Early Urinary Diversion in Radiation Cystitis
Diunggah oleh
Ninan ChackoHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Early Urinary Diversion in Radiation Cystitis
Diunggah oleh
Ninan ChackoHak Cipta:
Format Tersedia
ORIGINAL ARTICLE
ANZJSurg.com
Early urinary diversion with ileal conduit and vesicovaginostomy in
the treatment of radiation cystitis due to carcinoma cervix: a study
from a tertiary care hospital in South India
John Samuel Banerji, Antony Devasia, Nitin Sudhakar Kekre and Ninan Chacko
Department of Urology, Christian Medical College, Vellore, India
Key words
radiation cystitis, ileal conduit, vesicovaginostomy.
Correspondence
Dr John Samuel Banerji, Department of Urology,
Christian Medical College, Vellore 632004, India.
Email: johnsbanerji@cmcvellore.ac.in
J. S. Banerji MS, MCh, DNB; A. Devasia
MS, MCh, FRCS(Ed); N. S. Kekre MS, DNB;
N. Chacko MS, MCh, FRCS.
Accepted for publication 21 September 2014.
doi: 10.1111/ans.12898
Abstract
Background: To study the magnitude of radiation cystitis following radiation therapy
for carcinoma cervix, and propose an algorithm to decide on early diversion, with or
without vesicovaginostomy.
Methods: Women who developed radiation cystitis following radiotherapy for carcinoma cervix from January 1998 to December 2011 were included in this retrospective
study. Electronic hospital records were analysed to document the presence of radiation
cystitis. All women who developed evidence of radiation-induced cystitis, according to
the common toxicity and Radiation Therapy Oncology Group criteria, were included
in the study. We looked at transfusion requirements, number of hospital admissions,
quality of life and cost involved. Chi-square tests were done where applicable. SPSS
version 16 was used for analysis.
Results: Of the 902 patients who received radiation for carcinoma cervix in the
13-year period, 62 (6.87%) developed grade 3/4 cystitis. Twenty-eight of them underwent ileal conduit diversion, with 18 undergoing concomitant vesicovaginostomy.
When compared with the patients who did not have diversion, the transfusion requirements, number of hospital admissions and quality of life had a statistically significant
difference. Cost analysis of early diversion too showed a marginal benefit with early
diversion. The limitation of the study was that it was retrospective in nature.
Conclusion: In radiation cystitis, multiple hospital admissions and consequential
increase in cost is the norm. In severe disease, early diversion is a prudent, costeffective approach with good quality of life and early return to normal activity.
Introduction
Radiation therapy is an important armamentarium in the treatment of
pelvic malignancies. However, the bladder and the rectum do often
get inadvertently irradiated, especially in the pre-intensitymodulated radiation therapy era.
Radiation cystitis has a significant morbidity, requiring recurrent
hospital admissions. Added to this is the burden of recurrent transfusions, with its attendant risk of blood-borne infections. Although
modalities like alum instillation and hyperbaric oxygen have been
used, long-term efficacy data is lacking.
Carcinoma cervix being predominantly a disease of the lower
socio-economic group, economics begins to further dictate management protocols. As there were no recommended guidelines, we
embarked on this retrospective study to determine if we could formulate a management protocol for severe radiation cystitis.
2014 Royal Australasian College of Surgeons
The aim of this study was to evaluate the magnitude of radiation
cystitis following radiation therapy, for carcinoma cervix, and to
assess the impact of urinary diversion as a treatment modality in the
more severe forms of radiation cystitis. A cost analysis comparing
repeated admissions to early diversion was also performed.
Methodology
This was a retrospective study spanning from January 1998 to
December 2011, with approval of the institutional review board.
Electronic data review of patients who received radiotherapy for
carcinoma cervix was obtained.
All patients who had symptoms suggestive of radiation cystitis
according to the common toxicity criteria viz. burning micturition,
increased frequency, haematuria, incontinence, renal failure were
initially evaluated. They were then categorized according to the
ANZ J Surg (2014)
Banerji et al.
Radiation Therapy Oncology Group grading for radiation cystitis,
into the mild (grades 1 and 2) cystitis, and the severe cystitis (grades
3 and 4).
The study groups were the ones with severe radiation cystitis
(grades 3 and 4).
The parameters studied were time interval from radiation to the
development of cystitis, dosage of radiation received, requirement of
transfusions, number of admissions, cost for each admission and
cost of diversion procedure.
The initial management of all patients who presented with a first
episode of haematuria was a bladder wash. At the time of bladder
wash, obvious bleeding points were fulgurated, using a monopolar,
underwater diathermy through a resectoscope. Patients were then
catheterized with a 22-Fr three-way catheter, and their bladders
irrigated with normal saline for at least 24 h.
Subsequently, they were instructed to avoid overdistension
of the bladder and were instructed on frequent, timed voiding
habits.
Over the past 6 years, we began offering patients diversion, with
an aim of improving quality of life and decreasing cost. Patients
were deemed candidates for diversion if the haematuria was recurrent, necessitating more than three admissions.
Patients were deemed suitable for diversion, only after ensuring
that there was no recurrence of disease. These patients underwent a
thorough gynaecological examination and contrast enhanced computerized tomography scan of the abdomen. Those who had elevated
creatinine at presentation underwent ultrasonography of the
abdomen, for upper tract evaluation.
Initially, we were only performing an ileal conduit diversion.
However, as the bladder was being left intact, there was a theoretical
possibility of developing pyocystitis, and hence during the latter part
of the study, a vesicovaginostomy was also incorporated.
Vesicovaginostomy was performed using a Collins knife used
through a resectoscope. The resectoscope was inserted into the
bladder, and a full thickness perforation was created into
the vagina, ensuring that the bladder secretions would drain into the
vagina.
Statistical analysis was done using SPSS version 16 (SPSS Inc,
Chicago, IL, USA).
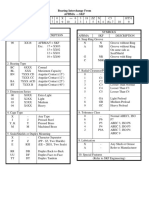
The 62 patients with severe cystitis were subsequently analysed.
Earlier, patients were being managed with bladder washes, fulguration and transfusions. Of these, 12 had multiple bladder washes
(more than three times). Four patients received intravesical alum
(1%), and two patients even had 1% formalin instillation. The flow
chart of management is given in Figure 1.
As there was no agreed protocol or guidelines anywhere in literature, these patients, during the earlier years, were managed according to surgeon choices and preferences. These patients constituted
group A (n = 34).
During the last 8 years, we have changed our policy of management, and are offering diversion in patients who have recurrent
haematuria, multiple admissions and transfusions. These constituted
group B (n = 28).
As can be seen from Table 2, the mean age of onset was similar in
the two groups.
However, the time interval to onset of cystitis (P = 0.0027, CI
0.5425 to 2.4575), the mean number of transfusions (P = <0.0001,
CI 2.8702 to 4.3298) and mean number of admissions to hospital (P
= <0.0001, CI 3.2109 to 4.7891) were statistically significant. The
radiation doses were similar in both groups, with no statistical difference between the groups. Both received a combination of external
beam radiotherapy and intracavitary brachytherapy.
The complications of radiation in the two groups were also
studied. Radiation proctitis was seen in both groups (group A
23.59%; group B 21.67%), but the difference was not statistically
significant (Table 3).
Five patients in group B presented with hydroureteronephrosis
and altered renal function. All of them underwent preoperative per
cutaneous nephrostomy placement, and once their renal parameters
improved, underwent diversion.
Of the 28 who underwent diversion, one patient developed deep
venous thrombosis and a superior vena cava obstruction (Grade IV
Clavien Dindo Classification). She was put on oral anticoagulation
with warfarin.
What was noteworthy is that although these patients received
radiation, none of them had a surgical site infection, or an
anastomotic leak.
Results
The total number of patients who developed radiation cystitis in the
13-year period was 184. Of these, 62 developed severe cystitis
(Table 1). Two patients died because of sepsis and one had a bladder
perforation, peritonitis and multi-organ dysfunction.
Table 1 Baseline data
Total cases of carcinoma cervix treated with radiation
Total no. of radiation cystitis
Grades 1 and 2 cystitis
Grades 3 and 4 cystitis
Deaths in grades 3 and 4 cystitis
Lost to follow-up
902
184
122
62
3
2
Fig. 1. Flow chart showing management of grades 3 and 4 radiation
cystitis.
2014 Royal Australasian College of Surgeons
Early urinary diversion for severe radiation cystitis
Table 2 Comparison of patients who were managed conservatively (group A) with those who underwent diversion (group B)
Mean group A (n = 34)
Range
Mean group B (n = 28)
Range
Age of onset
53.3 years (SD-3.12)
3470 years
50.3 years (SD-2.95)
3270
Mean number of transfusions
2 units (SD-1.22)
03 units
5.6 units (SD-1.65)
37 units
Mean number of admissions
1.2 (SD-1.62)
13
5.2 (SD-1.45)
28
Mean radiation dosage (EBRT and
brachy)
Time interval to onset of cystitis
51 Gy (SD-1.44)
5054.4 Gy
53.2 Gy (SD-1.25)
5253.2 Gy
8.3 years (SD-1.72)
610 years
9.8 years (SD-2.05)
412 years
Patient Global Impression of change
3 (n = 24)
5.2 (n = 28)
P-value
0.08
CI 1.9646 to 4.0354
t = 5.7959
SE Diff 0.17
<0.0001
CI 2.8702 to 4.3298
t = 9.8676
SE Diff 0.365
<0.0001
CI 3.2109 to 4.7891
t = 10.1397
SE Diff 0.394
0.09
0.0027
CI 0.5425 to 2.4575
t = 3.1337
SE Diff 0.479
0.06
EBRT, external beam radiotherapy.
Discussion
Table 3 Complications (groups A and B)
Radiation proctitis
Pre-renal azotemia
Hydroureteronephrosis
DVT/SVC obstruction
Group A (n = 34)
Group B (n = 28)
8
1
0
0
6
3
5
1
DVT, deep venous thrombosis; SVC, superior vena cava.
Follow-up
Follow-up was available for all the women in group B, and 25 of the
34 women in group A. The mean follow-up was 23.2 months (range:
1568 months) in group A and 13.2 months in group B (range: 620
months).
Quality of life changes were difficult to assess, and as there were
no previously used models to study the same, we used the Patients
Global Impression of Change scale. This was a simple tool, using a
telephonic question asked to patients, whether they felt any change
in their symptoms after treatment.
As expected, in group A, we were able to get only 24/34 patients
to respond. The average score there was 3/7. In group B, all 28
patients responded, and the mean score was 5.2/7. Though this was
not statistically significant (P = 0.06), the ones who underwent
diversion were extremely satisfied with the resultant improvement in
quality of life.
We also tried to address cost issues. The average inpatient bills for
urinary diversion in the form of ileal conduit with or without
vesicovaginostomy was Rs 55 000 (US$1000).
Each admission with haematuria necessitating bladder washes
and transfusion costs were about Rs 15 000 (US$272.72).
With a mean admission rate of 5.2 in the group A patients, this
would add up to a cost of about Rs 78 000 (US$1418). Thus, it was
evident that early diversion would indeed be cost-effective in this
setting of severe grade radiation cystitis.
2014 Royal Australasian College of Surgeons
Pelvic radiation for carcinoma cervix has been a mainstay of treatment for decades. However, toxicity to the bowel and bladder do
occur, especially with escalating doses of radiation in excess of
60 Gy.1 The most acceptable theories for late manifestations of
radiation cystitis is the ischaemic theory wherein endarteritis caused
by radiation causes ischaemic changes to the urothelium and the
detrusor muscle leading to ulceration, scarring and fibrosis.24
A recent study from India noted that 11.2% of patients had toxicities of all grades, and 1.2% of patients had severe (grades 3/4)
toxicity to the bladder.5 Our patient population had a marginally
higher rate of severe cystitis (6.78%). This could be due to the fact
that we had a mixed, mobile population where in about 30% of our
population are from other states. As the initial inciting factor viz.
radiation would have been given elsewhere, the dosimetry schedules
probably varied at different centres. Hence, the higher rates of severe
cystitis as compared with the oft mentioned 13%.
The management of cystitis depends on the grade of cystitis.
Those with grade 1 and 2 (Radiation Therapy Oncology Group)
cystitis generally are instructed about timed voiding. Vitamin E has
been used by many with varying results.
The severe grades are the more difficult to manage. A host of
different methods have been used, like argon plasma coagulation,
alum instillation, formalin instillation and even hyperbaric oxygen
therapy.
While alum and formalin have been around for a long time, there
are only a few studies to prove efficacy, with frequent instillations
necessary.
The use of formalin is not without danger of complications like
ureteral stenosis, fibrosis and bladder perforation. Studies show that
35% develop minor complications with as much as 105 developing
the severe complications with use of formalin.6
Alum irrigation, another common method used earlier6 was relegated to the background because of documentation of complications like neurological deterioration, anaemia and cardiomyopathy.7
Use of the argon plasma coagulator has been reported by Wines
and Lynch,8 but has been in only seven patients in whom grade of
cystitis was moderate, but not severe as in the type of patients who
presented to us.
The efficacy of hyperbaric oxygen therapy use in radiation cystitis
has been modest at best, with Del Pizzo et al.9 reporting 27% durable
response. They conclude that hyperbaric oxygen had good shortterm benefits, but was poor at long-term cure of the disease process.
In this scenario of severe cystitis, we would like to propose that
diversion does in fact address the host of related issues with radiation
cystitis, and contributes to improving quality of life. The need to
address the residual, defunct bladder arises from evidence that the
residual bladder could be a seat for a pyocystitis. Adeyoju et al.10
report their experience in 25 patients who they followed up, with a
suprapubic diversion, and noted that 28% developed complications,
of which pyocystis was an important complication. This was also
corroborated by Kemp and Dretler.1113
Hence, we resort to the technically easy vesicovaginostomy, to
ensure that pyocystis does not occur at a later point in time.
Contrary to belief that radiated bowel would not heal, none of our
patients had any post-operative morbidity with relation to ileo-ileal
anastomotic leak.
When analysing the economic burden of the disease, analysis
revealed that although the cost of diversion was more than that of
conservative measures, in those with severe cystitis, accumulative
cost would add up to more than that of diversion in the long run.
Added to this is the possible transfusion related morbidity associated
with multiple transfusions.
Limitations of our study include the retrospective nature of the
study.
Quality of life issues were assessed using the Patients Global
Impression of Improvement. We did not have data on 10 patients in
group A, and that was probably due to the fact that they had little
improvement. Although the change was not statistically significant,
this was the first attempt at reporting quality of life for radiation
cystitis.
These results could be a basis for future prospective studies, with
a more robust design.
Nevertheless, the excellent outcome with this procedure in these
otherwise moribund patients urges us to propose that early diversion
be considered in those patients who have had prior, multiple failed
Banerji et al.
cyst fulguration, those with bladder capacities <150 mL or those
requiring a whole blood volume equivalent transfusion.
Conclusion
In radiation-induced cystitis, multiple admissions necessitating
transfusions are the norm. Early diversion in a select group of
patients is a good, cost-effective option, with good quality of life,
and should be offered in the setting of severe radiation cystitis.
References
1. Pointreau Y, Atean I, Durdux C. Normal tissue tolerance to external
beam radiation therapy: bladder. Cancer Radiother. 2010; 14: 3638.
2. Pavlidakey PG, MacLennan GT. Radiation cystitis. J. Urol. 2009; 182:
11723.
3. Marks LB, Carroll PR, Dugan TC et al. The response of the urinary
bladder, urethra and ureter to radiation and chemotherapy. Int. J. Radiat.
Oncol. Biol. Phys. 1995; 31: 125780.
4. Crew JP, Jephcott CR, Reynard JM. Radiation-induced haemorrhagic
cystitis. Eur. Urol. 2001; 40: 11123.
5. Saibishkumar EP, Patel FD, Sharma SC. Evaluation of late toxicities of
patients with carcinoma of the cervix treated with radical radiotherapy:
an audit from India. Clin. Oncol. (R. Coll. Radiol.) 2006; 18: 307.
6. Donahue LA, Frank IN. Intravesical formalin for hemorrhagic cystitis:
analysis of therapy. J. Urol. 1989; 141: 80912.
7. Seear MD, Dimmick JE, Rogers PC. Acute aluminium toxicity after
continuous intravesical alum irrigation for haemorrhagic cystitis.
Urology 1990; 36: 3534.
8. Wines MP, Lynch WD. A new minimally invasive technique for treating
radiation cystitis: the argon-beam coagulator. BJU Int. 2006; 98: 6102.
9. Del Pizzo JJ, Chew BH, Jacobs SC, Sklar GN. Treatment of radiation
induced hemorrhagic cystitis with hyperbaric oxygen: long-term
followup. J. Urol. 1998; 160: 7313.
10. Adeyoju AB, Thornhill J, Lynch T, Grainer R, McDermott R, Butler
MR. The fate of the defunctionalized bladder following supravesical
urinary diversion. Br. J. Urol. 1996; 78: 803.
11. Kemp DR. The forgotten bladder after urinary diversion. Report of a
case of a sealed bladder. Br. J. Surg. 1966; 53: 2369.
12. Dretler SP. The occurrence of empyema cystis; management of the
bladder to be defunctionalized. J. Urol. 1972; 108: 824.
13. Fazili T, Bhat TR, Masood S, Palmer JH, Mufti GR. Fate of the leftover
bladder after supravesical urinary diversion for benign disease. J. Urol.
2006; 176: 6201.
2014 Royal Australasian College of Surgeons
Anda mungkin juga menyukai
- Fetal HydronephrosisDokumen12 halamanFetal HydronephrosisNinan ChackoBelum ada peringkat
- How To Make Dakin's Solution: SuppliesDokumen2 halamanHow To Make Dakin's Solution: Suppliesbradley_brown_1Belum ada peringkat
- Environment Matters 1 High Res PDFDokumen3 halamanEnvironment Matters 1 High Res PDFNinan ChackoBelum ada peringkat
- Cathere Care PDFDokumen1 halamanCathere Care PDFNinan ChackoBelum ada peringkat
- Themarriageyouwant PDFDokumen90 halamanThemarriageyouwant PDFNinan ChackoBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (120)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Essential Calculus Skills Practice Workbook With Full SolutionsDokumen528 halamanEssential Calculus Skills Practice Workbook With Full SolutionsGerardo Navarro Sánchez94% (65)
- Frye LGD As A Function of The Default Rate 091013 PDFDokumen13 halamanFrye LGD As A Function of The Default Rate 091013 PDFSushant SinghBelum ada peringkat
- B737-3 ATA 23 CommunicationsDokumen112 halamanB737-3 ATA 23 CommunicationsPaul RizlBelum ada peringkat
- Las Tech Drafting 3Q WKDokumen13 halamanLas Tech Drafting 3Q WKClemenda TuscanoBelum ada peringkat
- Esterification Oil of WintergreenDokumen8 halamanEsterification Oil of WintergreenMaria MahusayBelum ada peringkat
- EDS-A-0101: Automotive Restricted Hazardous Substances For PartsDokumen14 halamanEDS-A-0101: Automotive Restricted Hazardous Substances For PartsMuthu GaneshBelum ada peringkat
- Gujral FCMDokumen102 halamanGujral FCMcandiddreamsBelum ada peringkat
- Pusheen With Donut: Light Grey, Dark Grey, Brown, RoséDokumen13 halamanPusheen With Donut: Light Grey, Dark Grey, Brown, RosémafaldasBelum ada peringkat
- Underground Equipment SelectionDokumen44 halamanUnderground Equipment SelectionCherotich Silas cheboseiBelum ada peringkat
- Wang Jinhui - Competitive Physics - Thermodynamics, Electromagnetism and Relativity (2019, World Scientific Publishing Co. Pte. LTD.)Dokumen961 halamanWang Jinhui - Competitive Physics - Thermodynamics, Electromagnetism and Relativity (2019, World Scientific Publishing Co. Pte. LTD.)Paritosh PandeyBelum ada peringkat
- Anderson, Poul - Flandry 02 - A Circus of HellsDokumen110 halamanAnderson, Poul - Flandry 02 - A Circus of Hellsgosai83Belum ada peringkat
- Asco Series 238 ASCO Pilot Operated Solenoid Valves (Floating Diaphragm)Dokumen2 halamanAsco Series 238 ASCO Pilot Operated Solenoid Valves (Floating Diaphragm)Khyle Laurenz DuroBelum ada peringkat
- Data SiEMEx School SafetyPreparedness 25 26 NOVDokumen81 halamanData SiEMEx School SafetyPreparedness 25 26 NOVSuraj RajuBelum ada peringkat
- Vanish Magic Magazine VANISH MAGIC MAGAZINE 58 May 2019Dokumen118 halamanVanish Magic Magazine VANISH MAGIC MAGAZINE 58 May 2019mick byrnes100% (1)
- Haldex-Barnes 2-Stage Pump For Log SplittersDokumen2 halamanHaldex-Barnes 2-Stage Pump For Log SplittersPer Akkamaan AgessonBelum ada peringkat
- Carinthia Katalog DownloadDokumen16 halamanCarinthia Katalog DownloadOperator_010100% (2)
- IBM BladeCenter S RedBookDokumen36 halamanIBM BladeCenter S RedBookGuillermo García GándaraBelum ada peringkat
- Kimi No Na Wa LibropdfDokumen150 halamanKimi No Na Wa LibropdfSarangapani BorahBelum ada peringkat
- Resume: Satyam KumarDokumen3 halamanResume: Satyam KumarEr Satyam Kumar KrantiBelum ada peringkat
- 15 Benefits of CyclingDokumen8 halaman15 Benefits of CyclingJoycs PintoBelum ada peringkat
- 500 TransDokumen5 halaman500 TransRodney WellsBelum ada peringkat
- Sample Appellant BriefDokumen6 halamanSample Appellant BriefKaye Pascual89% (9)
- Science Magazine February 2020Dokumen133 halamanScience Magazine February 2020Elena González GonzálezBelum ada peringkat
- T.A.T.U. - Waste Management - Digital BookletDokumen14 halamanT.A.T.U. - Waste Management - Digital BookletMarieBLBelum ada peringkat
- 1F-Korean-Nami Mun - Miles From NowhereDokumen4 halaman1F-Korean-Nami Mun - Miles From NowhereNeil PatelBelum ada peringkat
- Discrete Wavelet TransformDokumen10 halamanDiscrete Wavelet TransformVigneshInfotechBelum ada peringkat
- Nomenclatura SKFDokumen1 halamanNomenclatura SKFJuan José MeroBelum ada peringkat
- Para Lec CombinedDokumen83 halamanPara Lec CombinedClent Earl Jason O. BascoBelum ada peringkat
- 331-10 331 Operators Manual enDokumen12 halaman331-10 331 Operators Manual enYahir VidalBelum ada peringkat
- G-3 L-17 Internal QuestionsDokumen4 halamanG-3 L-17 Internal QuestionsActivity MLZS BarhBelum ada peringkat