Renal Tumors in Infancy and Childhood
Diunggah oleh
madhuHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Renal Tumors in Infancy and Childhood
Diunggah oleh
madhuHak Cipta:
Format Tersedia
Pathology of renal tumors in infancy and childhood
Dr Sangeeta Desai
Pathology of Renal Tumors in Infancy and Childhood
Dr. Tanuja Shet
Dr Sangeeta Desai
Pathologists, Tata Memorial Hospital, Mumbai
The renal neoplasms in childhood are infrequent, often undifferentiated, have unusual
variants, mimic several other renal and extrarenal tumours and due to these reasons,
yield themselves to clinically significant diagnostic errors.
Significant advances in therapy & histology have led to parallel development of
protocols & various trials resulting in improved survival of children and young adults
with renal tumours. The role of pathologist in the total management of childhood renal
tumors cannot be overemphasized. Therapy is based on stage and histology!
Steps in grossing of renal tumors
Specimen must be submitted intact. Avoid frozen section & bivalving.
Weighing the specimen is mandatory. Stage I tumors weighing < 550mgs do not
require additional treatment.
Never strip capsule. Ink the external surface.
Locate vessels & ureter & take cut margins.
From the freshly cut surface, use tissue to molecular/ cytogenetics/ EM
Always sample the periphery of specimen and obviously uninvolved renal
parenchyma.
Submit nodes before tumor is cut to avoid floater.
Bisect the specimen such that tumor is seen well.
Serially slice the specimen 2 cm apart, incisions parallel to the initial one should
be made at the intervals of 2 cm avoiding sites of capsular infiltration.
Refrigerate in formalin & fix overnight
Grid the central slice and submit for histology entirely.
Why grid? - Essential for
Evaluating anaplasia
Evaluating post chemotherapy tumor (% necrosis)
Recognition of renal sinus
Detection of capsular invasion
Important anatomic considerations while grossing
Renal sinus is the concave region on the medial aspect of the kidney which contains
major renal vessels and portions of pelvicalyceal system. Medial sinus margin is
ragged connective tissue surrounding the resected renal vessels.
Pathology of Renal Tumors
Gaya Prasad Memorial Pathology Symposium
APCON 2005, Indore; 2nd December, 2005
Pathology of renal tumors in infancy and childhood
Dr Sangeeta Desai
Renal vein usually retracts and may give false impression of margin involvement, if the
tumour is in close proximity.
Essential features that must be documented in a histology report
Tumor type, favorable/ unfavorable histology
Extent of invasion, capsular invasion, status of renal sinus
Vascular / lymphatic emboli
Tumor kidney interface, nephrogenic rests
Margins
Lymph nodes number, metastasis +/-
Wilms tumour
Accurate staging and histology are very important since the therapeutic protocols are
stage related. Hence clinical stage determined by imaging and the operating surgeon
and pathologic stage determined by systematic gross and histologic examination are of
utmost importance.
Gross
There is nothing distinctive about gross features of WT. However, bilaterality,
multicentricity and renal vein thrombosis are more common in WT than in other renal
tumours.
Microscopy
Histology of WT is a recapitulation of nephrogenesis and aberrant epithelial and /or
mesenchymal differentiation. Depending on the predominance of the blastemal,
epithelial and mesenchymal elements, WT is characteristically described as tri-, bi- or
mono- phasic. Subtypes are classical triphasic (59%), blastemal predominant (25%),
epithelial predominant (8%) and mesenchymal predominant (8%). The predominant
pattern is the one which is noted in > 80% tumor. In pre-chemothrapy era, these
subtypes were important as the blastemal tumors fared badly; however in todays
chemotherapy era blastema is chemo sensitive while epithelial dominant tumors are
resistant to treatment
The reporting pathologist should be aware of nuclear details of blastema, since this
knowledge helps distinguish blastemal WT from the other NWT particularly on
aspiration cytology and biopsy. In blastemal cells, the ratio of length of the nucleus to
its width is <3; whereas in the cells of the mesenchymal elements the ratio is >3.
Pathology of Renal Tumors
Gaya Prasad Memorial Pathology Symposium
APCON 2005, Indore; 2nd December, 2005
Pathology of renal tumors in infancy and childhood
Dr Sangeeta Desai
Anaplasia in WT
Anaplasia is rare in WT cases <2 years of age.
Criteria for anaplasia are as follows: 1. Macronucleation: At least 3 fold nuclear
enlargement as compared with the nuclei of adjacent tumour cells which belong to the
same lineage. 2. Hyperchromasia 3. Markedly enlarged multipolar mitotic figures. The
diagnosis of anaplasia is made when all the three criteria meet and on scanner or low
power since the hyperchromatic enlarged nuclei stand out.
Anaplasia is classified as focal and diffuse. WT without anaplasia or with focal
anaplasia in any stage or diffuse anaplasia is stage I is categorized as tumour of
favourable histology (FH). Diffuse anaplasia in stage II, III, and IV is categorized as
anaplastic morphology, which denotes unfavourable histology (UH).
Please refer to the Suggested references for details on Anaplasia.
Staging of WT
Confirming or extending the clinical stage is one of the most important objectives of
pathologic study of the nephrectomy specimens. A case of stage I WT is converted to
stage II if the completely excised tumour is found: a. to extend into the perirenal soft
tissues or b. into the renal sinus lymphatics or blood vessels.
Stage II is converted to stage III if the tumour is found to be at the surgical resection
margin or lymph node metastasis.
Stage I WT with FH represents a WT, which is confined to the kidney and is completely
resected. It is associated with over 90% survival. However, relapse does occur in a few
patients with stage I FH WT. In recent years, two parameters, <550 g nephrectomy
specimen and age < 2 years have been correlated with the least possibility of relapse.
Non-Wilms tumours (NWT) of the kidney
NWT comprise mesoblastic nephroma (MN), clear cell sarcoma of kidney (CCSK),
rhabdoid tumour of kidney (RTK), renal cell carcinoma (RCC), papillary carcinoma,
PNET, angiomyolipoma and other rare tumours.
Mesoblastic nephroma (MN)
MN, a morphologically distinct tumor, is the predominant renal neoplasm in the first
three months of life, is uncommon after 6 months and very rare in adults. The vast
majority of patients are cured by surgical resection. A few recurrences and adverse
outcomes have been recorded, principally in patients older than three months at
presentation. This tumour has infiltrative borders and the risk of recurrence appears to
be dependent upon the completeness of the resection. Metastasis is rare.
Pathology of Renal Tumors
Gaya Prasad Memorial Pathology Symposium
APCON 2005, Indore; 2nd December, 2005
Pathology of renal tumors in infancy and childhood
Dr Sangeeta Desai
Gross
MN is usually large relative to the infant's kidney. Externally, the surface of the tumor
and kidney is smooth and the renal capsule and calyceal systems are stretched over
the tumor. The surface may be bosselated. The cut surface resembles that of a
leiomyoma: firm, whorled or trabeculated, and light colored. The tumor is
unencapsulated, typically interdigitates with the surrounding kidney, and may extend
into surrounding tissues. Renal vein invasion also occurs occasionally. Cysts,
hemorrhage, and necrosis are present in a minority of cases, particularly those that are
cellular on microscopic examination.
Microscopy
The classical pattern of MN is a moderately cellular proliferation of thick interlacing
bundles of spindle cells with elongate nuclei which usually infiltrate renal and perirenal
tissues. Entrapment of glomeruli and renal tubules is common. Mitotic figures are
usually in the range of 0 to 1 per 10 high power fields. Islands of cartilage and foci of
extramedullary hematopoiesis are present in some tumors.
Another, more common, pattern consists of a densely cellular proliferation of polygonal
cells with mitotic figures in the range of 8-30 per 10 high power fields, and often
pushing borders. This pattern has been called cellular MN. Cysts are common in this
pattern. The classical and cellular patterns often are mixed in the same tumor. Age and
completeness of resection are the primary risk factors for adverse outcome of MN, and
not histopathologic pattern.
There are cases which display overlap of cellular variant of MN and spindled variant of
CCSK, which suggests pathogenetic relationship between the two.
Differential diagnosis
MN usually is easily diagnosed when the histology and patients age are considered.
Preoperatively treated WT with stromal predominance may be confused with
congenital mesoblastic nephroma. This problem can usually be resolved by the
providing attention to the age, bilaterality, identification of blastema, nephrogenic rests
and tumour border.
CCSK
Originally called "bone-metastasizing renal tumor of childhood", CCSK is responsible
for maximum diagnostic discrepancies due to overlapping and variant patterns and is a
highly malignant neoplasm resistant to conventional therapy for WT, but often
responsive to doxorubicin-containing regimens. Thus, it is of considerable therapeutic
importance that CCSK be correctly diagnosed.
Pathology of Renal Tumors
Gaya Prasad Memorial Pathology Symposium
APCON 2005, Indore; 2nd December, 2005
Pathology of renal tumors in infancy and childhood
Dr Sangeeta Desai
Occurring in the same general age range as WT, CCSK comprises approximately 6%
of pediatric renal tumors. Most are diagnosed in patients between 12 and 36 months of
age. Approximately 66% of the patients are male. The propensity for metastasis to
bone and unusual sites is marked.
Gross
The appearance of the cut surfaces of this tumor is variable: it may be homogeneous,
gray and lobular or variegated, including firm gray whorled tissue and light pink soft
areas. Occasionally, the tumor may produce abundant mucin which gives a slimy
glistening appearance. Most appear well-circumscribed. Cysts ranging from a few
millimeters to centimeters in diameter are present in approximately a third of cases.
Often, the tumor weighs more than 500 g. Bilaterality has not been reported.
Microscopic
At low magnification, CCSK usually consists of a monotonous sheet of cells with lightly
staining cytoplasm. At higher magnification, the cells are arranged in cords separated
by septa composed of spindle cells with dark nuclei and a distinctive branching pattern
of small blood vessels. The cells in the cords have pale or vacuolated cytoplasm and
indistinct borders. Despite the name, the cytoplasm of CCSK is usually much less clear
than that of clear cell RCC and cytoplasmic clarity should not be relied upon to
establish the diagnosis. The nuclei contain finely dispersed chromatin and the nucleoli
are small. A characteristic feature is the infiltrative border between the CCSK and the
surrounding renal parenchyma.
Confusing variant patterns occur, including epithelioid, spindle cell, myxoid, cystic,
hyaline sclerosis, palisading and monstrocellular. The tumor should be sampled
generously to find classical areas.
Differential diagnosis
The distinctive vascular pattern and nuclear features of CCSK are often helpful in
distinguishing it from WT. However, in addition, some important points are as follows:
CCSK is unilateral and unicentric with infiltrative borders, unassociated with syndromes
and precursor lesions, blastema and nonrenal elements such as cartilage or muscle
are not found in CCSK and sclerotic stroma is uncommon in WT before therapy.
Exceptionally, CCSK may contain foci in which the cells have prominent nucleoli,
similar to those of RTK; other areas with classic pattern and lack of extreme
invasiveness, typical of CCSK usually will clarify the diagnosis.
Rhabdoid tumor of kidney (RTK)
The most malignant renal neoplasm of childhood, RTK is usually diagnosed in
advanced stage and metastasizes widely and causes death within 1 year of diagnosis.
The patients usually are very young at the time of diagnosis (NWTS median age 11
Pathology of Renal Tumors
Gaya Prasad Memorial Pathology Symposium
APCON 2005, Indore; 2nd December, 2005
Pathology of renal tumors in infancy and childhood
Dr Sangeeta Desai
months, and rare after 3 years) and there is a 1.5:1 predominance of boys to girls.
Associations with embryonal tumors of the central nervous system, neurovascular
hamartoma, paraneoplastic hypercalcemia and chromosome 22q11-12, 11p15.5
abnormalities have been reported.
Gross
RTK lacks the appearance of encapsulation often seen in cases of WT or CCSK. The
tumors usually are located medially in the kidney and the renal sinus and pelvis are
almost always infiltrated. They are typically yellow-gray or light tan friable tumors with
indistinct borders. Necrosis and hemorrhage are common.
Microscopy
RTK is typically diffuse and monotonous with poorly defined border. It consists of
medium or large polygonal cells with abundant eosinophilic cytoplasm, round nuclei
with thick nuclear membranes and large nucleoli. It is the resemblance of the
cytoplasm of these cells to differentiating rhabdomyoblasts which gave the tumor its
name. However, the resemblance to skeletal muscle is merely superficial and if definite
evidence of differentiation toward skeletal muscle is present, the tumor is not a
rhabdoid tumor. Often, the cytoplasm contains a large eosinophilic globular inclusion
which displaces the nucleus. Electron microscopy has shown that these consist of
aggregates of whorled filaments. As more cases have accrued to the NWTS, a wide
range of patterns has been appreciated, including sclerosing, epithelioid, spindle cell,
lymphomatoid, vascular, pseudopapillary, and cystic. Typically, these patterns are
mixed with the common pattern and with each other. The characteristic nuclear
features of large centrally placed nucleoli and thick nuclear membranes are usually
retained.
Differential diagnosis
A wide variety of renal and extrarenal tumors may mimic rhabdoid tumor in routine
sections. Cases of WT, congenital MN, RCC, urothelial carcinoma, collecting duct
carcinoma, oncocytoma, rhabdomyosarcoma, neuroendocrine carcinoma, and
lymphoma have been confused with RTK. Filamentous cytoplasmic inclusions or
conspicuous macronucleoli are the misleading features in most cases. Conventional
light microscopy is able to clarify most cases, but electron microscopy and
immunohistochemistry are sometimes necessary to show the characteristic features of
the mimics and exclude RTK. Occasionally, blastemal cells contain inclusions
suggestive of rhabdoid tumor, but the presence of characteristic aggregates of
blastema, such as nodules or serpentine groupings, clarifies the diagnosis.
RCC
Pathology of Renal Tumors
Gaya Prasad Memorial Pathology Symposium
APCON 2005, Indore; 2nd December, 2005
Pathology of renal tumors in infancy and childhood
Dr Sangeeta Desai
Conventional RCC is uncommon in children. Definite translocations associated with
RCC in children have been documented
Translocations involving chromosome Xp11.2
Renal carcinoma characterized by several different translocations involving
chromosome Xp11.2, all resulting in gene fusions involving the TFE3 gene
predominantly affect children and young adults. The most distinctive histopathologic
appearance is that of a carcinoma with papillary or nested architecture and clear cell
morphology. In keeping with the chromosomal translocation, the most distinctive
feature on immunohistochemistry is nuclear reactivity for TFE3 protein.
ASPL-TFE3 gene fusion t(X;17)(p11.2;q25)
The tumor cells in this tumor exhibit an organoid arrangement and pseudo
papillary pattern.
They also show extensive psammomatous calcifications. Each cell has
voluminous granular cytoplasm with distinct cell borders.
On EM The tumors exhibit a combination of features of both alveolar soft part
sarcoma and epithelial cells
t(6;11)(p21.1;q12) chromosome translocation
Tumor shows nests of polygonal clear cells with well defined cell membrane
A second population of smaller cells form clusters surrounded by nodules of pink
basement membrane like material stained with Periodic Acid Schiff D resistant
reaction.
On EM -The polygonal tumor cells contain abundant mitochondria and
membrane bound granules. The cytoplasm is rich in glycogen. Localized pools of
duplicated basement membrane material are prominent
Metanephric stromal tumor
MST is a recently recognized benign tumor which occurs in children (neonatal to 11
years old, mean age 24 months) and is equally prevalent in boys and girls. The most
common presentation is an abdominal mass, but hematuria or hypertension were the
presenting problem in some cases.
Gross
These are usually tan, lobulated, solid, and cystic (50%) tumors in the renal medulla.
Multifocal MST is present in more than 10% of cases, but bilaterality has not been
reported. The tumors appear well-circumscribed and were confined to the kidney. The
tumors ranged from 30 mm to 100 mm in diameter.
Microscopic pathology
Pathology of Renal Tumors
Gaya Prasad Memorial Pathology Symposium
APCON 2005, Indore; 2nd December, 2005
Pathology of renal tumors in infancy and childhood
Dr Sangeeta Desai
MST is unencapsulated and superficially infiltrates among renal structures. They tend
to infiltrate beneath the urothelium of the renal calices or pelvis. The general
appearance is of a variably cellular proliferation of spindle cells with tapered nuclei and
delicate cytoplasmic processes. The cells surround blood vessels or entrapped renal
tubules, forming hypocellular myxoid onion skin nodules. Entrapped renal tubules show
cystic change, epithelial hyperplasia; entrapped glomeruli show juxtaglomerular
hyperplasia; and entrapped arterioles may show angiodysplasia. Heterologous
differentiation toward glia, cartilage, and neuroectoderm may also be present.
MST is typically immunoreactive to CD34.
Molecular data have revealed that metanephric stromal tumor may represent the
biphasic middle portion of the spectrum of tumors with purely mesenchymal,
mesoblastic nephroma at one end and completely epithelial tumor, metanephric
adenoma at the other end.
Suggested References
1. Charles AK, Vujanic GM, Berry PJ. Renal tumours of childhood. Histopathology
1998; 32: 293-309.
2. Argani P, Perlman EJ, Breslow NE, Browning NG, Green DM, D'Angio GJ,
Beckwith JB. Clear cell sarcoma of the kidney: a review of 351 cases from the
National Wilms Tumor Study Group Pathology Center. Am J Surg Pathol 2000;
24: 4-18.
3. Argani P, Antonescu CR, Illei PB, Lui MY, Timmons CF, Newbury R, Reuter VE,
Garvin AJ, Perez-Atayde AR, Fletcher JA, Beckwith JB, Bridge JA, Ladanyi M.
Primary renal neoplasms with the ASPL-TFE3 gene fusion of alveolar soft part
sarcoma: a distinctive tumor entity previously included among renal cell
carcinomas of children and adolescents. Am J Pathol 2001;159:179-92.
4. Argani P, Hawkins A, Griffin CA, Goldstein JD, Haas M, Beckwith JB, Mankinen
CB, Perlman EJ. A distinctive pediatric renal neoplasm characterized by
epithelioid morphology, basement membrane production, focal HMB45
immunoreactivity, and t(6;11)(p21.1;q12) chromosome translocation. Am J Pathol
2001;158:2089-96.
5. Beckwith JB. National Wilms Tumor Study: an update for pathologists. Pediatr
Dev Pathol 1998; 1:79-84.
6. Faria P, Beckwith JB, Mishra K, Zuppan C, Weeks DA, Breslow N, Green DM.
Focal versus diffuse anaplasia in Wilms tumor--new definitions with prognostic
significance: a report from the National Wilms Tumor Study Group. Am J Surg
Pathol 1996; 20:909-20.
Pathology of Renal Tumors
Gaya Prasad Memorial Pathology Symposium
APCON 2005, Indore; 2nd December, 2005
Pathology of renal tumors in infancy and childhood
Dr Sangeeta Desai
Figure 1. Gross Specimen of Wilms Tumour
Fig 2. Triphasic Wilms tumour
Pathology of Renal Tumors
Gaya Prasad Memorial Pathology Symposium
APCON 2005, Indore; 2nd December, 2005
Pathology of renal tumors in infancy and childhood
Dr Sangeeta Desai
Fig 3. Anaplasia in Wilms tumour
Fig 4. Gross Specimen of Clear cell sarcoma
Pathology of Renal Tumors
Gaya Prasad Memorial Pathology Symposium
APCON 2005, Indore; 2nd December, 2005
10
Pathology of renal tumors in infancy and childhood
Dr Sangeeta Desai
Fig 5. Clear cell sarcoma
Fig 6. Mesoblastic_nephroma
Pathology of Renal Tumors
Gaya Prasad Memorial Pathology Symposium
APCON 2005, Indore; 2nd December, 2005
11
Pathology of renal tumors in infancy and childhood
Dr Sangeeta Desai
Fig 7. Mesoblastic nephroma
Fig 8. Rhabdoid Tumor
Pathology of Renal Tumors
Gaya Prasad Memorial Pathology Symposium
APCON 2005, Indore; 2nd December, 2005
12
Pathology of renal tumors in infancy and childhood
Dr Sangeeta Desai
Fig 9. Rhabdoid Tumor
Fig 10. Rhabdoid Tumor
Pathology of Renal Tumors
Gaya Prasad Memorial Pathology Symposium
APCON 2005, Indore; 2nd December, 2005
13
Anda mungkin juga menyukai
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5795)
- Renal Tumors in AdultsDokumen23 halamanRenal Tumors in AdultsmadhuBelum ada peringkat
- Self Study Guide: Disorders of Kidney, Glomerulonephritis, Kidney Failure, NephrolithiasisDokumen1 halamanSelf Study Guide: Disorders of Kidney, Glomerulonephritis, Kidney Failure, NephrolithiasismadhuBelum ada peringkat
- Pathologic Types Producing Nephrotic Syndrome (NS)Dokumen130 halamanPathologic Types Producing Nephrotic Syndrome (NS)madhuBelum ada peringkat
- Lecture 2 DR Ann Henry Forensic Applied Cognitive Psychology (Rape)Dokumen42 halamanLecture 2 DR Ann Henry Forensic Applied Cognitive Psychology (Rape)madhuBelum ada peringkat
- Tips For Urine Analysis: Max/Min Fill LineDokumen2 halamanTips For Urine Analysis: Max/Min Fill LinemadhuBelum ada peringkat
- Regeneration and Fibrous Repair: Leicester Warwick Medical SchoolDokumen29 halamanRegeneration and Fibrous Repair: Leicester Warwick Medical SchoolmadhuBelum ada peringkat
- Identifying and Interpreting Similes: Standards: 4th: R 3.5 5th: R1.5 6th: R 1.2 7th: R 1.1 8th: R 1.1Dokumen14 halamanIdentifying and Interpreting Similes: Standards: 4th: R 3.5 5th: R1.5 6th: R 1.2 7th: R 1.1 8th: R 1.1madhuBelum ada peringkat
- Renal StoneDokumen8 halamanRenal StonemadhuBelum ada peringkat
- Renal Tumors OverviewDokumen10 halamanRenal Tumors OverviewmadhuBelum ada peringkat
- Staphylococcus Streptococcus: Propertie S Morpholo Gy Culture & Biochemi Cal ReactionsDokumen3 halamanStaphylococcus Streptococcus: Propertie S Morpholo Gy Culture & Biochemi Cal ReactionsmadhuBelum ada peringkat
- Ch3 RegenDokumen51 halamanCh3 RegenmadhuBelum ada peringkat
- Today Is The First Day, of Rest of Your Life... !Dokumen41 halamanToday Is The First Day, of Rest of Your Life... !madhuBelum ada peringkat
- Glomerular DiseaseDokumen24 halamanGlomerular DiseasemadhuBelum ada peringkat
- View A Negative Experience in Your Life Like You'd Look at A Photo Negative. A Single Negative Can Create An Unlimited Number of Positive Prints.Dokumen90 halamanView A Negative Experience in Your Life Like You'd Look at A Photo Negative. A Single Negative Can Create An Unlimited Number of Positive Prints.madhuBelum ada peringkat
- 5.the Kidney - 5Dokumen19 halaman5.the Kidney - 5madhuBelum ada peringkat
- Division 3: Trauma EmergenciesDokumen48 halamanDivision 3: Trauma EmergenciesmadhuBelum ada peringkat
- First Foundations in Pathology Part 3: Growth and RepairDokumen46 halamanFirst Foundations in Pathology Part 3: Growth and RepairmadhuBelum ada peringkat
- 4 AbnormalitisOfCellGrowthDokumen28 halaman4 AbnormalitisOfCellGrowthmadhuBelum ada peringkat
- Alliteration: Reading SkillsDokumen17 halamanAlliteration: Reading SkillsmadhuBelum ada peringkat
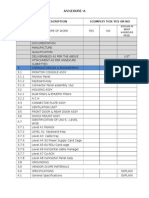
- Secto N Description (Comply) Tick Yes or No: Annexure-ADokumen2 halamanSecto N Description (Comply) Tick Yes or No: Annexure-AmadhuBelum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Mathematics Behind ContagionDokumen6 halamanThe Mathematics Behind Contagionkoonertex50% (2)
- A3 Report Template Checklist - SafetyCultureDokumen4 halamanA3 Report Template Checklist - SafetyCulturewarriorninBelum ada peringkat
- Resume Pet A Sol LanderDokumen3 halamanResume Pet A Sol LanderdreyesfinuliarBelum ada peringkat
- CE - 441 - Environmental Engineering II Lecture # 11 11-Nov-106, IEER, UET LahoreDokumen8 halamanCE - 441 - Environmental Engineering II Lecture # 11 11-Nov-106, IEER, UET LahoreWasif RiazBelum ada peringkat
- Modern Steel ConstructionDokumen70 halamanModern Steel ConstructionohundperBelum ada peringkat
- Floating Solar Photovoltaic Systems - An Overview and Their Feasibility at Kota in Rajasthan - IEEE Conference Publication - IEEE XploreDokumen3 halamanFloating Solar Photovoltaic Systems - An Overview and Their Feasibility at Kota in Rajasthan - IEEE Conference Publication - IEEE XploreJames KazoobaBelum ada peringkat
- Stats 116 SUDokumen128 halamanStats 116 SUCBelum ada peringkat
- Tok EssayDokumen2 halamanTok EssayNeto UkpongBelum ada peringkat
- TCC Number 153-4-4Dokumen1 halamanTCC Number 153-4-4jeremie gamonBelum ada peringkat
- 5G, 4G, Vonr Crash Course Complete Log AnaylsisDokumen11 halaman5G, 4G, Vonr Crash Course Complete Log AnaylsisJavier GonzalesBelum ada peringkat
- Allowable Nozzle LoadsDokumen6 halamanAllowable Nozzle Loads김동하Belum ada peringkat
- POLAR BEARS-Biology ProjectDokumen16 halamanPOLAR BEARS-Biology Projectserwaa21Belum ada peringkat
- SB Roadmap B1 1Dokumen161 halamanSB Roadmap B1 1Carmen Flores AloyBelum ada peringkat
- Networking With OrganizationsDokumen23 halamanNetworking With OrganizationsClaudette Lui Cabanos- Mercado-ReyesBelum ada peringkat
- Berghahn Dana ResumeDokumen2 halamanBerghahn Dana ResumeAnonymous fTYuIuK0pkBelum ada peringkat
- Master List WDokumen27 halamanMaster List Wefrem111Belum ada peringkat
- 1) About The Pandemic COVID-19Dokumen2 halaman1) About The Pandemic COVID-19محسين اشيكBelum ada peringkat
- Industrial Marketing Module 2Dokumen32 halamanIndustrial Marketing Module 2Raj Prixit RathoreBelum ada peringkat
- Learner Cala Guide: PART A: Identification of Knowledgeable Elderly Part BDokumen5 halamanLearner Cala Guide: PART A: Identification of Knowledgeable Elderly Part BPrimrose MurapeBelum ada peringkat
- Vivekananda'S Conception of Normative Ethics and Resolution Ethical Problems in BusinessDokumen8 halamanVivekananda'S Conception of Normative Ethics and Resolution Ethical Problems in BusinessYajat BhargavBelum ada peringkat
- Circuit Breaker - Ground & Test Device Type VR Electrically OperatedDokumen24 halamanCircuit Breaker - Ground & Test Device Type VR Electrically OperatedcadtilBelum ada peringkat
- Syllabus EM1Dokumen2 halamanSyllabus EM1Tyler AnthonyBelum ada peringkat
- Memo For Completed RubricDokumen3 halamanMemo For Completed Rubricnisev2003Belum ada peringkat
- D90KSDokumen1 halamanD90KSAmilton filhoBelum ada peringkat
- 3250-008 Foundations of Data Science Course Outline - Spring 2018Dokumen6 halaman3250-008 Foundations of Data Science Course Outline - Spring 2018vaneetBelum ada peringkat
- JamPlay 30 Minute Guitar Pratice TemplateDokumen23 halamanJamPlay 30 Minute Guitar Pratice TemplateSunkilr Sönny100% (4)
- Chapter - 01 Geography The Earth in The Solar SystemDokumen10 halamanChapter - 01 Geography The Earth in The Solar SystemKarsin ManochaBelum ada peringkat
- Robe Draft Geotechnical Report - Edited by k2nDokumen43 halamanRobe Draft Geotechnical Report - Edited by k2nASAMNEW GULILATBelum ada peringkat
- RKS IFC 2015 Solar CellDokumen23 halamanRKS IFC 2015 Solar CellAnugrah PangeranBelum ada peringkat
- EtchDokumen2 halamanEtchlex bactolBelum ada peringkat