Criteria For The Diagnosis of Acute Myocardial Infarction
Diunggah oleh
alexandraossesJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Criteria For The Diagnosis of Acute Myocardial Infarction
Diunggah oleh
alexandraossesHak Cipta:
Format Tersedia
2/21/12
Criteria for the diagnosis of acute m ocardial infarction
Official reprint from UpToDate www.uptodate.com
2012 UpToDate
Criteria for the diagnosis of acute m ocardial infarction
Authors
Guy S Reeder, MD
Harold L Kennedy, MD, MPH
Section Editors
Christopher P Cannon, MD
James Hoekstra, MD
Allan S Jaffe, MD
Deput Editor
Gordon M Saperia, MD, FACC
Disclosures
All topics are updated as new evidence becomes available and our peer review process is complete.
Literature review current through: ene 2012. | This topic last updated: jun 14, 2011.
INTRODUCTION Myocardial infarction (MI) is defined as a clinical (or pathologic) event caused
by myocardial ischemia in which there is evidence of myocardial injury or necrosis [1,2]. Criteria are
met when there is a rise and/or fall of cardiac biomarkers, along with supportive evidence in the
form of typical symptoms, suggestive electrocardiographic changes, or imaging evidence of new
loss of viable myocardium or new regional wall motion abnormality.
Initial care of the patient with suspected acute myocardial infarction (MI) should include the early
and simultaneous achievement of four goals:
Confirmation of the diagnosis by electrocardiogram (ECG) and biomarker measurement
Relief of ischemic pain
Assessment of the hemodynamic state and correction of abnormalities that may be present
Initiation of antithrombotic and reperfusion therapy if indicated
The management of patients with an ST segment elevation (Q wave) MI or non-ST segment
elevation acute coronary syndrome (ACS) is discussed elsewhere. (See "Overview of the acute
management of acute ST elevation myocardial infarction" and "Overview of the acute management
of unstable angina and acute non-ST elevation myocardial infarction".)
A related issue is the evaluation of a patient who presents with chest pain suggestive of an ACS in
whom the initial evaluation (ECG, cardiac enzymes) is not diagnostic. This issue is discussed
separately. (See "Initial evaluation and management of suspected acute coronary syndrome in the
emergency department", section on 'Observation'.)
DEFINITIONS
Acute coronar s ndrome The term acute coronary syndrome (ACS) is applied to patients in
whom there is a suspicion of myocardial ischemia. There are three types of ACS: ST elevation
(formerly Q-wave) MI (STEMI), non-ST elevation (formerly non-Q wave) MI (NSTEMI), and unstable
angina (UA). The first two are characterized by a typical rise and/or fall in biomarkers of myocyte
injury [3].
Two multicenter, international surveys published in 2002 - the Euro Heart Survey and the GRACE
registry - determined the relative frequency of these disorders in approximately 22,000 patients
admitted with an ACS [4,5]. STEMI occurred in 30 to 33 percent, NSTEMI in 25 percent, and UA in
38 to 42 percent.
Acute MI For many years, the diagnosis of acute MI relied on the revised criteria established
by the World Health Organization (WHO) in 1979 [6]. These criteria were epidemiological and aimed
www.uptodate.com/contents/criteria-for-the-diagnosis-of-acute-m ocardial-infarction?view=print
1/20
2/21/12
Criteria for the diagnosis of acute m ocardial infarction
at specificity. A joint European Society of Cardiology (ESC) and American College of Cardiology
(ACC) committee proposed a more clinically based definition of an acute, evolving, or recent MI in
2000 [1]. In 2007 the Joint Task Force of the European Society of Cardiology, American College of
Cardiology Foundation, the American Heart Association, and the World Health Federation
(ESC/ACCF/AHA/WHF) refined the 2000 criteria and defined acute MI as a clinical event consequent
to the death of cardiac myocytes (myocardial necrosis) that is caused by ischemia (as opposed to
other etiologies such as myocarditis or trauma) [2].
The criteria used to define MI differ somewhat depending upon the particular clinical circumstance
of the patient: those suspected of acute MI based upon their presentation, those undergoing either
coronary artery bypass graft surgery or percutaneous intervention, or those who have sustained
sudden unexpected, cardiac arrest with or without death [2]. (See 'After revascularization' below.)
For patients who have undergone recent revascularization or who have sustained cardiac arrest or
death, the criteria for the diagnosis of MI are given in detail in the table (table 1).
For all other patients in whom there is a suspicion of MI, a typical rise and/or gradual fall (troponin)
or more rapid rise and fall (CK-MB) of biochemical markers of myocardial necrosis, with at least one
of the following is required:
Ischemic symptoms
Development of pathologic Q waves on the ECG
ECG changes indicative of ischemia (ST segment elevation or depression)
Imaging evidence of new loss of viable myocardium or a new regional wall motion abnormality.
In addition, pathologic findings (generally at autopsy) of an acute MI are accepted criteria.
The joint task force further refined the definition of MI by developing a clinical classification
according to the assumed proximate cause of the myocardial ischemia:
Type 1: MI consequent to a pathologic process in the wall of the coronary artery (e.g. plaque
erosion/rupture, fissuring, or dissection)
Type 2: MI consequent to increased oxygen demand or decreased supply (e.g. coronary
artery spasm, coronary artery embolus, anemia, arrhythmias, hypertension or hypotension)
Type 3: Sudden unexpected cardiac death before blood samples for biomarkers could be
drawn or before their appearance in the blood
Type 4a: MI associated with percutaneous coronary intervention
Type 4b: MI associated with stent thrombosis
Type 5: MI associated with coronary artery bypass graft surgery
Unstable angina Unstable angina (UA) is considered to be present in patients with ischemic
symptoms suggestive of an ACS without elevation in biomarkers with or without ECG changes
indicative of ischemia. Due to the insensitivity of CK-MB compared to troponin, one must be
circumspect if that is the only biomarker available. Elevations of troponin with contemporary assays
probably take two to three hours, while elevations for CK-MB take longer. (See 'Cardiac
biomarkers' below.)
UA and NSTEMI are frequently indistinguishable at initial evaluation. ST segment and/or T wave
www.uptodate.com/contents/criteria-for-the-diagnosis-of-acute-m ocardial-infarction?view=print
2/20
2/21/12
Criteria for the diagnosis of acute m ocardial infarction
changes are often persistent in NSTEMI while, if they occur in UA, they are usually transient.
Regardless, of the category, ST segment change defines a higher-risk group [7].
After revasculari ation Following revascularization with either coronary artery bypass graft
surgery (CABG) or percutaneous coronary intervention (PCI) cardiac biomarkers may rise. Transient
elevations in troponins may represent necrosis, although the mechanism is unknown. Higher
elevations are associated with worse prognosis after CABG. A discussion of MI following PCI is found
elsewhere. (See "Periprocedural myocardial infarction following percutaneous coronary
intervention".)
The Joint ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction addressed
the issue of biomarker rise after revascularization procedures [2]. They state that for patients
undergoing PCI who have normal baseline troponin value (99th percentile URL) is mandatory in order
to use the definition below. If the baseline value is elevated or rising, it is impossible to tell if
elevations postprocedure are related to the initial insult or to additional injury. However, they also
state that if the troponin values are stable or falling before revascularization, the use of the
reinfarction criteria may be reasonable. We also believe it is reasonable to obtain a troponin prior
and proximate (within six hours at the outside) to PCI (baseline value). (See 'Recommended
approach' below.)
No criteria have been established to separate expected rises (such as needle trauma to the
myocardium at CABG) from those that represent a complication of the procedure (such as
unexpected coronary artery dissection due to wire trauma at PCI) [8]. In addition, the cut points
given below are controversial.
The definition of (periprocedural) myocardial infarction after revascularization requires a normal
baseline troponin (99th percentile URL) and is as follows below [2]:
Type 4a (associated with PCI): Increases of biomarkers greater than three times the 99th
percentile URL.
Type 4b: Increases of biomarkers associated with stent thrombosis as documented by
angiography or at autopsy.
Type 5 (associated with CABG): Increases of biomarkers greater than five times the
99th percentile URL plus either new pathological Q waves or new LBBB, or angiographically
documented new graft or native coronary artery occlusion, or imaging evidence of new loss of
viable myocardium.
Prior MI
Any one of the following three criteria satisfies the diagnosis for a prior (established) MI (table
1) [2]:
Development of pathologic Q waves (0.04 sec) on serial ECGs. The patient may or may not
remember previous symptoms. Biochemical markers of myocardial necrosis may have
normalized, depending upon the length of time that has passed since the MI occurred.
Pathologic findings of a healed or healing MI.
Evidence from an imaging study of a region of loss of viable myocardium that is thinned and
fails to contract, in the absence of a nonischemic cause. (See "Role of echocardiography in
acute myocardial infarction", section on 'Diagnosis of MI'.)
www.uptodate.com/contents/criteria-for-the-diagnosis-of-acute-m ocardial-infarction?view=print
3/20
2/21/12
Criteria for the diagnosis of acute m ocardial infarction
INITIAL EVALUATION For a patient presenting with a suspected acute MI, the characteristics
of the chest pain and the ECG findings permit initial risk stratification. An ECG and an abbreviated
history and physical examination should be obtained within 10 minutes of patient arrival [9]. Other
steps in the immediate management of patients suspected of an acute MI are discussed separately
(see "Initial evaluation and management of suspected acute coronary syndrome in the emergency
department", section on 'Immediate ED interventions').
The history should be targeted toward pain duration, character, similarity to possible previous
episodes, provoking factors, and past history of coronary disease risk factors. The physical
examination (including auscultation of the heart and lungs, measurement of blood pressure in both
arms, and assessment for heart failure or circulatory compromise, which are associated with a high
early mortality).
Patients with a strong clinical history and ST segment elevation or new left bundle branch block
should be assumed to have an acute MI and undergo immediate reperfusion therapy. (See
"Selecting a reperfusion strategy for acute ST elevation myocardial infarction".)
"Ruling in" an acute MI with newer troponin assays occurs in 80 percent of patients by two to three
hours after presentation; "ruling out" may take longer (up to six hours) (see 'Cardiac
biomarkers' below).
CHEST PAIN While chest pain is not required for the diagnosis of MI, its presence, particularly if
characteristic for myocardial ischemia, may influence decision making about the likelihood of the
presence of MI (table 2). A discussion of the characteristic of ischemic chest pain is found
elsewhere. (See "Diagnostic approach to chest pain in adults", section on 'Description of chest
pain'.)
Present Among patients with chest pain characteristic of myocardial ischemia (angina pectoris),
there are three primary presentations that suggest a change in the anginal pattern as ACS as
opposed to stable or exertional angina [3]:
Rest angina, which is usually more than 20 minutes in duration
New onset angina that markedly limits physical activity
Increasing angina that is more frequent, longer in duration, or occurs with less exertion than
previous angina
Absent Patients without features of typical angina are more likely to have another cause of
chest pain. Common causes include other cardiovascular, pulmonary, and gastrointestinal disorders
(table 3). (See "Diagnostic approach to chest pain in adults" and "Differential diagnosis of chest
pain in adults".)
In a review of over 430,000 patients with confirmed acute MI from the National Registry of
Myocardial Infarction 2, one-third had no chest pain on presentation to the hospital [10]. These
patients may present with dyspnea alone, nausea and/or vomiting, palpitations, syncope, or cardiac
arrest. They are more likely to be older, diabetic, and women. (See "Clinical features and diagnosis
of coronary heart disease in women".)
The absence of chest pain has important implications for therapy and prognosis. In the Registry
report, patients without chest pain were much less likely to be diagnosed with a confirmed MI on
admission (22 versus 50 percent in those with chest pain) and were less likely to be treated with
appropriate medical therapy and to receive fibrinolytic therapy or primary angioplasty (25 versus 74
percent) [10]. Not surprisingly, these differences were associated with an increase in in-hospital
mortality (23.3 versus 9.3 percent, adjusted odds ratio 2.21, 95 percent confidence interval 2.17 to
2.26).
www.uptodate.com/contents/criteria-for-the-diagnosis-of-acute-m ocardial-infarction?view=print
4/20
2/21/12
Criteria for the diagnosis of acute m ocardial infarction
ECG The electrocardiogram (ECG) is a mainstay in the initial diagnosis of patients with suspected
ACS. It allows initial categorization of the patient with a suspected MI into one of three groups
based on the pattern:
ST elevation MI (ST elevation or new left bundle branch block)
non-ST elevation ACS, with either NSTEMI or UA (ST-depression, T wave inversions, or
transient ST-elevation)
Undifferentiated chest pain syndrome (nondiagnostic ECG)
The 2004 ACC/AHA guideline on ST myocardial infarction (and the 2007 focused update) concluded
that it is reasonable for emergency medical service (EMS) personnel with advanced cardiac life
support training to perform and evaluate a 12-lead ECG on a patient suspected of having an acute
MI [9,11]. (See "Overview of the acute management of acute ST elevation myocardial infarction".)
ST elevation MI In patients with acute ST elevation MI, the electrocardiogram evolves through
a typical sequence. (See "Electrocardiogram in the diagnosis of myocardial ischemia and
infarction" and "ECG tutorial: Myocardial infarction".)
Although not frequently seen, the earliest change in an STEMI is the development of a hyperacute
or peaked T wave that reflects localized hyperkalemia. Thereafter, the ST segment elevates in the
leads recording electrical activity of the involved region of the myocardium; it has the following
appearance:
Initially, there is elevation of the J point and the ST segment retains its concave
configuration.
Over time, the ST segment elevation becomes more pronounced and the ST segment
becomes more convex or rounded upward.
The ST segment may eventually become indistinguishable from the T wave; the QRS-T
complex can actually resemble a monophasic action potential.
The joint ESC/ACCF/AHA/WHF committee for the definition of MI established specific ECG criteria for
the diagnosis of ST elevation MI, which include 2 mm of ST segment elevation the precordial leads
for men and 1.5 mm for women (who tend to have less ST elevation) and greater than 1mm in other
leads (table 4) [12]. An initial Q wave or abnormal R wave develops over a period of several hours
to days. Specific ECG criteria were also established for the diagnosis of a prior myocardial infarction
(table 5).
Over time there is further evolution of these ECG changes; the ST segment gradually returns to the
isoelectric baseline, the R wave amplitude becomes markedly reduced, and the Q wave deepens. In
addition, the T wave becomes inverted. These changes generally occur within the first two weeks
after the event, but may progress more rapidly, within several hours of presentation.
In addition to patients with ST elevation on the ECG, two other groups of patients with an acute
coronary syndrome are considered to have an STEMI: those with new or presumably new left
bundle branch block and those with a true posterior MI. (See 'Bundle branch block or paced
rhythm' below and "Electrocardiogram in the diagnosis of myocardial ischemia and infarction",
section on 'Posterior wall MI'.)
A separate issue, the assessment of patients with a suspected acute MI who have known left
bundle branch block or a paced rhythm, is discussed below. (See 'Bundle branch block or paced
rhythm' below.)
Absence of Q waves A subset of patients who present with initial ST segment elevation, do
www.uptodate.com/contents/criteria-for-the-diagnosis-of-acute-m ocardial-infarction?view=print
5/20
2/21/12
Criteria for the diagnosis of acute m ocardial infarction
not develop Q waves. These patients are treated for an ST elevation MI. Such patients have a
better prognosis than those who develop Q waves because of more frequent reperfusion, a less
severe infarction, and, at follow-up, better left ventricular function and improved survival. (See
"Electrocardiogram in the prognosis of myocardial infarction or unstable angina", section on
'Presence or absence of new Q waves'.)
Locali ation The electrocardiogram can be used to localize the MI, and at times, predict the
infarct-related artery. These issues are discussed separately. (See "Electrocardiogram in the
diagnosis of myocardial ischemia and infarction".)
If there is electrocardiographic evidence of inferior wall ischemia (ST or T wave changes in leads II,
III, and aVF), the right-sided leads V4R, V5R, and V6R should also be obtained to evaluate the
possibility of right ventricular infarction. The recording of right-sided leads in this setting was given
a class I recommendation by the 2004 ACC/AHA task force [9]. No changes to this approach were
made in the 2007 focused update of the 2004 ACC/AHA guidelines for the management of patients
with ST-elevation MI [11]. Posterior leads (V7-9) are also indicated for those who present with ST
segment depression in the inferior leads to evaluate the possibility of posterior infarction [13].
Other causes of ST elevation and Q waves Although ST segment elevation and Q waves
are consistent with acute MI (particularly if new), each alone can be seen in other disorders (table
6 and table 7). As examples, ST segment elevation can occur in myocarditis, acute pericarditis,
patients with old MI and persistent ST segment elevation often associated with wall motion
abnormalities, and with the early repolarization variant, and Q waves can be seen in hypertrophic
cardiomyopathy. (See "Electrocardiogram in the diagnosis of myocardial ischemia and infarction" and
"Pathogenesis and diagnosis of Q waves on the electrocardiogram" and "Clinical manifestations and
diagnosis of myocarditis in adults".)
Non-ST elevation ACS A non-ST elevation ACS is manifested by ST depressions and/or T wave
inversions without ST segment elevations or pathologic Q waves. These ST-T wave abnormalities
may be present diffusely in many leads; more commonly they are localized to the leads associated
with the region of ischemic myocardium. (See "Electrocardiogram in the diagnosis of myocardial
ischemia and infarction".)
As noted above, the two forms of non-ST elevation ACS (UA and NSTEMI) are frequently
indistinguishable at initial evaluation (prior to biomarker elevation). In a patient with an NSTEMI, ST
segment depressions usually evolve over the subsequent few days to result in residual ST segment
depression and T wave inversions, but not to the formation of pathologic Q waves. In a patient
with UA, ST segment and T wave changes usually resolve completely.
Nondiagnostic initial ECG The initial ECG is often not diagnostic in patients with MI. In two
series, for example, the initial ECG was not diagnostic in 45 percent and normal in 20 percent of
patients subsequently shown to have an acute MI [14,15]. In patients clinically suspected of
having an acute MI in whom the ECG is nondiagnostic, it is recommended that the ECG should be
repeated at 20 to 30 minute intervals for any patient with ongoing pain in whom the suspicion of
ACS remains high. In some patients, initially nondiagnostic electrocardiographic changes will evolve
into ST elevation or ST depression [14,16].
The efficacy of repeated ECGs was addressed in a study of 1000 patients presenting to the
emergency department with chest pain in whom serial ECGs were obtained every 20 minutes for an
average of two hours. Serial ECGs were equally specific (95 percent) but more sensitive than an
initial single ECG for detecting an acute MI (68 versus 55 percent) [14].
Bundle branch block or paced rh thm Both left bundle branch block (LBBB), which is present
in approximately 7 percent of patients with an acute MI [17], and pacing can interfere with the
www.uptodate.com/contents/criteria-for-the-diagnosis-of-acute-m ocardial-infarction?view=print
6/20
2/21/12
Criteria for the diagnosis of acute m ocardial infarction
electrocardiographic diagnosis of MI or coronary ischemia. Of note, approximately one-half of
patients with LBBB and an acute MI do not have chest pain [18]. New right bundle branch block,
while generally not interfering with the electrocardiographic diagnosis of STEMI, connotes an
adverse prognosis similar in degree to LBBB.
Patients with LBBB, compared to those without bundle branch block, are much less likely to receive
aspirin, beta blockers, and reperfusion therapy [17,18], particularly if they present without chest
pain [18]. Similar observations have been made in patients with a paced rhythm [19].
Careful evaluation of the ECG may show some evidence of coronary ischemia in patients with LBBB
or a paced rhythm. However, the clinical history and cardiac enzymes are of primary importance in
diagnosing MI in this setting. (See "Electrocardiographic diagnosis of myocardial infarction in the
presence of bundle branch block or a paced rhythm".)
CARDIAC BIOMARKERS A variety of biomarkers have been used to evaluate patients with a
suspected acute MI. The cardiac troponins I and T as well as the MB isoenzyme of creatine kinase
(CK-MB) are the most frequently used.
The use of these tests is discussed in detail elsewhere, but the general principles will be briefly
reviewed here. Values 99 percentile of the upper reference limit (URL) should be considered
abnormal [2]. This value for troponin and CK-MB will vary depending on the assay used. (See
"Troponins and creatine kinase as biomarkers of cardiac injury".)
The following discussion will emphasize the diagnostic role of cardiac markers. These markers as
well as many other factors are important for risk stratification. These issues for both ST elevation
and non-ST elevation MI are discussed separately. (See "Risk stratification for cardiac events after
acute ST elevation myocardial infarction" and "Risk stratification after unstable angina or non-ST
elevation myocardial infarction" and "Risk factors for adverse outcomes after unstable angina or
non-ST elevation myocardial infarction".)
An elevation in the concentration of troponin or CK-MB is required for the diagnosis of acute MI
[1,2]. If both are measured and the troponin value is normal but the CK-MB is elevated, MB is likely
due to release from noncardiac tissue. Follow-up on such individuals reveals that they do extremely
well without subsequent events [20].
Troponin is the preferred marker for the diagnosis of myocardial injury because of their increased
specificity and better sensitivity compared to CK-MB [1,2,9]. The preferential use of cTnI or cTnT
for AMI diagnosis was recommended by 2007 joint ESC/ACCF/AHA/WHF task force for the definition
of myocardial infarction (table 1) [20]. (See "Troponins and creatine kinase as biomarkers of cardiac
injury".)
An elevation in cardiac troponins must be interpreted in the context of the clinical history and ECG
findings since it can be seen in a variety of clinical settings and is therefore not specific for an
acute coronary syndrome. (See 'Other causes of biomarker elevation' below and "Elevated cardiac
troponin concentration in the absence of an acute coronary syndrome".)
As there can be chronic elevations of troponin in patients who do not have acute events, the
guidelines emphasize the need for a changing pattern of values [1,2,21]. The magnitude of change
needed to operationalize this recommendation varies from assay to assay, so it is optimal when the
clinical laboratory helps to make these distinctions [22].
Three points should be kept in mind when using troponin to diagnose AMI:
With contemporary troponin assays, most patients can be diagnosed within two to three
hours of presentation [23].
www.uptodate.com/contents/criteria-for-the-diagnosis-of-acute-m ocardial-infarction?view=print
7/20
2/21/12
Criteria for the diagnosis of acute m ocardial infarction
A negative test at the time of presentation, especially if the patient presents early after the
onset of symptoms, does not exclude myocardial injury.
AMI can be excluded in most patients by six hours, but the guidelines suggest that, if there is
a high degree of suspicion of an ACS, a 12-hour sample be obtained. [1,2,9]. However, very
few patients become positive after eight hours [24].
Other causes of biomarker elevation Elevations of biochemical markers diagnose cardiac
injury, not infarction due to coronary artery obstruction [25]. If an ischemic mechanism of injury is
present, for example, as indicated by ischemic ECG changes, then an ACS is diagnosed.
Otherwise, other mechanisms for cardiac injury must be considered (eg, heart failure, rapid atrial
fibrillation, myocarditis, anthracycline cardiotoxicity, subendocardial wall stress, myopericarditis,
sepsis, etc). As an example, small amounts of cardiac injury can occur in critically ill patients, which
may or may not represent an AMI [26,27]. Troponin elevations also occur in chronic kidney disease.
(See "Elevated cardiac troponin concentration in the absence of an acute coronary syndrome".)
In the emergency department setting, life-threatening causes of chest pain with troponin elevation
not due to coronary artery disease are acute pulmonary embolism, in which troponin release may
result from acute right heart overload, myocarditis [25], and stress-induced cardiomyopathy. (See
"Diagnosis of acute pulmonary embolism" and "Clinical manifestations and diagnosis of myocarditis in
adults", section on 'Cardiac enzymes'.)
Absence of biomarker elevation Using older assays, some patients with STEMI who were
rapidly reperfused did not develop a cardiac biomarker elevation. These patients were called
"aborted MIs." With contemporary troponin assays, this does not occur or is extremely rare. For
example, in an analysis of 767 patients with STEMI, the frequency of patients who had elevations
of troponin above the 99th percent value was 100 percent [28]. For patients with ST elevation on
the electrocardiogram and no biomarker elevation one of the other causes of ST elevation should be
considered (table 6). (See 'Other causes of ST elevation and Q waves' above and "Fibrinolytic
(thrombolytic) agents in acute ST elevation myocardial infarction: Therapeutic use", section on
'Introduction'.)
Discordant cardiac en mes biomarkers At least one third of patients with an ACS have
elevated troponins but normal CK-MB [20,29-31]. The frequency and prognostic significance of
discordant troponin and CK-MB were illustrated in a review of almost 30,000 such patients from the
multicenter CRUSADE initiative in the United States [31]. The following findings were noted:
The results were discordant in 28 percent of patients despite the fact that many centers
were still using either high cut-off values or inadequately sensitive troponin assays. Troponin
was more sensitive, as 18 percent had elevated troponin but normal CK-MB values. In
addition, 10 percent had false positive CK-MB elevations, as defined by normal troponin
values.
Compared to patients who were negative for both biomarkers, in-hospital mortality was not
increased in patients who were Tn-negative and CK-MB-positive (ie, false positives; 3.0
versus 2.7 percent, adjusted odds ratio 1.02, 95% CI 0.75-1.38).
Compared to patients who were negative for both biomarkers, there was a nonsignificant
trend toward increased mortality in patients who were Tn-positive/CK-MB-negative (4.5
versus 2.7 percent, adjusted odds ratio 1.15, 95 percent CI 0.86-1.54) and a significant
increase in mortality in patients who were positive for both biomarkers (5.9 versus 2.7
percent, adjusted odds ratio 1.53, 95 percent CI 1.18-1.98). The latter finding reflects the
www.uptodate.com/contents/criteria-for-the-diagnosis-of-acute-m ocardial-infarction?view=print
8/20
2/21/12
Criteria for the diagnosis of acute m ocardial infarction
fact that patients with larger insults do worse [32]. The two discordant groups were treated
similarly with antithrombotic agents and percutaneous coronary intervention so differences in
outcomes are less likely to be explained by differences in therapy. Thus, an isolated CK-MB
elevation has limited prognostic value in patients with a non-ST elevation ACS. Several metaanalyses suggest that patients with isolated troponin elevations do much worse than those
without elevations [33,34]. If high cut-off values are used, these effects are obfuscated by
the admixture of patients with and without real troponin elevations.
Similar findings were noted among 1825 patients with a non-ST elevation ACS in the TACTICS-TIMI
18 trial in whom troponin T was measured; 668 (37 percent) had elevated CK-MB, almost all of
whom had elevated troponin T, while 361 patients (20 percent) had an elevated troponin T with
normal CK-MB [30]. The latter patients the greatest benefit from an early invasive strategy. (See
"Coronary arteriography and revascularization for unstable angina or non-ST elevation acute
myocardial infarction".)
Recommended approach The following general statements apply to the biochemical diagnosis
of an acute MI [2].
Troponins are the markers of choice and should be used instead of CK-MB except when postprocedural MI, where CK-MB may be more useful [1,2]. (See "Troponins and creatine kinase as
biomarkers of cardiac injury", section on 'Late diagnosis and reinfarction'.)
We recommend the following approach [20]:
Measure serum troponin-I or troponin-T at first presentation.
If the troponin is not elevated, repeat at six to nine hours. It is not uncommon to measure a
second troponin earlier than six hours in patients who are highly suspected of having ongoing
NSTEMI, since 80 percent of patients who rule in will do so in two to three hours [23]. In an
occasional patient in whom the index of suspicion for acute MI is high, but the first two
troponin measurements are not elevated, a repeat measurement at 12 to 24 hours may be
necessary.
CK-MB is measured when a troponin assay is not available. Previously, CK-MB was advocated
to help diagnose reinfarction, but now troponin has subsumed that role [2]. Reinfarction is
diagnosed if there is a 20 percent increase of the value in the second sample [2].
Troponin elevations persist for one to two weeks after AMI, but values are usually not rising
or falling rapidly at this time, allowing one to distinguish acute from more chronic events
[2,21].
INFORMATION FOR PATIENTS UpToDate offers two types of patient education materials, The
Basics and Beyond the Basics. The Basics patient education pieces are written in plain language,
at the 5th to 6th grade reading level, and they answer the four or five key questions a patient might
have about a given condition. These articles are best for patients who want a general overview and
who prefer short, easy-to-read materials. Beyond the Basics patient education pieces are longer,
more sophisticated, and more detailed. These articles are written at the 10th to 12th grade reading
level and are best for patients who want in-depth information and are comfortable with some
medical jargon.
Here are the patient education articles that are relevant to this topic. We encourage you to print
or e-mail these topics to your patients. (You can also locate patient education articles on a variety
of subjects by searching on patient info and the keyword(s) of interest.)
www.uptodate.com/contents/criteria-for-the-diagnosis-of-acute-m ocardial-infarction?view=print
9/20
2/21/12
Criteria for the diagnosis of acute m ocardial infarction
Beyond the Basics topic (see "Patient information: Heart attack (Beyond the Basics)")
SUMMARY Myocardial infarction (MI) is defined as a clinical (or pathologic) event caused by
myocardial ischemia in which there is evidence of myocardial injury or necrosis. Criteria are met
when there is a rise and/or fall of cardiac biomarkers, along with supportive evidence in the form of
typical symptoms, suggestive electrocardiographic changes, or imaging evidence of new loss of
viable myocardium or new regional wall motion abnormality. (See 'Introduction' above.)
The criteria used to define MI differ somewhat depending upon the particular clinical circumstance
of the patient: those suspected of acute MI based upon their presentation; those undergoing either
coronary artery bypass graft surgery or percutaneous intervention; or those who have sustained
sudden, unexpected cardiac arrest with or without death (table 1). (See 'Definitions' above.)
We recommend the following approach to diagnose an acute MI (excluding patients who have just
undergone revascularization):
An ECG, an abbreviated history (which focuses on the chest pain), and physical examination
should be obtained within 10 minutes of patient arrival. (See 'ECG' above and 'Chest
pain' above.)
Measure serum troponin-I or troponin-T at first presentation. (See 'Cardiac
biomarkers' above.)
If the serum troponin is not elevated, repeat at six to nine hours. It is not uncommon to
measure a second troponin earlier than six hours in patients who are highly suspected of
having ongoing NSTEMI. In an occasional patient in whom the index of suspicion for acute MI
is high but the first two troponin measurements are not elevated, a repeat measurement at
12 to 24 hours may be necessary. (See 'Cardiac biomarkers' above.)
Measure serum creatine kinase-MB (CK-MB) when a troponin assay is not available. (See
'Cardiac biomarkers' above.)
For patients who have undergone recent revascularization with either percutaneous coronary
intervention (PCI) or coronary artery bypass graft surgery (CABG), we suggest measurement of
troponin after the procedure. In order to diagnose myocardial infarction resulting from either PCI or
CABG, the baseline troponin has to have been normal, and thus a troponin should be ordered prior
to all revascularization procedures. (See 'After revascularization' above.)
Use of UpToDate is subject to the Subscription and License Agreement.
REFERENCES
1. Alpert JS, Thygesen K, Antman E, Bassand JP. Myocardial infarction redefined--a consensus
document of The Joint European Society of Cardiology/American College of Cardiology
Committee for the redefinition of myocardial infarction. J Am Coll Cardiol 2000; 36:959.
2. Thygesen K, Alpert JS, White HD, Joint ESC/ACCF/AHA/WHF Task Force for the Redefinition of
Myocardial Infarction. Universal definition of myocardial infarction. Eur Heart J 2007; 28:2525.
3. Anderson J, Adams C, Antman E, et al. ACC/AHA 2007 guidelines for the management of
patients with unstable angina/non-ST-elevation myocardial infarction: a report of the
American College of Cardiology/American Heart Association Task Force on Practice Guidelines
(Writing Committee to revise the 2002 Guidelines for the Management of Patients with
Unstable Angina/Non-ST-Elevation Myocardial Infarction): developed in collaboration with the
www.uptodate.com/contents/criteria-for-the-diagnosis-of-acute-m ocardial-infarction?view=print
10/20
2/21/12
Criteria for the diagnosis of acute m ocardial infarction
American College of Emergency Physicians, American College or Physicians, Society for
Academic Emergency Medicine, Society for Cardiovascular Angiography and Interventions, and
Society of Thoracic Surgeons. J Am Coll Cardiol 2007; 50:e1
www.acc.org/qualityandscience/clinical/statements.htm (Accessed on September 18, 2007).
4. Hasdai D, Behar S, Wallentin L, et al. A prospective survey of the characteristics, treatments
and outcomes of patients with acute coronary syndromes in Europe and the Mediterranean
basin; the Euro Heart Survey of Acute Coronary Syndromes (Euro Heart Survey ACS). Eur
Heart J 2002; 23:1190.
5. Fox KA, Goodman SG, Klein W, et al. Management of acute coronary syndromes. Variations in
practice and outcome; findings from the Global Registry of Acute Coronary Events (GRACE).
Eur Heart J 2002; 23:1177.
6. Nomenclature and criteria for diagnosis of ischemic heart disease. Report of the Joint
International Society and Federation of Cardiology/World Health Organization task force on
standardization of clinical nomenclature. Circulation 1979; 59:607.
7. Cannon CP, McCabe CH, Stone PH, et al. The electrocardiogram predicts one-year outcome of
patients with unstable angina and non-Q wave myocardial infarction: results of the TIMI III
Registry ECG Ancillary Study. Thrombolysis in Myocardial Ischemia. J Am Coll Cardiol 1997;
30:133.
8. Pierpont GL, McFalls EO. Interpreting troponin elevations: do we need multiple diagnoses? Eur
Heart J 2009; 30:135.
9. Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA guidelines for the management of
patients with ST-elevation myocardial infarction: a report of the American College of
Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise
the 1999 Guidelines for the Management of Patients with Acute Myocardial Infarction).
Circulation 2004; 110:e82.
10. Canto JG, Shlipak MG, Rogers WJ, et al. Prevalence, clinical characteristics, and mortality
among patients with myocardial infarction presenting without chest pain. JAMA 2000;
283:3223.
11. www.acc.org/qualityandscience/clinical/statements.htm (Accessed on September 18, 2007).
www.acc.org/qualityandscience/clinical/statements.htm (Accessed on September 18, 2007).
12. Colaco R, Reay P, Beckett C, et al. False positive ECG reports of anterior myocardial infarction
in women. J Electrocardiol 2000; 33 Suppl:239.
13. Kulkarni AU, Brown R, Ayoubi M, Banka VS. Clinical use of posterior electrocardiographic leads:
a prospective electrocardiographic analysis during coronary occlusion. Am Heart J 1996;
131:736.
14. Fesmire FM, Percy RF, Bardoner JB, et al. Usefulness of automated serial 12-lead ECG
monitoring during the initial emergency department evaluation of patients with chest pain. Ann
Emerg Med 1998; 31:3.
15. Pope JH, Ruthazer R, Beshansky JR, et al. Clinical Features of Emergency Department Patients
Presenting with Symptoms Suggestive of Acute Cardiac Ischemia: A Multicenter Study. J
Thromb Thrombolysis 1998; 6:63.
16. Kudenchuk PJ, Maynard C, Cobb LA, et al. Utility of the prehospital electrocardiogram in
diagnosing acute coronary syndromes: the Myocardial Infarction Triage and Intervention
(MITI) Project. J Am Coll Cardiol 1998; 32:17.
17. Go AS, Barron HV, Rundle AC, et al. Bundle-branch block and in-hospital mortality in acute
myocardial infarction. National Registry of Myocardial Infarction 2 Investigators. Ann Intern
Med 1998; 129:690.
18. Shlipak MG, Go AS, Frederick PD, et al. Treatment and outcomes of left bundle-branch block
patients with myocardial infarction who present without chest pain. National Registry of
Myocardial Infarction 2 Investigators. J Am Coll Cardiol 2000; 36:706.
19. Rathore SS, Weinfurt KP, Gersh BJ, et al. Treatment of patients with myocardial infarction who
www.uptodate.com/contents/criteria-for-the-diagnosis-of-acute-m ocardial-infarction?view=print
11/20
2/21/12
Criteria for the diagnosis of acute m ocardial infarction
present with a paced rhythm. Ann Intern Med 2001; 134:644.
20. Goodman SG, Steg PG, Eagle KA, et al. The diagnostic and prognostic impact of the
redefinition of acute myocardial infarction: lessons from the Global Registry of Acute Coronary
Events (GRACE). Am Heart J 2006; 151:654.
21. Jaffe AS. Chasing troponin: how low can you go if you can see the rise? J Am Coll Cardiol
2006; 48:1763.
22. Thygesen K, Mair J, Katus H, et al. Recommendations for the use of cardiac troponin
measurement in acute cardiac care. Eur Heart J 2010; 31:2197.
23. Macrae AR, Kavsak PA, Lustig V, et al. Assessing the requirement for the 6-hour interval
between specimens in the American Heart Association Classification of Myocardial Infarction in
Epidemiology and Clinical Research Studies. Clin Chem 2006; 52:812.
24. Newby LK, Christenson RH, Ohman EM, et al. Value of serial troponin T measures for early and
late risk stratification in patients with acute coronary syndromes. The GUSTO-IIa
Investigators. Circulation 1998; 98:1853.
25. Jaffe AS, Babuin L, Apple FS. Biomarkers in acute cardiac disease: the present and the future.
J Am Coll Cardiol 2006; 48:1.
26. Guest TM, Ramanathan AV, Tuteur PG, et al. Myocardial injury in critically ill patients. A
frequently unrecognized complication. JAMA 1995; 273:1945.
27. Babuin L, Vasile VC, Rio Perez JA, et al. Elevated cardiac troponin is an independent risk factor
for short- and long-term mortality in medical intensive care unit patients. Crit Care Med 2008;
36:759.
28. Vasile VC, Babuin L, Ting HH, et al. Aborted myocardial infarction: is it real in the troponin era?
Am Heart J 2009; 157:636.
29. Meier MA, Al-Badr WH, Cooper JV, et al. The new definition of myocardial infarction: diagnostic
and prognostic implications in patients with acute coronary syndromes. Arch Intern Med 2002;
162:1585.
30. Kleiman NS, Lakkis N, Cannon CP, et al. Prospective analysis of creatine kinase muscle-brain
fraction and comparison with troponin T to predict cardiac risk and benefit of an invasive
strategy in patients with non-ST-elevation acute coronary syndromes. J Am Coll Cardiol 2002;
40:1044.
31. Newby LK, Roe MT, Chen AY, et al. Frequency and clinical implications of discordant creatine
kinase-MB and troponin measurements in acute coronary syndromes. J Am Coll Cardiol 2006;
47:312.
32. Antman EM, Tanasijevic MJ, Thompson B, et al. Cardiac-specific troponin I levels to predict
the risk of mortality in patients with acute coronary syndromes. N Engl J Med 1996; 335:1342.
33. Ottani F, Galvani M, Nicolini FA, et al. Elevated cardiac troponin levels predict the risk of
adverse outcome in patients with acute coronary syndromes. Am Heart J 2000; 140:917.
34. Heidenreich PA, Alloggiamento T, Melsop K, et al. The prognostic value of troponin in patients
with non-ST elevation acute coronary syndromes: a meta-analysis. J Am Coll Cardiol 2001;
38:478.
Topic 52 Version 10.0
www.uptodate.com/contents/criteria-for-the-diagnosis-of-acute-m ocardial-infarction?view=print
12/20
2/21/12
Criteria for the diagnosis of acute m ocardial infarction
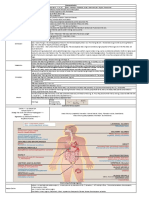
GRAPHICS
Definition of m ocardial infarction
Criteria for acute m ocardial infarction
The term myocardial infarction should be used when there is evidence of myocardial necrosis
in a clinical setting consistent with myocardial ischaemia. Under these conditions any one of
the following criteria meets the diagnosis for myocardial infarction:
Detection of rise and/or fall of cardiac biomarkers (preferably troponin) with at least one
value above the 99th percentile of the upper reference limit (URL) together with evidence
of myocardial ischaemia with at least one of the following:
Symptoms of ischaemia
EC G changes indicative of new ischaemia (new ST-T changes or new left bundle branch block
[LBBB])
Development of pathological Q waves in the EC G
Imaging evidence of new loss of viable myocardium or new regional wall motion abnormality
Sudden, unexpected cardiac death, involving cardiac arrest, often with symptoms
suggestive of myocardial ischaemia, and accompanied by presumably new ST elevation, or
new LBBB, and/or evidence of fresh thrombus by coronary angiography and/or at autopsy,
but death occurring before blood samples could be obtained, or at a time before the
appearance of cardiac biomarkers in the blood.
For percutaneous coronary interventions (PCI) in patients with normal baseline troponin
values, elevations of cardiac biomarkers above the 99th percentile URL are indicative of
peri-procedural myocardial necrosis. By convention, increases of biomarkers greater than 3
x 99th percentile URL have been designated as defining PCI-related myocardial infarction.
A subtype related to a documented stent thrombosis is recognized.
For coronary artery bypass grafting (CABG) in patients with normal baseline troponin
values, elevations of cardiac biomarkers above the 99th percentile URL are indicative of
peri-procedural myocardial necrosis. By convention, increases of biomarkers greater than 5
x 99th percentile URL plus either new pathological Q waves or new LBBB, or
angiographically documented new graft or native coronary artery occlusion, or imaging
evidence of new loss of viable myocardium have been designated as defining CABG-related
myocardial infarction.
Pathological findings of an acute myocardial infarction.
Criteria for prior m ocardial infarction
Any one of the following criteria meets the diagnosis for prior myocardial infarction:
Development of new pathological Q waves with or without symptoms.
Imaging evidence of a region of loss of viable myocardium that is thinned and fails to
contract, in the absence of a non-ischaemic cause.
Pathological findings of a healed or healing myocardial infarction.
Reproduced with permission from: Thygesen, K, Alpert, JS, White, HD, et al. Universal definition of
myocardial infarction: Kristian Thygesen, Joseph S. Alpert and Harvey D. White on behalf of the Joint
ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction. Eur Heart J 2007;
28:2525. Copyright 2007 Oxford University Press.
www.uptodate.com/contents/criteria-for-the-diagnosis-of-acute-m ocardial-infarction?view=print
13/20
2/21/12
Criteria for the diagnosis of acute m ocardial infarction
Coronar arter surger stud definitions of angina
Definite angina
Substernal discomfort precipitated by exertion, with a typical radiation to the shoulder, jaw
or inner aspect of the arm relieved by rest or nitroglycerin in less than 10 minutes
Probable angina
Has most of the features of definite angina but may not be entirely typical in some aspects
"Probabl not" angina
Defined as an atypical overall pattern of chest pain that does not fit the description of
definite angina
"Definitel not" angina
Chest pain is unrelated to activity, appears to be clearly of non-cardiac origin and is not
relieved by nitroglycerin
Adapted from CASS Investigators. National Heart Lung and Blood Institute Coronary Artery Study,
Circulation 1981; 63(Suppl I):I-81.
www.uptodate.com/contents/criteria-for-the-diagnosis-of-acute-m ocardial-infarction?view=print
14/20
2/21/12
Criteria for the diagnosis of acute m ocardial infarction
Alternative diagnoses to cardiac ischemia for patients with chest pain
Non-ischemic
cardiovascular
Aortic dissection*
Myocarditis
Pericarditis
Chest wall
Cervical disc disease
Pulmonar
Gastrointestinal
Pleuritis
Biliary
Pneumonia
Pulmonary embolus*
Tension pneumothorax*
Ps chiatric
C holangitis
C holecystitis
C holedocholithiasis
C olic
Esophageal
Esophagitis
Costochondritis
Affective disorders (eg,
depression)
Fibrositis
Anxiety disorders
Reflux
Herpes zoster (before the rash)
Neuropathic pain
Rib fracture
Sternoclavicular arthritis
Hyperventilation
Spasm
Rupture*
Panic disorder
Pancreatitis
Primary anxiety
Peptic ulcer
disease
Somatiform disorders
Thought disorders (eg, fixed
delusions)
Nonperforating
Perforating*
* Potentially life-threatening conditions. Adapted with permission from: ACC/AHA/ACP Guidelines for
the Management of Patients with Chronic Stable Angina. J Am Coll Cardiol 1999; 33:2092. Copyright
1999 American College of Cardiology.
www.uptodate.com/contents/criteria-for-the-diagnosis-of-acute-m ocardial-infarction?view=print
15/20
2/21/12
Criteria for the diagnosis of acute m ocardial infarction
ECG manifestations of acute m ocardial ischaemia (in absence of LVH and
LBBB)
ST elevation
New ST elevation at the J-point in two contiguous leads with the cut-off points: 0.2 mV in
men or 0.15 mV in women in leads V2 -V3 and/or 0.1 mV in other leads
ST depression and T-wave changes
New horizontal or down-sloping ST depression 0.05 mV in two contiguous leads; and/or T
inversion 0.1 mVin two contiguous leads with prominent R-wave or R/S ratio >1
Reproduced with permission from: Thygesen, K, Alpert, JS, White, HD, et al. Universal definition of
myocardial infarction: Kristian Thygesen, Joseph S. Alpert and Harvey D. White on behalf of the Joint
ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction. Eur Heart J 2007;
28:2525. Copyright 2007 Oxford University Press.
www.uptodate.com/contents/criteria-for-the-diagnosis-of-acute-m ocardial-infarction?view=print
16/20
2/21/12
Criteria for the diagnosis of acute m ocardial infarction
ECG changes associated with prior m ocardial infarction
Any Q-wave in leads V2 -V3 0.02 s or QS complex in leads V2 and V3
Q-wave 0.03 s and 0.1 mV deep or QS complex in leads I, II, aVL, aVF, or V4 -V6 in any two
leads of a contiguous lead grouping (I, aVL,V6 ; V4 -V6 ; II, III, and aVF)*
R-wave 0.04 s in V1 -V2 and R/S 1 with a concordant positive T-wave in the absence of a
conduction defect
* The same criteria are used for supplemental leads V7 -V9 , and for the Cabrera frontal plane lead
grouping. Reproduced with permission from: Thygesen, K, Alpert, JS, White, HD, et al. Universal
definition of myocardial infarction: Kristian Thygesen, Joseph S. Alpert and Harvey D. White on behalf
of the Joint ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction. Eur Heart J
2007; 28:2525. Copyright 2007 Oxford University Press.
www.uptodate.com/contents/criteria-for-the-diagnosis-of-acute-m ocardial-infarction?view=print
17/20
2/21/12
Criteria for the diagnosis of acute m ocardial infarction
Causes of ST segment elevation
Myocardial ischemia or infarction
Noninfarction, transmural ischemia (Prinzmetal's angina pattern or acute takotsubo syndrome)
Acute myocardial infarction (MI) usually due to coronary atherosclerosis or occasionally to other
causes (eg, acute takotsubo syndrome)
Post-MI (ventricular aneurysm pattern)
Acute pericarditis
Normal variants (including benign early repolarization)
Left ventricular hypertrophy or left bundle branch block (V1-V2 or V3)
Other
Myocarditis (may look like MI or pericarditis)
Massive pulmonary embolism (leads V1-V2 in occasional cases)
Brugada-type patterns (V1-V3 with right bundle branch block-appearing morphology)
Myocardial tumor
Myocardial trauma
Hyperkalemia (only leads V1 and V2)
Hypothermia (J wave/Osborn wave)
Hypercalcemia (rarely)
Post-DC cardioversion (rarely)
www.uptodate.com/contents/criteria-for-the-diagnosis-of-acute-m ocardial-infarction?view=print
18/20
2/21/12
Criteria for the diagnosis of acute m ocardial infarction
Causes of Q waves
Ph siologic or positional factors
Normal variant "septal" q waves
Normal variant Q waves in leads V1,V2, aVL, III, and aVF
Left pneumothorax or dextrocardia: loss of lateral precordial R wave progression
M ocardial injur
or infiltration
Acute processes: myocardial ischemia or infarction, myocarditis, hyperkalemia
Chronic processes: myocardial infarction, idiopathic cardiomyopathy, myocarditis,
amyloidosis, tumor, sarcoid, scleroderma, Chagas' disease, echinococcus cyst
Ventricular h pertroph
or enlargement
Left ventricle: slow R wave progression in which there are small or absent R waves in the
mid-precordial leads
Right ventricle: reversed R wave progression in which there is a progressive decrease in R
wave amplitude from V1 to the mid-lateral precordial leads, or slow R wave progression,
particularly with chronic obstructive lung disease or acute pulmonary embolism
Hypertrophic cardiomyopathy - may simulate anterior, inferior, posterior, or lateral infarcts
Conduction abnormalities
Left bundle branch block - slow R wave progression in which there are small or absent R
waves in the mid-precordial leads
Wolff-Parkinson-White patterns
www.uptodate.com/contents/criteria-for-the-diagnosis-of-acute-m ocardial-infarction?view=print
19/20
2/21/12
Criteria for the diagnosis of acute m ocardial infarction
2012 UpToDate, Inc. All rights reserved. |
Licensed to: Poudre Valle Healthcare Inc
DA3893C 392-4744.14]
Subscription and License Agreement | Release: 20.2 - C 20.3
| Support Tag: [ecapp1103p.utd.com-186.176.251.115-
www.uptodate.com/contents/criteria-for-the-diagnosis-of-acute-m ocardial-infarction?view=print
20/20
Anda mungkin juga menyukai
- A Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsDari EverandA Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsBelum ada peringkat
- IHD CAUSES CHEST PAINDokumen19 halamanIHD CAUSES CHEST PAINOsama MalikBelum ada peringkat
- Digitalis Toxicity Treatment and ManagementDokumen39 halamanDigitalis Toxicity Treatment and ManagementAnonymous 3OoumAUytBelum ada peringkat
- Cardiac Action PotentialDokumen41 halamanCardiac Action PotentialRadijska Postaja KoprivnicaBelum ada peringkat
- Coronary Artery DiseaseDokumen33 halamanCoronary Artery DiseaseAlma Rifa'Ana LiskaBelum ada peringkat
- Coronary Heart Disease: Angina Pectoris Myocardial InfarctionDokumen44 halamanCoronary Heart Disease: Angina Pectoris Myocardial Infarctionalejandrino_leoaugustoBelum ada peringkat
- Cvs PathoDokumen36 halamanCvs PathoISRAELBelum ada peringkat
- Cardiomyopathy: Leonard Shaju Joisy AloorDokumen34 halamanCardiomyopathy: Leonard Shaju Joisy AloorJoisy AloorBelum ada peringkat
- SICKLE CELL DISEASE: A CASE OF VASO-OCCLUSIVE CRISISDokumen44 halamanSICKLE CELL DISEASE: A CASE OF VASO-OCCLUSIVE CRISISNICHOLAS KAUMBA100% (1)
- Cardiomyopathy: M Taufik I, MDDokumen28 halamanCardiomyopathy: M Taufik I, MDChi RahmawatiBelum ada peringkat
- Advanced Knowledge Assessment in Adult Critical CareDokumen570 halamanAdvanced Knowledge Assessment in Adult Critical CareMajor EmadBelum ada peringkat
- Sickle Cell Disease: Symptoms and TreatmentDokumen13 halamanSickle Cell Disease: Symptoms and TreatmentAditya Rangga Fandiarta100% (1)
- Adrenergic DrugsDokumen33 halamanAdrenergic DrugsZsa Zsa FebryanaBelum ada peringkat
- The Lower Respiratory Tract Infection: Pneumonia: Ida Bagus Ngurah RaiDokumen32 halamanThe Lower Respiratory Tract Infection: Pneumonia: Ida Bagus Ngurah RaiFelicia adeline ChristianBelum ada peringkat
- Diseases of The AortaDokumen48 halamanDiseases of The AortaYibeltal AssefaBelum ada peringkat
- Anaesthesia and Atrial FibrillationDokumen15 halamanAnaesthesia and Atrial FibrillationNaresh Dhawan100% (1)
- Cardiovascular Disorders: BY: Maximin A. Pomperada, RN, MANDokumen65 halamanCardiovascular Disorders: BY: Maximin A. Pomperada, RN, MANRellie Castro100% (1)
- Sickle Cell Disease: Everything You Ever Wanted To KnowDokumen23 halamanSickle Cell Disease: Everything You Ever Wanted To KnowAnastasiafynn100% (1)
- IHDDokumen34 halamanIHDElly Msi ProbolinggoBelum ada peringkat
- Aortic StenosisDokumen3 halamanAortic StenosisMaxine BaraquiaBelum ada peringkat
- Rheumatic Fever and Rheumatic Heart DiseaseDokumen132 halamanRheumatic Fever and Rheumatic Heart DiseaseDamie FernandezBelum ada peringkat
- Mitral Valve ProlapseDokumen5 halamanMitral Valve ProlapseDerofiez Hana RuhyadinBelum ada peringkat
- Development of HeartDokumen15 halamanDevelopment of Heartash ashBelum ada peringkat
- 2021 CVD Prevention GlsDokumen147 halaman2021 CVD Prevention GlsRuslan RidcodubskiiBelum ada peringkat
- Implementing NICE guidance for hypertension case scenariosDokumen51 halamanImplementing NICE guidance for hypertension case scenariosrwev3Belum ada peringkat
- Frank-Starling LawDokumen5 halamanFrank-Starling LawNTA UGC-NETBelum ada peringkat
- Rhythm Control Versus Rate Control in Atrial Fibrillation - UpToDokumen39 halamanRhythm Control Versus Rate Control in Atrial Fibrillation - UpTohatsune100% (1)
- Cardiac BiomarkersDokumen7 halamanCardiac BiomarkersAnand VeerananBelum ada peringkat
- Hypertensive Heart DiseaseDokumen33 halamanHypertensive Heart Diseaserini_adriani6817Belum ada peringkat
- Cardiovascular Nursing: Study Online atDokumen7 halamanCardiovascular Nursing: Study Online atLilly DayeBelum ada peringkat
- Renal Transplant: 1) Steps Involved in Kidney TransplantationDokumen4 halamanRenal Transplant: 1) Steps Involved in Kidney TransplantationNadia SalwaniBelum ada peringkat
- Types and Management of Valvular Heart DiseaseDokumen60 halamanTypes and Management of Valvular Heart DiseaseIntan Kumalasari RambeBelum ada peringkat
- Ischemic Heart Disease 19.9.90Dokumen27 halamanIschemic Heart Disease 19.9.90Hamidreza GoodarzynejadBelum ada peringkat
- Ischemic Heart DiseaseDokumen116 halamanIschemic Heart DiseaseAndrew OrlovBelum ada peringkat
- Peripheral Arterial DiseaseDokumen5 halamanPeripheral Arterial Diseaseampogison08Belum ada peringkat
- Heart Failure RevisionDokumen4 halamanHeart Failure RevisionBlanaid MargaretBelum ada peringkat
- Ngaji Arrythmia Cordis 3Dokumen122 halamanNgaji Arrythmia Cordis 3Dhita Dwi NandaBelum ada peringkat
- 2022 ESC Cardio-Onco Guidelines Official Slide Set - Final - ProtectedDokumen158 halaman2022 ESC Cardio-Onco Guidelines Official Slide Set - Final - ProtectedAli Uğur SoysalBelum ada peringkat
- Antihypertensive DrugsDokumen78 halamanAntihypertensive DrugsOsannah Irish InsongBelum ada peringkat
- 2019 - MCardiology - Clinical Features of Val HT 2019 2Dokumen72 halaman2019 - MCardiology - Clinical Features of Val HT 2019 2Vaenusha MuruganBelum ada peringkat
- PATHOPHYSIOLOGY OF SHOCKDokumen56 halamanPATHOPHYSIOLOGY OF SHOCKDr. Haricharan ABelum ada peringkat
- Hypertension LecturesDokumen65 halamanHypertension LecturesAdebisiBelum ada peringkat
- Cad ....Dokumen94 halamanCad ....AnanthibalaBelum ada peringkat
- Left and Right Heart Cath Procedure OverviewDokumen43 halamanLeft and Right Heart Cath Procedure OverviewIr Soebagoes100% (2)
- Algorithms of Care (Myocardial Infarction)Dokumen3 halamanAlgorithms of Care (Myocardial Infarction)Julius Delos SantosBelum ada peringkat
- DR Sandeep - EISENMENGER SYNDROMEDokumen81 halamanDR Sandeep - EISENMENGER SYNDROMEAlexandrescuBelum ada peringkat
- ECG Changes in Drug and Electrolyte AbnormalitiesDokumen28 halamanECG Changes in Drug and Electrolyte AbnormalitiesNachiket Vijay PotdarBelum ada peringkat
- Buerger'S Disease: By: Ns. Yulia Prodi S1 Keperawatan Stikes Kepanjen 2014Dokumen18 halamanBuerger'S Disease: By: Ns. Yulia Prodi S1 Keperawatan Stikes Kepanjen 2014atik mayasariBelum ada peringkat
- Lactic Acidosis: An Update: Jansen Seheult, Gerard Fitzpatrick and Gerard BoranDokumen12 halamanLactic Acidosis: An Update: Jansen Seheult, Gerard Fitzpatrick and Gerard Borangasman2003Belum ada peringkat
- Local AnaestheticsDokumen26 halamanLocal Anaestheticsv_vijayakanth7656Belum ada peringkat
- Left-Sided Congestive Heart Failure Case PresentationDokumen64 halamanLeft-Sided Congestive Heart Failure Case PresentationNicole Villanueva, BSN - Level 3ABelum ada peringkat
- Cardiac AsthmaDokumen12 halamanCardiac AsthmaNeupane KsabBelum ada peringkat
- HF PresentationDokumen62 halamanHF Presentationapi-552486649Belum ada peringkat
- Preventive CardiologyDokumen28 halamanPreventive CardiologyerizonBelum ada peringkat
- JVP Guide: Assessing Jugular Venous Pulse Waves and PressureDokumen53 halamanJVP Guide: Assessing Jugular Venous Pulse Waves and PressureJoshua JayakaranBelum ada peringkat
- Peripheral Vascular (PVS) Examination OSCE Station GuideDokumen4 halamanPeripheral Vascular (PVS) Examination OSCE Station GuideNikita JacobsBelum ada peringkat
- cardiomyopathy types and causesDokumen39 halamancardiomyopathy types and causesأبوأحمد الحكيمBelum ada peringkat
- AnginaDokumen12 halamanAnginaDr-Sanjay SinghaniaBelum ada peringkat
- Cva Power PointDokumen167 halamanCva Power PointJen Passilan100% (14)
- BARORECEPTORS AND CHEMORECEPTORS: REGULATION OF CARDIAC PRESSURESDokumen4 halamanBARORECEPTORS AND CHEMORECEPTORS: REGULATION OF CARDIAC PRESSURESDrbee10Belum ada peringkat
- Cateter, Colocacion en Niños PDFDokumen10 halamanCateter, Colocacion en Niños PDFalexandraossesBelum ada peringkat
- Clinical Stability Versus Clinical Failure in Patients With Community-Acquired PneumoniaDokumen8 halamanClinical Stability Versus Clinical Failure in Patients With Community-Acquired PneumoniaalexandraossesBelum ada peringkat
- Gazzete Des Tribunaux: Extraordinary MurdersDokumen6 halamanGazzete Des Tribunaux: Extraordinary MurdersalexandraossesBelum ada peringkat
- Dylla. Herald Tribute, Sarasota - 3.23.09 - WlogoDokumen1 halamanDylla. Herald Tribute, Sarasota - 3.23.09 - WlogoalexandraossesBelum ada peringkat
- Assessing Severity of Patients With Community-Acquired PneumoniaDokumen12 halamanAssessing Severity of Patients With Community-Acquired PneumoniaalexandraossesBelum ada peringkat
- Septic Shock PDFDokumen23 halamanSeptic Shock PDFalexandraosses100% (1)
- Assessing Severity of Patients With Community-Acquired PneumoniaDokumen12 halamanAssessing Severity of Patients With Community-Acquired PneumoniaalexandraossesBelum ada peringkat
- Cateter, Colocacion en Niños PDFDokumen10 halamanCateter, Colocacion en Niños PDFalexandraossesBelum ada peringkat
- Cateter, Colocacion en Niños PDFDokumen10 halamanCateter, Colocacion en Niños PDFalexandraossesBelum ada peringkat
- Hipertonica en Sibilancias PDFDokumen8 halamanHipertonica en Sibilancias PDFalexandraossesBelum ada peringkat
- Sepsos Neonatal PDFDokumen8 halamanSepsos Neonatal PDFalexandraossesBelum ada peringkat
- Latihan Bahasa Melayu Kertas 1 UPSRDokumen7 halamanLatihan Bahasa Melayu Kertas 1 UPSRshahruddin Bin Subari89% (53)
- Gazzete Des Tribunaux: Extraordinary MurdersDokumen6 halamanGazzete Des Tribunaux: Extraordinary MurdersalexandraossesBelum ada peringkat
- UCI Machine Learning Repository - Heart Disease Data SetDokumen7 halamanUCI Machine Learning Repository - Heart Disease Data SetpriyankaBelum ada peringkat
- Cardiac Rehabilitation ProtocolDokumen5 halamanCardiac Rehabilitation Protocolmarkhabm100% (1)
- DrugsDokumen3 halamanDrugsMarion Liana DayritBelum ada peringkat
- PharmacologyDokumen25 halamanPharmacologygregBelum ada peringkat
- Pharmacology Misbah PDFDokumen238 halamanPharmacology Misbah PDFRiham Khamis86% (7)
- Modafinil Factsheet (Composite)Dokumen21 halamanModafinil Factsheet (Composite)Danilo ScodellaroBelum ada peringkat
- LipnCott Summary SmallerDokumen21 halamanLipnCott Summary SmallerAdil Yousaf0% (1)
- Possible Causes of Chest PainDokumen4 halamanPossible Causes of Chest PainironBelum ada peringkat
- Research Poster PresentationDokumen1 halamanResearch Poster Presentationapi-328441669Belum ada peringkat
- Pass ProgramDokumen528 halamanPass ProgramEvelyn Lee Russell67% (3)
- 0533FDokumen34 halaman0533Fgregorio250188Belum ada peringkat
- Exercitii BoliDokumen10 halamanExercitii BoliDanielaTanaseBelum ada peringkat
- Patient EducationDokumen252 halamanPatient EducationAnn Peng100% (2)
- Chest Pain. Surgical Treatment of Acute Coronary Syndrome (ACS)Dokumen21 halamanChest Pain. Surgical Treatment of Acute Coronary Syndrome (ACS)Hanif ZamriBelum ada peringkat
- 12 Lead EKG 101Dokumen84 halaman12 Lead EKG 101Clarke KrugmanBelum ada peringkat
- NCLEX Medications For NursesDokumen118 halamanNCLEX Medications For Nursesanum78611095% (64)
- Drug Study Amlodipine & HydrocortisoneDokumen4 halamanDrug Study Amlodipine & HydrocortisoneJohn Kristoffer JisonBelum ada peringkat
- Drug StudyDokumen4 halamanDrug StudyMäc LäntinBelum ada peringkat
- The Construction of Medical Disposal Medical Sociology and Medical Problem Solving in Practice CareDokumen31 halamanThe Construction of Medical Disposal Medical Sociology and Medical Problem Solving in Practice CareCronopialmenteBelum ada peringkat
- Ace The OSCE2 BookDokumen126 halamanAce The OSCE2 BookVijay Mg100% (5)
- Drug StudyDokumen4 halamanDrug Studyjazmine_caritos100% (2)
- 1recent ExamsDokumen42 halaman1recent Examsfamilymedicine1234Belum ada peringkat
- Doctor and Patient:: General Principles of History TakingDokumen12 halamanDoctor and Patient:: General Principles of History TakingVishal ParnerkarBelum ada peringkat
- Nurs 252 Critical Thinking SummaryDokumen5 halamanNurs 252 Critical Thinking Summaryapi-284824610Belum ada peringkat
- Acute Coronary Syndrome (Acs) : DR M. Arman Nasution SPPDDokumen162 halamanAcute Coronary Syndrome (Acs) : DR M. Arman Nasution SPPDfifahBelum ada peringkat
- Sample Haad QuestionDokumen20 halamanSample Haad QuestionBobet Reña100% (3)
- MKS Essential Notes in Internal Medicine - 1st EdDokumen163 halamanMKS Essential Notes in Internal Medicine - 1st EdZeeshan AhmedBelum ada peringkat
- Truth About TestosteroneDokumen34 halamanTruth About TestosteroneNaturalBioHealthBelum ada peringkat
- 10 Years Viva Collection 2009Dokumen417 halaman10 Years Viva Collection 2009yoshiuda100% (3)
- Hema, Onco, Cardiology Review NotesDokumen9 halamanHema, Onco, Cardiology Review Notesjeshema100% (1)