Staph. Aureus
Diunggah oleh
gdubs215Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Staph. Aureus
Diunggah oleh
gdubs215Hak Cipta:
Format Tersedia
MSSA:
- Penicillin, in high doses, is the drug of choice for penicillin- sensitive S. aureus, although these strains are rare.
- Strains that produce penicillinase but are methicillin sensitive should be treated with semisynthetic compounds
(e.g. flucloxacillin, dicloxacillin, nafcillin, oxacillin) which have bactericidal activity.
- Alternatives that are active against methicillin-sensitive S. aureus include first generation cephalosporins (e.g.
cephalothin, cefazolin) and beta-lactam/beta-lactamase combinations such as amoxycillin-clavulanic acid.
- Anti-pseudomonal agents such as piperacillin-tazobactam, ticarcillin-clavulanic acid
and the carbapenems are also active against MSSA although of course their spectrum of
activity is far broader than necessary for this
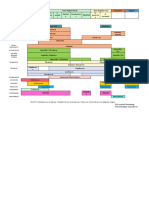
antimicrobial
therapy
- general
MRSA:
- Methicillin-resistant isolates are frequently cross-resistant to many antimicrobials including aminoglycosides, macrolides,
lincosamides, tetracyclines, co-trimoxazole, cephalosporins, carbapenems and beta-lactam/beta-lactamase combinations.
- Fluoroquinolone resistance is now widespread, particularly in MRSA isolates.
Although newer agents (e.g. levofloxacin, gatifloxacin, sparfloxacin and moxifloxacin) have improved Gram-positive
activity, the mechanism of cross-resistance amongst fluoroquinolones is such that susceptibility cannot be assumed
- Antibiotics with potential or proven activity against MRSA include vancomycin, teicoplanin, quinupristin-dalfopristin,
linezolid, rifampicin and fusidic acid.
laboratory
diagnosis
- S. aureus is arranged in grape-like clusters when viewed through the microscope.
- It is distinguished from other species by gold pigmentation of colonies and by positive results for
coagulase, mannitol fermentation and deoxyribonuclease tests
VISA:
- vancomycin-intermediate strains have all been sensitive to chloramphenicol, gentamicin, rifampicin, co-trimoxazole and tetracycline.
- The role of the recently approved antibiotics quinupristin / dalfopristin and linezolid
in the treatment of vancomycin-intermediate S. aureus infections is still unclear.
epidemiology
& development
of resistance
General:
- Vancomycin remains the drug of choice for MRSA, although it is intrinsically less active against Staphylococci than beta-lactams.
Tissue distribution and tissue penetration:
- has a wide volume of distribution but penetration into cerebrospinal fluid is poor.
- penetration into peritoneal dialysis fluid is unpredictable and may necessitate an intraperitoneal route
of administration for treatment of MRSA peritonitis in patients with a peritoneal dialysis catheter
Dosage adjustment in renal impairment
- intervals must be adjusted in patients with reduced creatinine clearance as renal excretion is the main route of drug elimination.
vancomycin
- Teicoplanin is a glycopeptide similar to vancomycin and is widely used in Europe, often in preference to vancomycin.
- It is usually active against both MSSA & MRSA.
General:
- These agents are streptogramins and are presented in combination at a fixed ratio of 30 : 70 (quinupristin: dalfopristin).
- The two compounds act synergistically on different sites of the 50S subunit of the bacterial ribosome to inhibit protein synthesis
Activity:
- It has good activity in vitro against a range of Gram-positive bacteria, including methicillin-resistant and
vancomycin-intermediate S. aureus.
- decreased in vivo susceptibility to quinupristin / dalfopristin has been noted with some erythromycin-resistant MRSA
Trials:
- Controlled trials indicate that quinupristin / dalfopristin and vancomycin are of comparable efficacy
for a range of MRSA infections, including skin infections, pneumonia and bacteraemia
teicoplanin
quinupristin:
dalfopristin
General:
- Rifampicin is a potent bactericidal agent which penetrates well into tissues and abscesses.
- High levels of resistance develop early if it is used alone; hence, it must
only be used with another antistaphylococcal agent to which the isolate is susceptible.
Trials:
- The role of rifampicin as an adjunctive drug in patients with S. aureus infections remains controversial.
Nonetheless, it is recommended in combination with gentamicin and either vancomycin or a semisynthetic
penicillin for prosthetic valve endocarditis.
- Humans are natural reservoirs for S. aureus and, as a surface commensal, it is most commonly found in the
anterior nares. - About 30% to 50% of healthy adults are colonised with S. aureus at any given time; 1020%
are persistently colonised
colonisation
& infection
General:
- Linezolid belongs to a new class of drugs called the oxazolidinones.
- It acts by inhibiting protein synthesis at an early stage of bacterial replication.
Activity:
- No cross resistance from other classes of antibiotics has been reported.
- It has inhibitory activity against a broad range of Gram-positive bacteria including MRSA and VISA
- Linezolid-resistant isolates have been recovered during clinical use, although reports are still rare
Trials:
- Clinical trials comparing vancomycin and linezolid in the treatment of infections caused
by MRSA have shown equivalent clinical and bacteriological success rates.
Staph
aureus
[created by
Paul Young
02/10/07]
- First described in the 1880s, S. aureus has adapted rapidly in the modern environment.
- Shortly after penicillin was first introduced, resistant strains of S. aureus producing penicillinase were reported.
- The development and use of semisynthetic penicillins
(e.g. flucloxacillin, oxacillin, cloxacillin and dicloxacillin) was quickly followed by new
resistance identified as early as 1961 in the United Kingdom
- Currently, in most USA and European hospitals, MRSA represents about 30% of all S. aureus isolates.
However, rates of up to 55% may be found in some ICUs.
- Furthermore, in some countries, methicillin-resistant S. aureus is no longer confined to the hospital
environment, having established itself as an important community pathogen, particularly in long-term
nursing care facilities in the USA
- Since the emergence of MRSA, the glycopeptide vancomycin has been the only uniformly effective
treatment for staphylococcal infections.
- Strains with reduced susceptibility to vancomycin referred to as vancomycin-intermediate or glycopeptide
intermediate S. aureus, have emerged, initially in 1996 in Japan, and subsequently in many areas including
the USA, UK, Europe, Australia and Asia.
- It is postulated that vancomycin-intermediate S. aureus arises from methicillin-resistant S. aureus clones
with heteroresistance, strains that are categorised as susceptible by conventional minimum inhibitory
concentration breakpoints but that generate vancomycin- intermediate S. aureus cells at high frequency
in their daughter
populations when exposed to vancomycin
- a truly vancomycin-resistant strain of S. aureus (minimum inhibitory concentration greater than 32 microg/ml
has been isolated in the USA from a renal dialysis patient with a history of prolonged exposure to multiple
antibiotics including vancomycin.
- This strain possesses the enterococcal vanA gene, an acquisition that had previously only been observed in vitro
Higher rates of nasal S. aureus carriage are found in
(i) intravenous drug users,
(ii) diabetics,
(iii) those with long-term indwelling catheters
(iv) patients with acquired immunodeficiency syndrome
(v) inflammatory skin disorders
- Colonisation with either methicillin-sensitive or methicillin-resistant S. aureus increases the risk of
subsequent infections with the same colonising strains, particularly in wound infections and central venous
catheter-related bacteraemia
linezolid
rifampicin
Activity:
- Fusidic acid inhibits protein synthesis and is active in vitro against MSSA and MRSA. However, resistance develops if it is
used alone and, like rifampicin, it must be administered with another antistaphylococcal agent to which the strain is susceptible.
Trials:
- There are only case reports or small studies evaluating the clinical efficacy of combinations of fusidic acid with other
antibiotics, including vancomycin, flucloxacillin, teicoplanin, rifampicin and gentamicin; results have been varied.
Nonetheless, it remains frequentpractice to add either rifampicin or fusidic acid to the regimen in patients who are
either failing to respond to treatment or who have a deep-seated infection such as osteomyelitis
fusidic
acid
- Nasal de-colonisation reduces the rate of infections by S. aureus, particularly surgical
site infections and bacteraemias in haemodialysis patients.
- The most effective agent available for eradication of S. aureus nasal carriage is topical mupirocin
clinical
infections
- S. aureus causes many illnesses, including pneumonia, bacteraemia and sepsis,
superficial and deep skin and soft tissue infections and toxin-mediated disease.
- It remains one of the commonest pathogens isolated in ventilatorassociated pneumonia and catheter-related bacteraemia.
- S. aureus bacteraemia has a propensity to seed to other sites including the heart valves, bones, joints and spinal canal.
-Secondary abscesses formed at distant sites may act as foci for recurrent infections.
- It is worth noting that S. aureus is a common pathogen for native and prosthetic valve endocarditis and that
intravenous catheters remain the commonest source of innoculation.
- endocarditis may be under-diagnosed and all patients with S. aureus bacteraemia should be investigated
by echocardiography, as a diagnosis of endocarditis determines the duration of therapy
Anda mungkin juga menyukai
- Anatomy Exam Review Muscles Innervations VasculatureDokumen27 halamanAnatomy Exam Review Muscles Innervations Vasculaturegdubs215Belum ada peringkat
- Vegetable Freezing ChartDokumen2 halamanVegetable Freezing Chartgdubs215100% (1)
- Renin Angiotensin Aldosterone SystemDokumen1 halamanRenin Angiotensin Aldosterone Systemgdubs215Belum ada peringkat
- Anatomy of AirwaysDokumen6 halamanAnatomy of Airwaysgdubs215Belum ada peringkat
- Important Vertebral Landmarks Level StructureDokumen5 halamanImportant Vertebral Landmarks Level Structuregdubs215Belum ada peringkat
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- AntibioticsDokumen2 halamanAntibioticsSaeed HasanBelum ada peringkat
- Fortified Drops Chart A4 Modified 1pdfpdf 2Dokumen1 halamanFortified Drops Chart A4 Modified 1pdfpdf 2Rubén SepúlvedaBelum ada peringkat
- AntibioticsDokumen2 halamanAntibioticsPGI Custodio, Ed KristianBelum ada peringkat
- 1 Classification of The AntibioticsDokumen5 halaman1 Classification of The AntibioticsRahma WatiBelum ada peringkat
- B Emergence During The COVID 19 Pandemic of I Klebsiella Pneumoniae I ST307 Co Producing KPC 3 and NDM 1 Carbapenemases BDokumen2 halamanB Emergence During The COVID 19 Pandemic of I Klebsiella Pneumoniae I ST307 Co Producing KPC 3 and NDM 1 Carbapenemases BBacteriología AmebpbaBelum ada peringkat
- JKT Surveillance PPRA 2021Dokumen28 halamanJKT Surveillance PPRA 2021priyantoBelum ada peringkat
- Antibiotic GuidelineDokumen11 halamanAntibiotic GuidelineSanjay ShresthaBelum ada peringkat
- Data Pasien TB JuliDokumen42 halamanData Pasien TB JuliTsubbatun NajahBelum ada peringkat
- WHO Antibiotics Not Recommended 2022Dokumen3 halamanWHO Antibiotics Not Recommended 2022mohamad arifBelum ada peringkat
- Principles of Management of MDR-TBDokumen22 halamanPrinciples of Management of MDR-TBGeorge VergheseBelum ada peringkat
- Antibióticos Lecturas PDFDokumen211 halamanAntibióticos Lecturas PDFDiego Francisco Garcia OrtizBelum ada peringkat
- DFSV - (TIN) Antibiotic Detection LimitsDokumen2 halamanDFSV - (TIN) Antibiotic Detection LimitsChevronelleBelum ada peringkat
- Panencefalitis Esclerosante SubagudaDokumen5 halamanPanencefalitis Esclerosante SubagudaVictor Euclides Briones MoralesBelum ada peringkat
- Sejarah Klasifikasi Antibiotik Dewi - 2017Dokumen58 halamanSejarah Klasifikasi Antibiotik Dewi - 2017dr.syafril SpJPBelum ada peringkat
- Leprosy Summary of MedsDokumen1 halamanLeprosy Summary of MedsNikki LegaspiBelum ada peringkat
- 1 s2.0 S0924857922001455 MainDokumen13 halaman1 s2.0 S0924857922001455 MainRobert StryjakBelum ada peringkat
- Antimicrobial Resistance and Clinical Use in Respiratory InfectionsDokumen23 halamanAntimicrobial Resistance and Clinical Use in Respiratory InfectionsWamique IzharBelum ada peringkat
- Anti-Fungal Compound Library (96-Well) : Product DetailsDokumen1 halamanAnti-Fungal Compound Library (96-Well) : Product DetailsSenuke TestBelum ada peringkat
- Kartu StokDokumen120 halamanKartu StokBintangRamadhanBelum ada peringkat
- A Ten Disk Procedure For The Detection of Antibiotic Resistance in EnterobacteriacaeDokumen7 halamanA Ten Disk Procedure For The Detection of Antibiotic Resistance in EnterobacteriacaeNguyen Huu HienBelum ada peringkat
- Mark M Calban MD MPM-HSDDokumen58 halamanMark M Calban MD MPM-HSDZllison Mae Teodoro Mangabat100% (1)
- IECDokumen6 halamanIECThefatRatBelum ada peringkat
- MVG09Dokumen4 halamanMVG09Sondos HarbiehBelum ada peringkat
- Antibiotics and Penicillin Allergy: Contra-Indicated Contra - Indicated Contra - IndicatedDokumen1 halamanAntibiotics and Penicillin Allergy: Contra-Indicated Contra - Indicated Contra - IndicatedJeferson BraxtonBelum ada peringkat
- Chapter 20 Winter 2020Dokumen48 halamanChapter 20 Winter 2020LESLI RODRIGUEZ BENDEZUBelum ada peringkat
- Ppra Ab Terapi PDFDokumen83 halamanPpra Ab Terapi PDFDIONYSIUS BENIBelum ada peringkat
- Ampi+Salbactum Amo+ Clavulanate Piper+Tazobactam: ST ST ND ND ND ND TH ST ND TH TH TH RD RD RD TH THDokumen1 halamanAmpi+Salbactum Amo+ Clavulanate Piper+Tazobactam: ST ST ND ND ND ND TH ST ND TH TH TH RD RD RD TH THAnnieBelum ada peringkat
- Jurnal Pengobatan Empiris Keratitis BakterialDokumen16 halamanJurnal Pengobatan Empiris Keratitis BakterialimuhammadfahmiBelum ada peringkat
- Biology Class Xii Cbse Investigatory Project On AntibioticsDokumen37 halamanBiology Class Xii Cbse Investigatory Project On AntibioticsSaveen Kadian75% (4)