Cytokine Response in Children Undergoing Surgery For Congenital Heart Disease
Diunggah oleh
Alessandro AlfieriJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Cytokine Response in Children Undergoing Surgery For Congenital Heart Disease
Diunggah oleh
Alessandro AlfieriHak Cipta:
Format Tersedia
Pediatr Cardiol (2006) 27:408413
DOI 10.1007/s00246-006-0934-y
Cytokine Response in Children Undergoing Surgery for
Congenital Heart Disease
Ashish B. Madhok Kaie Ojamaa Viraga Haridas
Vincent A. Parnell Savita Pahwa D. Chowdhury
Received: 26 October 2004 / Accepted: 20 July 2005
! Springer Science+Business Media, Inc. 2006
Abstract Pediatric cardiac surgery with cardiopulmonary
bypass (CPB) induces a complex inflammatory response
that may cause multiorgan dysfunction. The objective of
this study was to measure postoperative cytokine production and correlate the magnitude of this response with intraoperative variables and postoperative outcomes. Serum
samples from 20 children (median age, 15 months)
undergoing cardiac surgery with CPB were obtained preoperatively and on postoperative days (POD) 13. Serum
levels of interleukin (IL)-6, IL-8, and IL-10 increased
significantly on POD 1 (p < 0.01) vs pre-op values to 271
68, 44 9, 7.5 0.8 pg/ml, respectively, whereas serum
IL-1b, IL-12, and tumor neurosis factor -a were not significantly changed. The serum IL-6 and IL-8 levels correlated positively (p < 0.01) with the degree of postoperative
medical intervention as measured by the Therapeutic Interventional Scoring System and indicated a greater need
for inotropic support (p = 0.057). A negative correlation
(p < 0.01) between IL-6, IL-8, and mixed venous oxygen
A. B. Madhok K. Ojamaa D. Chowdhury (&)
Division of Pediatric Cardiology, Schneider Childrens Hospital,
269-01, 76th Avenue, New Hyde Park, NY 11040, USA
E-mail: dchowdhu@lij.edu
K. Ojamaa
The Feinstein Institute for Medical Research, 350 Community
Drive, Manhasset, NY 11030, USA
V. Haridas S. Pahwa
Division of Immunology, Schneider Childrens Hospital, 269-01,
76th Avenue, New Hyde Park, NY 11040, USA
V. A. Parnell
Division of Cardiothoracic Surgery, Schneider Childrens
Hospital, 269-01, 76th Avenue, New Hyde Park, NY 11040,
USA
123
saturation suggested compromised cardiopulmonary function. Patients with single ventricle anatomy had the highest
levels of IL-6 and IL-8 (629 131 and 70 17 pg/ml,
respectively), with a mean CPB time of 106 23 minutes.
Thus, the proinflammatory response after surgery with
CPB was associated with postoperative morbidity with
increased need for medical intervention.
Keywords Cytokines Interleukin Cardiopulmonary
bypass TISS Inotropes
Introduction
Pediatric patients who undergo heart surgery involving
cardiopulmonary bypass (CPB) are at risk of developing
inflammatory complications that can result in multisystem
organ dysfunction [5, 6, 7]. Several factors can trigger the
postoperative systemic inflammatory response including
surgical trauma, ischemiareperfusion injury, endotoxemia,
and activation of leukocytes by artificial surfaces, [20, 33].
This inflammatory process involves the activation of lymphocytes, monocytes/macrophages, endothelial cells, and
cardiac myocytes that can express and secrete many proinflammatory cytokines, including tumor necrosis factor
(TNF-a), interleukins (IL-1 , IL-6, and IL-8), as well as
antiinflammatory cytokines IL-4, IL-10, and transforming
growth factor (TGF-b) [14, 16, 17, 29, 34]. These biologically active factors have been implicated in the complications after cardiac surgery, including pulmonary
dysfunction, depressed cardiac contractile activity and impaired hypothalamicpituitarythyroid axis [911, 13, 26, 31].
Global myocardial ischemia followed by reperfusion
injury may result during surgery involving CPB with aortic
Pediatr Cardiol (2006) 27:408413
cross-clamping. Jansen and colleagues reported that TNF-a
could be detected after release of the aortic cross-clamp,
and that the duration of aortic cross-lamp was an independent predictor of postoperative serum TNF-a and IL-6
levels [21]. Furthermore, myocardial production and release of biologically active TNF-a and IL-8 may be involved in the postischemic myocardial depression or
stunning after CPB [4, 11, 22, 27, 34). Complement
activation and cytokine production have also been reported
in cardiac surgery performed without the aid of cardiopulmonary bypass [32].
The antiinflammatory cytokine IL-10 is also released
during CPB and has been shown to either directly inhibit
the release of proinflammatory cytokines [12, 14] or exert
antiinflammatory effects by triggering the release of IL-1
receptor antagonist and TNF soluble receptors 1 and 2 [25].
Several therapeutic strategies have been proposed that
aim to modulate the inflammatory response in this clinical
setting, including hemofiltration [2, 30], use of steroids and
nonsteroidal antiinflammatory agents [3, 15, 24], and
complement receptor blocking agents [8]. Ultrafiltration
procedures have been widely adopted and shown to be
effective in attenuating the inflammatory response, resulting
in improved postoperative hemodynamics, decreased
duration of mechanical ventilator support, and decreased
length of stay in intensive care unit [2, 30]. Treatment of
adults undergoing heart surgery with cardiopulmonary bypass with methylprednisolone has yielded promising results
showing reduced production of proinflammatory cytokines,
TNF-a, IL-6, and IL-8 and increased IL-10 [24, 32]. However, administration of steroids to pediatric patients undergoing CPB has not been shown to suppress the inflammatory
reaction, nor has it improved postoperative outcome measures [15]. Thus, novel therapeutic targets and approaches
are still necessary to minimize the systemic inflammatory
response in children undergoing cardiac surgery.
The objective of this study was to measure the cytokine
response in the postoperative period and correlate these
results with intraoperative variables and postoperative
outcomes.
Materials and Methods
The study protocol was approved by the institutes committee on human rights in research. Informed consent was
obtained from either parent(s) or guardian(s) before the
operation, and patients older than 7 years of age gave
consent. Twenty children of either gender younger than age
18 years who were subject to surgical correction of congenital heart defects with CPB were recruited into the
study. The median age, gender, and specific anatomic
defects of these patients are listed in Table 1.
409
Surgery and Anesthesia
Operations were performed by one cardiothoracic surgeon,
and conventional general anesthesia was used in all patients. Endotracheal intubation and placement of central
venous and arterial catheters were performed after
induction of anesthesia. Antibiotic prophylaxis was given at
the induction of anesthesia and at the end of the surgical
procedure. Heparinization was achieved with heparin sulfate, and its effect was reversed using protamine sulfate.
Aprotinin was administered to all patients, performed with
aortic and venous cannulation, membrane oxygenation, and
nonpulsatile flow. Similar techniques to maintain hematocrit and pH were used in all patients. If necessary at the end
of the surgical procedure intracardiac catheters (left and
right atria) were placed for postoperative care. Patients received standard care in the postoperative period in the
pediatric intensive care unit. Corticosteroids were not
administered.
Postoperative Management and Measures of Clinical
Outcome
Patients were continuously monitored in the intensive care
unit. Data on clinical outcomes, including quantities of
vasodilator and inotropic drugs, blood gas and lactate
analyses, urine output, blood pressures, cardiac rhythm,
and heart rates, were recorded daily. Mixed venous oxygen
saturation (MVSat) (%) of blood samples obtained from the
superior vena cava or pulmonary artery (when accessible)
was determined by standard blood gas analysis. The degree
of inotropic support required was calculated as described
by Wernovsky et al. [35]. The overall degree of postoperative care was analyzed by calculating the Therapeutic
Interventional Scoring System (TISS). TISS scores were
derived daily for 76 different therapeutic and monitoring
procedures and reflected the invasiveness, intensity, and
complexity of care rendered to the patient.
Cytokine Analysis
Blood samples for cytokine analysis were collected after
induction of anesthesia and before institution of CPB, and
on postoperative days (POD) 13. One milliliter of blood
was collected in a heparinized tube and the serum separated
by centrifugation (5000g for 10 minutes at 4"C) and stored
at )20"C until analyzed.
TNF-a and IL-1b, IL-12, IL-6, IL-8, and IL-10 were
measured by means of two commercially available kits, the
Human Th1/Th2 and Human Inflammatory Cytokine Bead
Array (BD Biosciences Pharmingen, San Jose, CA, USA).
The Cytokine Bead Array system generates data that are
comparable to enzyme-linked immunosorbant assays but in
123
410
a multiplexed or simultaneous fashion employing a
series of particles with discrete fluorescence intensities to
simultaneously detect multiple soluble analytes. The concentration of unknowns is calculated for the cytometric
bead array through the use of known standards and plotting
unknowns against a standard curve.
Pediatr Cardiol (2006) 27:408413
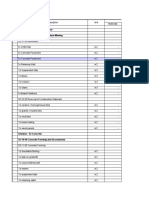
Table 1 Patient
parameters
characteristics
and
intra-
and
postoperative
Patients (n)
20
15 (0.1180)
Female (45%) Male (55%)
Results are expressed as median (ranges) or mean SE.
Analysis of the data at different time points was performed
using one-way repeated measures analysis of variance
(ANOVA) and pairwise multiple comparison procedures by
the HolmSidak method. Strength of association between
cytokines and clinical measures were assessed by Pearson
product moment correlation test. A p value < 0.05 was
considered significant. Data were analyzed using SigmaStat
statistical software, version 3.1 (Systat Software, Richmond, CA, USA).
Age (months)a
Gender
Anatomical defect (n)
Tetralogy of Fallot
Singled ventricle
Endocardial cushion defect
Ventricular septal defect
Transposition of the great arteries
Others (ASD, RHD, Ebsteins)
Intraoperative dataa
CPB time (minutes) (n = 20)
Cross-clamp time (minutes) (n = 18)
Postoperative outcomesa
Intensive care unit stay (days)
Mechanical ventilation (days)
Hospital stay (days)
TISS (cumulative POC 13)
Inotropic score (cumulative POD 13)
MVsat, % (POD 1)
Lactate, mmol/L (POD 1)
Results
ASD, atrial septal defect; RHD, rheumatic heart disease; POD,
postoperative day; TISS, Therapeutic Interventional Scoring System;
MVsat, mixed venous oxygen saturation
Statistical Analysis
5
4
4
2
2
3
91 (42212)
54 (22156)
5 (290)
2 (090)
8 (390)
125 (48188)
10.5 (063)
69 (3478)
2.1 (1.18.1)
Data are median (range)
Table 1 shows the types of congenital heart disease and the
number in each category. The median age was 15 months
(range 0.1180), with equal gender distribution. The mean
duration of CPB was 106 44 minutes (n = 20 patients),
and the mean aortic cross-clamp time was 69 40 minutes
(n = 18 patients). Postoperative outcome measures are
listed as median values and ranges. The TISS and inotropic
score for each patient represent the sum of the scores on
POD 13. MVsat (%) and blood lactate (mmol/L) levels are
those measured on POD 1.
Patients with single ventricle anatomy had the highest
serum IL-6 and IL-8 levels on POD 1, with mean SE values
of 629 131 and 70 17, respectively, and a mean CPB time
of 106 23 minutes. Six of eight cyanotic patients had
maximum serum IL-6 values > 100 pg/ml, whereas only 3 of
12 noncyanotic patients had these high values.
Table 2 summarizes the serum concentrations of TNF-a,
IL-1b, and IL-12 measured pre- and post-CBP. Although
serum TNF-a and IL-12 increased by POD2 these increases
did not reach statistical significance.
Inflammatory Response to CPB
Correlations of Clinical Outcomes with Cytokine
Responses
Figure 1 shows the serum levels of proinflammatory cytokines IL-6 and IL-8 and the inflammatory cytokine IL-10
following corrective heart surgery. Concentrations of all
three cytokines were significantly elevated on POD 1 compared to their preoperative values. POD 1 serum IL-6 and
IL-8 values were 271 68 and 44 9 pg/ml (mean SE),
respectively, compared with preoperative values of 46 12
and 16 2 pg/ml, respectively. All three cytokines declined
on POD 2 and 3 and were not significantly different from
their preoperative values. Serum IL-6 levels correlated
positively with IL-8, with a statistically significant (p <
0.001) correlation coefficient (r2) of 0.7742. Intraoperative
variables, including cardiopulmonary bypass time and aortic
cross-clamp time, did not significantly correlate with the
maximum postoperative serum IL-6 and IL-8 response (data
not shown).
123
The postoperative outcomes that were examined are listed
in Table 1. No significant correlation was found between
the maximum cytokine (IL-6, and IL-8 on POD 1) response
and total time in the intensive care unit, length of hospital
stay, and days of mechanical ventilation. However, serum
IL-8 concentrations on POD 1 correlated negatively with
MVsat, an indicator of decreased oxygen delivery to the
peripheral tissue, and positively with cumulative TISS
scores on POD 13. These correlations reached a level of
significance of p = 0.009, as shown in Fig. 2. Higher IL-8
levels also correlated with higher inotropic scores on POD
1 (p = 0.057), whereas no correlation was found with blood
lactate values (Table 3). Similar correlations were found
between the maximum serum IL-6 response and these
clinical outcome measures, as shown in Table 3.
Pediatr Cardiol (2006) 27:408413
411
Table 2 Cytokine response in the postoperative perioda
TNF-a (pg/ml)
Pre-CPB (n = 20)
POD 1 (n = 18)
POD 2 (n = 13)
POD 3 (n = 8)
1.9
1.6
3.4
1.1
2.1
1.6
5.9
1.4
IL-1b (pg/ml)
189
121
191
130
168
119
163
167
IL-12 (pg/ml)
106
89
157
86
142
124
189
160
Serum concentrations of TNF-a, IL-1b, and IL-12 taken pre- and
postsurgery (mean standard deviation). Values are not significantly
different among POD 13
POD, postoperative day
Fig. 1 Systemic inflammatory response after CPB. Serum concentrations of IL-6, IL-8, and IL-10 were measured preoperatively and on
postoperative day (POD) 13. Twenty patients underwent cardiopulmonary bypass surgery; n = 20 on pre- and POD 1, n = 13 on POD 2
and n = 8 on POD3. The horizontal line is the median value; the box
encompasses 25th to 75th percentiles, and caps represent 10 and 90%.
*p < 0.01 vs preoperative value; **p < 0.01 vs mean values at all
other time points. Statistical significance was determined by repeated
measures ANOVA with pairwise multiple comparison procedure
(HolmSidak method)
Discussion
In this study, we showed a significant positive correlation
between the magnitude of the inflammatory response as
measured by serum concentrations of IL-6 and IL-8 after
Fig. 2 Cytokine response correlates with postoperative outcomes. On
postoperative day (POD) 1, patient mixed venous oxygen saturation
(MVsat, %) values show significant negative correlation with serum
IL-8 levels (p < 0. 009). Cumulative TISS scores from POD 13
correlate significantly with serum IL-8 levels (p < 0.009). The line
represents the best fit linear regression curve. Significance of the
correlation coefficient was determined by ANOVA
CPB surgery and the degree of medical intervention
(TISS and inotropic score) of the pediatric patient in the
early postoperative period. Higher TISS scores with a
greater proinflammatory response reflected an increase in
postoperative management requirements. Similarly, the
need for inotropic support was greater in patients
with higher postoperative serurn IL-8 levels. MVsat was
3478% on POD 1, and these values correlated negatively
123
412
Pediatr Cardiol (2006) 27:408413
Table 3 Linear regression analysis between cytokine production and
postoperative outcomes
Postoperative outcome measurement
IL-8
r
pc
IL-6
r
pc
TISSa
Inotropic scoresa
MVbsat
Blood lactateb
0.610
0.009
0.470
0.057
)0.614
0.009
0.010
0.969
0.513
0.035
0.291
0.257
)0.575
0.016
0.084
0.748
TISS, Therapeutic Interventional Scoring System; MVsat, mixed
venous oxygen saturation
a
cumulative score for postoperative days 13
Value on postoperative day 1
determined by Pearson correlation test
with serum IL-8 concentrations, further supporting the
hypothesis that the magnitude of the inflammatory response has a direct effect on oxygen delivery to the
peripheral tissues and postoperative morbidity of the
pediatric patient. This inflammatory response was observed despite the routine use of modified ultrafiltration
procedures and aprotinin in our surgical practice to reduce
circulating cytokines and complement factors, and to increase hemoglobin, hematocrit, and platelet levels, as has
been reported by others [2, 18, 28, 30]. Our data support a
recent study showing significant correlations of postoperative serum IL-6 and IL-8 with increased inotropic
requirements and reduced arterial oxygen tension (PaO2)
2 hours after CPB [16]. In addition, these authors found
that the cytokine response correlated positively with
length of mechanical ventilation post-surgery which we
did not observe. In contrast to other studies [20], we did
not find a correlation between postoperative serum cytokines and the duration of CPB or aortic cross-clamp,
possibly due to the diverse nature of the surgical procedures. However, we did observe higher serum proinflammatory cytokines postoperatively in six of eight
cyanotic patients in whom the duration of CPB was > 90
minutes. Furthermore, all patients with single ventricle
anatomy had the highest levels of IL-6 and IL-8 (629
131 and 70 17 pg/ml, respectively), with a mean CPB
time of 106 23 minutes. One patient (with double
ventricle anatomy) with bronchomalacia had the highest
postoperative serum IL-6 and IL-8 concentrations (888
and 132 pg/ml, respectively), with a CPB time of 145
minutes and a complex postoperative course. Taken together, these data support the hypothesis that the duration
of CPB, the complexity of anatomical defect and surgical
repair, and the presence of cyanosis are contributing
factors to the postoperative inflammatory response.
123
Results from a recent study that tested the efficacy of
corticosteroid treatment to reduce the inflammatory response in pediatric cardiac surgery patients were negative,
with no effect on postoperative recovery [15]. Steroid
pretreatment remains controversial because steroids may
inhibit TNF-a, IL-6, and IL-8 production, thus preventing
peripheral vasodilatation, but they may also increase the
release of endotoxin [1, 3]. Thus, the search for novel
therapeutic targets is warranted in this clinical setting. The
identification of other mediators of inflammation, including
macrophage migration inhibitory factor and HMGB1 (high
mobility group box-1 protein), as well as a focus on pulmonary-derived cytokines may provide another strategy in
the treatment of postoperative inflammation in the heart
surgery patient [10, 23]. Since pulmonary injury and
multiorgan dysfunction remain significant complications
following cardiac surgery, continued efforts to identify the
mediators of these effects are required to potentially reduce
postoperative morbidity in the pediatric patient.
References
1. Andersen LW, Baek L, Thomsen BS, Rasmussen JP (1989) Effect of methylprednisone on endotoxemia and complement activation during cardiac surgery. J CardioThorac Anesth 3:544549
2. Berdat PA, Eichenberger E, Ebell J, et al. (2004) Elimination of
proinflammatory cytokines in pediatric cardiac surgery: analysis
of ultrafiltration method and filter type. J Thorac Cardiovasc Surg
127:16881696
3. Bourbon A, Vionnet M, Leprince P, et al. (2004) The effect of
methylprednisolone treatment on the cardiopulmonary bypassinduced systemic inflammatory response. Eur J Cardiothorac
Surg 26:932938
4. Burns SA, Newburger JW, Xiao M, et al. (1995) Induction of
interleukin-8 messenger RNA in heart and skeletal muscle during
pediatric cardiopulmonary bypass. Circulation 92(Suppl):315321
5. Butler J, Pathi VL, Paton RD, et al. (1996) Acute-phase responses
to cardiopulmonary bypass in children weighing less than 10
kilograms. Ann Thorac Surg 62:538542
6. Casey LC (1993) Role of cytokines in the pathogenesis of cardiopulmonary-induced multisystem organ failure. Ann Thorac Sura
56:S92S96
7. Casey WF, Hauser GJ, Hannallah RS, Midgley FM, Khan WN
(1992) Circulating endotoxin and tumor necrosis factor during
pediatric cardiac surgery. Crit Care Med 20:10901096
8. Chai PJ, Nassar R, Oakeley AE, et al. (2000) Soluble complement
receptor-1 protects heart, lung and cardiac myofilament function
from cardiopulmonary bypass damage. Circulation 101:541546
9. Chowdhury D, Ojamaa K, Parnell VA, et al. (2001) A prospective
randomized clinical study of thyroid hormone treatment after
operations for complex congenital heart disease. J Thorac Cardiovasc Surg 12:10231025
10. de Mendonca-Filho HT, Gomes RV, de Almeida Campos LA,
et al. (2004) Circulating levels of macrophage migration inhibitory factor are associated with mild pulmonary dysfunction after
cardiopulmonary bypass. Shock 22:533537
11. Finkel MS, Oddis CV, Jacob TD, et al. (1992) Negative inotropic
effects of cytokines on the heart mediated by nitric oxide. Science
257:387389
Pediatr Cardiol (2006) 27:408413
12. Fiorentino DF, Zlotnik A, Mosmann TR, Howard M, O Garra A
(1991) IL-10 inhibits cytokine prodution by activated macrophages, J Immunol 147:38153822
13. Gando S, Nishihira J, Kemmotsu O, et al. (2000) An increase in
macrophage migration inhibitory factor release in patients with
cardiopulmonary bypass surgery. Surg Today 30:689694
14. Gerard C, Bruyns C, Marchant A, et al. (1993) lnterleukin-10
reduces the release of tumor necrosis factor and prevents lethality
in experimental endotoxemia. J Exp Med 177:547550
15. Gessler P, Hohl V, Carrel T, et al. (2005) Administration of
steroids in pediatric cardiac surgery: impact on clinical outcome
and systemic inflammatory response. Pediatr Cardiol 26:595600
16. Gessler P, Pfenninger J, Pfammatter JP, et al. (2003) Plasma
levels of interleukin-8 and expression of interleukin-8 receptors
on circulating neutrophils and monocytes after cardiopulmonary
bypass in children. J.Thorac Cardiovasc Surg 126:718725
17. Gessler P, Pretre R, Hohl V, et al. (2004) CXC-chemokine
stimulation of neutrophils correlates with plasma levels of myeloperoxidase and lactoferrin and contributes to clinical outcome
after pediatric cardiac surgery. Shock 22:513520
18. Greilich PE, Brouse CF, Whittem CW, et al. (2003) Antifibrinolytic therapy during cardiopulmonary bypass reduces
proinflammatory cytokine levels: a randomized, double-blind,
placebo-controlled study of epsilon-aminocaproic acid and aprotinin. J Thorac Cardiovasc Surg 126:14981603
19. Hennein HA, Ebba H, Rodriguez JL, et al. (1994) Relationship of
the proinflammatory cytokines to myocardial ischemia and dysfunction after uncomplicated coronary revascularization. J Thorac Cardiovasc Surg 108:626635
20. Hirai S (2003) Systemic inflammatory response syndrome after
cardiac surgery under cardiopulmonary bypass. Ann Thorac
Cardiovasc Surg 9:365370
21. Jansen NJG, van Orveren W, van der Broek L, et al. (1991)
Inhibition by dexamethasone of the repefusion phenomena in
cardiopulmonary bypass. J Thorac Cardiovasc Surg 102:515525
22. Kapadia S, Lee J, Torre-Amine G, et al. (1995) Tumor necrosis
factor-a gene and protein expression in adult feline myocardium
after endotoxin administration. J Clin Invest 96:10421052
23. Lin X, Yang H, Sakuragi T, et al. (2005) Alpha-chemokine
receptor blockade reduces high mobility group box1 (HMGB1)
protein induced lung inflammation and injury and improves survival in sepsis. Am J Physiol Lung Cell Mol Physiol 289:583590
413
24. McBride WT, Allen S, Gormley SM, et al. (2004) Methylprednisolone favourably alters plasma and urinary cytokine homeostasis and subclinical renal injury at cardiac surgery. Cytokine
27:8189
25. McBride WT, Armstrong MA, Crockard AD, McMurray TJ, Rea
JM (1995) Cytokine balance and immunosuppresive changes at
cardiac surgery: contrasting response between patients and isolated CPB circuits. Br J Anaesth 75:724733
26. McMahon CK, Klein I, Ojamaa K (2003) lnterleukin-6 and thyroid hormone metabolism in pediatric cardiac surgery patients.
Thyroid 13:301304
27. Metinko AP, Kunkel SL, Standiford TJ, et al. (1992) Anoxia
hyperoxia induces monocyte-derived interleukin-8. J Clin Invest
90:791798
28. Millar AB, Armstrong L, van der Linden J, et al. (1993) Cytokine
production and hemofiltration in children undergoing cardiopulmonary bypass. Ann Thorac Surg 56:14991502
29. Qing M, Schumacher K, Heise R, et al. (2003) Intramyocardial
synthesis of pro- and anti-inflammatory cytokines in infants with
congenital cardiac defects. J Am Coll Cardiol 41:22662274
30. Sever K, Tansel T, Basaran M, et al. (2004) The benefits of
continuous ultrafiltration in pediatric cardiac surgery. Scand
Cardiovasc J 38:307311
31. Stayer SA, Diaz LK, East DL, et al. (2004) Changes in respiratory
mechanics among infants undergoing heart surgery. Anesth Analg J 98:4955
32. Tarnok A, Hambsch J, Emmrich F, et al. (1999) Complement
activation, cytokines, and adhesion molecules in children
undergoing cardiac surgery with or without cardiopulmonary
bypass. Pediatr Cardiol 20:113125
33. Varan B, Tokel K, Mercan S, Donmez A, Aslamaci S (2002)
Systemic inflammatory response related to cardiopulmonary bypass and its modification by methyl prednisolone; high dose
versus low dose. Pediatr cardiol 23:437441
34. Wan S, DeSmet JM, Barvais L, et al. (1996) Myocardium is a
major source of proinflammatory cytokines inpatients undergoing
cardiopulmonary bypass. J Thorac Cardiovasc Surg 112:806811
35. Wernovsky G, Wypij D, Jonas RA, et al. (1995) Postoperative
course and hemodynamic profile after the arterial switch operation in neonates and infants: a comparison of low-flow cardiopulmonary bypass and circulatory arrest. Circulation 92:2226
2235
123
Anda mungkin juga menyukai
- Cytokine Clearance With Cytosorb® During Cardiac Surgery: A Pilot Randomized Controlled TrialDokumen12 halamanCytokine Clearance With Cytosorb® During Cardiac Surgery: A Pilot Randomized Controlled Trialgra ndynBelum ada peringkat
- 2023_Mesenchymal Stem Cell Therapy in Acute Intracerebral Hemorrhage_ A Dose-Escalation Safety and Tolerability TrialDokumen11 halaman2023_Mesenchymal Stem Cell Therapy in Acute Intracerebral Hemorrhage_ A Dose-Escalation Safety and Tolerability TrialOlga Manco GuzmánBelum ada peringkat
- Accepted Manuscript: Journal of Cardiothoracic and Vascular AnesthesiaDokumen27 halamanAccepted Manuscript: Journal of Cardiothoracic and Vascular AnesthesiaRian AprizaBelum ada peringkat
- 2015 Article 1082Dokumen10 halaman2015 Article 1082atika sgrtBelum ada peringkat
- TransfusiDokumen10 halamanTransfusiDevia PebriyentiBelum ada peringkat
- Increase in Levels of BDNF Is Associated With InflammationDokumen8 halamanIncrease in Levels of BDNF Is Associated With InflammationVERONICA GUADALUPE PENNA NEAVESBelum ada peringkat
- 14 - Mazandarani2012Dokumen7 halaman14 - Mazandarani2012TandeanTommyNovenantoBelum ada peringkat
- Atwell 1998Dokumen6 halamanAtwell 1998cindyramadhanputri_4Belum ada peringkat
- cec y respuesta inflamatoriaDokumen11 halamancec y respuesta inflamatoriamaritzabericesBelum ada peringkat
- Impact of Intravenous Lidocaine On Myocardial InjuDokumen7 halamanImpact of Intravenous Lidocaine On Myocardial InjuRENAULTBelum ada peringkat
- Outcome With High Blood Lactate Levels During Cardiopulmonary Bypass in Adult Cardiac OperationDokumen5 halamanOutcome With High Blood Lactate Levels During Cardiopulmonary Bypass in Adult Cardiac OperationMuhammad RizqiBelum ada peringkat
- 18 - Heying2012Dokumen8 halaman18 - Heying2012TandeanTommyNovenantoBelum ada peringkat
- Clinical Characteristics and Treatment of Severe Encephalitis Associated With Neurogenic Pulmonary Edema Caused by Enterovirus 71 in ChinaDokumen6 halamanClinical Characteristics and Treatment of Severe Encephalitis Associated With Neurogenic Pulmonary Edema Caused by Enterovirus 71 in ChinanurulmaulidyahidayatBelum ada peringkat
- Recombinant Factor VII for Pediatric Cardiac Surgery BleedingDokumen7 halamanRecombinant Factor VII for Pediatric Cardiac Surgery BleedingYulii Di Bulan JulyBelum ada peringkat
- Journal 5Dokumen6 halamanJournal 5Claudia JessicaBelum ada peringkat
- ScribdDokumen8 halamanScribdMaria JuliaBelum ada peringkat
- Atherosclerosis 2007Dokumen8 halamanAtherosclerosis 2007Chalikias GeorgeBelum ada peringkat
- 20 - Doddakula2010Dokumen6 halaman20 - Doddakula2010TandeanTommyNovenantoBelum ada peringkat
- Isaksen 2019Dokumen8 halamanIsaksen 2019Filipe MendesBelum ada peringkat
- International Journal of Cardiology: Shou-Guo Zhao, Ji-Min Wang, Qian-Feng Han, Tai Li, Heng-Chen YaoDokumen2 halamanInternational Journal of Cardiology: Shou-Guo Zhao, Ji-Min Wang, Qian-Feng Han, Tai Li, Heng-Chen YaoMussaBelum ada peringkat
- E Cacy of Early Respiratory Physiotherapy and Mobilization After On-Pump Cardiac Surgery: A Prospective Randomized Controlled TrialDokumen15 halamanE Cacy of Early Respiratory Physiotherapy and Mobilization After On-Pump Cardiac Surgery: A Prospective Randomized Controlled TrialAsmaa GamalBelum ada peringkat
- VisionDokumen10 halamanVisionJoao LucasBelum ada peringkat
- Blood Conservation in Pediatric Cardiac SurgeryDokumen5 halamanBlood Conservation in Pediatric Cardiac Surgerymohanakrishna007Belum ada peringkat
- Inflammatory Cytokine Response in Patients With Septic Shock Secondary To Generalized PeritonitisDokumen9 halamanInflammatory Cytokine Response in Patients With Septic Shock Secondary To Generalized PeritonitisFerdian PriantoBelum ada peringkat
- 2a.330-Removal of Humoral Mediators and The Effect On The Survival of Septic Patients by Hemoperfusion With Neutral Microporous Resin ColumnDokumen7 halaman2a.330-Removal of Humoral Mediators and The Effect On The Survival of Septic Patients by Hemoperfusion With Neutral Microporous Resin Columngmejiar5237Belum ada peringkat
- Comparative Study Between Cardioprotective Effects of Intermitternt Antegrade Blood Cardioplegia With Terminal Warm Blood Reperfusion (Hot Shot) vs Intermittent Antegrade Blood Cardioplegia in PediatricDokumen18 halamanComparative Study Between Cardioprotective Effects of Intermitternt Antegrade Blood Cardioplegia With Terminal Warm Blood Reperfusion (Hot Shot) vs Intermittent Antegrade Blood Cardioplegia in PediatricalbadroeBelum ada peringkat
- Mca 25 510Dokumen6 halamanMca 25 510Delavemia RBelum ada peringkat
- Effects of Inspiratory Muscle Training Using An Electronic Device On Patients Undergoing Cardiac Surgery: A Randomized Controlled TrialDokumen9 halamanEffects of Inspiratory Muscle Training Using An Electronic Device On Patients Undergoing Cardiac Surgery: A Randomized Controlled TrialDaniel Lago BorgesBelum ada peringkat
- Nej Mo A 1401106Dokumen10 halamanNej Mo A 1401106Affan MsflBelum ada peringkat
- Knapik 2009Dokumen7 halamanKnapik 2009Dr XBelum ada peringkat
- HTTPSWWW Ncbi NLM Nih govpmcarticlesPMC5662220pdfpone 0187015 PDFDokumen19 halamanHTTPSWWW Ncbi NLM Nih govpmcarticlesPMC5662220pdfpone 0187015 PDFNawedAzamBelum ada peringkat
- Icvts Ivv355 FullDokumen7 halamanIcvts Ivv355 FullAldo AtjehBelum ada peringkat
- Research Article: Neutropenic Sepsis in The ICU: Outcome Predictors in A Two-Phase Model and Microbiology FindingsDokumen9 halamanResearch Article: Neutropenic Sepsis in The ICU: Outcome Predictors in A Two-Phase Model and Microbiology Findings28121998Belum ada peringkat
- Jurnal AnastesiDokumen7 halamanJurnal AnastesiStefania MarlinaBelum ada peringkat
- Prittie-2006-Journal of Veterinary Emergency and Critical CareDokumen11 halamanPrittie-2006-Journal of Veterinary Emergency and Critical Carejose fdoBelum ada peringkat
- CLN 66 01 107 PDFDokumen5 halamanCLN 66 01 107 PDFGloria KartikaBelum ada peringkat
- AvocadoDokumen16 halamanAvocadoKahinyaBelum ada peringkat
- Osteopathic Manipulative Therapy Induces Early Plasma Cytokine Release and Mobilization of A Population of Blood Dendritic CellsDokumen12 halamanOsteopathic Manipulative Therapy Induces Early Plasma Cytokine Release and Mobilization of A Population of Blood Dendritic CellsRafael MendietaBelum ada peringkat
- Song Zan 2019 Hypoalbuminemia A Novel Prognostic Factor ForDokumen9 halamanSong Zan 2019 Hypoalbuminemia A Novel Prognostic Factor ForRazan RabiBelum ada peringkat
- Obling Et Al-2023-Intensive Care MedicineDokumen12 halamanObling Et Al-2023-Intensive Care Medicinefatmaahmed3241Belum ada peringkat
- Effect of Early Physiotherapy On Intracranial PressureDokumen6 halamanEffect of Early Physiotherapy On Intracranial Pressurebendot29Belum ada peringkat
- Endocrinopathies in The ICU Patient Case FileDokumen2 halamanEndocrinopathies in The ICU Patient Case Filehttps://medical-phd.blogspot.comBelum ada peringkat
- Evaluation of Stress Hormones in Traumatic Brain Injury Patients With Gastrointestinal BleedingDokumen7 halamanEvaluation of Stress Hormones in Traumatic Brain Injury Patients With Gastrointestinal BleedingIvonne SoelionoBelum ada peringkat
- Prof Qaisar Khan TrialsDokumen56 halamanProf Qaisar Khan TrialsAsim NajamBelum ada peringkat
- Is Endocan a Marker for Pneumonia After SurgeryDokumen6 halamanIs Endocan a Marker for Pneumonia After SurgeryThomas HussonBelum ada peringkat
- Role of Ultrasonographic Inferior Venacaval Assessment in Surgeries Conducted Under General Anaesthesia-A Prospective Observational StudyDokumen6 halamanRole of Ultrasonographic Inferior Venacaval Assessment in Surgeries Conducted Under General Anaesthesia-A Prospective Observational StudyIJAR JOURNALBelum ada peringkat
- Anesthesia Considerations During Cytoreductive SurDokumen9 halamanAnesthesia Considerations During Cytoreductive Surdrardigustian2986Belum ada peringkat
- Circulation 2011 Kilgannon 2717 22Dokumen7 halamanCirculation 2011 Kilgannon 2717 22Na d'Nazaie CodeBelum ada peringkat
- Intraoperative-Inspiratory-Oxygen-Fraction-and.17Dokumen10 halamanIntraoperative-Inspiratory-Oxygen-Fraction-and.17AnarelysBelum ada peringkat
- Out 41Dokumen12 halamanOut 41natanatalisBelum ada peringkat
- 000380141Dokumen6 halaman000380141Just MahasiswaBelum ada peringkat
- Gastrointestinal Complications After Open Heart SurgeryDokumen7 halamanGastrointestinal Complications After Open Heart SurgerySarah Qurrotun AiniBelum ada peringkat
- Risk Factors For Intraoperative Massive Transfusion in Pediatric Liver Transplantation: A Multivariate AnalysisDokumen8 halamanRisk Factors For Intraoperative Massive Transfusion in Pediatric Liver Transplantation: A Multivariate AnalysisSanti ParambangBelum ada peringkat
- 001-Basic Surgical BackgroundDokumen101 halaman001-Basic Surgical BackgroundAhmed Zaghw100% (1)
- The Perioperative Complication Rate of Orthopedic PDFDokumen10 halamanThe Perioperative Complication Rate of Orthopedic PDFAnh Nguyen HuuBelum ada peringkat
- 1123 Insulin ProtocolDokumen7 halaman1123 Insulin ProtocolrosyadBelum ada peringkat
- Liu2009 Article SerumInterleukin-6AndInterleukDokumen9 halamanLiu2009 Article SerumInterleukin-6AndInterleukOkky IrawanBelum ada peringkat
- Dual Antiplatelet Therapy for Coronary and Peripheral Arterial DiseaseDari EverandDual Antiplatelet Therapy for Coronary and Peripheral Arterial DiseaseSorin BrenerBelum ada peringkat
- 10 12968@jowc 2019 28 10 658 PDFDokumen8 halaman10 12968@jowc 2019 28 10 658 PDFAlessandro AlfieriBelum ada peringkat
- HPV Indonesia PDFDokumen74 halamanHPV Indonesia PDFalessandro alfieriBelum ada peringkat
- Hiv Care SupportDokumen48 halamanHiv Care SupportAlessandro AlfieriBelum ada peringkat
- TDR: Health Research That Makes An Impact: For Research On Diseases of PovertyDokumen20 halamanTDR: Health Research That Makes An Impact: For Research On Diseases of PovertyAlessandro AlfieriBelum ada peringkat
- E90840Dokumen501 halamanE90840Raju NiraulaBelum ada peringkat
- Corneal Topography For Computerized Contact Lens FittingDokumen2 halamanCorneal Topography For Computerized Contact Lens FittingAlessandro AlfieriBelum ada peringkat
- Glaucoma UpdateDokumen1 halamanGlaucoma UpdateAlessandro AlfieriBelum ada peringkat
- ESC Guidelines on Dual Antiplatelet Therapy in Coronary Artery DiseaseDokumen48 halamanESC Guidelines on Dual Antiplatelet Therapy in Coronary Artery DiseaseAdriana VasilicaBelum ada peringkat
- Understanding Back Pain: I. M. Doctor, M.DDokumen52 halamanUnderstanding Back Pain: I. M. Doctor, M.DAlessandro Alfieri100% (1)
- The SCOPH ManualDokumen107 halamanThe SCOPH Manualapi-26041148Belum ada peringkat
- A Glial Derived Protein, S100B, in Neonates And.18Dokumen4 halamanA Glial Derived Protein, S100B, in Neonates And.18Alessandro AlfieriBelum ada peringkat
- Kangaroo - Mother - Care050508 PDFDokumen15 halamanKangaroo - Mother - Care050508 PDFAlessandro AlfieriBelum ada peringkat
- Hemofiltration During Cardiopulmonary Bypass In.11Dokumen9 halamanHemofiltration During Cardiopulmonary Bypass In.11Alessandro AlfieriBelum ada peringkat
- Acquired Mitochondria Optic NeuropathyDokumen11 halamanAcquired Mitochondria Optic NeuropathyAlessandro AlfieriBelum ada peringkat
- Cardio Pulmonary Resuscitation 2010: Djayanti SariDokumen26 halamanCardio Pulmonary Resuscitation 2010: Djayanti SariAlessandro AlfieriBelum ada peringkat
- AirwayDokumen31 halamanAirwayAlessandro AlfieriBelum ada peringkat
- Protokol Apnea AiimsDokumen16 halamanProtokol Apnea AiimsAlessandro AlfieriBelum ada peringkat
- Medication Calculation Examination Study Guide: IV CalculationsDokumen2 halamanMedication Calculation Examination Study Guide: IV Calculationswaqas_xsBelum ada peringkat
- LESSON 9 Steam Generators 2Dokumen12 halamanLESSON 9 Steam Generators 2Salt PapiBelum ada peringkat
- A Report On Kantajew MandirDokumen21 halamanA Report On Kantajew MandirMariam Nazia 1831388030Belum ada peringkat
- Rustom Shams PDFDokumen48 halamanRustom Shams PDFmtaha85Belum ada peringkat
- 9284 - Technical Instruction Addenum 3 Corrigendum 2Dokumen5 halaman9284 - Technical Instruction Addenum 3 Corrigendum 2Bambang HerimantoBelum ada peringkat
- SocorexDokumen6 halamanSocorexTedosBelum ada peringkat
- Mercury Poisoning Symptoms and TreatmentsDokumen1 halamanMercury Poisoning Symptoms and TreatmentsRakheeb BashaBelum ada peringkat
- Xt600e 3tb-3uw 90-95Dokumen46 halamanXt600e 3tb-3uw 90-95Kenneth SynnesBelum ada peringkat
- Unit Rates and Cost Per ItemDokumen213 halamanUnit Rates and Cost Per ItemDesiree Vera GrauelBelum ada peringkat
- Tugas Bahasa Inggris Analytical Exposition Text: Disusun Oleh: Nama:Hansel Hendrawan Effendy Kelas:XI IPA 1Dokumen4 halamanTugas Bahasa Inggris Analytical Exposition Text: Disusun Oleh: Nama:Hansel Hendrawan Effendy Kelas:XI IPA 1Hansel HendrawanBelum ada peringkat
- Unit 2 Water Treatment Ce3303Dokumen18 halamanUnit 2 Water Treatment Ce3303shivaBelum ada peringkat
- 02 1 Cohen Sutherland PDFDokumen3 halaman02 1 Cohen Sutherland PDFSarra AnitaBelum ada peringkat
- MCQs on PharmacologyDokumen101 halamanMCQs on PharmacologyMohammad Rashid88% (8)
- bk978 1 6817 4068 3ch1Dokumen28 halamanbk978 1 6817 4068 3ch1fysmaBelum ada peringkat
- The Beggar's Opera by Gay, John, 1685-1732Dokumen50 halamanThe Beggar's Opera by Gay, John, 1685-1732Gutenberg.orgBelum ada peringkat
- PathFit 1 (Lessons)Dokumen10 halamanPathFit 1 (Lessons)Patawaran, Myka R.Belum ada peringkat
- Desk PiDokumen21 halamanDesk PiThan LwinBelum ada peringkat
- Curriculam VitaeDokumen3 halamanCurriculam Vitaeharsha ShendeBelum ada peringkat
- If Sentences Type 1 First Type Conditionals Grammar Drills - 119169Dokumen2 halamanIf Sentences Type 1 First Type Conditionals Grammar Drills - 119169Ivanciu DanBelum ada peringkat
- Red Lion Edict-97 - Manual PDFDokumen282 halamanRed Lion Edict-97 - Manual PDFnaminalatrukBelum ada peringkat
- Sand Compaction MethodDokumen124 halamanSand Compaction Methodisaych33ze100% (1)
- Assessmentof Safety Cultureand Maturityin Mining Environments Caseof Njuli QuarryDokumen12 halamanAssessmentof Safety Cultureand Maturityin Mining Environments Caseof Njuli QuarryAbdurrohman AabBelum ada peringkat
- Danbury BrochureDokumen24 halamanDanbury BrochureQuique MartinBelum ada peringkat
- ForwardMails PDFDokumen7 halamanForwardMails PDFJesús Ramón Romero EusebioBelum ada peringkat
- Ap4955 PDFDokumen4 halamanAp4955 PDFGilvan HenriqueBelum ada peringkat
- EBSD Specimen Prep PaperDokumen36 halamanEBSD Specimen Prep PaperPaul RosiahBelum ada peringkat
- A New Aftercooler Is Used On Certain C9 Marine Engines (1063)Dokumen3 halamanA New Aftercooler Is Used On Certain C9 Marine Engines (1063)TASHKEELBelum ada peringkat
- Document 25Dokumen455 halamanDocument 25Pcnhs SalBelum ada peringkat
- School of Education, Arts and Sciences General Education Area 1 SEMESTER S.Y 2021-2022Dokumen4 halamanSchool of Education, Arts and Sciences General Education Area 1 SEMESTER S.Y 2021-2022JaylordPalattaoBelum ada peringkat
- Sato Printer Api Reference DocumentDokumen34 halamanSato Printer Api Reference Documentsupersteel.krwBelum ada peringkat