Far Eastern University
Diunggah oleh
Marvin UrgeDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Far Eastern University
Diunggah oleh
Marvin UrgeHak Cipta:
Format Tersedia
FAR EASTERN UNIVERSITY
Institute of Nursing
School Year 2009-2010
Marvin Nikko C. Urge 2007763651
BSN 135 – 139
I. CLINICAL QUESTION
Among women in labor, is antenatal oral dexamethasone as efficacious and safe as
intramuscular dexamethasone for reducing neonatal respiratory distress syndrome?
II. CITATION
Title: Antenatal Oral Dexamethasone for Neonatal Respiratory Distress Syndrome Increased
Neonatal Morbidity
Authors: Egerman Rs, Mercer Bm, Doss Jl, et al. A Randomized, Controlled Trial of Oral
and Intramuscular Dexamethasone in the Prevention of Neonatal Respiratory Distress
Syndrome. Am J Obstet Gynecol 1998 Nov; 179:1120–3
III.STUDY CHARACTERISTICS
Patients included
170 women who were 24–33 weeks gestation and had preterm labour, preterm rupture
of membranes, or a medical indication for delivery. Women were excluded if they had
previously received corticosteroids during the pregnancy, had received anticonvulsant
treatment or rifampin, had an infection other than cystitis or cervicitis, had advanced cervical
dilation ( 5 cm), or had known fetal pulmonary maturity through amniocentesis or vaginal
pool sampling. 5 women were unavailable for follow up.
Interventions Compared
oral dexamethasone vs. intramuscular dexamethasone
Outcomes monitored
Main outcome was neonatal respiratory distress syndrome, diagnosed in infants with an
oxygen requirement of >40% and symptoms of respiratory distress syndrome, confirmed by chest
radiography. Secondary outcomes were sepsis, intraventricular hemorrhage, necrotising
enterocolitis, and neonatal death.
Does the study focus on the significant problem?
Yes, the study focused on determining the better intervention for reducing neonatal
respiratory distress syndrome by comparing the effectiveness of both oral and intramuscular
dexamethasone.
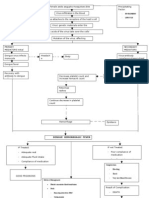
IV. METHODOLOGY/DESIGN
Methodology Used
Design
The design is a randomized controlled trial.
Setting
The location of testing done was in the United States of America.
Data Sources
Data sources were primary data. From the testing done in the experiment, data were
gathered. And guidelines were taken from secondary sources: 1). Egerman RS, Mercer BM,
Doss JL, et al. A randomized, controlled trial of oral and intramuscular dexamethasone in the
prevention of neonatal respiratory distress syndrome. Am J Obstet Gynecol 1998
Nov;179:1120–3 2). Crowley P. Prophylactic corticosteroids for preterm delivery (Cochrane
Review, latest revsion 19 Jan 96). In: Cochrane Library. Oxford: Update Software.
V. RESULTS OF THE STUDY
165 women were included in the intention to treat analysis. 99 infants were born to
women in the oral group and 84 infants were born to women in the intramuscular group. The
groups did not differ for the frequency of respiratory distress syndrome (34.3% in the oral
group v 29.8% in the intramuscular group, p=0.53). Infants of mothers who received oral
dexamethasone had increased rates of sepsis (10.1% v 1.2%, p=0.01) and intraventricular
hemorrhage (10.1% v 2.4%, p=0.04), but did not differ for rates of necrotising enterocolitis
(6.1% v 1.2%, p=0.13) or neonatal deaths (7.1% v 4.8%, p=0.55). Subgroup analyses of
women who delivered before 34 weeks gestation (n=112) showed similar results.
VI. AUTHOR’S CONCLUSION/RECOMMENDATIONS
Infants of women who received oral antenatal dexamethasone had similar rates of
neonatal respiratory distress syndrome as infants of women who received antenatal
intramuscular dexamethasone, but had higher rates of sepsis and intraventricular hemorrhage.
VII.APPLICABILITY
Does the study provide a direct enough answer to your clinical question in terms of type of
patients, intervention and outcome?
Yes, it provided direct answer. With the results shown in the study, the clinical question of
comparing the effectiveness between oral and intramuscular dexamethasone is answered.
Is it feasible to carry out nursing action in the real world?
Yes, the interventions are realistic and can be done and carried out in the real nursing
practice.
VIII.REVIEWER’S CONCLUSION/ COMMENTARY
Ellen Hodnett, RN, PhD
Professor and Heather M Reisman Chair in Perinatal Nursing Research University of Toronto
Toronto, Ontario, Canada
Preterm delivery occurs in 11% of all pregnancies and is a major cause of perinatal mortality and morbidity.1 The
benefits of prophylactic corticosteroids given to pregnant women to accelerate fetal lung maturity before preterm
delivery have been known for many years.2 Despite indisputable evidence of benefit, clinicians have been slow to
adopt this treatment, and thus preventable serious morbidity and deaths continue to occur. The trial by Egerman
et al evaluated a route of administration (oral) that is easier, less expensive, and probably more acceptable to
women. There are, however, a few worrisome methodological problems in this study. Mothers were randomised,
and therefore the data analysis should have been based on the pregnancy rather than the infant. There are 2
reasons for this: (1) one infant may have several adverse outcomes, and (2) one pregnancy may result in multiple
births. A few infants with multiple problems can make it seem that a pattern of greater morbidity has occurred in
one group, when only a few babies were actually affected, and these may have been the result of even fewer
pregnancies. The actual number of pregnancies with a serious adverse outcome may therefore be much smaller
than the numbers in the report suggest. There were 11 twin pregnancies in the oral group, compared with 6 in the
control group, and the report does not tell us how many infants or pregnancies had 1 or more serious adverse
outcomes. Furthermore, the trial had adequate statistical power to detect only large differences in respiratory
distress syndrome, necrotising enterocolitis, and neonatal deaths.
Thus, I am left with questions about how to interpret the study results, particularly
because, as the authors point out, there is no ready pharmokinetic explanation for the observed
differences. Despite these questions, there is clearly no basis to conclude that oral
administration of dexamethasone is as effective as the intramuscular route. Until we have
clear evidence to the contrary, I agree with the trial authors that oral administration cannot be
recommended.
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (894)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Caring for a Pregnant Woman with PROM and Severe OligohydramniosDokumen13 halamanCaring for a Pregnant Woman with PROM and Severe Oligohydramniosmanju100% (11)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Celine S. Udani BSN 135 I.Dokumen9 halamanCeline S. Udani BSN 135 I.Marvin UrgeBelum ada peringkat
- NR Pospartum PainDokumen2 halamanNR Pospartum PainMarvin UrgeBelum ada peringkat
- NCM Cardio HWDokumen4 halamanNCM Cardio HWMarvin UrgeBelum ada peringkat
- Ecologic ModelDokumen2 halamanEcologic ModelMarvin UrgeBelum ada peringkat
- Peptic Ulcer DiseaseDokumen57 halamanPeptic Ulcer DiseaseAnna VilceaBelum ada peringkat
- SMRT Radiation Therapy IntroDokumen18 halamanSMRT Radiation Therapy IntroDar WebBelum ada peringkat
- In vitro activity of tea-tree oil against clinical skin isolates of staphylococciDokumen6 halamanIn vitro activity of tea-tree oil against clinical skin isolates of staphylococciNICOLÁS SEBASTÍAN GOMEZ SEQUEDABelum ada peringkat
- Submerged Cultivation of Medicinal MushroomsDokumen30 halamanSubmerged Cultivation of Medicinal Mushroomsbravohr98Belum ada peringkat
- 6101 01 MSC 20080611Dokumen17 halaman6101 01 MSC 20080611sg noteBelum ada peringkat
- Stages of CancerDokumen9 halamanStages of CancerAlisha SharanBelum ada peringkat
- Austism Spectrum DisorderDokumen21 halamanAustism Spectrum DisorderFrancez Anne GuanzonBelum ada peringkat
- Water BugggssDokumen20 halamanWater BugggssShayna Evangelista Del ValleBelum ada peringkat
- Pathophysio DHF EDITEDDokumen3 halamanPathophysio DHF EDITEDricmichael100% (1)
- Genomic Imprinting Is An Epigenetic Phenomenon That Causes Genes To Be Expressed in A Parent-OfDokumen3 halamanGenomic Imprinting Is An Epigenetic Phenomenon That Causes Genes To Be Expressed in A Parent-OfRamy El-HadadBelum ada peringkat
- NEURULATION N Derivatives FDokumen70 halamanNEURULATION N Derivatives Ffilza farheenBelum ada peringkat
- Urine Formation. PDF My NoteDokumen11 halamanUrine Formation. PDF My NoteSurya JoyBelum ada peringkat
- Kumar Et Al 2008Dokumen16 halamanKumar Et Al 2008Ruth CastilloBelum ada peringkat
- DH2289E G6PD EnglishDokumen12 halamanDH2289E G6PD EnglishAmeer HamzaBelum ada peringkat
- Anca VasculitisDokumen12 halamanAnca Vasculitisatul_desai_3100% (2)
- PHILIPPINES Asthma Consensus Guidelines 2009Dokumen134 halamanPHILIPPINES Asthma Consensus Guidelines 2009Sirias_black50% (2)
- Rheumatoid ArthritisDokumen38 halamanRheumatoid ArthritisOlga GoryachevaBelum ada peringkat
- Lesson 5Dokumen46 halamanLesson 5Courtney BurkinBelum ada peringkat
- Current GM Crops & Transgenic AnimalsDokumen12 halamanCurrent GM Crops & Transgenic AnimalsJhayce Christian S. CapanayanBelum ada peringkat
- Haralabia BoletiDokumen5 halamanHaralabia BoletiHellenic Pasteur Institute - Athens, GreeceBelum ada peringkat
- People of AppalachianDokumen17 halamanPeople of AppalachianNestor BalboaBelum ada peringkat
- Transfusion 2015 ChapuyDokumen11 halamanTransfusion 2015 ChapuyNedelcu CarmenBelum ada peringkat
- Hemophilia and Its Treatment: Brief ReviewDokumen7 halamanHemophilia and Its Treatment: Brief ReviewSalsa BillaBelum ada peringkat
- Application For Job: Date: 17/05/2023Dokumen7 halamanApplication For Job: Date: 17/05/2023Bikila RusiBelum ada peringkat
- Flaccid Paraparesis Examination and Diagnosis GuideDokumen7 halamanFlaccid Paraparesis Examination and Diagnosis GuidePraptiwi 'tiw'Belum ada peringkat
- GeneticsDokumen48 halamanGeneticsDaja SewBelum ada peringkat
- Ers 2015Dokumen358 halamanErs 2015Dejan ŽujovićBelum ada peringkat
- Your Health Today Choices in A Changing Society 5th Edition Teague Test BankDokumen29 halamanYour Health Today Choices in A Changing Society 5th Edition Teague Test Banktaylorruiznqfpogxske100% (17)
- Intermediate MSUD: Maple Syrup Urine Disease (MSUD)Dokumen1 halamanIntermediate MSUD: Maple Syrup Urine Disease (MSUD)Awais_123Belum ada peringkat