Astm Bronsic CAN
Diunggah oleh
Alina GheDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Astm Bronsic CAN
Diunggah oleh
Alina GheHak Cipta:
Format Tersedia
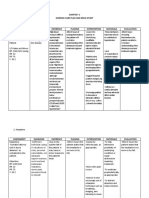
Prevention
Prevention strategies for asthma secondary prevention
econdary prevention of asthma is defined as intervention(s) for infants and children who are at high risk
for the development of asthma but who have not yet
developed asthma symptoms or signs. These patients have
a family history of allergic disease and 1 or more of the following: atopic dermatitis or eczema, allergic rhinitis, food
allergy, bronchial hyperreactivity, blood eosinophilia, elevated total IgE levels, elevated allergen-specific IgE, or
skin-test reactivity to specific allergens.13
Literature review
The evidence base for effective measures in the area of
secondary prevention of asthma is small. All of the studies
identified in a MEDLINE search are included in this review. Criteria for diagnosis of asthma are those described
by the individual investigators.
Current evidence
Evidence-based therapeutic interventions for the secondary prevention of asthma fall into 3 categories:
pharmacologic treatment422
control of environmental allergens and environmental
tobacco smoke2327
allergen-specific immunotherapy2832
DOI:10.1503/cmaj.045064
Pharmacologic treatment
H1-antihistamine medications are of limited therapeutic
benefit when administered in the usual doses to those with
established asthma.4 Nevertheless, in 3 prospective, doubleblind, placebo-controlled studies,58 the first-generation H1antihistamine ketotifen and the second-generation H1-antihistamine cetirizine, both of which have anti-allergic and
anti-inflammatory properties,4,9 were used with some success in the secondary prevention of asthma.
In a double-blind, parallel-group, placebo-controlled
study,5 121 infants and children with atopic dermatitis, who
were 136 months old at study entry, received ketotifen
twice daily for 1 year; the dose for those <14 kg was 0.8 mg
and for those 1423 kg the dose was 1.2 mg. At the end of
this time, only 13.1% of the ketotifen-treated children had
asthma in contrast with 41.6% of the placebo-treated children (p < 0.001); however, the beneficial effect of ketotifen
was observed only in children who had a raised total serum
IgE level at study entry. Adverse effects, including sedation,
were noted in the ketotifen-treated children. Children with
atopic dermatitis frequently have elevated total IgE; how-
ever, IgE does not correlate with asthma in the absence of
atopic dermatitis. Adverse effects, including sedation, were
noted in 6 of the 61 ketotifen-treated children compared
with 0 of the 60 children in the placebo group. Subsequent
trials to support this approach have not been published and
ketotifen is seldom used.
In a subsequent double-blind, placebo-controlled, parallel-group study,6 100 pre-asthmatic infants with a family
history of allergy and elevated total serum IgE levels were
treated with ketotifen at a dose of 0.5 mg every 12 h for
those 3 years of age and 1 mg every 12 h for those >3
years of age. Treatment was continued for 3 years. At the
conclusion of treatment, 9% of the 45 infants who were
given ketotifen had developed asthma and 35% of the 40
children given placebo had developed asthma (p = 0.003).
Adverse effects were not discussed in the report of the
study.
In a larger, rigorously designed, randomized, doubleblind, placebo-controlled investigation7 (the Early Treatment of the Atopic Child [ETAC] study) of 817 children
aged 1224 months at entry, cetirizine in a dose of 0.25
mg/kg or matching placebo was given twice daily for 18
months. There was a 6-month double-blind follow-up and
an additional 36-month open follow-up. At entry, no child
had a history of wheezing, nocturnal cough or pulmonary
disease of any kind. Asthma was defined as 3 episodes of
nocturnal cough with sleep disturbance or wheezing separated by at least 7 days in a clinical setting where asthma
was likely and other conditions had been excluded.
In contrast to placebo, cetirizine treatment delayed
asthma onset in children sensitized to house dust mites
(HDMs) (35 of 68 v. 16 of 56, p = 0.005) and in those sensitized to grass pollen (20 of 34 v. 10 of 36, p = 0.002), although not in the entire group enrolled in the study (intention-to-treat population; 150 of 398 v. 151 of 397).7 In the
grass pollen-sensitized children, the effect was sustained for
36 months after treatment was discontinued (p = 0.008). In
the children sensitized to HDMs, there was a gradual narrowing of the difference between cetirizine and placebo
treatments in terms of cumulative prevalence of asthma at
the end of 36 months, but no evidence of a rebound after
the treatment was stopped (p = 0.04). The effect on prevention of asthma symptoms, which was maintained after cetirizine treatment was discontinued, was attributed to downregulation of ICAM-1 expression and eosinophilic
inflammation.8,9 In the placebo-treated children, there was a
significantly higher risk of the development of asthma in
those sensitized to grass pollen, HDM, cat or egg allergen
at study entry.8
CMAJ SEPT. 13, 2005; 173 (6)
S25
Becker et al
In the ETAC study, cetirizine also had a topical glucocorticoid-sparing effect in atopic dermatitis10 and decreased
the frequency of acute urticaria episodes, which occurred in
5.8% of the cetirizine-treated children in contrast with
16.2% of the placebo-treated children.11 Unlike the preventative effect against asthma, the preventative effect against
urticaria disappeared when treatment was stopped. Despite
the relatively high cetirizine dose administered (0.25 mg/kg
twice daily), the long-term safety profile was excellent and
there were no adverse effects on growth, behaviour, psychosocial or cognitive development, as rigorously assessed
during active treatment and follow-up using validated instruments, including the McCarthy Scales of Childrens
Ability.1214
There are 2 additional relevant studies. A 24-month
study in which loratadine prevented viral upper respiratory
tract infections and associated wheezing and coughing in
children aged 2430 months has been completed but not
yet published.15 A long-term, prospective, randomized,
double-blind, placebo-controlled study of levocetirizine
(the pharmacologically active enantiomer of the racemate
cetirizine), 0.125 mg/kg twice daily, in children aged 1224
months is also underway.
Prospective, randomized, double-blind, placebocontrolled pharmacologic interventions are needed to test
other classes of medications, including inhaled glucocorticoids16 and oral leukotriene modifiers,17 which are effective
in infants and young children with an established diagnosis
of asthma, but have not been studied for their secondary
prevention effects in high-risk children who have not yet
developed asthma. Also, the topically applied calcineuron
inhibitors, such as pimecrolimus and tacrolimus, introduced recently for relief of skin inflammation in infants and
children with atopic dermatitis or eczema are of interest
with regard to their potential role in the secondary prevention of asthma.18 The possibility that allergen exposure
might decrease responsiveness to pharmacologic treatment
needs to be explored further. 19 In addition, new immunomodulators, which appear to be safe and effective in
clinical trials in humans, should eventually be studied for
the secondary prevention of asthma in at-risk individuals.
Examples of these interventions include anti-IgE with20 or
without21 specific allergen immunotherapy, cytokine antagonists21 and DNA vaccines, including immunostimulatory
sequences with23 or without specific allergen.
Overall, studies of secondary prevention have been disappointing, but in children already sensitized to HDM or
grass pollen allergens who do have atopic dermatitis, treatment with cetrizine may have some benefit.
Infection, environmental allergens and
environmental tobacco smoke
The long-term ramifications of the amount, timing and
extent of exposure to infections, environmental and food
S26
JAMC 13 SEPT. 2005; 173 (6)
allergens and environmental tobacco smoke and other respiratory irritants and the complex interactions of these factors with genetic factors are currently incompletely understood.1 Although sensitization of children can be prevented
by avoidance of environmental allergens, such as HDMs,24
there is no evidence that this is associated with secondary
prevention of asthma. However, most research efforts in
this area to date have focused on primary and tertiary prevention, rather than secondary prevention.1,25,26
The association between passive smoking and asthma in
children, including asthma development and asthma severity, is well-documented.27 However, it should be noted that
although avoidance of tobacco smoke exposure in at-risk
infants and children is logical and universally recommended by physicians, there are no studies proving that
avoidance of passive smoking is useful in the secondary prevention of asthma. Moreover, long-term changes in
parental smoking habits are difficult to achieve.28
Allergen-specific immunotherapy
Allergic rhinitis often precedes the onset of asthma. A 2year rigorously designed, prospective, randomized, doubleblind, placebo-controlled study28 followed 44 patients,
mean age 19 years (range 1038 years), with a documented
history of perennial atopic rhinitis, but no history of asthma
and normal pulmonary function tests, who were monosensitized to HDM (Dermatophagoides pteronyssinus) and had no
other allergies. In this group, D. pteronyssinus immunotherapy reduced the progression of rhinitis to asthma and prevented an associated increase in bronchial hyperreactivity.
After 1 year of treatment, patients receiving immunotherapy had increased PD20 FEV1 for methacholine (2.88-fold
increase, 95% CI 2.093.98) and showed further improvement after 2 years (OR 4.1, 95% CI 2.095.7). At the end
of the study, the PD20 FEV1 was within the normal range
for 50% of the treated patients (p < 0.0001) and significantly higher in this group than in those receiving placebo
(p < 0.0001); PD20 FEV1 > 8 mmol versus 2.9 mmol. None
of the patients treated with immunotherapy developed
asthma, yet 9% of those given placebo did. The investigators concluded that immunotherapy administered to carefully selected, monosensitized patients with perennial allergic rhinitis but no asthma reduces airway responsiveness
and thus holds some promise for secondary prevention of
asthma.
In another study,29 205 children, mean age 10.7 years
(range 614 years) with grass or birch pollen allergy (or
both) but without any other clinically important allergy or
asthma needing daily medications were randomly chosen to
receive allergen-specific immunotherapy for 3 years or assigned to an open control group. After 3 years, among
those without asthma, the treated children had significantly
fewer asthma symptoms, as evaluated by clinical diagnosis
(OR 2.52, 95% CI 1.35.1). The results of methacholine
bronchial provocation tests improved significantly in the
Prevention
treatment group during the winter (PC20 OR 2.75, 95% CI
1.26.3), but not during the allergy season (PC20 OR 1.43,
95% CI 0.82.7). The investigators concluded that immunotherapy can reduce the development of asthma in
children with seasonal rhinoconjunctivitis. However, the
conclusions that can be drawn from this randomized, clinical trial are limited by the fact that it was not double-blind
or placebo-controlled and that, before the start of immunotherapy, 20% of the children likely had mild asthma,
although they did not need daily treatment.
In other studies that were prospective, but not randomized, double-blind or placebo-controlled,30,31 and in a retrospective study,32 the investigators concluded that allergenspecific immunotherapy may prevent the onset of new
sensitization in children with respiratory symptoms and
monosensitization to HDMs.
Implications for research
1. Future research should consist of appropriately timed
and adequately powered, randomized, double-blind,
placebo-controlled studies of the following: additional
H1-antihistamines with anti-allergic, anti-inflammatory
effects; additional classes of pharmacologic treatment,
such as inhaled glucocorticoids, leukotriene modifiers
and topical calcineuron inhibitors; new immunomodulators, such as anti-IgE; and allergen-specific immunotherapy.
2. Also needed are randomized, controlled studies of the
role of avoidance of environmental allergens and tobacco smoke in the secondary prevention of asthma.
References
1. Wahn U, von Mutius E. Childhood risk factors for atopy and the importance
of early intervention. J Allergy Clin Immunol 2001;107(4):567-74.
2. Kulig M, Bergmann R, Klettke U, Wahn V, Tacke U, Wahn U. Natural
course of sensitization to food and inhalant allergens during the first 6 years
of life. J Allergy Clin Immunol 1999;103(6):1173-9.
3. National Asthma Education and Prevention Program expert panel report:
guidelines for the diagnosis and management of asthma update on selected
topics 2002. J Allergy Clin Immunol 2002;110(5 suppl.):S141-219.
4. Simons FE. Is antihistamine (H1-receptor antagonist) therapy useful in clinical asthma? Clin Exp Allergy 1999;29(suppl. 3):98-104.
5. Iikura Y, Naspitz CK, Mikawa H, Talaricoficho S, Baba M, Sole D, et al. Prevention of asthma by ketotifen in infants with atopic dermatitis. Ann Allergy
1992;68(3):233-6.
6. Bustos GJ, Bustos D, Bustos GJ, Romero O. Prevention of asthma with ketotifen in preasthmatic children: a three-year follow-up study. Clin Exp Allergy
1995;25(6):568-73.
7. Allergic factors associated with the development of asthma and the influence
of cetirizine in a double-blind, randomised, placebo-controlled trial: first results of ETAC. Early Treatment of the Atopic Child. Pediatr Allergy Immunol
1998;9(3):116-24.
8. Warner JO, ETAC Study Group. A double-blind, randomized, placebo-controlled trial of cetirizine in preventing the onset of asthma in children with
atopic dermatitis: 18 months treatment and 18 months posttreatment follow-up. J Allergy Clin Immunol 2001;108(6):929-37.
9. Leurs R, Church MK, Taglialatela M. H1-antihistamines: inverse agonism,
anti-inflammatory actions and cardiac effects. Clin Exp Allergy
2002;32(4):489-98.
10. Diepgen TL, Early Treatment of the Atopic Child Study Group. Long-term
treatment with cetirizine of infants with atopic dermatitis: a multi-country,
double-blind, randomized, placebo-controlled trial (the ETAC trial) over 18
months. Pediatr Allergy Immunol 2002;13(4):278-86.
11. Simons FE. Prevention of acute urticaria in young children with atopic dermatitis. J Allergy Clin Immunol 2001;107(4):703-6.
12. Simons FE. Prospective, long-term safety evaluation of the H1-receptor antagonist cetirizine in very young children with atopic dermatitis. J Allergy Clin
Immunol 1999;104(2 pt 1):433-40.
13. Stevenson J, Cornah D, Evrard P, Vanderheyden V, Billard C, Bax M, et al.
Long-term evaluation of the impact of the h1-receptor antagonist cetirizine
on the behavioral, cognitive and psychomotor development of very young
children with atopic dermatitis. Pediatr Res 2002;52(2):251-7.
14. de Longueville M, Deruyter B. RR, QT, and QTc in 799 infants aged 1-2
years. J Allergy Clin Immunol 1998;101:S198.
15. Grimfeld A, Holgate ST, Adam D, Bonini S, Borres M, Canonica GW, et al.
Preventive study phase I results: loratadine treatment reduces wheezing
episodes in children at risk for recurrent upper respiratory infections. Allergy
2000;55(Suppl 63):242.
16. Baker JW, Mellon M, Wald J, Welch M, Cruz-Rivera M, Walton-Bowen K.
A multiple-dosing, placebo-controlled study of budesonide inhalation suspension given once or twice daily for treatment of persistent asthma in young
children and infants. Pediatrics 1999;103(2):414-21.
17. Knorr B, Franchi LM, Bisgaard H, Vermeulen JH, LeSouf P, Santanello N,
et al. Montelukast, a leukotriene receptor antagonist, for the treatment of persistent asthma in children aged 2 to 5 years. Pediatrics 2001;108(3):E48.
18. Nimmagadda SR, Szefler SJ, Spahn JD, Surs W, Leung DY. Allergen exposure decreases glucocorticoid receptor binding affinity and steroid responsiveness in atopic asthmatics. Am J Respir Crit Care Med 1997;155(1):87-93.
19. Milgrom H, Fick RB Jr, Su JQ, Reimann JD, Bush RK, Watrous ML, et al.
Treatment of allergic asthma with monoclonal anti-IgE antibody. N Engl J
Med 1999;341(26):1966-73.
20. Kuehr J, Brauburger J, Zielen S, Schauer U, Kamin W, Von Berg A, et al. Efficacy of combination treatment with anti-IgE plus specific immunotherapy in
polysensitized children and adolescents with seasonal allergic rhinitis. J Allergy Clin Immunol 2002;109(2):274-80.
21. Barnes PJ. Cytokine-directed therapies for asthma. J Allergy Clin Immunol
2001;108(2 suppl):S72-6.
22. Simons FER, Shikishima Y, van Nest G, Eiden JJ, HayGlass KT. Allergenselective redirection of immunoregulatory responses in ragweed-allergic humans using Dynavax Amb a 1 immunostimulatory oligodeoxyribonucleotide
conjugate (AIC). J Allergy Clin Immunol 2003;111(2 pt 2):S267.
23. Arshad SH, Bojarskas J, Tsitoura S, Matthews S, Mealy B, Dean T, et al. Prevention of sensitization to house dust mite by allergen avoidance in school age
children: a randomized controlled study. Clin Exp Allergy 2002;32(6):843-9.
24. Liu AH, Murphy JR. Hygiene hypothesis: fact or fiction? J Allergy Clin Immunol 2003;111(3):471-8.
25. von Mutius E, Martinez FD. Prevention of allergic disease in childhood. In:
Adkinson NF Jr, Yunginger JW, Busse WW, Bochner BS, Holgate ST, Simons FER, editors. Middletons allergy: principles and practice. 6th ed. St. Louis:
Mosby; 2003:1169-74.
26. Cook DG, Strachan DP. Health effects of passive smoking. 10. Summary of
effects of parental smoking on the respiratory health of children and implications for research. Thorax 1999;54:357-66.
27. Irvine L, Crombie IK, Clark RA, Slane PW, Feyerabend C, Goodman KE, et
al. Advising parents of asthmatic children on passive smoking: randomised
controlled trial. BMJ 1999;318(7196):1456-9.
28. Grembiale RD, Camporota L, Naty S, Tranfa CME, Djukanovic R, Marsico
SA. Effects of specific immunotherapy in allergic rhinitic individuals with
bronchial hyperresponsiveness. Am J Respir Crit Care Med 2000;162(6):2048-52.
29. Moller C, Dreborg S, Ferdousi HA, Halken S, Host A, Jacobsen L, et al.
Pollen immunotherapy reduces the development of asthma in children with
seasonal rhinoconjunctivitis (the PAT-study). J Allergy Clin Immunol
2002;109(2):251-6.
30. Pajno GB, Barberio G, De Luca F, Morabito L, Parmiani S. Prevention of
new sensitizations in asthmatic children monosensitized to house dust mite by
specific immunotherapy. A six-year follow-up study. Clin Exp Allergy
2001;31(9):1392-7.
31. Des Roches A, Paradis L, Menardo JL, Bouges S, Daures JP, Bousquet J. Immunotherapy with a standardized Dermatophagoides pteronyssinus extract. VI.
Specific immunotherapy prevents the onset of new sensitizations in children.
J Allergy Clin Immunol 1997;99(4):450-3.
32. Jacobsen L, Dreborg S, Moller C. Immunotherapy as a preventive treatment
[abstract]. J Allergy Clin Immunol 1996;97:232.
CMAJ SEPT. 13, 2005; 173 (6)
S27
Anda mungkin juga menyukai
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Risk Perception: Nicolai Bodemer and Wolfgang GaissmaierDokumen14 halamanRisk Perception: Nicolai Bodemer and Wolfgang GaissmaierAlina GheBelum ada peringkat
- Craske 2001Dokumen20 halamanCraske 2001Alina GheBelum ada peringkat
- Freest On 1994Dokumen12 halamanFreest On 1994Alina GheBelum ada peringkat
- Anxiety and Panic in Chronic Obstructive Pulmonary Disease: The Role of Catastrophic ThoughtsDokumen13 halamanAnxiety and Panic in Chronic Obstructive Pulmonary Disease: The Role of Catastrophic ThoughtsAlina Ghe100% (1)
- Janssen 2008Dokumen8 halamanJanssen 2008Alina GheBelum ada peringkat
- 455 FullDokumen10 halaman455 FullAlina GheBelum ada peringkat
- 158 FullDokumen18 halaman158 FullAlina GheBelum ada peringkat
- Integrative Cancer Therapies: An Oncology Mind-Body Medicine Day Care Clinic: Concept and Case PresentationDokumen6 halamanIntegrative Cancer Therapies: An Oncology Mind-Body Medicine Day Care Clinic: Concept and Case PresentationAlina GheBelum ada peringkat
- 496 FullDokumen8 halaman496 FullAlina GheBelum ada peringkat
- 43 Full PDFDokumen10 halaman43 Full PDFAlina GheBelum ada peringkat
- 201 FullDokumen11 halaman201 FullAlina GheBelum ada peringkat
- 217 FullDokumen10 halaman217 FullAlina GheBelum ada peringkat
- 167 FullDokumen10 halaman167 FullAlina GheBelum ada peringkat
- 81 Full PDFDokumen13 halaman81 Full PDFAlina GheBelum ada peringkat
- Evaluare Pentru Terapia Cu OxigenDokumen3 halamanEvaluare Pentru Terapia Cu OxigenAlina GheBelum ada peringkat
- 346 FullDokumen16 halaman346 FullAlina GheBelum ada peringkat
- FingerprintpatternDokumen21 halamanFingerprintpatternAlina GheBelum ada peringkat
- Integrative Cancer Therapies: The Impact of Healing Touch On Pediatric Oncology PatientsDokumen7 halamanIntegrative Cancer Therapies: The Impact of Healing Touch On Pediatric Oncology PatientsAlina GheBelum ada peringkat
- Graphology by June.E.Downey (Book Written in 1919)Dokumen160 halamanGraphology by June.E.Downey (Book Written in 1919)Nav D100% (6)
- 283 FullDokumen22 halaman283 FullAlina GheBelum ada peringkat
- Managementul Emboliei Pulmonare PDFDokumen23 halamanManagementul Emboliei Pulmonare PDFAlina GheBelum ada peringkat
- Psychological Science: Business Not As UsualDokumen5 halamanPsychological Science: Business Not As UsualAlina GheBelum ada peringkat
- Balter GuidelinesDokumen30 halamanBalter GuidelinesAlina GheBelum ada peringkat
- Boala Parenchimatoasa Pulmonara DifuzaDokumen30 halamanBoala Parenchimatoasa Pulmonara DifuzaAlina GheBelum ada peringkat
- Umbra Cuvintelor Octavian PalerDokumen51 halamanUmbra Cuvintelor Octavian PalerCismaru Elena100% (1)
- Tratamentul Inhalator Al Astmului Bronsic La CopilDokumen14 halamanTratamentul Inhalator Al Astmului Bronsic La CopilAlina GheBelum ada peringkat
- Psychological Science: ''Top-Down'' Effects Where None Should Be Found: The El Greco Fallacy in Perception ResearchDokumen10 halamanPsychological Science: ''Top-Down'' Effects Where None Should Be Found: The El Greco Fallacy in Perception ResearchAlina GheBelum ada peringkat
- Hematopoiesis - Curs (Engl)Dokumen9 halamanHematopoiesis - Curs (Engl)Alina GheBelum ada peringkat
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (120)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Speech SkincareDokumen2 halamanSpeech SkincarePI40621 Fatin Alyaa Binti Abdullah ZawawiBelum ada peringkat
- GREEN Manual - 2021Dokumen157 halamanGREEN Manual - 2021Bon Ber Amad Orofeo100% (2)
- PE NotesDokumen20 halamanPE NotesAlma C WalshBelum ada peringkat
- PDEV Notes For Periodical ExamDokumen7 halamanPDEV Notes For Periodical ExamErjie GerasmioBelum ada peringkat
- UrosepsaDokumen2 halamanUrosepsaHazir AziriBelum ada peringkat
- 7 Medicine RheumatologyDokumen28 halaman7 Medicine RheumatologyAmitBelum ada peringkat
- Material Safety Data Sheet Ecol Lube SilDokumen4 halamanMaterial Safety Data Sheet Ecol Lube Silfs1640Belum ada peringkat
- M.pharm SyllabusDokumen47 halamanM.pharm SyllabustusharphaleBelum ada peringkat
- Course - Fundamentals of Traditional Chinese Medicine - Center For True HealingDokumen49 halamanCourse - Fundamentals of Traditional Chinese Medicine - Center For True HealingAry Nogueira100% (1)
- Ultrasound Diagnosis and Management of Intra-Uterine GrowthDokumen7 halamanUltrasound Diagnosis and Management of Intra-Uterine GrowthPablo VispoBelum ada peringkat
- Lack of Sleep Research PaperDokumen8 halamanLack of Sleep Research Papergw1sj1yb100% (1)
- CV UPDATE Agt, 2021Dokumen6 halamanCV UPDATE Agt, 2021nadita erischaBelum ada peringkat
- NCM112 LP1 Rosales Reflective Writing 2Dokumen4 halamanNCM112 LP1 Rosales Reflective Writing 2Christine CalleyBelum ada peringkat
- Evidence Based Midwifery Care: Peny Ariani, SST, M.KebDokumen27 halamanEvidence Based Midwifery Care: Peny Ariani, SST, M.KebShinta Purnama DewiBelum ada peringkat
- Breastcrawl PDFDokumen41 halamanBreastcrawl PDFFayrouz EssawiBelum ada peringkat
- ADHD in ChildrenDokumen10 halamanADHD in ChildrenDebbie KlippBelum ada peringkat
- Economics For Pharmaceutical ManagementDokumen29 halamanEconomics For Pharmaceutical ManagementTifa IstiwaBelum ada peringkat
- Title of The ResearchDokumen5 halamanTitle of The ResearchNAMAN PARMARBelum ada peringkat
- Nursing Questions& AnswersDokumen37 halamanNursing Questions& AnswersSanjeev KumarBelum ada peringkat
- Family PlanningDokumen15 halamanFamily PlanningOkky isBelum ada peringkat
- Test Bank For Essentials of Health Information Management 4th Edition by BowieDokumen24 halamanTest Bank For Essentials of Health Information Management 4th Edition by BowieCarolynValentinebaep100% (43)
- Bpacnz Antibiotics GuideDokumen40 halamanBpacnz Antibiotics GuideBulborea MihaelaBelum ada peringkat
- NCP For Dizziness and HeadacheDokumen4 halamanNCP For Dizziness and Headachekarthi karthi100% (1)
- KajalDokumen6 halamanKajalKaju ParmarBelum ada peringkat
- NursingDokumen9 halamanNursingIlie SmarandacheBelum ada peringkat
- Activity 11 Cardiac Tamponade NCPDokumen3 halamanActivity 11 Cardiac Tamponade NCPCloe CorpuzBelum ada peringkat
- Non-Hemolytic Transfusion ReactionDokumen32 halamanNon-Hemolytic Transfusion Reactiondreyngerous100% (4)
- Developed by The Teaching History of Pharmacy Committee of The History of Pharmacy SIG, 2017-18Dokumen75 halamanDeveloped by The Teaching History of Pharmacy Committee of The History of Pharmacy SIG, 2017-18Durga MadhuriBelum ada peringkat
- Comfort, Effectiveness, AND Self-Awareness AS Criteria OF Improvement IN Psychotherapy"2Dokumen10 halamanComfort, Effectiveness, AND Self-Awareness AS Criteria OF Improvement IN Psychotherapy"2Ilaria PacificoBelum ada peringkat
- Pathfit 2: Exercise Myths and FallaciesDokumen7 halamanPathfit 2: Exercise Myths and FallaciesKeen Jude CaminosBelum ada peringkat