Csim2.26 - Pituitary F (X) Unusual Diabetes
Diunggah oleh
AinahMahaniJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Csim2.26 - Pituitary F (X) Unusual Diabetes
Diunggah oleh
AinahMahaniHak Cipta:
Format Tersedia
1
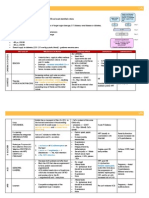
CSIM2.26
DIABETES
neonates diabetesneonates diabetes
PITUITARY
F(X):
UNUSUAL
MONOGENIC DIABETES
MATURITY ONSET DIABETES OF THE YOUNG AGE (MODY)
1. Maturity onset diabetes of the young (MODY) refers to any of several hereditary forms of
diabetes caused by mutations in an autosomal dominant gene disrupting insulin production.
2. MODY is often referred to as "monogenic diabetes" to distinguish it from the more common
types of diabetes (especially type 1 and type 2), which involve more complex combinations of
causes involving multiple genes (i.e., "polygenic") and environmental factors.
3. MODY 2 and MODY 3 are the most common forms. " MODY should not be confused with latent
autoimmune diabetes of adults (LADA) a form of type 1 DM, with slower progression to insulin
dependence in later life
4. MODY is caused by a mutation (or change) in a single gene. If a parent has this gene
mutation, any child they have, has a 50% chance of inheriting it from them.
5. Diagnosis/clinical features
a. Residual insulin secretion at least 3 years after diagnosis of type 1 DM
b. Young age of onset
c. Lack of metabolic syndrome in those presumed to have type 2 DM
6. Different type of MODY
a. Glucokinase MODY (32%)
b. Transcription factor MODY (68%)
c. MODYx
7. Beta cell physiology is key to pathophysiology. Glucokinase vs non-glucokinase
GLUCOKINASE MODY
1. Loss of function impairs glucose sensing.
2. It make 30% of MODY cases in UK and most common form of MODY in children.
3. Pathophysiology:
mutations in glycolytic site of GK
o >130 different mutations found to date
increased threshold for glucose-stimulated insulin secretion
insulin secretion remains regulated
microvascular complications not observed
pharmacological interventions not recommended
mild hyperglycaemia discordant with key role of GK in beta cell
o suggests degree of physiological adaptation
4. What does it looks like?
Presentation
- common in gestational diabetes
- rare in hospital diabetes clinics
- incidental
hyperglycaemia
children
in
Clinical features
- persistent, raised fasting glucose
- no extra-pancreatic features
- usually non-obese
- often asymptomatic
- parents & family: consider testing to support
dx.
TRANSCRIPTION FACTOR MODY
NF-IA & HNF-4A MODY
1. Clinical features
a. similar for HNF-Ia & HNF-4a
b. normoglycaemic in childhood
i. typically develop DM 12-30 years
ii. worsening glycaemia with age
neonates diabetesneonates diabetes
iii. may be misdiagnosed as type I DM
c. low renal threshold for glucose seen in HNF-Ia
d. poor control does lead to complications
e. parents & grandparents may have DM
f. HNF-1a
i. the most common form of MODY
2. Treatment
a. Sensitive to low dose sulphonylureas
i. low dose sulphonylureas are first line treatment
gliclazide
glibenclamide
ii. prandial secretogogues
b. In those diagnosed as type I DM
i. insulin can be stopped
HNF-IB MODY
1. HNF-1b function
o closely related to HNF-1a
o distinct DM phenotype
o pancreatic and genitourinary anomalies
2. Epidemiology
o 5-10% of MODY in UK
3. Clinical features
o RCAD: renal cysts & diabetes syndrome
o renal function variable: mild and RRT in up to 50%
o DM alone unusual
o patients not sensitive to sulphonylureas
o usually require insulin
NEONATES DIABETES
1. permanent neonatal diabetes
2. It is VERY RARE
3. Mechanism
a. GOF mutations KCNJII or ABCC8 genes in 40-50%
i. Kir6.2 & SURI subunits of K+ATP channel
ii. K+ channel cannot respond to ATP & permanently open
iii. no beta cell depolarisation
iv. failure of insulin release
b. insulin gene mutation 10%
i. require insulin therapy
4. Presentation & clinical features
a. neurological involvement in 20%
5.
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Slide Paparan - Dicky - Potensi Genomik DM BGSIDokumen27 halamanSlide Paparan - Dicky - Potensi Genomik DM BGSIFebrian DewiBelum ada peringkat
- Internal Medicine Quiz 4 DiabetesDokumen13 halamanInternal Medicine Quiz 4 DiabetesenzocruzinBelum ada peringkat
- Csim2.25 - Electrolyte Imbalance Iron Metabolism & StorageDokumen1 halamanCsim2.25 - Electrolyte Imbalance Iron Metabolism & StorageAinahMahaniBelum ada peringkat
- Urinary IncontinenceDokumen1 halamanUrinary IncontinenceAinahMahaniBelum ada peringkat
- Csim2.25 - Iron Metabolism & StorageDokumen4 halamanCsim2.25 - Iron Metabolism & StorageAinahMahaniBelum ada peringkat
- Csim2.26 - Pituitary F (X)Dokumen1 halamanCsim2.26 - Pituitary F (X)AinahMahaniBelum ada peringkat
- Csim2.25 - Electrolyte ImbalanceDokumen4 halamanCsim2.25 - Electrolyte ImbalanceAinahMahaniBelum ada peringkat
- CSIM2.26 - Pituitary FunctionDokumen3 halamanCSIM2.26 - Pituitary FunctionAinahMahaniBelum ada peringkat
- CSIM2.90 - Occupational AsthmaDokumen1 halamanCSIM2.90 - Occupational AsthmaAinahMahaniBelum ada peringkat
- Csim2.71 - The Patient With Proteinuria and HaematuriaDokumen11 halamanCsim2.71 - The Patient With Proteinuria and HaematuriaAinahMahaniBelum ada peringkat
- Csim2.25 - Electrolyte Imbalance Calcium and BoneDokumen7 halamanCsim2.25 - Electrolyte Imbalance Calcium and BoneAinahMahaniBelum ada peringkat
- Csim2.92 - HypoventilationDokumen1 halamanCsim2.92 - HypoventilationAinahMahaniBelum ada peringkat
- Csim2.94 - Interstitial Lung DiseaseDokumen3 halamanCsim2.94 - Interstitial Lung DiseaseAinahMahaniBelum ada peringkat
- CPTP - EpilepsyDokumen4 halamanCPTP - EpilepsyAinahMahaniBelum ada peringkat
- CSIM2.24 - Signal TransductionDokumen6 halamanCSIM2.24 - Signal TransductionAinahMahaniBelum ada peringkat
- CSIM2.91 - COPD and Pulmonary HypertensionDokumen2 halamanCSIM2.91 - COPD and Pulmonary HypertensionAinahMahaniBelum ada peringkat
- CPTP - Infection and Antibiotics 2Dokumen3 halamanCPTP - Infection and Antibiotics 2AinahMahaniBelum ada peringkat
- Penilaian Bahan MUAYYIDDokumen3 halamanPenilaian Bahan MUAYYIDAinahMahaniBelum ada peringkat
- Penilaian Bahan TamhidiDokumen3 halamanPenilaian Bahan TamhidiAinahMahaniBelum ada peringkat
- CPTP - Parkinson & MVMT DisordersDokumen2 halamanCPTP - Parkinson & MVMT DisordersAinahMahaniBelum ada peringkat
- CPTP - Poisonig MH Misuse of DrugsDokumen5 halamanCPTP - Poisonig MH Misuse of DrugsAinahMahaniBelum ada peringkat
- CPTP - Pregnancy & LactatingDokumen1 halamanCPTP - Pregnancy & LactatingAinahMahaniBelum ada peringkat
- Infection and AntibioticsDokumen4 halamanInfection and AntibioticsAinahMahaniBelum ada peringkat
- CPTP - HPT & HFDokumen4 halamanCPTP - HPT & HFAinahMahaniBelum ada peringkat
- CPTP - PainDokumen3 halamanCPTP - PainAinahMahaniBelum ada peringkat
- CPTP - Pud + Altered Bowel HabitDokumen3 halamanCPTP - Pud + Altered Bowel HabitAinahMahaniBelum ada peringkat
- CPTP - Diabetes and Lipid Lowering DrugsDokumen4 halamanCPTP - Diabetes and Lipid Lowering DrugsAinahMahaniBelum ada peringkat
- CPTP - Asthma & CopdDokumen5 halamanCPTP - Asthma & CopdAinahMahaniBelum ada peringkat
- CPTP - Af & Anti CoagulationDokumen4 halamanCPTP - Af & Anti CoagulationAinahMahaniBelum ada peringkat
- Infection and AntibioticsDokumen4 halamanInfection and AntibioticsAinahMahaniBelum ada peringkat
- Themed Week 7 - LIVERDokumen24 halamanThemed Week 7 - LIVERAinahMahaniBelum ada peringkat
- Tata Laksana DM Dan Hipertensi Sesuai StandarDokumen32 halamanTata Laksana DM Dan Hipertensi Sesuai Standardesi eka restiBelum ada peringkat
- Patience Abekavo Project WorkDokumen61 halamanPatience Abekavo Project WorkAdah EneBelum ada peringkat
- L Tiple Choice Questions: Pyetje-Davidson'sDokumen15 halamanL Tiple Choice Questions: Pyetje-Davidson'sNreca TokjonaBelum ada peringkat
- Definition of Diabetes Mellitus (DM)Dokumen12 halamanDefinition of Diabetes Mellitus (DM)Romarc Owen CorpuzBelum ada peringkat
- The Pathogenesis and Pathophysiology of Type 1 and Type 2 Diabetes MellitusDokumen13 halamanThe Pathogenesis and Pathophysiology of Type 1 and Type 2 Diabetes MellitusKimberlyn CustodioBelum ada peringkat
- Diabetes 11Dokumen7 halamanDiabetes 11mallikarjun_bgBelum ada peringkat
- UG PROJECT ADokumen56 halamanUG PROJECT AAdah EneBelum ada peringkat
- Diabetes: Submitted To: Uzma SarwarDokumen13 halamanDiabetes: Submitted To: Uzma SarwarSheeba HabBelum ada peringkat
- Tipos de Diabetes - Diabetes MonogenicaDokumen27 halamanTipos de Diabetes - Diabetes MonogenicaSara AmorimBelum ada peringkat
- Diabetes Mellitus 1Dokumen96 halamanDiabetes Mellitus 1manideepreddyBelum ada peringkat
- 12th BIO Chap 22 GENETICS BDokumen3 halaman12th BIO Chap 22 GENETICS BRaees Ali KhanBelum ada peringkat
- Maturity Onset Diabetes of The Young: Clinical Characteristics, Diagnosis and ManagementDokumen10 halamanMaturity Onset Diabetes of The Young: Clinical Characteristics, Diagnosis and ManagementatikahanifahBelum ada peringkat
- Expert Committee On The Diagnosis and Classification of Diabetes (2003) PDFDokumen16 halamanExpert Committee On The Diagnosis and Classification of Diabetes (2003) PDFPattyBelum ada peringkat
- Diabetes and The Nutrition and Diets For Its PreveDokumen16 halamanDiabetes and The Nutrition and Diets For Its PreveRam MBelum ada peringkat
- Diabetes Mellitus (Etiology, Classification, and Diagnosis)Dokumen6 halamanDiabetes Mellitus (Etiology, Classification, and Diagnosis)ayu permata dewiBelum ada peringkat
- Dm-Type-2 With Geno GramDokumen77 halamanDm-Type-2 With Geno GramRhajeeb Aennas SugalaBelum ada peringkat
- Diabetes Mellitus An OverviewDokumen4 halamanDiabetes Mellitus An OverviewALBelum ada peringkat
- Classification Pathophysiology Diagnosis of DMDokumen9 halamanClassification Pathophysiology Diagnosis of DMjohn haider gamolBelum ada peringkat
- Mutacion Del Gen GlucokinasaDokumen5 halamanMutacion Del Gen GlucokinasaJeancarlos QuispeBelum ada peringkat
- Swammy Plab 1 MockDokumen32 halamanSwammy Plab 1 Mockfreelancer08Belum ada peringkat
- Loddon Mallee Regional Diabetes Pathways Version 2 PDFDokumen30 halamanLoddon Mallee Regional Diabetes Pathways Version 2 PDFlatifa adluBelum ada peringkat
- The Diagnosis and Management of Atypical Types of Diabetes: Kathryn Evans Kreider, DNP, FNP-BCDokumen7 halamanThe Diagnosis and Management of Atypical Types of Diabetes: Kathryn Evans Kreider, DNP, FNP-BCromyBelum ada peringkat
- Diagnosis and Management of Type 2 Diabetes Mellitus ©stephen D. Sisson MD/Ambulatory Curriculum 2021Dokumen48 halamanDiagnosis and Management of Type 2 Diabetes Mellitus ©stephen D. Sisson MD/Ambulatory Curriculum 2021Carolina González RiveraBelum ada peringkat
- 239.mudassar DIABETES, PMDC 3811 PAID, Bushra 4011 Not PaidDokumen8 halaman239.mudassar DIABETES, PMDC 3811 PAID, Bushra 4011 Not PaidraychandwpBelum ada peringkat
- Diabetes MallitusDokumen33 halamanDiabetes Mallitushammu hothi100% (2)
- Diabetic Ketoacidosis DKA CeuDokumen36 halamanDiabetic Ketoacidosis DKA CeuancyoommenBelum ada peringkat
- DM Type 2Dokumen153 halamanDM Type 2Taufiqurrochman Nur AminBelum ada peringkat
- Endocrinology LastDokumen44 halamanEndocrinology Lastlestrange1984100% (1)