Patient Education and Counseling Volume 54 Issue 1 2004 Doi
Diunggah oleh
NisadiyahFaridatusShahihHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Patient Education and Counseling Volume 54 Issue 1 2004 Doi
Diunggah oleh
NisadiyahFaridatusShahihHak Cipta:
Format Tersedia
Patient Education and Counseling 54 (2004) 5560
Assessment of impact of medication counseling on patients medication
knowledge and compliance in an outpatient clinic in South India
Sivasankaran Ponnusankar a, , Mallayasamy Surulivelrajan b ,
Nunjundiah Anandamoorthy c , Bhojraj Suresh d
a
Center for Patient Counseling and Education, Department of Pharmacy Practice, JSS College of Pharmacy, Ooty, The Nilgiris, Tamilnadu, India
b SRMC & RI, Porur, Chennai, India
c Priyanka Clinic, Ooty, India
d JSS College of Pharmacy, Ooty, The Nilgiris, Tamilnadu, India
Received 15 November 2002; received in revised form 15 March 2003; accepted 9 June 2003
Abstract
The primary aim of this study was to assess the impact of patient medication counseling by comparing the levels of patients medication
knowledge and adherence achieved by medication counseling in an outpatient clinic. Ninety patients were randomized in the ratio of 1:2 into
either counseled or usual care group. Their medication knowledge was assessed by a questionnaire and adherence was assessed by pill count
method and self-assessment by the patients. Their medication knowledge was assessed at baseline and during their subsequent appointments.
The average medication knowledge score of the counseled group versus usual care group was 13.821.8064 and 11.783.5037. Compliance
score of the patients during their follow-up period was 92.29 4.5 and 84.71 11.80 for the counseled and control group, respectively.
Statistical analysis of medication knowledge was carried out and all the demographic characters and number of medication were individually
correlated with medication knowledge score and the difference observed was statistically significant. Compliance score of the patients was
92.29 4.5 and 84.71 11.8% for the counseled and usual care group, respectively.
2003 Published by Elsevier Ireland Ltd.
Keywords: Compliance; Medication counseling; Medication knowledge; India
1. Introduction
Poor adherence to the prescribed medication regimen is
a critical health care concern for the health care providers
all over the world [1]. The National Pharmaceutical Council of US estimated the medical costs related to prescription
medicine misuse and adverse reactions total more than US$
20 billion a year. When consequences such as lost productivity are included, annual are as high as US$ 100 billion
[2]. This is particularly true for chronic diseases [3].
Numerous studies have been performed to identify therapeutically non-adherent patients, to measure the degree of
non-adherence, to characterize the reasons and to develop
strategies for improving compliance [418]. Educating the
patients about their disease state and medications will result
in the improvement of their knowledge regarding medications and can increase their active participation in therapy
Corresponding author.
E-mail address: ponnusankarsivas@hotmail.com (S. Ponnusankar).
0738-3991/$ see front matter 2003 Published by Elsevier Ireland Ltd.
doi:10.1016/S0738-3991(03)00193-9
and improve medication adherence, this may ultimately improve the outcomes.
Pharmacists with their professional knowledge irrespective of their working place either in hospital or in community can play a vital role in educating the patients and can
improve medication adherence and clinical outcome. Numerous studies have established this fact [1922].
1.1. Pharmaceutical care
Pharmaceutical care is defined as the direct, responsible provision of medication related care for the purpose of
achieving definite outcomes that improves patient quality of
life [23].
Pharmaceutical care services is almost nil in all Indian
hospitals and pharmacists are underutilized in the Indian
health care system. A recent initiation of clinical pharmacy
education and service in India [24], changes the industry focus education to patient focused. Clinical pharmacy service
includes ward round participation, provision of drug information service and patient counseling, etc.
56
S. Ponnusankar et al. / Patient Education and Counseling 54 (2004) 5560
So, it is our interest to study the impact of patient counseling services on patient outcomes. Such evaluation should
lead to improved quality of service, and help justify and
even further expand the pharmacists role in patient care.
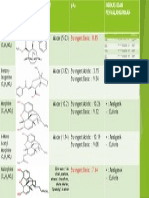
Table 1
Patient medication knowledge assessment form
Questions
Visit
1.2. Aim of the study
What is the name of this medication?/
Can you identify this medications?
I
II
III
What is the timings of this medications
and directions (if applicable)?
I
II
III
What these medications are for?
I
II
III
What is the dose of these medications?
I
II
III
Do you know how long you have to
take this medication?
I
II
III
Do you know what other food/medication
you have to avoid while taking this
medication?
I
II
III
The primary aim of this study was to assess the impact
of medication counseling on patient medication knowledge
and change in compliance behavior in an outpatient clinic
attached to the private hospital. We chose medication knowledge and adherence as our pilot end points before proceeding to study the effects on clinical outcome.
2. Materials and methods
The managing director of the private hospital and the
consultant physician of the outpatient clinic approved this
study. Patients meeting the inclusion criteria were randomized into the counseled and usual care group. Inclusion
criteria were: (i) patients with chronic conditions like hypertension, diabetes mellitus, cardiovascular conditions and
bronchial asthma, (ii) patients who had an established prescription and were diagnosed atleast 6 months before the
inclusion into the study. Exclusion criteria were: (i) patients
with cognitive or perceptual problems, (ii) patients who cannot be followed up.
Demographic data were obtained from all the patients. A
total of 90 patients were enrolled into the study in chronological order of their visits to the clinic and the study was
conducted for 9 months.
2.1. Randomization
A total of 90 data sheets were given to the consultant. Each
data sheet was coded as either (+), () or (0). The symbols
(+) and () was considered for the counseled group and (0)
was considered for the usual care group. After the consultation, the physician randomly picked one sheet and gives
it to the patient and sent the patient to the pharmacist. Depending upon the symbol of the data sheet, the patients were
enrolled into the counseled group or usual care group. A total of 30 patients were placed in the counseled group and
60 patients were placed in the usual care group. The ratio of
1:2 was chosen between the usual care and counseled group
as this was having the modest increase in power to detect
the differences more statistically significant.
Scores
B
Iinitial visit, II1st follow-up, III2nd follow-up; A, B, C, D
represents scoring (A: 3 marks, B: 2 marks, C: 1 mark, D: 0 mark).
in the medication knowledge assessment form, there was a
four-tiered grading scale that graded the patient as 0, 1, 2
and 3 according to their response. Four responses were expected for each question. Each response was assigned a particular score and then finally scores were added to get the
total score for the patient. The question asked to the patients
were: (a) what is the name of the medication you are taking during pregnancy/can you identify the medications? (b)
What are the timings of the medication? (c) What are the
medications for? (d) What are the doses of the medications?
(e) Do you know how long you have to take this medication?
(f) Do you know what other food/medication you have to
avoid while taking this? The expected response and scores
were: 3answering the questions correctly; 2answering
the questions partially; 1answering when prompted; 0
not answering the questions correctly.
Patient randomized to the counseled group received medication counseling from the pharmacist. This counseling session lasted 1520 min. Patient randomized into the usual care
group did not receive any counseling during the assessment
period.
2.3. Medication counseling
2.2. Counseling sessions and medication knowledge
assessment
Upon enrollment, patients were given a pretest to evaluate their knowledge regarding their disease and medications. For this purpose, medication knowledge assessment
form was designed and used (Table 1). For each question
At the out patient clinic, counseling sessions were performed at a separate corner of the clinic to ensure privacy.
One patient was counseled at a time. Counseling sessions
were designed so that all patients were counseled according to their individual understanding and attitude of their
medication. Pharmacist explained about their disease, the
S. Ponnusankar et al. / Patient Education and Counseling 54 (2004) 5560
name of the medications, identification of the medications,
dose, time of administration, purpose, duration of therapy of
their medication, food and other medications that have to be
avoided during their therapy, etc. Sufficient time was provided for the interaction of the patients with the pharmacist.
2.4. Follow-up visits
All patients were followed-up during their two subsequent
appointments, which was usually after 1 month, to assess
their medication knowledge and compliance.
2.5. Medication adherence
Medication adherence was assessed by the following two
methods:
(i) pill count method;
(ii) self-assessment method.
This was carried out during second appointment after the
enrollment. Patients were asked to bring back all the remaining medications and empty foils along with their medication
receipts. From this, medication adherence was calculated by
pill count method using the formula:
Percentage compliance
total number of doses the patient has
consumed since last appointment
=
100
total number of doses to be consumed
since last appointment
After this, patients were given a self-assessment form,
which was a bilingual one in both English and Tamil (local language). In this assessment patients who were rating
themselves less than always compliant were asked to state
the reason for their non-compliance.
2.6. Statistical analysis
Statistical analysis was carried out to study the difference
between the groups in medication knowledge by student
t-test. Influence of each demographic factor like age, sex,
education, number of drugs, duration of disease on medication knowledge was individually analyzed.
3. Results
Totally 90 patients were included in the study. Out of this
only 85 could be followed till the end of the study period.
Table 2 summarizes the baseline demographic data. Males
outnumbered females in the study population. In the total
selected patient population, majority of the patients had their
high/higher secondary education, their age between 41 and
60, consumed more than four drugs, duration of disease
57
Table 2
Baseline demographic data of patients
Factors
Number of patients
in counseled group
Number of patients
in usual care group
19 (63.33%)
11 (36.66%)
31 (51.66%)
29 (48.33%)
8 (26.6%)
6 (20%)
14 (46.66%)
9 (15%)
11 (18.33%)
30 (50%)
2 (6.66%)
10 (16.66%)
Age (in years)
40
4160
61
2 (6.66%)
20 (66.6%)
8 (26.6%)
5 (8.33%)
38 (63.33%)
17 (28.33%)
Number of drugs
3
4
9 (30%)
21 (70%)
30 (50%)
30 (50%)
Gender
Male
Female
Education
Illiterate
Middle school
High/higher secondary
school
Above school
Duration of disease (in years)
0.54
19 (63.33%)
59
7 (23.22%)
10
4 (13.33%)
36 (60%)
17 (28.33%)
7 (11.66%)
Diagnosis
Hypertension (HT)
HT & co-morbidities
Diabetes mellitus (DM)
DM & co-morbidities
7
45
3
5
1
19
1
9
(3.33%)
(63.33%)
(3.33%)
(30%)
(11.66%)
(75%)
(5%)
(8.33%)
0.54 years and established hypertension and co morbidities
patients were documented.
3.1. Medication knowledge score
Assessment of medication knowledge score was done using correlation between the score and demographic characters like age, education, diagnosis, duration of disease and
number of drugs. Table 3 summarizes the results of the correlations.
Baseline score of the males were higher than female
patient population. In the counseled group both the sex
showed statistically significant improvement from the baseline. Where as patients in the usual care group did not show
any statistically significant difference.
Baseline medication score showed a trend of gradual increase with the increase in the level of education. In the
counseled group, except graduates all other groups showed
a significant difference of score. In the usual care group, no
significant difference was observed.
Baseline medication score of the patients who were more
than 60 years of age are less, when compared with other
groups. In the counseled group, all the age group showed a
significant difference, where as in the usual care group did
not show any significant difference.
Baseline score of the patients who were taking 3 or less
number of medications was higher than the patients who are
58
S. Ponnusankar et al. / Patient Education and Counseling 54 (2004) 5560
Table 3
Effect of medication knowledge score and counseling
Factors
Gender
Male
Female
Baseline medication score
11.3 0.5293
10.4 0.4841
Medication score counseling group
Medication score usual care group
14.07 0.4742
13.57 0.4884
12.57 0.8155
11.3 0.5136
Education
Illiterate
Middle school
High/higher secondary school
Graduate
7.94
9.53
11.7
13.83
Age (in years)
40
4160
61
12.14 1.4869
10.98 0.4482
10.36 0.6997
16 0.00
13.8 0.4142
13.57 0.6116
14 1.3874
11.8 0.6126
11.5 0.9219
Number of drugs
3
4
11.87 0.5027
10.12 0.4978
14.3 0.3333
13.5 0.3847
12.51 0.6070
11.68 0.996
Duration of disease (in years)
0.54
59
10
11.17 0.4497
11.15 0.7247
9 1.0702
13.8 0.4917
13.57 0.5281
14 0.8164
12.31 0.5509
12.51 1.0257
8.85 1.4045
0.5908
0.8185
0.4491
0.8423
12.14
13.33
14.62
16
0.3400
0.6146
0.4317
1
9.25
10.09
12.43
14.72
0.9401
1.2318
0.6266
0.7310
P < 0.05.
P < 0.001.
consuming 4 and more number of medications. With counseled group, both the groups showed a significant difference. Usual care group did not show significant difference
in medication score.
Baseline medication score of the patients who had longer
duration of disease was less when compared with the patients
who had shorter duration of disease. Medication knowledge
score was significantly improved in the counseled group
when compared with usual care group.
3.2. Compliance assessment
3.2.1. Pill count method
Patients were asked to bring all the remaining medications and empty foils and medication receipts along with
their last prescription to assess the compliance. With the
help of remaining medications, the compliance was assessed (pill count). Due to the non-availability of previous
data regarding compliance baseline medication compliance could not be assessed for the first time. Medication
compliance could be assessed only during follow-up. Compliance score of the patients in the counseled group was
92.24 4.5 where as score of the patients in the usual
care group was 84.71 11.8. Counseling might have produced a positive effect on the compliance behavior of the
patients.
3.2.2. Compliance by self-assessment method
In this method of assessment of compliance, 75% of the
patients in the counseled group rated themselves as always
compliant against 66.6% in the usual care group. 25% in
the counseled group and 32.76% in the control group rated
themselves as compliant most of the time.
Patient who rated himself or herself less than always compliant were asked to state reasons for their non-compliance.
Most patients have rated forgetfulness (57.14% in the
counseled and 36.84% in the usual care group), and cost
of medications (28.57% in the counseled and 15.78% in
the usual care group). 11.1% of patients in the counseled
group and 47.36% in the usual care group stated side effects and lack of accessibility as reasons for their noncompliance.
4. Discussion and conclusion
There was a significant increase in the medication knowledge score of the patients in the counseled group compared to that in non-counseled group. Generally in Indian
hospitals, patients are not receiving counseling regarding their medications and therefore preliminary initiative
study was taken up and the study results shows counseling sessions was able to produce a statistically significant
improvements.
Determination of compliance by the pill count method and
self-assessment are the tools available for assessing compliance in the third world countries like ours, so these methods
were chosen for assessing compliance.
Compliance of the patients in the counseled group was
higher than the usual care group; counseling might have
produced a positive effect on the compliance behavior. Although this was a positive aspect, it cannot fully attributed to
S. Ponnusankar et al. / Patient Education and Counseling 54 (2004) 5560
counseling since the baseline compliance was not assessed
and this was the limitation of our study.
Since this study is the first of its kind in our country, we did
not have similar studies in our population to compare with.
Woronieki et al. [20] studied the effect of pharmacist counseling on long-term recall of drug information in 28 clinic
and hospital patients. By random assignment, patients were
placed into counseled and control group. All patients were
given pre-test before counseling and an identical post-test
after a period of 8 weeks. The counseled group scored better than the control group during the post test (88.10% versus 62.33%, P < 0.05). Similarly, in our study medication
knowledge of the patients in the counseled group was increased after the counseling.
By pill count method, it was found that compliance of
both the groups was well below 100%, however, in the
self-assessment large proportion of the patients rated themselves as always compliant. This showed either the patients
inflated their compliance or they were reluctant to admit
their non-compliance.
Other limitations of our study that are to be addressed are,
incomplete follow-up, in which five patients could not be
followed till the end of our study. The same investigator carried out medication knowledge assessment and counseling
and this might introduce bias to an extent into the study.
Assessing the medication adherence of the patients may
be good; it may not necessarily result in better clinical outcome. Clinical outcome measurement can only be carried
out during long-term follow-up of the patients. Since this
was a preliminary study from our department, we did not
measure the clinical outcome. Future studies will incorporate the use of clinical outcome to assess the role of pharmacist in quality health care.
4.1. Conclusion
Medication knowledge improvement was found to be statistically significant in the counseled group than the usual
care group. Compliance behavior of the patients showed a
positive trend. Since the baseline assessment of the compliance was not carried out, statistical analysis was not done.
Compliance of the patients in both the groups was found to
be good by pill count method and self-assessment method,
and these methods are liable to go unreliable since it depends
fully on the patient reports. Use of advanced systems like
medication event monitoring system might produce a clearer
picture of compliance scenario among the patient population
studied. Apart from the counseling other modalities such as
providing medication reminders, medication calendars and
emotional support and encouragement may improve compliance.
We are planning our future studies, which will incorporate the use of objective clinical outcome assessment (such
as change in blood pressure, blood sugar levels) to better establish the impact of pharmacists providing pharmaceutical
care in ambulatory settings.
59
4.2. Practice implications
Under developed countries may not have the facilities to
assess the adherence of the patients. However, pill count
method and self-assessment method moderately help the
pharmacists to assess the patient adherence. The concept of
pharmaceutical care provision in an outpatient clinic is well
established in developed countries, but yet to be initiated
in developing countries. This preliminary experiment in our
set-up, provision of pharmaceutical care by the pharmacists
in an outpatient clinic, was well received and encouraged by
the patients and medical fraternity.
Acknowledgements
Authors wish to thank FIP Foundation for Education and
Research, The Netherlands for providing FIPInternational
Travel Grant to present the summary of this paper at 61st
International Congress of FIP2001, Singapore.
References
[1] Vitalina R, Jean-Marie P, Kulvinder KS, Michelle KB, Judy WM
Cheng. Assessing the impact of medication consultations with a
medication event monitoring system. Hosp Pharm 1999;34:539
49.
[2] Dixie F. FDA proposed programs to give patients better medication
information. FDA Consumer Magazine 1995. http://www.fda.gov/
fdac/features/995 medinfo.html.
[3] Col N, Fanale JE, Kronholm P. The role of medication noncompliance
and adverse reactions in hospitalization of the elderly. Arch Intern
Med 1990;150:8415.
[4] Caldwell JR, Cobb S, Dowling MD. The dropout problem in antihypertensive treatment: a pilot study of social and emotional factors
influencing a patients ability to follow antihypertensive treatment. J
Chronic Dis 1970;22:57992.
[5] Urquhart J. Partial noncompliance in cardiovascular disease: risk
implications. Br J Clin Pract 1994;Suppl 3:112.
[6] Rudd P, Ramesh J, Bryant-Kosling C, Guerrero D. Gaps in cardiovascular medication taking: the tip of the ice berg. J Gen Intern Med
1993;8:65966.
[7] Lee JY, Kusek JW, Greene PG. Assessing medication adherence by
pill counts and electronic monitoring in the AfricanAmerican Study
of Kidney Disease and Hypertension. Am J Hypertens 1996;9:719
25.
[8] Urquhart J. Variable patient compliance in ambulatory trials: nuisance, threat, opportunity. J Antimicrob Chemother 1993;32:643
9.
[9] Waterhouse D, Calzone KA, Mele C, Brenner. Adherence to oral
tamoxifen: a comparison of patient self-report, pill-counts, and microelectronics monitoring. J Clin Oncol 1993;11:118997.
[10] Rudd P, Byyny RL, Zachary V, et al. The natural history of medication compliance in a drug trial: limitations of pill counts. Clin
Pharmacol Ther 1989;46:16976.
[11] Straka RJ, Fish JT, Benson SR. Patient self-reporting of compliance
does not correspond with electronic monitoring: an evaluation using
isosorbide dinitrate as a model drug. Pharmacotherapy 1997;17:126
32.
[12] Dickey FF, Mattar ME, Chudzik AM. Pharmacist counseling increases drug regimen compliance. Hospitals 1975;49:858.
60
S. Ponnusankar et al. / Patient Education and Counseling 54 (2004) 5560
[13] MacDonald ET, MacDonald JB, Phoenix M. Improving drug compliance after hospital discharge. Br Med J 1977;2:61821.
[14] Lobas NH, Lepinski PW, Abramowitz PW. Effects of pharmaceutical
care on medication cost and quality of patient care in an ambulatory
care clinic. AJHP 1992;49:16618.
[15] Mazzuca SA. Does patient education in chronic disease have therapeutic value? J Chronic Dis 1982;35:5219.
[16] Gibson FM, Hyneck ML, Scherrer JJ. Documented effectiveness of
clinical pharmacy services. AJHP 1982;39:19023.
[17] Hawe P, Higgins G. Can medication education improve the drug
compliance of the elderly? Evaluation of an in-hospital program.
Patient Educ Counsel 1990;16:15160.
[18] Morris LA, Halperin JA. Effects of written information on patient
knowledge and compliance: a literature review. Am J Publ Health
1979;69:4752.
[19] DeTullio PL, Corson ME. Effect of pharmacist counseling on ambulatory patients use of aerosolized bronchodilators. AJHP 1987;
44:18026.
[20] Woronieki CL, McKercher PL, Flagler DG. Effect of pharmacist
counseling on drug information recall. AJHP 1982;39:190710.
[21] Steven RB, Marilyn BS. Colour keyed medication counseling system.
AJHP 1981;38:7045.
[22] Maarrianne L, James AK, Adranne C, Christine E. A randomised
controlled trial of an enhanced compliance program for Helicobacter
Pylori therapy. Arch Int Med 1999;159:23126.
[23] Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm 1990;47:53343.
[24] Karin NH, Frank WM. Clinical pharmacy: a new beginning in India.
Aust J Hosp Phar 1998;25:3437.
Anda mungkin juga menyukai
- Strongest Basic: 8.85 Strongest Basic: 8.85: Benzoy-Lecgonine Benzoy - LecgonineDokumen1 halamanStrongest Basic: 8.85 Strongest Basic: 8.85: Benzoy-Lecgonine Benzoy - LecgonineNisadiyahFaridatusShahihBelum ada peringkat
- Firoz Et Al-2014-BJOG - An International Journal of Obstetrics & GynaecologyDokumen9 halamanFiroz Et Al-2014-BJOG - An International Journal of Obstetrics & GynaecologyImelda AtikaBelum ada peringkat
- Psidium Guajava (Guava) - A Plant of Multipurpose Medicinal Applications Barbalho 2012Dokumen6 halamanPsidium Guajava (Guava) - A Plant of Multipurpose Medicinal Applications Barbalho 2012Tiago AndradeBelum ada peringkat
- Msds Zonisamide PDFDokumen10 halamanMsds Zonisamide PDFNisadiyahFaridatusShahihBelum ada peringkat
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5795)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Spacers Vs Nebulizers in Children With Acute AsthmaDokumen3 halamanSpacers Vs Nebulizers in Children With Acute AsthmaRichard ChandraBelum ada peringkat
- Sonopuls 492Dokumen17 halamanSonopuls 492maroun machaalanyBelum ada peringkat
- CVS CaremarkDokumen10 halamanCVS CaremarkC4HCBelum ada peringkat
- Isolation 1Dokumen16 halamanIsolation 1Surabhi RairamBelum ada peringkat
- Abg Case StudiesDokumen22 halamanAbg Case StudiesMaria DalalBelum ada peringkat
- Steve de Shazer - in MemoriamDokumen2 halamanSteve de Shazer - in MemoriamKhoo Yi FengBelum ada peringkat
- Multiple SclerosisDokumen8 halamanMultiple SclerosisNader Smadi100% (1)
- Mp1 Biomedicalines Marketing: To: Quality Medical TradingDokumen4 halamanMp1 Biomedicalines Marketing: To: Quality Medical TradingJanna FabiaBelum ada peringkat
- 2013-04!16!17 IPC USP India SSS Agenda - Revised March 30Dokumen3 halaman2013-04!16!17 IPC USP India SSS Agenda - Revised March 30Jai KumarBelum ada peringkat
- Drug Study FormatDokumen2 halamanDrug Study FormatEmilie CajaBelum ada peringkat
- Towards Improving post-SSRI Sexual Dysfunction by Using Nutriceuticals: Lessons From A Case Study - Calabrò 2019Dokumen8 halamanTowards Improving post-SSRI Sexual Dysfunction by Using Nutriceuticals: Lessons From A Case Study - Calabrò 2019Julio JuarezBelum ada peringkat
- Homeopathic Remedy Guide For Headaches and Migraine DiseaseDokumen23 halamanHomeopathic Remedy Guide For Headaches and Migraine Diseasemiadelfior100% (1)
- Malignant Diseases of The CervixDokumen128 halamanMalignant Diseases of The Cervixnicewan0% (1)
- TTSH Nursing Survival GuideDokumen96 halamanTTSH Nursing Survival GuideSarip Dol100% (2)
- Attachment TheoryDokumen40 halamanAttachment Theorycristeacristina2007100% (9)
- Shen-Hammer Pulse Diagnosis and Overgrowth of CandidaDokumen4 halamanShen-Hammer Pulse Diagnosis and Overgrowth of CandidaRocío JMBelum ada peringkat
- Definition, Vocabulary and Academic Clarity-1Dokumen26 halamanDefinition, Vocabulary and Academic Clarity-1umarah khanumBelum ada peringkat
- Dorn Method Certification CourseDokumen10 halamanDorn Method Certification Coursejpepe100% (1)
- Pathology 2 TND LiveDokumen38 halamanPathology 2 TND Livepavan kumarBelum ada peringkat
- Update 2020 - Draft Baru 30 5 2019Dokumen9 halamanUpdate 2020 - Draft Baru 30 5 2019Ridho Naibaho NaibahoBelum ada peringkat
- Lembar Kerja Penilaian StudiDokumen3 halamanLembar Kerja Penilaian StudiMastering Archangel SchneiderBelum ada peringkat
- Lyme Disease ProtocolsDokumen2 halamanLyme Disease Protocolsramaflore100% (1)
- Soapp RDokumen7 halamanSoapp RAnaaaerobios100% (1)
- National Kidney FoundationDokumen16 halamanNational Kidney Foundationajeng puspitaBelum ada peringkat
- Para Instwise Adm Af Reporting Cancel r1Dokumen639 halamanPara Instwise Adm Af Reporting Cancel r1Rutvik DhoriyaBelum ada peringkat
- Malignant Soft Tissue TumorsDokumen21 halamanMalignant Soft Tissue TumorsEva GustianiBelum ada peringkat
- Drug Study AdenocarcinomaDokumen3 halamanDrug Study AdenocarcinomaJoyce AgorBelum ada peringkat
- Metered Dose InhalerDokumen61 halamanMetered Dose Inhalerdeepak374100% (1)
- AppendicitisDokumen17 halamanAppendicitisMarge Orge100% (1)
- Sociobiology and EthologSOCIOBIOLOGY-AND-ETHOLOGY - PptxyDokumen33 halamanSociobiology and EthologSOCIOBIOLOGY-AND-ETHOLOGY - PptxyJasmine ArateaBelum ada peringkat