Hydrophobic and Fibrillar Microporous PDF
Diunggah oleh
Liviu VlejuDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Hydrophobic and Fibrillar Microporous PDF
Diunggah oleh
Liviu VlejuHak Cipta:
Format Tersedia
Hydrophobicand fibrillar microporous
polyetherurethaneurea prosthesis:
an ESCAstudy on the internal and
external surfaces of explantedgrafts
Marie Therrien, Robert Guidoin,AlainAdnotand Roy&onPaynter*
Biomaterials
Unit,
Quebec
Quebec
City,
(Received
St-Franqois
dAssise
G 1 K 7P4,
13 March
1989;
Hospital
and
Departments
of Surgery
and
Chemical
Engineering,
Lava1 University,
Canada
revised
18 May
1989;
accepted
2 1 June
1989)
The ESCA study gives a good qualitative and quantitative elemental analysis of internal and external
surfaces of foreign materials. Microporous hydrophobic Mitrathane@ (a polyetherurethane urea) grafts
were implanted as blood conduits in dogs for up to 6 month. Surface analysis of explanted grafts
demonstrated the presence of different contaminants: sodium, chlorine, silicon, in patent grafts, i.e. those
implanted for 1 month and less. The sulphur probably comes from the presence of proteins on the surface of
the polymer and the high level of nitrogen is also protein-related. At 6 month implantation, the grafts were
occluded and a decrease of proteins on the surface was observed. The values of N/C and O/C ratios are also
reported. For the virgin material, these ratios correspond to the quantity of hard and soft segments; but, for
the explanted grafts, these parameters are also influenced by the presence of proteins due to the
VersaclearP washing which did not wash away all the proteins on the surface of the polymer. The SEM
photographs showed a certain degradation of polyurethane after 6 month of implantation. However, by
ESCA study, it is difficult to compare the surface of virgin and explanted grafts because it is masked by the
presence of proteins.
Keywords:
Vascular
Textile polyester
prostheses,
success
record
(ePTFE)
vein
diameter.
Possessing
relatively
blood-compatible
have
developed
produced
in
connected;
2PO.
1989
of
and
involved
vessels
<6
vitro
flexible
mm
in
segmented
poly-
the
wall
(Wheat
Ridge,
and hydrophobic
The
control
The
porosity
of
phase
second
one
CO,
of
the
on the opposite,
1 and 2). An X-ray
during
INRS-Energle,
the internal
1020,
The
These
were
were
not
one
spectro-
urethane
from
surfaces
the
vivo
the
polyurethane
for periods
graft in
of up to 6
of explanted
grafts.
City,
METHODS
Quebec
were
fabricated
elastomer
that
polyurethane
provided
on a rotating
previously
were
substitutes
for the following
1 month
implantations
been
implanted
and
were
reported
by
in dogs
as
performed
For each
in duplicate.
elsewhere9
can
be
et
Inc.
of poly-
a method
Annis
prescheduled
month.
grafts
Medica
spinning
mandril,
described
vascular
by Matrix
by electrostatic
prostheses
have
Et Co (Publishers)
in
implanted
on the results of ESCA analysis on
microporous
mandril.
Quebec
of
we
material
in diameter
of the hydrophobic
Varennes,
hydrophobic
aorta substitutes
AND
Hydrophobic
1 wk.
C.P.
prostheses,
and external
5 mm
Canada.
Butterworth
dogs as infrarenal
by
fabricated
photo-electron
understanding
is
to Dr R. Guidoln.
address:
microporous
Synthetic
separation
model
better
been
has
one
hydrophilic
those
USA)
polyetherurethane
of the PEUU on a rotating
has already
model*.
of small
of the first
was
Mitrathane@
of polyurethane
month. This paper focuses
properties,
production
obtain
behaviour
Mitrathane
of the autologous
in
in the
has yet
of hydrophilic
on the hydrophilic
To
and large
graft
study
published
MATERIALS
Inc.
(PEUU).
spinning
Correspondence
been
the
(Figures
*Present
repair
outstanding
hydrophilic
manufacturing6,
were
the
Medica
by
electrostatic
JOL
for
prostheses
pores
scopy
a good
blood conduits3-5.
Matrix
urea
vascular
the performance
saphenous
have
of medium
but no synthetic
been able to challenge
diameter
prostheses
for the replacement
arteries
urethanes
biodegradation
grafts, either woven or knitted and expanded
polytetrafluoroethylene
diameter
ESCA,
adapted
a/.3.
The
infrarenal
aorta
periods:
24 h,
period
of time,
Results
which
summarized
as
Ltd. 0142-9612/89/080517-04$03.00
Biomatenals
1989,
Vol
10 October
517
ESCA analysis on explanted grafts: M. Therrien et al.
follows: at death, all but the two grafts implanted for 6
month were patent. After 1 month implantation, all PEUU
grafts were yellow stained on both internal and external
surfaces and 6 month after implantation, the yellow
colouration was more evident (Figure 3), but proteins were
less abundant than at 1 month. Washing was sufficient to
remove most of the proteins.
Graft processing
The explanted samples were washed in Versaclean@ (Fisher
Scientific, Montreal, Quebec, Canada), a colloidal laboratory
detergent, after a first washing in a physiological saline
solution (30 min), then in distilled water (three 5 min
washes). This was followed by a 16 h wash in 5%
Versaclean, a 7 min distilled water wash and a 1 h wash in
12.5% Versaclean. Before going through the graded alcohol
series and critical point drying, the samples were again
rinsed in distilled water for 90 min (four changes).
ESCA study
Virgin samples were investigated in a SSX-100 spectrometer
(Surface Science Laboratories, Mountain View, CA, USA) at
Surface Science Western University of the University of
Western Ontario Canada. This instrument features a focused
monochromatic AlKa X-ray beam which is aligned with a
specific area of the sample surface using a fixed-focus
microscope. The explanted prostheses were evaluated on a
VG ESCA Lab MK2 (VG Scientific, East Grinstead, West
Figure 1 The SEM photographs of external surface (a) and transverse cut
(b) of virgin hydrophilic Mitrathane? Note that the microporous structure is
achieved by closed ceiled pores.
Figure 2
The SEM photographs of external surface (a) and transverse cut
(b) of virgin hydrophobic Mitrathane? The porosity is visible and the pores
communicate.
518
Biomaterials
1989, Vol 10 October
Figure 3
The macroscopic photographs
of explanted
hydrophobic
Mitrathane@ after I month (a) and 6 month (b) implantation. The yellow
staining is more evident after 6 month of implantation.
ESCA
Sussex, UK) which
University.
features
a MgKa
beam
at Lava1
RESULTS
In Table 1, the values for the apparent surface composition of
the prostheses are reported. Carbon, nitrogen and oxygen
are the major components of the polyurethane and sodium,
chlorine, silicon and sulphur are the minor elements
deposited on the surfaces. These components are due to
contamination during the preparation of the grafts and/or to
implantation.
The N/C and O/C ratios were calculated. The values
for the virgin and explanted polyurethane are presented in
Table 2.
In Tab/e 3, the estimated compositions of reference
proteins are reported. The percentage of carbon, nitrogen,
oxygen and sulphur are presented for a comparison with the
values of polyurethane.
DISCUSSION
Blood polyurethane interactions are affected by the surface
Table
Apparent
surface
composition
of prostheses
Time of
implantation
Surface
Na
Cl
SI
Internal
External
80
79
2
2
24 h
Internal
External
71
70
1 wk
Internal
External
1 month
6 month
17
19
1
P
8
10
20
19
0.1
-
0.5
0.4
73
19
0.2
0.2
Internal
External
69
75
10
6
20
19
0.2
0.2
0.1
-
0.1
0.2
0.2
Internal
External
76
74
4
6
19
20
0.2
*Present
Table 2
Results
of N/C
and
O/C
ratios
of prostheses
Time of
Implantation
Surface
Internal
External
80
79
24 h
Internal
External
71
70
1 wk
Internal
External
73
1 month
Internal
External
69
75
6 month
Internal
External
76
74
4
6
Table 3
Estimated
composition
N/C
o/c
2
2
17
19
0.03
0.03
0.21
0.24
8
10
20
19
0.1 1
0.14
0.28
0.27
19
0.10
0.26
10
6
20
19
0.14
0.08
0.29
0.25
19
20
0.05
0.08
0.25
0.27
of reference
materials
(proteinsJ
Protein
AlbumIn
Haemoglobin
Fibrinogen
y-globulin
65
65
67
63
14
14
12
14
18
18
20
23
2
3
1
ND
ND: no data.
analysis
on explanted
grafts:
M.
Therrien
et al.
properties of the polymer. ESCA studies allow a surface
analysis of virgin and explanted samples; their depth of
analysis is between 1 and 10 nm. The basis of the surface
analysis of polyurethanes is that the surface properties of a
polyurethane represent the sum of the effects of all the
chemical groups on the surface.
An ESCA study gives a good qualitative and quantitative
elemental analysis of the internal and external surfaces of
polyurethane grafts. In Tab/e 1, the percentage of elements
is reported. The first columns (C, N and 0) represent
concentrations of major elements and other columns
(Na
.S) show concentrations of minor components
calculated from survey scans. Sodium and chlorine are
common contaminants on many biomaterials. Silicon may
originate from polysiloxane, a mould-release agent used
during the manufacturing of the graft. The presence of
sulphur probably comes from the proteins on the surface of
the prosthesis. If we compare the percentages of sulphur on
virgin and explanted hydrophobic Mitrathane, we see some
differences that indicate the possible presence of proteins.
Furthermore, the concentration of nitrogen is higher for
explanted polyurethane than for virgin polyurethane and
sulphur seems more abundant on explanted grafts. Also, it
can be seen that the silicon found as a contaminant on the
virgin material is masked by adsorbed proteins on the
surfaceof explanted polyurethane. Finally, uponexamination
of Tab/e 3, we can conclude that the values for plasma
proteins are near the values of explanted Mitrathane.
For a period of 6 month implantation, a diminution of
proteins on the surface was observed. Parallel histological
studies9 showed fibrin and infiltration of blood elements into
the Mitrathane graft at 24 h, and at 1 wk. At 1 month, a thin
internal capsule was present on the graft flow surface of the
prosthesis. However, at 6 month, a complete occlusion
occurred. Most thrombi were anchored to the anastomoses
and were found to be non-adherent to the graft surface. This
is an explanation for the diminution of proteins.
Polyurethane is composed of soft and hard segments.
Soft segments come from polyether groups and hard
segments from urethane-urea groups. Biocompatibility of
biomaterials is due in part to alternation of soft and hard
segments. If the polymer has a lot of soft segments, its
surface is exposed to adsorption of proteins and conformational variations of fibrinogen and to a degradation of the
polymer. On the other hand, if a polymer has more hard
segments, the biocompatibility is much better because the
secondary amide groups, present in hard segments, form
reversible hydrogen bonds with peptide bonds in fibrinogen.
In Tab/e 2, the values for N/C and O/C ratios are
reported. For the virgin sample, the N/C ratio corresponds to
quantity of hard segments and the O/C ratio to the quantity
of soft segments. The soft segment concentration is high for
the virgin Mitrathane graft and the flow surface (internal) of
the prosthesis has more hard segments. Now, thecomparison
of these values (O/C and N/C) for the virgin and explanted
grafts is difficult because, for the explanted polyurethane
grafts, these results correspond rather to the presence of
proteins. For this reason, it is not yet possible to comment on
the increase or decrease of soft and hard segments on the
surface of explanted polyurethane grafts because the protein
layer masks the surface of the polymer.
CONCLUSION
The use of ESCA appeared to be the most appropriate
method for analysis of the internal and external surfaces of
Biomaterials
7989,
Vol
10 October
519
ESCA analysis on explanted grafts: M. Therrien er al.
polymer and allow a better understanding of the phenomenon
of degradation.
ACKNOWLEDGEMENTS
This work was supported by the Medical Research Council of
Canada (Grant MA 9429). The authors are indebted to
K. Horth and Y. Marois for their collaboration. The grafts
were kindly provided by Matrix Medica Inc.
REFERENCES
1
Figure 4
The SEM photograph of external surface of hydrophobic
Mitrarhane after 6 monrh of implantation. Nora the presence of biological
debris on the flow surface and some broken fibriis in the PU srrucrure.
vascular grafts because the penetration is only l-l 0 nm.
The results for the virgin and explanted hydrophobic
Mitrathane confirmed that these prostheses were submitted
to a surface degradation and/or an adsorption of proteins
during the implantation (Figure 4). The Versaclean washing
seems to be the best detergent for removal of most of the
proteins without changing the surface of polymer. The
scanning electron microscopy (SEM) photographs showed a
certain degradation of polyurethane after 6 month implantation. However, by ESCA study, it is difficult to compare the
surface of virgin and explanted grafts because it is masked
by the presence of proteins. To complete these findings,
other possible experimentation and analysis would be
necessary such as Fourier Transform Infrared-Attenuated
Total Reflectance (FTIR-ATR) (a surface analysis method
with a depth of 1000 nm) to see the infrared bands of
proteins and polymer. Differential Scanning Calorimetry
(DSC) could also be used to determine the glass transition
temperatures and melting temperatures of virgin and
explanted polyurethane which would characterize the
520
Biomaterials
1989, Vol 10 October
10
DeBakey, M., The development of vascular surgen/, Am. J. Surg.
1979.137.697-738
Reichle. F.A., Criteria for evaluation of new arterial prosthesis by
comparing vein with Dacron femoro-popliteal bypass, Surg. Gyn.
Obsrer. 1978. 146. 7 14-720
Annis, D., Bomat, A., Edwards, R.O., Higham, A.. Loveday, B. and
Wilson, J.. An elastomeric vascular prosthesis, Trans. Amer. Sot. Artif
lnr. Org. 1978, 24, 209-2 14
Leidner, J., Wong, E.W.C., MacGregor, D.C. and Wilson, G.J.. A novel
process for the manufacturing of porous grafts: process description
and product eva1uation.J. Biomed. Marer. Res. 1983,17,229-247
Hess, F.. Jerusalem, D.. Braun, B. and Grande, P.. Evaluation of the
patency rate of fibrous microvascular polyurethane prostheses after
implantation in the rat aorta, Microsurgery 1983, 4, 178-l 81
Gilding, D.K., Reed, A.M., Askill, I.N. and Eriana, S., Mitrathane? a
new polyether-urethane-urea for critical medical applications, Trans.
Amer. Sot. Artif lnr. Org. 1984, 30. 57 l-576
Ives. CL., Zamora. J.L.. Eskin, S.G., Weilbaecher, D.G., Gao, Z.R.,
Noon, G.P. and DeBakey, M.E., In viva investigation of a new
elastomeric vascular graft (Mitrathane), Trans. Amer. Sot. Anif lnr.
Org. 1984,30,
587-590
Paynter. R.W., Martz, H. and Guidoin, R., An X-ray photoelectron
spectroscopy study of the external surface of explanted mrcroporous
polyurethane vascular prostheses, Biomaterials 1987, 8, 94-99
Marois. Y., Guidoin. R.. Bayer, D.. Assayed, F., Doillon, C., Faynter, R.
and Marois, M., In viva evaluation of hydrophobic and fibrillar
microporous polyetherurethane urea graft, Biomaterials 1989, 10,
521-531
Stupp. S.I.. Kauffman. J.W. and Carr, S.H., Interactions between
segmented polyurethane surfaces and the plasma protein fibrinogen,
J. Biomed. Mar. Res. 1977, 11, 237-250
Anda mungkin juga menyukai
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Frenkel-Kontorova Model - IntroductionDokumen5 halamanThe Frenkel-Kontorova Model - Introductionreal thinkerBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Exp 10 - Exp 7 A Green Synthesis of Camphor UploadDokumen4 halamanExp 10 - Exp 7 A Green Synthesis of Camphor UploadUyen V. NguyenBelum ada peringkat
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Basics of Thermal Power PlantDokumen35 halamanBasics of Thermal Power PlantMansoor Chowdhury100% (1)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
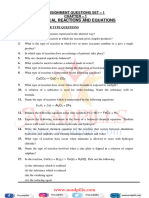
- Chemical Reactions and Equations Assignment Questions Set - 1Dokumen6 halamanChemical Reactions and Equations Assignment Questions Set - 1kayace8055Belum ada peringkat
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- SX2112Dokumen5 halamanSX2112AmenBelum ada peringkat
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- AQA GCSE Chem Combined End of Topic C1Dokumen9 halamanAQA GCSE Chem Combined End of Topic C1joeBelum ada peringkat
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Energy Conversion Technologies & HydrogenDokumen18 halamanEnergy Conversion Technologies & Hydrogenanon-530265100% (1)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Four Steps To Effective Pigment Dispersions Jadel Baptista DCC LanscoDokumen5 halamanFour Steps To Effective Pigment Dispersions Jadel Baptista DCC LanscoEyad AlsheiikhBelum ada peringkat
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Alat (GPT) Fs (Ifcc Mod.) : Mindray BS300Dokumen1 halamanAlat (GPT) Fs (Ifcc Mod.) : Mindray BS300armasfernandoBelum ada peringkat
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- Finalreport PDFDokumen47 halamanFinalreport PDFNelCamHerBelum ada peringkat
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- NAAMM EMMA 557-20 Standards For Expanded MetalDokumen18 halamanNAAMM EMMA 557-20 Standards For Expanded MetalScott NorrisBelum ada peringkat
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Environmental Chemistry and Microbiology - Unit 3 - Week 1Dokumen6 halamanEnvironmental Chemistry and Microbiology - Unit 3 - Week 1Abhijit NathBelum ada peringkat
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Herbert Brown and Edward N. Peters' : Abstract: 80% or (503 000)Dokumen5 halamanHerbert Brown and Edward N. Peters' : Abstract: 80% or (503 000)Liz HansBelum ada peringkat
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- EmileorConcerningEducation 10106815Dokumen165 halamanEmileorConcerningEducation 10106815Túlio Coelho SampaioBelum ada peringkat
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- Factors Influencing ToxicityDokumen7 halamanFactors Influencing ToxicityderrickBelum ada peringkat
- Module 6 - Ash, Water, Extractive and Crude Fiber Content DeterminationDokumen23 halamanModule 6 - Ash, Water, Extractive and Crude Fiber Content DeterminationPRINCESS NOELLEE TRAYVILLABelum ada peringkat
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Exergoeconomic Analysis of A Combined Heat and Power (CHP) SystemDokumen17 halamanExergoeconomic Analysis of A Combined Heat and Power (CHP) Systemjhugo_mirandaBelum ada peringkat
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Palm Oil RefiningDokumen10 halamanPalm Oil Refiningharrison_sBelum ada peringkat
- 2nd COTdetailedDokumen6 halaman2nd COTdetailedfe delgadoBelum ada peringkat
- Carbohydrates - Specific ReactionsDokumen5 halamanCarbohydrates - Specific ReactionsVanessa ParaisoBelum ada peringkat
- 025welding Engineering An Introduction - (2.5 Plasma Arc Welding)Dokumen3 halaman025welding Engineering An Introduction - (2.5 Plasma Arc Welding)Kamarul NizamBelum ada peringkat
- Benzop 092020 TRDokumen89 halamanBenzop 092020 TRAnakaya IRABelum ada peringkat
- Fire Resistant 08Dokumen36 halamanFire Resistant 08mehdi227Belum ada peringkat
- Basics of RadiobiologyDokumen61 halamanBasics of RadiobiologyLikhon Amin AponBelum ada peringkat
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Green Roof Energy SimulationDokumen11 halamanGreen Roof Energy SimulationAnas Khalid TahirBelum ada peringkat
- Catalogo Tecnico ING Plattella - UltimateDokumen16 halamanCatalogo Tecnico ING Plattella - UltimateVladimirBelum ada peringkat
- Worksheet Cellular Respiration#2 - Ch9 PDFDokumen6 halamanWorksheet Cellular Respiration#2 - Ch9 PDFTaniaBarrios-ChongBelum ada peringkat
- Void Swelling StraalsundDokumen7 halamanVoid Swelling StraalsundAzif Ali MoothantevileyilBelum ada peringkat
- Astm A53 A53mDokumen23 halamanAstm A53 A53mRaviprakash Chauhan100% (2)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)