Subdural Haematoma
Diunggah oleh
Benjamin Chosich0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
8 tayangan2 halamanSubdural haematomas are a collection of extravasated blood between the dura mater and arachoid mater. They are caused by disruption of bridging veins between the venous dural sinuses and brain. The majority of haemas are formed by head trauma.
Deskripsi Asli:
Hak Cipta
© © All Rights Reserved
Format Tersedia
DOCX, PDF, TXT atau baca online dari Scribd
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniSubdural haematomas are a collection of extravasated blood between the dura mater and arachoid mater. They are caused by disruption of bridging veins between the venous dural sinuses and brain. The majority of haemas are formed by head trauma.
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai DOCX, PDF, TXT atau baca online dari Scribd
0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
8 tayangan2 halamanSubdural Haematoma
Diunggah oleh
Benjamin ChosichSubdural haematomas are a collection of extravasated blood between the dura mater and arachoid mater. They are caused by disruption of bridging veins between the venous dural sinuses and brain. The majority of haemas are formed by head trauma.
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai DOCX, PDF, TXT atau baca online dari Scribd
Anda di halaman 1dari 2
Subdural haematoma
Definition: a collection of extravasated blood between the dura mater and
arachoid mater
Epidemiology:
Risk factors: age, alcohol abuse, previous traumatic brain injury,
anticoagulation
Aetiology:
Head trauma vast majority
Aneurysm rupture 0.5-7.9% of those with SAH cause a SDH
AV malformation
Meningioma
Dural metastases
Coagulopathy
Neurosurgery
Cocaine abuse
Pathophysiology:
Subdural haematomas are caused by disruption of bridging veins between
the venous dural sinuses and brain. These veins are at increased risk of
rupture in patients with cerebral atrophy, particularly with the elderly,
dementia, alcoholism and other neurodegenerative diseases.
The majority of haematomas are formed by head trauma.
The haematoma typically reaches peak volume due to increased
intracranial pressure or direct compression by the clot itself.
Approximately 30% of subdural haematomas are caused by arterial
rupture, typically small cortical arteries.
Less commonly, low intracranial pressure can cause cerebrospinal fluid
leak, which reduces the CSF pressure and thus buoyancy of the brain. This
causes traction on the supporting structures, which can tear the bridging
veins. In addition, the low intracranial pressure causes engorgement of
cerebral veins, predisposing to rupture.
If undrained, fibrous tissue will be synthesized around the haematoma,
which may in turn calcify. Approximately 50% of subdural haematomas will
liquefy forming a hygroma (SDH devoid of blood) whilst the remainder will
remain stable.
Clinical features:
Acute:
o Presents 1-2 days after onset
o Approximately 50% of patients are in a coma from the time of injury
o Only 12-38% have the classic lucid period followed by progressive
neurological decline
Chronic:
o Presents >15 days after onset
o Manifestations are insidious and include cognitive impairment,
headaches, apathy, seizures and somnolence
o Global cognitive deficits are more common than focal deficits (e.g.
hemiparesis)
o Symptoms may fluctuate or remain constant
Diagnosis:
CT scan: acute subdural haematomas appear as crescentic hyperdense
lesions. Subacute and chronic haematomas appear as isodense/hypodense
crescentic lesions and may deform the cerebral surface. There have been
few studies investigating the sensitivity of CT scan for detection of
subdural haematomas but it appears to be quite sensitive (>91%) based
on 1980s studies.
MRI scan: more sensitive for detection of intracranial haemorrhage.
Angiography: indicated for evaluation of subdural haematomas with no
clear cause to exclude structural lesions such as aneurysms and AV
malformations.
Management:
Acute symptomatic: (medical emergency)
o Evaluation: GCS score, CT findings, neurological examination,
clinical stability, co-morbidities, age
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Treatment of Fruit Juice Concentrate Wastewater by Electrocoagulation - Optimization of COD Removal (#400881) - 455944Dokumen5 halamanTreatment of Fruit Juice Concentrate Wastewater by Electrocoagulation - Optimization of COD Removal (#400881) - 455944Victoria LeahBelum ada peringkat
- PERSONS Finals Reviewer Chi 0809Dokumen153 halamanPERSONS Finals Reviewer Chi 0809Erika Angela GalceranBelum ada peringkat
- Business Startup Practical Plan PDFDokumen70 halamanBusiness Startup Practical Plan PDFShaji Viswanathan. Mcom, MBA (U.K)Belum ada peringkat
- Quiz EmbryologyDokumen41 halamanQuiz EmbryologyMedShare90% (67)
- Human Capital FormationDokumen9 halamanHuman Capital Formationtannu singh67% (6)
- CHAPTER3 Foundations of Individual BehaviorDokumen32 halamanCHAPTER3 Foundations of Individual BehaviorLynoj AbangBelum ada peringkat
- Maximizing Oredrive Development at Khoemacau MineDokumen54 halamanMaximizing Oredrive Development at Khoemacau MineModisa SibungaBelum ada peringkat
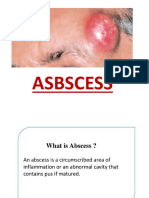
- ABSCESSDokumen35 halamanABSCESSlax prajapatiBelum ada peringkat
- Ensure Even Preload with Proper Tightening Tools and SequenceDokumen2 halamanEnsure Even Preload with Proper Tightening Tools and SequenceMachineryengBelum ada peringkat
- Genetically Engineered MicroorganismsDokumen6 halamanGenetically Engineered Microorganismsaishwarya joshiBelum ada peringkat
- Affidavit of Consent For Shared Parental AuthorityDokumen2 halamanAffidavit of Consent For Shared Parental AuthorityTet LegaspiBelum ada peringkat
- Assessment Formal AssessmentDokumen7 halamanAssessment Formal Assessmentashish33% (3)
- Chapter 4Dokumen26 halamanChapter 4Lana AlakhrasBelum ada peringkat
- Physical Education Worksheet AssessmentsDokumen3 halamanPhysical Education Worksheet AssessmentsMichaela Janne VegigaBelum ada peringkat
- The Ultimate Safari (A Short Story)Dokumen20 halamanThe Ultimate Safari (A Short Story)David AlcasidBelum ada peringkat
- Fundamentals of Fast SwimmingDokumen9 halamanFundamentals of Fast SwimmingTorcay Ulucay100% (1)
- Failures of Gabion Walls: Ganesh C. Chikute, Ishwar P. SonarDokumen7 halamanFailures of Gabion Walls: Ganesh C. Chikute, Ishwar P. SonarnavigareeBelum ada peringkat
- Gate Installation ReportDokumen3 halamanGate Installation ReportKumar AbhishekBelum ada peringkat
- Activity No 1 - Hydrocyanic AcidDokumen4 halamanActivity No 1 - Hydrocyanic Acidpharmaebooks100% (2)
- Pack Alimentacion Clin in Perin 14Dokumen194 halamanPack Alimentacion Clin in Perin 14Paz BustosBelum ada peringkat
- Micdak BackgroundDokumen3 halamanMicdak Backgroundappiah ernestBelum ada peringkat
- Hotel Housekeeping EQUIPMENTDokumen3 halamanHotel Housekeeping EQUIPMENTsamahjaafBelum ada peringkat
- Aphasia PDFDokumen4 halamanAphasia PDFRehab Wahsh100% (1)
- Sub Erna RekhaDokumen2 halamanSub Erna Rekhasurabhi mandalBelum ada peringkat
- Copia de Tissue Response To Dental CariesDokumen7 halamanCopia de Tissue Response To Dental Cariesjorefe12Belum ada peringkat
- Moral Character ViolationsDokumen2 halamanMoral Character ViolationsAnne SchindlerBelum ada peringkat
- Laboratorio 1Dokumen6 halamanLaboratorio 1Marlon DiazBelum ada peringkat
- The Danger of Microwave TechnologyDokumen16 halamanThe Danger of Microwave Technologyrey_hadesBelum ada peringkat
- Role of Family and Society in The Rehabiloitation of Offenders PDFDokumen4 halamanRole of Family and Society in The Rehabiloitation of Offenders PDFDevlika DasBelum ada peringkat
- QRF HD785-7Dokumen2 halamanQRF HD785-7Ralf MaurerBelum ada peringkat