Amino Enhancer For Patch
Diunggah oleh
untia_sariJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Amino Enhancer For Patch
Diunggah oleh
untia_sariHak Cipta:
Format Tersedia
Journal of Controlled Release 165 (2013) 91100
Contents lists available at SciVerse ScienceDirect
Journal of Controlled Release
journal homepage: www.elsevier.com/locate/jconrel
Amino acid derivatives as transdermal permeation enhancers
Barbora Janov, Barbora kolov, Katarna Tkrov, Lea Wojnarov, Tom imnek, Pemysl Mladnka,
Tom Filipsk, Michal ha, Jaroslav Roh, Karel Palt, Alexandr Hrablek, Kateina Vvrov
Charles University in Prague, Faculty of Pharmacy in Hradec Krlov, Czech Republic
a r t i c l e
i n f o
Article history:
Received 11 July 2012
Accepted 3 November 2012
Available online 12 November 2012
Keywords:
Transdermal drug delivery
in vitro/in vivo skin absorption
Penetration enhancer
Amino acid
Stratum corneum
a b s t r a c t
Transdermal permeation enhancers are compounds that temporarily decrease skin barrier properties to promote drug ux. In this study, we investigated enhancers with amino acids (proline, sarcosine, alanine,
-alanine, and glycine) attached to hydrophobic chain(s) via a biodegradable ester link. The double-chain
lipid-like substances displayed no enhancing effect, whereas single-chain substances signicantly increased
skin permeability. The proline derivative L-Pro2 reached enhancement ratios of up to 40 at 1% concentration,
which is higher than that of the well-established and standard enhancers Azone, DDAIP, DDAK, and Transkarbam
12. No stereoselectivity was observed. L-Pro2 acted synergistically with propylene glycol. Infrared studies
revealed that L-Pro2 forms a separate liquid ordered phase in the stratum corneum lipids and has no signicant
effect on proteins. L-Pro2 action was at least partially reversible as measured by skin electrical impedance.
Toxicity in keratinocyte (HaCaT) and broblast (3T3) cell lines showed IC50 values ranging from tens to hundreds
of M, which is comparable with standard enhancers. Furthermore, L-Pro2 was rapidly decomposed in plasma.
In vivo transdermal absorption studies in rats conrmed the enhancing activity of L-Pro2 and suggested its negligible skin toxicity and minimal effect on transepidermal water loss. These properties make L-Pro2 a promising
candidate for potential clinical use.
2012 Elsevier B.V. All rights reserved.
1. Introduction
Transdermal drug delivery offers several advantages over conventional routes of administration, such as avoidance of the rst-pass
metabolism, stable plasma levels, lower incidence of side effects, and
improved patient compliance. However, due to the remarkable barrier
properties of the skin's uppermost layer, the stratum corneum (SC),
transdermal administration has not yet achieved its full potential. One
approach to enabling this route of administration for a wider range of
drugs is the use of chemical compounds that temporarily increase
drug ux, known as permeation enhancers or penetration/absorption
promoters (for reviews, see refs. [16]). Although much effort has
gone into the development of these compounds, their wider use in
clinical practice is hampered by the fact that their mechanisms of action
and their potential toxicity are still not fully understood.
Already in the 1980s, many surfactant-like compounds with C10
C12 chain length have been identied as potent permeation enhancers
Abbreviations: Ala, alanine; Azone, N-dodecylazepan-2-one; DDAIP, dodecyl 2(dimethylaminopropanoate); DDAK, dodecyl 6-(dimethylamino)hexanoate; ER, enhancement ratio; Gly, glycine; HC, hydrocortisone; IR, infrared; PBS, phosphate-buffered saline;
PG, propylene glycol; Pro, proline; Sar, sarcosine; SC, stratum corneum; T12, Transkarbam
12; TEWL, transepidermal water loss; TH, theophylline.
Corresponding author at: Charles University in Prague, Faculty of Pharmacy in Hradec
Krlov, Heyrovskho 1203, 500 05 Hradec Krlov, Czech Republic. Tel.: +420 495 067
497; fax: +420 495 067 166.
E-mail address: katerina.vavrova@faf.cuni.cz (K. Vvrov).
0168-3659/$ see front matter 2012 Elsevier B.V. All rights reserved.
http://dx.doi.org/10.1016/j.jconrel.2012.11.003
[714]; for reviews, see refs. [1,6,15]. Most of these enhancers, however,
affect also viable epidermal cells provoking signicant skin irritation.
One of the rare exceptions to this rule is an alanine derivative dodecyl
2-(dimethylamino)propanoate (DDAIP, NexAct, [16]), probably because
of its biodegradability by epidermal esterases. To identify more enhancers or their combinations with high potency and low irritation risk,
Mitragotri's group developed a high-throughput screening tool based
on the effect of enhancer on the skin electrical properties [1720]. They
demonstrated that there exist classes of enhancers for which potency
and irritation are not particularly well related [17]. One of the compounds
which displayed apparent efcacy without noticeable irritation potential
was another amino acid derivative, N-lauroylsarcosine [21,22].
Thus, amino-acid derivatives seem to be among the most promising
class of permeation enhancers, especially those with a hydrophobic
tail attached to an amino acid head via a biodegradable linkage,
e.g. an ester bond (Fig. 1A). This molecular design is advantageous
due to the amphiphilic structure of such enhancer, which could allow
it to incorporate into the SC lipid barrier and disrupt the tight arrangement of the membrane lipids. Then, after reaching enzymatically active
nucleated epidermis, its labile bond could be hydrolyzed, thus releasing
known non-toxic compounds with much lower irritation potential.
This approach to designing permeation enhancers resulted in the identication of highly potent enhancers with favorable properties, such
as DDAIP [16], Transkarbam 12 (T12, [23,24]), tranexamic acid derivatives [25], and dodecyl 6-(dimethylamino)hexanoate (DDAK, [2628],
Fig. 1B).
92
B. Janov et al. / Journal of Controlled Release 165 (2013) 91100
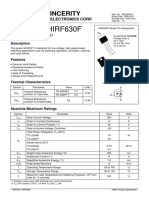
Fig. 1. Schematic representation of the design principles of the amino acid permeation enhancers (panel A), enhancers used as positive standards in this work (panel B), synthesis
(panel C), and structures of the studied amino acid permeation enhancers (panel D). Reagents and conditions: a dodecanol, HCl, 120 C, 7 h; b dodecanoic acid,
dicyclohexylcarbodiimide, 4-dimethylaminopyridine, CHCl3, rt, 20 h; c acetic anhydride, 4-dimethylaminopyridine, CHCl3, rt, 5 h; d ethylbromide, triethylamine, tetrahydrofuran, rt, 8 h. R1 and R2 = H, CH3, (CH2)3(Pro).
Here, we explore the use of the amino acids glycine (Gly), L- and
(L-Ala and D-Ala), -alanine (-Ala), sarcosine (Sar), and
L- and D-proline (L-Pro and D-Pro) as headgroup components of
permeation enhancers (Fig. 1D). Our interest in -amino acids was
originally based on L-serine, a starting amino acid in the biosynthesis
of the key skin barrier lipids, ceramides. We hypothesized that
enhancers and ceramides must bear a certain structural similarity to
ensure the molecular interaction required for their enhancing effect.
Thus, in a previous study, we attached two hydrophobic tails to
this amino acid to mimic the ceramide structure. We found that the
chain length was crucial: L-serine with 12C chains behaved as a moderate permeation enhancer [29,30] while its homolog 14S24, with the
same chain lengths as in ceramides, was able to repair skin barrier
perturbed by various insults [31,32]. The replacement of L-Ser by
Gly, i.e., removal of the hydroxymethyl group, increased its enhancing
activity, probably due to its lower ability to form hydrogen bonds
[29,30].
In this study, we prepared and studied a series of double-chain
enhancers based on the Gly homolog -Ala, its isomers L-Ala and
Sar, and also on the conformationally restricted cyclic amino acid
L-Pro. The latter two amino acids were included to test our hypothesis
that hydrogen bonding ability negatively inuences the enhancing
activity, and because Pro [33,34] and Sar [35] derivatives were previously reported to elicit permeation-enhancing activity. Interestingly,
Gly, -Ala, and Pro were also used to prepare prodrugs of 5-OHDPAT for transdermal iontophoretic delivery [36].
We also prepared a series of single-chain enhancers based on
the same amino acids to conrm our previous suggestion that the
removal of one long hydrophobic tail increases enhancing activity.
The effects of the prepared amino acid derivatives were compared
with known standard enhancers including Azone [37], DDAIP,
DDAK, and T12 (Fig. 1B). We also studied the reversibility of the effect
of L-Pro2, the best enhancer of this group, by electrical impedance
measurements, and its interaction with the skin barrier lipids and
proteins by infrared spectroscopy. For this purpose, L-Pro2D25
D-alanine
with perdeuterated alkyl chain was synthesized. The toxicities of
selected enhancers and the possible involvement of apoptosis were
assessed in keratinocyte HaCaT and broblast 3T3 cell cultures and
compared to known enhancers. Furthermore, L- and D-enantiomers
of selected enhancers were evaluated to address any potential stereoselective action/toxicity. The most potent enhancer, L-Pro2, was also
studied in vivo in rats to conrm its enhancing properties, toxicity,
effect on transepidermal water loss (TEWL) and biodegradability.
2. Materials and methods
2.1. Synthesis of enhancers
The synthetic procedures and properties of the prepared compounds
including deuterated L-Pro2D25 are given in the Supplementary data.
2.2. Donor samples for permeation studies
Control donor samples were prepared as 5% (w/v) suspensions
of theophylline (TH) or 2% (w/v) suspensions of hydrocortisone
(HC) in distilled water, 60% propylene glycol (PG, v/v), and isopropyl
myristate, respectively. TH (mol. weight 180 g/mol, logP ~ 0) and HC
(362 g/mol, logP 1.6) were selected as model permeability markers
representing drugs of different physicochemical properties. Enhancer
samples for co-application experiments were prepared by adding
1% (w/v) of the studied enhancer to the aforementioned drug suspensions. The samples were stirred at 50 C for 5 min and then
allowed to equilibrate at 37 C for 24 h. Before application to the
skin, the samples were resuspended. The concentrations were selected so that all samples were saturated with both the pertinent model
drug and studied enhancer to maintain the same thermodynamic
activity throughout the experiments. To determine whether the
added enhancers had any effects on the solubility of the drugs in
the donor solvent, the samples were prepared in triplicate as described above and allowed to equilibrate. After 24 h, the suspensions
B. Janov et al. / Journal of Controlled Release 165 (2013) 91100
were centrifuged at 6,700 g for 5 min; the supernatant was withdrawn, diluted with the pertinent mobile phase and analyzed by
HPLC. L-Pro2 donor samples for impedance and IR experiments
containing 1% (w/v) L-Pro2 in 60% PG without the model drug were
prepared likewise. Moreover, 1% enhancer dispersions in water and
60% PG without the drugs were also prepared to check their solubility
and stability at 37 C.
2.3. Permeation experiments
Skin permeability was evaluated using modied Franz diffusion cells
with an available diffusion area of 1 cm2 and an acceptor volume of approximately 17 ml. Frozen porcine skin (for details, see Supplementary
data) was slowly thawed, cut into pieces of 2 2 cm, mounted into
the diffusion cells dermal side down and sealed with silicone grease.
The acceptor compartment was lled with phosphate-buffered saline
(PBS, containing 10 mM phosphate buffer, 137 mM NaCl and 2.7 mM
KCl) at pH 7.4 with 0.03% of sodium azide as a preservative, and the
volume of the acceptor phase was measured for each cell and included
in the calculation. The Franz diffusion cells with mounted skin samples
were placed in a water bath with a constant temperature of 32 C
equipped with a magnetic stirrer. After an equilibration period of 1 h,
skin integrity was checked by measurement of the electrical impedance
(see later) and then 200 l (i.e., an innite dose) of the donor sample
was applied to the SC side of the skin and covered with a glass slide.
The acceptor phase was stirred at 32 C throughout the experiment.
Sink conditions were maintained for all drugs. Samples of the acceptor
phase (0.6 ml) were withdrawn at predetermined time intervals and
replaced with fresh buffer solution. The permeation experiments were
run for 48 h and 52 h for TH and HC, respectively, to reach the pseudo
steady-state to calculate the drug ux. TH and HC were determined by
HPLC as described previously [24]; for details, see Supplementary
data. The cumulative amount of the drug permeated across the skin,
corrected for the acceptor phase replacement, was plotted against
time, and the steady state ux was calculated from the linear region
of the plot. The enhancement ratio (ER) was calculated as a ratio of
the ux with and without the enhancer.
2.4. Skin electrical impedance
The skin integrity before each permeation experiment and the
reversibility of the skin barrier function after L-Pro2 treatment was
studied by measuring the transdermal electrical impedance using an
LCR meter 4080 (Conrad electronic, Hirschau, Germany, measuring
range 20 10 M, error at k values b 0.5%) operated in a parallel
mode with an alternating frequency of 120 Hz, parameters that
yield the best sensitivity to small impedance changes [38]. The skin
samples were mounted into the Franz diffusion cells, the acceptor
compartments were lled with PBS at pH 7.4, and the cells were
equilibrated at 32 C for 1 h as described above. Half a milliliter of
PBS was introduced into a donor compartment and the baseline
skin resistance (k cm 2) was measured by two stainless steel electrodes carefully immersed into PBS in the donor and acceptor compartments of the diffusion cell. The buffer solution was removed
from the donor compartment using a cotton swab, and 200 l of the
donor sample containing 1% (w/v) of L-Pro2 in 60% PG was applied.
The rst set of control cells received 200 l of 60% PG without the
enhancer, and the second set received 200 l of distilled water to
distinguish the effect of hydration from that of PG and L-Pro2. The
donor samples were removed after 2 h or 48 h and the skin surface
was washed twice with 0.5 ml of PBS and gently blotted dry. The
impedance was measured for 20 h or 63 h. The reported values are
normalized to the baseline value (i.e., the impedance before treatment) of each skin fragment.
93
2.5. Isolation of SC and SC lipids
The SC sheets were isolated by trypsin treatment [39] and the
lipids were extracted using a modied Bligh and Dyer method [40].
For details, see Supplementary data.
2.6. Infrared (IR) spectroscopy
Before the experiment, SC sheets were cut into small pieces
(ca. 1 mg) and treated with 50 l of distilled water (control), 60%
PG, or 1% L-Pro2 in 60% PG at 32 C. Isolated SC lipids were either
untreated (control), or treated with 20 l of 60% PG, 1% L-Pro2 in
60% PG or 1% L-Pro2D25 in 60% PG at 32 C. After 2 h, the excess solution was carefully removed and the samples were examined by IR
spectroscopy. Fourier transform IR spectra of the samples were
collected on a Nicolet 6700 FT-IR spectrometer (Thermo Scientic,
USA) equipped with a single-reection MIRacle attenuated total
reectance (ATR) germanium crystal. A clamping mechanism with a
constant clamping pressure was used for all experiments. The spectra
were generated by co-addition of 128 scans collected at 4 cm 1 resolution. The spectra were analyzed using the Bruker OPUS software.
The exact peak positions were determined from second derivative
spectra and by peak tting if needed.
2.7. Cell lines
The HaCaT spontaneously immortalized human keratinocyte cell
line was purchased from the Cell Lines Service (Eppelheim, Germany)
and the 3T3-Swiss albino mouse embryonic broblast cell line was
from the American Type Culture Collection (ATCC, distributed by
LGC Standards, Poland). Cells were cultured in Dulbecco's modied
Eagle's medium (DMEM, Lonza, Belgium) supplemented with 10%
heat-inactivated fetal bovine serum (Lonza), 1% penicillin/streptomycin
solution (Lonza) and 10 mM HEPES buffer (Sigma, Germany) in 75 cm2
tissue culture asks (TPP, Switzerland) at 37 C in a humidied atmosphere of 5% CO2. Sub-conuent cells were subcultured every
34 days. For cytotoxicity experiments and caspase activity determinations, cells were seeded in 96-well plates (TPP) at a density of 5000 cells
per well. For morphology and uorescence assessments, cells were
seeded at a density of 75,000 cells per well in 12-well plates (TPP)
24 h prior to the addition of the test drugs. The cells plus test substances
were then incubated for 48 h under standard conditions. Whereas
DDAK and DDAIP (both in the form of hydrochlorides) were dissolved
in PBS, dimethylsulfoxide was used to dissolve Azone, and ethanol
was used for T12, Sar2, L-Pro2, and D-Pro2. The corresponding concentrations of solvents were always present in the control incubation
media.
2.8. Cellular toxicities of selected enhancers
Cellular toxicities were determined by the ability of active
mitochondria to change yellow 3-(4,5-dimethylthiazol-2-yl)-2,
5-difenyltetrazolium bromide (MTT; Sigma) to purple formazan.
After the 48-h experimental incubations, 25 l of MTT solution in
PBS (3 mg/ml) was added to 100 l medium in each well. After incubation for 2 h at 37 C, the cells were lysed with 0.1 M hydrochloric
acid in isopropanol with 10% Triton X-100. Plates were vigorously
shaken for 3 h to fully dissolve the formazan crystals. The optical densities were measured at = 570 nm, subtracting the = 690 nm
background using a Tecan Innite 200 M plate reader (Tecan, Austria).
The viabilities of experimental groups were expressed as percentages
of untreated controls (100%).
Changes in cellular morphology were evaluated using an inverted
epiuorescence microscope (Eclipse TS100, Nikon, Japan) equipped
with a digital cooled camera (1300Q, VDS Vosskhler, Germany)
and software NIS-Elements AR 2.30 (Laboratory Imaging, Czech
94
B. Janov et al. / Journal of Controlled Release 165 (2013) 91100
Republic). Cellular death was visualized using double staining of
nuclei with Hoechst 33342 (Molecular Probes) and propidium iodide
(PI; Molecular Probes), which are well established as sensitive procedures for determining apoptosis and necrosis. Hoechst 33342 is a
blue-uorescent probe (ex = 360 nm; em = 460 nm) that stains all
nuclei. In apoptotic cells, chromatin condensation occurs and apoptotic cells can thus be identied as those with condensed and more
intensely stained chromatin. The red DNA-binding dye, PI (ex =
560 nm; em = 630 nm), is unable to cross the plasma membrane of
living cells, but readily enters necrotic (or late-stage apoptotic) cells
and stains their nuclei red. Cells were loaded with 3 g/ml of Hoechst
33342 and 10 g/ml of PI for 15 min at room temperature and sample
images were taken using the microscope set-up described above.
2.9. Caspase activity
To assess the possible involvement of apoptosis in cell killing,
the activities of basic initiator (apical) as well as effector (executive)
caspases were determined after 48-h incubations of cells with selected concentrations of permeation enhancers. The cells were lysed by
adding 100 l of lysis buffer (100 mM HEPES, 10 mM CHAPS,
10 mM DTT, pH 7.4) to 100 l medium in each well. Lysates were immediately frozen at 80 C. Thawed lysates were then used for
caspase activity assessments using luminescent kits for caspases 3/7,
8 and 9 (Promega, U.S.A.). The caspase activities of experimental
groups were corrected for the protein content in each sample (BCA
kit, Sigma) and were expressed as a percentage of activities of untreated
controls (100%). The luminescence was measured using a Tecan Innite
200 M plate reader.
2.10. In vivo transdermal permeation, TEWL and dermal toxicity
Wistar:Han female rats (Biotest s.r.o., Czech Republic) were housed
in cages in an air-conditioned room with a periodic 12-h lightdark
cycles for two weeks. During this period, the rats had free access to
tap water and standard pellet diet for rodents. Before the experiments,
they were fasted overnight. The study was performed under the
supervision of the Ethical Committee of Charles University in Prague,
Faculty of Pharmacy in Hradec Krlov and conformed to The Guide
for the Care and Use of Laboratory Animals published by the US National
Institutes of Health (NIH Publication No. 85-23, revised 1996).
The rats were anaesthetized with 1.05 g/kg urethane i.p., hair on
the back was removed using an electric clipper and the formulations
(1.2 ml/kg of 5% TH in 60% PG with or without 1% L-Pro2) were
applied to 4 cm2 gauze patch, which was held in place with nonirritating occlusive patch. Blood samples were collected from the left
common iliac artery each 30 min for 8 h. TH in plasma samples was
determined by HPLC using protein precipitation with methanol and
caffeine as an internal standard (see Supplementary data).
For TEWL and toxicity measurements, rats received a) no treatment, b) 60% PG, c) 1% L-Pro2 in 60% PG, or d) 5% L-Pro2 in 60% PG
(all at 400 l in a 4 cm 2 gauze patch) for 6 h. After this period, the
patches were removed; the surface of the skin briey washed with
ethanol to remove the residual formulations, blotted dry and carefully
inspected for any erythema/edema/dryness. After 30 min, TEWL was
recorded using Tewameter TM 300 (Courage + Khazaka, Germany).
Animals were killed by intravenous administration of 1 ml of 1 M KCl
and skin biopsies were collected from the sites exposed to the tested
formulations. The effect of L-Pro2 on skin viability was determined by
a TTC assay (see Supplementary data).
2.11. Stability of L-Pro2 in rat plasma and PBS at 37 C
Rat plasma or PBS at pH 7.4 (1 ml, n = 4) containing L-Pro2 at
50 g/ml were incubated at 37 C. At predetermined time intervals,
10 l samples were withdrawn and vigorously mixed with 90 l of
methanol. The PBS samples were analyzed directly, plasma samples
were centrifuged at 6700 g for 5 min; the supernatant was withdrawn and then analyzed by HPLC (see Supplementary data).
2.12. Statistical analysis
A two-tailed Student's t-test was used when comparing two
different conditions. When comparing three or more conditions, a
one-way analysis of variance (ANOVA) with a Bonferroni post-hoc
test was performed using SigmaStat for Windows 3.5 (SPSS, U.S.A.).
In all cases, p b 0.05 was considered signicant. The concentrations
of enhancers inducing a 50% decrease in viability (IC50) were calculated using the CalcuSyn 2.0 software (Biosoft, Cambridge, U.K.).
Data are presented as means SEM and the number of replicates
(n) is given in the pertinent gures.
3. Results
3.1. Synthesis
The target compounds were designed as amino acid dodecyl esters
having either another 12C chain (referred to as double-chain
enhancers) or a short acetyl or ethyl (single-chain enhancers) at its
amino group. To simplify their synthesis, the common fragments,
i.e., the dodecyl esters, were synthesized rst and used for the preparation of both enhancer series; the amino group was acylated
by carbodiimide coupling or using acetic anhydride, or alkylated by
ethylbromide (Fig. 1C and D). All products were crystalline, except
for the Pro derivatives. The logP values ranged from 4.9 to 6.8 in the
single chain enhancers and 10.412.1 in the double chain compounds.
At 1% concentration, all enhancers were saturated in water and 60%
PG (the solubilities were less than or equal to 0.58%), and stable for at
least 48 h.
3.2. Single-chain amino acid derivatives are better enhancers than
double-chain derivatives
The ux values of the model drug TH through the skin with and
without the studied amino acid derivatives and standard enhancers
are presented in Fig. 2. Panel A shows the ability of the studied
enhancers to increase the ux of TH when dispersed in a simple
aqueous vehicle. Without an enhancer, the ux of TH was 4.04
0.41 g/cm 2/h. Azone, which is used as a standard for permeationenhancing activity [37], increased this value 2.7-fold under these
conditions, DDAIP was inactive, while enhancers DDAK and T12 enhanced TH ux up to 7-fold. A non-signicant increase in ux (similar
to that shown by Azone), was elicited by all the studied double-chain
enhancers. The single-chain enhancers were generally more effective
than their double-chain counterparts (except for -Ala2), with the
most active compound being L-Pro2, giving a TH ux of 27.9
3.1 g/cm 2/h and a corresponding ER value of 6.9. L-Pro2 was signicantly more active than Azone and DDAIP, and comparable to DDAK
and T12. The second best enhancer was Sar2 with an ER value of
6.2, followed by Gly2 (ER = 3.9) and L-Ala2 (ER = 3.6). The solubility
of TH in the aqueous donor sample was 8.6 0.2 mg/ml. The
double-chain enhancers increased its solubility by 10%. It means
that the rather small insignicant increase in ux of TH in the presence of the double-chain substances was caused by the increased
solubility of TH in the donor vehicle. The single-chain enhancers
had no effect on TH solubility in the donor vehicle, suggesting a different mechanism of action. We also tested some of the intermediates,
i.e., amino acid dodecyl esters with a free amino group, but no signicant effects were observed (data not shown).
B. Janov et al. / Journal of Controlled Release 165 (2013) 91100
95
Fig. 3. The effects of L- and D-enantiomers of Pro12, Pro2, ProEt, and Ala2 permeation
enhancers (1%) on the transdermal ux of a model drug TH (5%) dispersed in water
(panel A) and in 60% PG (panel B). Control represents the ux of TH without an enhancer.
MeanSEM, n4 for the double-chain enhancers and8 for the single-chain ones; * indicates statistically signicant difference compared to the respective control at pb 0.05.
3.5. The skin permeation-enhancing activity of Pro and Ala derivatives
is not stereoselective
Fig. 2. The effects of the prepared amino acid permeation enhancers (1%) on the transdermal ux of a model drug TH (5%) dispersed in water (panel A) and in 60% PG (panel
B), respectively. Control represents the ux of TH without an enhancer. Mean SEM,
n 4 for the double-chain enhancers and 8 for the single-chain ones; * indicates
statistically signicant difference compared to the respective control or as indicated
at p b 0.05.
3.3. The most active permeation enhancer L-Pro2 acts synergistically
with PG
The enhancers were then combined with PG in an attempt
to increase their activity because (co)solvents like PG or ethanol
often act synergistically with amphiphilic surfactant-like enhancers
[8,12,13,41,42]. In 60% PG, the ux of TH without enhancers was
1.78 0.48 g/cm 2/h, which was slightly lower than that in a simple
aqueous vehicle (Fig. 2, panel B). However, when PG was combined
with the most active enhancer L-Pro2, the TH ux value increased to
70.3 7.7 g/cm 2/h, which is 40 times higher than that of PG alone
and 2.5 times higher than that of L-Pro2 dispersed in water. Such
synergy was not observed for the other studied enhancers, for
which the TH ux values were similar when applied in water or PG.
None of the positive controls, i.e., known enhancers reached the activity of L-Pro2. DDAIP, DDAK, and T12 reached ER values of 7.8, 23, and
19, respectively thus, L-Pro2 was signicantly more efcient than
all of them. The solubility of TH in 60% PG was 25 2 mg/ml; none
of the tested enhancers altered this value signicantly suggesting
their direct action in SC. We also investigated a lipophilic isopropyl
myristate as a donor vehicle. However, none of the prepared enhancers was able to increase the TH ux (2.63 0.63 g/cm 2/h)
signicantly under these conditions (data not shown).
As several of the studied amino acid enhancers are chiral, we examined whether their interaction with chiral SC components including
ceramides or proteins differs between enantiomers. Thus, we also
prepared the unnatural D-enantiomers of the selected enhancers,
namely D-Pro2, D-Pro12, D-ProEt, and D-Ala2. However, no signicant
difference was observed between the L- and D-enantiomers, either
double- or single-chain (Fig. 3).
3.6. L-Pro2 signicantly increases skin permeability for both lipophilic
and hydrophilic permeability markers
To further examine the ability of L-Pro2 to improve skin permeability
for a broader range of potential drugs, the ux of HC, a relatively large
lipophilic neutral molecule, was studied. The ux of HC in 60% PG
through the skin was 0.14 0.09 g/cm2/h. Combining PG with 1%
2
L-Pro2 increased the HC ux 47 times to 6.54 0.87 g/cm /h; the
skin permeation prole is shown in Fig. 4A. The solubility of HC in
the donor sample was 8.9 0.3 mg/ml; L-Pro2 increased this value
1.3-fold. That means that a part of the enhancing activity of L-Pro2
towards HC permeation was caused by an indirect increase of
the drug solubility in the donor vehicle. In terms of the permeability
coefcients Kp, which are independent of donor concentration,
5
L-Pro2 increased Kp value 31 times (from 1.80 10
cm/h to 5.65
104 cm/h).
Furthermore, skin electrical impedance was selected to probe the
ability of L-Pro2 to enhance the skin permeation of hydrophilic
permeants and to show that its action has a relatively rapid onset. The
baseline impedance values varied between 7.5 and 26.8 k cm2.
After 2 h and 48 h L-Pro2 treatment, the skin impedance reached 2.0
7.9 k cm2 and 1.51.9 k cm2, respectively (i.e., 35% and 8% of
the impedance before treatment), which was signicantly lower than
for PG alone (4.214.9 k cm2, i.e., 74% of the baseline after 2 h and
4.27.7 k cm2, i.e., 28% of the baseline after 48 h PG treatment,
Fig. 4B).
3.7. L-Pro2 enhancement is reversible
3.4. Substitution of N-acetyl by N-ethyl in Pro-derived enhancers
decreases enhancing activity
We also prepared and evaluated Pro derivatives in which the
N-acetyl was substituted with an ethyl group to mimic the basic tertiary amino group in the highly active enhancers DDAK and DDAIP.
However, this change led to a signicant decrease in activity, almost
to values comparable with the double-chain enhancers (Fig. 3).
Measurement of electrical impedance was further used to study
the ability of the skin permeability to recover from the action of
L-Pro2 enhancer. Each sample (water, 60% PG, and 1% L-Pro2 in 60%
PG) was applied to the skin for 2 h or 48 h, removed, and the skin impedance measured for 20 h or 63 h (Fig. 5). PG-treated skin served as
a control to distinguish between the actions of PG and L-Pro2; another
control received only water for 2 h in order to distinguish between
96
B. Janov et al. / Journal of Controlled Release 165 (2013) 91100
Fig. 4. The effects of L-Pro2 in 60% PG on the skin permeation of HC (2%) (panel A) and
skin electrical impedance after 2 and 48 h treatment (panel B). MeanSEM, n4; * indicates statistically signicant difference compared to the respective control (i.e., without
L-Pro2) at pb 0.05.
the action of PG and hydration. Fig. 5 shows that the PG alone had no
signicant effect on skin impedance and that the observed decrease
is fully attributable to the hydration of the skin [43]. Nevertheless,
L-Pro2 in PG signicantly decreased skin impedance already after
2-h application. After L-Pro2 had been removed from the skin surface,
the impedance further decreased, plateaued, and 6 h after the end
of the treatment, began to rise, reaching signicant recovery at 20 h
(Fig. 5A). Similar trend was observed after 48-h application of
L-Pro2 (Fig. 5B).
3.8. L-Pro2 forms separated liquid ordered phase in the SC lipids; PG
changes conformation of SC proteins
The mechanisms of action of L-Pro2 and PG in the skin barrier
were studied using IR spectroscopy. First, isolated SC sheets were
examined. Upon treatment with the enhancers, signicant changes
were found in the protein regions, in particular in the amide I vibrations, which are mostly composed of amide carbonyl stretching, and
are sensitive to changes in protein conformation. Untreated SC displayed a strong amide I vibration at around 1650 cm1 and a weak
one at 1620 cm1 typical of -helix and -sheet protein conformation,
respectively. The prevailing -helix was consistent with previous studies on SC proteins [44]. Treatment with PG and L-Pro2 in PG for 2 h
resulted in a shift of both vibrations towards higher wavenumbers
(Fig. 6AB), suggesting a partial change in hydrogen bonding of
the amide oxygens. The most prominent change in the amide region
was the decrease in the relative area of the -helix band from
Fig. 6. The effects of L-Pro2 on the protein (panels AC) and lipid (panels DF) components of SC studied using IR spectroscopy. A and B wavenumbers of amide I bands at
around 1650 and 1620 cm1, corresponding to -helix and -sheet protein conformation
in SC, respectively; C relative area of -helical conformation in SC proteins; D and E
wavenumbers and bandwidths, respectively, of symmetric methylene stretching of isolated SC lipids; F wavenumbers of symmetric CD2 stretching of L-Pro2D25, either
neat or in the SC lipids. MeanSEM, n6; *Statistically signicant difference compared
to the respective control or as indicated at pb 0.05.
approximately 67% to 48% (Fig. 6C). All these effects on the SC proteins
were caused by PG rather than L-Pro2.
For a more detailed investigation of the effects of PG and L-Pro2
on skin barrier lipids, isolated SC lipids were used to exclude the contribution of amino acid side chain vibrations in the CH stretching
region (Fig. 6DE). L-Pro2 was found to incorporate into the SC lipids
as reected by an increase in the area of CH stretching bands (not
shown). Such enhancer incorporation caused an increase in wavenumbers of both symmetric and asymmetric methylene stretching
from 2848.9 cm1 to 2850.2 cm1, and 2916.4 cm1 to 2918.4 cm1,
respectively, and peak broadening by 2.0 cm1 and 8.3 cm1,
respectively.
For a more precise interpretation of these results, we synthesized
L-Pro2D25 with perdeuterated alkyl chain to distinguish between
the methylene vibrations originating from the SC lipids and the
enhancer [45,46]. Incorporation of L-Pro2D25 did not increase the
SC lipid chain disorder suggesting that this enhancer forms a separate
phase within the SC lipids (Fig. 6DE). Examination of the CD2
stretching bands of neat enhancer and the SC lipids that had been
exposed to 1% L-Pro2D25 in 60% PG for 2 h revealed these separate
enhancer domains exist in a liquid ordered phase (Fig. 6F). This was
assigned according to literature data on CD2 vibrations [4749].
3.9. Toxicities of selected enhancers in HaCaT and 3T3 cell lines are
comparable to known enhancers
Fig. 5. The reversibility of L-Pro2 effects on skin electrical impedance when applied for
2 h (A) and 48 h (B). The data are expressed as % of the baseline value at time 0.
Mean SEM, n = 410; *Statistically signicant differences compared to the respective
control, i.e., PG-treated skin at p b 0.05, + indicates statistically signicant differences
at indicated time intervals at p b 0.05.
The toxicity experiments were run for 48 h, since most of the
studied enhancers did not induce a 50% reduction in cell viability
after 24 h. Following the 48-h incubations with HaCaT keratinocyte
or 3T3 broblast cell lines, all examined permeation enhancers
induced dose-dependent reductions in cellular viability. The IC50
values i.e., the concentration of drugs inducing a 50% decrease in
B. Janov et al. / Journal of Controlled Release 165 (2013) 91100
97
viability of all agents were lower in HaCaT cells (indicating higher
toxicity) as compared to the 3T3 cell line (Fig. 7, panel B). In both
cell lines, T12 was the most toxic agent, with IC50 values of ~ 20 M.
The toxicity of the most active enhancer L-Pro2 was approximately
two-fold higher than that of Azone, but similar to a widely used
enhancer DDAIP and also to DDAK. No signicant difference in toxicity was observed between the L- and D-enantiomers. The changes in
cellular morphology were followed by epiuorescence microscopy
(Fig. 7A). Following the 48-h incubations, peripheral membrane
blebbing occurred in a dose-dependent manner followed by the loss
of cell shape and rounding up of cells. Furthermore, severe nuclear
condensations occurred and eventually complete loss of cellular
viability was followed by the formation of cell debris. Although in individual permeation enhancers these changes occurred at different
concentrations, no conspicuous qualitative differences were observed
among the examined compounds.
We also examined the possible involvement of apoptosis by determining the effects of selected enhancers (at concentrations inducing
partial toxicity) on caspase activity. In HaCaT cells (Fig. 7C), relatively
slight (approximately two-fold) but signicant activation of all
caspases was observed with DDAK and T12; caspases 3/7 were also
activated by Azone. In 3T3 cells (Fig. 7D), a signicant increase in
caspase activity was observed with T12 and Pro derivatives. Whereas
T12 increased caspase activity approximately two-fold, comparable to
the effect seen with an equitoxic T12 dose in HaCaT cells, the effects
of L-Pro2 and D-Pro2 were particularly pronounced, reaching
14001800% of the control cells. All three caspases generally reached
comparable levels with all assayed permeation enhancers.
(Fig. 8A). Without the enhancer, the plasma concentrations of TH
were below 0.1 g/ml. With 1% L-Pro2, the plasma levels of TH
began to rise after 4 h and reached 1.27 0.09 g/ml after 8 h
administration.
Theoretically, an enhancer should increase drug ux into the body
without simultaneously increasing the loss of water and endogenous
substances from the body [3]. To test this assumption, TEWL [50]
was measured in vivo at the skin sites exposed to this enhancer for
6 h, i.e., under the conditions leading to signicant drug permeation.
The TEWL value was increased up to 1.7-fold after the application of
the tested formulations, but no signicant differences were observed
between 60% PG and L-Pro2 in PG, even when it was applied at 5
times higher concentration than was needed for the enhancement
effect (Fig. 8B). Thus, this increase of water loss could be attributed
mainly to PG. Furthermore, no visible changes (i.e., no erythema/
edema/dryness) were observed in the rats treated with L-Pro2 at
either 1% or 5% concentration in PG. To study the dermal toxicity
more closely, cell viability was determined in skin biopsies after 6-h
exposure to enhancers. Fig. 8C shows that under these conditions,
the permeation enhancement effect of L-Pro2 was not accompanied
by any signicant decrease of skin cell viability.
During the in vivo permeation study, no L-Pro2 was found in plasma suggesting either low systemic absorption or decomposition of
this enhancer in metabolically active skin layers or plasma. To study
the biodegradability of L-Pro2, it was incubated with rat plasma and
in PBS pH 7.4 at 37 C as a control. A decomposition of L-Pro2
with a half-life of ~ 2.5 h was found in plasma, while no signicant
decrease in concentration was found in PBS (Fig. 8D).
3.10. L-Pro2 enhances transdermal permeation of TH in rats in vivo with
negligible effects on TEWL and skin cell viability
4. Discussion
To examine the permeation-enhancing effect of L-Pro2 in vivo,
plasma concentrations of TH after transdermal administration of 5%
TH in 60% PG with or without 1% L-Pro2 to rats were monitored
In this study, we investigated a series of transdermal permeation
enhancers containing an amino acid linked to a hydrophobic chain(s)
via a labile ester bond. The double-chain compounds were designed
to resemble ceramides (neutral sphingolipids in the SC intercellular
Fig. 7. Toxicity of selected permeation enhancers in HaCaT keratinocyte and 3T3 broblast cell lines. A cellular morphology, B IC50 values, CD effects of selected enhancers on
the activity of caspases 3/7, 8, and 9 in HaCaT (C) and 3T3 cells (D). Mean SEM, n 4; *Statistically signicant difference compared to the respective control at p b 0.05.
98
B. Janov et al. / Journal of Controlled Release 165 (2013) 91100
Fig. 8. The enhancement activity of 1% L-Pro2 on transdermal delivery of TH in rats
in vivo (panel A), effects of 6-h administration of L-Pro2 (at 1% and 5%) and the vehicle
itself (60% PG) on TEWL and viability of dermal cells (panels B and C, respectively) in
rats in vivo, and metabolization of this enhancer in rat plasma compared to its stability
in PBS at pH 7.4 at 37 C (panel D). Mean SEM, n 3; *Statistically signicant difference compared to the respective control at p b 0.05.
lipid lamellae [51,52]), which are believed to be important targets of
the enhancers [2,3]. The 12C chains were selected based on previous
studies showing that this particular length was optimal for high
enhancing activity [714]; for reviews, see [1,6,15]. However, these
double-chain lipid-like compounds failed to increase skin permeability. On the contrary, their homologs, in which one of the two
12C chains had been shortened to two carbons (referred to as
single-chain enhancers), displayed substantially increased potency.
Similar results were previously found in dicarboxylic acid permeation
enhancers that were also more active with only one 12C chain [53].
Possible reasons for the lack of activity of the double-chain compounds may either be their inadequate permeability into the SC
lipid barrier or their similarity to ceramides, resulting in their inability to perturb the tight packing of these lipid membranes. Both possibilities are supported by data on ceramides showing changes in their
behavior in lipid membranes upon shortening of the acyl chain,
including their ability to translocate through the lipid lamellae and
inuence their permeability [54,55]. In fact, the only highly active
permeation enhancer having two hydrophobic chains is T12, a relatively unusual structure with a carbamic acid salt in its polar head.
Nevertheless, the mechanism of action of T12 involves the release
of carbon dioxide in SC, after which it continues acting as a singlechain enhancer [24]. Thus, the presence of only one 12C chain
seems to be an important prerequisite for potent permeation
enhancers.
In terms of polar head structure, the results of this study conrmed the previously proposed negative effect of hydrogen bonding
(especially of H-bond donors) on enhancing activity [29,30]. While
the enhancing potencies of Gly, Ala, and -Ala were similar, the Sar
and Pro derivatives, which are disubstituted amides, i.e., hydrogen
bond acceptors only, displayed increased activity. This is consistent
with previous studies showing that Sar and Pro-based compounds
are potent permeation enhancers [3335]. The negative role of hydrogen bonding may be viewed in terms of higher membrane cohesion
in the polar head region in addition to hydrophobic interactions
between the chains. However, the substitution of amide in Pro enhancers by a tertiary amino group resulted in a marked decrease in
activity. This is an interesting, yet unexplained nding because a
basic tertiary amine is an important structural feature in DDAIP and
DDAK [16,26]. This suggests that hydrogen bonding is not simply a
negative factor but that an optimum level of bonding is needed for
proper incorporation of an enhancer into the SC lipid lamellae, as
proposed previously [53].
This study also demonstrated that the action of Pro and Ala-based
enhancers is not stereoselective. We compared the activity of several
enhancer enantiomers based on the assumption that enhancers interact with chiral skin barrier constituents, either ceramides or proteins,
and that such interaction may be stereoselective. However, we found
no differences in the action of enhancer enantiomers, which is consistent with previous data on enhancers with the chiral center in the
hydrophobic chain [56] or the polar head [26].
After dening the basic structureactivity relationships, we focused on the best enhancer of this series, L-Pro2. This agent was
able to enhance the permeation of two model drugs with different
physicochemical properties: TH, a relatively small compound (molecular weight of 180 g/mol) of medium lipophilicity (logP ~ 0) that
is likely to cross the SC lipid lamellae by free-volume diffusion, and
HC, a two-fold larger lipophilic substance (362 g/mol, logP ~ 1.6)
that also permeates by lateral diffusion [57]. In addition, a signicant
decrease in skin electrical impedance was found upon the action of
L-Pro2. Skin impedance or resistance is often used as a rapid parameter for screening permeation enhancers [58,59] and reects the skin
permeability for ions [60,61]. Thus, L-Pro2 inuences different permeation pathways through the skin barrier, which gives it the opportunity to enhance the permeation of a relatively wide range of drugs.
Given its advantages for measuring skin permeability, we also used
the electrical impedance method to determine what happens to skin
permeability following the removal of L-Pro2 from its surface. The
results showed a signicant increase in impedance, i.e., a decrease in
permeability, after enhancer removal, suggesting partial recovery of
the skin barrier function. The most likely explanation of this behavior
is that L-Pro2 does not persist in the skin barrier and is relatively rapidly
eliminated, probably by simple diffusion into lower epidermal layers.
Similar reversibility of skin impedance was observed previously after
the treatment with permeation enhancer [26], iontophoresis [62,63],
or their combination [64].
L-Pro2 was also found to act synergistically with PG, which is in
good agreement with previous studies [8,12,13,41,42]. This may be
due to their action on different targets in the skin barrier. PG is a
small solvent molecule, previously suggested to inuence the conformation of SC proteins [65]. Because L-Pro2 is an amphiphilic compound, it was expected to incorporate into the SC intercellular lipid
lamellae with its polar head anchored in the polar membrane region
and the hydrophobic chain protruding into the hydrophobic core of
the lamellae. To study this hypothesis, interactions between L-Pro2
and PG and isolated SC or SC lipids were studied by IR spectroscopy.
This technique has been widely used to monitor the action of enhancers in the skin barrier [17,24,35,42,45,46,21]. It conrmed that
PG changes the hydrogen-bonding network of the SC proteins, and
increases the proportion of protein in the -sheet conformation,
probably by solvation of the peptide bonds. The contribution of
L-Pro2 to these changes was negligible, probably due to its more lipophilic nature. This enhancer was found to incorporate into the SC
lipids, broadening both methylene stretching bands and shifting
them to higher wavenumbers. This may be an indication of the lipid
disordering; however, such experiment cannot distinguish between
the lipid and enhancer chain. Thus, we repeated the experiment
with deuterated enhancer L-Pro2D25. This approach did not reveal
any SC lipid chain uidization but suggested that L-Pro2 acts by
formation of separate liquid ordered domains within the SC lipids
B. Janov et al. / Journal of Controlled Release 165 (2013) 91100
similarly to oleic acid [45,46]. Such phase separation may lead to formation of more permeable interfacial defects in the skin lipid barrier
[46]. This proposed mechanism of L-Pro2 action is consistent with its
reversibility, because following elimination of the enhancer (i.e., its
penetration into deeper skin layers), the lipids may spontaneously
reassemble.
We also examined the toxicity of selected enhancers in two skin
cell lines including keratinocytes and broblasts. The IC50 values
showed that the cellular toxicities of the studied Pro and Sar derivatives did not exceed that of a clinically used enhancer DDAIP. We
were interested in the possible involvement of apoptosis in the cellular toxicity of the studied enhancers. Apoptosis is the most important
form of programmed cell death and has been implicated in the cytotoxic action of numerous xenobiotic compounds. Whereas caspase
8 is the principal signaling molecule of the extrinsic (receptormediated) apoptotic pathway, caspase 9 is the key mediator of the
intrinsic (mitochondrial) pathway. Caspases 3 and 7 are the main
executioner death proteases, catalyzing the specic cleavage of
many key cellular proteins, and are activated in the apoptotic cell
by both extrinsic and intrinsic pathways. In particular, caspase 3 is indispensable for apoptotic chromatin condensation and DNA fragmentation. Whereas T12 increased caspase activity approximately
two-fold in both cell lines, L-Pro2 had no effect in the HaCaT
keratinocytes but caused a pronounced increase in caspase activity
in the 3T3 broblasts. This clearly warrants further study, but is of
no particular concern, as the overall toxicity was lower in 3T3
cells than in HaCaT (Fig. 7B). All three caspases generally reached
comparable levels; hence, the observed proapoptotic action of
some enhancers probably cannot be specically attributed to any
exclusive apoptotic pathway.
All these in vitro characteristics suggested that L-Pro2 is a promising transdermal permeation enhancer. Thus, we also performed a
proof of principle in vivo study in rats. Although rat skin structure
and permeability are different from human skin [66,67], the activity
of established enhancers was found to be reasonably similar
[6870]. Indeed, our experiments demonstrated a pronounced and
relatively rapid enhancement of transdermal absorption of a model
drug TH by 1% L-Pro2 without any signicant dermal toxicity. This
enhancement was also accompanied by moderate increase in water
loss, but this was attributed mainly to the PG vehicle. Furthermore,
the validity of the design principle of this class of enhancers, i.e., biodegradability of the ester linkage, was conrmed by a simple experiment in rat plasma as a representative of an enzymatically active
biological environment. In plasma, L-Pro2 was relatively rapidly
decomposed, but it was stable in PBS suggesting an enzymatic nature
of this reaction. Given its undetectable concentrations in plasma at
8 h and plasma half-life of 2.5 h, its systemic exposure is likely to be
very low. Thus, we expect that this enhancer, being an ester, may be
enzymatically hydrolyzed producing safe compounds already in
viable epidermis or early in plasma.
In conclusion, amino acid permeation enhancers, in particular the
proline-based compound L-Pro2, possess an advantageous combination of high activity, reversible action, and low toxicity, which make
them promising candidates for potential clinical use. The limitations
of the current study include the lack of data on long-term dermal
and systemic toxicities, and enhancers' absorption, metabolization
and elimination. This ADME characterization of the most promising
enhancers clearly warrants further studies.
Acknowledgements
This work was supported by the Czech Science Foundation (project no. 207/11/0365) and Charles University (SVV 265 001). We
also thank Hana Mikeov and Assoc. Prof. Ji Kune for IR and
NMR spectroscopy.
99
Appendix A. Supplementary data
Supplementary data to this article can be found online at http://
dx.doi.org/10.1016/j.jconrel.2012.11.003.
References
[1] T.M. Suhonen, J.A. Bouwstra, A. Urtti, Chemical enhancement of percutaneous
absorption in relation to stratum corneum structural alterations, J. Control.
Release 59 (2) (1999) 149161.
[2] B.W. Barry, Novel mechanisms and devices to enable successful transdermal drug
delivery, Eur. J. Pharm. Sci. 14 (2) (2001) 101114.
[3] A.C. Williams, B.W. Barry, Penetration enhancers, Adv. Drug Deliv. Rev. 56 (5)
(2004) 603618.
[4] D. Kaushik, P. Batheja, B. Kilfoyle, V. Rai, B. Michniak-Kohn, Percutaneous permeation modiers: enhancement versus retardation, Expert Opin. Drug Deliv. 5 (5)
(2008) 517529.
[5] M.R. Prausnitz, R. Langer, Transdermal drug delivery, Nat. Biotechnol. 26 (11)
(2008) 12611268.
[6] K. Vavrova, J. Zbytovska, A. Hrabalek, Amphiphilic transdermal permeation
enhancers: structureactivity relationships, Curr. Med. Chem. 12 (19) (2005)
22732291.
[7] E.R. Cooper, Penetrating topical pharmaceutical compositions containing
N-(2-hydroxyethyl)pyrrolidone. US 4,537,776 (1985).
[8] E.R. Cooper, Increased skin permeability for lipophilic molecules, J. Pharm. Sci. 73
(8) (1984) 11531156.
[9] M.L. Francoeur, R.O. Potts, Topical compositions of lipophilic pharmaceutical
agents. US 4,959,365 (1990).
[10] E.R. Cooper, Penetrating topical pharmaceutical compositions containing
9-(2-hydroxyethoxymethyl)guanine. EP 0,095,813 (1983).
[11] E.R. Cooper, Penetrating topical pharmaceutical compositions containing
1-dodecyl-azacycloheptan-2-one. US 4,557,934 (1985).
[12] M.L. Francoeur, R.O. Potts, Transdermal ux enhancing compositions to treat
hypertension, diabetes and angina pectoris. US 5,391,548 (1995).
[13] M.L. Francoeur, R.O. Potts, Transdermal ux enhancing compositions. US
5,196,410 (1993).
[14] S. Andega, N. Kanikkannan, M. Singh, Comparison of the effect of fatty alcohols on
the permeation of melatonin between porcine and human skin, J. Control. Release
77 (12) (2001) 1725.
[15] N. Kanikkannan, K. Kandimalla, S.S. Lamba, M. Singh, Structureactivity relationship of chemical penetration enhancers in transdermal drug delivery, Curr. Med.
Chem. 7 (6) (2000) 593608.
[16] S. Buyuktimkin, N. Buyuktimkin, J.H. Rytting, Synthesis and enhancing effect
of dodecyl 2-(N, N-dimethylamino)propionate on the transepidermal delivery
of indomethacin, clonidine, and hydrocortisone, Pharm. Res. 10 (11) (1993)
16321637.
[17] P. Karande, A. Jain, K. Ergun, V. Kispersky, S. Mitragotri, Design principles of
chemical penetration enhancers for transdermal drug delivery, Proc. Natl. Acad.
Sci. U. S. A. 102 (13) (2005) 46884693.
[18] P. Karande, A. Jain, S. Mitragotri, Discovery of transdermal penetration enhancers
by high-throughput screening, Nat. Biotechnol. 22 (2) (2004) 192197.
[19] P. Karande, S. Mitragotri, High throughput screening of transdermal formulations,
Pharm. Res. 19 (5) (2002) 655660.
[20] A. Arora, E. Kisak, P. Karande, J. Newsam, S. Mitragotri, Multicomponent chemical
enhancer formulations for transdermal drug delivery: more is not always better,
J. Control. Release 144 (2) (2010) 175180.
[21] P. Karande, A. Jain, A. Arora, M.J. Ho, S. Mitragotri, Synergistic effects of chemical
enhancers on skin permeability: a case study of sodium lauroylsarcosinate and
sorbitan monolaurate, Eur. J. Pharm. Sci. 31 (1) (2007) 17.
[22] P. Karande, A. Jain, S. Mitragotri, Insights into synergistic interactions in binary
mixtures of chemical permeation enhancers for transdermal drug delivery,
J. Control. Release 115 (1) (2006) 8593.
[23] A. Hrabalek, P. Dolezal, K. Vavrova, J. Zbytovska, T. Holas, J. Klimentova, J.
Novotny, Synthesis and enhancing effect of transkarbam 12 on the transdermal
delivery of theophylline, clotrimazole, obufen, and griseofulvin, Pharm. Res. 23
(5) (2006) 912919.
[24] M. Novotny, J. Klimentova, B. Janusova, K. Palat, A. Hrabalek, K. Vavrova, Ammonium carbamates as highly active transdermal permeation enhancers with a
dual mechanism of action, J. Control. Release 150 (2) (2011) 164170.
[25] K. Vavrova, A. Hrabalek, P. Dolezal, T. Holas, J. Klimentova, Biodegradable derivatives of tranexamic acid as transdermal permeation enhancers, J. Control. Release
104 (1) (2005) 4149.
[26] J. Novotny, P. Kovarikova, M. Novotny, B. Janusova, A. Hrabalek, K. Vavrova,
Dimethylamino acid esters as biodegradable and reversible transdermal permeation enhancers: effects of linking chain length, chirality and polyuorination,
Pharm. Res. 26 (4) (2009) 811821.
[27] K. Vavrova, P. Kovarikova, B. Skolova, M. Libalova, J. Roh, R. Cap, A. Holy, A.
Hrabalek, Enhanced topical and transdermal delivery of antineoplastic and
antiviral acyclic nucleoside phosphonate cPr-PMEDAP, Pharm. Res. 28 (12)
(2011) 31053115.
[28] K. Vavrova, K. Lorencova, J. Novotny, A. Holy, A. Hrabalek, Permeation enhancer
dodecyl 6-(dimethylamino)hexanoate increases transdermal and topical delivery
of adefovir: inuence of pH, ion-pairing and skin species, Eur. J. Pharm. Biopharm.
70 (3) (2008) 901907.
100
B. Janov et al. / Journal of Controlled Release 165 (2013) 91100
[29] K. Vavrova, A. Hrabalek, P. Dolezal, T. Holas, J. Zbytovska, L-Serine and glycine
based ceramide analogues as transdermal permeation enhancers: polar head
size and hydrogen bonding, Bioorg. Med. Chem. Lett. 13 (14) (2003) 23512353.
[30] K. Vavrova, A. Hrabalek, P. Dolezal, L. Samalova, K. Palat, J. Zbytovska, T. Holas, J.
Klimentova, Synthetic ceramide analogues as skin permeation enhancers: structureactivity relationships, Bioorg. Med. Chem. 11 (24) (2003) 53815390.
[31] K. Vvrov, A. Hrablek, S. Mac-Mary, P. Humbert, P. Muret, Ceramide analogue
14S24 selectively recovers perturbed human skin barrier, Br. J. Dermatol. 157
(4) (2007) 704712.
[32] K. Vvrov, J. Zbytovsk, K. Palt, T. Holas, J. Klimentov, A. Hrablek, P. Doleal,
Ceramide analogue 14S24 ((S)-2-tetracosanoylamino-3-hydroxypropionic acid
tetradecyl ester) is effective in skin barrier repair in vitro, Eur. J. Pharm. Sci. 21
(5) (2004) 581587.
[33] W.T. Harris, S.N. Tenjarla, J.M. Holbrook, J. Smith, C. Mead, J. Entrekin, n-pentyl
N-acetylprolinate. A new skin penetration enhancer, J. Pharm. Sci. 84 (5)
(1995) 640642.
[34] S.N. Tenjarla, R. Kasina, P. Puranajoti, M.S. Omar, W.T. Harris, Synthesis and evaluation of N-acetylprolinate esters novel skin penetration enhancers, Int. J.
Pharm. 192 (2) (1999) 147158.
[35] Y.C. Kim, J.H. Park, P.J. Ludovice, M.R. Prausnitz, Synergistic enhancement of skin
permeability by N-lauroylsarcosine and ethanol, Int. J. Pharm. 352 (12) (2008)
129138.
[36] O.W. Ackaert, J. De Graan, R. Capancioni, O.E. Della Pasqua, D. Dijkstra, B.H.
Westerink, M. Danhof, J.A. Bouwstra, The in vitro and in vivo evaluation of new
synthesized prodrugs of 5-OH-DPAT for iontophoretic delivery, J. Control. Release
144 (3) (2010) 296305.
[37] R.B. Stoughton, Enhanced percutaneous penetration with 1-dodecylazacycloheptan2-one, Arch. Dermatol. 118 (7) (1982) 474477.
[38] W.J. Fasano, P.M. Hinderliter, The Tinsley LCR Databridge Model 6401 and electrical impedance measurements to evaluate skin integrity in vitro, Toxicol. in Vitro
18 (5) (2004) 725729.
[39] A.M. Kligman, E. Christophers, Preparation of isolated sheets of human stratum
corneum, Arch. Dermatol. 88 (1963) 702705.
[40] E.G. Bligh, W.J. Dyer, A rapid method of total lipid extraction and purication, Can.
J. Biochem. Physiol. 37 (8) (1959) 911917.
[41] E.R. Cooper, E.W. Merritt, R.L. Smith, Effect of fatty acids and alcohols on the
penetration of acyclovir across human skin in vitro, J. Pharm. Sci. 74 (6) (1985)
688689.
[42] V.H. Mak, R.O. Potts, R.H. Guy, Percutaneous penetration enhancement in vivo
measured by attenuated total reectance infrared spectroscopy, Pharm. Res. 7
(8) (1990) 835841.
[43] I.H. Blank, J.E. Finesinger, Electrical resistance of the skin; effect of size of electrodes, exercise and cutaneous hydration, Arch. Neurol. Psychiatry 56 (5)
(1946) 544557.
[44] G. Bernard, M. Auger, J. Soucy, R. Pouliot, Physical characterization of the stratum
corneum of an in vitro psoriatic skin model by ATR-FTIR and Raman spectroscopies, Biochim. Biophys. Acta 1770 (9) (2007) 13171323.
[45] A. Naik, L.A.R.M. Pechtold, R.O. Potts, R.H. Guy, Mechanism of oleic acid-induced
skin penetration enhancement in vivo in humans, J. Control. Release 37 (3)
(1995) 299306.
[46] B. Ongpipattanakul, R.R. Burnette, R.O. Potts, M.L. Francoeur, Evidence that oleic
acid exists in a separate phase within stratum corneum lipids, Pharm. Res. 8 (3)
(1991) 350354.
[47] E. Brief, S. Kwak, J.T. Cheng, N. Kitson, J. Thewalt, M. Laeur, Phase behavior
of an equimolar mixture of N-palmitoyl-D-erythro-sphingosine, cholesterol, and
palmitic acid, a mixture with optimized hydrophobic matching, Langmuir 25
(13) (2009) 75237532.
[48] C. Pare, M. Laeur, F. Liu, R.N. Lewis, R.N. McElhaney, Differential scanning calorimetry and (2)H nuclear magnetic resonance and Fourier transform infrared
spectroscopy studies of the effects of transmembrane alpha-helical peptides on
the organization of phosphatidylcholine bilayers, Biochim. Biophys. Acta 1511
(1) (2001) 6073.
[49] V. Velkova, M. Laeur, Inuence of the lipid composition on the organization of
skin lipid model mixtures: an infrared spectroscopy investigation, Chem. Phys.
Lipids 117 (12) (2002) 6374.
[50] J. Pinnagoda, R.A. Tupker, T. Agner, J. Serup, Guidelines for transepidermal water
loss (TEWL) measurement. A report from the Standardization Group of the European Society of Contact Dermatitis, Contact Dermatitis 22 (3) (1990) 164178.
[51] J. Novotny, A. Hrabalek, K. Vavrova, Synthesis and structureactivity relationships
of skin ceramides, Curr. Med. Chem. 17 (21) (2010) 23012324.
[52] J. van Smeden, L. Hoppel, R. van der Heijden, T. Hankemeier, R.J. Vreeken, J.A.
Bouwstra, LC/MS analysis of stratum corneum lipids: ceramide proling and
discovery, J. Lipid Res. 52 (6) (2011) 12111221.
[53] M. Novotny, A. Hrabalek, B. Janusova, J. Novotny, K. Vavrova, Dicarboxylic acid
esters as transdermal permeation enhancers: effects of chain number and
geometric isomers, Bioorg. Med. Chem. Lett. 19 (2) (2009) 344347.
[54] J. Novotny, B. Janusova, M. Novotny, A. Hrabalek, K. Vavrova, Short-chain
ceramides decrease skin barrier properties, Skin Pharmacol. Physiol. 22 (1)
(2009) 2230.
[55] J. Novotny, K. Pospechova, A. Hrabalek, R. Cap, K. Vavrova, Synthesis of uorescent C24-ceramide: evidence for acyl chain length dependent differences in
penetration of exogenous NBD-ceramides into human skin, Bioorg. Med. Chem.
Lett. 19 (24) (2009) 69756977.
[56] K. Vavrova, A. Hrabalek, P. Dolezal, Enhancement effects of (R) and (S) enantiomers and the racemate of a model enhancer on permeation of theophylline
through human skin, Arch. Dermatol. Res. 294 (8) (2002) 383385.
[57] S. Mitragotri, Modeling skin permeability to hydrophilic and hydrophobic solutes
based on four permeation pathways, J. Control. Release 86 (1) (2003) 6992.
[58] J.E. Seto, B.E. Polat, B. Vanveller, R.F. Lopez, R. Langer, D. Blankschtein, Fluorescent
penetration enhancers for transdermal applications, J. Control. Release 158 (1)
(2012) 8592.
[59] P. Karande, A. Jain, S. Mitragotri, Relationships between skin's electrical impedance and permeability in the presence of chemical enhancers, J. Control. Release
110 (2) (2006) 307313.
[60] S.Y. Oh, L. Leung, D. Bommannan, R.H. Guy, R.O. Potts, Effect of current, ionic
strength and temperature on the electrical properties of skin, J. Control. Release
27 (1993) 115125.
[61] R.O. Potts, R.H. Guy, M.L. Francoeur, Routes of ionic permeability through
mammalian skin, Solid State Ionics 5356 (1992) 165169.
[62] N.G. Turner, Y.N. Kalia, R.H. Guy, The effect of current on skin barrier function in
vivo: recovery kinetics post-iontophoresis, Pharm. Res. 14 (9) (1997) 12521257.
[63] C. Curdy, Y.N. Kalia, R.H. Guy, Post-iontophoresis recovery of human skin impedance in vivo, Eur. J. Pharm. Biopharm. 53 (1) (2002) 1521.
[64] Y.N. Kalia, R.H. Guy, Interaction between penetration enhancers and iontophoresis:
effect on human skin impedance in vivo, J. Control. Release 44 (1) (1997) 3342.
[65] S.Y. Lin, K.J. Duan, T.C. Lin, Simultaneous determination of the protein conversion
process in porcine stratum corneum after pretreatment with skin enhancers by a
combined microscopic FT-IR/DSC system, Spectrochim. Acta A 52 (12) (1996)
16711678.
[66] F.P. Schmook, J.G. Meingassner, A. Billich, Comparison of human skin or epidermis
models with human and animal skin in in-vitro percutaneous absorption, Int. J.
Pharm. 215 (12) (2001) 5156.
[67] M.J. Bartek, J.A. LaBudde, H.I. Maibach, Skin permeability in vivo: comparison in
rat, rabbit, pig and man, J. Invest. Dermatol. 58 (3) (1972) 114123.
[68] E.M. Niazy, Differences in penetration-enhancing effect of Azone through excised
rabbit, rat, hailess mouse, guinea pig and human skins, Int. J. Pharm. 130 (1996)
225230.
[69] A. Ahad, M. Aqil, K. Kohli, Y. Sultana, M. Mujeeb, A. Ali, Role of novel terpenes in
transcutaneous permeation of valsartan: effectiveness and mechanism of action,
Drug Dev. Ind. Pharm. 37 (5) (2011) 583596.
[70] A. Ahad, M. Aqil, K. Kohli, Y. Sultana, M. Mujeeb, A. Ali, Interactions between novel
terpenes and main components of rat and human skin: mechanistic view
for transdermal delivery of propranolol hydrochloride, Curr. Drug Deliv. 8 (2)
(2011) 213224.
Anda mungkin juga menyukai
- Terpen EnhancerDokumen12 halamanTerpen Enhanceruntia_sariBelum ada peringkat
- Design Expert 7zxDokumen10 halamanDesign Expert 7zxuntia_sariBelum ada peringkat
- Rheumatoid AthritisDokumen43 halamanRheumatoid Athritisuntia_sariBelum ada peringkat
- Transdermal Drug Delivery System: A Review: The Pharma InnovationDokumen10 halamanTransdermal Drug Delivery System: A Review: The Pharma Innovationuntia_sariBelum ada peringkat
- Chitosan As Adhesive PDFDokumen15 halamanChitosan As Adhesive PDFuntia_sariBelum ada peringkat
- Colloids and Surfaces B: BiointerfacesDokumen7 halamanColloids and Surfaces B: Biointerfacesuntia_sariBelum ada peringkat
- Bio EnhancerDokumen8 halamanBio Enhanceruntia_sariBelum ada peringkat
- Jamu (Ginger and Kaempferia) PDFDokumen23 halamanJamu (Ginger and Kaempferia) PDFuntia_sariBelum ada peringkat
- Aloe Vera Crosslink CADokumen11 halamanAloe Vera Crosslink CAuntia_sariBelum ada peringkat
- PatchDokumen12 halamanPatchuntia_sariBelum ada peringkat
- PatchDokumen12 halamanPatchuntia_sariBelum ada peringkat
- PatchDokumen11 halamanPatchuntia_sariBelum ada peringkat
- Psygium Guajava For DismenorheaDokumen6 halamanPsygium Guajava For Dismenorheauntia_sariBelum ada peringkat
- Bio EnhancerDokumen8 halamanBio Enhanceruntia_sariBelum ada peringkat
- Prof Salman 12 Feb 2015Dokumen25 halamanProf Salman 12 Feb 2015untia_sariBelum ada peringkat
- Hydrogrel PatchDokumen11 halamanHydrogrel Patchuntia_sariBelum ada peringkat
- Review Article: Superdisintegrants: An OverviewDokumen5 halamanReview Article: Superdisintegrants: An OverviewferperezbrBelum ada peringkat
- Review Article: Superdisintegrants: An OverviewDokumen5 halamanReview Article: Superdisintegrants: An OverviewferperezbrBelum ada peringkat
- Patch Buccal PDFDokumen26 halamanPatch Buccal PDFuntia_sariBelum ada peringkat
- A Thiolase of Mycobacterium Tuberculosis Is Required For Virulence and Production of Androstenedione and Androstadienedione From Cholesterol PDFDokumen8 halamanA Thiolase of Mycobacterium Tuberculosis Is Required For Virulence and Production of Androstenedione and Androstadienedione From Cholesterol PDFuntia_sariBelum ada peringkat
- Review Article: Superdisintegrants: An OverviewDokumen5 halamanReview Article: Superdisintegrants: An OverviewferperezbrBelum ada peringkat
- Kul Bioprocess DevelopmentDokumen25 halamanKul Bioprocess Developmentuntia_sariBelum ada peringkat
- Kul Bioprocess DevelopmentDokumen25 halamanKul Bioprocess Developmentuntia_sariBelum ada peringkat
- Formulation and Evaluation of Transdermal Patches of Propranolol HydrochlorideDokumen7 halamanFormulation and Evaluation of Transdermal Patches of Propranolol HydrochlorideIOSR Journal of PharmacyBelum ada peringkat
- Psychoneuroimmunology: Stress Effects and Immunity During InfectionDokumen13 halamanPsychoneuroimmunology: Stress Effects and Immunity During Infectionuntia_sariBelum ada peringkat
- Odt BerberineDokumen9 halamanOdt Berberineuntia_sariBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5784)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (72)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Today's Topics: Procedures More Examples MARS Intro Number SystemsDokumen43 halamanToday's Topics: Procedures More Examples MARS Intro Number SystemsUlas GulerBelum ada peringkat
- DEVELOPMENT of Material ResourcesDokumen21 halamanDEVELOPMENT of Material ResourcesJennifer ManaogBelum ada peringkat
- PhlebotomyDokumen20 halamanPhlebotomyaguilarsuzette20Belum ada peringkat
- Data SheetDokumen6 halamanData SheetAshfaaq OchatoyaBelum ada peringkat
- L6 - (JLD 2.0) - Basic Mathematics - 5th MayDokumen64 halamanL6 - (JLD 2.0) - Basic Mathematics - 5th MayAyesha SinghBelum ada peringkat
- الإطار المفاهيمي للتنمية المستدامةDokumen16 halamanالإطار المفاهيمي للتنمية المستدامةboualemdzBelum ada peringkat
- Chapter 12: Media Access Control (MAC)Dokumen66 halamanChapter 12: Media Access Control (MAC)soumyaBelum ada peringkat
- The Analysis and Documentation FrameworkDokumen19 halamanThe Analysis and Documentation FrameworkDon XiaoBelum ada peringkat
- Historicizing Rappaport's Pigs For The AncestorsDokumen29 halamanHistoricizing Rappaport's Pigs For The AncestorsObservador20Belum ada peringkat
- M.A Chaudary Greenhall OL Physics NotesDokumen139 halamanM.A Chaudary Greenhall OL Physics NotesArshad KhanBelum ada peringkat
- Astero E0201E-20 991063Dokumen186 halamanAstero E0201E-20 991063Thinh Nguyen100% (1)
- STS PPT Chapter 1 7 PDFDokumen405 halamanSTS PPT Chapter 1 7 PDFearl beanscentBelum ada peringkat
- Course Outline: Return To Course IndexDokumen9 halamanCourse Outline: Return To Course Indexoswaldo58Belum ada peringkat
- Glister Company LTD: Management StructureDokumen6 halamanGlister Company LTD: Management StructureGirish P MehtaBelum ada peringkat
- Embryology QuestionDokumen19 halamanEmbryology QuestionVarun Arunagiri100% (17)
- Mavroidis, Petros C - Trade in Goods - The GATT and The Other Agreements Regulating Trade in GoodsDokumen541 halamanMavroidis, Petros C - Trade in Goods - The GATT and The Other Agreements Regulating Trade in GoodsDenny Bhatara100% (1)
- Guide Doing Business in Tanzania Digital 1Dokumen36 halamanGuide Doing Business in Tanzania Digital 1Yaula SiminyuBelum ada peringkat
- Flexible Cable Carriers and Protection Systems GuideDokumen146 halamanFlexible Cable Carriers and Protection Systems Guidebachir diengBelum ada peringkat
- Manifesto of Pakistan Awami Tehreek (PAT)Dokumen35 halamanManifesto of Pakistan Awami Tehreek (PAT)MinhajBooksBelum ada peringkat
- sjzl20092663-ZXDU68T301 (V4.1R01M01) Installation Manual PDFDokumen81 halamansjzl20092663-ZXDU68T301 (V4.1R01M01) Installation Manual PDFRamiz3zBelum ada peringkat
- Net Change JDEWorld A73 16Dokumen82 halamanNet Change JDEWorld A73 16Manoj LugunBelum ada peringkat
- Retail Banking: by Prof Santosh KumarDokumen30 halamanRetail Banking: by Prof Santosh KumarSuraj KumarBelum ada peringkat
- Aspectsofproductionspart1 1Dokumen41 halamanAspectsofproductionspart1 1Michelle Melody OlivarBelum ada peringkat
- Project Report On BSNLDokumen91 halamanProject Report On BSNLmanavBelum ada peringkat
- Type of ActuatorDokumen4 halamanType of Actuatorim4uim4uim4uim4uBelum ada peringkat
- Quantitative Analysis For Business Midterm - SolutionDokumen6 halamanQuantitative Analysis For Business Midterm - SolutionYiPingHungBelum ada peringkat
- COMDokumen17 halamanCOMmarcy ginez peña garciaBelum ada peringkat
- MDHA Write-Up For Prospective StudentsDokumen1 halamanMDHA Write-Up For Prospective StudentsprashantBelum ada peringkat
- Babok v3 Knowledge Area Summary v0.15 (DRAFT)Dokumen2 halamanBabok v3 Knowledge Area Summary v0.15 (DRAFT)vkcon100% (1)
- HarrodsDokumen2 halamanHarrodsCristina BobocBelum ada peringkat