4 - GAther Source BIO
Diunggah oleh
ashrafalmiHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
4 - GAther Source BIO
Diunggah oleh
ashrafalmiHak Cipta:
Format Tersedia
1.
1: HUMAN RESPIRATORY SYSTEM
The human respiratory system consists of the nose, trachea, bronchi & a pair
of lungs.
The air passage during inhalation:
Nose trachea
Bronchus Bronchiole
Alveolus
Air inhaled through the nose or the mouth cavity.
The nostrils open into a nasal cavity with many olfactory hairs.
The olfactory hairs filter & prevent dust particles from entering the lungs.
The wall of the nasal cavity is lined with mucus membranes that keeps it moist
& helps to trap the dust.
The nasal cavity is connected to the trachea.
The trachea connects the larynx with two bronchi that lead into the lungs.
The lung is a soft spongy organ with a network of air sacs.
In each of the lungs, the bronchus divides into tiny ducts called bronchioles.
Each bronchioles ends in an air sac known as an alveolus.
Gas exchange takes place in the alveolus
O2 from the inhaled air diffuses through the thin wall of the alveolus into the
blood capillary
blood plasma.
In the plasma, O2 diffuse into the red blood cells & combines with Hb to form
oxyhaemoglobin.
At the same time, CO2 & water molecules from the blood capillary diffuse into
the alveolus.
The CO2 & water (in the form of vapour) is expelled from the body during
exhalation.
Mechanism of Ventilation
Breathing occurs in 2 stages:
Inspiration/inhalation is the process in
which air is actively inhaled into the
lungs.
Expiration/exhalation is the process in which air is exhaled from the
lungs.
Adaptations for gaseous exchange in the lungs.
The alveoli provide a large surface area for gaseous exchange. The
respiratory surface of a human is made-up of over 700 million alveoli, inside a
pair of lungs.
The surfaces of the alveoli are moist for gases to dissolve before diffusion
can occur.
The alveoli have thin walls (one cell thick) which minimize the distance for
gas diffusion.
The walls are permeable to diffusion of O2 & CO2.
The alveoli are surrounded by numerous blood capillaries, which bring CO2
for diffusion into the alveoli & carry away O 2 to the circulatory blood system.
Structure of Hb & the transport of O2
Hb is a respiratory pigment, which is found in the red blood cells to assist in
the transport of O2.
Hb is a conjugated protein with a quaternary structure. It consists of 4
p/peptide chains, 2- & 2- chains, that coil closely together to form a nearly
spherical structure.
Each p/peptide chain contains a haem group.
One Hb molecule can bind loosely & reversibly with 4 molecules of O 2 to form
oxyhaemoglobin molecule.
Hb + 4O2
Hb (O2)4
Each red blood cell contain about 250 x 10 6 molecules of Hb.
Because each Hb molecule consists of 4 haem groups, each red blood cell of
mammal can transport a total of about 1000 x 10 6 O2 molecules.
The high capacity of red blood cells in transporting O 2 molecules is due to the
fact that the red blood cells do not contain nuclei & the surface area to volume
ratio of the biconcave disc shaped cells is extremely high.
The high efficiency of the Hb in absorbing O 2 can be explained as
follows:
1. Hb & O2 can be easily bonded even at low O 2 concentrations. Therefore,
blood can be saturated with O2 immediately once in contact with water & air.
2. The O2 content in red blood cells is much higher than the content in the
plasma.
3. Despite having a high affinity for O2, Hb can also release O2 quite easily
when there is a drop in partial O2 pressure. Low partial O2 pressure occurs
frequently in inner tissues of the body.
Oxygen Dissociation Curves
O2 dissociation curves show the relationship between the degree of Hb
saturation with O2 at different values of partial pressure of O2.
When the PO2 is high as in the lung capillaries, Hb has a high affinity for O 2 to
form Hb(O2)4.
When the PO2 is low as in the respiring tissues, the Hb(O 2)4 dissociates & O2
is liberated.
The sigmoid shape of the O2 dissociation curve shows that blood can be
saturated with O2 even at a very low PO2.This is what is meant by the high
affinity pf Hb for O2.
The sigmoid shape of the O 2 dissociation curve also shows that the
percentage of O2 saturation in Hb declines steeply as the O2 pressure falls.
The Hb responds by releasing more O 2 as shown by the steep curve at the
lower level of PO2 as in respiring tissues.
The O2 dissociation curve for Hb is different under different condition of
CO2 pressure as in respiring tissues.
Increase in CO2 pressure will shift the O2 dissociation curve to the right.
This effect is known as Bohrs effect.
This means that as the CO2 pressure increases, the rate of O2 combination
with Hb decreases, or the dissociation of O 2 from oxyhemoglobin is more
efficient.
Therefore, the rate of O 2 dissociate from Hb(O2)4 is higher in the tissues that
contain higher CO2 pressure due to respiration.
Conversely, the rate of O2 combination with Hb is higher in the lungs that
contain lower CO2 pressure due to release of CO2 to the atmosphere.
O2 dissociation curve of Hb & myoglobin in comparison
Myoglobin acts as O2 store in the muscles.
Myoglobin is a protein conjugate having chemical similarities to Hb.
Compared to Hb, myoglobin shows a higher affinity towards O 2 & becomes
easily saturated even at very low O2 concentration.
Its O2 dissociation curve is displaced well to the left of Hb.
It only begins to release O2 when the partial pressure of O2 is below 20mmHg.
In this way, it acts as a store of O 2 in resting muscle, only releasing it when
supplies of HbO2 have been exhausted. (e.g; strenuous exercise)
O2 Dissociation Curves of Hb in Fetus & Mother.
The fetus has a very high O2 demand.
The fetal Hb is one of a type which has a higher affinity for O 2 than the
mothers Hb. O2 is therefore readily unloaded from the mothers blood to the
fetal blood.
A graph for fetal Hb shows a shift to the left from curve for adult Hb.
CO2 TRANSPORT IN BLOOD
CO2 is transported in the blood in 3 ways;
1. In aqueous solution (5%)
About 5% of the CO2 does not diffuse into the red blood cells, but dissolves
into the plasma & becomes carbonic acid, H 2CO3, and carried as such in the
blood.
2. Combined with protein (10-20%)
CO2 can combine with the amino group at one end of the
haemoglobin p/peptide to form a neutral carbamino-haemoglobin
compound.
The amount of CO2 that is able to combine with Hb depends on the
amount of O2 already being carried by
the Hb.
The less the amount of O2 being carried by the Hb molecule, the more
CO2 that can be carried by the Hb.
3. As Hydrogen carbonate (85%)
CO2 produced by the tissue diffuses passively into the bloodstream &
passes into the erythrocytes where it combines with water to form
carbonic acid.
The reaction is catalysed by carbonic anhydrase.
The carbonic acid quickly dissociates into a hydrogen ion (H +) & a
hydrogencarbonate ion (HCO3-).
H2CO3
H+ + HCO3-
The hydrogen carbonate ions (HCO 3-) diffuse out of the erythrocyte into the
plasma .
The erythrocyte membrane is relatively impermeable to cations such as Na + &
K+ .
To maintain electrical neutrality, the chloride ions (Cl -) diffuse into the
erythrocyte to balance the hydrogen carbonate ions diffusing out.
The process is called a chloride shift.
The concentration of H+ in the cell increases, pH decreases. The Hb(O 2)4
dissociates & O2 released to the cell for cellular respiration.
The Hb acts as a buffer combines with H+ to form haemoglobinic acid (HHb).
Exchange of gases between air in the alveolar space & blood in the
pulmonary capillaries.
1.2: Control of Breathing/Respiration
The control is involuntary & involves negative feedback mechanisms.
The breathing rate is controlled involuntary by respiratory center, which is
located in the medulla of the brain.
The respiratory center is divided into;
i)
Inspiratory center control inspiration & found at the ventral
ii)
part of the respiratory center.
Expiratory center controls expiration & found at the dorsal &
lateral parts of the respiratory center.
Chemoreceptors are receptor cells that can be stimulated by chemicals
including H+ concentration caused by CO2.
These chemoreceptors are stimulated by
increase in [H+] (low pH) & they can produce impulse that is sent to the
respiratory center in the brain by sensory nerve.
There are 2 types of chemoreseptors that detect [H +];
i. The Peripheral Chemoreceptors, the carotid & aortic bodies, found on
the carotid arteries & aorta, are stimulated by the high concentration of
CO2 & H+.
Nerve impulses are sent from the peripheral chemoreceptors to
the respiratory center.
ii. The central chemoreceptors in the medulla are sensitive to H + & not CO2
concentration.
As arterial [CO2] increases some of the molecules diffuse into
the cerebrospinal fluid surrounding the medulla.
This results in a corresponding increase in [H +] & decrease in
pH.
CO2 + H2O
H2CO3
H+ + HCO3-
The central chemoreceptors in the medulla are stimulated by H +.
Impulse are then sent to the respiratory center.
The sequence of events that occurs in the process of involuntary controlled
breathing:
1. CO2 from respiration is detected by chemoreceptor & the impulses generated
are sent to the respiratory center that controls the rate of breathing.
2. From the respiratory center impulses is sent to the diaphragm & external intercostal muscle respectively.
3. Both muscles contract, resulting an expansion of thoracic cavity, which
causes the lung to inflate, inspiration occurs.
4. When the lung expand, stretch receptors within the walls of alveoli &
bronchioles are stimulated.
5. Inhibitory impulses are sent to inspiratory center, which cut off inspiratory
activity.
6. Such action results in the relaxation of the respiratory muscles.
7. The thoracic cavity contracts deflating the lungs & resulting in expiration.
8. The walls of the alveoli & bronchiole contract & no inhibitory impulse is sent to
the respiratory center. The cycle can begin again.
Voluntary (conscious) control
Breathing can be altered voluntarily to a limited extent by the higher centers in
the cerebral hemispheres to permit activities like singing, talking & holding the
breath for a short while.
1.3:GASES EXCHANGE IN PLANTS
Stoma- structure & Functions
Gaseous exchange in plants occurs mainly through pores called stomata.
They are found on the epidermis of leaves & stems of flowering plants.
Lenticels found in the bark of stem & root hairs with thin walls & large surface
area also allow gaseous exchange to take place.
Each stoma consist of a stomatal pore surrounded by two guard cells.
Each guard cell is kidney-shapes & contains chloroplasts.
It has a thinner outer wall & a thicker, less elastic, inner wall.
Changes in turgor pressure of guard cells causes the opening or closing of
the stomatal pore.
The stomatal pore allows exchange of CO 2 & O2 for photosynthesis &
respiration & control water loss to the surroundings.
Mechanism of opening & closing
Stomata open & close because of changes in turgor pressure of their guard
cells.
Stomata opens when the guard cells become turgid.
When the cells swell with water, the thin outer walls bulge out & force the
inner walls into a crescent shape.
As a result the guard cells buckle & the stoma opens.
Stoma closes when the guard cells become flaccid.
This is because when water leaves the guard cells, there is no turgor
pressure, causing the leaf to wilt & the guard cells to close.
Turgid Guard Cells
Flaccid Guard Cells
Hypothesis of opening & closing
1. CO2 concentration in the leaf
When there is light, photosynthesis takes place & CO2 is used.
The pH of the guard cell is increase.
This causes the enzyme amylase to change starch to sugar, lowering
of the water potential & the stoma opens.
At night, the process is reversed as accumulation of CO2 by
respiration lowers the pH.
Sugar is changed to starch by the amylase & the starch does not
affect the water potential.
2. Photosynthesis in the guard cells & the accumulation of sugar
When there is light, photosynthesis takes place in the chloroplasts of
the guard cells resulting an accumulation of sugar in the guard cells.
The sugar reduces the water potential of the guard cells & water moves
in from neighbouring cells by osmosis, the guard cells become turgid &
the stoma open.
The water potential of the guard cells reverses & the stoma closes.
At night, there is no photosynthesis, therefore no sugar production
[sugar ] in guard cells.
3. Potassium ion Hypothesis
When there is light, especially blue light, it stimulates the proton pump in the
membrane of the guard cells. This causes a fast accumulation of H + in the
cells.
This in turn causes the opening of K+ channel & a fast uptake of K+ ions.
An increase in K+ concentration lowers the water potential that causes the
water to diffuse in by osmosis, increasing the turgor pressure & the stoma
opens.
In some species, Cl- accompanies the K+ in and out of the guard cells, thus
maintaining electrical neutrality.
At night, the reverse process take place when there is no light. K + diffuses
out, water also leaves.
The guard cells lose turgor, & the stomata close.
Anda mungkin juga menyukai
- Chapter 1 - Cell As A Basic Unit of Life - Part 1Dokumen27 halamanChapter 1 - Cell As A Basic Unit of Life - Part 1ashrafalmiBelum ada peringkat
- Daily Lesson Plan English KSSR Year 4Dokumen4 halamanDaily Lesson Plan English KSSR Year 4ashrafalmi100% (2)
- Daily Lesson Plan KSSR Year 4 2014 (Grammar)Dokumen4 halamanDaily Lesson Plan KSSR Year 4 2014 (Grammar)ashrafalmi100% (3)
- The FriendshipDokumen1 halamanThe FriendshipashrafalmiBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- A-Z Survival Items Post SHTFDokumen28 halamanA-Z Survival Items Post SHTFekott100% (1)
- Module 17 Building and Enhancing New Literacies Across The Curriculum BADARANDokumen10 halamanModule 17 Building and Enhancing New Literacies Across The Curriculum BADARANLance AustriaBelum ada peringkat
- Refrigerador de Vacunas Vesfrost MKF 074Dokumen5 halamanRefrigerador de Vacunas Vesfrost MKF 074Brevas CuchoBelum ada peringkat
- Invenio Flyer enDokumen2 halamanInvenio Flyer enErcx Hijo de AlgoBelum ada peringkat
- Dreizler EDokumen265 halamanDreizler ERobis OliveiraBelum ada peringkat
- HAI ROBOTICS Introduction ENV2022.0829 MarketingDokumen40 halamanHAI ROBOTICS Introduction ENV2022.0829 MarketingKit WooBelum ada peringkat
- How Do I Predict Event Timing Saturn Nakshatra PDFDokumen5 halamanHow Do I Predict Event Timing Saturn Nakshatra PDFpiyushBelum ada peringkat
- SOLVING THE STEADY STATE SOLVER AND UNSTEADY or TRANSIENT SOLVER 2D HEAT CONDUCTION PROBLEM BY USINGDokumen3 halamanSOLVING THE STEADY STATE SOLVER AND UNSTEADY or TRANSIENT SOLVER 2D HEAT CONDUCTION PROBLEM BY USINGGodwin LarryBelum ada peringkat
- D&D 3.5 Edition - Fiendish Codex I - Hordes of The Abyss PDFDokumen191 halamanD&D 3.5 Edition - Fiendish Codex I - Hordes of The Abyss PDFIgnacio Peralta93% (15)
- Define Variable and ConstantDokumen17 halamanDefine Variable and ConstantSenthil MuruganBelum ada peringkat
- LCP-027 VectraLCPDesignGuideTG AM 0613Dokumen80 halamanLCP-027 VectraLCPDesignGuideTG AM 0613Evert100% (1)
- 3 HVDC Converter Control PDFDokumen78 halaman3 HVDC Converter Control PDFJanaki BonigalaBelum ada peringkat
- 7 Ways To Support Your Babys Learning Today Monti KidsDokumen19 halaman7 Ways To Support Your Babys Learning Today Monti KidsMareim A HachiBelum ada peringkat
- First Aid Transportation of The InjuredDokumen30 halamanFirst Aid Transportation of The InjuredMuhammad Naveed Akhtar100% (1)
- A List of 142 Adjectives To Learn For Success in The TOEFLDokumen4 halamanA List of 142 Adjectives To Learn For Success in The TOEFLchintyaBelum ada peringkat
- 4.9 Design of Compression Members: L 4.7 UsingDokumen22 halaman4.9 Design of Compression Members: L 4.7 Usingctc1212100% (1)
- Sample Paper Book StandardDokumen24 halamanSample Paper Book StandardArpana GuptaBelum ada peringkat
- Project Report On HeritageDokumen39 halamanProject Report On HeritageBALA YOGESH YANDAMURIBelum ada peringkat
- Lab Activity 5Dokumen5 halamanLab Activity 5Jasmin CeciliaBelum ada peringkat
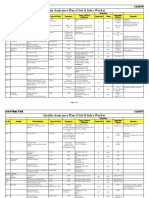
- Quality Assurance Plan - CivilDokumen11 halamanQuality Assurance Plan - CivilDeviPrasadNathBelum ada peringkat
- Mythology GreekDokumen8 halamanMythology GreekJeff RamosBelum ada peringkat
- Standalone Financial Results, Limited Review Report For December 31, 2016 (Result)Dokumen4 halamanStandalone Financial Results, Limited Review Report For December 31, 2016 (Result)Shyam SunderBelum ada peringkat
- Corporate Members List Iei Mysore Local CentreDokumen296 halamanCorporate Members List Iei Mysore Local CentreNagarjun GowdaBelum ada peringkat
- Quadratic SDokumen20 halamanQuadratic SAnubastBelum ada peringkat
- Clock of Destiny Book-1Dokumen46 halamanClock of Destiny Book-1Bass Mcm87% (15)
- INDUSTRIAL PHD POSITION - Sensor Fusion Enabled Indoor PositioningDokumen8 halamanINDUSTRIAL PHD POSITION - Sensor Fusion Enabled Indoor Positioningzeeshan ahmedBelum ada peringkat
- Yuzu InstallerDokumen3 halamanYuzu InstallerJohnnel PrietosBelum ada peringkat
- AnkitKumar InternshalaResume PDFDokumen2 halamanAnkitKumar InternshalaResume PDFkusha010Belum ada peringkat
- 1.12 Properties of The Ism - FlexibilityDokumen4 halaman1.12 Properties of The Ism - FlexibilityyomnahelmyBelum ada peringkat
- Mastering American EnglishDokumen120 halamanMastering American Englishmarharnwe80% (10)