What Have We Learned About Vitamin D Dosing? by Joseph Pizzorno, ND
Diunggah oleh
InnoVision Health MediaHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
What Have We Learned About Vitamin D Dosing? by Joseph Pizzorno, ND
Diunggah oleh
InnoVision Health MediaHak Cipta:
Format Tersedia
This article is protected by copyright. To share or copy this article, please visit copyright.com. Use ISSN#1543953X.
To subscribe, visit imjournal.com.
THE PATH AHEAD
What Have We Learned About Vitamin D Dosing?
Joseph Pizzorno, ND, Editor in Chief
ver the past several years, the surprising prevalence of A comprehensive review study
O vitamin D deficiency has become broadly recognized. A
number of studies have attempted to determine the mini-
mum, optimum, and toxic dosages, while others have used supple-
focused on estimating the optimal
serum level of 25(OH)D3 for a range
of measures such as disease inci-
mental vitamin D to prevent and treat a diverse range of diseases. dence, neurological function, and
And, as might be expected, drug companies are investing substan- bone density.6 Included in their review was the observation that
tial research dollars to find patentable vitamin D analogues, with normal, healthy levels in outdoor workers such as farmers is 135
some notable successes. nmol/L and for lifeguards 163 nmol/L.
There have been several excellent review articles on the efficacy The researchers found that bone density in males aged 20 to
of vitamin D (including in IMCJ: see “Vitamin D [Cholecalciferol]: 49 increased in proportion to increased 25(OH)D3 blood levels
A Paradigm Shift With Implications for All Healthcare Providers” in throughout the measured range: max 180 nmol/L for Caucasians,
IMCJ 2004;3.5: 44-54 and “Preparing Patients for Proper Sun while for Hispanics it peaked at 118 nmol/L and African Americans
Exposure” in IMCJ 2009;8.4:52-54), so I see no need to replicate at 90 nmol/L. Risk of fracture decreased proportionately with
that now. However, the issue of dosing has not yet been, in my opin- serum vitamin D levels throughout the measured range, so optimal
ion, adequately addressed. Here I will review the research on vita- levels were probably not achieved.
min D dosing. In addition, I will present some initial results from a Lower-extremity function in the elderly (average age 71
very exciting, ground-breaking corporate wellness program in years), as measured by the 8-foot walk and sit-to-stand tests, found
Canada that I am involved in where we are fully applying the prin- that walk time increased through the range (max 220 nmol/L),
ciples of natural/functional/integrative medicine to a group of blue- while sit-to-stand optimized at 130.
collar workers. As part of the project, we are running several labora- For periodontal disease, the degree of bone loss and tooth loss
tory tests to evaluate nutritional status and toxic load. One of the found was progressively lower in proportion to the level range
nutrients we have tested, supplemented, and followed is vitamin D. measured. Since the study only measured up to 100 nmol/L, the
This project is quite important for integrative medicine as we are likely higher optimal level to mitigate this disease is not known.
able to objectively measure the impact of our interventions in a For colon cancer, the risk decreased throughout the measured
large population of 1500 workers. range. Those with 25(OH)D3 >91.5 nmol/L have 27% the inci-
dence of colon cancer compared with those below 48.0.
Incidence of Deficiency My suggestion for the optimum level of vitamin D as mea-
In addition to the well-known osteoporosis connection, low sured by 25(OH)D3 is Caucasians, 125 to 175 nmol/L; Hispanics,
vitamin D levels are associated with, for example, increased inci- 100 to 150 nmol/L; and African Americans, 80 to 120 nmol/L. I
dence of cardiovascular disease, cancer, autoimmune diseases such was not able to determine in this review why the optimal range
as multiple sclerosis, pain, loss of cognitive function, and decreased appears to differ according to ethnic background.
strength.1,2 An 8.7-year follow-up study on 13 331 adults aged 20
years or older found that those in the lowest quartile of 25(OH)D3 Loading Versus Maintenance Dose
have a 26% increased rate of all-cause mortality.3 New research There is no widely accepted upper limit to daily vitamin D
continues to add to this list. dosage. In the past, the US Institute of Medicine recommended an
Deficiency of vitamin D is now recognized as a pandemic, with upper limit of 2000 IU/d. However, a comprehensive review found,
more than half of the world’s population currently at risk.4 Research “The clinical trial evidence shows that a prolonged intake of 250 μg
in the United States shows vitamin D deficiency in 36% of healthy (10 000 IU)/d of vitamin D3) is likely to pose no risk of adverse
young adults, 80% of healthy Caucasian infants, and 52% of adoles- effects in almost all individuals in the general population.”7
cent African Americans and Hispanic children.5 In addition, rickets However, almost all articles supporting this dosage as universally
is resurfacing in the 21st century as a major public health problem. safe are written by a single author.
We still do not definitively know the incidence of vitamin D Several studies have looked at the impact of oral vitamin D
deficiency. At this time, it appears to me that approximately 50% of supplementation and changes in serum 25(OH)D3 levels. One
the “healthy” North American population and greater than 80% of study measured dose response (nmol/L) in post-menopausal
those with a chronic disease are deficient. African American women given 800 IU/d for 2 years and then
2000 IU/d for another year. They found that 2000 IU/d was
Minimum Versus Optimal Level enough to reach a 50 nmol/L blood level but not enough to reach
At this time, there is no consensus on minimum, optimal, or the more desirable 75 nmol/L the researchers had targeted.8
toxic levels of vitamin D. However, I believe the body of research is A comprehensive study looked for the dosage necessary to
now large enough that some guidelines can be set. achieve a 25(OH)D3 level of at least 75 nmol/L. Those above a
8 Integrative Medicine • Vol. 9, No. 1 • Feb/Mar 2010 Pizzorno—The Path Ahead
baseline of 55 nmol/L were initially given 3800 IU/d while those old for causing hypercalcemia. They found that hypercalcemia
under were given 5000 IU/d. Dosages were then modified periodi- only results when 25(OH)D3 concentrations have consistently
cally for each person in order to achieve a target level of >75 been above 375 to 500 nmol/L. The maximum safe level of vita-
nmol/L. The required dosage ranged from a low of 800 IU/d to a min has been estimated as 275 nmol/L with a persistent level of
high of 6800 IU/d. Through data analysis and an algorithm, 375 causing hypercalcemia.11,12
researchers determined that the average person needed a dosage of Representative toxicity reports are as follows:
4600 IU/d to achieve at least 75 nmol/L.9 Only 1 person (dosage • A 3-month-old girl given 320 000 IU/d for 8 days; result
unspecified) exceeded 200 nmol/L, peaking at 220. = hypercalcemia.13
Perhaps the best study of dosage and safety was a 2007 report • A 7-year-old boy given 300 000 IU/d for 8 days; result =
in which 12 patients with multiple sclerosis where treated with anorexia, nausea, vomiting, polydypsia, polyuria, consti-
escalating dosages of vitamin D starting at 4000 IU/d and increas- pation, and hypercalcemia.14
ing to 40 000 IU/d over 28 weeks.10 Comprehensive testing was • A 58-year-old woman with diabetes mellitus and rheu-
done to detect toxicity: serum calcium, urinary calcium/creatine, matoid arthritis given 188 640 IU of vitamin D3 for 60
liver enzymes, serum creatinine, electrolytes, serum protein, and days; result = fatigue, constipation, back pain, forgetful-
parathyroid hormone. The only change researchers detected was a ness, nausea, vomiting, and hypercalcemia. Her 25(OH)
decrease in parathyroid hormone (and a remarkable 55% decrease D3 was 1171 nmol/L.15
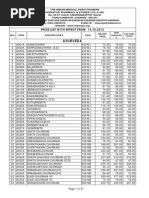
in spinal lesions!). The effect of the various dosages can be seen in • A 77-year-old woman given 50 000 IU/d for 6 days;
Table 1 (multiply by 40 to convert to IUs). result = hypercalcemia.16
• Eight patients drinking milk from the same dairy that had
800 made an error in vitamin D fortification. Dosages ranged
from 116 000 to 464 000 IU/d. Result = 7 had hypercalce-
Serum 25(OH)D (nmoI/L)
mia, and 1 had hypercalciuria but normocalcemia. The
600 * 25(OH)D3 ranged from 297 to 1168 nmol/L. 11
* • Patient age and vitamin D dosage not specified. Of note in
this study is that the initial 25(OH)D3 was 570 nmol/L and
400 calcium did not stabilize until it dropped to 285 nmol/L. 12
* A large public health study was done in Boston where a dairy
*
200 that provided home deliveries accidentally enriched the milk with
70 to 600 times the maximum legal amount of vitamin D; 11 000
households were delivered the overdosed milk.17 Searching hospi-
0 tal records found 56 people with hypercalcinosis; 2 died. Following
Baseline Calcium 700 1400 2800 5600 7000
were their symptoms:
Figure. Vitamin D3 Dose Schedule (mg/wk)
Reprinted with permission from the American Journal of Clinical Nutrition, 2007; 86(3):645-51. Anorexia 32%
Weight loss 27%
As can be seen, the dosage that caused serum 25(OH)D3 to Weakness 27%
exceed the totally safe level of 200 in a significant portion of the Fatigue 21%
study group was 16 000 IU/d. The limitations of this study are Disorientation 14%
that it was short term (only 4 weeks per dosage level) and in Vomiting 14%
patients known to especially need vitamin D. Nonetheless, this Dehydration 14%
appears to be the definitive study at this time. Polyuria 12%
When following the effect of vitamin D dosing (whether Constipation 11%
oral or sun exposure), keep in mind the following half lives: Asymptomatic 12%
Ingested D3 2 to 6 hours in the blood
(food or supplement) before depositing in tissues Contraindications, Adverse Events, and Drug
Tissue D3 2 months (sun-produced form) Interactions
25(OH)D3 15 days (circulating form) Sarcoidosis patients react poorly to vitamin D supplementa-
1,25(OH)2D3 15 hours (most active form) tion. It appears to interact with the fundamental pathophysiology
resulting in over production of 1,25(OH)2D3 and increased granu-
Toxic Dose loma production. Even summer sunlight exposure can increase D
For ethical reasons, no systematic studies have examined levels high enough to cause hypercalcemia in these patients.
vitamin D intoxication in humans. However, there have been The most significant drug interactions appear to be with
numerous anecdotal reports that have described accidental poi- the vitamin D analogues. There are some moderate interactions
soning with either vitamin D3 or vitamin D2. that are not contraindications but rather indicate the need for
One recent study specifically looked for the dosage thresh- attention. Vitamin D increases the absorption of aluminum from
Pizzorno—The Path Ahead Integrative Medicine • Vol. 9, No. 1 • Feb/Mar 2010 9
aluminum-containing antacids and statins; increases the activity several surprises here. I had expected older participants to have
of digoxin since it increases calcium absorption—same problem more difficulty absorbing vitamin D, but the opposite appeared
with other calcium-channel inhibitors as well as diuretics that to be the case. However, a closer look at the data revealed that
increase calcium retention; and increases the activity of CYP3A4 older participants were better at taking their vitamin D. I had
so drugs metabolized by this liver enzyme will be cleared more also expected weight/BMI to be negative factors, but BMI cor-
quickly. Drugs.com has a useful list of potential interactions that relation, while negative as expected, was weak. The mercury
can be quickly checked. long shot also did not show a correlation. While more definitive
Adverse reactions to vitamin D supplementation appear to multiple correlation analysis may show us something new, the
primarily occur only at accidental dosages as noted above. bottom line appears to be simply that dosage and duration are
A more subtle potential problem with large dosages of vita- the primary factors.
min D is its dependence on adequate amounts of vitamins A and What does this tell us about vitamin D dosages? That a
K2. It is beyond the scope of this editorial to address this in depth. loading dose of 10 000 IU/d for 3 months and maintenance of
The key is that vitamins A, D, and K2 work intricately together in a 5000 IU/d is not enough for most people in northern climes;
surprisingly diverse range of physiological functions. As vitamin D after 1 year of intervention, most of the participants had still not
levels normalize, deficiencies of vitamins A or K2 become clinically improved into normal range (let alone optimal range) with this
apparent. The paradox of soft-tissue calcium deposition in patients regime. Based on the research I reviewed above, I think a main-
with osteoporosis appears largely due to this imbalance between tenance dose of 5000 is still probably about right. However, the
vitamins D, A, and K2. Similarly, much of the toxicity associated loading dose needs to be much higher, perhaps 20 000 IU for 3
with high dosages of vitamin A appear to be due to inadequate to 6 months. The only way to be sure is to periodically measure
vitamin D. Bottom line, when supplementing with vitamin D, be your patient’s serum 25(OH)D3.
sure to include modest amounts of vitamins A and K2. Finally, of clinical significance are the anecdotes and reports
of improved “energy” of the participants and objective measures
Direct Experience With 1500 Canadians of improved health. Obviously, we did not only provide them
This review of the research is interesting, but what happens vitamin D, but also lifestyle counseling, a multivitamin, etc. The
when applied to a blue-collar population? As noted above, I have bottom line is that applying the principles promulgated by this
the privilege of applying integrative medicine principles to a journal is well received and effective.
large population of Canadians primarily located in a single prov-
ince. Following is what we learned about vitamin D. Personal Experience
Using a cutoff of 80 nmol/L (32.0 ng/L), we found that a As part of the project, all of us involved in design and imple-
surprising 81% of the study group were deficient. Our intervention mentation are running the same lab tests on ourselves as we are
was to first provide a 1-page educational handout to the partici- on the participants. I was quite surprised to find that my vitamin
pants and to then provide a no-cost supplemental vitamin D in the D levels were also low, despite my healthy diet, love of the sun
form of capsules or liquid drops. The challenge was determining a (yes, we do occasionally get sun in Seattle), and regular use of a
loading dose that would normalize most of the group with mini- good-quality multivitamin. Thus began my own adventure find-
mal risk of excess in any and to then determine a maintenance ing my right dosage. At this time, all I can say is that a daily dose
dose. Early on, we were recommending 2000 to 4000 IU/day, but, of 5000 is not enough to maintain my levels at 80 nmol/L, let
as we looked at the emerging research on vitamin D, we soon real- alone get it into my self-determined optimal range for Caucasians
ized we needed much larger loading and maintenance dosages. of 125 to 175 nmol/L. And for my wife Lara, after 2 years of
Thus, we began recommending a loading dose of 8000 to 15 000 continuously losing bone despite everything I knew to do—
IU/d typically for 3 months and then an average daily mainte- including supplementation with vitamin D—we decided to run
nance dose of 5000 IU/d. An average of a year later we asked if a genomic test on her to look at various genes involved in bone
they took the vitamin D we provided them and remeasured their health. We found she has the VDR BB variant, meaning she has
serum 25(OH)D3. Remarkably, 90% took the vitamin D we pre- trouble absorbing and using vitamin D. Two years of experi-
scribed them. This unprecedented compliance resulted in their menting with increasing dosages of vitamin D supplementation
average serum 25(OH)D3 increasing 41% and the number below finally revealed that for her to maintain a normal serum 25(OH)
80 nmol/L decreasing to 53%. Of particular importance, no one’s D3 level of 100 to 150 nmol/L requires a surprising 10 000 IU/d.
vitamin D level went into the toxic range. Only a few were over We do live in Seattle, so sunlight is hard to come by.
200, with 3 exceeding our preferred upper limit of 250: 269, 275,
and 283. No adverse events were reported. Cost Effectiveness
A key question, then, is what factors should be taken into This is a no-brainer. I found 1 study that showed those with
consideration when recommending a loading and maintenance vitamin D deficiency experiencing 39% higher annual health
dose? Although 90% took their vitamin D, only 35% made it into care costs than those with normal levels.18 Vitamin D is cheap—
the normal range. Obvious factors to consider include age, for example a bottle of 360 capsules at 2000 IU/capsule costs
weight/body-mass index (BMI), dosage and duration, and, just around $12.00. So a person taking 5000 IU/d would spend only
for the heck of it, blood mercury. The only correlations I found $30.00 a year and likely prevent several orders of magnitude
were for dose and duration (0.41) and age (0.16). There were more in health-care costs.
10 Integrative Medicine • Vol. 9, No. 1 • Feb/Mar 2010 Pizzorno—The Path Ahead
Summary release Coenzyme Q10-β-Cyclodextrin Complex (MicroActive
After looking at the research and considering our experi- Co-Q10).” They compare the relative bioavailability of an improved
ence with 1500 blue-collar workers, I am making the following coQ10 bound to cyclodextrin inclusion with both a conventional
observations and recommendations: coQ10 softgel formulation and a crystalline co-Q10. The results of
the first study indicated that MicroActive Co-Q10 showed a sus-
1. The incidence of deficiency in the general population is tained release and that its bioavailability was significantly better
apparently greater than 50% and likely less than 10% have than the crystalline form, while in the second study, the 0- to
optimal levels of vitamin D. These numbers are all worse 24-hour absorption confirmed the sustained-release property of
in those who suffer almost any chronic disease as well as the MicroActive Co-Q10 complex as well as the significantly higher
those with dark skin—though the story is still develop- and uniform bioavailability. Also, all the subjects in the accumula-
ing, so on this latter observation the research is mixed. tion phase of this second study showed a minimum of doubling in
2. Interpretation of serum 25(OH)D3 levels is as follows the plasma co-Q10 levels after 21 days of MicroActive Co-Q10 sup-
(divide by 2.5 to get ng/L): plementation, which represents a 100% response rate.
– minimum: 80 nmol/L; Now that he has completed his careful study of the
– optimum: Caucasians, 125 to 175 nmol/L; Hispanics, Standardized Information on Dietary Ingredients (SIDI) Program,
100 to 150 nmol/L; African Americans, 80 to 120 Rick Liva, ND, RPh, returns with his critique, which will run in 2
nmol/L; parts. The SIDI program was developed by the Joint Standardized
– safe upper limit: 250 nmol/L; Ingredient Information Protocol (SIIP) Working Group, a joint
– lowest level with any documented toxicity: 375 nmol/L; trade association effort with participants representing both ingre-
– certain toxic level: 500 nmol/L. dient suppliers and finished product manufacturers. The objective
3. The only way to determine the proper vitamin D sup- of the working group is to develop standardized quality-control
plementation is by periodically measuring serum guidelines that ingredient suppliers can voluntarily use to help
25(OH)D3—no specific dosage regime meets the needs convey relevant and required information to their customers or
of everyone. manufacturers. The resulting SIDI guidelines are both comprehen-
4. The average loading dose appears to be 20 000 IU for 3 sive and flexible so as to be applicable across multiple product cat-
to 6 months. egories (eg, vitamins, minerals, botanicals, and other dietary
5. The average maintenance dose appears to be 5000 IU/d— ingredients). There are, however, some limitations. Rick delves into
less during the summer for those who get sun exposure. the pros and cons of SIDI in this issue and in the next will take a
6. Ensure your patient’s vitamins A and K2 levels are ade- look at the sample Botanical Template filled in by the SIIP Working
quate and check for possible drug interactions. Group and will offer suggestions as to what would make the tem-
7. Contraindicated in those with sarcoidosis and other plates stronger.
granulomatous diseases. Our interview this month is unusual as we address an area
we have not covered before. James V. Hardt, PhD, has spent more
What have we learned about vitamin D dosing? Increase the than 3 decades studying the electrophysiological basis of spiritual
dosage a lot—4 to 10 times the current RDI recommendations. states. He has published research in such scholarly journals as
Science, Psychophysiology and the Journal of Experimental Psychology
In This Issue and has coauthored or has pending more than 30 patents for the
As usual at the end of the year, we include our annual index. technology he has developed based on electroencephalography
In this we compile articles—listed by both author and topic—for measurement and feedback. I think you will find “Deciphering
all issues in 2009 (8.1-8.6). We are sure this will be a useful tool for the Electrophysiological Basis of Spiritual States” quite interest-
years to come. ing. I had the great fortune of spending a week studying with him,
We continue our periodic articles on nutrient and herbs. using his technology to increase my alpha waves. I found it a life-
Kathy Abascal, JD, RH (AHG), and Eric Yarnell, ND, RH (AHG), present changing experience.
to us cinnamon—note I do not use the scientific name and therein With seemingly everything in flux in health care, John Weeks’s
lies part of the story they tell us. The German Commission E has Industry Insights is an important read. Really, how will this health-
approved this herb to treat loss of appetite and dyspeptic com- care reform play out for us integrative medicine folks?
plaints such as mild spastic conditions of the gastrointestinal tract, I continue to be astounded by the insights Bill Benda, MD,
bloating, and flatulence. The article also outlines cinnamon’s his- brings in BackTalk. While I may not always agree with him, he
tory and folk use; chemical composition; pharmacology; clinical certainly makes me think. The issue of titles is indeed fraught with
applications; dosages; and safety, including drug interactions. I am social, financial, legal, and practice complications. As usual, no
disappointed that there does not appear to be research on so many easy solutions.
of its traditional uses. For example, one of the traditional uses Last, I am sorry to report that W. John Diamond, MD, author
taught me by my mentor John Bastyr, ND, was to use powdered of “Allostatic Medicine: Bringing Stress, Coping, and Chronic
cinnamon as a topical styptic. Disease into Focus” (published last issue, IMCJ 2009;8.6:40-44)
For original research, Doddabele Madhavi, PhD, and Daniel passed away in December of 2009 while we were doing the final
Kagan, PhD, provide “A Study on the Bioavailability of a Sustained- edits on Part II. We are working with his son, David Diamond, to
Pizzorno—The Path Ahead Integrative Medicine • Vol. 9, No. 1 • Feb/Mar 2010 11
F INALLY, A HOLISTIC WAY TO LOSE
publish the second half of his article, and you will find that coming
in the next issue, Apr/May 2010. We most regret the loss of Dr
Diamond, whose work we greatly respect, and apologize for the
disruption in sequentiality of his article. WEIGHT AND KEEP IT OFF...
Joseph Pizzorno, ND, Editor in Chief
drpizzorno@innovisionhm.com
http://twitter.com/drpizzorno
References
1. Bordelon P, Ghetu MV, Langan RC. Recognition and management of vitamin D defi-
ciency. Am Fam Physician. 2009;80(8):841-846.
2. Stechschulte SA, Kirsner RS, Federman DG. Vitamin D: bone and beyond, rationale
and recommendations for supplementation. Am J Med. 2009;122(9):793-802.
ONLY
$18.95
3. Melamed ML, Michos ED, Post W, Astor B. 25-hydroxyvitamin D levels and the risk of
mortality in the general population. Arch Intern Med. 2008;168(15):1629-1637.
4. Holick MF, Chen TC. Vitamin D deficiency: a worldwide problem with health conse- plus shipping
quences. Am J Clin Nutr. 2008;87(4):1080S-1086S and handling
5. Goldstein D. The epidemic of vitamin D deficiency. J Pediatr Nurs. 2009;24(4):345-346.
6. Bischoff-Ferrari HA, Giovannucci E, Willett WC, Dietrich T, Dawson-Hughes B.
Estimation of optimal serum concentrations of 25-hydroxyvitamin D for multiple
health outcomes. Am J Clin Nutr. 2006;84(1):18-28.
7. Vieth R. Vitamin D toxicity, policy, and science. J Bone Miner Res. 2007;22 Suppl
2:V64-V68.
8. Talwar SA, Aloia JF, Pollack S, Yeh JK. Dose response to vitamin D supplementation
among postmenopausal African American women. Am J Clin Nutr.
2007;86(6):1657-1662.
9. Aloia JF, Patel M, Dimaano R, et al. Vitamin D intake to attain a desired serum
25-hydroxyvitamin D concentration. Am J Clin Nutr. 2008;87(6):1952-1958.
10. Kimball SM, Ursell MR, O’Connor P, Vieth R. Safety of vitamin D3 in adults with mul-
tiple sclerosis. Am J Clin Nutr, 2007;86(3):645-651.
11. Jacobus CH, Holick MF, Shao Q, et al. Hypervitaminosis D associated with drinking
milk. N Engl J Med. 1992;326(18):1173-1177.
12. Lilienfeld-Toal H, Messerschmidt W, Sturm B, Ochs H. 25-hydroxy-vitamin D levels in a S AY GOODBYE TO THOSE
UNWANTED POUNDS!
patient with hypervitaminosis D. Klin Wochenschr. 1978;56(14):715-717.
13. Ezgu FS, Buyan N, Gündüz M, Tümer L, Okur I, Hasanoglu A. Vitamin D intoxication
and hypercalcaemia in an infant treated with pamidronate infusions. Eur J Pediatr. In this complete revision of the Alternative Medicine
2004;163(3):163-165.
14. Barrueto F Jr, Wang-Flores HH, Howland MA, Hoffman RS, Nelson LS. Acute vitamin Definitive Guide best seller, Dr. Ellen Kamhi provides
D intoxication in a child. Pediatrics. 2005;116(3):e453-e456. a complete, achieveable weight-loss and weight-
15. Klontz KC, Acheson DW. Dietary supplement–induced vitamin D intoxication. N Engl J
Med. 2007;357(3):308-309. management program. New concepts in weight
16. Lee DC, Lee GY. The use of pamidronate for hypercalcemia secondary to acute vitamin management–inlcuding metabolic syndrome, insulin
D intoxication. J Toxicol Clin Toxicol. 1998;36(7):719-721.
17. Blank S, Scanlon KS, Sinks TH, Lett S, Falk H. An outbreak of hypervitaminosis D asso-
resistance and the role of hormones such as ghrelin–
ciated with the overfortification of milk from a home-delivery dairy. Am J Pub Health. are supported with the latest scientific studies. Also
1995;85(5):656-659. includes new ideas for overcoming diet challenges,
18. Peiris AN, Bailey BA, Manning T. The relationship of vitamin D deficiency to health
care costs in veterans. Mil Med. 2008;173(12):1214-1218. tasty recipes and an eating plan, at-home exercises
and much, much more!
To order this and other great health books, visit
naturalsolutionsmag.com/go/shop or call
800-841-2665 or visit your local bookseller.
Distributed by
CELESTIAL ARTS/TEN SPEED PRESS
12 Integrative Medicine • Vol. 9, No. 1 • Feb/Mar 2010 Pizzorno—The Path Ahead
Anda mungkin juga menyukai
- Nicholas Gonzalez, MDDokumen1 halamanNicholas Gonzalez, MDInnoVision Health MediaBelum ada peringkat
- Patient Handout-InflammationDokumen1 halamanPatient Handout-InflammationInnoVision Health MediaBelum ada peringkat
- Self-Administered EFT (Emotional Freedom Techniques) in Individuals With Fibromyalgia: A Randomized TrialDokumen6 halamanSelf-Administered EFT (Emotional Freedom Techniques) in Individuals With Fibromyalgia: A Randomized TrialInnoVision Health Media100% (1)
- Brilliance Versus BlindersDokumen2 halamanBrilliance Versus BlindersInnoVision Health MediaBelum ada peringkat
- Fooling Mother Nature Is Usually A Bad Idea by Joe Pizzorno, NDDokumen3 halamanFooling Mother Nature Is Usually A Bad Idea by Joe Pizzorno, NDInnoVision Health MediaBelum ada peringkat
- Efficacy of Extract of Pelargonium Sidoides in Children With Acute Non-Group A Beta-Hemolytic Streptococcus Tonsillopharyngitis: A Randomized, Double-Blind, Placebo-Controlled TrialDokumen11 halamanEfficacy of Extract of Pelargonium Sidoides in Children With Acute Non-Group A Beta-Hemolytic Streptococcus Tonsillopharyngitis: A Randomized, Double-Blind, Placebo-Controlled TrialInnoVision Health Media100% (1)
- Mind-Body Medicine Researcher Elizabeth Blackburn Shares Nobel Prize, Plus MoreDokumen1 halamanMind-Body Medicine Researcher Elizabeth Blackburn Shares Nobel Prize, Plus MoreInnoVision Health MediaBelum ada peringkat
- Quantum Physics and Mind-Body MedicineDokumen1 halamanQuantum Physics and Mind-Body MedicineInnoVision Health MediaBelum ada peringkat
- Endless Energy: The Essential Guide To Energy HealthDokumen2 halamanEndless Energy: The Essential Guide To Energy HealthInnoVision Health MediaBelum ada peringkat
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5795)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Featured Companies That Provide Contract ManufacturingDokumen6 halamanFeatured Companies That Provide Contract Manufacturingvibhor_26janBelum ada peringkat
- WWW Fujisilysia Com Technology ApplicationsDokumen4 halamanWWW Fujisilysia Com Technology ApplicationsArnab BaruaBelum ada peringkat
- CDRR'S QPIRA Training Workshop On Drug Registration: Eliza G. SisonDokumen35 halamanCDRR'S QPIRA Training Workshop On Drug Registration: Eliza G. SisonAidee SmithBelum ada peringkat
- Selleck Inhibitor Catalog - JuneDokumen124 halamanSelleck Inhibitor Catalog - JuneSelleck ChemBelum ada peringkat
- DR Fuad Mirzayev of WHO Global TB Programme Presenting in Webinar in Lead Up To TB 2016 and AIDS 2016Dokumen13 halamanDR Fuad Mirzayev of WHO Global TB Programme Presenting in Webinar in Lead Up To TB 2016 and AIDS 2016bobbyramakantBelum ada peringkat
- Price List From 14.10.2013Dokumen27 halamanPrice List From 14.10.2013jasoneinsteinBelum ada peringkat
- Oxoferin Ward PPT UPDATEDDokumen27 halamanOxoferin Ward PPT UPDATEDdrusmanjamilhcmdBelum ada peringkat
- 1 - DS SATK Form - Initial Application of LTO 1.1Dokumen4 halaman1 - DS SATK Form - Initial Application of LTO 1.1Rudejane TanBelum ada peringkat
- BASF Glyoxal BrochureDokumen8 halamanBASF Glyoxal BrochureMukund KsBelum ada peringkat
- Analytical Method Development by High Performance Liquid ChromatographyDokumen9 halamanAnalytical Method Development by High Performance Liquid ChromatographyEditor IJTSRDBelum ada peringkat
- Researching Alzheimer's Medicines - Setbacks and Stepping StonesDokumen20 halamanResearching Alzheimer's Medicines - Setbacks and Stepping StonesOscar EspinozaBelum ada peringkat
- Fludarabine PhosphateDokumen3 halamanFludarabine PhosphateMulayam Singh YadavBelum ada peringkat
- Daftar Alat-Alat Yang Ada Diruangan Instalasi Gawat Darurat RS Bina Kasih Pekanbaru Lemari High AlertDokumen5 halamanDaftar Alat-Alat Yang Ada Diruangan Instalasi Gawat Darurat RS Bina Kasih Pekanbaru Lemari High AlertRiwiyoko YrsBelum ada peringkat
- Lecture Notes-Pharmacy Therapeutic CommitteeDokumen6 halamanLecture Notes-Pharmacy Therapeutic CommitteePatras BhattiBelum ada peringkat
- The EFPIA Disclosure Code: Your Questions AnsweredDokumen9 halamanThe EFPIA Disclosure Code: Your Questions AnsweredSvetlana PhillipovaBelum ada peringkat
- Homeo & Herbal RemediesDokumen175 halamanHomeo & Herbal Remediesjk.dasgupta100% (2)
- SM ProjectDokumen6 halamanSM ProjectSiddharth SrivastavBelum ada peringkat
- Lioresal: (Baclofen)Dokumen11 halamanLioresal: (Baclofen)ddandan_2Belum ada peringkat
- Guideline On Preparation of Site Master FilesDokumen8 halamanGuideline On Preparation of Site Master FilesIshara VithanaBelum ada peringkat
- A Review of Antidiabetic Potential of Ethnomedicinal Plants 2167 0412.1000165Dokumen8 halamanA Review of Antidiabetic Potential of Ethnomedicinal Plants 2167 0412.1000165Davia FendieBelum ada peringkat
- KAHKASHADokumen107 halamanKAHKASHAcity9848835243 cyberBelum ada peringkat
- Sandoz 2010 - 2011 Pocket GuideDokumen118 halamanSandoz 2010 - 2011 Pocket Guidemaheshgandla21Belum ada peringkat
- Determination of Vismodegib by Gradient ReversePhase High-Performance Liquid ChromatographyDokumen7 halamanDetermination of Vismodegib by Gradient ReversePhase High-Performance Liquid ChromatographyHiep X NguyenBelum ada peringkat
- Titr SensorbroeDokumen28 halamanTitr SensorbroeNgoc TruongBelum ada peringkat
- Kaiser Permanente: Good Health Is No SecretDokumen6 halamanKaiser Permanente: Good Health Is No SecretThomas Dominic CazneauBelum ada peringkat
- Impact of Training On Medical Representative in Their Performance Special Reference of Alembic Pharmaceuticals LTDDokumen6 halamanImpact of Training On Medical Representative in Their Performance Special Reference of Alembic Pharmaceuticals LTDaijbmBelum ada peringkat
- Cele TequeDokumen14 halamanCele TequeJoycee PerezBelum ada peringkat
- Morphine and Alternative Opioids in Cancer Pain: The EAPC RecommendationsDokumen7 halamanMorphine and Alternative Opioids in Cancer Pain: The EAPC RecommendationsSri HariBelum ada peringkat
- A Study of Cryo Stemcell Banking in Mumbai - Awareness and Acceptance by CustomerDokumen45 halamanA Study of Cryo Stemcell Banking in Mumbai - Awareness and Acceptance by Customerabhijit055Belum ada peringkat
- List of Members Who Can Vote: Panel - Iii Cosmetics, Toiletries, Soaps, Detergents & Essential OilsDokumen14 halamanList of Members Who Can Vote: Panel - Iii Cosmetics, Toiletries, Soaps, Detergents & Essential OilsGirish GuptaBelum ada peringkat