by Zakharian et al.
[159]. So modied fullerenes have the potential to provide a signicant anti-
cancer activity in cell culture, as demonstrated with C60-paclitaxel conjugate.
Research continues into ways to increase the solubility of fullerenes and to
investigate the toxicity of fullerenes and their derived compounds.
5.9 Peptides nanoparticles
Peptides that specically interact with receptors over-expressed by cancer
cells have been successfully developed as targeting molecules for drug deliv-
ery and in vivo imaging [160]. Te interaction of peptides and proteins with
the cell membrane results in their penetration into the cell, or the formation
of pores within the cell membrane. Because of their ability to target and
enter cells, peptide and protein carriers hold great potential for the deliv-
ery of genes and antisense oligonucleotides to cancer cells [160]. Bombesin
(BBN) peptide and its analogs can be used to target gastrin-releasing pep-
tide (GRP) receptors. Tus, in vivo GRP receptors are over-expressed in
GBM, small cell lung, gastric, pancreatic, prostate, breast, cervical, and co-
lon cancers. Recently, GNPs functionalized by a high load of thioctic acid-
bombesin peptide were used to target prostate tumor xenografts in SCID
mice. Using normal and prostate tumor-bearing mice, they showed that
this compound exhibits a high binding anity to the tumor, and conrmed
that these constructs are GRP receptor specic and accumulate with high
selectivity in GRP receptor-rich pancreatic acine [161]. Fibroblast growth
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch05_Bionanoparticles.indd 45 Manila Typesetting Company 08/22/2012 11:44PM
46 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
factor analogs can be used to target cells expressing broblast growth factor
receptors (FGFRs). Tis receptor family is often expressed both on tumor
cells and neo-vasculature. Truncated human basic broblast growth factor
peptide (tbFGF) was recently used to achieve targeting of liposomes carry-
ing chemotherapeutic drugs [162]. Tis peptide contains both the bFGF
receptor binding site and a part of the heparin-binding site, which allows
it to bind FGFRs on a cell surface, without stimulating cellular prolifera-
tion. Somatostatin and its analogs can be used to target somatostatin recep-
tors over-expressed in both small cell and non-small cell lung cancers. Te
albumin-bound paclitaxel (Abraxane) is currently being tested as a rst-line
therapy, or in combination with other drugs, for metastatic breast cancer and
other cancers that have been shown to be sensitive to taxane drugs, such as
ovarian and prostate. Preclinical studies have shown that the concentration
of paclitaxel, bound to albumin in endothelial cells and in the extra-vascular
space, was signicantly increased [163]. Peptides can also act as therapeutic
agents conjugated to NPs. Melittin is a cytolytic peptide that represent a
potential candidate for cancer chemotherapy. Melittin is a 26 amino acid
a-helical peptide derived from the venom of the honeybee Apis mellifera.
It is a nonspecic cytolytic peptide that attacks all lipid membranes, lead-
ing to signicant toxicity when injected intravenously. Te basis of melittins
action is a physical and chemical disruption of membrane structure result-
ing in a profound compromise of the cell permeability. Recently, it has been
demonstrated that synthetic nanoscale vehicles like PFC nanoparticles can
deliver melittin by exible passive and active molecular targeting to kill both
established solid tumors and precancerous lesions. Tis study has proposed
a novel linking strategy to generate biocompatible peptide-nanostructures
for lipidic nanocarriers, including PFC nanoemulsions, liposomes, as well as
cells for combined molecular imaging and cell-targeted therapeutics [164].
5.10 Silica nanoparticles
Silica is major component of sand and glass, and it has been used in the syn-
thesis of NPs. Functional groups can also be added to the surface, making
them appealing for designs for dierent applications. Immunouorescent la-
beling of both a cancer cell surface marker and tissue sections by dye-doped
silica NPs has demonstrated high specicity and high intensity [165].
Dierent strategies have been explored for using silica NP probes to target
cancer cells. Anity and specicity associated with the antibody-antigen
recognition have been studied in developing immunoassays. Primary or sec-
ondary antibodies are covalently immobilized onto the NP surface in order
to selectively and eciently bind various cancer cells [166]. In one study, a
mouse anti-human CD10 antibody was used as the recognition element on
NPs. Fluorescence microscopy was then used to image the leukemia cells.
Te brightly uorescent cells bound with NPs were easily detected under
the uorescence microscope [167]. Other anity reagents, such as receptor
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch05_Bionanoparticles.indd 46 Manila Typesetting Company 08/22/2012 11:44PM
Nzwovznrrcrr Trcnworoorrs 47
ligands and recognition peptides, can also be attached onto NPs in order to
label cell-membrane proteins. For instance, folic acid was attached to dye-
doped silica NPs and targeted to SCC-9 cancer cells, which over-express
folate receptors [168].
Peptide-targeted uptake is another ecient technique for cancer cell im-
aging. Tis technique is based on the propensity of the cells to recognize
and internalize NPs labeled with specic peptides, and even deliver them to
specic cellular compartments. Human lung adenocarcinoma (A549) cells
(in vitro) and rat brain tissue (in vivo) were successfully labeled using TAT-
labeled NPs. Using this strategy, diagnostic and therapeutic agents can be
delivered to the biological target of interest [168]. Recently, aptamers have
emerged as a novel class of ligands. Aptamers are short strands of DNA/
RNA for recognition of a variety of targets, including proteins and small
molecules, as well as complex samples. Aptamers have signicant advantages
over antibodies and peptides, including high anity, excellent specicity,
and lack of immunogenicity. Specic targeting of acute leukemia cells with
aptamer-conjugated NPs has been developed using uorescence microscopy
or ow cytometry [169]. NP-aptamer conjugates greatly increase the uo-
rescence signal from the cell. Tis property shows the potential applications
of silica NPs in the elucidation of cells with low densities of aptamer binding
sites, or with relatively weak binding probes where the uorescence signal
from the uorophore is too weak for observation [170]. Tris(2,2-bipyridyl)
dichlororuthenium(II) hexahydrate (RuBpy)-doped silica NPs have been
used as highly sensitive and photostable labels in Aymetrix GeneChips
technology. Biotin-labeled cRNA samples from a human lung cancer cell
line were hybridized on the arrays, and then incubated with streptavidin and
staining with PEG-biotin-labeled NPs. Even with the present unfavorable
imaging modality and existing optical excitation and detection systems of the
GeneChips, the uorescent silica NPs were demonstrated to be superior to
the traditional streptavidin-phycoerythrin (SAPE). Fluorescent silica NPs
can act as nonviral vectors for gene delivery and biophotonics methods, and
may be used to optically monitor intracellular tracking and gene transfec-
tion. Te potential of cationic silica NPs was investigated for in vivo gene
transfer [171]. Te NPs were tested for their ability to transfer genes in vivo
in the mouse lung, and a two-fold increase in the expression levels was found
with silica particles in comparison to enhanced green uorescent protein
(EGFP) alone. Silica NPs are also promising candidates for improved drug
delivery systems because of their intrinsic hydrophilicity, biocompatibility,
and nontoxicity, as well as the excellent protection they provide for their
encapsulated drugs. With drug molecules loaded into silica NPs, surface
modication of the NPs with bio-recognition entities can allow specic cells
or receptors in the body to be located. Upon target recognition, NPs can
then release their drug payload at a rate precisely controlled by tailoring the
internal structure of the particles according to a desired diusion (release)
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch05_Bionanoparticles.indd 47 Manila Typesetting Company 08/22/2012 11:44PM
48 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
prole. Te high surface area (>900 m2/g), tunable pore diameter and
uniform mesoporous structure of the mesoporous silica NPs oer unique
advantages for loading and releasing large quantities of biomedical agents.
Mesopores loaded with guest molecules were capped by inorganic NPs, or
large organic molecules, via a chemically cleavable disulde linkage to the
mesoporous NP surface. Since drug molecules are eectively physically
trapped, they are unable to leach out of the mesoporous NP host thus pre-
venting any premature release. Compared with many current biodegradable
polymer-based drug delivery systems, that rely on the hydrolysis-induced
erosion of the carrier structure, the mesoporous NP structure provides the
ability to release the cargo in a controlled manner [172].
5.11 Quantum dots
Quantum dots (QDs) (Figure 2-2) are structurally colloidal semiconductor
nanocrystals, ranging from 2 to 10 nm in diameter. QDs can be synthesized
from various types of semiconductor materials via colloidal synthesis or elec-
trochemistry. Te most commonly used QDs are cadmium selenide (CdSe),
cadmium telluride (CdTe), indium phosphide (InP), and indium arsenide
(InAs). Tese NPs have unique photophysical properties, such that upon
excitation they emit uorescence that is brighter and more stable than that
of traditional uorophores, and their size can be varied to achieve excita-
tion and emission at dierent wavelengths. QDs can be used as probes for
high-resolution molecular imaging of cellular components, for tracking cell
activities and movement inside the body, for specic targeting interaction
through antibodies linked onto NPs surface, with specic tumor-associated
antigens expressed on cancer cell surface. Tis interaction permits penetra-
tion inside targeted cancer cells of specic drugs, protein, siRNA, genetic
materials, and antisense oligonucleotides and modulates genic expression
into the cancer cells genome. In vivo cancer targeting and imaging in liv-
ing animals by QDs was rst demonstrated by Gao et al., [173] wherein
both subcutaneous injection of QD tagged cancer cells (prostate cancer)
and systemic injection of multifunctional QD probes were used to achieve
sensitive and multicolor uorescence imaging of cancer cells. Te utility of
the quantum dot (QD)-aptamer(Apt)-doxorubicin (Dox) conjugate [QD-
Apt(Dox)] as a novel targeted cancer imaging, therapy, and sensing system
has been demonstrated in a recent a study. Te targeted QD imaging sys-
tem (QD-Apt) was capable of dierential uptake and imaging of prostate
cancer cells that express the prostate specic membrane antigen (PSMA)
[174]. Te Tan et al. [175] study group conjugated siRNA targeting the
gene encoding human epidermal growth factor receptor-2 (HEGFR-2) to
QDs by using these last ones not only as carriers, but also as a means to
monitor the transfection eciency. By directing antibodies against EGFR-2
over-expressed by breast cancer cells, it was possible to induce a selective
interaction of siRNA-QDs conjugates with cancer cells, and a receptor-
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch05_Bionanoparticles.indd 48 Manila Typesetting Company 08/22/2012 11:44PM
Nzwovznrrcrr Trcnworoorrs 49
mediated endocytosis of conjugates and subsequent silencing eects on the
target gene through RNA interference. CdSe particles may leak cytotoxic
cadmium ions after long-term exposure to ultraviolet light, whereas CdTe
particles produce reactive oxygen species as a result of the loss of their pro-
tective coating after longterm circulation.
5.12 Dendrimers
A dendrimer is generally dened as a macromolecule which is characterized
by its highly branched 3D structure, which provides a high degree of sur-
face functionality and versatily (Figure 2-2) [176]. Te generation number
and the chemical composition of the core, branches, and surface functional
groups, determine the size, shape, and reactivity of dendrimers. Dendrimers
have attracted attention as possible drug carriers because of their unique
properties, namely their well dened three-dimensional structure, the avail-
ability of many functional surface groups, their low polydispersity, and
their ability to mimic. Dendrimers can function as drug carriers either by
encapsulating drugs within the dendritic structure, or by inter-acting with
drugs at their terminal functional groups via electrostatic or covalent bonds
(prodrug) [177]. Dendrimers have been studied extensively for targeting
and delivery of therapeutic agents for cancer and of contrast agents for mag-
netic resonance imaging. Te avidimers are dendrimers targeted to tumor
vasculature using a methotrexatepolyamidoamine (PAMAM) bioconjugate
platform functionalized with small targeting ligands [178]. Te authors dem-
onstrated in vitro, that drug-free dendrimer conjugates were not cytotoxic,
and that drug-loaded dendrimer conjugates had no eect on folate receptor-
negative cells. Polyanionic PAMAM dendrimers showed rapid serosal
transfer rates in crossing an adult rat intestine in vitro, and had low tis-
sue deposition. Te transport of PAMAM and surface-modied PAMAM
across cell monolayer follows endocytosis-mediated cellular internalization.
However, non-biodegradable dendrimers may potentially accumulate in lys-
osomes depending on their frequency and dose of administration. Various
studies report that PEG-modied dendrimers show reduction of cytotox-
icity and immunogenicity, high exocytosis rate and low accumulation in
endothelial cells, with excellent solubility and a favorable pharmacokinetic
[179]. Amine-terminated polyamidoamine (PAMAM) dendrimers appear
to be an ideal class of building blocks for developing multifunctional gene
vectors. Angiopep is a high brain penetration peptide, which targets to the
low-density lipoprotein receptor-related protein-1. Ke et al. [180] coupled
angiopep to PEGylated PAMAM dendrimer G5.0 via the distal end of PEG,
and used it to deliver pEGFP-N2 plasmid to the brain both in vitro and in
vivo. Te plasmid DNA covalently labeled with uorescent dye, ethidium
monoazide bromide (EMA), was detected in the brain of the mice treated with
the PAMAMPEG-Angiopep/DNA. Multimodal dendrimer- conjugated
magnetouorescent nanoworms, called dendriworms, were developed recently
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch05_Bionanoparticles.indd 49 Manila Typesetting Company 08/22/2012 11:44PM
50 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
for siRNA delivery [181]. Te magnetic core in dendriworms enables in
vivo imaging of dendriworms with MR while PAMAM dendrimers con-
jugated to the magnetic core, allows nucleic acid delivery and targeting.
Dendriworms accumulate in the lungs and the reticuloendothelial ltration
organs following systemic delivery. Dendriworms administered with CED,
eciently delivered EGFR siRNA to suppress the expression of EGFR in
glioblastoma tumors in a mouse model [181]. Yang et al. [182] prepared
epidermal growth factor (EGF)-carrying boronated PAMAM dendrimer
G4.0 for neutron capture therapy of brain tumors. Doxorubicin was conju-
gated to RGD-coupled PEGylated PAMAM dendrimer, via a degradable
disulde spacer, for controlled release in the treatment of glioma tumors
[183]. PAMAM dendrimers have been tested as genetic material carriers.
SuperFect-DNA complexes, a transfection reagent consisting of activated
dendrimers, are characterized by high stability and provide more ecient
transport of DNA into the nucleus. Te high transfection eciency of den-
drimers may be due to their well-dened shape but also to the low pK of
the amines [184].
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch05_Bionanoparticles.indd 50 Manila Typesetting Company 08/22/2012 11:44PM
6. Nanomedicine applications in brain tumors
In the last decade various studies have demonstrated the value of nano-
technology in brain tumor treatment. Nanomedicine can give many ideal
devices for delivery of specic compounds to brain tumors, loading them
into nanoparticle-based carriers via a variety of chemical methods including
encapsulation, adsorption and covalent linkage. In brain tumor treatment,
various molecules at dierent steps and pathways, such as cell immortaliza-
tion and apoptosis escape, tumor neoangiogenesis, and invasion of normal
tissues have been studied as possible targets of a novel therapeutic model.
Recent advances in molecular, biological and genetic diagnostic techniques
have evidenced new cerebral glioma-associated biomarkers and their impli-
cations for gliomas progression. Te possibility to block the more contem-
porary pathway into glioma by molecular-based targeted approaches, using
a nanocarrier loaded with anti-cancer agent, represents an interesting thera-
peutic strategy. Tis new strategy could permit overcoming of the BBB and
to delivery drugs and/or genetic probes into brain tumor cells in a selec-
tive manner. Te future challenges of this approach may be the possibility
to modify the cell genome, and induce it to a reversion into the wild-type
conditions, the enhancing of immune system anti-tumor capacity, and the
targeted drug-delivery into brain tumor cells. Bernardi et al. [185] evalu-
ated the ecacy of immunonanoshells in vitro against medulloblastoma and
malignant glioma cell lines. Te authors, using an antibody against human
epidermal growth factor receptor (HER2) to target gold-silica nanoshells
to medulloblastoma cells, demonstrated cell death in the HER2-over-
expressing medulloblastoma cell lines, after exposure to laser light. In glioma
cell lines, they showed the capacity of these immunonanoshells in causing
leading cell death in U373 and U87 malignant glioma cell lines. Tis mecha-
nism may be very innovative also in the diagnosis of brain tumors. In fact,
nanoparticle targeting methods, iron-oxide nanoparticle-based MRI con-
trast agents, targeted nanoparticle-based MRI contrast agents and intraop-
erative nanoparticle-enabled brain tumor delineation, may produce contrast
enhancement at an earlier stage of gliomas [100]. Another emerging specic
contrast agent is represented by a nanoprobe that targets gliomas which
may express membrane-bound matrix metalloproteinase-2 (MMP-2). Tis
nanoprobe, named chlorotoxin-conjugated superparamagnetic nanoprobe
(PEG-coated nanoparticles), has the capacity to selectively detect neoplas-
tic cells in gliomas, medulloblastoma, prostate cancer, sarcoma, and intes-
tinal cancer [47]. Wang et al. [186] in a recent study have demonstrated,
using a molecular targeting of glioma cells through CD133 antigen over-
expressed on the surface of GBM cells, a prominent photothermal selective
damage of targeted glioma cells. Molecular targeting in this case has been
performed using carbon nanotubes, conjugated with anti-CD133 monoclo-
nal antibodies. Te eciency of liposomal and other nanoplatforms systems
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch06_Bionanoparticles.indd 51 Manila Typesetting Company 08/22/2012 11:45PM
52 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
has been enhanced by various molecular targeting, such as IL-13 expres-
sion, transferring receptor and LDL surface receptor pathways. Glioma cells
show an up-regulation of expression of IL-13 receptor a2 on their surface
cells. In a recent study, the improvement of internalization of doxorubicin-
loaded nanoliposomes, targeted with conjugated IL-13, and cytotoxicity in
U251 glioma cells has been shown. In an in vivo animal model the authors
demonstrated the inhibition of the growth of subcutaneously implanted
gliomas [187]. In anticancer gene therapy, the eciency of liposomes has
been increased through surface ligand targeting, via monoclonal antibodies
to specic receptors up-regulated in glioma cells surface such as transfer-
ring receptors, LDL receptors, IL-13 receptors. A biopolymeric gene deliv-
ery nanoparticle has recently been shown to be eective in vivo in delaying
tumor growth. Tis polymeric nanoparticle-based non-viral gene delivery
vector is cationic albumin-conjugated pegylated nanoparticle, in which is
incorporated a plasmid encoding proapoptotic Apo2 ligand/tumor necrosis
factor-related apoptosis-inducing ligand (Apo2L/TRAIL). After intrave-
nous injection of plasmid-loaded nanoparticles, and subsequent accumu-
lation in a C6 murine glioma model, incorporation of plasmid DNA into
the host cell genome and inhibition of tumor growth, lead to a prolonged
survival in mice bearing implanted C6 gliomas [188]. An alternative thera-
peutic strategy is the photodynamic therapy (PDT) with targeted delivery
systems. PDT involves the intratumoral release of photosensitizers com-
bined with local excitation by an appropriate wavelength of light, resulting
in the production of oxygen and other reactive oxygen species which initiate
apoptosis and cytotoxicity and microvascular injury, within treated neoplas-
tic tissues. Te recent molecularly-targeting approach leads to the selective
detection of cancer cells, through molecular recognition processes, such as
ligand-receptor or antibody-antigen interaction. PDT is an interesting ap-
proach for the treatment of cerebral gliomas, resulting in a very selective
loco-regional therapeutic approach with an important improvement in lo-
cal control of tumors and a signicantly improved survival [44]. A recent
in vitro and in vivo study has shown the ecacy of indomethacin-loaded
nanocapsules in signicantly reducing the tumor size of implanted glioma
in rats. Moreover pathological analysis demonstrated the lack of some im-
portant malignant characteristics typical of GBM, such as mitotic index and
microvascular proliferation [189].
Gold nanostructures demonstrate great potential in imaging in diagnos-
tics serving as molecular contrast agents. Because of high extinction coef-
cient gold nanoparticles can be utilized as contrast agents for dark eld,
light scattering, and two-photon luminescence imaging. Moreover, gold
nanomaterials were used for signal amplication in photoacoustic tomogra-
phy (PAT). PAT is an advanced diagnostic hybrid technique based on laser-
induced thermoelastic expansion through biological tissue which allows
combining benets of optical and ultrasound imaging [190]. PAT allowed
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch06_Bionanoparticles.indd 52 Manila Typesetting Company 08/22/2012 11:45PM
Nzwornrcrwr Avvrrczrrows rw Bnzrw Tuons 53
non-invasive in vivo molecular imaging of living small animal brain vascular
system [190] and, even more, imaging of important hallmarks of a tumor
development and progression such as angiogenesis [191] and hypoxia [192].
Wang and coworkers applied PEGylated gold nanoshells as exogenous NIR
contrast agent for laserinduced PAT of the rat brain in vivo with high spatial
resolution and satisfactory sensitivity [194].
Nanotechnology non-viral gene delivery systems, such as carbon nano-
tubes, represent an interesting therapeutic choice. Tese systems carry short
interfering RNA (siRNA) molecules that exert RNA interference on target
gene expression after their internalization into the target tumor cells and
release. Zhang et al. [151] with in vitro studies, used siRNA that speci-
cally targeted murine telomerase reverse transcriptase and showed that de-
livery of siRNA via carbon nanotubes into tumor cells, silenced the target
gene, inhibited the proliferation of cancer cells in vitro and suppressed tu-
mor growth in mouse models. Higher therapeutic index per nanoparticle
systems application in brain tumor treatment will need better engineering
for higher loading and better controlled releasing of the drug into a tumor
site, and an improvement in the development of most functional drugs. A
new interesting and promising strategy to reach a localized drug delivery to
tumor tissue is magnetizing targeting. Tis approach has the advantage that
the accumulation and retention of drug-loaded magnetic NPs in cancer cells
can be enhanced, by the attraction of NPs to the tumor location using an ex-
ternally applied magnetic eld [194]. Schneider et al. [195] have examined a
double-punched approach to overcome the escape of glioblastoma cells to
immune surveillance, through an active specic immunization (ASI) with
Newcastle-Disease-Virus infected tumor cells, and blocked the TGF-b pro-
duction by delivery of TGF-b AONs using polybutyl cyanoacrylate NPs.
Tis approach induced a signicant decrease in plasma TGF-b2 level, as
well as an increase in rate of high anity IL-2 receptor (CD25) on lym-
phocytes and consequently of antitumoral cytotoxicity. By using anti-FAK
phosphotothioate AONs packaging into liposomes in U251 MG cells, the
down-regulation of expression levels of FAK and the activation of apopto-
sis, through increase in caspase-3 activity, a key-mediator of apoptosis in
mammalian cells, has been shown [196]. Paclitaxel (PTX), one of the most
successful anticancer drugs, is the rst of a new class of microtubule stabi-
lizing agents and has demonstrable antitumor activity in glioma cell lines.
However, because of the poor aqueous solubility and low therapeutic index
of PTX, the clinical application is extremely limited. Furthermore, it is re-
ported that the activity of PTX against brain tumors has been disappointing
in a phase II study, because of drug-resistance and poor penetration across
the BBB [197]. A recent study demonstrated that drug-loaded MPEGylated
poly(-caprolactone) (PCL) long-circulating nanoparticles provided a sus-
tained release of the embedded drug, and higher, or at least comparable in
vitro cytotoxicity to that of Taxol injection against C6 glioblastoma cells
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch06_Bionanoparticles.indd 53 Manila Typesetting Company 08/22/2012 11:45PM
54 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
[198]. It has been demonstrated that Angiopep-2 modied drug delivery
system could enhance delivery of a gene drug and a near infrared uorescent
probe across the BBB [166]. Te potential therapeutic eect of Angiopep-
conjugated PEGePCL nanoparticles, loaded with PTX as a dual-targeting
drug delivery system in the treatment of glioma, was evaluated in a recent
study. Poly(ethyleneglycol)-co-poly(e-caprolactone) (PEGePCL) nanopar-
ticles were conjugated to Angiopep for enhanced delivery across the BBB as
well as for targeting the tumor via LRP-mediated endocytosis. Angiopep-
conjugated PEG e PCL nanoparticles were internalized by U87 MG glioma
cells, and displayed higher cell uptake and stronger inhibition and apopto-
sis toward glioma cells due to LRP-mediated endocytosis. As well as this,
the angiopep-conjugated PEGePCL nanoparticles construct increases the
transport of the nanoparticles across the BBB, and target the brain glioma
by the in vitro co-culture model and in vivo imaging of brain uorescence
[199]. In an ongoing phase I clinical trial, paclitaxel albumin-stabilized NP
formulation is being used in treating advanced cancers such as bladder can-
cer, brain and CNS tumors. Te authors demonstrated, in a subset of pa-
tients, a decrease in tumor vascular permeability [200]. Majoros et al. [178]
evaluated a multifunctional dendrimer conjugated with uorescein iso-
thiocyanate (for imaging studies), folic acid (for targeting cancer cells over-
expressing folate receptors), and paclitaxel (chemotherapeutic drug). Te
authors demonstrated in vitro, that drug-free dendrimer conjugates were
not cytotoxic, and that drug-loaded dendrimer conjugates had no eect on
folate receptor-negative cells. It is known that NPs may trigger an inamma-
tory process, resulting in the release of dierent proinammatory cytokines,
chemokines, reactive oxygen species, and transcription factors that could
explain some known side eects. Tese mechanisms may involve microglia
and interact in dierent ways with normal brain tissue and glioma cells. All
these aspects are very crucial, in modulating an eective strategy of molec-
ular therapeutic approach, trying to hit an important molecular pathway,
such as neovascularization, invasiveness and interaction between tumor and
perilesional tissue. Te more recent experimental studies on the molecular
approach in glioma treatment, have been performed hypothesizing a single
molecular target. Tis strategy has shown poor results as demonstrated by
the actual pharmacological and molecular multimodal strategy of treatment.
Te authors think, that using the intrinsic capacity of NPs should be very
interesting in attempting to structure a new nanoparticle-based molecular
approach against two or more molecular targets, contemporaneously. In a
laboratory approach, the authors are trying to create an engineerized carrier,
loaded with an antisense molecule against hypoxic ischemic factor-1 a and
IL-8. HIF-1a appears to be a highly involved factor in the development
of a characteristic tumour phenotype inuencing growth rate, invasiveness
and metastasis. HIF-1a actively regulates downstream processes, and is
also itself inuenced by the tumor microenviroment in many dierent ways.
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch06_Bionanoparticles.indd 54 Manila Typesetting Company 08/22/2012 11:45PM
Nzwornrcrwr Avvrrczrrows rw Bnzrw Tuons 55
As a result, local hypoxia, due to increased proliferation or insucient oxy-
gen supply, inactivation of tumor suppressors, oncogenes and growth fac-
tors, along with other cell types, such as macrophages, contribute to form
a tumor microenviroment capable of modulating the HIF response itself.
Antisense inhibition of HIF may be a strong target for anti-angiogenic ther-
apy. Te authors study group has recently shown high expression levels of
PGES-1 (Prostaglandine E 1 Sinthase) and IL-8 in high grade glioma cells
and microglial cells, strongly correlate with the grading of a tumor [31, 201].
During progression gliomagenesis, leukocyte inltration and necrosis are
two biological phenomena associated with the development of neovascu-
larization. In malignant gliomas, IL-8 further localizes in oxygen-deprived
cells surrounding necrosis. Macrophages are known to produce high lev-
els of IL-8, which has a tumorigenic activity, by inducing tumour growth
and angiogenesis. Tumor pseudopalisading cells secrete HIF which induces
IL-8 secretion. IL-8binding chemokine receptors CXCR1, CXCR2 and
the Duy antigen receptor for chemokines (DARC) were found in all astro-
cytoma grades by reverse transcription/PCR analysis. Tese results support
a model in which IL-8 expression, by induction of inammatory stimuli,
may be an early step in astrocytoma development. It seems that augmented
IL-8 directly and/or indirectly promotes angiogenesis by binding to DARC,
and induces leukocyte inltration and activation by binding to CXCR1 and
CXCR2. Te contemporary actions of IL-8 into glioma angiogenesis and
leukocyte inltration, as well as macrophages, microglial cells, and ECM
components involvement, suggest IL-8 as a future interesting target in brain
tumor treatment.
6.1 Brain tumor drug targeting
As previously reported the limiting factor in brain tumor treatment is the
delivery of therapeutic agents to the brain across the BBB. A restricted num-
ber of liposoluble small molecules cross the BBB by free diusion, while
other molecules must use specic systems to be transported across the BBB.
Te rapid advances in molecular biology have propelled the development of
novel drug delivery systems that take advantage of a better understanding
of the BBB.
6.1.1 Systemic approaches
An intravenous route is the commonly practiced method for administration
of larger doses of drugs into the body. It delivers drugs directly into gen-
eral circulation by avoiding its rst-pass metabolism, and has potential to
transport drugs to the brain [202]. Te delivered drug can access the brain
by crossing the vascular barrier. However, there is little accumulation of the
drug in the brain because of the BBB and rapid clearance of the extracellular
uid. In addition, the brain availability of the drug is largely aected by the
half life of the drug in the plasma, rapid metabolism, the level of non-specic
binding to plasma proteins, and the permeability of the compound across
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch06_Bionanoparticles.indd 55 Manila Typesetting Company 08/22/2012 11:45PM
56 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
the BBB and into peripheral tissues. Te outcome of the route was found
to be quite eective in delivery of drugs to the brain when administered
using a suitable carrier system like polymeric depots, liposomes or lipid car-
riers. Several drugs like hexapeptide dalargin, doxorubicin, loperamide, and
tubocurarine have been successfully delivered to the brain, using polysorbate
80-coated nanoparticles intravenously.
Intra-arterial administration allows the drug to access the brain vascu-
lature before it enters peripheral tissue, by avoiding rst pass metabolism.
It is a form of regional delivery to brain tumors, designed to enhance the
intra-tumoral concentrations of a given drug. An eective anticancer eect
was achieved with intra-arterial administration of a p53 (tumor suppressor
gene) containing adenoviral vector in a model of human malignant glioma
[203]. Te basic mechanism behind the bioavailability of the drug in the
brain may be due to movement of the drug in capillaries, then to choroid
plexus epithelium, and nally reaching CSF, or by falling into arterial blood
and then going to CSF through white matter and a perivascular pathway.
A trans-nasal route has been utilized for delivering drugs for systemic
action, by crossing the nasal mucosa. Te respiratory region of the nose is
considered to be the major site for drug absorption into the systemic circu-
lation, where the compounds can be absorbed by transcellular pathways or
paracellular passive absorption, carrier-mediated transport, and absorption
through transcytosis pathways. In the brain, a better targeting action can be
achieved, due to direct movement of the drug from the sub mucosa space
of the nose into the CSF compartment of brain [23]. Te highly permeable
nasal epithelium allows rapid drug absorption to the brain, due to high total
blood ow, porous endothelial membrane, large surface area and avoidance
of rst-pass metabolism. Many agents, active in the CNS, are more eective
when given nasally, and provide the advantage of small dose, self adminis-
tration and avoidance of sterile techniques. Transnasal delivery has some
limitations including damage of the nasal mucosa on frequent use of this
route, rapid clearance from the nasal cavity by mucociliary clearance system,
interference due to nasal congestion, elimination of some quantity of the
drug absorbed systemically via the normal clearance mechanism, and the
possibility of partial degradation or irritation to the nasal mucosa [204].
6.1.2 Physiological approaches
Te brain requires essential substances for metabolism and survival, such as
glucose, insulin, growth hormone, low density lipoprotein, etc. Tese sub-
stances are recognized by specic receptors or transport mechanisms, result-
ing in specic transport into the brain. Terefore, the most eective way of
delivering neuro-active drugs is via transporters or internalizing receptors.
Drugs can be modied to take advantage of native BBB nutrient transport
systems, or by conjugation to ligands that recognize receptors expressed at
the BBB. Receptor and adsorptive mediated transcytosis has provided the
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch06_Bionanoparticles.indd 56 Manila Typesetting Company 08/22/2012 11:45PM
Nzwornrcrwr Avvrrczrrows rw Bnzrw Tuons 57
rationale for the development of vector-based strategies, in which the thera-
peutic agent is delivered as a conjugate with a transport vector.
6.1.2.1 Receptor-mediated transcytosis
Large molecules which are necessary for the normal function of the brain
are delivered to the brain by specic receptors. Tese receptors are highly
expressed on the endothelial cells forming the BBB. In this process, the re-
quired physical characteristics are the endocytosis at the luminal (blood)
side after receptor-ligand binding, the movement through the endothelial
cytoplasm, and the exocytosis of the drug or ligand-attached drug or cargo
at the abluminal (brain) side. Te endosomal/lysosomal systems, can poten-
tially degrade drug molecules, therapeutic protein and peptides and genetic
materials. Te physiologic approach comprises targeting these receptors at
the BBB by specic ligands, modied ligands, and antibodies. Terapeutic
compounds are able to cross the BBB after association/conjugation to these
specic ligands. Receptor-mediated transcytosis has been demonstrated for
transferrin, insulin, insulin-like growth factors (IGF-1 and IGF-2), leptin,
and the low-density lipoprotein receptor-related protein (LRP).
Transferrin receptor (TR) is a transmembrane glycoprotein. Te TR
is also expressed on hepatocytes, erythrocytes, intestinal cells, monocytes,
choroid plexus epithelial cells, neurons, and endothelial cells of the BBB.
Te TR mediates cellular uptake of iron bound to transferrin. Drug tar-
geting to the TR can be achieved by using the endogenous ligand trans-
ferrin, or by using antibodies directed against the TR. Cationic liposomes
coupled with transferrin caused a signicant enhancement of luciferase
gene expression activity in C6 glioma cells, primary hippocampal neurons
and primary cortical neurons [205]. Te binding of the antibody to TR
enables it to penetrate the BBB. Ulbrich et al. [206] studied human seru-
malbumin (HAS) NPs with covalently coupled transferring, or transferrin
receptor monoclonal antibodies (OX26 or R17-217), for brain delivery of
loperamide. Results showed that signicant anti-nociceptive eects were de-
tected with loperamide-loaded HAS NPs with covalently bound transfer-
ring of the OX20 or R17-217 antibodies. In a recent study van Rooy et al.
[207], demonstrated that dierent targeting ligands, R17-217 (against TfR)
showed a signicant enhanced brain uptake of liposomes in vivo. Using the
brain capillary depletion method, the authors determined the uptake of 3H-
labelled liposomes in brain capillaries and found R17-217 liposomes were
10 times higher than un-targeted liposomes, suggesting that the high mo-
lecular weight and high anity for the receptor may have contributed to its
strong brain targeting ability [165].
Te insulin receptor (IR) is a large protein having a molecular weight
of 300 kDa. A novel study reports that a genetically engineered human/
mouse chimeric form of the human insulin receptor monoclonal antibody
(HIRMAb) in an adult Rhesus monkey, has showed that humanized
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch06_Bionanoparticles.indd 57 Manila Typesetting Company 08/22/2012 11:45PM
58 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
HIRMAb was rapidly transported into all parts of the primate brain after
intravenous administration, suggesting its potential for delivering both drug
and gene across the BBB in human [208].
Low-density lipoprotein receptor related proteins 1 and 2 (LRP1 and
LRP2) are multifunctional, multi-ligand scavenger and signaling receptors.
Tey can interact with a diverse range of molecules and mediators, including
ApoE, tissue plasminogen activator (tPA), plasminogen activator inhibitor
1 (PAI-1), lactoferrin, melanotransferrin, a2 macroglobulin (a2 M), recep-
tor associated protein (RAP), HIV-1 TAT protein, Heparin cofactor II,
heat shock protein 96 (HSP-96), and engineered angiopeps. Several drugs
that normally do not cross the BBB, including tubocurarine, loperamide,
dalargin, 8-chloro-4-hydroxy-1-oxol, quinoline-5-oxide choline salt (MRZ
2/576), and doxorubicin show higher concentrations in the brain when as-
sociated with polysorbate 80-coated nanoparticles.
Lactoferrin (Lf ) is a mammalian cationic iron-binding glycoprotein be-
longing to the transferrin family. Lf was reported to be transported into the
brain via LRP mediated transcytosis. Drug-loaded Lf-NPs were taken up
by the brain and produced therapeutic ecacy, as demonstrated by the sig-
nicant attenuation of the striatum lesion [209].
Another group of LRP ligands, known as angiopeps, has also been re-
ported as a highly eective BBB targeting ligand. Angiopeps belong to a
family of peptides derived from the Kunitz domains of aprotinin and other
human proteins. Te most studied is angiopep 2, which has shown greater
transcytosis capacity and parenchymal accumulation. Moreover, their abil-
ity in eciently facilitating nanocarrier transport across the BBB in vivo
has been conrmed with dendrimers, and more recently with amphoteri-
cin B-loaded polymeric micelles [180]. Chemical conjugation of angiopep
2 with 3 molecules of paclitaxel (ANG1005) was shown to be particularly
eective in enhancing drug uptake into the brain using an in situ rat brain
perfusion model.
Recently Tosi et al. [210] developed a poly(D,L-lactide-co-glycolide)
(PLGA) nanoparticles with two surface modied ligands namely a BBB-
penetrating peptide (similopioid peptide, g7) for transporting across the
BBB, and a sialic acid residue (SA) for the interaction with receptors in the
brain tissue to prolong the NP residence time. Te researchers reported a
remarkably high dose in the CNS over a prolonged period of time (24 h).
Tese results were attributed to the ability of SA g7 nanoparticles to cross
the BBB and remain within the brain parenchyma.
6.1.2.2 Adsorptive-mediated transcytosis
During the past decade, several peptides have been described that allow the
intracellular delivery of polar biologically active compounds in vitro and in
vivo. Tese peptides possess multiple positive charges, and some of them
share common features, such as hydrophobicity and helical moment, the
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch06_Bionanoparticles.indd 58 Manila Typesetting Company 08/22/2012 11:45PM
Nzwornrcrwr Avvrrczrrows rw Bnzrw Tuons 59
ability to interact with a lipid membrane and the ability to adopt a signicant
secondary structure upon binding to lipids. Since these peptides penetrate
into cells by a receptor-independent non-endocytotic process, attempts have
been made to demonstrate that the interaction with the lipid matrix of the
plasma membrane could play a key role in peptides cell uptake. Tey have
been successfully used as vectors for the delivery of drugs that are P-gp sub-
strates, by eectively by-passing the P-gp in the BBB. Te application of
CPPs is based on the premise that a biologically active cargo can be attached
to CPPs and translocated into cells. Te link between the CPPs and the
cargo is commonly a covalent bond and seldom a non-covalent bond. A large
variety of cargo molecules/materials have been eectively delivered into cells
via CPPs, including small molecules, proteins, peptides, fragments of DNA,
liposomes and nanoparticles.
SynB vectors are a new family of vectors derived from the antimicrobial
peptide protegrin 1 (PG-1), a 18-amino-acid peptide. Tese linear peptides
are able to interact with the cell surface and cross the plasma membrane with-
out any membrane-disrupting activity. Furthermore, the internalization of
these peptide vectors into cells does not appear to depend on a chiral recep-
tor, since the D-enantio form penetrates as eciently as the parent peptide
(L-form), and retro-inverso sequences exhibit identical penetrating activity.
Tese linear protegrin analogues were the starting point for developing a new
potent strategy for drug delivery into complex biological membranes. Adenot
and colleagues [211] studied brain uptake of a number of free and SynB3
vectorized chemotherapeutic agents using both in situ brain perfusion and
in vitro BBB/cell model. Tey reported that SynB3s conjugation with vari-
ous poorly brain-penetrating drugs enhanced their brain penetration, with
no eect on tight junction integrity. Te transcription factor Tat, involved
in the replication cycle of human immunodeciency virus (HIV), was dem-
onstrated to penetrate into cells [212]. One of the most interesting demon-
strations of the eectiveness of TAT-shuttled nanocarriers across the BBB
was accomplished by TAT-conjugated CdS:Mn/ZnS quantum dots [213].
Histological data showed that TAT-Qdots migrated beyond endothelial cells
and reached the brain parenchyma. Recently, Liu et al. [214] produced com-
pelling evidence that TAT facilitates human brain endothelial cell uptake
of nanoparticles self-assembled from TAT-PEG-b-cholesterol in vitro, and
that the nanoparticles with TAT were able to cross the BBB and translocate
around the cell nucleus of neurons. Biodistribution studies of FITC-loaded
NPs in rabbits and ecacy studies in a C. neoformans meningitis rabbit
model, revealed that these NPs crossed the BBB and produced antimicro-
bial activity against the pathological strains in the brain tissue with a similar
ecacy as amphotericin B, suggesting a therapeutic dose was delivered by
TAT containing nanoparticles. Qin et al. [215] prepared liposomes using
cholesterol-PEG2000-TAT (TAT-LIP) and compared them to liposomes
fabricated from cholesterol-PEG2000 polymer (LLIP) and conventional
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch06_Bionanoparticles.indd 59 Manila Typesetting Company 08/22/2012 11:45PM
60 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
cholesterol formulation (LIP) in vitro and in vivo. Tese data suggested
that adsorptive transcytosis could be one of the mechanisms for TAT-LIP
transport across the BBB, and the positive charge of the TAT-LIP played
an important role in enhancing this transport. AMT enables many poorly
brain-penetrating drugs to cross the BBB, and holds potential for promoting
drug delivery into the brain. However, because it is a non-specic process, the
adsorptive process also occurs in the blood vessels and in other organs. Tis
poses a challenge for both achieving therapeutic concentration in the brain
and limiting the drug distribution in non-target organs.
6.1.2.3 Eux pump inhibition
Passive diusion of substances across the BBB may depend on their lipo-
philicity and molecular weight. However, a large number of compounds are
rapidly euxed from the brain into the blood by extremely eective eux
pumps expressed in the BBB. Tese eux systems include Pglycoprotein
(Pgp) and multidrug resistance proteins (MRPs). Tere exists also, an enzy-
matic barrier to drug transport in the BBB. Specically, the activity of many
enzymes that participate in the metabolism and inactivation of endogenous
compounds, such as g-glutamyl transpeptidase, alkaline phosphatase, and
aromatic acid decarboxylase is elevated in cerebral microvessels. To circum-
vent this obstacle, it is possible to administer the drug with a pharmaco-
logical modulator, which inhibits eux transport systems in brain capillary
endothelial cells. One promising example of such pharmacological modula-
tors is represented by a class of Pluronic block copolymers. Tese block
copolymers consist of hydrophilic ethylene oxide (EO), and hydrophobic
propylene oxide (PO) blocks arranged in a basic A-B-A tri-block structure
EOn/2-POm-EOn/2. Te block copolymers with various numbers of hy-
drophilic EO (n) and hydrophobic PO (m) units, are characterized by a
distinct hydrophilic-lipophilic balance (HLB). Due to their amphiphilic
character these copolymers display surfactant properties including the ability
to interact with hydrophobic surfaces and biological membranes. Extensive
studies have conrmed that Pluronic P85, a Pluronic block copolymer,
can be used not only as an eective eux pump inhibitor, but also as a drug
delivery vehicle [216]. Studies in multidrug resistant cancer cells, polarized
intestinal epithelial cells, Caco-2, and polarized BBB monolayers provided
compelling evidence that selected Pluronic block copolymers can inhibit
drug eux transport systems [217]. Te most studied Pluronic P85
showed the ability to enhance the BBB permeability for a wide range of
drugs, including doxorubicin, etoposide, taxol, 3-azido-3-deoxythymidine,
valproic acid, and loperamide in the bovine brain microvessel. Evidence sug-
gests that the inhibition mechanisms of Pluronic block copolymers on
P-gp activity in the BBB involve three eects, namely copolymer interaction
with the cell membrane, inhibition of P-gp ATPase activity, and depletion
of cellular ATP [216].
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch06_Bionanoparticles.indd 60 Manila Typesetting Company 08/22/2012 11:45PM
Nzwornrcrwr Avvrrczrrows rw Bnzrw Tuons 61
6.1.2.4 Cell-mediated drug transport
Cell-mediated drug transport employs specic cells that take up drug-
loaded nano or microcarriers, trac them through the BBB, and deliver the
drugs to their target sites. Generally speaking during the process of brain
inammation (Parkinsons disease, stroke, brain tumours, HIV) extensive
recruitment of leukocytes in the brain can be demonstrated. Mononuclear
phagocytes and T cells migrate towards the site of the inammation, involv-
ing the processes known as diapedesis and chemotaxis. Tese cells show the
tendency to endocytose colloidal materials (microparticles, liposomes, mi-
crocarriers) and successively, for exocytosis to release these compounds. In a
recent study, Jain et al. [25] used RGD-anchored magnetic liposomes as the
targeting ligand for integrin receptors expressed on neutrophils and mono-
cytes, to facilitate cell uptake of liposomes containing the anti-inammatory
drug diclofenac. Te uptake of drug/liposomes by cells was improved with
RGD modication, increasing to about 16%. Te most striking result is
that by the incorporation of magnetic particles and with the application of
a magnetic eld, the percentage drug dose that reached the brain was ele-
vated from 3.25% to 21.53% for RGD-modied magnetic liposomes. If this
targeting eect can be translated into drug ecacy without toxicity, then
this combined strategy will revolutionize the treatment of all CNS diseases
which have an inammatory component. Te potential level of toxicity, aris-
ing from repeated dosing of magnetic materials, must be addressed before
this approach can be developed into a clinical treatment. Qin et al. [218]
have reported a similar RGD-liposome approach for the delivery of ferulic
acid to monocytes/neutrophils in the brain using an inammatory animal
model. Te results showed that drug-loaded RGD-liposomes reached the
brain at a level 6-fold higher than that of the drug solution, and 3-folds
higher than that of the drug-loaded plain liposomes. Panyam et al. [219]
showed that the dynamics of endocytosis and exocytosis of PLGA nano-
particles in cells can be inuenced by concentration, time and energy. Tis
suggests that by surface modication of the nanocarrier, their uptake into
and release from cells can be modulated. As previously shown, the combined
strategy of magnetic liposomes and monocytes targeting ligands can maxi-
mise the monocytes recruitment at the brain, and may prove to be a very
eective approach for drug delivery to the diseased brain which has an in-
ammation component [25]. However, the safety of this route has yet to be
fully assessed. It is unknown whether its combination with the use of mag-
netic particles may lead to any iron toxicity in long term use. Furthermore,
the selectivity and maximum capacity of this strategy for delivery of drugs
across the BBB warrants further study.
6.1.3 Direct CNS approaches
In this strategy the drug substances are directly delivered to CNS by the use
of chemical substance, or by the application of energy like ultrasonic waves
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch06_Bionanoparticles.indd 61 Manila Typesetting Company 08/22/2012 11:45PM
62 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
or electromagnetic radiations, which helps in the opening of tight junc-
tions. Because the tight junctions act as a tightly bound wall, one method
for the penetration of the BBB is by disruption. Te disruption of the BBB
must be transient and reversible in order to have any role in the delivery of
therapeutic molecules. Disruption of the BBB can be achieved by infusion
of hypertonic solutions [23]. Hypertonic solutions cause opening of tight
junctions due to higher osmotic pressure, which leads to a shrinking of
endothelial cells, by which disarrangement of extracellular proteins occurs,
and nally entry of the drug which takes place paracellularly [23]. Various
osmotic substances have already been tested, and amongst these mannitol
has been found to be eective and safe. Mannitol has been used for several
years for treating brain tumors, where the barrier is opened for 30 min
when a 25% solution of the drug is allowed for 30s [220]. Lysophosphatidic
acid increases TJ permeability in cultured brain endothelial cells via the
activation of PKC-alpha channels, which reduces caudin-5 expression
and F-actin recombination [221]. Tese substances show a rapid, dose-
dependent and reversible action, where the eect can be attenuated by
activation of protein kinase C. Cyclodextrins (CDs) are cyclic oligosac-
charides composed glucose units, namely a-, b-, g-CD. Monnaert and col-
leagues [222] studied the endothelial permeability and toxicity of native,
methylated, and hydroxypropylated a-, b-, g-CD in an in vitro cell model.
Native a-, b-CD elicited a rapid increase in sucrose permeability of ce-
rebral endothelial cell monolayers, which correlated with their ability to
extract phospholipids [222]. High concentrations of hydroxypropyl g-CD
and g-CD increased doxorubicin passage through the brain endothelial cell
monolayers, but at the expense of a loss of the BBB integrity and decreased
junctional staining of occludin. Tis nding suggests that oligosaccharide
units are likely to be responsible for the toxicity of CDs in the brain, because
of their extraction of lipophilic components of the BBB, phospholipids and
cholesterol, which may break down the brain endothelial cell monolayers
[223]. Biologically active vasoactive agents such as bradykinin, angiotensin
peptides, leukotrienes, histamine and VEGF are also capable, under some
circumstances, of disrupting the BBB, suggesting that they may play a role
in modulating the BBB permeability. Bradykinin is a plasma kinin pro-
duced from a plasma globulin kininogen by the action of specic enzyme
kalikreins. Tis is found to permeate the BBB by action on B2 receptors
expressed on the endothelium of luminal membrane. It can modulate in-
tercellular tight junctions by elevating the calcium level of the membrane
which activates actin/myosin bres leading to leaching out of junctional
proteins and loosening of the tight junction. In the case of brain gliomas,
microvascular permeability in tumour tissue is more sensitive to the ef-
fects of these biological compounds than the normal brain endothelia cells.
Terefore, these stimuli when used in combination with imaging materials,
gene or anticancer drugs, can potentially boost the preferential delivery of
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch06_Bionanoparticles.indd 62 Manila Typesetting Company 08/22/2012 11:45PM
Nzwornrcrwr Avvrrczrrows rw Bnzrw Tuons 63
these materials to the brain tumour to achieve tumour diagnosis, tumour
gene therapy or chemotherapeutic treatment. Cereport, a synthetic pep-
tide analogue of bradykinin, increases the permeability of the BBB by tran-
siently disrupting the TJ and shows specic time, dose and size dependent
actions on human brain microvascular endothelial cells [224]. Studies have
shown that Cereport is capable of enhancing the BBB transport of a num-
ber of drugs, including carboplatin, loperamide, and acyclovir in dierent
types of diseased animal models [225]. Because Cereport has no toxicity
by itself, it can selectively increase drug uptake in the brain tumour and
shows less eect in a non-permeable normal brain. When attached to the
surface of a liposome, Cereport is even more eective in facilitating Evans
blue transport into the brain compared to free Cereport with liposome
[226]. Tis study also demonstrated that Cereport attached liposomes can
be potentially used for transporting dierent types of drugs, including P-gp
substrates, via transient TJ opening.
Several modulators with the capacity to temporarily open a TJ to en-
hance the transport of drugs and traces have been evaluated. 45 kDa bio-
logical molecule zonula occludens toxin (Zot), an active TJ modulator at the
BBB, can induce a reversible, concentration-dependent TJ opening, which
increases the paracellular transport of sucrose and inulin (permeability
markers) without detectable short-term toxicity, in cultured bovine brain
capillary endothelia cells [227]. In addition, it also permits an enhanced
transport of the therapeutic agents doxorubicin and paclitaxel that would
normally have very low transportation across the BBB.
Viruses can also act as stimuli and open the TJ via upregulation of
chemokines as a precursor for inltration of inammatory cells into
the CNS. Immunohistochemical analysis of CNS tissue, from HIV-1-
seronegative and HIV-1-infected patients revealed signicant tight junction
disruption in patients who died with HIV encephalitis, as shown by frag-
mentation or absence of immunoreactivity for occluding and ZO-1 [228].
Tese phenomena were associated with accumulation of activated HIV-1-
infected brain macrophages, brinogen leakage, and marked astrocytosis,
suggesting that the main route of HIV-1-infected monocyte entry into the
CNS could be the disrupted BBB structure.
Te capacity of energy-based physical methods, such as ultrasound,
microwave or electromagnetic elds, to open the BBB has been also inves-
tigated. Te important advantage of this approach is its specicity for tar-
geting to a specic area of brain. Focused ultrasound techniques concentrate
acoustic energy in a focal spot deep in the body with minimal eect to tis-
sues outside the eld of focus. Tis allows it to non-invasively induce local
biological eects deep inside the body. Hynynen et al. [229] showed that
the introduction of a preformed gas bubble before focused ultrasound expo-
sure would allow transient opening of the BBB locally without causing acute
damage to the neurons. Te gas bubble not only connes the ultrasound
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch06_Bionanoparticles.indd 63 Manila Typesetting Company 08/22/2012 11:45PM
64 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
eect to the vasculature, but also reduces the power needed to open the
BBB, making it possible for the ultrasound to be applied through the intact
skull. Te possible explanations are the temperature of ultrasonic waves that
induces thermal lesions leading to alteration of permeability and general-
ized opening of BBB [230], or the cavitation eect produced by the injected
uid that leads to formation of small air lled cavity in barriers luminal
membrane, making the entry of drugs easier into the brain and the pos-
sible formation of micro-bubbles by the ultrasound contrast agent. With
the passage of time, these bubbles increase in size and nally burst leading
to the opening of barrier tight junctions without damaging the tissues. In
combination with an imaging device such as MRI, ultrasound becomes a
non-invasive approach to open targeted regions of the BBB, to permit the
delivery of drugs and other therapeutic molecules across the BBB. Tis
method is now used mostly as diagnostic tool using a contrast agent for
imaging the brain microenvironment as well as tumors. Sheikov et al. [231]
studied the eect of focused ultrasound in a rabbit model and revealed that
at the acoustic power applied (0.55W and 3W), TJ opening occurred with
leakage of dye and contrast matter. Evidence suggests that the reversible dis-
ruption of the BBB, by bursts of low frequency MRI-guided ultrasound, en-
hances the brain delivery of monoclonal antibody-Herceptin (trastuzumab)
in mice and doxorubicin in rats [232]. It was suggested that the mechanisms
for transport of molecules by focused ultrasound may involve transcytosis,
transendothelial openings-fenestration and channel formation, widening of
interendothelial clefts, and opening of TJs and passage through the injured
endothelium [231].
In addition several other approaches have been tested for disruption of
the junctional barrier including simian immunodeciency viruses (SIV)
and BBB permeation enhancers. Studies have shown that the viruses were
able to disrupt the barrier, due to changes in the expression of the tight
junctional protein zo-1 (decreased synthesis) on endothelial cells of cere-
bral capillaries in some trials [233]. Additionally, permeation enhancers
have also been found to increase the drug permeability across the BBB.
Permeation enhancers are the chemical substances belonging to the family
of surfactants. Primary alcohols have the property of increasing BBB uptake
due to transient opening by these chemicals. Te various examples of these
agents are ethanol, surfactants like sodium dodecyl sulfate (SDS), glycerol
and polysorbate-80 (Tween-80), polyethylene glycol hydroxy stearate, etc.
Tese agents act by destabilizing the membrane, leading to BBB disruption
and entry of drug into brain. However, disruption of BBB even for brief
periods may expose the brain to infection and damage from toxins. Also,
the more serious disadvantage of this method is the astrogliatic reactions
(astrogliosis) produced by leakage of plasma proteins like albumin from the
blood (albumin is toxic to astrocytes).
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch06_Bionanoparticles.indd 64 Manila Typesetting Company 08/22/2012 11:45PM
Nzwornrcrwr Avvrrczrrows rw Bnzrw Tuons 65
6.1.3.1 Intracerebral routes
Intracerebral delivery involves delivery of the drug directly into the brain
parenchyma. Drugs can be injected directly via intrathecal catheters, by con-
trolled release matrices, microencapsulated chemicals or recombinant cells.
Tese strategies are, however, highly invasive and disadvantages such as infec-
tion, catheter obstruction and discomfort for the patient have been reported.
Tese invasive strategies rely on the diusion of therapeutic molecules, but
this mechanism is very limited in the cerebral parenchyma. Intraventricular
drug infusion involves placing a catheter into the cerebrospinal uid of the
ventricles, and relies on drug diusion from local depot sites to the brain
parenchyma. Te major problem with bolus injection is slower movement of
compounds within the brain due to the limited diusion coecient. Hence
a large amount of dose is required for an appropriate drug concentration in
the parenchyma. However, diusion is a poor mode of drug delivery to the
brain, and the limited volume of distribution of therapeutic drugs into the
brain limits the value. Because the cerebrospinal uid is completely absorbed
into the venous circulation, the infused drug into ventricular spaces is rap-
idly transported to the peripheral blood circulation, with minimal penetra-
tion into the brain parenchyma. A similar approach has been used for the
intraventricular or intracerebral injection of genetically engineered cells that
secrete a specic protein factor, or the injection of biodegradable polymer
that releases the therapeutic substance. Te Ommaya reservoir, a catheter
with a pump system, can deliver intermittent bolus injections of antican-
cer drugs directly into the CSF. Similarly vapour pressure activated devices
like the Ommaya reservoir pump (Vygon Neuro, Norristown, USA)
(a dome-shaped device, with a catheter attached to the underside used to
deliver chemotherapy) containing etoposide, an antitumor agent used for
treating metastatic brain tumor showed 100-fold more eective concentra-
tion. Local and site-specic delivery of chemotherapeutic agents increases
drug concentration at the tumor target, decreases systemic exposure and
toxicities, and increases the duration of exposure of the tumor to the drug.
Experimental and clinical studies have demonstrated a statistically sig-
nicant increase in survival associated with local therapy for brain tumors
[234]. Te intrathecal route involves delivery of neurotherapeutic agents to
the brain by direct administration of drugs through the intrathecal route
into the cisterna magna of the brain. Tough it is substantially less invasive
than intraventricular administration, this method fails to result in drug ac-
cumulation in parenchymal structures of the deep brain, which is highly
essential for sustained drug release. Te major disadvantage of this route is
the chance of the drug spreading along the distal space of the spinal canal,
which was understood when etoposide administered through this route into
dogs led to ataxia and loss of muscle coordination. Te general principle
of convection-enhanced delivery (CED) involves the stereotactically guided
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch06_Bionanoparticles.indd 65 Manila Typesetting Company 08/22/2012 11:45PM
66 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
insertion of a small-caliber catheter into the brain parenchyma. Trough
this catheter, the drug is actively pumped into the brain parenchyma and
penetrates into the interstitial space. Because infusion is delivered directly
into the brain parenchyma via a cannula, the BBB is bypassed and specic
regions can be targeted for treatment [235]. Tis method has demonstrated
in laboratory experiments to deliver high molecular weight proteins 2 cm
from the injection site in the brain parenchyma [236]. Te success of CED
relies on precise placement of the catheters and other infusion parameters
for delivery into the correct location in the brain parenchyma.
Implants are made up of biodegradable/non-biodegradable polymeric
materials encapsulating drugs inside them. Te basic mechanism behind
drug release from these devices is diusion. Tese implants are placed inside
the brain surgically, where they release the drug for a predetermined level
of time. Polymer depots have been used for the delivery of drugs into the
cerebral environment in the tumor cavity of the brain, with the drug being
present inside the polymer matrix as a core material. It oers sustained re-
lease of drugs by the biodegradation of polymer. Similarly Gliadel wafer
(MGI Pharma, Bloomington, USA), a polymer depot containing carmus-
tine showed its release over a period of 5 days when placed in the tumor
resection cavity [237]. Tis system was composed of a lipophilic anticancer
agent, carmustine, incorporated into a poly(carboxypropane)-sebacic acid
(PCPP-SA) belonging to the series of polyanhydrides. Te therapeutic eect
of the Gliadels wafer was tested in two phase III clinical trials [238239].
Te median survival time obtained with treated patients was signicantly
prolonged in comparison with untreated patients (2-month increase).
However, with the application of this system, infections and cerebral edemas
due to the high concentration of carmustine and obstructive hydrocephalus
resulting from the dislodgment of the wafer, were also demonstrated.
6.1.4 Drug modications and prodrugs
Physicochemical properties of drugs, such as lipophilicity, lack of ionization
at physiological pH, and molecular weight, determine the extent to which
drugs can cross the BBB. Various attempts have been made to overcome the
limited access of drugs to the brain by chemical modication of the drug.
One strategy for modication of the drug is lipidization, which involves the
addition of lipid-like molecules through modication of the hydrophilic
moieties on the drug structure. Lipid-soluble molecules are believed to be
transported through the barrier, by accessing small pores that form tran-
siently within the lipid bilayer. Te addition of hydrophobic groups to a
molecule may enhance its brain transfer by passive diusion. Consecutive
addition of methyl groups, in a series of barbiturates, increased lipophilic-
ity and brain penetration in animals. Tis strategy has been frequently em-
ployed, but the results have often been disappointing. Te best examples of
such attempts are the series of lipophilic analogues of nitrosoureas, where
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch06_Bionanoparticles.indd 66 Manila Typesetting Company 08/22/2012 11:45PM
Nzwornrcrwr Avvrrczrrows rw Bnzrw Tuons 67
a quantitative structural activity relationship (QSAR) study indicated that
the anti-neoplastic activity was inversely proportional to the lipophilic-
ity. Tis is because the more lipophilic analogs become less soluble in the
aqueous plasma and bind more readily to plasma proteins, leading to lower
concentrations of the drug available for diusion into the CNS, and dem-
onstrate diminished alkylating activity and increased dose limiting toxicity.
Hence, when a drug is delivered via the circulatory system for the treatment
of CNS diseases, a delicate balance between cerebro-vascular permeability
and plasma solubility is required.
Te chemical delivery systems (CDS) require multiple chemical or enzy-
matic transformations prior to release of the active drug. Te CDS are based
on a dihydropyridone-quaternary pyridinium ion redox system, which relies
on chemistry analogous to the ubiquitous NAD1-NADH coenzyme sys-
tem. Te drug is converted into a 1,4-dihydropyridine moiety-containing
conjugate which is the CDS. Upon systemic administration in animals,
there is extensive tissue distribution with the conjugate accessing most of
the compartments, including the brain. Te unstable dihydropyridine deriv-
ative is oxidized to form the hydrophilic polar quaternary pyridinium salt,
which is eliminated from most tissues but retained in the brain as a result
of the BBB, thus locking in this ionized moiety. Subsequently, the carrier is
cleaved to provide the free active drug. A further approach for the delivery
of small molecules into the brain is to modify the drug so that mimics a
nutrient, thus giving it access to one of several specialized carrier-mediated
transport systems within the BBB. Essential compounds, such as amino ac-
ids, hexoses, vitamins and neuropeptides, normally need specic carriers to
permeate into the brain. Dopamine is not transported eciently through
the BBB. Modication of dopamine to its neutral amino-acid precursor,
L-dopa, enhances brain uptake because of its anity for the neutral amino-
acid transporter within the barrier.
Prodrugs are pharmacologically inactive compounds that result from
transient chemical modications of biologically active species. Te chemi-
cal change is usually designed to improve some decient physicochemical
property, such as membrane permeability or water solubility. After adminis-
tration, the prodrug is brought closer to the receptor site and is maintained
there for longer periods of time. Here it is converted to the active form,
usually via a single activating step. Once in the CNS, hydrolysis of the modi-
fying group will release the active compound. Going to extremes on the li-
pophilic precursor scale, a possible choice for CNS prodrugs is coupling the
drug to a lipid moiety, such as fatty acid, glyceride or phospholipids. While
increased lipophilicity may improve movement across the BBB, it also tends
to increase uptake into other tissues, causing an increased tissue burden.
Tis selectivity in delivery is especially detrimental when potent drugs such
as steroids or cytotoxic agents are considered, since toxicity is exacerbated at
nontarget sites. Moreover, while increased lipophilicity may facilitate drug
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch06_Bionanoparticles.indd 67 Manila Typesetting Company 08/22/2012 11:45PM
68 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
uptake into the CNS, it also enhances eux processes. Tis can result in
poor tissue retention and short biological action.
A prodrug lock-in mechanism for drug targeting is characterized by the
attachment of four dierent additional functions to active moiety like an ad-
juster (A), a bulkier lipophillic moiety (L), spacer (S) and a targetor (T) for
locking them into the brain. Te drug is packed by the covalently attached
lipophilic group (L) to enhance lipid solubility and to disguise the nature
of the molecule through an ester bond, or sometimes through a C-terminal
adjuster (A) at the carboxyl terminal and targetor (T) that undergoes
enzymatic oxidation and turns to an ionic, membrane-impermeable moi-
ety (T+). Te membrane impermeable conjugates locked into the brain
undergo sequential metabolism and yield the drug in the CNS. A spacer
(S) consisting of strategically used amino acids is provided to ensure timely
removal of the charged targeter [240]. Several drugs are also being tried for
prodrug mediated drug delivery and include zidovudine, ganciclovir, lomus-
tine, benzylpenicillin, estradiol, enkephalin, TRH, and kyotorphin.
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch06_Bionanoparticles.indd 68 Manila Typesetting Company 08/22/2012 11:45PM
7. Experimental studies
Nanoparticle systems, can represent ideal devices for delivery of specic com-
pounds to brain tumors across the BBB [45, 241242]. Nanotechnology
and nanomedicine have been utilized to perform new therapeutic intracere-
bral drug delivery systems, and to develop treatments for various diseases
and disorders. By using nanotechnology in drug design and delivery, it will
be possible to deliver the drug to the targeted tissue and cells across the
BBB, to release the drug at the controlled rate, and to be able to escape from
degradation processes. Solid tumors require therapies to actively penetrate
deeply into the tumor in order to aect a large proportion of cancer cells.
Nanotechnology provides a unique advantage in glioma therapy since the
size scale is on the order of the proteins used for cell function. Te size
and shape of NPs can be tuned to exert a desired therapeutic response on a
specic target.
Antiangiogenic approaches have been extensively exploited to provide
a rationally designed therapy for the treatment of malignant gliomas. Te
brain tumor endothelium, with characteristics of high proliferation, high
permeability, and high expression of proangiogenic factors, is a particularly
appealing therapeutic target for this strategy [243245]. Antiangiogenic
approaches in glioma therapy have been strongly directed against a VEGF
pathway. In an in vivo murine model, created by implantation of U-87 MG
malignant glioma cells in mice, Im et al. [246] demonstrated the suppression
of ability of glioma cells to form tumors in mice. Tis result was obtained
after transfection of antisense VEGF cDNA, in an antisense orienta-
tion through the recombinant adenoviral vector Ad5CMV-alphaVEGF.
Infection of U-87 MG malignant glioma cells resulted in the reduction
of the level of the endogenous VEGF mRNA, and in reduced production
of the VEGF targeted secretory form. Agemy et al. [247] have proposed a
multifunctional theranostic NP in which the CGKRK peptide provides the
targeting function that takes the NPs to tumor vascular cells and into their
mitochondria. Te NP uses the mitochondria-targeted
D
[KLAKLAK]
2
peptide as the drug and iron oxide, as a diagnostic component for MRI.
In addition, the NP was combined with the tumor-penetrating peptide
iRGD which enhances the NP penetration into the extravascular tumor
tissue. Systemic treatment of GBM-bearing mice with this compound
eradicated most tumors in one GBM mouse model, and signicantly de-
layed tumor development in another. An important molecular target used
to selectively detect glioma cells is IL-13, based on up-regulated expression
of IL-13a2 on the surface of GBM cells. In a recent study, Madhankumar
et al. [187] showed the improvement of internalization of doxorubicin-
loaded nano liposomes targeted with conjugated IL-13, as compared to non-
targeted nano liposomes in U251 glioma cells. In an in vivo animal model,
the authors demonstrated growth inhibition of subcutaneously implanted
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch07_Bionanoparticles.indd 69 Manila Typesetting Company 08/22/2012 11:45PM
70 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
gliomas. Bernardi et al. [185] evaluated the ecacy of immunonanoshells
in vitro against both medulloblastoma and malignant glioma cell lines. In
this study, the authors, using gold-silica nanoshells, coated with an anti-
body against human epidermal growth factor receptor (HER2) to target
medulloblastoma cells, showed cell death in the HER2-overexpressing
medulloblastoma cell lines after exposure to laser light. Te same authors
conjugated gold-silica nanoshells to an antibody specic to interleukin-13
receptor alpha 2 (IL-13Ra2), strongly expressed in gliomas, demonstrating
that these immunonanoshells are capable of leading to cell death in U373
and U87 malignant glioma cell lines. Convection-enhanced delivery (CED)
techniques were developed to address the diusion limited penetration of
agents directly delivered to the brain. Tis strategy has been used to deliver
proteins and small particles, including liposomes and polymeric nanopar-
ticles into the brain. CED provides penetration through a large volume of
brain tissue but it is limited by unpredictable drug distribution and poten-
tially high intracranial pressures. Combining polymeric controlled release
with CED could improve the drug distribution limitations of implantable
wafers while also oering spatiotemporal distribution control that is lacking
from CED. Poly(lactic-co-glycolic acid) (PLGA) is capable of encapsulating
and releasing a variety of agents, including chemotherapy drugs, for long pe-
riods of time. Te authors evaluated the ecacy of CED of surface-modied,
drug-loaded, PLGA NPs to treat intracranial glioma using the topoisomerase
I inhibitor camptothecin (CPT). CPT is an attractive drug for delivery by
controlled release because it has known anticancer activity, but is limited
by low solubility and serious systemic toxicity. Te NPs were shown to be
eective both in culture and in vivo, with a statistically signicant survival
benet observed in all animals treated [248]. CED of iron oxide NPs in a
mouse glioma model results in MRI contrast of the nanoparticles and eec-
tive intratumoral and peritumoral distribution of nanoparticles in the brain.
A signicant therapeutic eect was found after CED of both IONPs and
EGFRvIIIAb-IONPs in mice. Dispersion of the NPs over days, after the
infusion has nished, may potentially target inltrating tumor cells outside
the tumor mass that are potentially responsible for tumor recurrence and
the demise of patients. Use of bioconjugated magnetic NPs may permit the
advancement of CED in the treatment of malignant gliomas due to their
sensitive imaging qualities on standard T2 weighted MRI and therapeutic
eects [249]. Cyclo-oxygenase (COX)-2 is the key enzyme in arachidonic
acid metabolism resulting in prostaglandin production, and is induced by
several factors, such as growth factors, cytokines, and tumor promoters. In
particular, COX-2 expression and prostaglandin production are associated
with tumorigenesis and tumor progression. Celecoxib, a selective COX-2 in-
hibitor, has been reported to mediate growth inhibitory eects and to induce
apoptosis in various cancer cell lines. PLGA nanoparticles incorporating
celecoxib were prepared for antitumor drug delivery. PLGA nanoparticles
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch07_Bionanoparticles.indd 70 Manila Typesetting Company 08/22/2012 11:45PM
Exvrnrrwrzr Srunrrs 71
incorporating celecoxib showed the same cytotoxicity against U87MG tu-
mor cells as celecoxib itself. Furthermore, celecoxib did not aect the degree
of migration of U87MG cells. When C6 rat glioma cells were used, PLGA
nanoparticles incorporating celecoxib showed dose-dependent cytotoxicity
similar to that of celecoxib itself. Neither celecoxib nor PLGA nanoparticles
incorporating celecoxib aected COX-2 expression in C6 cells on a Western
blot assay [250]. Curcumin is a polyphenolic compound derived from the
Indian spice turmeric. NanoCurc
TM
, a recently described polymeric nano-
particle formulation of curcumin was used to treat medulloblastoma and
glioblastoma cells. Tis formulation caused a dose-dependent decrease in
growth of multiple brain tumor cell cultures, including the embryonal tu-
mor derived lines DAOY and D283Med, and the glioblastoma neurosphere
lines HSR-GBM1 and JHH -GBM14. Te reductions in viable cell mass
observed were associated with a combination of G2/M arrest and apoptotic
induction. Curcumin also signicantly decreased anchorage independent
clonogenic growth and reduced the CD133-positive stem-like population.
Levels of STAT3 were also attenuated. Tese data suggest that curcumin
nanoparticles can inhibit malignant brain tumor growth through the modu-
lation of cell proliferation, survival and stem cell phenotype [251].
Gene therapy has the potential to eectively medicate cancer by treat-
ing the root of the disease. Tis technology involves the delivery of DNA
molecules to cancer cells to insert or modify a gene in an eort to treat the
disease. Te delivery of DNA can be accomplished using a variety of vectors
including viruses, cell-based systems, and synthetic vectors. For glioma gene
therapy, viral vectors have been used to deliver suicide genes, pro-apoptotic
genes, p53, cytokines, and caspases. Tese studies have shown promising
preclinical results, but clinical trials have been limited by the fact that trans-
duced cells were found only within a very short distance of the delivery
site. To overcome these limitations, synthetic vectors have been developed
to more safely deliver DNA. In this study the authors investigate targeted
gene delivery to C6 glioma cells in a xenograft mouse model using chlo-
rotoxin (CTX) labeled nanoparticles. Te developed nanovector consists
of an iron oxide nanoparticle core, coated with a copolymer of chitosan,
polyethylene glycol (PEG) and polyethylenimine (PEI). Te CTX promote
specic uptake of nanovectors into glioma cells, exposing a higher propor-
tion of target cells to the delivered payload. Tese results could provide in-
sight into the design of more eective gene delivery vehicles for improved
treatment outcome of gene therapy for glioma. In brain tumor treatment,
the eciency of liposomes as nonviral gene delivery vectors has been in-
creased through surface ligand targeting, via mABs specic to certain re-
ceptors upregulated on glioma cell surfaces, such as transferrin receptors,
low-density lipoprotein receptors, and IL-13 receptors. A biopolymeric
gene delivery NP has recently been shown to be eective in vivo in delay-
ing tumor growth. Tis polymeric NP-based nonviral gene delivery vector
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch07_Bionanoparticles.indd 71 Manila Typesetting Company 08/22/2012 11:45PM
72 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
is a cationic albumin-conjugated pegylated nanoparticle that incorporates a
plasmid encoding proapoptotic Apo2 ligand/tumor necrosis factor-related
apoptosis-inducing ligand (Apo2L/TRAIL). After intravenous injection of
plasmid-loaded NPs in a C6 murine glioma model, plasmid DNA is in-
corporated into the host cell genome, thus inhibiting tumor growth, with
a prolonged survival [188]. Another gene therapy approach is the injection
in cancer cells with genes that can destroy the cells. A pro-drug or an inac-
tive form of a toxic drug is administered to the patients, and this drug will
kill o any cancer cells with the suicide genes in them. Te use of specic
NPs can represent a valid alternative to overcome possible toxic and infec-
tive eects of classic gene therapy. Te use of NP nonviral gene delivery
systems such as carbon nanotubes blocks a selective genic unction without
toxic eect on cellular phenotype. Tese systems have the ability to carry
short single genes, and also short DNA fragments or small interfering RNA
(siRNA) molecules that exert RNA interference on target gene expression
after their internalization [151]. Te antisense strategies constitute a very
interesting approach into molecular nanoparticle-based glioma therapy. Te
past and ongoing clinical trials are characterized by use of a nanoprobe as
carrier loaded with a single antisense molecule directed against a specic
target. An interesting and innovative idea may be performed using a new
platform in which a NP-based carrier system, in a targeted manner, may at
the same time direct two dierent antisense molecules directed against two
dierent targets or just antisense molecules with the capacity to interact and
block two molecular targets of the same tumor pathway or of two dierent
ones [31, 244]. A polymeric nanobioconjugate drug based on biodegrad-
able, nontoxic, and nonimmunogenic polymalic acid as a universal delivery
nanoplatform was used for design and synthesis of nanomedicine drug for
i.v. treatment of brain tumors. Te polymeric drug passes through the brain
tumor barrier (BTB) and tumor cell membrane using tandem monoclonal
antibodies targeting the BTB and tumor cells. Te next step for polymeric
drug action was inhibition of tumor angiogenesis by specically blocking
the synthesis of a tumor neovascular trimer protein, laminin-411, by at-
tached antisense oligonucleotides (AONs). Te AONs were released into
the target cell cytoplasm via pH-activated trileucine, an endosomal escape
moiety. Introduction of a trileucine endosome escape unit resulted in sig-
nicantly increased AON delivery to tumor cells, inhibition of laminin-411
synthesis in vitro and in vivo, specic accumulation in brain tumors, and
suppression of intracranial glioma growth [252]. One of the most promising
new strategies is the RNA interference (RNAi)-based approach, wherein
small double-stranded RNA molecules can sequence specically to inhibit
the expression of targeted oncogenes. To harness the full potential of this
approach, the prime requirements are to deliver the siRNA molecules with
high selectivity and eciency into tumor cells, and to monitor both siRNA
delivery and the resulting knock-down eects at the single cell level. Herein,
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch07_Bionanoparticles.indd 72 Manila Typesetting Company 08/22/2012 11:45PM
Exvrnrrwrzr Srunrrs 73
the authors describe the synthesis and target-specic delivery of multifunc-
tional siRNA-QD constructs for selectively inhibiting the expression of
epidermal growth factor receptor variant III (EGFRvIII) in target human
U87 glioblastoma cells, and subsequently monitoring the resulting down-
regulated signaling pathway with high eciency. Tis study demonstrates
the multi-functional siRNA-QD strategy focusing on targeted delivery,
high transfection eciency, and multi-modal imaging/tracking. Tese novel
methods and applications complement recent advances in nanomaterial-
based siRNA delivery, nanomaterial-based molecular imaging, and siRNA-
based chemotherapeutic strategies reported recently. Tis strategy could
also provide highly useful information regarding biosurface chemistry of
nanomaterials. In addition, the application of multi-functional siRNAQDs
to modulate the key cancer signaling pathways is important not only for se-
lective chemotherapeutic strategy but also for dissecting signaling cascades
triggered by inhibiting specic proteins [253].
Although immunotherapy is being investigated as an adjunct treatment,
the ability of gliomas to escape immune response will continue to be a sig-
nicant obstacle to this strategy. One approach to overcome the local im-
munosuppressive tumor microenvironment is the activation of the innate
immune system by toll-like receptor (TLR) agonists such as CpG oligonu-
cleotides (CpG). Because the TLR9, CpG receptor, is located intracellularly,
the authors have hypothesized that methods that enhance CpG internaliza-
tion may also potentiate its immunostimulatory response. In this study, it
has been reported that carbon nanotubes enhanced CpG uptake by tumor-
associated phagocytic cells, and resulted in their activation both in vitro and
in vivo. Furthermore, a single injection of low-dose CNTCpG complexes
eradicated intracranial gliomas through activation of NK and CD8 cells.
Tese ndings demonstrate that CNTs are nontoxic vehicles that can im-
prove CpG uptake into tumor-associated inammatory cells, leading to a
more robust anti-tumor response [254]. Alizadeh et al. [255] evaluated
the mechanism of cyclodextrin-based nanoparticle (CDP-NP) uptake into
a murine glioma model. Using mixed in vitro culture systems, the authors
demonstrated that CDP-NP was preferentially taken up by BV2 and N9
microglia (MG) cells as compared to GL261 glioma cells. Fluorescent mi-
croscopy and ow cytometry analysis of intracranial GL261 gliomas con-
rmed these ndings, and demonstrated a predominant CDP-NP uptake by
macrophages (MP) and MG within and around the tumor site. In conclu-
sion, these studies better characterize the cellular distribution of CDP-NP
in brain tumors, and demonstrate that MP and MG could potentially be
used as nanoparticle drug carriers into malignant brain tumors. Schneider
et al. [195] recently examined a double-punched approach to overcome the
escape of glioblastoma cells from immune surveillance through an active
specic immunization. Te authors, using Newcastle disease virus-infected
tumor cells and an antisense oligonucleotide against the TGF-b loaded in
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch07_Bionanoparticles.indd 73 Manila Typesetting Company 08/22/2012 11:45PM
74 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
polybutyl cyanoacrylate NPs, demonstrated a signicant decrease in plasma
TGF-b2 and an increase in antitumoral cytotoxicity.
In vitro study of PDT with targeted delivery systems is an alternative
to current adjuvant therapy, and it is characterized by low morbidity and
lack of susceptibility to the development of resistance. PDT involves the
use and delivery of photosensitizers combined with local excitation by the
appropriate wavelength of light, resulting in the production of ROS, which
initiate apoptosis and cytotoxicity in many types of tumors. Moreover,
PDT produces within treated neoplastic tissue microvascular injury leading
to inammation and hypoxia. Tis therapeutic approach is more selective
and less toxic than chemotherapy, because the drug is not activated until
the light is delivered. Te recent molecular targeting approach selectively
detects cancer cells through molecular-recognition processes such as ligand-
receptor or antibody-antigen interactions. PDT is an interesting approach
for the treatment of malignant gliomas, resulting in a localized treatment
approach with an important improvement in local control of tumors and
a signicantly improved survival rate [44]. In a recent study, Wang et al.
[186] have demonstrated prominent photothermal selective damage of 426
targeted glioma cells. Molecular targeting, in this case, has been performed
using carbon nanotubes conjugated with mABs specic to CD133. PDT
using the nanobiohybrid photocatalyst resulted in the destruction of over
80% of A172 glioma cells with high levels of IL13R expression, whereas in
the case of U87 cells characterized by lower antigen presentation, cytotox-
icity at the same conditions reached a plateau of 50% and did not increase
at higher photocatalyst concentrations [139140]. Moreover, no cytotoxic-
ity was observed for normal human astrocytes (NHA) known to be not
IL13R-expressing [139140]. Recently Tian et al. [256] showed the feasi-
bility of encapsulating the alkylating agent, temozolomide [(3,4-dihydro-
3-methyl-4-oxoimidazo [5,1-d]-as-tetrazine-8-carboxamide (TMZ)], into
polybutylcyanoacrylate (PBCA) NPs by polymerization. Compared with
TMZ solution, TMZ-PBCA nanoparticles exhibited sustained release in
vitro. Furthermore, based on the pattern of distribution in body organs,
higher concentrations of TMZ can be detected in the brain after binding to
PBCA nanoparticles coated with polysorbate-80, which may be more use-
ful for treating brain tumors. Te prepared formulation may also reduce the
toxicity of chemotherapy. Steiniger et al. [257] demonstrated in a murine
glioblastoma model, a statistically signicant increase in survival time of
glioblastoma-bearing rats treated with doxorubicin bound to polysorbate-
coated NPs, compared to the control groups treated with other doxorubicin
formulations. More than 20% of the animals showed a long-term remis-
sion and no drug-NP complex neurotoxicity was observed. In an ongoing
phase I clinical trial, paclitaxel albumin-stabilized NP formulation is be-
ing used in treating advanced cancers such as bladder cancer, and brain and
CNS tumors. Te authors demonstrated in a subset of patients a decrease
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch07_Bionanoparticles.indd 74 Manila Typesetting Company 08/22/2012 11:45PM
Exvrnrrwrzr Srunrrs 75
in tumor vascular permeability. In a recent study, in vivo murine U87MG
glioblastoma multiforme model, liposomal topotecan increased survival
more than 20-fold [258]. Te eciency of liposomal and other NP-based
drug delivery systems, such as colloidal nonlipidic coated polymeric NPs,
microspheres, and micelles, is enhanced by targeting of various molecules.
In a novel research, MPEGylated PCL nanoparticles containing paclitaxel
were prepared by the emulsion and evaporation technique. C6 glioblastoma
cell viability studies showed that MPEG-NP/paclitaxel could produce
higher or at least comparable cytotoxicity than Taxol injection. As demon-
strated by in vivo real-time uorescence imaging analysis in intracranial C6
glioblastoma bearing mice, the MPEGylated PCL nanoparticles displayed
much stronger uorescence signal in tumor tissue, and larger area-under-
curve than non-MPEGylated PCL nanoparticles. Te therapeutic improve-
ment of MPEG-NP/paclitaxel in vivo against intracranial C6 glioblastoma
was also obtained based on the eect of passive tumor targeting [198]. One
interesting approach consists of coating a NP with polysorbate 80, which
adsorbs apolipoproteins B and E, and allows receptor-mediated endocytosis
by brain capillary endothelial cells. In these studies, 40% of the rats treated
with doxorubicin loaded nanoparticles survived the duration of the study
(6 months), with no evidence of residual tumor. Similarly, PEGylated doxo-
rubicin loaded solid lipid nanoparticles can enhance delivery across the BBB
after intravenous administration in rabbits [259]. Doxorubicin was pres-
ent in the brain only after administration of the nanoparticle formulation
and the extent of doxorubicin transport was dependent on the extent of
PEG modication. Recently, a promising chemotherapeutic drug (SN-38)
incorporated in micelles was compared with CPT-11, a prodrug of SN-38,
for the glioblastoma treatment in mice. Te growth-inhibitory eects of
the drug-loaded micelles were 34- to 444-fold more potent than those of
CPT-11. In addition, when the drug was incorporated in the nanovectors, a
signicantly potent anti-tumor activity against an orthotopic glioblastoma
multiforme xenograft and signicantly longer survival rates than CPT-11
were observed [260].
A new strategy to achieve selective drug delivery to tumor tissue is mag-
netic targeting. Tis approach has the advantage of enhancing the attraction
of drug-loaded magnetic NPs in cancer cells by using an externally ap-
plied magnetic eld [194]. Among the other polymer-derived drug delivery
systems, the nanoconjugate Polycen (based on polymalic acid) has been
studied in animal models of human glioma, using intracranial injections of
human cancer cells. Antiangiogenic results have been obtained in rats by
injection, in vivo, of human glioma U87MG xenografts [261]. A novel study
aimed to examine the applicability of polyethyleneimine (PEI)-modied
magnetic nanoparticles (GPEI) as a potential vascular drug/gene carrier to
brain tumors. Te obtained data show that cationic magnetic nanoparticles
GPEI exhibit high cell penetration ability and low cell toxicity. In addition,
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch07_Bionanoparticles.indd 75 Manila Typesetting Company 08/22/2012 11:45PM
76 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
GPEI could be magnetically captured in glioma lesions following clinically-
viable intra-carotid administration. Furthermore, the extent of GPEI accu-
mulation was 5.2-fold higher than that of G100 in the tumor lesions, but
not in the contra-lateral normal brain, revealing higher target selectivity of
cationic nanoparticles [262].
Polycen conjugated with appropriate mABs specic to a tumor cell sur-
face receptor may represent a potential new drug for glioma treatment. A
recent in vitro and in vivo study in rats has demonstrated the ecacy of
indomethacin-loaded nanocapsules, with a signicant reduction of the mi-
totic index and the microvascular proliferation in implanted glioma [189].
Recently, Etame et al. [263] have been described the rst demonstration
of focal enhanced delivery of AuNPs with therapeutic potential into the
cerebral hemisphere using MRgFUS in a rat model. Te authors show
the rst direct evidence of localization of AuNPs within the brain paren-
chyma suggesting BBB transgression. Tese results suggest a potential role
for MRgFUS in the delivery of AuNPs, with therapeutic potential into the
CNS for targeting neurological disorders.
Te use of stem cells, as cellular carriers is a promising therapeutic strat-
egy to deliver specic drug-loaded NPs. Currently, several studies highlight
that caution should be used in the therapeutic exploitation of MSCs for
malignant conditions. Indeed, the exact biological function of MSCs in
brain tumors is still unclear. Some studies indicate that MSCs promote tu-
mor development either by providing a niche for cancer stem cells, through
impairing immune surveillance, or by dierentiation into cancer-associated
broblastlike cells. Te applications of NP systems with stem cells include
longterm labeling of stem cells with superparamagnetic iron oxide NPs, uo-
rochrome loaded NPs, or quantum dots to monitor their fate and regenera-
tive potential [264]. Te migratory behavior of stem cells towards glioma in
vivo has been routinely demonstrated with this approach. NP systems have
also been used for gene transfection. For example, biodegradable polymer
NPs have been developed to deliver the VEGF gene to human MSCs and
human ESC-derived cells to promote angiogenesis [265].
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
ASME_Ch07_Bionanoparticles.indd 76 Manila Typesetting Company 08/22/2012 11:45PM
8. Conclusions
Te treatment of brain cancer is one of the most dicult challenges in neu-
rosurgery and oncology. Malignant gliomas involve, in their progression,
multiple aberrant signaling pathways and the BBB restricts the delivery of
many chemotherapeutic agents. Targeted therapies have successfully been
applied in cancers, but their ecacy remains low in malignant brain tumors
[266]. Tere are several factors underlying the disappointing results in brain
cancer therapeutics including limited tumor cell drug uptake, intracellular
drug metabolism, inherent tumor sensitivity to chemotherapy, and cellular
mechanisms of resistance. Te results in the rst experimental studies sug-
gest that a single antiangiogenic therapy is not sucient to eradicate glioma
[31, 245].
Nanotechnology provides a unique opportunity to combat cancer on the
molecular scale through careful engineering of nanomedicines to speci-
cally interact with cancer cells and inhibit cancer cell function. Beyond use
of NPs as nanomedicines, more focus should be placed on use of NPs as
tools to learn more about cancer biology and failure of treatments. It is also
possible to take into neoplastic tissue, novel selective contrast enhancement
molecules to visualize brain tumors and to study in vivo all of their charac-
teristics, such as cellular proliferation, angiogenesis, necrosis, tumor-safe tis-
sue interface, and edema [45, 43, 267]. Tere are signicant opportunities
to investigate the use of nuclear imaging techniques such as positron emis-
sion tomography (PET) and single-photon emission computed tomography
(SPECT) for development of radiolabeled nanoparticles targeting cancer.
Te versatility, sensitivity and tomographic imaging capabilities of these
imaging modalities will provide excellent opportunities for future develop-
ment of targeted nanoparticle formulations. Te unique properties of engi-
neered nanomaterials endow them with dynamic physiochemical features
dierent from those of bulk materials with the same compositions. Tese
unique properties are very attractive for pharmaceutical and clinical appli-
cations. Engineering of nanoparticles for combined therapeutic and diag-
nostic applications (theranostic nanoparticles) requires knowledge of their
material, chemical, physical, biochemical, and toxicological properties and is
under intense investigation. Te surface of nanoparticles can be modied to
achieve targeted delivery and improved biocompatibility. Compounds may
also be encapsulated within the interior core of nanoparticles for multiple
functions. It is known that in malignant brain tumors the BBB is normally
in a breakdown mode. Nanoparticle-based delivery systems could increase
the overcoming of the BBB by the use of drugs with a targeted-cell specic-
ity modality. Tis approach permits the use of a lower dose of drug, a selec-
tive drug delivery to target tumor cells, both into the central core of tumor
and into the distal foci of tumor cells within areas often characterized from
integrity of the BBB [45]. Tis aspect is very important in early diagnosis,
78 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
in recurrences, in preoperative histological and grade diagnosis, and in pre-
operative treatment planning.
Te ability to monitor biodistribution of treatments, migration of cells
throughout the body, and tumor development and evolution in real-time,
can elucidate new pathways that cancer cells rely on. Tis information will
be invaluable for improvement of therapy. Tere is a need, therefore, to de-
velop novel approaches for the accurate detection of early-stage of cancer
and for targeted therapies based on the cancer-specic markers, which could
lead to personalized medicine. Considerable eort has been made toward
the research and development of multifunctional nano-particle systems for
cancer targeted imaging and therapy. Teranostic nanomedicine represent
an integrated nanotherapeutic system, which can diagnose, deliver targeted
therapy, and monitor the response to therapy. Tis integration of diagnostic
imaging capability with therapeutic interventions is critical to addressing
the challenges of brain tumor hetereogeneity and adaptation. As a platform
technology, nanomedicine has the advantage of being able to target multiple
tumor markers and deliver multiple agents simultaneously for synergy in
addressing the challenges of cancer hetereogeneity and adaptative resistance.
Recently many reviews have discussed about characteristics and biomedi-
cal applications on magnetic nanoparticles and reported that it can simulta-
neously act as diagnostic molecular imaging agent and carries dierent
type of drug at same time [268]. In coming years, we may expect growing
numbers of reports involving novel hybrid structures based upon nucleic
acids, such as siRNAs for the targeted silencing of the major genetic path-
ways associated with brain cancer development and progression [201, 269],
and single strand DNA short aptamers for ecient, inexpensive, and non-
immunogenic alternatives to antibodies.
Although nano-derived applications have great potentials, there are some
concerns about the potential nanoparticles have to cause adverse eects on
human health and the environment. Te dierent properties that make
nanoparticles so promising are at the same time properties that are likely to
have impact on ecosystems and organisms. Nanoparticles are likely to cause
dierent impacts on human health, occupation health and the environment,
depending on the size, shape and chemical composition of the nanoparticle.
Tere is therefore great uncertainty about what the actual risks of nano-
particle to human health and the environment are. Nanotechnology is still
a relatively young eld, and little is known about the long-term eects of
exposure to nanomaterials, especially in clearance organs such as the liver,
spleen, and kidneys. Furthermore, the potential toxicity associated with
the wide variety of nanomaterials available, ranges from completely inert
to highly toxic, which could slow their advancement into the clinic. Tere
is a need for further research on more types of nanomaterials to get a basic
understanding on how they interact with the biological system and where
in the body they might go. Additionally, it seems very important to nd
Cowcrusrows 79
out whether there is a dierence between ultrane particles and engineered
nanoparticles. As the variety of engineered nanoparticles increases every day
and more of them nd their way into commercialisation, screening methods
determining whether the nanoparticles have properties that should be more
thoroughly tested, is highly needed. Moreover, the eciency of targeting
nanoparticles to the tumor is not very high and the targeting is always not
perfect. Te majority of the nanotechnology approaches applied in brain on-
cology reported are in the stages of in vitro or animal model testing. Prior to
the use of nanoengineered materials in clinical applications, major concerns,
including biocompatibility and biodistribution, biosafety, side-eects, and
long-term eects have to be addressed. Furthermore, personalized diagnos-
tics and the identication of unique biological targets (epitope sequences),
related to problems posed by disease variance, appear to be essential for
clinical success.
Objects of debate are the results about the long-term eects of inter-
actions between nanoparticles, and coating of molecules and target cells.
In order for this promising eld to rapidly progress, focus must be placed
on elucidating the safety of these novel materials. Tis will rely on the de-
velopment of better characterization tools and methodologies, and more
reproducible synthesis strategies so that accurate and broadly applicable
conclusions can be drawn. Biomaterials can be formulated with anti-cancer
drugs to produce injectable or implantable polymer-drug conjugates allow-
ing sustained, localized delivery of therapeutic levels of the entrapped drug,
protein, gene, or other potential therapeutic. Besides, basic knowledge of cell
biology, tumor biology, immunology and cancer biology are necessary to the
rational design of nanoparticles for brain tumor therapy.
An optimal realization of a system that overcomes the problems associ-
ated with novel strategies in brain tumor treatments requires the identica-
tion of specic neoplastic markers, the development of technology for the
biomarker-targeted delivery of therapeutic agents, and the simultaneous
capability of avoiding biological and biophysical barriers.
References
1. Burger, P.C., Dubois, P.J., Schold, S.C. Jr., Smith, K.R. Jr., Odom, G.L., et al.,
1983, Computerized tomographic and pathological studies of the untreated,
quiescent, and recurrent glioblastoma multiforme, J. Neurosurg., 58, pp. 159
169.
2. Yung, W.K., Albright, R., Olson, J., Fredericks, R., Fink, K., et al., 2000, A
phase II study of temozolamide vs. procarbazine in patients with glioblastoma
multiforme at rst relapse, Br. J. Cancer, 83, pp. 588593.
3. Ruben, J.D., Dally, M., Bailey, M., Smith, R., Mclean, C.A., Fedele, P., 2006,
Cerebral radiation necrosis: incidence, outcomes, and risk factors with
emphasis on radiation parameters and chemotherapy, Int. J. Radiat. Oncol.
Biol. Phys., 65, pp. 499508.
4. Caruso, G., Cao, M., Alafaci, C., Raudino, G., Cafarella, D., et al., 2011,
Could nanoparticles systems have a role in the treatment of cerebral gliomas?
Nanomedicine, 7, pp. 744752.
5. Caruso, G., Raudino, G., Cao, M., Alafaci, C., Granata, F., 2010,
Nanotechnology platforms in diagnosis and treatments of primary brain
tumors, Recent Pat. Nanotechn., 4, pp. 119122.
6. Chintala, S.K., Gokaslan, Z.L., Go, Y., Sawaya, R., Nicolson, G.L., Rao, J.S.,
1996, Role of extracellular matrix proteins in regulation of human glioma cell
invasion in vitro, Clin. Exp. Metastasis, 14, pp. 358366.
7. Hanahan, D. and Folkman, J., 1996, Patterns and emerging mechanisms of
the angiogenic switch during tumorigenesis, Cell, 86, pp. 353364.
8. Uhm, J.H., Dooley, N.P., Villemure, J.-G., Yong, V.W., 1997, Mechanisms of
glioma invasion: role of matrix metalloproteinases, Can. J. Neurol. Sci., 24,
pp. 315.
9. Gladson, C.L., 1996 Expression of integrin alpha v beta 3 in small blood
vessels of glioblastoma tumors, J. Neuropathol. Exp. Neurol., 55, pp. 1143
1149.
10. Cao, M., German, A., Caruso, G., Meli, F., Galatioto, S., et al., 2004
An immunohistochemical study of extracellular matrix proteins laminin,
bronectin and type IV collagen in paediatric glioblastoma multiforme, Acta
Neurochir. (Wien), 146, pp. 11131118.
11. Miner, J.H., 2008, Laminins and their roles in mammals, Microsc. Res. Tech.,
71, pp. 349356.
12. Pardridge, W.M., 2003, Blood-brain barrier drug targeting: the future of brain
drug development, Mol. Interv., 3, pp. 90105.
13. Egleton, R.D., and Davis, T.P., 1997, Bioavailability and transport of peptides
and peptide drugs into the brain, Peptides, 18, pp. 14311439.
14. Engelhardt, B., and Sorokin, L., 2009, Te bloodbrain and the blood
cerebrospinal uid barriers: function and dysfunction, Semin. Immunopathol.,
31, pp. 497511.
15. Cardoso, F.L., Brites, D., Brito, M.A., 2010, Looking at the bloodbrain
barrier: molecular anatomy and possible investigation approaches, Brain Res.
Rev., 64, pp. 328363.
82 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
16. Soma, T., Chiba, H., Kato-Mori, Y., Wada, T., Yamashita, T., 2004, Tr (207)
of claudin-5 is involved in size-selective loosening of the endothelial barrier by
cyclic AMP, Exp. Cell. Res., 300, pp. 202212.
17. Hawkins, B.T., and Davis, T.P., 2005, Te bloodbrain barrier/neurovascular
unit in health and disease, Pharmacol. Rev., 57, pp. 173185.
18. Petty, M.A., and Lo, E.H., 2002, Junctional complexes of the blood-brain
barrier: permeability changes in neuroinammation, Prog. Neurobiol., 68,
pp. 311323.
19. Uchino, H., Kanai, Y., Kim, K., Wempe, M.F., Chairoungdua, Y., et al., 2002,
Transport of amino acid-related compounds mediated by L-type amino acid
transporter1 (LAT1): Insights into the mechanisms of substrate recognition,
Mol. Pharmacol., 61, pp. 729737.
20. Girardin, F., 2006, Membrane transporter proteins: a challenge for CNS drug
development, Dialogues Clin. Neurosci., 8, pp. 311321.
21. Urquhart, B.L., and Kim, R.B., 2009, Bloodbrain barrier transporters and
response to CNS-active drugs, Eur. J. Clin. Pharmacol., 65, pp. 10631070.
22. Kemper, E.M., Boogerd, W., Tuis, I., Beijnen, J.H., van Tellingen, O., 2004,
Modulation of the bloodbrain barrier in oncology: therapeutic opportunities
for the treatment of brain tumours? Cancer Treat. Rev., 30, pp. 415423.
23. Pardridge, W.M., 2007, Bloodbrain barrier delivery, Drug Discov. Today,
12, pp. 5461.
24. Moos, T., and Morgan, E.H., 2004, Te metabolism of neuronal iron and its
pathogenic role in neurological disease: review, Ann. N. Y. Acad. Sci., 1012,
pp. 1426.
25. Jain, S., Mishra, V., Singh, P., Dubey, P.K., Saraf, D.K., Vyas, S.P., 2003,
RGD-anchored magnetic liposomes for monocytes/neutrophils-mediated
brain targeting, Int. J. Pharm., 261, pp. 4355.
26. Farokhzad, O.C., and Langer, R., 2009, Impact of nanotechnology on drug
delivery, ACS Nano, 3, pp. 1620.
27. Sinha, R., Kim, G.J., Nie, S., Shin, D.M., 2006, Nanotechnology in cancer
therapeutics: Bioconjugated nanoparticles for drug delivery, Mol. Canc. Ter.,
5, pp. 19091917.
28. Brigger, I., Dubernet, C., Couvreur, P., 2002, Nanoparticles in cancer therapy
and diagnosis, Adv. Drug Deliv. Rev., 54, pp. 631651.
29. Koo, O.M., Rubinstein, I., Onyuksel, H., 2005, Role of nanotechnology
in targeted drug delivery and imaging: a concise review, Nanomedicine, 1,
pp. 193212.
30. Wen, P.Y., Yung, W.K., Lamborn, K.R., Dahia, P.L., Wang, Y., et al., 2006,
Phase I/II study of imatinib mesylate for recurrent malignant gliomas: North
American Brain Tumor Consortium Study 99-08, Clin. Cancer Res., 12,
pp. 48994907.
31. Caruso, G., Cao, M., Raudino, G., Alafaci, C., Salpietro, F.M., Tomasello, F.,
2010, Antisense oligonucleotides as an innovative therapeutic strategy in the
treatment of high-grade gliomas, Rec. Pat. CNS Drug Discov., 5, pp. 5369.
32. Moghimi, S.M., 2006, Recent developments in polymeric nanoparticle
engineering and their applications in experimental and clinical oncology,
Anticancer Agents Med. Chem., 6, pp. 553561.
Rrrrnrwcrs 83
33. Kim, K., Lee, M., Park, H., Kim, J.H., Kim, S., et al., 2006, Cell-permeable
and biocompatible polymeric nanoparticles for apoptosis imaging, J. Am.
Chem. Soc., 128, pp. 34903491.
34. Nasongkla, N., Bey, E., Ren, J., Ai, H., Khemtong, C., et al., 2006,
Multifunctional polymeric micelles as cancer-targeted, MRI-ultrasensitive
drug delivery systems, Nano Lett., 6, pp. 24272430.
35. Moghimi, S.M., Hunter, A.C., Murray, J.C., 2001, Long-circulating and
target-specic nanoparticles: theory to practice, Pharmacol. Rev., 53,
pp. 283318.
36. Moghimi, S. M., and Szebeni, J., 2003, Stealth liposomes and long circulating
nanoparticles: critical issues in pharmacokinetics, opsonization and protein-
binding properties, Prog. Lipid Res., 42, pp. 463478.
37. Oh, P., Li, Y., Yu, J., Durr, E., Krasinka, K.M., et al., 2004, Subtractive
proteomic mapping of the endothelial surface in lung and solid tumours for
tissue-specic therapy, Nature, 429, pp. 629635.
38. Panyam, J., and Labhasetwar, V., 2004, Biodegradable nanoparticles for
drug and gene delivery to cells and tissues, Adv. Drug Deliv. Rev., 55,
pp. 329347.
39. Veerareddy, P.R., and Vobalabonia, V., 2004, Lipid-based formulas of
amphotericin B, Drugs Today, 40, pp. 133145.
40. Agrawal, A.K., and Gupta, C.M., 2000, Tuftsin-bearing liposomes in
treatment of macrophage-based infections, Adv. Drug Deliv. Rev., 41,
pp. 135146.
41. Dileo, J., Banerjee, R., Whitmore, M., Nayak, J., Falo, L., Huang, L., 2003,
LPD mediated antigen delivery to antigen presenting cells results in enhanced
anti-tumor immune responses, Mol. Ter., 7, pp. 640648.
42. Bonifaz, L., Bonnyay, D., Mahnke, K., Rivera, M., Nussenzweig, M.C.,
Steinman, R.M., 2002, Ecient targeting of protein antigen to the dendritic
cell receptor DEC-205 in the steady state leads to antigen presentation on
major histocompatibility complex class I products and peripheral CD8+ T cell
tolerance, J. Exp. Med., 196, pp. 16271638.
43. Bhojani, M.S., Van Dort, M., Rehemtulla, A., Ross, B.D., 2010, Targeted
imaging and therapy of brain cancer using theranostic nanoparticles, Mol.
Pharm., 7, pp. 19211929.
44. Reddy, G.R., Bhojani, M.S., McConville, P., Moody, J., Moat, B.A., et al.,
2006, Vascular targeted Nanoparticles for imaging and treatment of brain
tumors, Clin. Cancer Res., 12, pp. 66776686.
45. Porkka, K., Laakkonen, P., Homan, J.A., Bernasconi, M., Ruoslathi, E., 2002,
A fragment of the HMGN2 protein homes to the nuclei of tumor cells and
tumor endothelial cells in vivo, Proc. Natl. Acad. Sci. U.S.A., 99, pp. 7444
7449.
46. Christian, S., Pilch, J., Akerman, M.E., Porkka, K., Laakkonen, P., Ruoslahti,
E., 2003, Nucleolin expressed at the cell surface is a marker of endothelial cells
in angiogenic blood vessels, J. Cell. Biol., 163, pp. 871878.
47. Sun, C., Veiseh, O., Gunn, J., Fang, C., Hansen, S., et al., 2008, In vivo
MRI detection of gliomas by chlorotoxin-conjugated superparamagnetic
nanoprobes, Small, 4, pp. 372379.
84 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
48. Barnes, C.P., Sell, S.A., Boland, E.D., Simpson, D.G., Bowlin, G.L., 2007,
Nanober technology: Designing the next generation of tissue engineering
scaolds, Adv. Drug Deliv. Rev., 59, pp. 14131433.
49. Boulaiz, H., Alvarez, P.J., Ramirez, A., Marchal, J.A., Prados, J., et al., 2011,
Nanomedicine: application areas and development prospects, Int. J. Mol.
Sci., 12, pp. 33033321.
50. Duncan, R., 2003, Te dawning era of polymer therapeutics, Nat. Rev. Drug
Discov., 2, pp. 347360.
51. Panyam, J., and Labhasetwar, V., 2003, Biodegradable nanoparticles for drug
and gene delivery to cells and tissue, Adv. Drug Deliv. Rev., 55, pp. 329
347.
52. Couvreur, P., Barratt, G., Fattal, E., Legrand, P., Vauthier, C., 2002,
Nanocapsule technology: a review, Crit. Rev. Ter. Drug Carrier Syst., 19,
pp. 99134.
53. Sawant, R., and Torchilin, V., 2010, Intracellular transduction using cell-
penetrating peptides, Mol. Biosyst., 6, pp. 628640.
54. Musacchio, T. and Torchilin, V.P., 2011, Recent developments in lipid-based
pharmaceutical nanocarriers, Front. Biosci., 16, pp. 13881412.
55. Stachelek, S.J., Finley, M.J., Alferiev, I.S., Wang, F., Tsai, R.K., et al., 2011, Te
eect of CD47 modied polymer surfaces on inammatory cell attachment
and activation, Biomaterials, 32, pp. 43174326.
56. Tokarev, I. and Minko, S., 2010, Stimuli-responsive porous hydrogels at
interfaces for molecular ltration, separation, controlled release, and gating in
capsules and membranes, Adv. Mater., 22, pp. 34463462.
57. Lamprecht, A., Ubrich, N., Yamamoto, H., Schfer, U., Takeuchi, H., et al.,
2001, Biodegradable nanoparticles for targeted drug delivery in treatment of
inammatory bowel disease, J. Pharmacol. Exp. Ter., 299, pp. 775781.
58. Choi, C.H., Alabi, C.A., Webster, P., Davis, M.E., 2010, Mechanism of active
targeting in solid tumors with transferrin-containing gold nanoparticles, Proc.
Natl. Acad. Sci. U.S.A., 107, pp. 12351240.
59. Maeda, H., Wu, J., Sawa, T., Matsumura, Y., Hori, K., 2000, Tumor vascular
permeability and the EPR eect in macromolecular therapeutics: a review,
J. Control Release, 65, pp. 271284.
60. Chytil, P., Etrych, T., Konak, C., Sirova, M., Mrkvan, T., et al., 2008, New
HPMA copolymer-based drug carriers with covalently bound hydrophobic
substituents for solid tumour targeting, J. Control Release, 127, pp. 121
130.
61. Sahoo, S.K., and Labhasetwar, V., 2005, Enhanced antiproliferative activity
of transferrin-conjugated paclitaxel-loaded nanoparticles is mediated via
sustained intracellular drug retention, Mol. Pharm., 2, pp. 373383.
62. Choi, S.H., Lee, S.H., Park, T.G., 2006, Temperature-sensitive pluronic/
poly(ethylenimine) nanocapsules for thermally triggered disruption of intra-
cellular endosomal compartment, Biomacromolecules, 7, pp. 18641870.
63. Oishi, M., Kataoka, K., Nagasaki, Y., 2006, pH-responsive three-layered
PEGylated polyplex micelle based on a lactosylated ABC triblock copolymer
as a targetable and endosome-disruptive nonviral gene vector, Bioconjug.
Chem., 17, pp. 677688.
Rrrrnrwcrs 85
64. Trollet, C., Scherman, D., Bigey, P., 2008, Delivery of DNA into muscle for
treating systemic diseases: advantages and challenges, Methods Mol. Biol.,
423, pp. 199214.
65. OBrien, J.A., Holt, M., Whiteside, G., Lummis, S.C., Hastings, M.H., 2001,
Modications to the hand-held Gene Gun: improvements for in vitro biolistic
transfection of organotypic neuronal tissue, J. Neurosci. Methods, 112,
pp. 5764.
66. Guo, S., Huang, Y., Zhang, W., Wang, W., Wei, T., et al., 2011,
Ternary complexes of amphiphilic polycaprolactone-graft-poly(N, N-
dimethylaminoethylmethacrylate), DNA and polyglutamic acid-graft-poly
(ethylene glycol) for gene delivery, Biomaterials, 32, pp. 42834292.
67. Lee, S.H., Choi, S.H., Kim, S.H., Park, T.G., 2008, Termally sensitive
cationic polymer nanocapsules for specic cytosolic delivery and ecient gene
silencing of siRNA: swelling induced physical disruption of endosome by cold
shock, J. Control Release, 125, pp. 2532.
68. Weber, N., Ortega, P., Clemente, M.I., Shcharbin, D., Bryszewska, M., et
al., 2008, Characterization of carbosilane dendrimers as eective carriers of
siRNA to HIV-infected lymphocytes, J. Control Release, 132, pp. 5564.
69. Chono, S., Li, S.D., Conwell, C.C., Huang, L., 2008, An ecient and low
immunostimulatory nanoparticle formulation for systemic siRNA delivery to
the tumor, J. Control Release, 131, pp. 6469.
70. Hu, D., Gong. P., Ma, Y., Cai, L., 2009, Research advancement and prospects
of nanotechnology in early diagnosis and treatment of cancer, Chinese
J. Cancer, 28, pp. 17.
71. Kumari, A., Yadav, K.S., Yadav, S.C., 2010, Biodegradable polymeric
nanoparticles based drug delivery systems, Colloids and Surfaces B:
Biointerfaces, 75, pp. 18.
72. Kateb, B., Chiu, K., Black, K.L., Yamamoto, V., Khalsa, B., 2011,
Nanoplatforms for constructing new approaches to cancer treatment,
imaging, and drug delivery: What should be the policy? NeuroImage, 54,
pp. S106S124.
73. Rozkhova, E.A., 2011, Nanoscale materials for tackling brain cancer: recent
progress and outlook, Adv. Mater., 23, pp. 136150.
74. Jain, K.K., 2005, Nanotechnology in clinical laboratory diagnostics, Clin.
Chim. Acta, 358, pp. 3754.
75. Wang, Y.X., Hussain, S.M., Krestin, G.P., 2011, Superparamagnetic iron
oxide contrast agents: physicochemical characteristics and applications in MR
imaging, Eur. Radiol., 11, pp. 23192331.
76. Neuwelt, E.A., Vrallyay, P., Bag, A.G., et al., 2004, Imaging of iron oxide
nanoparticles by MR and light microscopy in patients with malignant brain
tumours, Neuropathol. Appl. Neurobiol., 30, pp. 456471.
77. Salata, O.V., 2004, Applications of nanoparticles in biology and medicine,
J. Nanobiotechnology, 2, p. 3.
78. Hede, S., and Huilgol, N., 2006, Nano: Te new nemesis of cancer, J. Cancer
Res. Ter., 2, pp. 186195.
79. Perou, C.M., Srlie, T., Eisen, M.B., Rijn, M., Jerey, S.S., et al., 2000,
Molecular portraits of breast tumours, Nature, 406, pp. 747752.
86 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
80. Kennedy, G.C., Matsuzaki, H., Dong, S., Liu, W.M., Huang, J., et al.,
2003, Large-scale genotyping of complex DNA, Nat. Biotechnol., 21,
pp. 12331237.
81. Weissleder, R., and Pittet, M.J., 2008, Imaging in the era of molecular
oncology, Nature, 452, pp. 580589.
82. Kraitchman, D.L., Heldman, A.W., Atalar, E., Amado, L.C., Martin, B.J., et
al., 2003, In vivo magnetic resonance imaging of mesenchymal stem cells in
myocardial infarction, Circulation, 107, pp. 22902293.
83. Nida, D.L., Rahman, M.S., Carslon, K.D., Richards-Kortum, R., Follen, M.,
2005, Fluorescent nanocrystals for use in early cancer detection, Gynecol.
Oncol., 99, pp. S89S94.
84. Cross, S.E., Jin, Y.S., Rao, J., Gimzewski, J.K., 2007, Nanomechanical
analysis of cells from cancer patients, Nat. Nanotechnol., 2, pp. 780783.
85. Gao, X., Cui, Y., Levenson, R.M., Chung, L.W., Nie, S., 2004, In vivo cancer
targeting and imaging with semiconductor quantum dots, Nat. Biotechnol.,
22, pp. 969976.
86. Rapaport, N., Gao, Z., Kennedy, A., 2007, Multifunctional nanoparticles
for combining ultrasonic tumor imaging and targeted chemotherapy, J. Natl.
Cancer Inst., 99, pp. 10951106.
87. Tang, N., Du, G., Wang, N., Liu, C., Hang, H., Liang, W., 2007, Improving
penetration in tumors with nanoassemblies of phospholipids and doxorubicin,
J. Natl. Cancer Inst., 99, pp. 10041015.
88. Chakravarty, P., Marches, R., Zimmerman, N.S., Swaord, A.D., Bajaj, P.,
et al., 2008, Termal ablation of tumor cells with antibody-functionalized
single-walled carbon nanotubes, Proc. Natl. Acad. Sci. U.S.A., 105,
pp. 86978702.
89. MacBeath, G., 2002, Protein microarrays and proteonomics, Nat. Genet., 32,
pp. 526532.
90. Lesniak, M.S., Upadhyay, U., Goodwin, R., Tyler, B., Brem, H., 2005, Local
delivery of doxorubicin for the treatment of malignant brain tumors in rats,
Anticancer Res., 25, pp. 38253831.
91. Misra, A., Ganesh, S., Shahiwala, A., Shah, S.P., 2003, Drug delivery
to the central nervous system: A review, J. Pharm. Pharm. Sci., 6,
pp. 252273.
92. Beduneau, A., Saulnier, P., Benoit, J.P., 2007, Active targeting of brain tumors
using nanocarriers, Biomaterials, 28, pp. 49474967.
93. Liu, Z., Cai, W., He, L., Nakayama, N., Chen, K., et al., 2007, In vivo
biodistribution and highly ecient tumor targeting of carbon nanotubes in
mice, Nat. Nano., 2, pp. 4752.
94. Bangham, A.D., Standish, M.M., Watkins, J.C., 1965, Diusion of univalent
ions across the lamellae of swollen phospholipids, J. Mol. Biol., 13, pp. 238
252.
95. Heath, T.D., Fraley, R.T., Papahdjopoulos, D., 1980, Antibody targeting of
liposomes: cell specicity obtained by conjugation of F(ab)2 to vesicle surface,
Science, 210, pp. 539541.
96. Duncan, R., 2006, Polymer conjugates as anticancer nanomedicines, Nat.
Rev. Cancer, 6, pp. 688701.
Rrrrnrwcrs 87
97. Fonseca, C., Simoes, S., Gaspar, R., 2002, Paclitaxel-loaded PLGA
nanoparticles: preparation, physiochemical characterization and in vitro anti-
tumoral activity, J. Control. Release, 83, pp. 273286.
98. Avgoustakis, K., Beletsi, A., Panagi, Z., Klepetsanis, P., Karydas, A.G.,
Ithakissios, D.S., 2002, PLGA-mPEG nanoparticles of cisplatin: in vitro
nanoparticle degradation, in vitro drug release and in vivo drug residence in
blood properties, J. Control. Release, 79, pp. 123135.
99. Gao, H., Wang, Y.N., Fan, Y.G., Ma, J.B., 2005, Synthesis of a
biodegradable tadpole-shaped polymer via the coupling reaction of poly-
lactide onto mono(6-(2-aminoethyl)amino-6-deoxy)-beta-cyclodextrin
and its properties as the new carrier of protein delivery system, J. Control
Release, 107, pp. 158173.
100. Koo, Y.L., Reddy, G.R., Bhojani, M., Schneider, R., Philbert, M.A., et al.,
2006, Brain cancer diagnosis and therapy with nanoplatforms, Adv. Drug
Deliv. Rev., 58, pp. 15561557.
101. Lee, H., Lee, E., Kim, D.K., Jang, N.K., Jeong, Y.Y., Jon, S., 2006, Antibio-
fouling polymer-coated superparamagnetic iron oxide nanoparticles as
potential magnetic resonance contrast agents for in vivo cancer imaging, J. Am.
Chem. Soc., 128, pp. 73837389.
102. Pinhassi, R.I., Assaraf, Y.G., Farber, S., Stark, M., Ickowicz, D., et al., 2010,
Arabinogalactan-folic acid-drug conjugate for targeted delivery and target-
activated release of anticancer drugs to folate receptor-overexpressing cells,
Biomacromolecules, 11, pp. 294303.
103. Rice, J.R., Gerberich, J.L., Nowotnik, D.P., Howell, S.B., 2006, Preclinical
ecacy and pharmacokinetics of AP5346, a novel diaminocyclohexane-
platinum tumor targeting drug delivery system, Clin. Cancer Res., 1, pp.
22482254.
104. Matsumura, Y., 2008, Poly (amino acid) micelle nanocarriers in preclinical
and clinical studies, Adv. Drug Deliv. Rev., 60, pp. 899914.
105. Homsi, K., Simon, G.R., Garrett, C.R., Springett, G., De Centi, R., 2007,
Phase I trial of poly-L-glutamata comptothecin (CT-2106) administered
weekly in patients with advanced solid malignancies, Clin. Cancer Res., 13,
pp. 58555861.
106. Boddy, A.V., Plummer, E.R., Todd, R., Sludden, J., Grin, M., et al., 2005,
A phase I and pharmacokinetic study of paclitaxel poliglumex (XYOTAX),
investigating both 3-weekly and 2-weekly schedules, Clin. Cancer Res., 11,
pp. 78347840.
107. Savic, R., Eisenberg, A., Maysinger, D., 2006, Block copolymer micelles as
delivery vehicles of hydrophobic drugs: micelle-cell interactions, J. Drug
Target, 14, pp. 343355.
108. Shen, Y., Jiasheng, T., 2009, Synthesis and characterization of low molecular
weight hyaluronic acid-based cationic micelles for ecient siRNA delivery,
Carbohydrate Polym., 77, pp. 95104.
109. Kim, D.W., Kim, S.Y., Kim, H.K., Kim, S.W., Shin, S.W., et al., 2007,
Multicenter phase II trial of Genexol-PM, a novel Cremophor-free, polymeric
micelle formulation of paclitaxel, with cisplatin in patients with advanced non-
small-cell lung cancer, Ann. Oncol., 18, pp. 20092014.
88 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
110. Kenmotsu, H., Yasunaga, M., Goto, K., Nagano, T., Kuroda, J., et al., 2010,
Te antitumor activity of NK012, an SN-38-incorporating micelle, in
combination with bevacizumab against lung cancer xenografts, Cancer, 116,
pp. 45974604.
111. Bey, E.A., Bentle, M.S., Reinicke, K.E., Dong, Y., Yang, C.R., et al., 2007, An
NQO1- and PARP-1-mediated cell death pathway induced in non-small-cell
lung cancer cells by beta-lapachone, Proc. Natl. Acad. Sci. U.S.A., 104, pp.
1183211837.
112. Blanco, E., Bey, E.A., Khemtong, C., Yang, S.G., Setti-Guthi, J., et al., 2010,
Beta-lapachone micellar nanotherapeutics for non-small cell lung cancer
therapy, Cancer Res., 70, pp. 38963904.
113. Khong, T., and Spencer, A., 2011, Targeting heat shock protein 90 induces
apoptosis anf inhibits critical survival and proliferation pathways in multiple
myeloma, Mol. Cancer Ter., 10, pp. 19091917.
114. Richardson, P.G., Ghana-khan, A.A., Alsina, M., Albitar, M., Berman,
D., et al., 2010, Tanespimycin monotherapy in relapsed multiple
myeloma: results of a phase 1 dose-escalation study, Br. J. Haematol., 150,
pp. 438445.
115. Misra, A., Ganesh, S., Shahiwala, A., 2003, Drug delivery to the central
nervous system: a review, J. Pharm. Pharmaceut. Sci., 6, pp. 252273.
116. Needham, D., Anyarambhatla, G., Kong, G., Dewhirst, M.W., 2000,
A new temperature-sensitive liposome for use with mild hyperthermia:
characterization and testing in a human tumor xenograft model, Cancer Res.,
60, pp. 19971201.
117. Vail, D.M., Amantea, M.A., Colbern, G.T., Martin, F.J., Hilger, R.A.,
Working, P.K., 2004, Pegylated liposomal doxorubicin: proof of principle
using preclinical animal models and pharmacokinetic studies, Semin. Oncol.,
31, pp. 1635.
118. Lorusso, D., Ferrandina, G., Lo Voi, R., Fagotti, A., Scambia, G., 2004, Role
of pegylated liposomal doxorubicin (PLD) in epithelial ovarian cancer,
J. Chemother., 4, pp. 98103.
119. Kuesters, G.M., and Campbell, R.B., 2010, Conjugation of bevacizumab to
cationic liposomes enhances their tumor-targeting potential, Nanomedicine,
5, pp. 181192.
120. Zamboni, W.C., 2008, Concept and clinical evaluation of carrier-mediated
anticancer agents, Oncologist, 13, pp. 248260.
121. Ciureda, L., Del Bufalo, D., Desideri, M., Di Sanza, C., Stoppacciaro. A., et
al., 2009, Growth-inhibitory and antiangiogenic activity of the MEK inhibitor
PD0325901 in malignant melanoma with or without BRAF mutations,
Neoplasia, 11, pp. 720731.
122. Kang, S.H., Cho, H.J., Shim, G., Lee, S., Kim, S.H., et al., 2011, Cationic
liposomal co-delivery of small interfering RNA and a MEK inhibitor for
enhanced anticancer ecacy, Pharm. Res., 28, pp. 30693078.
123. Dritschilo, A., Huang, C.H., Rudin, C.M., Marshall, J., Collins, B.,
et al., 2006, Phase I study of liposome-encapsulated c-raf antisense
oligodeoxyribonucleotide infusion in combination with radiation therapy in
patients with advanced malignancies, Clin. Cancer Res., 12, pp. 12511259.
Rrrrnrwcrs 89
124. Ressler, S., Mlineritsch, B., Greil, R., 2011, Zoledronic acid for adjuvant
use in patients with breast cancer, Expert Rev. Anticancer Ther., 11,
pp. 333349.
125. Marra, M., Salzano, G., Leonetti, C., Tassone, P., Scarsella, M., et al., 2011,
Nanotechnologies to use bisphosphonates as potent anticancer agents: the
eects of zoledronic acid encapsulated into liposomes, Nanomedicine, 403,
pp. 292297.
126. Chithrani, B.D., Ghazani, A.A., Chan, W.C., 2006, Determining the size and
shape dependence of gold nanoparticle uptake into mammalian cells, Nano
Lett., 6, pp. 662668.
127. Libutti, S., Paciotti, G., Myer, L., Haynes, R., Gannon, W., et al., 2009, Results
of a completed phase I clinical trial of CYT-6091: a pegylated colloidal gold-
TNF, Nanomedicine, 27, p. 3586.
128. Hirsch, L., Staord, R., Bankson, J., Sershen, S., Rivera, B., et al., 2003,
Nanoshell-mediated near-infrared thermal therapy of tumors under magnetic
resonance guidance, PNAS, 100, pp. 1354913554.
129. Kattumuri, V., Katti, K., Bhaskaran, S., Boote, E.J., Casteel, S.W., et al.,
2007, Gum arabic as a phytochemical construct for the stabilization of gold
nanoparticles: in vivo pharmacokinetics and X-ray-contrast-imaging studies,
Small, 3, pp. 333341.
130. Shi, X., Wang, S., Meshinchi, S., Van Antwerp, M.E., Bi, X., Lee, J., Baker, J.R.,
2007, Dendrimer-entrapped gold nanoparticles as a platform for cancer-cell
targeting and imaging, Small, 3, pp. 12451252.
131. Bhattacharya, R., and Mukherjee, P., 2008, Biological properties of naked
metal nanoparticles, Adv. Drug Deliv. Rev., 60, pp. 12891306.
132. Lara, H.H., Ayala-Nunez, N.V., Ixtepan-Turrent, L., Rodriguez-Padilla,
C., 2010, Mode of antiviral action of silver nanoparticles against HIV-1,
J. Nanobiotechnology, 8:1.
133. Sheikpranbabu, S., Kalishwaralal, K., Venkataraman, D., Eom, S.H., Park, J.,
Gurunathan, S., 2009, Silver nanoparticles inhibit VEGF-and IL-1-induced
vascular permeability via Src dependent pathway in porcine retinal endothelial
cells, J. Nanobiotechnology, 7:8.
134. Sriram, M.I., Kanth, S.B.M., Kalishwaralal, K., Gurunathan, S., 2010,
Antitumor activity of silver nanoparticles in Daltons lymphoma ascites tumor
models, Int. J. Nanomedicine, 5, pp. 753762.
135. Zhang, X., Kono, H., Liu, Z., et al., 2007, A transparent and photo-patternable
superhydrophobic lm, Chem Commun., 46, pp. 49494951.
136. Teron, J., Walker, J.A., Cloete, T.E., 2008, Nanotechnology and water
treatment: applications and emerging opportunities, Crit. Rev. Microbiol., 34,
pp. 4369.
137. Yamaguchi, S., Kobayashi, H., Narita, T., et al., 2010, Novel photodynamic
therapy using water-dispersed TiO2- polyethylene glycol compound: evaluation
of antitumor eect on glioma cells and spheroids in vitro, Photochem
Photobiol., 86, pp. 964971.
138. Seo, J.W., Chung, H., Kim, M.Y., Lee, J., Choi, I.H., Cheon, J., 2007,
Development of water-soluble single-crystalline TiO2 nanoparticles for
photocatalytic cancer-cell treatment, Small, 3, pp. 850853.
90 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
139. Rozhkova, E.A., Ulasov, I., Lai, B., Dimitrijevic, N.M., Lesniak, M.S., Rajh,
T., 2009, A high-performance nanobio phocatalyst for targeted cancer-cell
therapy, Nano Lett., 9, pp. 33373342.
140. Rajh, T., Dimitrijevic, N.M., Rozhkova, E.A., 2011, Titanium dioxide
nanoparticles in advanced imaging and nanotherapeutics, Methods Mol. Biol.,
726, pp. 6375.
141. Lopez, T., Figueras, F., Manjarrez, J., et al., 2010, Catalytic nanomedicine: a
new eld in antitumor treatment using supported platinum nanoparticles. In
vitro DNA degradation and in vivo tests with C6 animal model on Wistar
rats, Eur. J. Med. Chem., 45, pp. 19821990.
142. Dimitrijevic, N.M., Rozhkova, E.A., Rajh, T., 2009, Dynamics of localized
charges in dopamine-modied TiO(2) and their eect on the formation of
reactive oxygen species, J. Am. Chem. Soc., 131, pp. 28932899.
143. Sykova, E., and Jendelova, P., 2005, Magnetic resonance tracking of implanted
adult and embryonic stem cells in injured brain and spinal cord, Ann. N.Y.
Acad. Sci., 1049, pp. 146160.
144. Beg, S., Rizwan, M., Sheick, A.M., hasnain, M.S., Anwer, K., Kohli, K., 2011,
Advancement in carbon nanotubes: basics, biomedical applications and
toxicity, J. Pharm. Pharmacol., 63, pp. 141163.
145. Li, Y., Cousins, B.G., Ulijn, R.V., Kinloch, I.A., 2009, A study of the dynamic
interaction of surfactants with graphite and carbon nanotubes using Fmoc-
aminoacids as a model system, Langmuir, 25, pp. 1176011767.
146. Antonelli, A., Serani, S., Menotta, A., Sfara, C., Pierig, F., et al. 2010,
Improved cellular uptake of functionalized single-walled carbon nanotubes,
Nanotechnology, 21:425101.
147. Salvador-Morales, C., Flahaut, E., Sim, E., Sloan, J., Green, M.L., Sim, R.B.,
2006, Complement activation and protein adsorption by carbon nanotubes,
Mol. Immunol., 43, pp. 193201.
148. Liu, Z., Chen, K., Davis, C., Sherlock, S., Cao, Q., Chen, X., Dai, H., 2008,
Drug delivery with carbon nanotubes for in vivo cancer treatment, Cancer
Res., 68, pp. 66526660.
149. Lay, C.L., Liu, Q.L., Tan, H.R., Liu, Y., 2010, Delivery of paclitaxel by
physically loading onto poly(ethylene glycol)(PEG)-graftcarbon nanotubes for
potent cancer therapeutics, Nanotechnology, 21:065101.
150. Kam, N.W., OConnell, M., Wisdom, J.A., Dai, H., 2005, Carbon nanotubes
as multifunctional biological transporters and near-infrared agents for
selective cancer cell destruction, Proc. Natl. Acad. Sci. U.S.A., 102,
pp. 1160011605.
151. Zhang, Z., Yang, X., Zhang, Y., Zeng, B., Wang, S., et al., 2006, Delivery
of telomerase reverse transcriptase small interfering RNA in complex with
positively charged single walled carbon nanotubes suppresses tumor growth,
Clin. Cancer Res., 12, pp. 49334939.
152. Brennan, M.E., Coleman, J.N., Drury, A., Lahr, B., Kobayashi, T., Blau,
W.J., 2007, Nonlinear photoluminescence from van Hove singularities in
multiwalled carbon nanotubes, Optic Letters, 28, pp. 26542665.
153. Park, E.J., Roh, J., Kim, S.N., Kang, M.S., Han, Y.A., et al., 2011, A single
intratracheal instillation of single-walled carbon nanotubes induced early
Rrrrnrwcrs 91
lung brosis and subchronic tissue damage in mice, Arch. Toxicol., 85,
pp. 11211131.
154. Aillon, K.L., Xie, Y., El-Gendy, N., Berkland, C.J., Forrest, M.L., 2009, Eects
of nanomaterial physicochemical properties on in vivo toxicity, Adv. Drug
Deliv. Rev., 61, pp. 457466.
155. Nasibulin, A.G., Pikhitsa, P.V., Jiang, H., Brown, D.P., Krasheninnikov, A.V.,
et al., 2007, A novel hybrid carbon material Nat. Nanotechnol., 2, pp. 156
161.
156. Yamakoshi, Y., Umezawa, N., Ryu, A., Arakane, K., Miyata, N., et al.,
2003, Active oxygen species generated from photoexcited fullerene (C60)
as potential medicines: O2-*versus 1O2, J. Am. Chem. Soc., 125, pp.
1280312809.
157. Iwamoto, Y., and Yamakoshi, Y., 2006, A highly water-soluble C60-NVP
copolymer: a potential material for photodynamic therapy, Chem. Commun.,
46, pp. 48054807.
158. Liu, J., Ohta, S., Sonoda, A., Yamada, M., Yamamoto, M., et al., 2007,
Preparation of PEG-conjugated fullerene containing Gd3+ ions for photo-
dynamic therapy, J. Control Release, 117, pp. 104110.
159. Zakharian, T.Y., Seryshev, A., Sitharaman, B., Gilbert, B.E., Knight, V., Wilson,
L.J., 2005, A fullerene-paclitaxel chemotherapeutic: synthesis, characterization,
and study of biological activity in tissue culture, J. Am. Chem. Soc., 127, pp.
1250812509.
160. Abes, S., Ivanova, G.D., Abes, R., Arzumanov, A.A., Williams, D., et al., 2009,
Peptide-based delivery of steric-block PNA oligonucleotides, Methods Mol.
Biol., 480, pp. 8599.
161. Chanda, N., Kattamuri, V., Shukla, V., Zambre, A., Katti, K., et al., 2010,
Bombesin functionalized gold nanoparticles show in vitro and in vivo cancer
receptor specicity, Proc. Natl. Acad. Sci. U.S.A., 107, pp. 87608765.
162. Chen, X., Wang, X., Wang, Y., Yang, L., Hu, J., et al., 2010, Improved tumor-
targeting drug delivery and therapeutic ecacy by cationic liposome modied
with truncated bFGF peptide, J. Control. Release, 145, pp. 1725.
163. Desai, A., Vyas, T., Amiji, M., 2008, Cytotoxicity and apoptosis enhancement
in brain tumor cells upon coadministration of paclitaxel and ceramide in
nanoemulsion formulations, J. Pharm. Sci., 97, pp. 27452756.
164. Pan, H., Soman, N.R., Schlesinger, P.H., Lanza, G.M., Wickline, S.A., 2009,
Cytolitic peptides nanoparticles (NanoBees) for cancer therapy, Wires
Nanomed. Nanobiotechnol., 3, pp. 318327.
165. Choi, J., Burns, A.A., Williams, R.M., Zhou, Z., Flesken-Nikitin, A., et al.,
2007, Core-shell silica nanoparticles as uorescent labels for nanomedicine,
J. Biomed. Opt., 12, 064007.
166. He, X.X., Duan, J.H., Wang, K.M., Tan, W.H., Lin, X., He, C.M., 2004, A
novel fluorescent label based on organic dye-doped silica nanoparticles for
HepG liver cancer cell recognition, J. Nanosci. Nanotechnol., 4, pp. 585
589.
167. Santra, S., Liesenfeld, B., Dutta, D., Chatel, D., Batich, C.D., 2005, Folate
conjugated uorescent silica nanoparticles for labeling neoplastic cells,
J. Nanosci. Nanotechnol., 5, pp. 899904.
92 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
168. Santra, S., Yang, H., Dutta, D., Stanley, J.T., Holloway, P.H., 2004, TAT
conjugated FITC doped silica nanoparticles for bioimaging applications,
Chem. Commun., pp. 28102811.
169. Smith, J.E., Medley, C.D., Tang, Z.W., Shangguan, D.H., Lofton, C., Tan, W.H.,
2007, Aptamer-conjugated nanoparticles for the collection and detection of
multiple cancer cells, Anal. Chem., 79, pp. 30753082.
170. Wang, L., Lofton, C., Popp, M., Tan, W.H., 2007, Using luminescent
nanoparticles as staining probes for Aymetrix GeneChips, Bioconjugate
Chem., 18, pp. 610613.
171. Ravi Kumar, M.N.V., Sameti, M., Mohapatra, S.S., Kong, X., Lockey, R.F.,
et al., 2004, Cationic silica nanoparticles as gene carriers: Synthesis, charac-
terization and transfection eciency in vitro & in vivo, J. Nanosci. Nano-
technol., 4, pp. 876881.
172. Jin, S., and Ye, K.M., 2007, Nanoparticle-mediated drug delivery and gene
therapy, Biotechnol. Prog., 23, pp. 3241.
173. Gao, X., Chung, L.W., Nie, S., 2007, Quantum dots for in vivo molecules and
cellular imaging, Methods Mol. Biol., 374, pp. 135145.
174. Bakalgot, V., Zhang, L., Levy-Nissembaum, E., Jon, S., Kantoff, P.V.,
Langer, R., Farokhzad, O.C., 2007, Quantum Dot-Aptamer conjugates
for synchronous cancer imaging, therapy and sensing of drug delivery
based on bi-fluorescence resonance energy transfer, Nano Lett., 7,
pp. 30653070.
175. Tan, W.B., Jiang, S., Zhang, Y., 2007, Quantum-dot based nanoparticles for
targeted silencing of HER2/neu gene via RNA interference, Biomaterials, 28,
pp. 15651571.
176. Tekade, R.K., Kumar, P.V., Jain, N.K., 2009, Dendrimers in oncology: an
expanding horizon, Chem. Rev., 109, pp. 4987.
177. Bharali, D.J., Khalil, M., Gurbuz, M., Simone, T.M., Mousa, S.A., 2009,
Nanoparticles and cancer therapy: a concise review with emphasis on
dendrimers, Int. J. Nanomedicine, 4, pp. 17.
178. Majoros, I.J., Myc, A., Tomas, T., Mehta, C.B., Baker, J.R. Jr., 2006,
PAMAM dendrimer-based multifunctional conjugate for cancer therapy:
synthesis, characterization, and functionality, Biomacromolecules, 7, pp. 572
579.
179. Desai, P.N., Yuan, Q., Yang, H., 2010, Synthesis and characterization of
photocurable polyamidoamine dendrimer hydrogels as a versatile platform
for tissue engineering and drug delivery, Biomacromolecules, 11, pp. 666
673.
180. Ke, W.L., Shao, K., Huang, R.Q., Han, L., Liu, Y., et al., 2009, Gene delivery
targeted to brain using an Angiopep-conjugated polyethyleneglycol-modied
polyamidoamine dendrimer, Biomaterials, 30, pp. 69766985.
181. Agrawal, A., Min, D.H., Singh, N., Zhu, H., Birjiniuk, A., et al., 2009,
Functional delivery of siRNA in mice using dendriworms, ACS Nano, 3,
pp. 24952504.
182. Yang, W., Barth, R.F., Wu, G., Huo, T., Tjarks, W., et al., 2009, Convection
enhanced delivery of boronated EGF as a molecular targeting agent for
neutron capture therapy of brain tumors, J. Neurooncol., 95, pp. 355365.
Rrrrnrwcrs 93
183. Zhang, L., Zhu, S., Qian, L., Pei, Y., Qiu, Y., Jiang, Y., 2011, RGD-modied
PEG-PANAM-DOX conjugates: in vitro and in vivo studies for glioma, Eur.
J. Pharm. Biopharm., 79, pp. 232240.
184. Klajnert, B., and Bryszewska, M., 2001, Dendrimers: properties and
applications, Acta Biochim. Pol., 48, pp. 199208.
185. Bernardi, R.J., Lowery, A.R., Tompson, P.A., Blaney, S.M., West, J.L., 2008,
Immunonanoshells for targeted photothermal ablation in medulloblastoma
and glioma: an in vitro evaluation using human cell lines, J. Neurooncol., 86,
pp. 165172.
186. Wang, C., Huang, Y., Peng, C., 2009, Photothermal ablation of stem-cell
like glioblastoma using carbon nanotubes functionalized with anti-CD133,
ICBME Proceedings, 23, pp. 888891.
187. Madhankumar, A.B., Slage-Webb, B., Mintz, A., Sheehan, J.M., Connor, J.R.,
2006, Interleukin-13 receptor-targeted nanovesicles are a potential therapy
for glioblastoma multiforme, Mol. Cancer. Ter., 5, pp. 31623169.
188. Lu, W., Sun, Q., Wan, J., She, Z., Jiang, X., 2006, Cationic albumin-conjugated
pegylated Nanoparticles allow gene delivery into brain tumors via intravenous
administration, Cancer Res., 66, pp. 1187811886.
189. Bernardi, A., Braganhol, E., Jager, E., et al., 2009, Indomethacin-loaded
nanocapsules treatment reduces in vivo glioblastoma growth in a rat glioma
model, Cancer Lett., 281, pp. 5363.
190. Wang, X., Pang, Y., Ku, G., Xie, X., Stoica, G., Wang, L.W., 2003, Noninvasive
laser-induced photoacoustic tomography for structural and functional in vivo
imaging of the brain, Nat. Biotechnol., 21, pp. 803806.
191. Pan, D., Pramanik, M., Senpan, A., et al., 2011, Molecular photoacoustic
imaging of angiogenesis with integrin-targeted gold nanobeacons, Faseb. J.,
25, pp. 875882.
192. Li, M., Oh, J., Xie, X., et al., 2008, Simultaneous molecular and hypoxia
imaging of brain tumors in vivo using spectroscopic photoacoustic tomography,
Proceedings IEEE, 96, pp. 481489.
193. Wang, Y., Xie, X., Wang, X., et al., 2004, Photoacoustic tomography of a nanoshell
contrast agent in the in vivo rat brain, Nano Lett., 4, pp. 16891692.
194. Chertok, B., David, A.E., Huang, Y., Yang, V.C., 2007, Glioma selectivity of
magnetically targeted Nanoparticles: a role of abnormal tumor hydrodynamics,
J. Control Release, 122, pp. 315323.
195. Schneider, T., Becker, A., Ringe, K., Reinhold, A., Firsching, R., et al., 2008,
Brain tumor therapy by combined vaccination and antisense oligonucleotide
delivery with nanoparticles, J Neuroimmunol., 195, pp. 2127.
196. Wu, Z.M., Yuan, X.H., Jiang, P.C., Li, Z.Q., Wu, T., 2006, Antisense
oligonucleodes targeting the focal adhesion kinase inhibit proliferation, induce
apoptosis and cooperate with cytotoxic drugs in human glioma cells, J. Neuro.-
Oncol., 77, pp. 117123.
197. Chang, S.M., Kuhn, J.G., Robins, H.I., Schold, S.C. Jr., Spence, A.M., et al.,
2001, A phase II study of paclitaxel in patients with recurrent malignant
glioma using dierent doses depending upon the concomitant use of
anticonvulsants: a North American brain tumor consortium report, Cancer,
91, pp. 417422.
94 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
198. Xin, H., Chen, L., Gu, J., Ren, X., Wei, Z., et al., 2010, Enhanced anti-
glioblastoma ecacy by PTX-loaded PEGylated poly(-caprolactone) nano-
particles: In vitro and in vivo evaluation, Int. J. Pharmacol., 402, pp. 238
247.
199. Xin, H., Jiang, X., Gu, J., Sha, X., Chen, L., et al., 2011, Angiopep-conjugated
poly(ethylene glycol)-co-poly(e-caprolactone) nanoparticles as dual-targeting
drug delivery system for brain glioma, Biomaterials, 32, pp. 42934305.
200. Chien, A.J., Illi, J.A., Ko, A.H., Korn, W.H., Fong, L., et al., 2009, A phase I
study of a 2-day lapatinib chemosensitization pulse preceding Nanoparticle
albumin-bound Paclitaxlel for advanced solid malignancies, Clin. Cancer Res.,
15, pp. 55695575.
201. Caruso, G., Cao, M., Raudino, G., Alafaci, C., Tomasello, F., 2010, New
Terapeutic Strategies in Gliomas Treatment, in Brain Tumors - Current
and Emerging Terapeutic Strategies, A.L. Abujamra, ed., InTech., Rijeka.,
pp. 281306.
202. Huynh, G.H., Deen, D.F., Szoka Jr., F.C., 2006, Barriers to carrier mediated
drug and gene delivery to brain tumors, J. Control Release, 110, pp. 236
259.
203. Abe, T., Wakimoto, H., Bookstein, R., Maneval, D.C., Chiocca, E.A., Basilion,
J.P., 2002, Intra-arterial delivery of p53-containing adenoviral vector into
experimental brain tumors, Cancer Gene Ter., 9, pp. 228235.
204. Ali, J., Ali, M., Baboota, S., Sahani, J.K., Ramassamy, C., et al., 2010, Poten tial
of nanoparticulate drug delivery systems by intranasal administration, Curr.
Pharm. Des., 16, pp. 16441653.
205. da Cruz, M.T., Simoes, S., de Lima, M.C., 2004, Improving lipoplex-mediated
gene transfer into C6 glioma cells and primary neurons, Exp. Neurol., 187,
pp. 6575.
206. Ulbrich, K., Hekmatara, T., Herbert, E., Kreuter, J., 2009, Transferrin- and
transferrinreceptor-antibody-modied nanoparticles enable drug delivery
across the bloodbrain barrier (BBB), Eur. J. Pharm. Biopharm., 71,
pp. 251256.
207. van Rooy, I., Mastrobattista, E., Storm, G., W.E. Hennink, W.E., Schielers, R.M.,
2011, Comparison of ve dierent targeting ligands to enhance accumulation of
liposomes into the brain, J. Control Release, 150, pp. 3036.
208. Boado, RJ., Zhang, Y., Pardridge, W.M., 2007, Humanization of anti-human
insulin receptor antibody for drug targeting across the human bloodbrain
barrier, Biotechnol. Bioeng., 96, pp. 381391.
209. Hu, K., Shi, Y., Jiang, W., Han, J., Huang, S., Jiang, X., 2011, Lactoferrin
conjugated PEGPLGA nanoparticles for brain delivery: preparation,
characterization and ecacy in Parkinsons disease, Int. J. Pharm., 415,
pp. 273283.
210. Tosi, G., Vergoni, A.V., Ruozi, B.Z., Bondioli, Z., Badiali, L., et al., 2010,
Sialic acid and glycopeptides conjugated PLGA nanoparticles for central
nervous system targeting: in vivo pharmacological evidence and bio distribution,
J. Control Release, 145, pp. 4957.
211. Adenot, M., Merida, P., Lahana, R., 2007, Applications of a bloodbrain
barrier technology platform to predict CNS penetration of various chemo-
Rrrrnrwcrs 95
therapeutic agents. 2. Cationic peptide vectors for brain delivery, Chemotherapy,
53, pp. 7376.
212. Rapoport, N., Marin, A.P., Timoshin, A.A., 2000, Eect of a polymeric
surfactant on electron transport in HL-60 cells, Arch. Biochem. Biophys.,
384, pp. 100108.
213. Santra, S., Yang, H., Holloway, P.H., Stanley, J.T., Mericle, R.A., 2005,
Synthesis of waterdispersible uorescent, radio-opaque, and paramagnetic
CdS:Mn/ZnS quantum dots: a multifunctional probe for bioimaging, J. Am.
Chem. Soc., 127, pp. 16561657.
214. Liu, L., Venkatraman, S.S., Yang, Y.Y., Guo, K., Lu, J. et al., 2008, Polymeric
micelles anchored with TAT for delivery of antibiotics across the bloodbrain
barrier, Biopolymers, 90, pp. 617623.
215. Qin, Y., Chen, H., Yuan, W., Kuai, R., Zhang, Q., et al., 2011, Liposome
formulated with TAT-modied cholesterol for enhancing the brain delivery,
Int. J. Pharm., 420, pp. 304312.
216. Kabanov, A.V., Batrakova, E.V., Miller, D.V., 2003, Pluronic block copoly mers
as modulators of drug eux transporter activity in the bloodbrain barrier,
Adv. Drug Deliv. Rev., 55, pp. 151164.
217. Batrakova, E.V., Li, S., Alakhov, V.Y., Elmquist, W.F., Miller, D.W., Kabanov,
A.V., 2003, Sensitization of cells overexpressing multidrug resistant protein
by Pluronic P85, Pharm. Res., 20, pp. 15811590.
218. Qin, J., Chen, D., Hu, H., Cui, Q., Qiao, M., Chen, B., 2007, Surface
modication of RGDliposomes for selective drug delivery to monocytes/
neutrophils in brain, Chem. Pharm. Bull., 55, pp. 11921197.
219. Panyam, J., and Labhasetwar, V., 2003, Dynamics of endocytosis and
exocytosis of poly(D, Llactide-co-glycolide) nanoparticles in vascular smooth
muscle cells, Pharm. Res., 20, pp. 212220.
220. Begley, D.J., 2004, Delivery of therapeutic agents to the central nervous
system: the problems and the possibilities, Pharmacol. Ter., 104, pp. 2945.
221. Schulze, C., Smales, C., Rubin, L.L., Staddon, J.M., 1997, Lysophosphatidic
acid increases tight junction permeability in cultured brain endothelial cells, J.
Neurochem., 68, pp. 9911000.
222. Monnaert, V., Betbeder, D., Fenart, L., Bricout, H., Lenfant, A.M., et al., 2004,
Eects of gamma- and hydroxypropyl-gamma-cyclodextrins on the transport
of doxorubicin across an in vitro model of bloodbrain barrier, J. Pharmacol.
Exp. Ter, 311, pp. 11151120.
223. Tilloy, S., Monnaert, V., Fenart, L., Bricout, H., Cecchelli, R., Monier, E.,
2006, Methylated beta-cyclodextrin as P-gp modulators for deliverance of
doxorubicin across an in vitro model of bloodbrain barrier, Bioorg. Med.
Chem. Lett., 16, pp. 21542157.
224. Mackic, J.B., Stins, M., Jovanovic, S., Kim, K.S., Bartus, R.T., Zlokovic,
B.V., 1999, Cereport (RMP-7) increases the permeability of human brain
microvascular endothelial cell monolayers, Pharm. Res., 16, pp. 13601365.
225. Emerich, D.F., Snodgrass, P., Dean, R., Agostino, M., Hasler, B., et al., 1999,
Enhanced delivery of carboplatin into brain tumours with intravenous
Cereport (RMP-7): dramatic dierences and insight gained from dosing
parameters, Br. J. Cancer, 80, pp. 964970.
96 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
226. Zhang, X., Xie, Y., Jin, Y., Hou, X., Ye, L., Lou, J., 2004, Te eect of RMP-7
and its derivative on transporting Evans blue liposomes into the brain, Drug
Deliv., 11, pp. 301309.
227. Karyekar, C.S., Fasano, A., Raje, S., Lu, R., Dowling, T.C., Eddington, N.D.,
2003, Zonula occludens toxin increases the permeability of molecular weight
markers and chemotherapeutic agents across the bovine brain microvessel
endothelial cells, J. Pharm. Sci., 92, pp. 414423.
228. Dallasta, L.M., Pisarov, L.M., Esplen, L.A., Werley, J.V., Moses, A.V., et al.,
1999, Bloodbrain barrier tight junction disruption in human immu-
nodeciency virus-1 encephalitis, Am. J. Pathol., 155, pp. 19151927.
229. Hynynen, K., McDannold,N., Vykhodtseva, N., Jolesz, F.A., 2001,
Noninvasive MR imaging-guided focal opening of the bloodbrain barrier in
rabbits, Radiology, 220, pp. 640646.
230. McDannold, N., Vykhodtseva, N., Hynynen, K., 2004, Use of ultrasound
pulses combined with denity for targeted bloodbrain barrier disruption: a
feasibility study, Ultrasound Med. Biol., 33, pp. 584590.
231. Sheikov, N. McDannold, N. Vykhodtseva, N., Jolesz, F., Hynynen, K.,
2004, Cellular mechanisms of the bloodbrain barrier opening induced
by ultrasound in presence of microbubbles, Ultrasound Med. Biol., 30,
pp. 979989.
232. Treat, L.H., McDannold, N. Vykhodtseva, N., Zhang, Y., Tam, K. Hynynen,
K., 2007, Targeted delivery of doxorubicin to the rat brain at therapeutic
levels using MRI-guided focused ultrasound, Int. J. Cancer, 121, pp. 901
907.
233. Maclean, A.G., Belenchia, G.E., Bieniemy, D.N., Moroney-Rasmussen, T.A.,
Lackner, A.A., 2005, Simian immunodeciency virus disrupts extended
lengths of the blood-brain barrier, J. Med. Primatol., 34, pp. 237242.
234. Pandit, J.K., Singh, S., Muthu, M.S., 2006, Controlled release formulations in
neurology practice, Ann. Indian Acad. Neurol., 9, pp. 207216.
235. Takur, A., Gahane, A., Bhadoriya, S.S., Jain, S.K., Jain, R., Mishra, H., 2011,
Major hurdles for brain tumor therapy and the ways to overcome them: A
review, J. Pharmacy Res., 4, pp. 13151318.
236. Bobo, R.H., Douglas, W., Akbasak, A., Morrison, P.F., Dedrick, R.L., Oldeld,
E.H., 1994, Convection-enhanced delivery of macromolecules in the brain,
Proc. Natl. Acad. Sci. U.S.A., 91, pp. 20762080.
237. Attenello, F.J., Mukherjee, D., Datoo, G., McGirt, M.J., Bohan, et al., 2008,
Use of Gliadel (BCNU) wafer in the surgical treatment of malignant
glioma: a 10-year institutional experience, Ann. Surg. Oncol., 15, pp. 2887
2893.
238. Brem, H., Piantadosi, S., Burger, P.C., Walker, M., Selker, R., Bick, N.A., 1995,
Placebo controlled trial of safety and ecacy of intraoperative controlled
delivery by biodegradable polymers for recurrent gliomas, Lancet, 345,
pp. 10081012.
239. Westphal, M., Hilt, D.C., Bortey, E., Delavault, P., Olivares, R., et al., 2003,
A phase 3 trial of local chemotherapy with biodegradable carmustine (BCNU)
wafers (Gliadel wafers) in patients with primary malignant gliomas, Neuro.-
Oncol., 5, pp. 7988.
Rrrrnrwcrs 97
240. Pavan, B., Dalpiaz, A., Ciliberti, N., Biondi, C., Manfredini, S., Vertuani, S.,
2008, Progress in drug delivery to the central nervous system by the prodrug
approach, Molecules, 13, pp. 10351065.
241. Nair, B.G., Varghese, S.H., Nair, R., Yoshida, Y., Maekawa, T., Kumar, D.S.,
2011, Nanotechnology platforms; an innovative approach to brain tumor
therapy, Med. Chem., 7, pp. 488503.
242. Collins, K.L., orringer, D.A., Patil, P.G., 2010, Nanotechnology in
neurosurgery, J. Nanotechnol. Eng. Med., 1, pp. 115.
243. Cao, M., Caruso, G., Barresi, V., Pino, M.A., Venza, M., et al., 2012,
Immunohistochemical study of CD68 and CR3/43 in astrocytic gliomas, J.
Anal. Oncol., 1, pp. 4249.
244. Raudino, G., Cao, M., Caruso, G., Alafaci, C., Tomasello, F., 2011,
Nanoparticle-based cerebral drug delivery systems and antiangiogenic
approach in gliomas treatment, Rec. Pat. Nanotech., 5, pp. 239244.
245. Wang, Y., Luang, L., 2012; Multifunctional theranostic nanoparticles for brain
tumors, Mol. Ter., 20, p. 1.
246. Im, S.A., Gomez-Manzano, C., Fueyo, J., et al., 1999, Antiangiogenesis
treatment for gliomas: Transfer of antisense-vascular endothelial growth
factor inhibits tumor growth in vivo, Cancer Res., 59, pp. 895900.
247. Agemy, L., Friedmann-Morvinski, D., Kotamraju, V.R., Roth, L., Sugahara,
K.N., et al., 2011, Targeted nanoparticle enhanced proapoptotic peptide as
potential therapy for glioblastoma, PNAS, 42, pp. 1745017455.
248. Sawyer, A.J., Saucier-Sawyer, J.K., Booth, C.J., Liu, J., Patel, T., Piepmeier,
J.M., Saltzman, W.M., 2011, Convection-enhanced delivery of camptothecin-
loaded polymer nanoparticles for treatment of intracranial tumors, Drug.
Deliv. Transl. Res., 1, pp. 3442.
249. Hadjipanayis, C.G., Machaidze, R., Kaluzova, M., Wang, L., Schuette, A.J.,
et al., 2010, EGFRvIII antibody conjugated iron oxide nanoparticles for MRI
guided convection-enhanced delivery and targeted therapy of glioblastoma,
Cancer Res., 70, pp. 63036312.
250. Kim, T., Jeong, Y., Jin, S., Pei, J., Jung, T., et al., 2011, Preparation of polylactide-
co-glycolide nanoparticles incorporating celecoxib and their antitumor activity
against brain tumor cells, Int. J. Nanomed., 6, pp. 26212631.
251. Lim, K.J., Bisht, S., Bar, E.E., Maitra, A., Eberhart, C.G., 2011, A polymeric
nanoparticle formulation of curcumin inhibits growth, clonogenicity
and stem-like fraction in malignant brain tumors, Cancer Biol. Ter., 11,
pp. 464473.
252. Ding, H., Inoue, S., Ljubimov, A.V., Patil, R., Portilla-Arias, J., et al.,
2010, Inhibition of brain tumor growth by intravenous poly(b-L-malic
acid) nanobioconjugate with pH-dependent drug release, PNAS, 107,
pp. 1814318148.
253. Jung, J., Solanki, A., Memoli, K.A., Kamei, K., Kim, H., et al., 2010, Selective
inhibition of human brain tumor cell proliferation via multifunctional quantum
dot-based siRNA delivery, Angew Chem. Int. Ed. Engl., 49, pp. 103107.
254. Zhao, D., Alizadeh, D., Zhang, L., Liu, W., Farrukh, O., et al., 2011, Carbon
nanotubes enhance CpG uptake and potentiate antiglioma immunity, Clin.
Cancer Res., 17, pp. 771782.
98 Nzwovznrrcrrs zwn Bnzrw Tuon Tnrzrrwr
255. Alizadeh, D., Zhang, L., Hwang, J., Schluep, T., Badie, B., 2010, Tumor-
associated macrophages are predominant carriers of cyclodextrin-based
nanoparticles into gliomas, Manomedicine, 6, pp. 382390.
256. Tian, X., Lin, X., Wei, F., Feng, W., Huang, Z., et al., 2011, Enhanced brain
targeting of temozolomide in polysorbate-80 coated polybutylcyanoacrylate
nanoparticles, Int. J. Nanomed., 6, pp. 445452.
257. Steiniger, S.C.J., Kreuter, J., Khalansky, A.S., Skidan, I.N., Bobruskin, A.I.,
et al., 2004, Chemotherapy of glioblastoma in rats using doxorubicin-loaded
nanoparticles, Int. J. Cancer, 109, pp. 759767.
258. Orringer, D.A., Koo, Y., Kopelman, R., Sagher, O., 2009, Small solutions for
big problems: the application of nanoparticles to brain tumor diagnosis and
therapy, Clin. Pharmacol. Ter., 85, pp. 531534.
259. Zara, G.P., Cavalli, R., Bargoni, A., Fundar, A., Vighetto, D., 2002,
Intravenous administration to rabbits of non-stealth and stealth doxorubicin-
loaded solid lipid nanoparticles at increasing concentrations of stealth agent:
pharmacokinetics and distribution of doxorubicin in brain and other tissues,
J. Drug Target., 10, pp. 327335.
260. Kuroda, J., Kuratsu, J., Yasunaga, M., 2009, Potent antitumor eect of SN-
38-incorporating polymeric micelle, NK012, against malignant glioma, Int. J.
Cancer, 124, pp. 25052511.
261. Ljubimova, J.Y., Fujita, M., Khazenzon, N.M., Lee, B.S., Wachsmann-Hogiu,
S., et al., 2008, Nanoconjugate based on polymalic acid for tumor targeting,
Chem. Biol. Interact., 171, pp. 195203.
262. Chertok, B., David, A.E., Yang, V.C., 2010, Polyethyleneimine-modied iron
oxide nanoparticles for brain tumor drug delivery using magnetic targeting and
intra-carotid administration, Biomaterials, 31, pp. 63176324.
263. Etame, A.B., Diaz, R.J., OReilly, M.A., Smith, C.A., Mainprize, T.G., et al.,
2012, Enhanced delivery of gold nanoparticles with therapeutical potential
into the brain using MRI-guided focused ultrasound, Nanomedicine, (in
press).
264. Yukawa, H., Mizufune, S., Mamori, C., Kagami, Y., Oishi, K., et al., 2009,
Quantum dots for labeling adipose tissue-derived stem cells, Cell Transplant.,
18, pp. 591599.
265. Yang, F., Cho, S.W., Son, S.M., Bogatyrev, S.R., Singh, D., et al., 2010,
Genetic engineering of human stem cells for enhanced angiogenesis using
biodegradable polymeric nanoparticles, Proc. Natl. Acad. Sci. U.S.A., 107,
pp. 33173322.
266. Caruso, G., Cao, M., Raudino, G., Tomasello, C., Alafaci, C., Tomasello, F., 2012,
Nanomedicine and Brain Tumors Treatment, in Patenting Nanomedicines.
Legal Aspects, Intellectual Property and Grant Opportunities, E.B. Souto, ed.,
Springer Verlag, Berlin Heidelberg, pp. 167204.
267. Shubayev, V.I., Pisanic II, T.R., Jin, S., 2009, Magnetic nanoparticles for
theragnostics, Adv. Drug Deliv. Rev., 61, pp. 467477.
268. Wankhede, M., Bouras, A., Kaluzova, M., Hadjipanayis, C.G., 2012,
Magnetic nanoparticles: an emerging technology for malignant brain tumor
imaging and therapy, Exp. Rev. Clin. Pharmacol., 5, pp. 173186.
Rrrrnrwcrs 99
269. Caruso, G., Cao, M., Raudino, G., Raudino, F., Venza, M., Tomasello, F.,
2012, Antisense Oligonucleotides in the Treatment of Malignant Gliomas,
in From Nucleic Acid Sequences to Molecular Medicine, RNA Technologies,
V.A. Erdmann and J. Barciszewski, eds., Springer Verlag, Berlin Heidelberg,
pp. 215246.
Gerardo Caruso, MD (University of Messina, School Medicine, 1990) is
currently an Assistant Neurosurgeon, Neurosurgical Clinic, University of
Messina, Italy. He has been a Member of the Italian Society of Neurosurgery
since 1996 and a Member of the American Nanosociety since 2011.
Dr. Caruso previously served as an ocer in the Italian Navy and has also
served as a reviewer for a number of international technical journals.
Maria Cao, MD (University of Messina, School Medicine, 1994) is
currently an Assistant Neurosurgeon, Neurosurgical Clinic, University of
Messina, Italy. She has been a Member of the Italian Society of Neurosurgery
since 2000, a Member of the Italian Association of Neuro-oncology since 2000,
and a Member of the European Association of Neuro-oncology since 2002.
Dr. Cao has PhD in Neurooncology. Dr. Cao is also Assistant Professor,
Department of Neuroscience, Neurosurgical Clinic, University of Messina,
Italy, and a reviewer for several technical journals.
Giuseppe Raudino, MD (University of Catania, School of Medicine,
2005) is currently a Neurosurgeon at Villa Salus, Clinic, Department
of Neurosurgery, Augusta (SR), Italy. He is also a level II Post-Residency
Master in Molecular Diagnosis and Translational Medicine, completing
nal work regarding angiogenesis and functional genomics of high-grade
gliomas.
Francesco Tomasello, MD (University of Messina, School Medicine, 1970)
was most recently Dean of the Faculty of Medicine, University of Messina,
Italy, until 2004. Previously he was Director, Residency in Neurosurgery
Program, Neurosurgical Clinic, University of Messina Medical School.
In 2004, Professor Tomasello was President of the Italian Society of
Neurosurgery. From 19951999, he was Vice-President of the European
Association of Neurosurgical Societies (EANS). Professor Tomasello was
also a consultant to the Italian Ministry of Health in 2003, and in 2004 was
elected a member of the Congress of Neurological Surgeons (USA).
Anda mungkin juga menyukai
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5795)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Presentation 1Dokumen36 halamanPresentation 1Alice Chews IceBelum ada peringkat
- Biochemistry of AgingDokumen2 halamanBiochemistry of AgingKaedehara KazuhaBelum ada peringkat
- Pain PhysiologyDokumen40 halamanPain PhysiologyAnmol Jain100% (1)
- EclampsiaDokumen8 halamanEclampsiaKristine Castillo100% (1)
- NCP - JaundiceDokumen5 halamanNCP - JaundiceQueen Shine0% (1)
- TASK 1.6 MonologueDokumen5 halamanTASK 1.6 MonologueLore HernandezBelum ada peringkat
- ORE - UK Dental Reference BooksDokumen4 halamanORE - UK Dental Reference BooksKisshore ReddyBelum ada peringkat
- MCQDokumen20 halamanMCQanuj sharma100% (2)
- Polymerase Chain ReactionDokumen19 halamanPolymerase Chain ReactionKamila Haidari100% (1)
- Neutrophil EbookDokumen468 halamanNeutrophil EbookNathália LuísaBelum ada peringkat
- Antidepressants in Pregnancy4 2016Dokumen60 halamanAntidepressants in Pregnancy4 2016هناء همة العلياBelum ada peringkat
- GE IV TH SemDokumen185 halamanGE IV TH Semrahul vivekBelum ada peringkat
- Melanocytes - MelaninDokumen27 halamanMelanocytes - MelaninJanelleBelum ada peringkat
- Children With DisabilitiesDokumen644 halamanChildren With DisabilitiesNeurodesarrollo Infantil100% (2)
- Biomolecules 11 01176 v2Dokumen24 halamanBiomolecules 11 01176 v2Soumam DuttaBelum ada peringkat
- Case Study Genome Edited Human EmbryosDokumen2 halamanCase Study Genome Edited Human EmbryosDivya Dharshini RBelum ada peringkat
- Sturge Weber Syndrome Case Report StudyDokumen11 halamanSturge Weber Syndrome Case Report StudyOphtalmology100% (3)
- Tmp1a96 TMPDokumen80 halamanTmp1a96 TMPFrontiersBelum ada peringkat
- Datasheet of IU1 - CAS 314245-33-5Dokumen2 halamanDatasheet of IU1 - CAS 314245-33-5LouisBelum ada peringkat
- Joseph MerrickDokumen12 halamanJoseph Merrickyairherrera100% (1)
- Hepa B TestDokumen1 halamanHepa B TestsmilingfroggyBelum ada peringkat
- snc2d Biology Unit TestDokumen6 halamansnc2d Biology Unit Testapi-3078129790% (3)
- Immunology and Immunochemistry 1-1Dokumen70 halamanImmunology and Immunochemistry 1-1Afram MaxwellBelum ada peringkat
- Immunology Serology in Laboratory Medicine 5th Edition Turgeon Test BankDokumen9 halamanImmunology Serology in Laboratory Medicine 5th Edition Turgeon Test Bankconalguineveree6o100% (28)
- Pathoma ChecklistDokumen3 halamanPathoma ChecklistChimpBelum ada peringkat
- Lab2 Supplemental HardyWeinbergGuide QuestionsDokumen4 halamanLab2 Supplemental HardyWeinbergGuide QuestionsFelisha0% (1)
- Equilibrium: Application To Drug Design: Nature BiotechnologyDokumen5 halamanEquilibrium: Application To Drug Design: Nature BiotechnologysgybleeBelum ada peringkat
- Inflammatory Bowel DiseaseDokumen27 halamanInflammatory Bowel DiseaseMihai VladescuBelum ada peringkat
- Approach To Skin Adnexal TumorsDokumen20 halamanApproach To Skin Adnexal TumorsNirmalya Chakrabarti100% (1)
- Cell and Organs of The Immune SystemDokumen43 halamanCell and Organs of The Immune Systemcyrhenmie100% (1)