Breast Cancer in Association With Thyroid Disorders
Diunggah oleh
Ridwan FajiriHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Breast Cancer in Association With Thyroid Disorders
Diunggah oleh
Ridwan FajiriHak Cipta:
Format Tersedia
Breast Cancer Research
Vol 5 No 5
Turken et al.
Open Access
Research article
Breast cancer in association with thyroid disorders
Orhan Turken1, Yavuz NarIn2, Sezai DemIrbas3, M Emin Onde4, Ozkan Sayan5,
E Gokhan KandemIr1, Mustafa YaylacI1 and Ahmet Ozturk5
1GATA
Haydarpasa Training Hospital, Medical Oncology Department, KadIkoy, Istanbul, Turkey
Haydarpasa Training Hospital, Nuclear Medicine Department, KadIkoy, Istanbul, Turkey
3GATA Haydarpasa Training Hospital, General Surgery Department, KadIkoy, Istanbul, Turkey
4GATA Haydarpasa Training Hospital, Endocrinology Department, KadIkoy, Istanbul, Turkey
5GATA Haydarpasa Training Hospital, Hematology Department, KadIkoy, Istanbul, Turkey
2GATA
Corresponding author: Orhan Turken (e-mail: oturken@hotmail.com)
Received: 21 Feb 2003 Revisions requested: 1 Apr 2003 Revisions received: 14 Apr 2003 Accepted: 24 Apr 2003 Published: 5 Jun 2003
Breast Cancer Res 2003, 5:R110-R113 (DOI 10.1186/bcr609)
2003 Turken et al., licensee BioMed Central Ltd (Print ISSN 1465-5411; Online ISSN 1465-542X). This is an Open Access article: verbatim
copying and redistribution of this article are permitted in all media for any purpose, provided this notice is preserved along with the article's original
URL.
See related Commentary: http://breast-cancer-research.com/content/5/5/235
Abstract
Background: The relationship between breast cancer and
thyroid diseases is controversial. Discrepant results have been
reported in the literature. The incidences of autoimmune and
nonautoimmune thyroid diseases were investigated in patients
with breast cancer and age-matched control individuals without
breast or thyroid disease.
Methods: Clinical and ultrasound evaluation of thyroid gland,
determination of serum thyroid hormone and antibody levels,
and fine-needle aspiration of thyroid gland were performed in
150 breast cancer patients and 100 control individuals.
Results: The mean values for anti-thyroid peroxidase
antibodies were significantly higher in breast cancer patients
than in control individuals (P = 0.030). The incidences of
autoimmune and nonautoimmune thyroid diseases were higher
in breast cancer patients than in control individuals (38%
versus 17%, P = 0.001; 26% versus 9%, P = 0.001,
respectively).
Conclusion: Our results indicate an increased prevalence of
autoimmune and nonautoimmune thyroid diseases in breast
cancer patients.
Keywords: breast, cancer, thyroid
Introduction
Breast cancer is a hormone-dependent neoplasm. Conflicting results regarding the clinical correlation between breast
cancer and thyroid diseases have been reported in the literature. Many studies showed that thyroid diseases are
common among women with breast cancer [16], whereas
other reports did not confirm such an association of breast
cancer with thyroid diseases [711]. Almost every form of
thyroid disease, including nodular hyperplasia [12], hyperthyroidism [13] and thyroid cancer [14,15], has been identified in association with breast cancer. These findings
have led to the investigation of the relationship between
breast cancer and autoimmune thyroid diseases (AITDs).
R110
Such a relationship is not a new observation, and some
authors have reported a higher prevalance of AITDs among
breast cancer patients than in age-matched control individuals [1618]. The precise significance of this association
remains elusive, and some reports have shown that the
presence of thyroid peroxidase (TPO) antibodies is associated with a significant improvement in outcome among
breast cancer patients [19] and is of similar importance to
other prognostic indices such as axillary nodal status and
tumour size [20]. The aim of the present prospective study
was to determine the prevalence of thyroid diseases in
patients with breast cancer as compared with that in the
general female population.
AITD = autoimmune thyroid disease; ER = oestrogen receptor; FNA = fine-needle aspiration; T3 = triiodothyronine; T4 = thyroxine; TSH = thyroidstimulating hormone; TPO = thyroid peroxidase.
Available online http://breast-cancer-research.com/content/5/5/R110
Materials and methods
Patient selection
A total of 150 consecutive women with breast cancer and
100 age-matched control women were included in the
present study, during the period from May 1998 to
December 2002. Breast cancer patients were
3880 years old (median age 63 years) and were without
any known thyroid disease. Three or four weeks after surgical procedure, the patients were evaluated before starting chemotherapy, hormone therapy or radiotherapy.
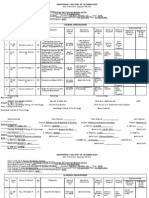
Table 1
Patient distribution according to clinical and ultrasound
evaluation of thyroid gland
Normal gland
Patients (n [%])
Control (n [%])
63 (42)
70 (70)
P
0.001
Diffuse goitre
12 (8)
4 (4)
0.29
Nodular goitre
75 (50)
26 (26)
0.001
Examinations
All patients underwent the following five examinations.
First, each patient underwent palpation of the thyroid
gland.
Second, ultrasonographic evaluation of the thyroid gland
was conducted by the same radiologist using an ultrasound scan fitted with a hand-held 6.611 MHz linear
transducer. The volume of each lobe was calculated using
the following formula: volume = length width height
0.479 [19]. Upper and lower normal lobe volume limits
were 18 ml and 10 ml, respectively.
Third, serum free triiodothyronine (T3) and free thyroxine
(T4) levels were determined, based on a solid-phase I125
radioimmunoassay designed for the quantitative measurement of free T3 and free T4 levels in serum using Coat-ACount kit containing radioactive I125-T3 or -T4 analogue
(DPC, Los Angeles, CA, USA). Also, serum thyroid-stimulating hormone (TSH) levels were measured using a
immunoradiometric assay designed for quantitative measurement of TSH in serum using Coat-A-Count kit containing radioactive I125-polyclonal anti-TSH (Diagnostics
Products Coorporation, Los Angeles, CA, USA). The
normal ranges were 2.26.8 pmol/l (1.44.4 pg/ml) for free
T3, 0.82.0 ng/dl for free T4 and 0.35.0 IU/ml for TSH.
Fourth, all patients underwent serological determination of
thyroid autoantibodies based on a direct Anti-TPO
radioimmunoassay kit for quantitative determination of
anti-TPO autoantibodies (Immunotech, Prague, Czech
Republic). Also, autoantibodies specific for thyroglobulin
were measured using a quantitative indirect enzyme
immunoassay based on the sandwich method (antithyroglobulin immunoradiometric assay kit; Immunotech,
Prague, Czech Republic). The normal ranges were
060 IU/ml for antithyroglobulin antibodies and
020 IU/ml for anti-TPO antibodies.
Finally, after informed consent had been obtained from
each patient, fine-needle aspiration (FNA) of the thyroid
gland was performed in breast cancer patients who had a
palpable thyroid nodule. The aspiration was performed
using a 22 guage needle and the smears were air dried
and dyed with MayGruenwaldGiemsa dye. FNA smears
were considered diagnostic for autoimmune thyroiditis if
there was an abundance of lymphocytes and plasmacytes
in a diffuse pattern and/or coexistence of many lymphocytes and oxyphilic epithelial cells.
Patients were separated into three groups according to
clinical and ultrasound findings: normal gland, diffuse
goitre and nodular goitre. Those women without any
breast or thyroid disease were the control group. Patients
were also classified into the following subgroups according to menopausal and oestrogen receptor (ER) status:
premenopausal and postmenopausal; and ER negative
and ER positive.
Statistics
Results are expressed as the mean standard deviation.
Clinical and other data were analyzed using MannWhitney
U and student t-test, as applied by the computerized statistical program SPSS (SPSS Inc., Chicago, IL, USA).
Results
The separation of patients into groups on the basis of
histopathological diagnosis is shown in Table 1. A total of
118 (79%) patients had invasive ductal carcinoma,
15 (10%) had invasive lobular carcinoma and 17 (11%)
had mixed (invasive ductal and lobular) carcinoma. In
breast cancer patients, diffuse goitre was identified in
12 cases (8%) and nodular goitre in 75 cases (50%). In
the remaining (42%) patients, thyroid glands were totally
normal by ultrasound and physical examination. In the
control group, diffuse goitre was identified in four (4%)
and nodular goitre in 26 (26%). Thus, the prevalence of
nodular goitre in the cancer group was higher, and this
finding was statistically significant (50% versus 26%;
P = 0.001; Table 1). With respect to thyroid volumes, measured ultrasonographically, the mean volumes of diffuse
thyroid gIand were 23.1 ml (range 1726 ml) in the breast
cancer patients and 21.9 ml (range 1627 ml) in the
control group. The mean volumes of nodular goitre in
breast cancer patients and in the control group were
19.2 ml (range 1321 ml) and 18.7 ml (range 1121 ml),
respectively.
R111
Breast Cancer Research
Vol 5 No 5
Turken et al.
Table 2
Table 3
Serum thyroid hormone and antibody levels
Classification of patients in relation to functional thyroid
diseases
Patients
Control
Free T3 (pmol/l)
8.47 0.75
4.48 0.75
0.48
Free T4 (ng/dl)
2.64 0.91
1.42 0.31
0.51
TSH (IU/ml)
3.12 1.40
1.46 0.82
0.27
TPO antibodies (IU/ml)
105.82 21.46
23.08 4.16
0.030
Tyroglobulin
antibodies (IU/ml)
140.92 21.52
27.75 7.60
0.094
Patients (n [%])
Control (n [%])
6 (4)
1 (1)
0.24
Hyperthyroidism
Hypothyroidism
4 (3)
0.152
Nontoxic goitre
77 (51)
29 (29)
0.001
Table 4
T3, triiodothyronine; T4, thyroxine; TPO, thyroid peroxidase; TSH,
thyroid-stimulating hormone.
Evaluation of thyroid function was based on serum thyroid
hormones. The mean values for serum thyroid hormones
were 8.47 0.75 pmol/l for free T3, 2.64 0.91 ng/dl for
free T4 and 3.12 1.40 IU/ml for TSH in breast cancer
patients, and 4.48 0.75 pmol/l, 1.42 0.31 ng/dl and
1.46 0.82 IU/ml, respectively, in the control group. The
differences between breast cancer patients and the
control group in mean serum free T3, free T4 and TSH
levels were not statistically significant (Table 2). Nontoxic
goitre was found in 77 (51%) of the breast cancer
patients and in 29 (29%) of the control individuals
(P = 0.001; Table 3).
The mean values for serum thyroid autoantibodies were
105.82 21.46 IU/ml for anti-TPO antibodies and
140.92 21.52 IU/ml for antithyroglobulin antibodies in
breast cancer patients, and 23.08 4.16 IU/ml and
27.75 7.60 IU/ml, respectively, in the control group.
Thus, the mean value for serum anti-TPO antibodies was
higher in breast cancer patients than in the control group
(P = 0.030), whereas the difference between the groups in
mean values for serum antithyroglobulin antibodies was
not statistically significant (P = 0.094). Autoimmune thyroiditis was defined by increased serum levels of at least
one thyroid autoantibody or diagnostic FNA findings, or
both. Among the breast cancer patients, autoimmune thyroiditis was diagnosed by autoantibodies in 42 (28%), by
FNA in four (2%) and by both in 11 (7%). The difference in
the frequency of autoimmune thyroiditis between breast
cancer patients and control group was statistically significant (P = 0.001; Table 4). On the other hand, non-AITD
was identified, with neither thyroid autoantibody in plasma
nor FNA findings specific to autoimmune thyroiditis, in the
patients with nodular or diffuse goitre.
R112
The mean thyroid hormone and autoantibody values were
compared between breast cancer patients and the control
group, according to menopausal and ER status. The differences between two groups according to both menopausal
status and ER status were not significant.
Classification of patients based on autoimmune and nonautoimmune thyroid disorders
Patients (n [%])
Controls (n [%])
Normal
54 (36)
74(74)
0.0001
Non-AITD
39 (26)
9 (9)
0.001
Autoimmune thyroiditis
57 (38)
17 (17)
0.001
AITD, autoimmune thyroid disease.
Discussion
The coincidence of thyroid disease and breast cancer has
long been a subject of debate. Although associations with
hyperthyroidism, hypothyroidism, thyroiditis and nontoxic
goitre have been reported in the literature, no convincing
evidence exists of a causal role for overt thyroid disease in
breast cancer. Geographical variations in the incidence of
breast cancer have been attributed to differences in
dietary iodine intake, and an effect of iodine on the breast
has been postulated [1]. The possible interactions
between thyroid gland and breast tissue are based on the
common property of the mammary and thyroid epithelial
cell to concentrate iodine by a membrane active transport
mechanism [18] as well as on the presence of TSH receptors in fatty tissue, which is abundant in mammary gland
[21]. Additionally, some endocrine stimuli identified in
thyroid products that exert a simultaneous action on the
breast and the various thyroid antibodies, which could
also interact with receptors on breast tumours, have been
postulated to be responsible for the coincidence of
mammary and thyroid gland disorders [15,22].
The present study found a high prevalance of goitre as
well as a high prevalence of autoimmune thyroiditis, confirmed mainly by antibody positivity, in breast cancer
patients. An association of autoimmune thyroid disease
with breast cancer has been reported in the literature
[1,16]. In those studies, increased serum levels of thyroid
antibodies were identified. Although Mittra and coworkers
[1] found the levels of thyroid antibodies in British women
to be lower than those in Japanese women, they found no
differences between incidences in breast cancer among
Available online http://breast-cancer-research.com/content/5/5/R110
women of either race. With the use of specific immunoassays for TPO and thyroglobulin antibodies, an increased
level of TPO has been demonstrated in breast cancer.
References
1.
2.
It has been proposed that the presence of thyroid abnormalities may influence breast cancer progression [19]. A
recent report suggested a better prognosis for breast
cancer among patients with increased levels of TPO [19].
It has been proposed that the immune response might be
directed both by tumour and by thyroid tissue [20], or that
the tumour and thyroid tissue share common properties,
as they both express TPO and the sodium iodide symporter gene [23,24]. Although high TPO level has been
shown to be a very important factor in antibody-dependent
cell cytotoxicity in the thyroid, and there may be a possible
association between autoimmune thyroiditis and the
immune system, there is no agreement on the significance
of its association with breast cancer.
The relationship between thyroiditis and prognostic factors
for breast cancer such as ER and stage has been investigated. In one study [1], a higher frequency of thyroiditis was
described in more advanced stages of breast cancer. In
another study reported by Giani and coworkers [18] no relationship was found between ER status and the presence of
serum thyroid antibodies. We found no correlations among
ER status, menopausal status and thyroid antibody levels.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
In addition to the reported high prevalance of autoimmune
thyroiditis among breast cancer patients, the incidence of
breast cancer among patients with chronic thyroiditis has
been investigated. In a study conducted by Ito and
Maruchi [2], those investigators reported that there was
an increase in risk for breast cancer among patients with
Hashimotos thyroiditis.
16.
Conclusion
19.
In this paper, we have studied thyroid autoantibody levels
and thyroid function tests in breast cancer patients and
controls. Abnormal thyroid gland characteristics were
revealed in the breast cancer patients compared with the
control group. The incidence of nodular goitre was significantly higher in the patients with breast cancer. Regarding
functional thyroid disorders, nontoxic goitre was significantly associated with breast carcinoma. There was a significant difference between the groups in terms of TPO Ab
levels; however, no difference was demonstrated for other
variables, such as Tg Ab and TFT.
These results indicate a significant association between
breast cancer and autoimmune and non-autoimmune
thyroid disorders. However, more research on this subject
is required to confirm this association.
17.
18.
20.
21.
22.
23.
24.
Mittra I, Perrin J, Kumaoka S: Thyroid and other autoantibodies
in British and Japanese women: an epidemiological study of
breast cancer. BMJ 1976, 1:257-259.
Ito K, Maruchi N: Breast cancer in patients with Hashimotos
thyroiditis. Lancet 1975, 2:1119-1121.
Kapdi JJ, Wolfe JN: Breast cancer relationship to thyroid supplements for hypothyroidism. JAMA 1976, 236:1124-1127.
Rasmusson B, Rasmussen UF, Hegedus L, Perrild H, Bech K,
Hoier-Madsen M: Thyroid function in patients with breast
cancer. J Cancer Clin Oncol 1987, 23:553-556.
Mittra I, Haysward JL: Hypothalamicpituitarythyroid axis in
breast cancer. Lancet 1974, 1:885-888.
Shering SG, Zbar AP, Moriatry M: Thyroid disorders and breast
cancer. Eur J Cancer Prev 1996, 5:504-506.
Maruchi N, Annegers JF, Kurland LT: Hashimotos thyroiditis
and breast cancer. Mayo Clin Proc 1976, 51:263-265.
Lemmarie M, Baugnet-Mahieu L: Thyroid function in women
with breast cancer. Eur J Cancer Clin Oncol 1986, 22:301-307.
Moossa AR, Price-Evans DA, Brewer AC: Thyroid status and
breast cancer: reappraisal of an old relationship. Ann R Coll
Surg 1973, 53:178-188.
Kurland LT, Annegers JF: Breast cancer and Hashimotos thyroiditis [letter]. Lancet 1976, 1:808.
Anker GB, Lonning PE, Aakvaag : Thyroid function in postmenopausal breast cancer patients treated with tamoxifen.
Scand J Clin Lab Invest 1998, 58:103-107.
Smyth PPA, Smith DF, McDermott P, Murray J, Geraghty JG,
OHiggins NJ: A direct relationship between thyroid enlargement and breast cancer. J Clin Endocrinol Metabol 1996, 81:
937-941.
Goldman MB: Thyroid diseases and breast cancer. Epidemiology Rev 1990, 12:28-30.
McThernan A, Weiss NS, Daling JR: Incidence of thyroid cancer
in women in relation to known or suspected risk factors for
breast cancer. Cancer Res 1987, 47:292-294.
Ron E, Curtis R, Hooffman DA, Flannery JT: Multiple primary
breast and thyroid cancer. Br J Cancer 1984, 49:87-90.
Gogas J, Kouskos E, Tseleni-Balafouta S, Markopoulos C,
Revenas K, Gogas G, Kostakis A: Autoimmune thyroid disease
in women with breast carcinoma. Eur J Surg Oncol 2001, 27:
626-630.
Myhil J, Reeve TS, Hales IB: Thyroid function in breast cancer.
Acta Endocrinol 1966, 51:290-300.
Giani C, Fierabracci P, Bonacci R, Gigliotti A, Campani D,
DeNegri F, Cecchetti D, Martino E, Pinchera A: Relationship
between breast cancer and thyroid disease: relevance of
autoimmune thyroid disorders in breast malignancy. J Endocr
Metab 1986, 81:990-994.
Smyth PPA, Kilbane MT, Murray MJ, Mc Dermott EWM, Smith DF,
OHiggins NJ: Serum thyroid peroxidase autoantibodies,
thyroid volume and outcome in breast cancer. Clin Endocr
Metab 1988, 83:2711-2716.
Smyth PPA: Autoimmune thyroid disease and breast cancer: a
chance association. J Endocrinol Invest 2000, 23:42-43.
Davies TF: The thyrotrophin receptors spread themselves
around. J Clin Endocrinol Metabol 1994, 79:1232-1238.
Dumont JE, Maenhaut C: Growth factors controlling the thyroid
gland. Baillieres Clin Endocrinol Metabol 1991, 5:727-753.
Spitzweg C, Joba W, Eisenmenger W, Heufelder A: Analysis of
human sodium iodide symporter gene expression in extrathyroidal tissues and cloning of its complementary deoxyribonucleic acids from salivary gland, mammary gland and gastric
mucosa. J Clin Endocrinol Metab 1998, 83:1746-1751.
Kilbane MTTA, Shering SG, Symith DF, McDermott EWM, OHiggins NJ, Symith PPA: Thyroid peroxidase (TPO): an autoantigen common to the thyroid and breast. J Endocrinol 1998,
156:323.
Correspondence
Orhan Turken, GATA Haydarpasa Training Hospital, Medical Oncology
Department, KadIkoy, Istanbul, Turkey. Tel: +9 0216 325 7250/1810;
fax: +9 0216 325 7257; e-mail: oturken@hotmail.com
Competing interests
None declared.
R113
Anda mungkin juga menyukai
- FirstMarathon RunnersWorldTrainingGuideDokumen7 halamanFirstMarathon RunnersWorldTrainingGuideDaisilySamuelBelum ada peringkat
- Diagnosis, Treatment, and Prevention of Typhoid Fever (WHO)Dokumen48 halamanDiagnosis, Treatment, and Prevention of Typhoid Fever (WHO)Nina KharimaBelum ada peringkat
- Guidelines Manage Typhoid Fever OutbreaksDokumen39 halamanGuidelines Manage Typhoid Fever OutbreaksNatasha ChandraBelum ada peringkat
- Cholesterol Granuloma Presenting As A Mass Obstructing The External Ear CanalDokumen5 halamanCholesterol Granuloma Presenting As A Mass Obstructing The External Ear CanalRidwan FajiriBelum ada peringkat
- Thyroid MetastasectomyDokumen6 halamanThyroid MetastasectomyRidwan FajiriBelum ada peringkat
- Update On The Diagnosis and Treatment of Caustic IngestionDokumen6 halamanUpdate On The Diagnosis and Treatment of Caustic IngestionRidwan FajiriBelum ada peringkat
- The Efficiency of Sucralfate in Corrosive Esophagitis A Randomized, Prospective StudyDokumen5 halamanThe Efficiency of Sucralfate in Corrosive Esophagitis A Randomized, Prospective StudyRidwan FajiriBelum ada peringkat
- Endoscopic Endonasal Approaches To Management of Cholesterol Granuloma of The Petrosus ApexDokumen5 halamanEndoscopic Endonasal Approaches To Management of Cholesterol Granuloma of The Petrosus ApexRidwan FajiriBelum ada peringkat
- Drugs in Pregnancy and LactationDokumen6 halamanDrugs in Pregnancy and LactationRidwan FajiriBelum ada peringkat
- Over The Counter Medications in PregnancyDokumen8 halamanOver The Counter Medications in PregnancyRidwan FajiriBelum ada peringkat
- The Teratogenicity of Anticonvulsant DrugsDokumen7 halamanThe Teratogenicity of Anticonvulsant DrugsRidwan FajiriBelum ada peringkat
- Hum. Reprod. Update 2010 Van Gelder 378 94Dokumen17 halamanHum. Reprod. Update 2010 Van Gelder 378 94Rismawati AcenkBelum ada peringkat
- Face Approximation and Information About Facial Soft Tissue ThicknessDokumen7 halamanFace Approximation and Information About Facial Soft Tissue ThicknessRidwan FajiriBelum ada peringkat
- Treating Asthma and Comorbid Allergic Rhintis in Pregnancy A Review of The Current GuidelinesDokumen10 halamanTreating Asthma and Comorbid Allergic Rhintis in Pregnancy A Review of The Current GuidelinesRidwan FajiriBelum ada peringkat
- The Teratogenicity of Anticonvulsant Drugs A Progress ReportDokumen3 halamanThe Teratogenicity of Anticonvulsant Drugs A Progress ReportRidwan FajiriBelum ada peringkat
- 3D Facial Reconstruction Tissue Depth Measurement From MRI ScansDokumen67 halaman3D Facial Reconstruction Tissue Depth Measurement From MRI ScansRidwan FajiriBelum ada peringkat
- Caroline Wilkinson - Facial Reconstruction ReviewDokumen16 halamanCaroline Wilkinson - Facial Reconstruction ReviewNahts Stainik WakrsBelum ada peringkat
- Advanced Life Support AlgoritmaDokumen1 halamanAdvanced Life Support AlgoritmaRidwan FajiriBelum ada peringkat
- Forensic Dentistry in Human Identification A Review of The LiteratureDokumen6 halamanForensic Dentistry in Human Identification A Review of The LiteratureRidwan FajiriBelum ada peringkat
- Wilkinson C., Computerized Forensic Facial Reconstruction, 2005Dokumen5 halamanWilkinson C., Computerized Forensic Facial Reconstruction, 2005Ridwan FajiriBelum ada peringkat
- Acute PainDokumen629 halamanAcute PainRidwan Fajiri100% (1)
- Wilkinson C., Computerized Forensic Facial Reconstruction, 2005Dokumen5 halamanWilkinson C., Computerized Forensic Facial Reconstruction, 2005Ridwan FajiriBelum ada peringkat
- Accuracy and Reliability of Facial Soft Tissue Depth Measurements Using Cone Beam Computer TomographyDokumen6 halamanAccuracy and Reliability of Facial Soft Tissue Depth Measurements Using Cone Beam Computer TomographyRidwan FajiriBelum ada peringkat
- Racial Characteristics of Human Teeth With Special Emphasis On The Mongoloid DentitionDokumen7 halamanRacial Characteristics of Human Teeth With Special Emphasis On The Mongoloid DentitionRidwan FajiriBelum ada peringkat
- Forensic Dentistry in Human Identification A Review of The LiteratureDokumen6 halamanForensic Dentistry in Human Identification A Review of The LiteratureRidwan FajiriBelum ada peringkat
- 3D Facial Reconstruction Tissue Depth Measurement From MRI ScansDokumen67 halaman3D Facial Reconstruction Tissue Depth Measurement From MRI ScansRidwan FajiriBelum ada peringkat
- Injury Severity ScoringDokumen12 halamanInjury Severity ScoringJavier del MattoBelum ada peringkat
- Procalcitonin To Guide Duration of Antibiotic Therapy in IntensiveDokumen7 halamanProcalcitonin To Guide Duration of Antibiotic Therapy in IntensiveRidwan FajiriBelum ada peringkat
- Cutaneous Manifestations of HIVDokumen26 halamanCutaneous Manifestations of HIVRidwan FajiriBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5784)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (72)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Medical Certificate: To Whom It May ConcernDokumen8 halamanMedical Certificate: To Whom It May Concernvissia guzmanBelum ada peringkat
- Cover Letter - NursingDokumen1 halamanCover Letter - Nursingapi-621785757Belum ada peringkat
- Anatomy-Esophagus & StomachDokumen5 halamanAnatomy-Esophagus & StomachAlbert CorderoBelum ada peringkat
- Ectopic PregnancyDokumen1 halamanEctopic PregnancyBheru Lal50% (2)
- Dose Conversions of ErythromycinDokumen4 halamanDose Conversions of ErythromycinastridridddddddsdBelum ada peringkat
- KAREEN PRC FILE Corrected FinalDokumen10 halamanKAREEN PRC FILE Corrected Finaljedkath2008Belum ada peringkat
- NNF Level II PDFDokumen33 halamanNNF Level II PDFDr ASHUTOSH BhardwajBelum ada peringkat
- Askep DislokasiDokumen19 halamanAskep DislokasiHana Syifana RobbyaniBelum ada peringkat
- Renal Calculi: /Stone/NephrolithiasisDokumen25 halamanRenal Calculi: /Stone/NephrolithiasisrohitBelum ada peringkat
- DNB Paper - IDokumen7 halamanDNB Paper - Isushil chaudhari100% (7)
- ToC - Nursing Administration Scope Standards of Practice 2E PDFDokumen1 halamanToC - Nursing Administration Scope Standards of Practice 2E PDFSailee RautBelum ada peringkat
- Sedation in The IcuDokumen4 halamanSedation in The Icuprashsubbu100% (1)
- Periodontal FlapsDokumen65 halamanPeriodontal FlapsSaleh AlsadiBelum ada peringkat
- NDP GuidelinesDokumen5 halamanNDP GuidelinesYaj AnilomBelum ada peringkat
- Client-Doula Agreement PDFDokumen5 halamanClient-Doula Agreement PDFDwjell WrightBelum ada peringkat
- JCM 03 00986Dokumen11 halamanJCM 03 00986yangkahBelum ada peringkat
- Core MGMT PDFDokumen517 halamanCore MGMT PDFCristianFranceschiBelum ada peringkat
- FibrothecomaDokumen94 halamanFibrothecomaMindy SantiagoBelum ada peringkat
- Emt Schedule 2014-15 RVD 10-27-14Dokumen3 halamanEmt Schedule 2014-15 RVD 10-27-14api-257829824Belum ada peringkat
- Benefits of Colostrum for NewbornsDokumen3 halamanBenefits of Colostrum for NewbornsAlia SalviraBelum ada peringkat
- Pfo IntroDokumen9 halamanPfo IntroabdirashidBelum ada peringkat
- DR Perla D Santos OcampoDokumen2 halamanDR Perla D Santos OcampoAiza CabolesBelum ada peringkat
- Crack The Core Exam - Volume 2 4th PDFDokumen508 halamanCrack The Core Exam - Volume 2 4th PDFQuỳnh Trâm86% (7)
- Disruption of Radiologist WorkflowDokumen6 halamanDisruption of Radiologist WorkflowChrisBelum ada peringkat
- Manual of Temporal Bone DissectionDokumen82 halamanManual of Temporal Bone DissectionBungbu Tn100% (3)
- Science in The Art of Osteopathy PDFDokumen378 halamanScience in The Art of Osteopathy PDFPetru Acozmei100% (5)
- Wound DehiscenceDokumen3 halamanWound DehiscenceDanickz Natura MallariBelum ada peringkat
- Complication of FractureDokumen38 halamanComplication of FractureAshok BalwadaBelum ada peringkat
- Pathophysiology of SyncopeDokumen2 halamanPathophysiology of SyncopeErwin Chiquete, MD, PhDBelum ada peringkat
- DNB Anesthesia JuneDokumen22 halamanDNB Anesthesia JuneDebangshu KumarBelum ada peringkat