Effects of AntiPyretics
Diunggah oleh
2 FunkyHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Effects of AntiPyretics
Diunggah oleh
2 FunkyHak Cipta:
Format Tersedia
INDIAN PEDIATRICS
VOLUME 34-MAY 1997
Personal Practice
Antipyretic Therapy
K. Rajeshwari
Fever is among the most common manifestations of disease and antipyresis is one
of the most usual therapeutic intervention
undertaken. A variety of microbial products including endotoxins and exotoxins
are recognized as exogenous pyrogens
which induce host cells to produce mediators known as endogenous pyrogens. The
best studied endogenous pyrogen is interleukin 1, others include tumor necrosis factor and interferons(l). Most known endogenous pyrogens act on the anterior hypothalamus to elicit local generation of prostaglandins. Fever represents the response
of the host to a neurologic signal demanding thermal upregulation. Studies have
shown temperature elevation to enhance
several parameters of immune function like
T cell activation, mononuclear production
of leukocyte migration inhibition factor,
neutrophil function and macrophage oxidative metabolism(2,3) while high temperatures prove deleterious by altering natural
killer cell activity, generation of cytotoxic T
lymphocytes and alteration in neutrophil
morphology and function(4). While the
clinical situation is much too complex to allow definite conclusions, the preponderance of evidence suggests that temperatures in the range of usual fever may renFrom the Department of Pediatrics, Hindu Rao
Hospital, Delhi 110 007.
Reprint requests: Dr. K. Rajeshwari, Department of
Pediatrics, Hindu Rao Hospital, Delhi 110 007.
der many host defenses *noro active andmany pathogens more susceptible to there
defenses more active and many pathogens
more susceptible to these defenses. Thus
the limited data that exist do support the
hypothesis that fever has some beneficial
effects in human infection. This communication addresses the need and available
modalities for antipyresis in pediatric practice.
Is Antipyresis Required?
A common stated reason for aggressive
antipyretic therapy is the prevention of febrile seizures or other central nervous system effects. Although the height of fever is
considered important in seizure induction^), it is not clear whether aggressive
antipyresis alters the risk of an initial febrile seizure. Epilepsy may manifest during febrile episodes. Fever may precipitate
status epilepticus in some children and further result in motor incoordination and
other disabilities(6). Most physicians can
recall instances of transient delirium in febrile patients but it is difficult to determine
whether the reversible manifestation arises
from the fever or from the disease producing the fever(7). It is yet not scientifically
proved whether antipyretic therapy can
prevent or reverse delirium in identifiable
high risk situations or minimize risk of status epilepticus.
Another common reason for antipyretic
therapy is symptomatic treatment of fever.
It is less clear exactly what symptoms are
being treated and to what extent
antipyresis actually makes the patient feel
better. Conversely, there is a possibility
that a febrile patient given antipyretics may
become abruptly afebrile or even hypother407
PERSONAL PRACTICE
mic with profuse diaphoresis and greater
discomfort than if untreated(8). In treating
fever symptomatically one should not lose
sight of the fact that elevated temperature
whatever their physiologic function do
serve as a signal both to the patient and to
the caregiver. Non specific suppression of
fever may deprive one of clues to a need
for further diagnostic investigation or for
changes in therapy.
In the light of available scientific data,
the decision for antipyresis is usually based
on the "perceived" risk and benefits, both
of the fever itself and of the available treatments. The definition of dangerous hyperpyrexia requiring treatment is clearcut and
supported by clinical data. A rectal temperature above 41.4C is definitely harmful
and requires therapy(9). In other patients, a
cited reason for trying to suppress fever is
concern about hypoxic injury to tissues, especially the cardiovascular system. Metabolic rate and tissue oxygen demand increase with elevated body temperature.
Cardiac compromise has been reported at
extreme hyperthermic temperatures. Similarly, subclinical compromise of cardiac
function has been documented during febrile illnesses. Thus patients with severe
valvular heart disease with precarious coronary perfusion may benefit from prompt
antipyresis to prevent worsening of clinical
condition.
In addition to the antipyretic effect,
most commonly used antipyretics particularly Non Steroidal Anti Inflammatory
Drugs (NSAIDS), have considerable analgesic effect which promotes a general feeling of well being for the duration of effect.
In the usual clinical setting, antipyresis is
generally resorted to for promotion of this
feeling of "well being" as well as for reduction of fever, often to allay anxiety and reassure the patient and relatives. In this context, the effect (beneficial or otherwise) of
408
antipyretics on the biological process is as
yet not clear.
Physical Antipyresis
Physical modalities such as sponging,
ice packs or cooling blankets are most often
used in conjunction with pharmacological
antipyresis. It has been shown that use of
iced water or alcohol in water is superior to
sponging with tepid water though associated with more patient discomfort(lO). External cooling by sponging in a bath tub with
5-10 cm of tepid water increases evaporation and promotes heat loss. Cold water
should be avoided because it results in peripheral vasoconstriction and shivering,
causes greater discomfort to the child and
may also increase the core body temperature(10,11). Sponging for 20 minutes was
found to be ineffective(12) and sponging
for 2-4 hours has been recommended(13).
Wet compresses covering the lower legs or
trunk are frequently used to lower the
body temperature. Usually they are
changed after 10-15 minutes and repeated
till the skin feels cool. No controlled trials
proving their efficacy are available.
There is a fundamental illogic to the use
of external application of cold to lower
body temperature in a patient with true
fever. Because of the altered hypothalamic
set point, the patient is already responding
as if to a cold environment. Physical methods should only be used after administration of antipyretic drugs, so that the hypothalamic set point is lowered from its febrile values. Even in this setting, their utility in the reduction of fever can be debated.
One study found that sponging febrile children with tepid water after antipyretic
therapy had no more effect on defervescence than antipyretics alone(12). Thus
physical methods may be used only if there
is failure of pharmacotherapy or when temperature is to be lowered for a reason not
associated with true fever (heat stroke, or
INDIAN PEDIATRICS
induction of profound hypothermia in
head trauma or cardiac surgery)(13)
Pharmacological Antipyresis
Antipyresis occurs with differsnt classes of substance including steroids, acetylsalicylic acid, dipyrone, acetaminophen
and the non steroidal anti-inflammatory
agents represented by indomethacin,
mefenamic acid, ibuprofen and the latest
nimesulide. Some antipyretics are anti-inflammatory, some are not while most have
pronounced analgesic properties. The decision to choose an antipyretic should be dictated by efficacy, safety, duration of effect
and cost.
One of the oldest antipyretics in use is
acetyl salicylic acid (ASA). The mode of
action of ASA is not wholly understood. It
inhibits cyclo-oxygenase which catalyses
the conversion of arachidonic acid to prostaglandin E2. This reduction of prostaglandin E2 in the brain is believed to lower the
hypothalamic set point. Since ASA also
possesses anti-inflammatory activity, this is
beneficial in patient with inflammatory
processes. Both the absolute (reduction of
initial temperature) and relative (in comparison to paracetamol or other drugs)
antipyretic efficacy of ASA in febrile children have been extensively evaluated(1418). Compared to paracetamol, ASA has
equal antipyretic efficacy. Differences in
the onset and duration of action may exist
for different doses, but similar doses of
each drug produced a similar time of onset
(0.6-0.9 hours) and duration of action (at
least 3 hours)(15). Adverse effects of ASA
after a single dose (hepatotoxicity) are also
known. Use of salicylates has demonstrated a strong statistical association with Reye
syndrome; patients with Reye syndrome
were found to have significantly higher total and average daily doses of salicylates
than matched controls(19). The easy avail-
VOLUME 34-MAY 1997
ability of ASA increases the chance of toxicity. Further, at therapeutic plasma levels,
ASA affects blood coagulation. Hence because of availability of equally potent and
safer drugs, ASA is currently not recommended as a first line antipyretic.
Another antipyretic in use for a considerable time is acetaminophen (paracetamol).
As with ASA, the antipyretic effect of
paracetamol is believed to be caused by its
ability to decrease prostaglandin synthesis
in the brain. Since paracetamol does not inhibit the synthesis of prostaglandins in the
periphery, it does not possess any anti-inflammatory effects. Ibuprofen belongs to the
propionic acid group of NSAIDS. The
antipyretic effects of paracetamol and
ibuprofen have been compared in various
studies(20-26). The largest double blind acetaminophen controlled trial has established the safety of ibuprofen for
antipyresis in children. It involved 84192
children and proved that the risk of gastrointestinal bleeding, renal failure or anaphylaxis was not increased following short
term use of ibuprofen(23). Some of these
studies have also shown a longer duration
of action for ibuprofen (8 hours) vis-a-vis
acetaminophen(20,22). In a dose of 10 mg/
kg, ibuprofen suspension, and possibly 5
mg/kg ibuprofen, produce equally tolerated, greater and longer lasting fever control
than 10 mg/kg paracetamol elixir, especially in children with oral temperatures above
100.5F(20). While further confirmatory evidence is awaited, ibuprofen liquid (10 mg/
kg) and paracetamol (15 mg/kg) administered every 6 hours for 24 to 48 hours appeared to be most effective in reducing fever. Lower ibuprofen doses (2.5 mg/kg
and 5 mg/kg) were less effective than
paracetamol and 10 mg/kg ibuprofen(24).
When administered every 6 hourly, there
was no significant difference between 10
mg/kg ibuprofen therapy and 15 mg/kg
paracetamol. Thus used in these doses, the
409
PERSONAL PRACTICE
above drugs are equally efficacious. Dose de-
pendent efficacy has also been found for
5,10 and 20 mg/kg paracetamol but the
duration of action differed in the trials performed^). More data are required from
prospective comparative trials together
with the recently adjusted higher dose and
shorter dosage intervals of acetaminophen.
There is only one study comparing the
antipyretic efficacy of ibuprofen and
paracetamol in children wijih febrile seizures(28). Other studies in children
without
febrile
seizures
have
demonstrated
significantly
lower
temperatures at 3-5 hours after initial dose
of ibuprofen(29,30). Clinicians usually
pursue rapid fever reduction in children
with febrile seizures. In this respect a
0.5C greater temperature reduction at 4
hours was documented with ibuprofen.
Few recurrent seizures occurred in this
study and seizure prophylaxis was not
evaluated. No placebo controlled groups
were used. A large placebo controlled
trial is necessary to determine whether
antipyretics, especially ibuprofen can
prevent febrile seizure recurrences.
Dipyrone (Metamizol), a pyrazolone, is also
effective as an antipyretic. However, the
mechanism by which dipyrone exerts its
antipyretic effect is still unclear. It probably
has a direct action on the central nervous
system and possibly an additional peripheral inhibition of endogenous pyrogen synthesis and release. Double blind clinical trials on dipyrone are not available. The
antipyretic effect of this drug was compared with paracetamol in a single blind
controlled trial(31). Dipyrone in dose range
of 13.2 to 22.3 mg/kg was superior to
paracetamol (dose range 13.2-22.3 mg/kg)
1.5 hours to 6 hours after drug intake. The
only reported adverse effect of this drug is
agranulocytosis, the risk of which is approximately 1 per million per week of
treatment(32). However, because of contro410
versy raised over this, dipyrone is not
marketed in several countries. Most of the
reports dealing with the risk of agranulocytosis were based on observations of small
numbers of cases and matched controls(33,34). Additional graded dose comparative trials with dipyrone should be carried out in order to determine the optimum
dose for treating febrile children.
The latest drug Nimesulide (4-nitro-2phenoxymethane sulfonanilide) is a non
steroidal anti-inflammatory drug with analgesic and antipyretic properties. Its efficacy has been compared with naproxen,
ASA, paracetamol and mefenamic acid(3538). Though these demonstrated the superior efficacy of nimesulide, these studies
were not double blinded and comprised
small groups of children. More controlled
data is necessary before drawing any firm
conclusions. However, this drug may offer
a theoretical advantage of reduced frequency in dosing (8-12 hourly).
Corticosteroids are also highly effective
antipyretics. Although they have a place in
the treatment of certain infections wherein
the effects of inflammation may be devastating, their adverse effects on host defenses and risk of bowel perforation in inflammatory states have prevented them from
being used for antipyresis per se(39,40).
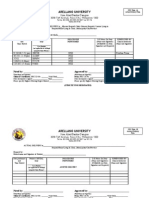
Table I summarizes the available pharmacological antipyretics with their age
wise recommended doses and frequency of
administration(37,41-43).
Recent data indicates that factors other
than the type of antipyretic agent employed are also important determinants of
the response to therapy. Multivariate analysis indicates that pharmacokinetics of
ibuprofen and perhaps all antipyretics are
determined by age and initial temperature(43). Thus if studies are conducted age
wise, using different doses of antipyretic
VOLUME 34-MAY 1997
INDIAN PEDIATRICS
TABLE IDose and Frequency of Administration of Commonly Used Antipyretics
Drug
Dose
Frequency of administration
Remarks
Ibuprofen(43)
10 mg/kg/dose
6-8 hourly
Age wise dose not stated
Nimesulide(37)
Acetyl salicylic
acid(42)
1.5 mg/kg/dose
30-65 mg/kg/
24 hours
8-12 hourly
4-6 hourly
Age wise dose not stated
Not recommended as first
line antipyretic
Paracetamol(41)
2-3 years
4-5 years
6-8 years
10 mg/kg/dose
12-15 mg/kg/dose
15-20 mg/kg/dose
4-6 hourly
4-6 hourly
4-6 hourly
Perhaps the safest
antipyretic
drugs over various temperature ranges,
clear cut differences may emerge regarding
their efficacy.
Fixed Dose Antipyretic Drug Combinations
Such combinations are commercially
available and are being aggressively promoted by some pharmaceutical companies.
Unfortunately, there is no concrete scientific data in the form of randomized controlled trials to guide the clinician regarding the utility or otherwise of such fixed
dose antipyretic drug combinations. Theoretically, a combination of two antipyretic
drugs may be expected to result in a greater antipyresis, analgesia and feeling of
"well being". However, this could also result in more risks of adverse effects. Further, the doses of antipyretics vary at different ages (especially paracetamol) and
formulation of optimal drug combinations
over the entire age range seems impossible.
It would therefore be prudent to avoid
fixed dose antipyretic drug combinations
until concrete scientific evidence to the contrary is available.
Concluding Comment
Prompt physical antipyresis is indicated
when temperature is to be lowered for a
reason not associated with true fever (heat
stroke, or induction of profound hypothermia in head trauma or cardiac surgery).
Further, antipyretic therapy is warranted
for dangerous hyperpyrexia (rectal temperature >41.1C) and fever in subjects with
precarious coronary perfusion (severe valvular heart disease). In the vast majority of
febrile infectious illnesses, there is no concrete evidence that fever is detrimental or
that antipyretic therapy offers any significant benefit. Despite this, in the actual clinical setting, antipyretic agents are invariably
prescribed for a combination of antipyresis,
analgesia and general feeling of "well being".
A variety of pharmocologic agents are
available for antipyresis. The so called superiority of one drug over the other is marginal and has no therapeutic significance.
Given in appropriate doses, ibuprofen and
paracetamol are equally efficacious and
safe. Pending the availability of firm scientific evidence, it would be prudent to avoid
fixed dose antipyretic drug combinations.
REFERENCES
1.
Endres S, Van der Meer JWM, Dinarallo
CA. Interleukin-1 in the pathogenesis of
fever. Eur J Clin Invest 1987; 17: 467-474.
2.
Jampel HD, Duff GW, Gershon RK,
Atkins E, Durum SK. Fever and immuno
411
PERSONAL PRACTICE
regulation III: Fever augments the primary in vitro humoral immune response. J
Exp Med 1983; 157:1229-1238.
3.
Roberts NJ, Sandberg K. Hyperthermia
and human leukocyte migration inhibition factor (LIF). J Immun 1979; 122:19901993.
4.
Azocar J, Yunis EJ, Essex M. Sensitivity of
human
natural
killer
cells
to
hyperthermia. Lancet 1982; 1:16-17.
5.
Millichap JG. Studies in febrile seizures:
Height of body temperature-A measure of
the febrile seizure threshold. Pediatrics
1959; 23: 76-85.
phenol and acetyl salicylic acid. J Pediatr
1957; 50: 552-555.
17. Eden AN, Kaufman A. Clinical compari
son of three antipyretic agents. Amer J
Dis Child 1967,114: 284-287.
18.
Heremans G, Dehaen F, Rom M, Ramet J,
Verboven M, Loeb H. A single blind parallel group study investigating antipyretic
properties of ibuprofen syrup versus acetylsalicylic acid syrup in febrile children.
Br J Clin Prac 1988; 42: 245-247.
19.
Hurtwitz ES, Barett MJ, Bregman D,
Gunn W. Public Health Service study of
Reye syndrome and medications. Report
of the main study. JAMA 1987; 257: 19051911.
20.
Walson PD, Galleta G, Pharma D, Braden
NJ, Alexander L. lburopfen, acetaminophen and placebo treatment of febrile
children. Clin Pharmacol Ther 1989; 46: 917.
21.
Wilson JT, Brown D, Kearns GL, Eichler
VF, Johnson VA, Bertrand KM. Single
dose placebo controlled comparative
study of ibuprofen and acetaminophen
antipyresis in children. J Pediatr 1991;
119:803-811.
22.
Sheth UK, Gupta K, Paul T, Pispati PK.
Measurement of antipyretic activity of
ibuprofen and paracetamol in children. J
Clin Pharmacol 1980; 20: 672-675.
6.
Fishman MA. Febrile seizures: Treatment
controversy. J Pediatr 1979, 94: 177-184.
7.
Lipowski ZJ. Delirium (acute confusional
states). JAMA 1987, 258:1789-1792.
8.
Done AK. Treatment of fever in 1982: A
review. Am J Med 1983; 74 (Suppl): 27-35.
9.
Schmitt BD. Fever in childhood. Pediatrics 1984; 74 (Suppl): 929-936.
10.
Steel RW, Tanaka PT, Lara RP, Bass JW.
Evaluation of sponging and of oral
antipyretic therapy to reduce fever. J
Pediatr 1970; 77: 824-825.
11.
Aynsley GA, Pickerning D. Tepid spong
ing in pyrexia. Br Med J 1975; 2: 393-394.
12.
Newman J. Evaluation of sponging to reduce body temperature in febrile children. Can Med Assoc J 1985; 132: 641-642.
23.
Barbara S, Sugarman B. Antipyresis and
fever. Arch Intern Med 1990; 150: 15891597.
Lesko SM, Mitchell AA. An assessment of
the safety of Pediatric ibuprofen. JAMA
1995; 273: 929-933.
24.
Walson PD, Galleta G, Pharm D, Braden
NJ, Alexander L. Comparison of
multidose ibuprofen and acetaminophen
therapy in febrile children. Amer J Dis
Child 1992; 146: 626-632.
25.
Breart G. Jonville AP, Courcier S, Lassale
C, Goehrs JM. A comparative efficacy and
tolerance of ibuprofen syrup and acetaminophen syrup in children with pyrexia associated with infectious diseases and
treated with antibiotics. Clin Pharmacol
1994; 46:197-201.
13.
14.
Hunter J. Study of antipyretic therapy in
current use. Arch Dis Child 1973; 48: 313315.
15.
Tarlin L, Landrigan P. A comparison of
the antipyretic effect of Acetaminophen
and Aspirin. Amer J Dis Child 1972; 124:
880-882.
16.
Colgan MT, Mintz AA. The comparative
antipyretic effect of N acetyl-P-amino-
412
VOLUME 34-MAY 1997
INDIAN TEDIATRICS
26.
Ambedkar YK, Desai RZ. Antipyretic activity of ibuprofen and paracetamol in
children with pyrexia. Br ] Clin Prac 1985;
39:140-143.
27.
Adam D, Stankov G. Treatment of fever
in childhood. Eur J Pediatr 1994; 153: 394402.
28.
Esch AV, Henriette A, Moll VS,
Steyerberg EW, Offringa M, Habbema
DF. Antipyretic efficacy of ibuprofen and
acetaminophen in children with febrile
seizures. Arch Pediatr Adolesc Med 1995;
149: 632-637.
29.
Kauffman RE, Sawyer LA, Scheinbaum
ML. Antipyretic efficacy of ibuprofen vs
acetaminophen. Amer J Dis Child 1992;
146: 622-625.
30.
Sidler J, Frey B, Baerlocher K. A double
blind comparison of ibuprofen and
paracetamol in juvenile pyrexia. Br J Clin
Pract 1990; 44 (Suppl 70): 22-25.
31.
Ottolegni A. Pediatric use of dipyrone as
an antipyretic agent. Minerva Pediatr
1971; 23:1981-1984.
32.
The International Agranulocytosis and
Aplastic Anemia Study. Risks of
agranulocytosis and aplastic anemia. A
first report of their relation to drug use
with special references to analgesics.
JAMA 1986; 256:1749-1757.
36.
Cappella L, Guerra A, Landizi L,
Cavazzuti GB. Efficacy and tolerability of
Nimesulide and Lysine Acetyl Salicylate
in the treatment of Pediatric acute upper
respiratory tract inflammation. Drugs
1993; 46 (Suppl 1): 222-225.
37.
Polidori G, Titti G, Pieragostini P, Comito
A, Scaricabarozzi I. A comparison of
Nimesulide and Paracetamol in the treat
ment of fever due to inflammatory diseases of the upper respiratory tract in
children. Drugs 1993; 46 (Suppl 1): 231233.
38.
Salzberg R, Giambonini S, Maurizio M,
Roulet D, Zahn J, Monti T. A double blind
comparison of Nimesulide and Mefenamic acid in the treatment of acute
upper respiratory tract infections in
children. Drugs 1993; 46 (Suppl 1): 208211.
39.
Mastersky J, Kass EH. Is suppression of
fever or hypothermia useful in experimental and clinical infectious disease? J
Infect Dis 1970; 121: 81-86.
40.
Rremine SG, Me Ilrath DC. Bowel perforation in steroid treated patients. Ann
Surg 1980; 192: 581-586.
41.
Wilson JT, Ksantikul V, Harbison R.
Death in an adolescent following an overdose
of
acetaminophen
and
phenobarbital. Am J Dis Child 1978; 132:
466-473.
33.
Discombe G. Agranulocytosis caused by
amidopyrone: An unavoidable cause of
death. BMJ1952,1:1270-1273.
34.
Huguley CH. Agranulocytosis induced
by dipyrone, a hazardous antipyretic and
analgesic. JAMA 1964; 189: 938-941.
42.
Done AK, Yaffe SJ, Clayton JM. Aspirin
dosage for infants and children. J Pediatr
1979; 95: 617-625.
35.
Rodriguez LES, Viveros HAA, Lujan ME.
Assessment of the efficacy and safety of
Nimesulide vs Naproxen in Pediatric patients with respiratory tract infection.
Drugs 1993; 46 (Suppl): 226-230.
43.
Brown RD, Wilson JT, Kearns JL, Pharm
D, Valarie F, Eichler RN. Single dose
pharmacokinetics of ibuprofen and acetaminophen in febrile children. J Clin
Pharmacol 1992; 32: 231-241.
413
Anda mungkin juga menyukai
- 05 N002 28712Dokumen17 halaman05 N002 28712Alfian FahrosiBelum ada peringkat
- Evaluation of Efficacy and Tolerability of Acetaminophen Paracetamol and Mefenamic Acid As Antipyretic in Pediatric Pati PDFDokumen7 halamanEvaluation of Efficacy and Tolerability of Acetaminophen Paracetamol and Mefenamic Acid As Antipyretic in Pediatric Pati PDFrasdiantiBelum ada peringkat
- JournalReading - Learning Activity - Intrapartal Care - CamahalanDokumen3 halamanJournalReading - Learning Activity - Intrapartal Care - CamahalanJohn RyBelum ada peringkat
- Fever: Central Nervous System ConditionsDokumen14 halamanFever: Central Nervous System ConditionsthelordhaniBelum ada peringkat
- Jurnal Inter Farkol 2.Dokumen13 halamanJurnal Inter Farkol 2.cahyamasita14Belum ada peringkat
- Lenhardt 09 PDFDokumen6 halamanLenhardt 09 PDFHarling MaysBelum ada peringkat
- Edwards AbstractDokumen3 halamanEdwards Abstracteen265Belum ada peringkat
- Epilepsy & Behavior: Jerome Niquet, Roger Baldwin, Michael Gezalian, Claude G. WasterlainDokumen5 halamanEpilepsy & Behavior: Jerome Niquet, Roger Baldwin, Michael Gezalian, Claude G. WasterlainCarinka VidañosBelum ada peringkat
- Mechanism of AntipyreticsDokumen12 halamanMechanism of AntipyreticsAnamaria Blaga PetreanBelum ada peringkat
- Topical Review: Hyperthermia Exacerbates Ischaemic Brain InjuryDokumen11 halamanTopical Review: Hyperthermia Exacerbates Ischaemic Brain Injuryspin_echoBelum ada peringkat
- Aronoff and Neilson - 2001 - Antipyretics Mechanisms of Action and Clinical UsDokumen12 halamanAronoff and Neilson - 2001 - Antipyretics Mechanisms of Action and Clinical UsstrijkijzerBelum ada peringkat
- Antipyretic: Drugs FeverDokumen3 halamanAntipyretic: Drugs Feverumesh123patilBelum ada peringkat
- Management of Fever in Critically Ill Patients With InfectionDokumen6 halamanManagement of Fever in Critically Ill Patients With InfectionAnonymous La9pmFYPBelum ada peringkat
- Diagnosis and Management of Heatstroke: I Gede Yasa AsmaraDokumen8 halamanDiagnosis and Management of Heatstroke: I Gede Yasa AsmaraputryaBelum ada peringkat
- Fever: Pathophysiology and Clinical ApproachDokumen21 halamanFever: Pathophysiology and Clinical ApproachPooja ShashidharanBelum ada peringkat
- Fever During AnesthesiaDokumen19 halamanFever During AnesthesiaWindy SuryaBelum ada peringkat
- Mechanisms of Action, Physiological Effects, and Complications of HypothermiaDokumen17 halamanMechanisms of Action, Physiological Effects, and Complications of HypothermiaamaliaBelum ada peringkat
- 307 857 2 PBDokumen8 halaman307 857 2 PBBangkit Youga PratamaBelum ada peringkat
- Effect of Intravenous Propacetamol On BL PDFDokumen6 halamanEffect of Intravenous Propacetamol On BL PDFRahmat ullahBelum ada peringkat
- Research ProposalDokumen4 halamanResearch Proposalapi-3215069410% (1)
- Scientifi C Evidence-Based Effects of Hydrotherapy On Various Systems of The BodyDokumen12 halamanScientifi C Evidence-Based Effects of Hydrotherapy On Various Systems of The BodyDeni MalikBelum ada peringkat
- Fever Pediatrics 2011Dokumen10 halamanFever Pediatrics 2011jmfbravoBelum ada peringkat
- PEA Glaucoma TreatmentDokumen9 halamanPEA Glaucoma TreatmentMenoddin shaikhBelum ada peringkat
- AntiDokumen29 halamanAntideepak_143Belum ada peringkat
- Hypothermia May Facilitate Liver Transplant in Patients With Increased Intracranial PressureDokumen18 halamanHypothermia May Facilitate Liver Transplant in Patients With Increased Intracranial Pressurexai_teovisioBelum ada peringkat
- ¿Who's Afraid of FeverDokumen6 halaman¿Who's Afraid of FeverJosep Bras MarquillasBelum ada peringkat
- Pharmacological Management of FeverDokumen6 halamanPharmacological Management of FeverNabillaMerdikaPutriKusumaBelum ada peringkat
- Management of Neonatal Morbidities During Hypothermia Treatment 2015Dokumen6 halamanManagement of Neonatal Morbidities During Hypothermia Treatment 2015Vanessa CruzBelum ada peringkat
- Therapeutic HypothermiaDokumen7 halamanTherapeutic HypothermiaTracyBelum ada peringkat
- Fever: The Long and Short of It: Denise Goh Li MengDokumen5 halamanFever: The Long and Short of It: Denise Goh Li MengPuannita SariBelum ada peringkat
- Review of Anatomy and Physiology - Febrile SeizureDokumen17 halamanReview of Anatomy and Physiology - Febrile SeizureSundaraBharathi75% (4)
- Pediatrics: Fever and Antipyretic Use in ChildrenDokumen10 halamanPediatrics: Fever and Antipyretic Use in Childrenramon_otto6228100% (1)
- NursingCareinFever VrdiNorden1996Dokumen5 halamanNursingCareinFever VrdiNorden1996Pritam MajiBelum ada peringkat
- BFCDokumen7 halamanBFCKalvinKonOjalesStrangerBelum ada peringkat
- HTTPS:WWW - scielosp.org:PDF:Bwho:2003.v81n5:372 374Dokumen3 halamanHTTPS:WWW - scielosp.org:PDF:Bwho:2003.v81n5:372 374tinosan3Belum ada peringkat
- Swamedikasi DemamDokumen25 halamanSwamedikasi DemamrosawpBelum ada peringkat
- The Ice Bath Path To Enhanced Sperm Health And Fertility - Based On The Teachings Of Dr. Andrew Huberman: Ice Baths And Male Reproductive HealthDari EverandThe Ice Bath Path To Enhanced Sperm Health And Fertility - Based On The Teachings Of Dr. Andrew Huberman: Ice Baths And Male Reproductive HealthBelum ada peringkat
- Paracetamol Suppositories: Should We Give It As Antipyretic in Children?Dokumen27 halamanParacetamol Suppositories: Should We Give It As Antipyretic in Children?Arrum Chyntia YuliyantiBelum ada peringkat
- Anestesia de Paciente PediátricoDokumen4 halamanAnestesia de Paciente PediátricoPollín GrinshBelum ada peringkat
- Cerebro Lys inDokumen18 halamanCerebro Lys inKathleen PalomariaBelum ada peringkat
- OTC Advisor - Fever, Cough, Cold, and Allergy FINAL PDFDokumen33 halamanOTC Advisor - Fever, Cough, Cold, and Allergy FINAL PDFmorsi0% (1)
- 0812 Hypoxic Ischemic Encephalopathy PDFDokumen35 halaman0812 Hypoxic Ischemic Encephalopathy PDFPutriBelum ada peringkat
- Antipyretic Therapy: K.E. ElizabethDokumen1 halamanAntipyretic Therapy: K.E. ElizabethShruthi KyBelum ada peringkat
- 0091 - 010 - Fever and The Inflammatory ResponseDokumen6 halaman0091 - 010 - Fever and The Inflammatory ResponsePedro Rodriguez ABelum ada peringkat
- Literature Review Febrile SeizureDokumen6 halamanLiterature Review Febrile SeizureArdyanto WijayaBelum ada peringkat
- Jurnal Terapi Rendam Kaki PDFDokumen7 halamanJurnal Terapi Rendam Kaki PDFFIRMAN SYAH PERMADIBelum ada peringkat
- Targeted Temperature Management in Brain Injured  Patients PDFDokumen23 halamanTargeted Temperature Management in Brain Injured  Patients PDFCamilo Benavides BurbanoBelum ada peringkat
- Urits2019 Article AComprehensiveUpdateOfCurrentADokumen10 halamanUrits2019 Article AComprehensiveUpdateOfCurrentAyantiBelum ada peringkat
- Thermal Hydrotherapy Improves Quality of Life and Hemodynamic Function in Patients With Chronic Heart FailureDokumen6 halamanThermal Hydrotherapy Improves Quality of Life and Hemodynamic Function in Patients With Chronic Heart FailurearitabrunoBelum ada peringkat
- NursingCareinFever VrdiNorden1996Dokumen5 halamanNursingCareinFever VrdiNorden1996hany abo fofaBelum ada peringkat
- (Ingles) Aproximación Febril en El Paciente en UCIDokumen14 halaman(Ingles) Aproximación Febril en El Paciente en UCIRoberto Augusto Laos OlaecheaBelum ada peringkat
- Thermal Regulation: Mary Frances D. PateDokumen17 halamanThermal Regulation: Mary Frances D. PateWinny Shiru MachiraBelum ada peringkat
- Prostaglandin and Endorphin Levels in Adolescent Primary Dismenore Given Warm and Cold HydrotherapyDokumen7 halamanProstaglandin and Endorphin Levels in Adolescent Primary Dismenore Given Warm and Cold HydrotherapyRoro RatuningrumBelum ada peringkat
- Febrile SeizureDokumen8 halamanFebrile Seizureanon_944507650Belum ada peringkat
- Voluntary Activation of The Sympathetic Nervous System and Attenuation of The Innate Immune Response in HumansDokumen6 halamanVoluntary Activation of The Sympathetic Nervous System and Attenuation of The Innate Immune Response in HumansGerson De La FuenteBelum ada peringkat
- Manejo de La Sepsis 2Dokumen5 halamanManejo de La Sepsis 2Rachmi Pratiwi Febrita PartiBelum ada peringkat
- Fernandez, John Michael BSN403 Group 10: I. Clinical QuestionDokumen5 halamanFernandez, John Michael BSN403 Group 10: I. Clinical QuestionJohn Michael FernandezBelum ada peringkat
- Hypothermia Pa Tho PhysiologyDokumen11 halamanHypothermia Pa Tho Physiologygvazquez85Belum ada peringkat
- Drug Fever - UpToDateDokumen17 halamanDrug Fever - UpToDatehgeniauxBelum ada peringkat
- Improving EyesightDokumen2 halamanImproving Eyesight2 FunkyBelum ada peringkat
- Technical Specialist Interview Questions: Topinterviewquestions - InfoDokumen11 halamanTechnical Specialist Interview Questions: Topinterviewquestions - Info2 FunkyBelum ada peringkat
- Yoga and CelibacyDokumen7 halamanYoga and CelibacyIvan CilerBelum ada peringkat
- Words of WisdomDokumen2 halamanWords of Wisdom2 FunkyBelum ada peringkat
- Improving EyesightDokumen2 halamanImproving Eyesight2 FunkyBelum ada peringkat
- MCITP Windows Admin Interview QuestionsDokumen20 halamanMCITP Windows Admin Interview Questions2 FunkyBelum ada peringkat
- VNC For Secure ConnectionsDokumen1 halamanVNC For Secure Connections2 FunkyBelum ada peringkat
- Old Sayings Quotes and QuipsDokumen9 halamanOld Sayings Quotes and Quips2 FunkyBelum ada peringkat
- Acharya, Brajaratna - Vedic MantrasiddhiDokumen59 halamanAcharya, Brajaratna - Vedic Mantrasiddhi2 FunkyBelum ada peringkat
- Ebook - Hack - Discovery NmapDokumen16 halamanEbook - Hack - Discovery Nmapapi-26021296100% (3)
- IpnatDokumen1 halamanIpnat2 FunkyBelum ada peringkat
- Golden Dawn - Meditation With The Archangel GabrielDokumen2 halamanGolden Dawn - Meditation With The Archangel GabrielSargeras777100% (4)
- DruggedDokumen2 halamanDrugged2 FunkyBelum ada peringkat
- Lab2 LectureDokumen57 halamanLab2 Lecture2 FunkyBelum ada peringkat
- Shrimad Valmiki Ramayan SKT Hindi DpSharma Vol07 YuddhaKandaPurvardh 1927Dokumen739 halamanShrimad Valmiki Ramayan SKT Hindi DpSharma Vol07 YuddhaKandaPurvardh 1927rudragni108100% (1)
- Rife FrequenciesDokumen3 halamanRife Frequencies2 Funky88% (16)
- Ipf HowtoDokumen56 halamanIpf Howto2 FunkyBelum ada peringkat
- Ashta Lakshmi StotramDokumen3 halamanAshta Lakshmi Stotramsindhu.s88% (8)
- Tantra of The Great Liberation: This Version of Mahanirvana Tantra (Edition 1913) Has Been Coping FromDokumen14 halamanTantra of The Great Liberation: This Version of Mahanirvana Tantra (Edition 1913) Has Been Coping From2 FunkyBelum ada peringkat
- Ak 200401 YoginisDokumen2 halamanAk 200401 Yoginis2 FunkyBelum ada peringkat
- Shrimad Valmiki Ramayan SKT Hindi DpSharma Vol07 YuddhaKandaPurvardh 1927Dokumen739 halamanShrimad Valmiki Ramayan SKT Hindi DpSharma Vol07 YuddhaKandaPurvardh 1927rudragni108100% (1)
- 72 Spirits From Weyer &CDokumen2 halaman72 Spirits From Weyer &C2 FunkyBelum ada peringkat
- Ashta Lakshmi StotramDokumen3 halamanAshta Lakshmi Stotramsindhu.s88% (8)
- Filter SamplesDokumen8 halamanFilter Samples2 FunkyBelum ada peringkat
- Jataka ChandrikaDokumen14 halamanJataka ChandrikalovershivaBelum ada peringkat
- Ashtavakra GitaDokumen9 halamanAshtavakra GitaNikul JoshiBelum ada peringkat
- Tantra of The Great Liberation: This Version of Mahanirvana Tantra (Edition 1913) Has Been Coping FromDokumen14 halamanTantra of The Great Liberation: This Version of Mahanirvana Tantra (Edition 1913) Has Been Coping From2 FunkyBelum ada peringkat
- Julie-Ann Amos - Be Prepared! Pass That Job Interview (4th Ed.) (2009)Dokumen97 halamanJulie-Ann Amos - Be Prepared! Pass That Job Interview (4th Ed.) (2009)Cristian JimboreanBelum ada peringkat
- Qameic Seals of The ArchangelsDokumen6 halamanQameic Seals of The Archangelsasterion32100% (6)
- On Call Survival Guide PDFDokumen78 halamanOn Call Survival Guide PDFBangun Said SantosoBelum ada peringkat
- Design Consideration in Reducing Stress in RPDDokumen11 halamanDesign Consideration in Reducing Stress in RPDAnkit NarolaBelum ada peringkat
- Flight Surgeon BrochureDokumen2 halamanFlight Surgeon BrochurejohnsmartsBelum ada peringkat
- Notes GITDokumen7 halamanNotes GITEhsanTamizBelum ada peringkat
- Neonatal Care Pocket Guide For Hospital Physicians Neonatal Care Pocket Guide For Hospital PhysiciansDokumen75 halamanNeonatal Care Pocket Guide For Hospital Physicians Neonatal Care Pocket Guide For Hospital PhysiciansSebastian SpatariuBelum ada peringkat
- Websites For Review of RadiologyDokumen1 halamanWebsites For Review of RadiologyHaluk AlibazogluBelum ada peringkat
- Egyptian Hospital Accreditation Program: Standards: Sixth Edition May 2005Dokumen71 halamanEgyptian Hospital Accreditation Program: Standards: Sixth Edition May 2005khayisamBelum ada peringkat
- KaranDokumen6 halamanKaranogidoBelum ada peringkat
- Medical and Mental Health NeedsDokumen10 halamanMedical and Mental Health NeedsKim OlsenBelum ada peringkat
- NPWT RENASYS and PICO Clinical GuidelinesDokumen78 halamanNPWT RENASYS and PICO Clinical GuidelinesAgung GinanjarBelum ada peringkat
- PLLV Client Consent FormDokumen4 halamanPLLV Client Consent Formapi-237715517Belum ada peringkat
- A LilingDokumen3 halamanA LilingJohn Vincent Dy OcampoBelum ada peringkat
- Guidelines For The Diagnosis and Treatment of Cobalamin and Folate DisordersDokumen6 halamanGuidelines For The Diagnosis and Treatment of Cobalamin and Folate DisordersOndire PatrickBelum ada peringkat
- Fluoride TherapyDokumen4 halamanFluoride TherapyمعتزباللهBelum ada peringkat
- Androgenetic Alopecia and Coronary Artery Disease CASE CONTROL STUDY DR RAHUL KUMAR SHARMA SKIN SPECIALIST AJMERDokumen2 halamanAndrogenetic Alopecia and Coronary Artery Disease CASE CONTROL STUDY DR RAHUL KUMAR SHARMA SKIN SPECIALIST AJMERRahul SharmaBelum ada peringkat
- Css Rizky Rafiqoh Afdin InggrisDokumen19 halamanCss Rizky Rafiqoh Afdin InggrisSyukri Be DeBelum ada peringkat
- Faculty of Medicine - Cairo University Program Specification For MBBCH (2010-2011)Dokumen11 halamanFaculty of Medicine - Cairo University Program Specification For MBBCH (2010-2011)Osama MahfouzBelum ada peringkat
- Neonatology Today May 2023 NeoHeart at WCDokumen332 halamanNeonatology Today May 2023 NeoHeart at WCTANDO JAM THE GREATBelum ada peringkat
- LMRASSIGNMENTDokumen2 halamanLMRASSIGNMENTjaoBelum ada peringkat
- Arellano University: Jose Abad Santos CampusDokumen7 halamanArellano University: Jose Abad Santos CampusLloyd VargasBelum ada peringkat
- Canadian Journal of Emergency MedicineDokumen4 halamanCanadian Journal of Emergency MedicineWily GustafiantoBelum ada peringkat
- Lipa Muz Ter 05 eDokumen82 halamanLipa Muz Ter 05 ezero LinBelum ada peringkat
- ScheduleDokumen7 halamanScheduleJigar AnadkatBelum ada peringkat
- Shoes and Techniques Hans - April - 2014Dokumen214 halamanShoes and Techniques Hans - April - 2014L.E. Velez97% (39)
- Pulmonary EdemaDokumen28 halamanPulmonary EdemaMohammed Elias100% (1)
- Speech & Language Therapy in Practice, Spring 1999Dokumen32 halamanSpeech & Language Therapy in Practice, Spring 1999Speech & Language Therapy in PracticeBelum ada peringkat
- Singh 2016 PDFDokumen2 halamanSingh 2016 PDFAffina Noor RasyidyaBelum ada peringkat
- 1319 FullDokumen5 halaman1319 FullFreddy Campos SotoBelum ada peringkat
- Periodontal Case StudyDokumen26 halamanPeriodontal Case StudySwapnilSauravBelum ada peringkat
- Sudden Onset Leg PainDokumen16 halamanSudden Onset Leg PainNafisNomanBelum ada peringkat