DSA10 Scoliosis, Posture and Muscle Balance
Diunggah oleh
William JonesHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
DSA10 Scoliosis, Posture and Muscle Balance
Diunggah oleh
William JonesHak Cipta:
Format Tersedia
DSA10: Scoliosis, Posture and Muscle Balance
Sharon Gustowski, DO, MPH
Reading Assignment(s)- This DSA
OPTIONAL/Supplemental
Foundations of Osteopathic Medicine. (2010). Chila, Anthony G. Lippincott Williams & Wilkins, 3rd Edition.
Chapter 36, Postural Considerations in Osteopathic Diagnosis and Treatment
There is a really great quizlet card set someone else made that I copied and edited to our quizlet course that
has most of this info in them. Students can substitute them for the info about scoliosis, x-ray measurements
and heel lift therapy in this DSA. Note, however, the quizlet set DOES NOT contain info about the postural
balance model or home exercises.
Objectives:
A. Integrate a postural screening exam into a standard physical exam.
B. Recall the differential diagnosis for patients who have various postural abnormalities, including
kyphosis, lordosis or scoliosis.
C. Recognize the indications for screening exams for scoliosis.
D. Recognize the indications for radiologic exams related to posture and know which tests to order.
E. Recall first-line interventions for postural abnormalities once they are identified.
F. Identify sacral-base unleveling.
G. Apply heel-lift therapy for patients with sacral base unleveling
H. Using a postural-balance model, identify which muscle groups are prone to weakness and which ones
are prone to tightness.
I. Design a simple home exercise program or physical therapy prescription for patients who have postural
abnormalities.
A. Integrate a postural screening exam into a standard physical exam.
C. Recognize the indications for screening exams for scoliosis.
Be sure the foundation is level and all will be well. -A.T. Still, MD, DO
A full standing postural screening exam (SPSE), which includes a screen for scoliosis, should be a part of your
standard complete history and physical. This exam can be performed in about 2 minutes. How and when a
physician chooses to perform this exam is variable, but it is recommended
that you perform it regularly in the same order. Dr. Gustowski performs
this exam first, as part of the transition of the patient sitting in the chair to
sitting on the examination table.
The state of Texas mandates that spinal screening for scoliosis be
performed at 6th and 9th grade. You can find out more at this website:
http://www.dshs.state.tx.us/spinal/spinalguide.shtm
The intention is to identify adolescents
with small spinal curves and refer them
for treatment before these curves
become too severe. Literature does not
support or refute the usefulness of this
screening exam. Scoliosis is present
when there is a rib hump. There may be
1 or 2, depending on if the curve is C- or
S-shaped.
DSA10: Scoliosis, Posture and Muscle Balance
Sharon Gustowski, DO, MPH
B. Recall the differential diagnosis for patients who have various postural abnormalities, including
kyphosis, lordosis or scoliosis.
As the twig is bent so grows the tree.
The standing postural screening exam is designed to screen for postural abnormalities and is part of
the data that is gathered to determine a diagnosis. Sometimes a postural abnormality is not contributing to a
patients chief complaint. If this is case, make note and recheck for progression on subsequent visits.
Often, patients are unaware of their posture as postural abnormalities do not always cause pain. When
patients have postural abnormalities, it is important to differentiate functional from structural ones. Functional
abnormalities are often reversible and may be treatable
with OMT, physical therapy and exercise. Functional
curves include those due to sprains/strains, somatic
dysfunction, muscular imbalance, and poor posture.
Structural abnormalities may require more aggressive
treatment such as surgery, and for pain relief, injections or
pharmaceuticals. Structural curves include those due to
boney or ligamentous or muscular conditions that are not
changeable, such as congenital malformations,
compression fractures, short leg syndrome or severe
arthritic conditions.
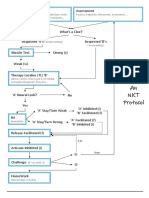
Determine if the curve is structural or functional
using active or passive range of motion testing as shown
in the diagram to the right. A nonstructural curve is the
same as a functional or compensatory curve.
The following text is from: Campbells Operative Orthopaedics , Twelfth Edition S. Terry Canale, and James H. Beaty
Chapter 41 , 1691-1895.e24 Copyright 2013 by Mosby, an imprint of Elsevier Inc. Chapter 41 Scoliosis and Kyphosis
Scoliosis
The word scoliosis is derived from the Greek word meaning crooked. Scoliosis is defined as a lateral deviation of the
normal vertical line of the spine. The lateral curvature of the spine also is associated with rotation of the vertebrae. This
produces a three-dimensional deformity of the spine that occurs in the sagittal, frontal, and coronal planes.
The Scoliosis Research Society recommends that idiopathic scoliosis be classified according to the age of the patient
when the diagnosis is made. Infantile scoliosis occurs from birth to 3 years of age; juvenile idiopathic scoliosis, between
the ages of 4 and 10 years; and adolescent idiopathic scoliosis, between 10 years of age and skeletal maturity. This
traditional chronological definition of scoliosis is important because major differences exist between the subtypes ( Table
41-1 ).
TABLE 41-1 Classification of Idiopathic Scoliosis by Age
PARAMETER
Age at presentation
Male:female
INFANTILE
Birth to 3 yr
1:1 to 2:1
Incidence
United States: 2%-3%
Great Britain: 30%
Left thoracic
L:R (2:1)
Left thoracic/right lumbar
Mental deficiency, CDH,
plagiocephaly, congenital
heart defects
High
Curve types
Associated findings
Risk of
cardiopulmonary
compromise
Risk of curve
progression
<6 mo: low
>1 yr: high
JUVENILE
4 to 9 yr
<6 yr: 1:3
>6 yr: 1:6
United States: 12%-15%
Great Britain: 12%-15%
Right thoracic
R:L (6:1)
ADOLESCENT
10 to 20 yr
1:6
None
None
Intermediate
Low
67%
23%
United States: 85%
Great Britain: 55%
Right thoracic
R:L (8:1)
DSA10: Scoliosis, Posture and Muscle Balance
Sharon Gustowski, DO, MPH
Rate of curve
progression
Curve resolution
Curve magnitude and
maturity
Orthotic management
Surgical treatment
Risk of crankshaft
Gradual progression: 2 to 3
degrees/yr
Malignant progression: 10
degrees/yr
<1 yr: 90%
>1 yr: 20%
Gradual progression: 70 to
90 degrees
Malignant progression: >90
degrees
Effective at delaying and
slowing rate of progression
Ultimate progression: 100%
Instrumentation without
fusion <8 yr
After 8 y: ASF-PSF
After 11 y: PSF
High
Progression at puberty: 6
degrees/yr
Malignant progression: 10
degrees/yr
20%
1 to 2 degrees/month during
puberty
Progression at puberty: 50 to
90 degrees
Malignant progression: >90
degrees
Decreases rate of progression
until puberty (failure rate: 30%
to 80%)
Instrumentation without fusion
<8 yr
After 8 y: ASF-PSF
After 1 y: PSF
High
Curves > 90 degrees are rare
Rare
Effectively controls curves <
40 degrees (success rate:
75% to 80%)
PSF with instrumentation
ASF if younger than 11 yr with
open triradiate cartilage
Low
Modified from Mardjetko SM: Infantile and juvenile scoliosis. In Bridwell KH, DeWald RL, editors: The textbook of spinal surgery, ed 2, Philadelphia,
1997, Lippincott-Raven.
Scoliosis also can be classified based on the etiology and associated conditions. Idiopathic scoliosis is the
most common type seen, but the exact etiology of this type of scoliosis is not known. Congenital scoliosis is
caused by a failure in vertebral formation or segmentation of the involved vertebrae. Scoliosis also can be
classified based on associated conditions, such as neuromuscular disorders (cerebral palsy, muscular
dystrophy, or other neuromuscular disorders), associated syndromes, or generalized disease
(neurofibromatosis, Marfan syndrome, bone dysplasia, tumors, or post irradiation). A distinction should be
made between early-onset and late-onset scoliosis because the deformity may affect cardiopulmonary
development. During childhood, not only do the lungs grow in size, but also the alveoli and arteries multiply
and the pattern of vascularity changes. The alveoli in the pulmonary tree increase by about 10-fold between
infancy and 4 years of age and are not completely developed until 8 years of age. Scoliotic deformity limits the
space available for lung growth, and children who develop significant scoliosis before the age of 5 years
generally have disabling dyspnea or cardiorespiratory failure.
Scoliosis
1:20 children develop some scoliosis by age 10-15, and
1:200 have symptoms.
The curve is amed by side of convexity. If kyphosis is also
present, then the curve may be called a kyphoscoliosis
Severity classification is based on an x-ray measurement
called the Cobb angle:
Mild = 5-15 degrees.
The use of a brace is recommended with curves
greater than 25. Literature regarding the use of
exercise, physical therapy or OMT is scant, but
those modalities are recommended
Moderate = 15-45 degrees
Surgery is indicated with curves that reach 45
Severe = >50 degrees
This degree of curvature can compromise cardiac
and lung function.
Causes of Scoliosis
Causes of scoliosis are divided into Congenital, Acquired or
Idiopathic. Between 70-90% of cases of scoliosis are
idiopathic- that means that no one knows the cause. However,
3
DSA10: Scoliosis, Posture and Muscle Balance
Sharon Gustowski, DO, MPH
somatic dysfunction is not considered a cause of scoliosis in most medical literature, and thus the incidence of
scoliosis due to somatic dysfunction is not known.
Congenital
Associated with other syndromes
Failure of Fusion (hemi-vertebrae,
(Klippel-Feil syndrome)
wedge vertebrae
Neuromuscular syndrome
Facet tropism
Failure of Segmentation (bar vertebrae)
Often requires bracing, surgery, etc. No good studies on use of OMT, physical therapy or exercise.
About 35% incidence of patients w/congenital scoliosis having other conditions and spinal cord and
nervous system tumors/anomalies. Aggressive investigation (MRI) and treatment is recommended.
Use OMT as adjunct to assist with muscle balance and growth.
Acquired
Degenerative process such as arthropathies,
spinal stenosis, degenerative disc disease
Spinal tumors
Post-Infection
Bone metabolic disorders (rickets,
osteoporosis)
Short leg syndrome
Surgery
Trauma: fractures, strain and sprains,
especially in the lower extremity (somatic
dysfunction)
Radiation in/near the spine
Poor habitual posture
Pregnancy
Obesity
Muscular imbalance- Muscular imbalances
may be acquired through trauma or
neuromuscular diseases
Gait abnormality- gait abnormalities may be
acquired through trauma or neuromuscular
diseases
OMT may be primary treatment in cases where somatic dysfunction is the cause
Idiopathic
No known cause= no definitive treatment. Rule out other causes (congenital and acquired). OMT may be
primary treatment.
NOT ON EXAM, but some food for thought: The metaphysical/alternative medicine practitioners relate scoliosis to The
inability to flow with the support of life; fear and trying to hold onto old ideas; not trusting life; lack of integrity; no courage
of convictions. For more information about metaphysical causations, try You Can Heal Your Life by Louise L. Hay, or
Anatomy of the Spirit by Carolyn Myss.
Scoliosis due to Somatic Dysfunction
Scoliosis due to somatic dysfunction alone should be reversible- as somatic dysfunction is treatable with OMT.
Scoliosis due to somatic dysfunction is the result of the body compensating to keep the eyes level with the
horizon.
Common areas of somatic dysfunction which may lead to scoliosis include:
Ankle sprains in which the calcaneus/talus remains out of alignment causing foot pronation and
subsequent innominate rotation and scoliosis (see diagram below).
Innominate and Sacral Shears significantly alter the alignment of the pelvis, and the spine
compensates.
Psoas strain can cause side bending to the same side, and consequent compensation in the rest of the
spine.
Cranial strains, especially a lateral strain. Consider the sphenoid and occiput as the top two vertebrae.
DSA10: Scoliosis, Posture and Muscle Balance
Sharon Gustowski, DO, MPH
Kyphosis (also called thoracic kyphosis) and Lumbar Lordosis
The causes of kyphosis and lordosis include those that cause scoliosis. In addition, lumbar lordosis can be
due to spondylolisthesis or spondylolysis. Work-up and treatment is similar to that for scoliosis, although
bracing is not commonly used. OMT may or may not resolve the abnormal curves, however, OMT will help
preserve normal functioning of visceral organs (neurologic model), lymphatic &venous circulation
(respiratory/circulatory model), rib cage motion (biomechanics/ metabolic/energy model).
D. Recognize the indications for radiologic exams related to posture and know which tests to order.
Radiologic exams should be performed on children with newly diagnosed scoliosis. If OMT is being
utilized as the primary treatment and no congenital malformation is identified (the scoliosis is mild, the child has
had minor trauma, there are no cognitive, developmental, metabolic or neurologic deficits), it is acceptable to
perform a trial of OMT, physical therapy and home exercises for 1-2 months prior to obtaining radiographs, as
the curve may be functional and therefore treatable with OMT. Plain film x-rays are ordered and are often
called a scoliosis series or a postural series. They include PA and lateral views of the cervical, thoracic and
lumbar spines. The radiologist will measure the degree of spinal curvatures (Cobb angle, lumbosacral angle)
and identify bony abnormalities. Yearly x-rays can be performed to measure curve progression.
Osteopathic physicians have developed a method for evaluating the levelness of the sacral base, which
can cause scoliosis, called Standing Postural X-rays. Foundations of Osteopathic Medicine textbooks (all
editions) have chapters which discuss how these x-rays are obtained and measured. The x-rays are accurate
in detecting sacral base unleveling within 1.5 3.0 mm3. The patient stands barefoot with feet parallel and
under hips. The floor must be level and the X-ray equipment is square to the floor. A-P pelvis X-ray taken with
metal plumb line if available. Measurements are then taken to determine the amount of declination the sacral
base, usually in millimeters. The diagram below represents these measurements. In class, we will go over
how these measurements are
made.
DSA10: Scoliosis, Posture and Muscle Balance
Sharon Gustowski, DO, MPH
Foundations of Osteopathic Medicine.
(2010). Chila, Anthony G. Lippincott
Williams & Wilkins, 3rd Edition. Chapter
36, Postural Considerations in
Osteopathic Diagnosis and Treatment
E. Recall first-line interventions for postural abnormalities once they are identified.
Up to 70% of the population has a short leg. (Hoffman Kent S., Hoffman Lorrie L.: Effects of adding sacral
base leveling to osteopathic manipulative treatment of back pain: a pilot study. JAOA 1994;94:217-226.)
Out of 1100 patients with an unlevel sacral base, leveling the discrepancy partially or completely alleviated
symptoms of 90% of the patients. However, disparities less than 9 mm (3/8 inch) seldom cause low back pain.
(Beal M. D.: A review of the short leg problem. JAOA 1950;50:109-121.)
Severe curves identified early in life require more aggressive treatment due to the associated
cardiopulmonary risks. Otherwise, treatment is based on each patients presentation, associated conditions
and desire for cosmetic correction (for self-esteem, etc.). There is no definitive treatment for scoliosis and one
treatment does not fit all. OMT can be performed in conjunction with other treatments. OMT is directed at
removing somatic dysfunction anywhere in the body to promote optimal
In addition to standard care, physical therapy and home exercise programs are indicated. Home exercise
programs may include home stretching & strengthening, weight training, swimming, yoga, pilates, tai-chi.
Exercises which are performed bilaterally and include the spine are best.
Osteopathic physicians are in a unique position to identify and treat scoliosis due to sacral- base
unleveling with a combination of OMT, home exercises, and use of a heel lift.
DSA10: Scoliosis, Posture and Muscle Balance
Sharon Gustowski, DO, MPH
F. Identify sacral-base unleveling.
Sacral base unleveling is where the sacrum tilts to one side due to a short leg (short leg syndrome). This
condition is identified using as Standing Postural Screening Exam (iliac crest heights are unequal), along with
identification of a superior medial malleolus on supine exam. The short leg can be congenital or acquired due
to any trauma, boney, muscular or ligamentous disorder of the low back, pelvis or lower extremity. Surgery is
also considered a trauma to the body and hip or knee replacements can result in a leg length discrepancy also.
Ankle joint sprains are one example of a common cause of a short leg, which is often treatable with OMT.
Short legs are often congenital. Remember that bones grow along lines of stress. Short leg syndrome should
only be diagnosed after removal of all reversible somatic dysfunctions and when other causes have been ruled
out.
Note the following changes which occur with a short leg The iliac crest is lower on the side of the short leg (standing
exam)
The medial malleolus is superior on the side of the short leg
(supine exam)
The pelvis side shifts (side bends) away from the side of the
short leg
The innominate rotates anteriorly on the side of the short
leg
o The opposite innominate rotates posteriorly on the
long leg side
The lumbar spine side bends on the side of the short leg
(convexity is opposite short leg side)
The thoracic and cervical spines compensate to keep the
eyes level
Treatment of short leg syndrome includes proper diagnosis and
identification of the cause of the short leg. OMT is indicated to
remove somatic dysfunction which may be causing the short
leg. This may take at least 3 treatments. Patients who do not
achieve correction of 3 OMT treatments should have standing
postural x-rays performed for determination of the amount of
sacral base unleveling with potential initiation of heel lift
therapy. In the event that standing postural x-rays are not
obtainable, empiric use of a heel lift can be done but its not recommended routinely.
Lift therapy is based on the millimeters of declination of the sacral base.
G.
Apply heel-lift therapy for patients with sacral base unleveling
Probably not necessary to lift if sacral base unleveling <5 mm
Lift based on the sacral base, not femoral head heights
Lift only if side of lumbar convexity is on the side of the short leg
One method to use when initiating a heel lift:
Start at 1/16 of an inch in fragile patients (elderly, chronically ill)
Begin with 1/8 of an inch if not fragile
Increase lift no faster than every 2 weeks
Increase lift to comfort of the patient (resolution of symptoms)
Use no more than inside the shoe. If more is needed, the lift has to be built into the heel by a
cobbler (shoe repair person).
Replace full length immediately if short leg is due to anatomic changes (fracture, hip prosthesis)
Another method is to use the Heilig Formula: L<[SBU]/[D+C]
7
DSA10: Scoliosis, Posture and Muscle Balance
Sharon Gustowski, DO, MPH
L= Lift, SBU (Sacral Base Unleveling); D=Duration (1= 0-10 yrs, 2= 11-30, 3= >30); C
Compensation (0= none, 1= lumbar rotation and sidebending, 2 = boney changes)
Some Symptoms of a Short Leg include: Pain in one or more of these regions: plantar fascia, ankle, knee, low
back, hip, thoracic, neck. Headache and fatigue are often also present. If a heel lift is used improperly, it can
produce the same symptoms! Be careful using a heel lift!
H. Using a postural-balance model, identify which muscle groups are prone to weakness and which
ones are prone to tightness.
The following is from: Robert Kessler, D.O., Department of Osteopathic Manipulative Medicine, 2010, Touro
University Nevada College of Osteopathic Medicine
Muscle Imbalance
An initial musculoskeletal injury causes hypertonic muscles. Hypertonic muscles:
have lower excitability thresh holds (facilitation).
become activated more easily during movements when they should not be active.
more powerfully inhibit their antagonists (Sherringtons law of reciprocal inhibition).
delay the activation of agonists in the same group, which are relatively inhibited.
This leads to improper firing patterns during activity. These effects are proportional to the degree of hyper
tonicity. The longer these adaptive patterns of facilitation and inhibition last, the greater the ceroplastic
reprogramming (engrains) of movement occur as coordinated between the central and peripheral nervous
systems. (hard wiring abnormal movement patterns into place)
Muscle Imbalance Results in:
Abnormal proprioception from the periphery, changing normal motor response.
Decreased range of motion.
Abnormal gait.
Unequal pressure on weight bearing joints.
Centralization of the adaptation but uncoordinated movements from the periphery.
8
DSA10: Scoliosis, Posture and Muscle Balance
Sharon Gustowski, DO, MPH
The first layer of these adaptations thus make further injury more likely and there for cause more
adaptations in a vicious cycle of injury-adaptation-injury-adaptation
This ultimately results in patterns of dysfunction, which manifest themselves clinically.
Region
Lower Extremity
Upper Extremity
Muscles Prone to Hypertonicity
Iliopsoas
Quadratus lumborum
Piriformis
Hamstrings
Lumbar erector spinae
Rectus femoris
Tensor fascia lata
Pectorals
Latissimus dorsi
Upper trapezius
Scalenes
Sternocleidomastoid
Suboccipital group
Muscles Prone to Inhibition
Gluteous maximus, medius,
minimus
Rectus abdominis
External and internal obliques
Vastus lateralis and medius
Tibialia anterior
Fibularis longus and brevis
Rhomboids
Lower and middle trapezius
Rhomboids
Deltoids
Supraspinatus
Longus and capitus colli
Muscles prone to hypertonicity should be stretched. Muscles prone to inhibition (also called weakness) should
be strengthened. Stretch just up to point of pain- stretches should not hurt. Strengthen to the point of fatigue,
not pain. Keep good posture when exercising.
Case History to illustrate postural balance model
A 32 year old patient presents with chronic back pain. He was fine when he started medical school 2 years
ago but over the last 6 months he has developed a dull lumbar ache, which is worst when he first gets out of
bed or gets out of a chair after sitting for a long time. After a class he has trouble straightening up but after he
slowly stretches he feels better. He also has dull infrascapular aching and a frequent sub occipital headache.
The following are your findings from a Standing Postural Screening Exam and one reason why these
dysfunctions occur, according to a biomechanical/muscle balance model
Increased lumbar and cervical lordosis
The lumbar lordosis is maintained by the hypertonic iliopsoas, which causes a deep dull ache in the
lumbar area and a difficulty in extension (hard to get up from chair). This begins because he
habitually sits 14 hours a day, with shortened iliopsoas, and doesnt stretch. The deep, anterior
cervicals are inhibited while the superficial cervicals become hypertonic, leading to the neck moving
anteriorly, its lordosis increasing and hypertonicity of the suboccipital muscles , which must now
contract to keep the patients eyes forward
Increased thoracic kyphosis
Round shoulders
The latissimus dorsi, and pectorals become hypertonic leading to round shoulders and an increases
thoracic kyphosis.
Arms internally rotated
To allow the scapula to protract, the hypertonic pectoralis inhibit the lower trapezius and rhomboids.
Now there is instability of the scapula and the upper trapezius and levator scapula become
hypertonic to stabilize it.
Knees flexed
At the same time, the hypertonic iliopsoas inhibits the gluteal muscles.
You get hypertonicity of the hamstrings.
Flat feet
Reflexive inhibition of the tibialis anterior and peroneus longus and brevis cause flat feet.
9
DSA10: Scoliosis, Posture and Muscle Balance
Sharon Gustowski, DO, MPH
He will have pain at the junctional areas where the increased spinal curves cross the midline and at the
apexes of these curves (dull infrascapular and suboccipital pain).
I. Design a simple home exercise program or physical therapy prescription for patients who have postural
abnormalities.
Exercises have been given to you in the associated OMM Lab, which can be used in an exercise
program. Keep the program simple and use common sense- stretch areas of the low back and thighs in cases
of low back pain; stretch the neck and shoulders in cases of upper back or neck pain.
A home exercise program is designed to improve the quality of muscle function by stretching the
hypertonic muscles and retraining (strengthening) the inhibited muscles. Consider adding aerobic exercise to
improve nutritive support to the tissues.
Cases for OLM
Case 1
A 13-year-old female presents with scoliosis which was
detected at her school. She is asymptomatic. The patient has
no significant past medical history, in that she has had the
usual childhood illnesses, is up to date on her vaccines, has not
broken any bones, takes no medications and has had no
surgeries. She denies having any significant injuries but has
had numerous minor ones, all of which have healed. She plays
the violin and is on the soccer team at school.
Exam is positive for a rib hump on the right side in the midthoracics, the right shoulder is elevated, the left iliac crest is
elevated and thoracic kyphosis is present. Her spinal curve
does not resolve with side bending. DTRs, sensation, active
range of motion, and muscle strength in the upper and lower
extremities is intact. Osteopathic exam reveals T6-10 N SLRR,
R paravertebral muscle tightness in the thoracics, L PVM
tightness in the lumbars, Left innominate posteriorly rotated, OA
NSRRL, L 1st rib inhalation s/d. X-rays of her thoracic spine are
ordered, and measurements are on the diagram.
What is severity of this patients scoliosis?
What is an appropriate treatment strategy?
Case 2
A 32-year-old male presents with low back pain for 5 years. He denies acute trauma at the time and states
that it has slowly been getting worse to the point that he has pain almost daily. He denies paresthesias or
weakness in his extremities.
Review of systems is negative.
His past medical history is negative and he takes no medications.
Neurologic and Musculoskeletal strength exams are within normal limits
Standing Postural Screening Exam:
Right AC superior, right iliac crest superior, pelvis rotated to the right
Positive rib hump on the right mid-thoracics
Increased lumbar lordosis
Osteopathic Exam:
Right superior 1st rib, Scapula lateral with levator scapulae tender point, left positive standing
flexion test, L inferior ASIS, L superior PSIS, L medial malleolus superior, L2-5 NSRRL, R on R
sacral torsion, L pes planus
10
DSA10: Scoliosis, Posture and Muscle Balance
Sharon Gustowski, DO, MPH
The patient is informed that he has a scoliotic curve in his spine. Upon further questioning, he admits
to having noticed that his shoulders werent level and his trousers have had to be hemmed to different
lengths since he was a teenager.
Three OMT treatments directed at resolving his somatic dysfunctions results in 1-2 days of relief of his
pain but no resolution.
On the 4th visit, you order a standing postural x-ray (next 2 pages).
What is the patients innominate diagnosis?
What are his x-ray measurements?
What is the appropriate lift to begin with?
11
Anda mungkin juga menyukai
- Integrative Pathways: Navigating Chronic Illness with a Mind-Body-Spirit ApproachDari EverandIntegrative Pathways: Navigating Chronic Illness with a Mind-Body-Spirit ApproachBelum ada peringkat
- The Inverted Orthotic Technique: A Process of Foot Stabilization for Pronated FeetDari EverandThe Inverted Orthotic Technique: A Process of Foot Stabilization for Pronated FeetBelum ada peringkat
- Methods For Assessing Leg Length DiscrepancyDokumen13 halamanMethods For Assessing Leg Length DiscrepancyKanika SinhaBelum ada peringkat
- Lumbar Spine ExamDokumen2 halamanLumbar Spine ExamJulius AdamsBelum ada peringkat
- Naturopathic Medicine: By: Beverlyn C. Bagolos and Marianne MacanlayDokumen19 halamanNaturopathic Medicine: By: Beverlyn C. Bagolos and Marianne Macanlaynicole cenaBelum ada peringkat
- No Mas Dolor Con ProloDokumen562 halamanNo Mas Dolor Con ProlojfarcoBelum ada peringkat
- The Pettibon Spinal Biomechanics SystemDokumen67 halamanThe Pettibon Spinal Biomechanics Systemcristian darabanBelum ada peringkat
- Muscle Energy Technique OverviewDokumen4 halamanMuscle Energy Technique OverviewRia Sands100% (2)
- L Kalichman PDFDokumen28 halamanL Kalichman PDFShahul HameedBelum ada peringkat
- The Road To Good Health: Discover ChiropracticDokumen17 halamanThe Road To Good Health: Discover ChiropracticFioravanti AlessandroBelum ada peringkat
- AssessmentDokumen228 halamanAssessmentsylschebe22gmailBelum ada peringkat
- WWW - Chiropractic SportsDokumen5 halamanWWW - Chiropractic Sportsapi-3714923Belum ada peringkat
- Rs Ebook DownloadDokumen63 halamanRs Ebook DownloadDr-Heather McDowellBelum ada peringkat
- Motion Palpation Neil Davies PART 1Dokumen9 halamanMotion Palpation Neil Davies PART 1Scott JacksonBelum ada peringkat
- Spinal Care and Its Effects On Human Physiology in Sickness and in HealthDokumen196 halamanSpinal Care and Its Effects On Human Physiology in Sickness and in HealthMichael Koontz67% (3)
- Eye Movement Disorder PDFDokumen115 halamanEye Movement Disorder PDFGilberto FerreiraBelum ada peringkat
- NKT FlowChart - PDF Version 1 PDFDokumen2 halamanNKT FlowChart - PDF Version 1 PDFJay SarkBelum ada peringkat
- Application of Fascial Manipulation Technique in Chronic Shoulder Pain Ok PDFDokumen8 halamanApplication of Fascial Manipulation Technique in Chronic Shoulder Pain Ok PDFBruno DiasBelum ada peringkat
- Osteopathy ProspectusDokumen20 halamanOsteopathy Prospectussdun7Belum ada peringkat
- Spinal Manipulation For Back and Neck Pain Does It WorkDokumen3 halamanSpinal Manipulation For Back and Neck Pain Does It Workbkcc14Belum ada peringkat
- Electronic Edge ExampleDokumen138 halamanElectronic Edge Examplezarrin77Belum ada peringkat
- Medicare ListingDokumen9 halamanMedicare ListingCris CarrilloCarrilloBelum ada peringkat
- TECH 614 Full Spine I (Castellucci)Dokumen10 halamanTECH 614 Full Spine I (Castellucci)Robert StraubBelum ada peringkat
- The Nervous System: The Central Processing UnitDokumen192 halamanThe Nervous System: The Central Processing UnitHossein KhorramiBelum ada peringkat
- Gonstead Ifec ProneDokumen5 halamanGonstead Ifec ProneAurelien BoschatBelum ada peringkat
- CCEB Exam Content July 2013Dokumen24 halamanCCEB Exam Content July 2013StarLink1Belum ada peringkat
- CWK en DemoDokumen16 halamanCWK en DemoVishal YogiBelum ada peringkat
- Lecture 1: Lumbar: Indirect ObjectivesDokumen11 halamanLecture 1: Lumbar: Indirect ObjectiveseugeniaBelum ada peringkat
- 1 Reviews Evidences HandoutDokumen25 halaman1 Reviews Evidences Handoutsefhilla putriBelum ada peringkat
- M1 Introduction To Manual TherapyDokumen101 halamanM1 Introduction To Manual TherapySylvia LoongBelum ada peringkat
- ChiropracticDokumen4 halamanChiropracticYe Myint100% (1)
- Gonstead Chronology PDFDokumen6 halamanGonstead Chronology PDFstansimpson1122Belum ada peringkat
- The Chiropractor Starter GuideDokumen18 halamanThe Chiropractor Starter GuidejaneweiBelum ada peringkat
- Chiropractic Treatment PlanDokumen40 halamanChiropractic Treatment Planapi-542121685Belum ada peringkat
- Chiropractic Business Plan TemplateDokumen11 halamanChiropractic Business Plan TemplateAhmed M. RafatBelum ada peringkat
- Manipulation Education ManualDokumen51 halamanManipulation Education Manualpainfree888100% (1)
- Listing System C2 - L5Dokumen8 halamanListing System C2 - L5呂桂村Belum ada peringkat
- Chiropractic IntroductionDokumen17 halamanChiropractic IntroductionDr. Krishna N. Sharma100% (1)
- Neural Prolotherapy For NeuralgiaDokumen4 halamanNeural Prolotherapy For NeuralgiaMariel Yarrod100% (1)
- Common Medical Terms, Abbreviations, and Acronyms Approved For Arizona WIC UseDokumen7 halamanCommon Medical Terms, Abbreviations, and Acronyms Approved For Arizona WIC UseAsif Raza SoomroBelum ada peringkat
- Turocy Strain Counterstrain PATS06Dokumen46 halamanTurocy Strain Counterstrain PATS06Yap Grace K Xiulin100% (2)
- A Proposed Evidence-Based Shoulder Special Testing Examination Algorithm - Clinical Utility Based On A Systematic Review of The LiteratureDokumen14 halamanA Proposed Evidence-Based Shoulder Special Testing Examination Algorithm - Clinical Utility Based On A Systematic Review of The LiteratureAfonso MacedoBelum ada peringkat
- Chiropractic Marketing: Market Segmentation & Growth StrategyDokumen11 halamanChiropractic Marketing: Market Segmentation & Growth StrategySubhashis Priyadarshi Sahoo100% (1)
- Chiropractic Treatment Techniques-2016Dokumen9 halamanChiropractic Treatment Techniques-2016Dr. Mateen ShaikhBelum ada peringkat
- Physiotherapy and Mental HealthDokumen27 halamanPhysiotherapy and Mental Healthlilz_rodriguesBelum ada peringkat
- CLIN 4801 Tutorials On Descriptive ListingsDokumen5 halamanCLIN 4801 Tutorials On Descriptive Listingsjoe joeBelum ada peringkat
- The Effects of Scapular Stabilization Based Exercise Therapy On PDFDokumen15 halamanThe Effects of Scapular Stabilization Based Exercise Therapy On PDFElisabete SilvaBelum ada peringkat
- Fascial Dysfunction: Manual Therapy Approaches - Health Systems & ServicesDokumen6 halamanFascial Dysfunction: Manual Therapy Approaches - Health Systems & ServicesxamekytyBelum ada peringkat
- Welcome To FIT CHIROPRACTIC and Wellness CenterDokumen38 halamanWelcome To FIT CHIROPRACTIC and Wellness CenterKemberly Semaña PentonBelum ada peringkat
- Raphael Rettner - End PMS NowDokumen58 halamanRaphael Rettner - End PMS NowYuldash100% (1)
- Clinical Chiropractic Volume 14 Issue 1 March 2011Dokumen35 halamanClinical Chiropractic Volume 14 Issue 1 March 2011i_claudyaBelum ada peringkat
- Occupational Therapy Rehabilitation Paraplegic PatientDokumen7 halamanOccupational Therapy Rehabilitation Paraplegic PatientAlina PasăreBelum ada peringkat
- Regenerative Medicine Manual ISSCA 2020 EnglishDokumen21 halamanRegenerative Medicine Manual ISSCA 2020 EnglishDana MihutBelum ada peringkat
- Chiro HIODokumen18 halamanChiro HIOPierre SERPAGGIBelum ada peringkat
- 2018 Stretching Ebook LRDokumen11 halaman2018 Stretching Ebook LRUmme AyeshaBelum ada peringkat
- Week 2 Ortho Tests Figure NoDokumen14 halamanWeek 2 Ortho Tests Figure Noapi-468597987Belum ada peringkat
- What Can I Do With My Studies in Kinesiology?Dokumen3 halamanWhat Can I Do With My Studies in Kinesiology?hello12345helloBelum ada peringkat
- The Shoulder PainDokumen14 halamanThe Shoulder PainLev KalikaBelum ada peringkat
- Clinical Nutrition IntakeDokumen6 halamanClinical Nutrition IntakeAudrygodwynBelum ada peringkat
- Spine Owners Guide PDFDokumen139 halamanSpine Owners Guide PDFhiggs1Belum ada peringkat
- Antibiotics Chart 1Dokumen7 halamanAntibiotics Chart 1Vee MendBelum ada peringkat
- Epididymitis Practice Essentials: Signs and SymptomsDokumen43 halamanEpididymitis Practice Essentials: Signs and SymptomsbadbearpstBelum ada peringkat
- G.R. No. 132319. May 12, 2000Dokumen2 halamanG.R. No. 132319. May 12, 2000Chua RoxyBelum ada peringkat
- 3 On Your Side Investigates: Jailed and AbusedDokumen102 halaman3 On Your Side Investigates: Jailed and AbusedShaCamree GowdyBelum ada peringkat
- Be Your Own Doctor With Acupressure - Dr. Dhiren GalaDokumen69 halamanBe Your Own Doctor With Acupressure - Dr. Dhiren GalaParag Chhaper100% (2)
- Mindfulness and Psychology-Mark WilliamsDokumen7 halamanMindfulness and Psychology-Mark WilliamsssanagavBelum ada peringkat
- B.SC Nursing - 2019 - 2 - Aug Sept - Pharmacology Pathology andDokumen1 halamanB.SC Nursing - 2019 - 2 - Aug Sept - Pharmacology Pathology andshubham vermaBelum ada peringkat
- DC-TMD SQ Shortform 2013-05-12Dokumen2 halamanDC-TMD SQ Shortform 2013-05-12Luz MendozaBelum ada peringkat
- Endocrine System Review Flashcards - QuizletDokumen5 halamanEndocrine System Review Flashcards - QuizletDani Anyika100% (1)
- Cold Chain Medication List 2021Dokumen13 halamanCold Chain Medication List 2021sumaiyakhan880Belum ada peringkat
- Simultaneous Determination of Methylparaben + Propylparaben + Hidrocortisone Topical Cream PDFDokumen7 halamanSimultaneous Determination of Methylparaben + Propylparaben + Hidrocortisone Topical Cream PDFNájla KassabBelum ada peringkat
- Parecoxib PDFDokumen7 halamanParecoxib PDFawardani13Belum ada peringkat
- KalanchoeDokumen1 halamanKalanchoeAnonymous iOYpj92Belum ada peringkat
- Assessment Standard 4 Traits Employability Skills TESTDokumen5 halamanAssessment Standard 4 Traits Employability Skills TESTnurse1990Belum ada peringkat
- Hospital and Clinical Pharmacist PDFDokumen23 halamanHospital and Clinical Pharmacist PDFmajd67% (6)
- Cam4 6 1861Dokumen10 halamanCam4 6 1861Ćatke TkećaBelum ada peringkat
- Guidelines TAVI TAVRDokumen15 halamanGuidelines TAVI TAVRRossellaDisalvo100% (1)
- 35521Dokumen12 halaman35521Kyle MaogBelum ada peringkat
- Uremic Encephalopathy-ReviewDokumen30 halamanUremic Encephalopathy-ReviewFeddyFebriyantoManurung100% (1)
- Intensive Behavioral Therapy For Autism Spectrum Disorders: Coverage RationaleDokumen14 halamanIntensive Behavioral Therapy For Autism Spectrum Disorders: Coverage Rationalediana100% (1)
- Surving Sepsis Campaign ResultDokumen8 halamanSurving Sepsis Campaign Resultmaria arenas de itaBelum ada peringkat
- Nursing Note Sample 17Dokumen6 halamanNursing Note Sample 17Lanzen Dragneel100% (1)
- Drug Tariff July 2014 PDFDokumen784 halamanDrug Tariff July 2014 PDFGisela Cristina MendesBelum ada peringkat
- Genodermatosis MCQsDokumen152 halamanGenodermatosis MCQsDr.Tawheed88% (8)
- The Impact of Stress On Academic Success in College StudentsDokumen4 halamanThe Impact of Stress On Academic Success in College StudentsSha RonBelum ada peringkat
- Barium Swallow (Esophagram) :: Positions and Barium Images PurposeDokumen3 halamanBarium Swallow (Esophagram) :: Positions and Barium Images PurposeAaron SmithBelum ada peringkat
- 080 - Hospital Information Document For New StaffDokumen2 halaman080 - Hospital Information Document For New StaffleicesterbugBelum ada peringkat
- Rational Use of The Drug (Rud) : Rovina Ruslami, DR., SPPD, PHDDokumen31 halamanRational Use of The Drug (Rud) : Rovina Ruslami, DR., SPPD, PHDamaliaramadhaniBelum ada peringkat
- Nutrition in Pediatrics PDFDokumen1.121 halamanNutrition in Pediatrics PDFPutri Wulan Sukmawati100% (5)