Other Acupuncture Reflection 6
Diunggah oleh
Indra SyafriDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Other Acupuncture Reflection 6
Diunggah oleh
Indra SyafriHak Cipta:
Format Tersedia
techniques, which might include Sotai from
her earlier practice days, or a different
ordering of the needling and moxibustion,
demonstrating in the real-world clinical arena
that it is the actual patient, and her problem,
that drives the treatment, not a rigid
application of protocols. As someone who
kept prodding Kiiko Matsumoto Sensei to
develop a more clear series of steps for her
approach, which I have done for APM/CCA,
I find myself often discouraged by the overly
rigid way in which some of my students, and
graduates, and even faculty practice this
approach.
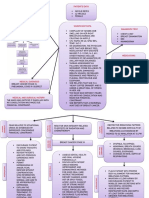
Part III: APM Pragmatics
Reflection Six: The steps to
APM Clinical Practice
THE PROBLEM:
One of the big risks in developing basic
protocols in order to teach students the
Ordinary Skills of Acupuncture is that
students and practitioners may miss the
complexity of the process, and begin to
merely apply these basic protocols with little
attention to what is actually required, or to
the larger changes that could take place, or
that are taking place outside the
practitioners awareness, thus selling their
own practice, and their patients, short in
many cases.
At times like those, I greatly appreciate her
serious reservations against standardizing her
approach in any way, and her readiness and
ability to go outside the protocols that do
emerge from her last two books whenever the
clinical reality requires it. This series of
Reflections so far has been my attempt to
problematize the development of the
APM/CCA approach over the past three
decades, so as to reveal more of the depth
and breadth such an approach can take on
for anyone who grapples, as I had to, with
the various traps and gaps that arose in the
process. What I practice is based first of all
on my own person, on my store of
experiences in the world, good and bad, in
sickness and in health, and no one has had
the same personal experiences as someone
else. Secondly, APM/CCA is based on
everything I have learned about the body, the
mind, and things spiritual, from within and
outside of AOM studies, which again no one
else would ever replicate in the same way.
And finally, the things that continue to
fascinate me about acupuncture, about
needling, my allergy to moxa, my interest in
having recourse only to those fine needles,
without cupping, without guasha, without tui
na, and in the Neo-Confucian approach to
embodied learning will not be replicated
exactly by someone else, and numerous
versions of this practice will emerge, by
graduates, and even by people who just read
Protocols and Practice
The use of repetitive protocols and strategies
can also lead to boredom or even burnout
which might account for how some AOM
graduates keep gravitating from one seminar
to another without ever settling in on a
personal style all their own. This issue is
something Kiiko Matsumoto has also
grappled with for the past 25 years, where
many students have trouble following her
deft and ever adaptable series of checks for
reflexes, and needling, and surveillance for
signs of significant changes that redirect how
the needling and moxa and ancillary
techniques are to be applied. Some who
finally feel they are grasping it will grow
despondent if Kiiko Matsumoto Sensei goes
into their booth only to critique their time
spent on a basic protocol, which they may be
doing exactly as described in one of her
recent books, when the actual problem the
patient came with has not changed yet. She
will often resort to a different series of
my books, who will refer to their practice as
APM, or something similar.
something, clarified something to the
patient, perhaps while performing the
physical examination or even while needling
a point, but just as often before leaving the
patient for 10 minutes or so after all the
needles have been inserted, or even when
saying a last thing to send the patient off,
that spirit clarity has just been initiated, that
the patient has just had a bodily-felt sense of
their acupuncture holding pattern, of what
was bringing them to this place and this
practice to remove some of these
obstructions: an experience that is so intense,
so important as to be beyond words. At such
moments, a practitioner totally in tune with
the patient might say something no more
articulate than: Pretty intense, No?
making any further conversation about what
just happened redundant.
After three decades of practice I am as
convinced as I was a decade ago that I had to
attach a name to my approach and I am
comfortable with the one that I have chosen.
It fits what I do, what I have developed over
my professional career. It situates
acupuncture as Wei KeExternal medicine
aimed, as Yitian Ni says so elegantly, at
navigating the channels, which is how it has
always been articulated in China. But I have
no interest in attempting to watch over how
those who use this practice name what they
do when they leave the college, if they ever
even trained here.
So as I end this Sixth Reflection, speaking
about what I love, what I do, what I continue
to practice without ever believing I will be
done making changes if they seem necessary
to teach this better, I realize that in the end
no one trained at the Tri-State College of
Acupuncture will ever practice exactly like
any of the faculty they have trained with. In
the very fertile atmosphere that we have
created here, which breeds diversity and
creativity, every faculty member, and each
graduate, will eventually shape a practice that
integrates in aspects from many sources,
some from one main style, others from other
styles, mixed with their own very special
personal qualities, to exhibit an integrative
approach that can pull from multiple sources
to meet the challenges of the clinical realm.
In those moments, quite rare as a new
practitioner and more and more frequent as
one works on ones own self-development and
ones own humanity as a practitioner and as a
person, such instances of High Skills will
reveal the deeper and more profound layer
where the arrival of Qi and the encounter of
the patients and the practitioners Shen
converge, beyond logic, beyond theory,
instances perhaps of what the Dao De Jing
refers to as wuwei where much happens
with apparently little action taking place, as if
by itself.
As practitioners gain more and more
experience using these ordinary skills of
acupuncture, and as they mature as clinicians
and just with the passage of time and the
wisdom greater experience affords, every
practitioner will have experiences they cannot
explain merely based on these ordinary skills.
It is with that proviso that I will share aspects
of a case, from the Four Exams through the
patients final reflections on our work
together, that proved quite complex, with a
series of parallel conditions stemming from
very different causes, some more physical,
some more psychological, and some clearly
spiritual, which were able to be treated, if
one looks just at the acupuncture point
strategies, in fairly similar ways.
In such moments that will renew their sense
of awe at what can transpire just with the
twirling of a few needles, they will recognize
that they knew the moment they said
The meaning of this apparent paradox, and
the way in which any experienced
acupuncture practitioner can navigate the
channels and treat complex conditions
through what appear to be very similar
moves , through the performance of
apparently ordinary skills of acupuncture,
making acupuncture nevertheless endlessly
adaptable, is borne out in the real-world of
human relatedness with our patients. This
adaptability is at the crux of what makes
acupuncture a practice situated in the tacit
dimension where one must always strive to
know much more than one can say, to engage
as Neo-Confucian Master Wang Yang-ming
would stress by drilling into the depth of a
practice and all its moves, to interiorize it,
to embody it and to trust in that tacit
dimension where we meet our patients in the
raw.
Edith entered my office originally skeptical
about acupuncture.
She suffered from a litany of complaints
centering around her right lower quadrant
muscle spasms and discomfort, as diagnosed
by her physical therapist.
I was already engaged in the process of the
Four Exams, attending to her manifestations,
like flags flapping, some quietly, some more
vigorously in the wind, as I observed her
movements, watched her facial expressions as
she shared something of her experience of
illness. As she dove into a litany of
complaints with a certain frenzy and
frustration, I sank, as I always do when the
signs and symptoms come too fast and
furious, into a mindful space from which I
could attend to what she was sharing without
trying to figure out the logic of it all.
In such moments, any well trained
practitioner knows that at any time, and with
any needling technique, one might be about
to be confronted by a fierce power, the power
of the patients holding pattern, her pain, her
suffering, her distress and the intense
experience of all that, at a level of intensity
that may prove quite overpowering.
In this mindful approach to the Four Exams,
aimed at attending to the signs and
symptoms as a composite whole, as a gift
from the patient who is sharing her
experience in her own way with me, there is
no place for me for the clinical, professional
approach one sees in TCM, where each sign
and symptom has predetermined clinical
meaning leading to a logical diagnosis.
The ability to reflect back on such
extraordinary moments in acupuncture
practice, coupled with time and experience,
will allow any acupuncturist well trained in
the Ordinary Skills of Acupuncture to
attain those High Skills that are called for
in such challenging moments. And when that
starts to happen, one has become a Reflective
Acupuncture Practitioner, who never would
have arrived at that point without first
attaining the ordinary skills that serve as a
prelude to those higher ones. To strive too
early for the high skills, without going
through the discipline of ordinary practice,
will lead to a practice where the practitioner
is quite impressed with his own skills, even as
the patient and her experience of illness is
being ignored.
Rather, I pay attention to what I hear, see,
sense with my entire body and mind, and all
my senses, waiting for a sense that I am
starting to get it, to know where I want to
begin the Palpation Exam to search for the
thorns, stains, knots and obstructions that
are at the root of all chronic disorders as the
Ling Shu tells us at the end of Chapter I.
There are some who turn some aspects of the
Four Exams, meant to gather data in the
form of relevant clinical manifestations, into
diagnosisleading to fundamental
misnomers such as pulse diagnosis or
tongue diagnosis or facial diagnosis. It is
Introduction to Chaos: a litany of
complaintsThe Four Exams as Authentic
Human Relatedness
my considered opinion that privileging any of
these data gathering/fact finding activities
over others reifies them, and leads to a
practice that is Practitioner-, not PatientCentered.
the established medical profession which,
in this instance, was unable to find a
solution to [her] presenting problem: a severe
abdominal spasm, lower back pain, and
assorted upper and lower gastrointestinal
complaints. After months of testing, Edith
ended up in the care of a physical therapist
who began work on the muscular aspect of
her problem, and who referred her to me for
acupuncture, knowing that I, too, worked on
releasing such muscular holding patterns.
It may be that pulse and tongue assessment
are closer to a diagnostic activity than the
other aspects of the Four Exams, especially
for a practitioner of Chinese Medicine (read,
internal, herbal medicine). I can only speak
to the tacit approach to intake, assessment
and treatment planning in acupuncture as I
have come to experience, and hence know it.
As Edith shared her story with me, I could
not help but notice her agitation stemming
from a fundamental skepticism about the
treatment she was contemplating with me. I
set about immediately reframing her
complaints into acupuncture and myofascial
images of constraintholding patternsthat
would ready her for the palpation phase of
my initial examination. I remarked
frequently that while her symptoms may have
proved baffling to her physicians, she was
describing acupuncture patterns that were
classic and, hopefully therefore, treatable.
It is this tacit experience that I wish to share
in following Edith and her transformations
in our work together.
The Four ExamsTaking It All In
At 53, and now in the throes of menopause,
this successful medical writer appeared weary,
lacking in vitality, with a collapsed posture
that mirrored her description of her
experience of illness. Though she had no
difficulty making eye contact, her glance was
wary and she admitted feeling cynical about
the possibility of a therapy like acupuncture
being able to make sense of and alleviate
complaints that had eluded orthopedists,
internists, gastroenterologists, a physiatrist,
an ENT, an allergist, and a physical
therapist.
In addition to her severe muscle spasm which
the physical therapist had located in the right
lower external oblique, she also suffered from
lower back pain stemming apparently from
an old herniated disc at L5-S1, irritable
bowel, gastritis and reflux, a painful coccyx
and a cool sensation in her throat, with
secondary menopausal symptoms clouding
the picture. Her appetite, which used to be
fine, was reduced to eating to get by. She
denied being thirsty and preferred hot
drinks, and consumed 6 glasses of water a
day, drinking alcohol only on weekends with
meals. She preferred salty foods and disliked
bitter as well as spicy food.
As she described being subjected to X-rays,
MRIs, a sonogram, an endoscopy, a
colonoscopy, and allergy tests over the
course of four months, her voice grew almost
desperate, yet resigned, with a quickening
pace in her verbal description that was
accompanied by shallow, constricted
breathing and a visible tightness in her throat
muscles.
Her gastrointestinal symptoms included
belching, mouth ulcers, bloating, acid
regurgitation and indigestion and the
primary severe abdominal pain, with a feeling
of food stuck in the throat after
swallowing. Her bowel movements were
painful, and she suffered from irregular
Ediths experience of her primary complaint
was underscored by the fact that, having
studied a wide array of biomedical clinical
sciences and psychology, she had full faith in
bowel movements oscillating between
constipation with hard stools and loose stools
or diarrhea with undigested food present.
She resorted to laxatives when constipated.
the past she had bouts of what her internist
diagnosed as benign arrhythmia, with
occasional irregular heartbeat and cold hands
and feet. She had dry skin and scalp
psoriasis.
Her urogenital symptoms included frequent
urination and recurrent yeast and bladder
infections, with terrible sexual energy. She
suffered occasional discomfort during sexual
relations, mainly due to vaginal dryness and
irregular and uncomfortable menstrual
symptoms associated with menopause, which
included hot flashes and night sweats. She
reported four pregnancies, and two
deliveries, but made little mention of her
children.
Her mother, still living, had high blood
pressure, osteoporosis and thyroid problems,
and her father died at the age of 45 from
coronary disease. She had no siblings, and
one of her grandparents had diabetes.
Her medical tests revealed an old L5-S1
herniated disc, which did not explain her
abdominal spasms according to her
physicians, and reflux and gastritis. Ediths
medications included Acifed and carafate for
the gastric distress, valium for what was
clearly now being seen by her physicians as a
nervous condition, the liboderm patch for
her menopausal/ hormonal symptoms and
motrin occasionally for her menstrual and
other discomforts.
Her energy, which used to be great, was
terrible now. Her energy was best in the
morning and peaked in the late afternoon.
While she reported growing easily fatigued,
she walked every day for exercise and kept to
her regimen of back exercises as well.
Emotionally, she felt lousy right now -- very
anxious, nervous, and was experiencing
occasional depression, anxiety, nervousness,
and fear attacks. Her abdominal discomfort
and the associated distress played a large role
in these mood changes, as did her
menopausal hormonal shifts.
Her pelvic and abdominal sonograms were
normal and a later CT scan was also normal.
Feeling for Holding Patterns
I gather my symptoms in an exhaustive intake
form that the patient fills out, which I scan
for likely locations of holding patterns,
patterns of somato-visceral or viscero-somatic
constrictions, which might also entail what
Wilhelm Reich referred to as character
armor. After a brief face-to-face interview to
go over the intake form and to begin to
solidify the patient-practitioner relationship, I
ask the patient to get ready and lie on the
table while I go out to complete my
acupuncture imaging, looking carefully at
the form and the patients own drawing
where they shade in the areas where they feel
pain or discomfort, to visualize from an
acupuncture meridian and three heater
perspective, the most likely location of the
patients holding patterns (jingluo
obstructions).
She reported enjoying her work, but found it
very stressful. She suffered from disturbed
sleep, and found it difficult to stay asleep due
to shifting her position in bed owing to the
abdominal pain and her husbands snoring.
This, coupled with the report of occasional
painful sexual relations, were the only
references to her husband.
Both her lower back pain, which she
reported as dull, and abdominal discomfort
and spasms, which she reported as severe,
were relieved somewhat by heat and were
worse at the end of the day.
She denied a history of smoking and
reported normal to low blood pressure. In
came to see as moveable, living areas that had
to be palpated for tight, tender or gel-like
constrictions (kori, equivalent to adhesions,
trigger points and fibrotic tissue, depending
on severity and chronicity). This Japanese
attention to palpatory findings has
characterized the teachings of the college ever
since, and corrected for an overly intellectual
French meridian perspective, which was
academically compelling but too often
lacking in such palpatory sophistication.
In this case palpation was facilitated by the
fact that her physical therapist, whose work I
knew well and who did in depth myofascial
examinations of her patients, had lead Edith
to identify muscular constrictions and dull
discomfort in her lumbar muscles bilaterally,
and in her coccyx area. Her right lower
external oblique was the site of her severe
abdominal pain, and my palpation confirmed
bilateral quadratus lumborum trigger points,
which did not reproduce the patients
primary complaint when steady pressure was
applied but rather dull discomfort locally.
Palpation of her right lower external oblique
and latissimus dorsi muscle trigger points,
near GB 26, 27 and 28, and Spl 21
respectively, were exquisitely tender and did
recreate her pain which I explained to her
was a very optimistic sign that acupuncture
release might well improve her symptoms. I
showed her pictures of Travells referral
patterns for the lower external oblique and
latissimus dorsi muscles, and explained how
the acupuncture meridians of dai mai and
the great luo of the spleen had pain referral
pathways that were identical.
Given that Edith was a medical writer, I
referenced Travells last chapter in the old
volume I, on abdominal and thoracic trigger
point referral patterns. I also gave her a 5
minute mini-course during the intake, which
she followed easily, on viscero-somatic and
somato-visceral interactions, according to
Travel. I explained that her condition, which
originally appeared viscero-somatic, where
visceral dysfunction or disease creates somatic
surface, myofascial discomfort (ruled out by
the pelvic and abdominal sonograms and CT
scan), might well be a case of somato-visceral
distress where myofascial constrictions
created her visceral discomfort and
functional disturbance(what would even two
decades ago have been labeled
psychosomatic) . In that scenario, I explained
to her, continuing my acupuncture reframing
while palpating her oblique and lat muscles
face up, it is possible the muscle
constrictions, stemming perhaps over a long
period of time from her posture while
hunched over the desk writing, combined
with her old back history, may have
conspired to create this severe muscle spasm
and discomfort. She agreed that her posture,
which her physical therapist was working on
with her, might be a contributing factor, but
cited considerable stress as well. I suggested
that her menopausal symptoms certainly did
not help the situation, and mused, being the
same age as Edith, that middle age angst was
no thrill either. I joked that I could make my
retirement fortune writing an amusing book
on how middle age should come with a users
manual, which was the first time she laughed
Further meridian and mu/shu palpation
also revealed extreme tenderness at GB 41
bilaterally, right Spleen 4 and 6, and the
Stomach meridian from Stomach 36-39,
worse on the right, as well as deep tenderness
at Kidney 16 area bilaterally, right worse,
Stomach 24 and 25 on the right, conception
vessel 10 (tight) and 12 (empty with no tone),
Stomach 25-26 left, and the right mu points
for the Liver and Gallbladder, namely Liver
14 and Gallbladder 24. This palpation was
guided by the pathways of dai mai and
chongmai, the Stomach leg yangming
meridian and what I term mu-point boogey
influenced long ago by grand rounds at the
Tri-State College of Acupuncture with Kiiko
Matsumoto. Her free-form abdominal Hara
palpation and palpation to check distal
points and local releases revolutionalized my
own understanding of mu and shu points,
and acupuncture points in general, which I
in this initial encounter, even though I used
humor repeatedly to try to bring some levity
to the rather strong palpation for trigger
points, to prepare her for possible discomfort
during the acupuncture stimulation of these
local areas of irritation and distress (which I
refer to when teaching my students as
assessment of a patients deqi tolerance
level, which is to say their tolerance to
feeling the needling sensations of
acupuncture).
therapeutic and begins to initiate therapeutic
changes.
Clinical Manifestations and their AOM
differentiation
Primary & secondary complaint: the
patient was very specific in listing her
complaints as follows: oblique
abdominal muscle spasm; lower back
pain; irritable bowel; painful
coccyx; occasional cool sensation in
throat; menopausal symptoms, which
started suddenly in November, 2001,
four months before consulting me.
Medical diagnoses of these
complaints by patients physicians
and other healthcare providers:
gastritis, reflux, menopause,
herniated L5-S1 disc, muscle spasm.
Treatments to date for these
complaints including medications:
axid and carafate for the digestive
symptoms, valium for the overall
anxiety and discomfort/distress,
liboderm patch for menopausal
symptoms, occasional motrin for
pain, physical therapy to loosen
spasms and strengthen back.
Relevant family medical history: her
mother suffered from hypertension,
osteoporosis and thyroid problems;
her father died at age 45 of coronary
disease; her grandparents suffered
from diabetes.
Past personal medical history: no
injuries, accidents or surgeries were
reported, but stress was underscored
as a constant factor, growing more of
late.
Diet: eats to get by: bran and decaf
coffee for breakfast; yogurt or
sandwich for lunch; pasta, salad and
A Response of Guarded Optimism
By the end of the palpation phase of the
examination, Edith expressed a willingness to
give three treatments a shot, as she
quipped, which was what I suggested to her,
one that same day and two more spaced at
weekly intervals.
It is important to note that the treatment had
already begun as the intake transformed into
education and the palpation served to locate
her holding pattern and validate her
experience of illness and begin the release of
these tight areas.
In the concept of tongshenming which Ted
Kaptchuk translates as penetrating divine
illumination in his introduction to
Acupuncture in Practice with Hugh
MacPherson, it is thought that practitioners
sometimes manage to set the healing process
in motion during the initial encounter, even
before initiating the acupuncture, massage or
herbal treatments themselves. Some
practitioners and texts refer to this as the
patients and doctors shen connecting, to
catalyze a healing response. Others, like Ted
Kaptchuk, might refer to this as prodding the
patients placebo capacity.
If this relationship is forged during the
palpation phase, it becomes impossible to
distinguish palpatory examination from
palpatory treatment, as palpation becomes
juice for dinner; chicken 2-3 times
per week, dairy 4 days a week; 6
glasses of water a day and 2 cups
decaf coffee or tea; wine with dinner
on the weekends only.
night in the lower back and right
abdomen and ribcage.
AOM differentiation: cold bi right
tendindomuscular meridian of Gallbladder and
great luo of the Spleen deficiency.
Gastrointestinal S&S: belching,
bloating, acid regurgitation,
indigestion, food stuck in throat
after eating, painful bowel
movements, alternating hard and
loose stools, undigested food in the
stools, occasional laxative use.
Cardiovascular S&S: normal to low
blood pressure, benign arrythmias in
the past, palpitations, occasional
irregular heart beat.
AOM differentiation: deficient heart Qi.
AOM differentiation of above clinical
manifestations: middle heater dysfunction/
constrained Liver qi/ Spleen Qi
deficiency/diaphragmatic constriction.
Skin and hair S&S: dry skin and
scalp psoriasis.
AOM differentiation: deficient Yin.
Urogenital and reproductive S&S:
frequent urination, urinary tract
infections, terrible sexual energy,
hot flashes, night sweats, vaginal
dryness.
APM Etiology & Pathology:
The Bodymind Continuum
AOM differentiation: lower heater dysfunction/
Kidney-Bladder imbalance/pelvic collapse.
While this patient worked as an editor of
psychology textbooks and journals, she
seemed to react to these new symptoms with
physical symptoms of anxiety, palpitations
and viscerally, in the digestive track
especially. She did not attribute any of these
symptoms to specific psychological factors,
more generally referring to her experience of
illness as signs of stress. In fact, she had
reached menopause, was finding sexual
relations painful and her sexual energy
terrible, which many of my female patients
would have situated more centrally in the
overall picture as the distress that comes with
aging, an end to reproductive capacity and
the empty nest syndrome, and pending
retirement. She therefore seemed to situate
herself more on the body side of what I term
the bodymind continuum, and sought
physical solutions for these complaints.
Energy and exercise levels: terrible
energy which used to be great,
easily fatigued but manages to walk
and do back exercises every day.
AOM differentiation: deficient Kidney Qi.
Emotions and sleep: emotionally
lousy right now-very anxious,
nervous, with fear attacks and
disturbed sleep, waking 3-4 AM from
shifting positions due to husband
snoring.
AOM differentiation: constrained Liver Qi,
diaphragmatic constriction.
Musculoskeletal S&S: dull, aching
pain, better with heat and worse at
Acupuncture Imaging:
reactions that could exact a serious toll on
the body if left unaddressed. Such a disorder
as this had come to be seen as minor,
something a physical therapist might address,
thus ignoring the deep experience of distress
this patient was experiencing, and the
obvious fear that some serious, and perhaps
life threatening disorder, was going
undetected. After all, her father had died of a
coronary at the age of 45.
From a meridian perspective, this patients
primary holding pattern occupied the
pathway of the belt channel, dai mai, which
encircles the waist and travels along the lines
of the external oblique musculature, on the
right in this case. The great luo pathway of
the Spleen was also implicated as this spreads
throughout the lateral ribcage. From a zangfu
perspective of the three heaters, I would call
this a case of pelvic collapse, where constraint
in the middle heater leads to collapse of
Spleen Qi, and congestion in the lower
heater.
In looking at the meridian aspect of a
disorder I incorporate Travells referred
pathways of myofascial trigger points, as a
much more detailed way of speaking about
meridian energetics in general, and of the
tendinomuscular meridians and cutaneous
regions in particular, those aspects of the
meridian system that can be seen and
touched, in particular.
In classical acupuncture theory, yang, the
meridian system, protects yin, the organ
system. Thus attacks on the body from the
outside, whether in the form of atmospheric
assaults, repetitive strain, injury or any
stressors that initiate the stress response and
an overactive sympathetic system and
musculature prepared for fight-orflight(Selye), might lead to tendinomuscular
excess.
Trigger point referrals:
In a careful review of Travell and Simons
Myofascial Pain and Dysfunction: the Trigger
Point Manual, the picture of myototic unit of
interactive muscle trigger points emerged,
implicating the external and internal
abdominal obliques, psoas, erector spinae,
multifidi, rotatores, serratus posterior
inferior, all of which assist the quadratus
lumborum in extension and may be activated
by a side-bent, cross-legged posture like the
one she described when she told me how she
sat at work.
In the absence of signs of external pathogenic
invasions in cases like this patients, and with
comprehensive medical workups that were all
negative, I started by seeing this perhaps as a
case of a complex, somatovisceral holding
pattern: myofascial/somatic constrictions
encompassing visceral symptoms with the
associated distress. Early on, given my
training in Van Nghis French meridian
perspective, I learned to appreciate that such
disorders might be located within the
superficial meridian systems, but might lead
to deep-seated emotional distress as the
resulting visceral (zangfu) symptomatology
continued to elude medical diagnosis. Such
patients who returned frequently to their
physicians were more often than not seen as
hypochondriacs in the age of psychosomatic
medicine, and the modern version of this
perspective would ignorantly assign the
blame to stress without realizing that stress
involves a very real physiological set of
Travell underscores the fact that poor elbow
support at the desk can be a further
contributory factor.
Palpation of the psoas and paraspinal
musculature yielded no tight or reactive
trigger points, which one might have
suspected had her lumbar disc problem been
involved in this abdominal pain.
The serratus posterior inferior was reactive,
and trigger points here can cause nagging,
annoying achiness in the lower thoracic
region. The external obliques, lower near
Gallbladder 26-28 and upper near Liver 14 to
Gallbladder 24, including the serratus
anterior near Spleen 21, were all exquisitely
tender and tight. This corroborated the
meridian assessment of dai mai and the luo
of the Spleen.
distended abdomen with excessive flatus.
Contraction of the abdominal muscles is
inhibited by the TrPs so that the patient
cannot pull the stomach in. This apparent
distension is readily distinguished from that
due to ascites on physical examination(ibid,
p. 952). They conclude that right upper
quadrant pain caused by contracted upper
external oblique trigger points might easily
lead to pain and discomfort that might be
confused with gallbladder disease.
Travell and Simons explanation for visceral
symptomatology from these abdominal and
back trigger points is worth noting in its
entirety: Active TrPs in the upper portion of
the abdominal external oblique muscle,
which overlies the ribcage anteriorly, are
likely to produce heartburn and other
symptoms commonly associated with hiatal
hernia. These costal and subcostal TrPs in
abdominal muscles also may produce deep
epigatric pain that occasionally extends to
other parts of the abdomen (MPD, vol. I, p.
941).
Travell and Simons site a series of common
stress factors that might activate such
abdominal trigger points:
body fatigue
over exercise of the abdominal
muscles
emotional tension
straining during defecation due to
constipation
poor posture leaning forward for
hours, thus tensing and shortening
abdominal muscles with failure to
properly support the back
The picture grew more complicated as I
learned from her in a followup treatment
that she had been diagnosed with a small
hiatal hernia at one point by a specialist, a
clear Spleen Zang deficiency sign that would
allow for Liver Zang invading Spleen
dysfunction which she did exhibit, and
Spleen Qi Sinking dysfunction as well.
The authors underscore the fact that it
has been recognized since the 1920s
that persistent abdominal pain is as
likely to originate in abdominal-wall
muscles or be referred from chest-wall
muscles as it is to originate in
abdominal viscera(ibid, p. 956).
Travell and Simons stress how confusing and
enigmatic such abdominal symptoms often
prove. Understanding the reciprocal
somatovisceral and viscerosomatic effects of
TrPs helps to unravel some of this
uncertainty. Myofascial TrPs in an abdominal
muscle may produce referred abdominal pain
and visceral disorders (somatovisceral effects)
that, together, closely mimic visceral disease.
Conversely, visceral disease can profoundly
influence somatic sensory perception and can
activate TrPs in somatic structures that may
perpetuate pain and other symptoms long
after the patient has recovered from the
initiating visceral disease(ibid, p. 951) They
go on to share their experience of active
abdominal trigger points, especially in the
rectus abdominus, which may cause a lax,
Differential diagnosis of visceral diseases
that can cause the same symptoms of
discomfort and distress as abdominal
muscle trigger points include:
10
articular dysfunctions
fibromyalgia
appendicitis
peptic ulcer
gallstone colic
colitis
painful rib syndrome
intractable dysmenorrhea
urinary tract disease
hiatal hernia
reflux esophagitis
gastric carcinoma
chronic cholecystitis or uretral
colic
inguinal hernia
hepatitis
pancreatitis
ovarian cysts
diverticulosis
umbilical hernia
thoracic radiculopathy
costrochondritis
ascariasis parasites
ascites
Reactions over the past 5 months: she
received a diagnosis of genetic osteopenia,
which was ruled out as a cause of her primary
complaint that brought her for acupuncture,
but clearly agitated her (growing older,
developing genetic disease) and was put on
fosamax. She presents this time with right
hip pain primarily.
Treatment 1: Did side lying for right QL,
serratus, lower external oblique and GB 29,
30, 31, 34, 38, 41(possible hip involvement
the complexity of aging) with same root
chong mai/dai mai treatment as initially.
It is therefore essential that patients with
undiagnosed abdominal pain be evaluated by
a physician to rule out visceral disease (ibid,
p. 956).
Reactions to Treatment: the new hip area
pain was definitely better.
Treatment 2: same root points but face down
taiyang zone adding bilateral QL trigger
points and bilateral Bl. 23 for Kidney Qi, and
right GB 30 which was now symptomatic.
The authors add that abdominal breathing, a
common stress reduction technique, is
extremely valuable for somatovisceral
abdominal pain.
Reactions to Treatment: the patient reported
feeling definitely better.
____________________________________
Treatment 3-4: same taiyang zone treatment
for QL and right hip.
Round One of Treatment (6 over 2 months,
starting with once weekly for three weeks):
Round Three of Treatments (patient returns
for 4 treatments over 6 weeks):
Acupuncture Diagnosis: constrained chong
mai and dai mai; diaphragmatic
constriction(APM); Middle heater
dysfunction.
Treatment: Sp 4/ Per 6; GB 41/TH 5; LI4/
Liv3; Sp 6, St 36, 37, 39; Kid 2 and 3; GB
26-28, GB 24, Liv 14
Reaction over past one year: The hips have
been fine, the patient is here for a follow-up
up on right daimai area discomfort which is
mildly symptomatic. When I mentioned that
it seemed she had really become very clear
about when she felt a return for more
acupuncture made sense, she responded:
Ive learned that when it starts to bother me,
a series of 3 or so treatments takes care of it.
I told her perhaps one or at most two
treatments might do it this time, as I always
try to empower the patient to only come to
treatment when they feel they need it. She
answered very clearly that she felt safer
planning on all three.
Additional treatment for allergies in last
treatment: Sp 5, LU 7, LI 4, LI 20, Bl 2, St 2
Round Two of Treatments (4 treatments
over 4 months):
11
St 25 and Kid 16 on the right, where
reactive, with distal St 36, 37 and 39.
Treatment: Same distal and local
chong/daimai treatment as initially.
Last treatment: The patient reported feeling
much better but not totally gone; I want one
more treatment. I repeated the same
treatment and did not see her for quite some
time.
Reactions to Treatment: Feels better but still
concerned about return of right sided GB 25
area discomfort.
Treatment: do side lying adding tender TrPs
at iliac crest and GB 25 area and same distal
chong/dai mai treatment.
Round 4 of Treatment:
Reactions to Treatment: Great for Two
Days! I sense it is almost gone!
Reactions to Round Three of Treatment:
Much better overall, the patient came 6
months later for a follow-up preventative
series of 2-3 treatment on the right daimai
area discomfort, which was barely noticeable,
plus new flexor carpi ulnaris bilateral
discomfort, from much more computer work
.
Last Treatment: do side lying as above, and
then face down for QL bilateral and rt hip
GB 30 area (piriformis TrP) with huge
releases of all trigger points Then do face up
for chongmai/daimai as before.
Treatments 1-2: GB 41, 27, left, Liver 3,
bilateral flexor carpi ulnaris TrPs near SI 7
and distal to Ht 3, bilateral Kid 3 and Ht. 7
(SI muscle channel).
Reactions to treatments 1-2: the new arm
symptoms are totally gone, but she wants 3rd
treatment as preventative for right daimai
area. The same daimai treatment was
administered.
Reactions to Round 4: Right quadrant
abdominal discomfort 95% better; bilateral
flexor carpi ulnaris TrPs much better.
A Final Round:
Reactions to last series of treatments: The
patient reported being fine for one and a half
years, since her last treatment of Round 4.
She is here today for mild rt LQ discomfort
and some GI distress with abdominal
discomfort.
RAP-UP: Issues raised by this case from
the patients and the practitioners
perspectives:
Treatment: treat dai and chong mai, distally
and locally as before, and release local Sp 15,
12
and validated her experience of right lower
and upper quadrant pain and the associated
distress.
In the palpation phase of the examination- astreatment, which is pivotal in the
Acupuncture Physical Medicine approach I
have developed over the past two decades, I
of course try to make the patient
comfortable, and give them as accurate a
feeling of what the acupuncture treatment is
going to entail as possible to allay any fears.
As I proceeded in this fashion with Edith, I
did so keenly aware of her strong skepticism
toward acupuncture for her condition.
More like an osteopath than a
psychotherapist, I found the strain in her
body fabric, in the belt channel that choked
her, and strained it further through informed
touch and needling, to prod it to release, a
few notches at a time, so that she might
breathe more easily and feel more at ease in
herself. I also avoided an overly psychological
approach to my communication with her
because of her career editing psychological
materials, and the fact that she was skeptical
of acupuncture from the start, and would
have undoubtedly reacted with concern if I
took on a psychotherapeutic air.
But I also try immediately to validate the
persons experience of illness by always by
laying my hands on the areas of discomfort
and distress that the patient identified on the
charts diagrams of the body, and during the
Four Exams, and try to match my verbal
communication with my somatic
communication, drawing on acupuncture or
trigger-point images and three heater
findings while I am palpating, to embody this
phase in such a way that the patient has a
more pronounced bodily-felt sense, to quote
Gendlin yet again, of their complaint. This
phase of the palpation marked a shift in
Ediths attitude toward me in particular and
toward acupuncture in general, as she
displayed guarded surprise that I found the
location of her complaint so readily.
The Human Dimension entailed in my work
with Edith revolved around slipping in
suggestions of how the emotional strains of
menopause and the subsequent bodily
changes, her children leaving home and the
aging process in general could lead to the
constrictions she was experiencing. These
comments and reframes were performed
during the actual palpation for her holding
pattern and their acupuncture release, thus
grounding the comments in the physical
realm of the palpation and needling. A
different patient responding to all these
changes from the mind side of the bodymind
continuum would have most certainly
required more talk time, and a different way
of reframing the holding pattern.
I capitulated to this patients clearly more
physical explanations for her problems, and
therefore did not probe into her marriage,
her children, her likes and dislikes, her work,
listening instead, and watching and sensing
how she responded to this discussion of her
emotional life. While I did make some
passing remarks about the aging process and
what the experience of menopause might
entail, slipping in as it were signs of empathy
and compassion for her experience into our
discussions together, I made most of my
communication center around what I located
in her body, and around her bodily feltsense of these somatic constrictions. I
focused on the holding pattern that matched
Progress to Date
At the time of this writing, a year had passed
since the last treatment. In her reflective
assessment of her own initial intake form,
Edith reported complete absence of the
abdominal discomfort and lower back pain,
which she rated as a 0 on her own VAS scale
(0-10), that brought her for treatment. She
also reported complete relief from the
13
original painful coccyx , feeling of food stuck
in the throat and cool throat sensation, all
rated 0 on the VAS scale. Her written report
of the other changes she experienced during
and since acupuncture treatment display a
wry sense of humor that was almost totally
absent in the initial encounter, obscured as it
was by her discomfort and distress. It is
hard to believe, she writes now, that I
reported a poor appetite in 2002. I certainly
eat more than to get by, and have resumed
nibbling (when the warmer weather arrives,
it will be time to get back to outdoor exercise
to shed several pounds gained over the
winter!). She also reports greatly improved
sleep, which she rated an 8 on her VAS scale
four years ago and now puts at a 3, with
greatly improved energy as well. She admits
to still being a type A person, and still gets
stressed over work and some family matters.
But she is very reflective of the need to begin
tapering down her work load, and is slowly
utilizing the help of an assistant to step into
her shoes during her absences or eventual
retirement or resignation from her current
position.
Edith was not an easy acupuncture patient.
With a background in anatomy, neurology,
biology, and psychology, and a better than
average understanding of how the mind and
body work in health and illness, she
displayed more than a healthy skepticism
toward acupuncture from the start. She
would have never considered acupuncture
treatment on her own, and it took a direct
referral from her physical therapist, whom
she respected tremendously, and who had
excellent results for a cat allergy in her
treatments with me, to bring her to my door.
Originally skeptical about acupuncture, she
soon became a convert.
My goal is to serve as a change-agent for my
patients, helping to release problematic
holding patterns, thereby prodding them to
become their own healers. The renewed
vitality liberated by acupuncture release of
such blockages leads to emotional, spiritual
as well as physical relief, as this case reveals. I
believe that any seasoned acupuncturist from
any style or tradition of practice sees this sort
of change in their patients body, mind and
spirit, and it is this sort of change that
provides the impetus for our continued work
in this direction.
The only prescription medication Edith takes
now is Fosamax for osteopenia, as well as
over the counter calcium and fiber. All in
all, she states now, I consider myself to be a
healthy specimen, in glaring contrast to her
self-portrayal as a sufferer of a staggering
litany of complaints four years ago which
now loom as a distant, albeit painful,
memory, and I owe it to the acupuncture
treatment I received.
Edith reports being thrilled to be included
as a case study for the faculty development
course that lead to this study.
Ediths experience of acupuncture, which
reframed her elusive, albeit severe,
complaints, into acupuncture images that
lead to positive change overall, is precisely
what I hope for and of course do not always
witness. Her final words about this
experience made my day when I first read
them, and such experiences of change
through acupuncture continue to inspire and
fascinate me after thirty two years of practice
and teaching.
Her menopausal symptoms have also
lessened tremendously, with the passage of
time, and she never felt the need to address
those with acupuncture, rating them now a
bearable 3 on the VAS scale.
Epilogue
I have only superlatives when describing my
acupuncture experience, Edith now reports.
14
I had to take a leap of sorts to go for
acupuncture treatment, and now theres no
going back.
What I have learned with patients like Edith,
and from the readings and reflections of the
past 6 months, is that the Ordinary Skills are
all those that allow us to take in what we are
hearing, seeing, feeling, sensing, initiate an
intervention with needles in the case of
acupuncture, and attend to the changes that
these interventions bring about, while
attuning (tiao) our interventions to these
changes.
In a bright, aware, spirited person like Edith,
who did reflect hard on her plight, it takes
small prods Ordinary Skills, to set her own
spirit and Heart-Mind in motion to restore
normalcy.
In other cases, a practitioner might need far
more adept skills of reframing, education,
and support to help a patient gain greater
spirit clarity (shenming). This takes us into the
realm of High Skills, where a Neo-Confucian
doctor, for example, would take it for granted
that he must work at self-cultivation and
attend to his own spirit clarity and HeartMind if he is ever to be able to prod spirit
clarity (tongshenming) in his patients; this will
be the focus of coming Reflections.
Sources:
Seem, Mark. Bodymind Energetics: Toward a
Dynamic Model of Health, Thorsons Press,
Rochester VT, 1990
Seem, Mark. ACUPUNCTURE Physical
Medicine, Blue Poppy Press, Boulder, CO, 2000,
especially pp. 91-92 and 112 114.
Travell, Janet and Simons, David. Myofascial
Pain and Dysfunction: the Trigger Point
Manual, Volumes I and II (per muscle trigger
points cited in this case study)
15
Anda mungkin juga menyukai
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Breast Cancer Concept MapDokumen2 halamanBreast Cancer Concept MapMaria Cristina100% (1)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Standards TattooingDokumen12 halamanStandards Tattooingcaleyramsay100% (1)
- Nutritional Reference GuideDokumen362 halamanNutritional Reference Guidebecap9100% (9)
- Useful Vocabs For OET Writing & Speaking PDFDokumen2 halamanUseful Vocabs For OET Writing & Speaking PDFLiju K Oommen100% (3)
- Recommended Books For MRCOG Part 2 ExaminationsDokumen9 halamanRecommended Books For MRCOG Part 2 Examinationssaqii67% (6)
- Nursing Care of Children with Reproductive DisordersDokumen11 halamanNursing Care of Children with Reproductive DisordersMavis Avelino100% (1)
- Kiiko Matsumoto Style Allergies TreatmentDokumen3 halamanKiiko Matsumoto Style Allergies TreatmentIndra SyafriBelum ada peringkat
- Other Acupuncture Reflection 1Dokumen11 halamanOther Acupuncture Reflection 1Indra SyafriBelum ada peringkat
- Hazard Prevention Through Effective Safety and Health Training - Table - ContentsDokumen1 halamanHazard Prevention Through Effective Safety and Health Training - Table - ContentsAmeenudeen0% (1)
- 43 Extra Acupuncture PointsDokumen3 halaman43 Extra Acupuncture PointsIndra Syafri100% (3)
- Mission Indradhanush: Submitted By-Jayesh Agrawal Mba-Rural Development Semester-IstDokumen20 halamanMission Indradhanush: Submitted By-Jayesh Agrawal Mba-Rural Development Semester-IstJayeshAgrawalBelum ada peringkat
- Mtap - Virology NotesDokumen7 halamanMtap - Virology NotesMoira Pauline LibroraniaBelum ada peringkat
- 16-Protein and Aloe Vera Hair Fluid For Damaged HairDokumen1 halaman16-Protein and Aloe Vera Hair Fluid For Damaged HairIndra SyafriBelum ada peringkat
- 17-Detangling Hair Conditioner Lotion For Long HairDokumen1 halaman17-Detangling Hair Conditioner Lotion For Long HairIndra SyafriBelum ada peringkat
- 13-Leave-In Conditioning Mousse With UV ProtectionDokumen1 halaman13-Leave-In Conditioning Mousse With UV ProtectionIndra SyafriBelum ada peringkat
- 20-Sheabutter UV Hair PolishDokumen1 halaman20-Sheabutter UV Hair PolishIndra SyafriBelum ada peringkat
- 11 Cream BlushDokumen1 halaman11 Cream BlushIndra SyafriBelum ada peringkat
- Hypertension 2006 Macklin 838 45 PDFDokumen9 halamanHypertension 2006 Macklin 838 45 PDFIndra SyafriBelum ada peringkat
- 05-Skin Tightening TreatmentDokumen1 halaman05-Skin Tightening TreatmentIndra SyafriBelum ada peringkat
- 10-Gel-Blush With Mica PigmentsDokumen1 halaman10-Gel-Blush With Mica PigmentsIndra SyafriBelum ada peringkat
- Acupuncture and Herbs - 3Dokumen10 halamanAcupuncture and Herbs - 3Indra SyafriBelum ada peringkat
- 12-Body Butter With Shea Butter and Cacao ButterDokumen1 halaman12-Body Butter With Shea Butter and Cacao ButterIndra SyafriBelum ada peringkat
- 02-Face Body Cream With Vitamin E PDFDokumen1 halaman02-Face Body Cream With Vitamin E PDFIndra SyafriBelum ada peringkat
- 04-Mild Conditioning ShampooDokumen1 halaman04-Mild Conditioning ShampooIndra SyafriBelum ada peringkat
- Acupuncture and Herbs - 2Dokumen12 halamanAcupuncture and Herbs - 2Indra SyafriBelum ada peringkat
- MoonDragon 2Dokumen10 halamanMoonDragon 2Indra SyafriBelum ada peringkat
- MoonDragon 1Dokumen9 halamanMoonDragon 1Indra SyafriBelum ada peringkat
- Other Acupuncture Reflection 4Dokumen13 halamanOther Acupuncture Reflection 4Indra SyafriBelum ada peringkat
- Acupuncture and Herbs - 1Dokumen14 halamanAcupuncture and Herbs - 1Indra SyafriBelum ada peringkat
- Other Acupuncture Reflection 10Dokumen10 halamanOther Acupuncture Reflection 10Indra SyafriBelum ada peringkat
- Acupuncture Treatment of Dysmenorrhea (SchoolAkp)Dokumen3 halamanAcupuncture Treatment of Dysmenorrhea (SchoolAkp)Indra SyafriBelum ada peringkat
- Other Acupuncture Reflection 5Dokumen12 halamanOther Acupuncture Reflection 5Indra SyafriBelum ada peringkat
- Other Acupuncture Reflection 3Dokumen20 halamanOther Acupuncture Reflection 3Indra SyafriBelum ada peringkat
- PDF TestDokumen20 halamanPDF TestRicardo TeixeiraBelum ada peringkat
- Reflecting on Acupuncture's Cultural Shift to Integrative MedicineDokumen8 halamanReflecting on Acupuncture's Cultural Shift to Integrative MedicineIndra SyafriBelum ada peringkat
- Other Acupuncture Reflection 7Dokumen22 halamanOther Acupuncture Reflection 7Indra Syafri100% (1)
- Other Acupuncture Reflection 8Dokumen7 halamanOther Acupuncture Reflection 8Indra SyafriBelum ada peringkat
- Other Acupuncture Reflection 2Dokumen15 halamanOther Acupuncture Reflection 2Indra Syafri100% (2)
- Honey Promotes Better Healing Than Silver Sulfadiazine for BurnsDokumen8 halamanHoney Promotes Better Healing Than Silver Sulfadiazine for BurnsFEBRIA RAMADONABelum ada peringkat
- Asthease CapsuleDokumen3 halamanAsthease Capsulehk_scribdBelum ada peringkat
- Point of Care TestingDokumen24 halamanPoint of Care TestingfowziBelum ada peringkat
- Priyanshu - Sarkar - Project Report On Internship ProgramDokumen25 halamanPriyanshu - Sarkar - Project Report On Internship ProgramLog InBelum ada peringkat
- Health 6 Quarter 1 Module5Dokumen15 halamanHealth 6 Quarter 1 Module5Cindy EsperanzateBelum ada peringkat
- Handouts - Dr. Ahmed Leithey - Management of Endodontically Treated TeethDokumen8 halamanHandouts - Dr. Ahmed Leithey - Management of Endodontically Treated TeethAbdelfattah EL KadyBelum ada peringkat
- Airway Management - CHFDokumen2 halamanAirway Management - CHFRindang_Citraw_1819Belum ada peringkat
- Capstone OutlineDokumen3 halamanCapstone Outlineapi-395468231Belum ada peringkat
- The Periodic Health ExaminationDokumen30 halamanThe Periodic Health ExaminationabstabsBelum ada peringkat
- Bwdi DR, Chemist&Stp Final ListDokumen226 halamanBwdi DR, Chemist&Stp Final ListzaheerbcBelum ada peringkat
- Philippine Medical Technology: Education & Career GuideDokumen64 halamanPhilippine Medical Technology: Education & Career GuideLovely Reianne ManigbasBelum ada peringkat
- Leprosy (Morbus Hansen) : Dr. Uun Khusnul Khotimah, SPKKDokumen38 halamanLeprosy (Morbus Hansen) : Dr. Uun Khusnul Khotimah, SPKKagilBelum ada peringkat
- Effective Messages in Vaccine Promotion: A Randomized Trial: PEDIATRICS March 2014Dokumen11 halamanEffective Messages in Vaccine Promotion: A Randomized Trial: PEDIATRICS March 2014Kroof KayBelum ada peringkat
- Sanford Chris CVDokumen9 halamanSanford Chris CVChris SanfordBelum ada peringkat
- Understanding PneumoniaDokumen26 halamanUnderstanding PneumoniaNo StradamusBelum ada peringkat
- Assess Ability To Learn or Perform Desired Health-Related CareDokumen6 halamanAssess Ability To Learn or Perform Desired Health-Related CareMarielle J GarciaBelum ada peringkat
- Zhang 2019. - The Effectiveness and Safety of Acupuncture For Myasthenia GravisDokumen10 halamanZhang 2019. - The Effectiveness and Safety of Acupuncture For Myasthenia GravisVioline MartaliaBelum ada peringkat
- Ugaiet2011brochure - PDF KleDokumen59 halamanUgaiet2011brochure - PDF Klezuber2022Belum ada peringkat
- Indonesia Hires OK PDFDokumen94 halamanIndonesia Hires OK PDFikaBelum ada peringkat
- What Is Brain CancerDokumen3 halamanWhat Is Brain Canceryash vardhanBelum ada peringkat
- Argumentative Essay FinalDokumen3 halamanArgumentative Essay Finalapi-248602269Belum ada peringkat