Obesity and Functional Constipation A Community-Based Study in Iran
Diunggah oleh
Moa ClauDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Obesity and Functional Constipation A Community-Based Study in Iran
Diunggah oleh
Moa ClauHak Cipta:
Format Tersedia
Obesity and Functional Constipation; a Community-Based
Study in Iran
Mohamad Amin Pourhoseingholi, Seyed Ali Kaboli, Asma Pourhoseingholi, Bijan Moghimi-Dehkordi, Azadeh Safaee,
Babak Khoshkrood Mansoori, Manijeh Habibi, Mohammad Reza Zali
Research Center of Gastroenterology and Liver Diseases, Shahid Beheshti University (M.C.), Tehran, Iran
Abstract
Background: Many factors have been linked to the
occurrence of constipation, but few studies exist regarding
the link between obesity and constipation. The aim of this
study was to assess the association between body mass index
(BMI) and functional constipation in the Iranian community.
Methods: From May 2006 to December 2007, a cross
sectional study was conducted in the Tehran province and a
total of 18,180 adult persons were drawn up randomly. One
questionnaire was lled in two stages through interviews. In
the rst part, personal characteristics and 11 gastrointestinal
symptoms were listed. Those who reported at least one of
these 11 symptoms were referred for the second interview.
The second part of the questionnaire consisted of questions
about different gastrointestinal disorders based on the Rome
III criteria including functional constipation. Results: 459
adult persons were found to have functional constipation. The
meanSD of BMI was 26.54.7 and 60% of the patients had
a BMI more than 25. Age and education were signicantly
associated factors with obesity, showing that older patients
and less educated patients were more overweight and obese.
Smoking, marital status and sex were not signicantly
associated with obesity but, up to 60% of low educated
women who had functional constipation, had a BMI more
than 25. Conclusions: Our study showed that about 60% of
patients with functional constipation were overweight, which
was more than the mean of our community. In addition there
may be an association between higher BMI level and the low
education level with constipation in Iranian women.
Key words
Obesity functional constipation Iranian community
Received: 23.09.2008 Accepted: 14.11.2008
J Gastrointestin Liver Dis
June 2009 Vol.18 No 2, 151-155
Address for correspondence:
Bijan Moghimi-Dehkordi
7th Floor of Taleghani Hospital,
Research Center of Gastroenterology
and Liver Diseases
Email: b_moghimi_de@yahoo.com
Introduction
The prevalence of obesity is increasing worldwide.
Obesity is a major health problem in Iran [1]. Although
the potential role of obesity in gastrointestinal symptoms
is unclear, it is possible that gastrointestinal disorders and
obesity have more in common than merely high population
prevalence rates. Functional gastrointestinal disorders are
hypothesized to be a result of an initial inammatory insult
to the gastrointestinal tract that modies visceral sensitivity
and/or motility [2]. Obesity may therefore increase the risk
of functional gastrointestinal disorders due to the release
of proinammatory cytokines. Epidemiologic data indicate
that obesity is associated with a wide range of chronic
gastrointestinal complaints, many of which overlap with
functional gastrointestinal disorders such as irritable bowel
syndrome (IBS) or dyspepsia [3-7].
Constipation is a common problem and affects between
2% and 28% of the general population [8-11].
Constipation is an important public health issue because
of its impact on patient well-being and productivity, in
addition to the costs of medical consultation [12]. It appears
that environmental factors play an important role in the
etiology of constipation. The relationship of constipation
with lifestyle behaviors such as an unhealthy diet, smoking,
excessive alcohol consumption, and lack of exercise has also
been investigated [13, 14]; however, only one investigator
has reported an association between obesity and constipation
in adults [15] and others have studied this association in
obese children [16, 17].
The aim of the present study was to evaluate the
association between obesity and functional constipation so
the results could reveal new insights into the relation between
patients BMI and their symptoms.
Methods
This study was part of a cross-sectional household survey
conducted from May 2006 to December 2007 in Tehran
province, Iran, which was designed to nd the prevalence
of gastrointestinal symptoms and disorders and their related
factors [18, 19]. A total of 18,180 adult persons were drawn
152
up randomly. Sampling strategy was on the basis of the
list of postal codes and systematic samples of these postal
codes and their related addresses were drawn from the
databank registry of Tehran central post ofce. Trained health
personnel from each corresponding local health centre were
sent to each selected house of all these 18,180 individuals,
door-to-door and face-to-face, and then they were asked
to participate in the rst interview according to the rst
part of our questionnaire. Before the interview survey, the
interviewer explained the purpose of these questions to all
eligible individuals and requested their participation. The
research protocol was approved by the Ethics Committee
of the Research Center for Gastroenterology and Liver
Diseases, Shaheed Beheshti Medical University.
The questionnaire comprised two parts. The rst part
which was lled out by trained health personnel, consisted
of questions about personal and family characteristics such
as age, sex, occupation, educational level, and household
income. In addition, interviewers asked them regarding 11
gastrointestinal symptoms (yes or no) including abdominal
pain or distress, constipation, diarrhea, bloating, heartburn,
acid regurgitation, proctalgia, nausea and vomiting, fecal
incontinence, existence of blood in the stool or black
stool (melena), weight loss or anorexia, and difculty in
swallowing. Those who reported at least one of these 11
gastrointestinal symptoms were selected for participation in
the second interview. The second part of the questionnaire
consisted of questions about functional bowel disorders
(including functional constipation, functional diarrhea, IBS,
functional bloating, etc.) on the basis of Rome III criteria.
The Rome III criteria were translated and standardized
for Persian language. Testretest reliability of the Persian
version of the questionnaire was good and Cronbachs
values were all higher than 70% for all major symptoms
and disorders but some minor corrections were made after
the pilot testing.
According to the Rome III criteria, constipation was
dened as the presence of at least one or two of the upcoming
symptoms, for at least three months, with the onset at least
six months preceding this study.
1. Straining during in at least 25% of defecations (at
least often).
2. Lumpy or hard stools in at least 25% of defecations
(at least often).
3. Sensation of incomplete evacuation in at least 25% of
defecations (at least sometimes).
4. Sensation of anorectal obstruction/blockage in at least
25% of defecations (at least sometimes).
5. Manual maneuvers to facilitate in at least 25% of
defecations (e.g., digital evacuation, support of the pelvic
oor) (at least sometimes).
6. Fewer than three defecations per week (at least
often).
Using the equation of BMI=weight (kg)/height square
(m2), BMI was calculated. For this study, the BMI was further
grouped into three categories: being underweight and
normal weight was established when the BMI was less than
Pourhoseingholi et al
25 kg/m2; being overweight was dened as a BMI between
25 and 29.9 kg/m2; and being obese, as a BMI 30 kg/m2.
These denitions are consistent with the recommendations
of the World Health Organization [20].
Some demographic and clinical variables including sex
(male/female), age, marital status (single, married, widow),
education (less than high school, upper high school), tobacco
smoking (non-smokers, and current-smokers of cigarettes,
cigars, or pipes) were included in the analysis.
All statistical analysis was carried out using SAS version
9.1. ANOVA was used to compare the means of continuous
variables and Pearsons chi-square and contingency tables
were performed to test the independence between discrete
classications variables. A P-value of 0.05 or less was
considered statistically signicant and all reported P values
were two sided.
Results
Of the 18,180 subjects, a total of 2,790 participants
had at least one gastrointestinal symptom (15.3%). BMI
was measured for 2,547 participants and the meanSD of
BMI was 25.954.87 (due to some domestic problems the
interviewers were unable to measure BMI in up to 90%
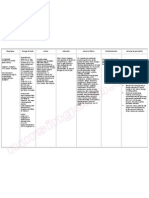
of participants). Table I shows the relationship between
obesity and individual symptoms from the rst interview in
these 2,790 participants indicating a signicant association
between BMI and bloating, heartburn, nausea and vomiting,
weight loss and incontinence.
A total of 459 adult persons were found to have functional
constipation based on Rome III criteria in second interview.
The meanSD age was 47.315.8 and 70% of patients were
female. 18% of the constipated patients had a history of
gastrointestinal medication use, among them 12 patients
with history of using laxative drugs including Lactulose,
Bizacodyl, Sorbitol and Syr.Mom. The percentage of
constipated patients with a history of abdominal surgery was
40% (24% in men and 45.2% in women) and in women with
history of abdominal surgery the most frequent surgery was
cesarean section. From the total of constipated patients, the
BMI was measured for 386 patients. The meanSD of BMI
was 26.54.7. Up to 60% of patients had BMI more than
25 (40% being overweight and 20% being obese). Table
II indicates the relation between BMI and demographic
factors. Age and education were signicant associated factors
with obesity, showing that older patients and less educated
patients had a tendency to be overweight and obese.
Smoking, marital status and sex were not signicant but
up to 60% of women with low education (less than high
school) who had functional constipation had BMI more than
25, whereas highly educated women, only 43.3%, had BMI
more than 25 (P<0.001).
Table III indicates the distribution of symptoms and
clinical factors with BMI consisting of functional constipation
symptoms, abdominal pain and history of abdominal surgery.
No signicant associations were observed between clinical
factors and obesity.
Obesity and functional constipation in Iran
153
Table I. Gastrointestinal symptoms and body mass index
Body mass index (kg/m2)
Individual symptoms
(%)
P value
<25 (n=1158)
25-30 (n=959)
30 (n=430)
MeanSD:22.012.6
MeanSD:27.251.4
MeanSD:33.673.7
<0.001
Abdominal pain
484 (41.8%)
374 (39%)
169 (39.3%)
0.38
Constipation
0.72
468 (40.4%)
373 (38.9%)
175 (40.7%)
Diarrhea
98 (8.5%)
86 (9%)
35 (8.1%)
0.85
Bloating
628 (54.2%)
561 (58.5%)
268 (62.3%)
0.009
Heartburn
630 (54.4%)
580 (60.5%)
225 (52.3%)
0.04
Anal pain
154 (13.3%)
150 (15.6%)
72 (16.7%)
0.14
Anal bleeding
65 (5.6%)
64 (6.8%)
27 (6.3%)
0.54
Nausea and vomiting
107 (9.2%)
59 (6.2%)
42 (9.8%)
0.01
Weight loss
155 (13.4%)
65 (6.8%)
26 (6%)
<0.001
Dysphagia
62 (5.4%)
43 (4.5%)
33 (7.7%)
0.05
Incontinence
15 (1.3%)
14 (1.5%)
14 (3.3%)
0.02
Table II. Demographic factors and BMI in patients with functional constipation
Body mass index (kg/m2)
Demographic factors (%)
P value
<25 (n=157)
25-30 (n=156)
30 (n=73)
MeanSD:22.361.9
MeanSD:27.351.4
MeanSD:33.733.5
<0.001
116 (75%)
109 (70%)
58 (80%)
0.29
0.001
Sex
Female
Age
Mean age (SD)
43.5 (16.9)
48.1 (14.2)
50.9 (13.8)
15-35 years
57 (36.3%)
29 (18.6%)
10 (13.7%)
36-60 years
74 (47.1%)
96 (61.5%)
49 (67.1%)
>60 years
26 (16.6%)
31 (20%)
14 (19.2%)
113 (75%)
119 (78%)
55 (70%)
0.66
123 (81%)
137 (89%)
68 (93%)
0.02
18 (12%)
18 (12%)
10 (14%)
0.87
0.001
Marital status
Married
Education
Less than high school
Smoking
Current smoker
Discussion
We studied the association between BMI and functional
constipation in the Iranian community. From the first
interview the prevalence of gastrointestinal symptoms was
15.3% which conforms with a similar previous study in
northwestern Iran where it was reported that the prevalence
rate of at least one or more gastrointestinal symptoms was
14.3% [21]. In addition a signicant association was found
between obesity and gastrointestinal symptoms including
bloating, heartburn and nausea vomiting. Some recent studies
have reported that obesity was independently associated
with heartburn [3, 4], bloating [4] and nausea vomiting [6].
Although no signicant association was found between the
self report of constipation and BMI in the rst interview,
our study observed a greater percentage of obese individuals
with functional constipation according to Rome III criteria
than in normal BMI individuals. In contrast, no signicant
relationship was observed between BMI and constipation
in other studies, although constipation was somewhat
more frequent in obese patients [4-6]. These ndings from
the western population may appear to be surprising, as
constipation has been historically linked with sedentary
lifestyles. In Iranian women, as women in developed
countries, the level of education was negatively related to
BMI, while in men the association was positive [22]. There
may be an association between higher BMI level, low
educational state and constipation in Iranian women. Our
study showed that in patients with functional constipation
about 60% of constipated patients had BMI25, which was
154
Pourhoseingholi et al
Table III. Clinical factors and BMI in patients with functional constipation
Body mass index (kg/m2)
Clinical factors (%)
P value
<25
25-30
30
Fewer than three defecations per week
109 (70%)
101 (65%)
43 (59%)
0.28
Lumpy or hard stools
134 (85%)
135 (86%)
62 (85%)
0.93
Straining
136 (87%)
139 (89%)
68 (93%)
0.34
Sensation of incomplete evacuation
100 (64%)
95 (61%)
43 (59%)
0.76
Sensation of anorectal obstruction/blockage
44 (28%)
37 (24%)
17 (23%)
0.61
Manual maneuvers to facilitate
44 (28%)
46 (29%)
14 (20%)
0.24
69 (44%)
58 (37%)
30 (41%)
0.47
55 (36%)
66 (42%)
34 (47%)
0.20
Symptoms
Abdominal pain
Yes
History of abdominal surgery
Yes
more than the mean of our community [23]. The prevalence
of obesity and overweight in Iran is as high as in the US.
However Iranian women are more obese than American
women and Iranian men are less obese than their American
counterparts. This discrepancy might be due to the low rate
of smoking among Iranian women [24]. Another interesting
nding in this study was the high number of patients who
had undergone abdominal surgery even though there was
no signicant relationship observed with obesity. This is
due to the fact that a great number of patients were women
with a history of a cesarean section. According to statistics
from the Ministry of Health and Medical Education, Iranian
women are more likely to have cesarean sections and this
rate has increased from 35% to 42% [25].
The etiology of constipation in obese people is not clear.
Disordered eating patterns such as bingeing have been shown
to be an independent contributor to constipation in adults
[26]. In addition obese people may eat less ber or have
less physical activity, which could change their defecation
pattern [27].
In conclusion a clear association between obesity
and constipation could be assessed in this study and this
association is increased for elderly and less educated people
(especially in women). However it might require further
studies to explore the underlying factors. The limitation of
this study was that we had no healthy people to compare
with patients as a control group. Therefore further studies
should be carried out in order to nd the difference between
healthy people and constipated people with obesity.
Acknowledgment
This study was sponsored by a grant from the Research
Center for Gastrointestinal and Liver Disease (RCGLD),
Taleghani hospital Tehran, Iran. The assistance of all
persons involved in obtaining interview information, and the
cooperation of the participants is much appreciated.
Conicts of interest
None to declare.
References
1. Kelishadi R, Alikhani S, Delavari A, Alaedini F, Safaie A, Hojatzadeh
E. Obesity and associated lifestyle behaviours in Iran: ndings
from the First National Non-communicable Disease Risk Factor
Surveillance Survey. Public Health Nutr 2008; 11: 246-251.
2. Bercik P, Verdu EF, Collins SM. Is irritable bowel syndrome a lowgrade inammatory bowel disease? Gastroenterol Clin North Am
2005; 34: 235245.
3. Van Oijen MG, Josemanders DF, Laheij RJ, van Rossum LG, Tan
AC, Jansen JB. Gastrointestinal disorders and symptoms: does body
mass index matter? Neth J Med 2006; 64: 45-49.
4. Delgado-Aros S, Locke GR 3rd, Camilleri M, et al. Obesity is
associated with increased risk of gastrointestinal symptoms: a
population-based study. Am J Gastroenterol 2004; 99: 1801-1806.
5. Talley NJ, Quan C, Jones MP, Horowitz M. Association of upper
and lower gastrointestinal tract symptoms with body mass index in
an Australian cohort. Neurogastroenterol Motil 2004; 4: 413-419.
6. Talley NJ, Howell S, Poulton R. Obesity and chronic gastrointestinal
tract symptoms in young adults: a birth cohort study. Am J
Gastroenterol 2004; 99: 1807-1814.
7. Aro P, Ronkainen J, Talley NJ, Storskrubb T, Bolling-Sternevald E,
Agrus L. Body mass index and chronic unexplained gastrointestinal
symptoms: an adult endoscopic population based study. Gut 2005;
54: 1377-1383.
8. Higgins PD, Johanson JF. Epidemiology of constipation in North
America: a systematic review. Am J Gastroenterol 2004; 99:
750759.
9. Adibi P, Behzad E, Pirzadeh S, Mohseni M. Bowel habit reference
values and abnormalities in healthy adults. Dig Dis Sci 2007; 52:
1810-1813.
10. Corazziari E. Definition and epidemiology of functional
gastrointestinal disorders. Best Pract Res Clin Gastroenterol 2004;
18: 613631.
11. Harris LA. Prevalence and ramications of chronic constipation.
Manag Care Interface 2005; 18: 2330.
12. Locke GR 3rd, Pemberton JH, Phillips SF. AGA technical review
on constipation. Gastroenterology 2000; 119: 17661778.
13. Campbell AJ, Busby WJ, Horwath CC. Factors associated with
constipation in a community based sample of people aged 70 years
and over. J Epidemiol Community Health 1993; 47: 2326.
14. Sandler RS, Jordan MC, Shelton BJ. Demographic and dietary
determinants of constipation in the US population. Am J Public
Health 1990; 80: 185189.
Obesity and functional constipation in Iran
15. Pecora P, Suraci C, Antonelli M, De Maria S, Marrocco W.
Constipation and obesity: a statistical analysis. Boll Soc It Biol Sper
1981; 57: 2384-2388.
16. Misra S, Lee A, Gensel K. Chronic constipation in overweight
children. JPEN J Parenter Enteral Nutr 2006; 30: 81-84.
17. Pashankar DS, Loening-Baucke V. Increased prevalence of obesity
in children with functional constipation evaluated in an academic
medical center. Pediatrics 2005; 116: e377-380.
18. Zarghi A, Pourhoseingholi MA, Habibi M, Nejad MR, Ramezankhani
A, Zali MR. Prevalence of gastrointestinal symptoms in the
population of Tehran, Iran. Trop Med Int Health 2007; 12 (suppl);
181-182.
19. Zarghi A, Pourhoseingholi MA, Habibi M, et al. Prevalence of
gastrointestinal symptoms and the inuence of demographic factors.
Am J Gastroenterol 2007; 102 (suppl): 441-441.
20. World Health Organization (WHO): Obesity: preventing and
managing the global epidemic. Report of a WHO Consultation on
Obesity, Geneva, 35 June 1997. Geneva, WHO, 1998.
21. Khoshbaten M, Hekmatdoost A, Ghasemi H, Entezariasl M.
155
22.
23.
24.
25.
26.
27.
Prevalence of gastrointestinal symptoms and signs in northwestern
Tabriz, Iran. Indian J Gastroenterol 2004; 23: 168-170.
Maddah M, Eshraghian MR, Djazayery A, Mirdamadi R. Association
of body mass index with educational level in Iranian men and women.
Eur J Clin Nutr 2003; 57: 819-823.
Janghorbani M, Amini M, Willett WC, et al. First nationwide survey
of prevalence of overweight, underweight, and abdominal obesity in
Iranian adults. Obesity (Silver Spring) 2007; 15: 2797-2808.
Bahrami H, Sadatsafavi M, Pourshams A, et al. Obesity and
hypertension in an Iranian cohort study; Iranian women experience
higher rates of obesity and hypertension than American women.
BMC Public Health 2006; 6: 158.
Ministry of Health and Medical Sciences - Iran Statistic Center,
September 2000.
Crowell MD, Cheskin LJ, Musial F. Prevalence of gastrointestinal
symptoms in obese and normal weight binge eaters. Am J
Gastroenterol 1994; 89: 387-391.
Van der Sijp JR, Kamm MA, Nightengale JM, et al. Circulating
gastrointestinal hormone abnormalities in patients with severe
idiopathic constipation. Am J Gastroenterol 1998; 93: 1351-1356.
Anda mungkin juga menyukai
- Obesity and Functional Constipation A Community-Based Study in IranDokumen6 halamanObesity and Functional Constipation A Community-Based Study in IranMonaBelum ada peringkat
- Breakfast SkippingDokumen6 halamanBreakfast SkippingselviannisameldiBelum ada peringkat
- Public AccessDokumen38 halamanPublic AccessAdy Fitra SaragihBelum ada peringkat
- Nin Research Paperon DiabetesDokumen4 halamanNin Research Paperon DiabetesAvantikaBelum ada peringkat
- Prevalence of Overweight and Obesity and Weight Loss Practice Among Beijing Adults, 2011Dokumen10 halamanPrevalence of Overweight and Obesity and Weight Loss Practice Among Beijing Adults, 2011Aboy GunawanBelum ada peringkat
- Shahad 4Dokumen15 halamanShahad 4Mohammed OmarBelum ada peringkat
- Comparison of Body Mass Index On Children With Functional Constipation and Healthy ControlsDokumen5 halamanComparison of Body Mass Index On Children With Functional Constipation and Healthy ControlsGita TrisnawatiBelum ada peringkat
- 5 - IJMPS - A Study of Prevalence of Obesity in Adolescents of A Select PrimaryDokumen4 halaman5 - IJMPS - A Study of Prevalence of Obesity in Adolescents of A Select PrimaryTJPRC PublicationsBelum ada peringkat
- Da QingDokumen18 halamanDa QingAlina PopaBelum ada peringkat
- Nutrients 12 01200Dokumen13 halamanNutrients 12 01200andaradwikeBelum ada peringkat
- Obesity and Health-Related Lifestyle Factors in The General Population in Romania: A Cross Sectional StudyDokumen9 halamanObesity and Health-Related Lifestyle Factors in The General Population in Romania: A Cross Sectional StudyLiviu LivaxBelum ada peringkat
- Shahad 7Dokumen10 halamanShahad 7Mohammed OmarBelum ada peringkat
- Shahad 3Dokumen5 halamanShahad 3Mohammed OmarBelum ada peringkat
- Pi Is 0022534712054948Dokumen5 halamanPi Is 0022534712054948Key NduetBelum ada peringkat
- Nutritional Knowledge, Food Habits and Health Attitude of Chinese University Students - A Cross Sectional StudyDokumen11 halamanNutritional Knowledge, Food Habits and Health Attitude of Chinese University Students - A Cross Sectional StudyJaymier SahibulBelum ada peringkat
- Body Mass Index at Age 18 - 20 and Later Risk of Spontaneous Abortion in The Health Examinees Study (HEXA)Dokumen8 halamanBody Mass Index at Age 18 - 20 and Later Risk of Spontaneous Abortion in The Health Examinees Study (HEXA)Faradiba NoviandiniBelum ada peringkat
- Quality of Life in Pregnant Women With and Without ConstipationDokumen8 halamanQuality of Life in Pregnant Women With and Without ConstipationMichimichi 78Belum ada peringkat
- Pi Is 1542356508007295Dokumen5 halamanPi Is 1542356508007295zeegerzBelum ada peringkat
- Correlation and Comparison of Body Mass Index and Oral Health Status Among Urban South Indian Population: A Pilot StudyDokumen6 halamanCorrelation and Comparison of Body Mass Index and Oral Health Status Among Urban South Indian Population: A Pilot StudyAboy GunawanBelum ada peringkat
- Research Presentations of Dietetic Internship Participants: Research Proceedings - Nutrition and Food SectionDari EverandResearch Presentations of Dietetic Internship Participants: Research Proceedings - Nutrition and Food SectionBelum ada peringkat
- Hubungan Aktivitas Fisik Dengan Kejadian Obesitas Pada Orang Dewasa Di Indonesia (Analisis Data Riskesdas 2007) Sudikno, Milla Herdayati Dan BesralDokumen13 halamanHubungan Aktivitas Fisik Dengan Kejadian Obesitas Pada Orang Dewasa Di Indonesia (Analisis Data Riskesdas 2007) Sudikno, Milla Herdayati Dan BesralAulya Adha DiniBelum ada peringkat
- Age MenarcheDokumen7 halamanAge MenarchenamiracarolineBelum ada peringkat
- Overweight and Obesity and Associated Risk Factors Among The Iranian Middle-Aged WomenDokumen12 halamanOverweight and Obesity and Associated Risk Factors Among The Iranian Middle-Aged WomenagnesBelum ada peringkat
- WhoDokumen13 halamanWhoKCcheungBelum ada peringkat
- Brief Resume of The Intended WorkDokumen10 halamanBrief Resume of The Intended WorkPooja PrakashBelum ada peringkat
- Obezitatea La Copii Si Boala ParodontalaDokumen8 halamanObezitatea La Copii Si Boala ParodontalaLavinia PascuBelum ada peringkat
- JAPI Body FatDokumen6 halamanJAPI Body FatBhupendra MahantaBelum ada peringkat
- Dokumen Tanpa JudulDokumen10 halamanDokumen Tanpa JudulZakia AmeliaBelum ada peringkat
- Comparison of Different Anthropometric Measures in The Adult Population in Serbia As Indicators of Obesity Data From The National Health Survey 2013Dokumen10 halamanComparison of Different Anthropometric Measures in The Adult Population in Serbia As Indicators of Obesity Data From The National Health Survey 2013snezaimBelum ada peringkat
- 9 FullDokumen7 halaman9 FullSaudah Sii SipitBelum ada peringkat
- Articulo GastroDokumen7 halamanArticulo GastroAngel Guadalupe Garcia SiordiaBelum ada peringkat
- Obesity and Physical Activity Literature ReviewDokumen5 halamanObesity and Physical Activity Literature Reviewea8d1b6n100% (1)
- A Study On The Relationship Between Mindful Eating, Eating Attitudes and Behaviors and Abdominal Obesity in Adult WomenDokumen5 halamanA Study On The Relationship Between Mindful Eating, Eating Attitudes and Behaviors and Abdominal Obesity in Adult WomenInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Downloaded From Uva-Dare, The Institutional Repository of The University of Amsterdam (Uva)Dokumen28 halamanDownloaded From Uva-Dare, The Institutional Repository of The University of Amsterdam (Uva)Indah Putri permatasariBelum ada peringkat
- Fereidouni2015 Article AreIranianObeseWomenCandidateFDokumen7 halamanFereidouni2015 Article AreIranianObeseWomenCandidateFFrancisco TBelum ada peringkat
- Long Term Outcome of Functional Childhood ConstipationDokumen6 halamanLong Term Outcome of Functional Childhood ConstipationShirleuy GonçalvesBelum ada peringkat
- The Prevalence of Obesity Among Health Staffs in Muar Health District Office in 2018: A Cross Sectional StudyDokumen14 halamanThe Prevalence of Obesity Among Health Staffs in Muar Health District Office in 2018: A Cross Sectional StudyPBR NOR HAZWANI BINTI ABDULLAHBelum ada peringkat
- QoL Obese ChildrenDokumen7 halamanQoL Obese ChildrenLiga Sabatina de BaloncestoBelum ada peringkat
- Jurnal ObesitasDokumen20 halamanJurnal ObesitasTan Endy100% (1)
- Spirulina ObesidadeDokumen10 halamanSpirulina ObesidadeIsabela CastroBelum ada peringkat
- 392 MS Published Physical Activity IAFDokumen6 halaman392 MS Published Physical Activity IAFharijan9Belum ada peringkat
- The Secrets You Should Know About Sexual Medicine; Part One; Obesity and Sexual DysfunctionDari EverandThe Secrets You Should Know About Sexual Medicine; Part One; Obesity and Sexual DysfunctionBelum ada peringkat
- Developing Suitable Methods of Nutritional Status Assessment: A Continuous ChallengeDokumen9 halamanDeveloping Suitable Methods of Nutritional Status Assessment: A Continuous Challengeparampam21Belum ada peringkat
- Jurnal Ibu MenopouseDokumen15 halamanJurnal Ibu MenopouserahmatBelum ada peringkat
- High Prevalence of Preobesity and Obesity Among Medical Students of Lahore and Its Relation With Dietary Habits and Physical ActivityDokumen1 halamanHigh Prevalence of Preobesity and Obesity Among Medical Students of Lahore and Its Relation With Dietary Habits and Physical ActivityMuqtada AliBelum ada peringkat
- Running Head: METABOLIC SYNDROME 1Dokumen8 halamanRunning Head: METABOLIC SYNDROME 1springday_2004Belum ada peringkat
- Association Between Dietary Patterns and The Risk of Metabolic Syndrome Among Lebanese AdultsDokumen9 halamanAssociation Between Dietary Patterns and The Risk of Metabolic Syndrome Among Lebanese AdultsThalia KarampasiBelum ada peringkat
- Akne Obese Lipid 2009Dokumen5 halamanAkne Obese Lipid 2009Henyta TsuBelum ada peringkat
- 7 Skippingmeals PDFDokumen10 halaman7 Skippingmeals PDFchacaimutBelum ada peringkat
- tmp393C TMPDokumen10 halamantmp393C TMPFrontiersBelum ada peringkat
- Pcos Ob JournalDokumen10 halamanPcos Ob JournalSean SialanaBelum ada peringkat
- Effects of A Meal Replacement On Body CompositionDokumen10 halamanEffects of A Meal Replacement On Body CompositionGiffariBelum ada peringkat
- Reeducação AlimentarDokumen6 halamanReeducação AlimentarTiago Kazama BulhõesBelum ada peringkat
- Community Health Project Assignment 01068804Dokumen14 halamanCommunity Health Project Assignment 01068804John HortonBelum ada peringkat
- Am. J. Epidemiol.-2003-Ma-85-92Dokumen8 halamanAm. J. Epidemiol.-2003-Ma-85-92Eima Siti NurimahBelum ada peringkat
- Aliment Pharmacol Ther - 2004 - ChangDokumen9 halamanAliment Pharmacol Ther - 2004 - ChangCynthia SuarezBelum ada peringkat
- Papers: Eating Disorders in Adolescent Females With and Without Type 1 Diabetes: Cross Sectional StudyDokumen4 halamanPapers: Eating Disorders in Adolescent Females With and Without Type 1 Diabetes: Cross Sectional StudyWilliam PalandengBelum ada peringkat
- Nutrients 11 00148Dokumen11 halamanNutrients 11 00148Putri N.AprilliaBelum ada peringkat
- Nutrients: Weight Management Interventions in Women With and Without PCOS: A Systematic ReviewDokumen19 halamanNutrients: Weight Management Interventions in Women With and Without PCOS: A Systematic ReviewMariam QaisBelum ada peringkat
- Complementary and Alternative Medical Lab Testing Part 11: MenDari EverandComplementary and Alternative Medical Lab Testing Part 11: MenBelum ada peringkat
- Clostridium Difficile Infection (CDI) Management Guideline: C. Difficile Tests Available at NMDokumen6 halamanClostridium Difficile Infection (CDI) Management Guideline: C. Difficile Tests Available at NMMoa ClauBelum ada peringkat
- EU Digital COVID Certificate Certificat Digital European COVIDDokumen2 halamanEU Digital COVID Certificate Certificat Digital European COVIDMoa ClauBelum ada peringkat
- Child Marriage Brochure HR 164Dokumen8 halamanChild Marriage Brochure HR 164Moa Clau100% (1)
- J. Pediatr. Psychol. 2003 Cox 375 82Dokumen8 halamanJ. Pediatr. Psychol. 2003 Cox 375 82Moa ClauBelum ada peringkat
- Pediatrics 2010 Van Dijk E309 17Dokumen11 halamanPediatrics 2010 Van Dijk E309 17Moa ClauBelum ada peringkat
- 05 ConstipationDokumen13 halaman05 ConstipationNatanael NababanBelum ada peringkat
- An Gonosom Ind CarDokumen32 halamanAn Gonosom Ind CarMoa ClauBelum ada peringkat
- BMI Group Calculator EnglishDokumen5 halamanBMI Group Calculator EnglishMcarl MatelBelum ada peringkat
- Diabetes in Palliative Care CompletedDokumen4 halamanDiabetes in Palliative Care Completedaya PermatasariBelum ada peringkat
- EdX - Critical ThinkingDokumen2 halamanEdX - Critical Thinkingjotape_89Belum ada peringkat
- Bmi AnamayDokumen16 halamanBmi AnamayArman MoralesBelum ada peringkat
- Patient Positioning and AnaesthesiaDokumen24 halamanPatient Positioning and AnaesthesiaGrishma KothariBelum ada peringkat
- Inverse Abdominoplasty 2017Dokumen202 halamanInverse Abdominoplasty 2017Ahmed AttiaBelum ada peringkat
- Diet ModificationDokumen3 halamanDiet ModificationJhayneBelum ada peringkat
- 800 and 1600 TrainingDokumen15 halaman800 and 1600 Trainingschenkerk100% (4)
- Some Sampling Distribution ProblemsDokumen3 halamanSome Sampling Distribution ProblemsvuduyducBelum ada peringkat
- Congestive Heart FailureDokumen64 halamanCongestive Heart FailureBentoys StreetBelum ada peringkat
- History of PastaDokumen7 halamanHistory of PastaSunil KumarBelum ada peringkat
- Eating Fruits Is HealthyDokumen4 halamanEating Fruits Is HealthyGabriela Elena StanciuBelum ada peringkat
- Research Paper Annotated BibliographyDokumen4 halamanResearch Paper Annotated Bibliographyalam4ndBelum ada peringkat
- School Report Card Final 2018-2019Dokumen20 halamanSchool Report Card Final 2018-2019Honey Grace GonzalesBelum ada peringkat
- BMI W HFA GFTSISHSDokumen2 halamanBMI W HFA GFTSISHSRizal LeonardoBelum ada peringkat
- Fitt Log Worksheet 5Dokumen2 halamanFitt Log Worksheet 5api-270355373Belum ada peringkat
- Natures Hidden Health MiracleDokumen38 halamanNatures Hidden Health MiracleGorneau100% (2)
- Preserving Body Image and Self-EsteemDokumen47 halamanPreserving Body Image and Self-EsteemGhostBelum ada peringkat
- Elc 030 (Week 2)Dokumen21 halamanElc 030 (Week 2)ahmad mukhlisBelum ada peringkat
- Pre DiabetesDokumen4 halamanPre DiabetessweetloliepopBelum ada peringkat
- Clonidine HydrochlorideDokumen1 halamanClonidine HydrochlorideLovelyn Joy Abubo CortezBelum ada peringkat
- q1 Grade 8 Pe DLL Week 1Dokumen12 halamanq1 Grade 8 Pe DLL Week 1Kristel G. Garcia100% (2)
- Physiology of Lactation NewDokumen28 halamanPhysiology of Lactation NewLala SumatraBelum ada peringkat
- Bodybuilding Made SimpleDokumen96 halamanBodybuilding Made Simplewiseguy21250% (2)
- HYper and Hypo TGDokumen43 halamanHYper and Hypo TGRiajoy AsisBelum ada peringkat
- JEP Journal of Exercise PhysiologyDokumen7 halamanJEP Journal of Exercise PhysiologykambuaBelum ada peringkat
- Diet and Activity Analysis PaperDokumen19 halamanDiet and Activity Analysis Paperapi-353042837Belum ada peringkat
- 31 MicrobiomeDokumen17 halaman31 Microbiomeapi-261182081Belum ada peringkat
- Pedia StickersDokumen8 halamanPedia Stickersmkct111100% (1)
- Jurnal Virgin Coconut Oil (VCO)Dokumen8 halamanJurnal Virgin Coconut Oil (VCO)Tamam Ibrahim SatrioBelum ada peringkat