HD 201 E1 20140127 Histology of The Male Reproductive System
Diunggah oleh
Maxine AlbaDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
HD 201 E1 20140127 Histology of The Male Reproductive System
Diunggah oleh
Maxine AlbaHak Cipta:
Format Tersedia
1
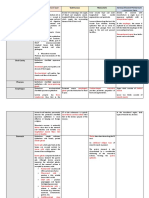
HD 201: Human Ontogeny and Parturition
Histology of the Male Reproductive System
January 27, 2014
Harold Louis Trinidad, MD
Topic Outline
I. Overview
II. Testis
a. Seminiferous Tubules
b. Interstitial Tissue
c. Spermatogenesis
d. Temperature Regulation
III. Intratesticular Ducts
a. Tubuli Recti
b. Rete Testis
IV. Extratesticular Ducts
a. Ductuli Efferentes
b. Epididymis
c. Ductus Deferens
d. Urethra
V. Accessory Glands
a. Seminal Vesicles
b. Prostate Gland
c. Bulbourethral Glands
d. Capacitance
VI. Male Fertility
Objectives
differentiate the different tract structures
enumerate the different phases of spermatogenesis
trace the pathway of spermatozoa from the testis to the
penile urethra
list the functions of the different accessory glands
understand how these structures and processes impact
fertility
OVERVIEW
The male reproductive system consists of the testes,
intratesticular ducts, extratesticular ducts, accessory
glands, and penis.
Figure 2. Diagram showing the anatomy of a testis.
Figure 3. Micrograph showing a section of a testis. (Source:
http://embryology.med.unsw.edu.au/embryology/images/b/b5/Testis_hi
stology_001.jpg)
Seminiferous Tubules
Seminiferous (Germinal) Epithelium
Spermatogenic Cells (germ cells)
Sertoli Cells (non-germ cells)
Basement Membrane
innermost layer contains flattened, smooth-muscle like
myoid cells which allow weak contractions of the tubule
Figure 1. Overview of the male reproductive system.
TESTIS
Structure
Tunica Albuginea
o dense connective tissue capsule covering the testis
o homologous to the covering of the ovaries
Mediastinum Testis
o thickened portion of the tunica albuginea on the
posterior side of the testis
o sends out fibrous septa which penetrate and divide
the organ into 300 testicular lobules
Testicular Lobule
o occupied by 1 to 4 seminiferous tubules containing
spermatogenic cells and supporting cells (Sertoli
cells)
o surrounded by interstitial loose connective tissue
rich in blood vessels, lymphatic vessels, nerves, and
endocrine interstitial cells (Leydig cells)
Function
production of male gametes
production of male sexual hormone
Castillo, Cerrillo, Chanyungco
Figure 4. Seminiferous tubule. myoid cells (M), interstitial (Leydig) cells
(IC), fibroblasts (F), spermatogonia (SG), Sertoli cells (SC), primary
spermatocytes (PS), connective tissue (CT)
Sertoli Cells
approximately columnar or pyramidal cells that largely
envelop cells of spermatogenic lineage
the bases adhere to the basal lamina and the apical
ends frequently extend to the lumen
Page 1 / 7
Histology of the Male Reproductive System
HD 201
has poorly defined outline in light microscopy due to
numerous
lateral
processes
surrounding
the
spermatogenic cells
contains receptors for follicle-stimulating hormone and
testosterone
Function
Nutrition and Development (of spermatogenic cells)
o lactate
o transferrin plasma protein for iron transport
o growth factors FGF, TGF, TGF, EGF, IGF
Other Secretions
o androgen-binding protein (ABP) concentrates
testosterone to a level required for spermiogenesis
o inhibin suppresses synthesis and release of FSH
in a feedback loop with the adenohypophysis
o anti-Mllerian hormone (AMH) / Mllerianinhibiting substance (MIS) causes regression of
the embryonic Mllerian ducts
Structural Functions
o blood-testis barrier formed by tight occluding
junctions between the basolateral membranes of
adjacent Sertoli cells
Blood-Testis Barrier
prevents autoimmune attacks against the spermatogenic
cells
progeny spermatocytes might express different plasma
membrane antigens compared to spermatogonia, thus
the testis might recognize it as non-self
also functions in conserving Sertoli cell secretory
products like androgen-bindring protein
tightest blood-tissue barrier in mammals
Figure 6. Interstitial tissue. myoid cells (M), interstitial (Leydig) cells
(IC), seminiferous tubule (ST)
Spermatogenesis
process by which spermatogonia (primitive germ cells)
become spermatozoa (mature, highly-specialized
gametes)
involves spermatocytogenesis (period of cellular
division) and spermiogenesis (metamorphic period
where no cellular division occurs)
process requires FSH and LH for testosterone
synthesis and maximal sperm production
some effects of testosterone including male
reproductive tract functions and spermatohgenesis
are mediated by estradiol and dihydrotestosterone
(DHT)
the hormones do not directly affect the germ cells;
rather, the effects are mediated by Sertoli cells
Spermatocytogenesis
Stages associations of cells in different states of
differentiation (I-VI) lasting 16 days
Waves adjacent areas containing different groups of
cells in certain stages
Cycles length of time for stages to reoccur in a
segment of the tubule (considering there are 4 cycles for
completion, 4 x 16 days = 64 days minimum)
Stages of Development
Figure 5. Blood-testis barrier. (Source: http://os1.amc.nl/celbiologie/
20122013/auc/mannelijk/graphics/c0000001.jpg)
Interstitial Tissue
filled with connective tissue containing
o mast cells and macrophages
o nerves
o lymphatics
o blood vessels
o interstitial cells of Leydig.
Leydig Cells
rounded or polygonal cells with central nuclei and
eosinophilic cytoplasm rich in small lipid droplets
contains receptors for luteinizing hormone
activated during embryonic life and puberty
Function
synthesis and endocrine secretion of testosterone
Embryonic Life
o testosterone synthesis stimulated by human
chorionic gonadotropin (hCG)
o testosterone needed for the development of ducts
and other parts of the male reproductive system
Puberty
o testosterone synthesis stimulated by luteinizing
hormone (LH) from the adenohypophysis
o testosterone needed for development of the
secondary male sex characteristics
Castillo, Cerrillo, Chanyungco
Spermatogonia
primitive germ cells located basally in the epithelium next
to the basement membrane
Type A
o Type A0 / Ad (stem cells)
dark; undergo clonal division but rarely divide
o Type A1 / Ap (progenitor cells)
pale; eventually divide into Type B
Type B
o undergo further mitosis
o final mitosis results in primary spermatocytes
o cellular divisions have incomplete cytokinesis thus
cells remain attached to one another via
cytoplasmic intercellular bridges
Spermatocytes
Primary Spermatocytes
o undergo meiosis I with a prolonged prophase (22
days)
o meiosis I is completed within the adluminal
compartment
Secondary Spermatocytes
o undergo rapid completion of meiosis II to produce
spermatids
o chromosomal cross-over occurs
Spermatids
thin, elongated cells with darker, more condensed nuclei
undergo spermiogenesis to become full-fledged and
mature spermatozoa
Page 2 / 7
Histology of the Male Reproductive System
HD 201
testosterone
o converted to dihydrotestosterone (DHT) and
estradiol which are essential for spermatogenesis
and normal development of tract organs
o exerts negative feedback on HPO axis
dual regulation both FSH and LH required for
quantitatively normal spermatogenesis (initiation /
maintenance / reinitiation)
Temperature Regulation
spermatogenic DNA polymerase B and recombinase
prefer lower optimal temperature (2 C lower than core
body temperature)
cryptorchidism (undescended testis) have no effect on
testosterone, however, body temperature may affect
enzymes
Regulation
o scrotum has thin skin, no fat, but have sweat glands
o cremaster muscle lowers or raises the testes
o dartos muscle tightens or loosens scrotal skin
o pampiniform plexus cools arterial blood near venous
blood via counter-current mechanism; this also
retains testosterone within testis)
INTRATESTICULAR DUCTS
within the mediastinum testis
cells arriving at the intratesticular ducts are still unable to
swim on their own
convey spermatozoa and liquid out of the testis to
efferent ducts
Tubuli Recti
Figure 7. Spermatogenesis.
Spermiogenesis
final stage in sperm production
process where spermatids transform to spermatozoa
no cell division occurs during this process
Phases
Golgi Phase
o migration of mitochondria to one end of the nucleus
o packaging of acrosomal enzymes by Golgi body
Cap Phase
o condensation of chromatin, elongation of body
o formation of acrosomal cap
Acrosomal Phase
o further condensation of nucleus
o elongation of one centriole as flagellum
Maturation Phase
o formation of axoneme and midpiece
o shedding of excess cytoplasm as polar (residual)
body
short, straight, narrow connecting passageways from the
seminiferous tubules to the rete testis
epithelium: low columnar (similar to Sertoli cells)
rare to find in slide preparations and hard to identify
Rete Testis
a labyrinth of epithelium-lined channels embedded in the
fibrous stroma of the mediastinum testis
connected to the head of the epididymis via 10-20
efferent ductules (ductuli efferentes)
epithelium: cuboidal
tends to be all over the place when looking at the
mediastinum testis
has irregular openings (vs oval shape of seminiferous
tubules)
Figure 8. Spermiogenesis.
Spermiation
release of spermatids from the seminiferous tubules (60
days)
removal of excess cytoplasm and organelles (polar body)
o migrates distally as the immotile sperm moves
distally in the reproductive tract (testosterone
required)
glycoprotein coat around the acrosome
o removed by male FPP (fertilization-promoting
polypeptide) and female heparin
Hormonal Influences
FSH initiation of spermatogenesis prior to puberty
LH initiation of spermatogenesis (via testosterone)
after puberty
Castillo, Cerrillo, Chanyungco
Figure 9. Magnified view of a seminiferous tubule, straight tubule, and
rete testis. rete testis (R), tubulus rectus (T), seminiferous tubule (S)
Page 3 / 7
Histology of the Male Reproductive System
HD 201
Epididymis
Figure 10. Straight tubule (tubulus rectus) connecting a seminiferous
tubule to the rete testis. rete testis (R), connective tissue (CT) of the
mediastinum, tubulus rectus (T), seminiferous tubule (S)
single highly coiled tube about 6 meters long consisting
of 4 parts:
o initial segment
o caput (proximal region) with contractile and
peristaltic smooth muscle layer
o corpus (middle region) final maturation site of
sperm where cytoplasm in the tail is removed and
sperm becomes motile. However, they will still need
to rely on epididymis for complete motility.
o cauda (distal region) storage site of sperm (10-14
days after spermiation), contractile only during
sexual stimulation
epithelium: pseudostratified columnar cells with nonmotile stereocilia and regenerative basal cells
has smooth circular lumen (vs scallop shaped
appearance of ductuli efferetes)
place where sperm cells are stored until they are needed
once sperm cells enter the epididymis, it reaches the
middle or corpus region via peristaltic contractions
once sperm cells are able to swim (only forward
direction), theyll be released during sexual stimulation
during intercourse
Figure 11. Micrograph showing simple cuboidal epithelium lining the
rete testis (R).
EXTRATESTICULAR DUCTS
Ductuli Efferentes (Efferent Ductules)
drains the rete testis and empty into the epididymis
epithelium: non-ciliated cuboidal cells alternating with
taller ciliated cells
o shorter cells: more absorptive
o taller cells: more ciliated
this unique arrangement gives a scalloped-appearance
of the cells lining the epithelium (interspersed tall and
short cells)
ciliary action in the ductuli epithelial wall propels the still
non-motile spermatozoa towards the epididymis
removes 90% of testicular fluid (water, ions, proteins)
and concentrates secretions leading to a high
concentration of sperm cells than fluid volume
these might have a small lumen and may be confused
with seminiferous tubules containing spermatids
require FSH and estrogen receptors
Figure 12. Efferent ductules (E) lined by a simple epithelium consisting
of patches of cuboidal cells with water-absorbing microvilli alternating
with patches of taller ciliated cells.
Castillo, Cerrillo, Chanyungco
Figure 13. Epididymis. tunica vaginalis (TV), blood vessels (V), duct of
epididymis (DE), stereocilia (arrow)
Figure 14. The epididymis consists of pseudostratified columnar
epithelium surrounded by connective tissue. basal cell (B), smooth
muscle (SM), sperm (S) in the epididymal lumen
Page 4 / 7
Histology of the Male Reproductive System
Ductus (Vas) Deferens
long straight tube with thick, muscular wall
epithelium: pseudostratified columnar epithelium with
sparse stereocilia
mostly muscular with a small lumen and folded mucosa
highly muscular with a middle circular layer of smooth
muscle in between two longitudinal layers
secretes the second fraction of ejaculate (5%) which
allow sperm motility
HD 201
developed from vas deferens, looks like the prostate but
more tubular
epithelium: pseudostratified columnar epithelium thrown
into numerous branching mucosal folds
surrounded by two layers of smooth muscle (inner
circular, outer longitudinal)
produces the third fraction of semen (46-80%)
o helps with how the sperm cells will function in the
female reproductive tract
o fructose food for the sperm
o prostaglandins suppression of female immune
system; decreased response to inflammation
o flavins give semen an off-white to yellowish color;
fluorescent (used in CSI to locate presence of
semen)
o fertilization-promoting peptide (FPP)
keep acrosomal cap intact
serve as protective structure as sperm enters
female genital tract
influences gel formation
Summary of Fractions of Semen
1st Fraction survival in reproduction prostate
2nd Fraction swimming environment vas deferens
3rd Fraction nutrients and substances for function
later in the female reproductive tract seminal vesicle
Functions
these secretions become a coagulum once it enters the
female reproductive tract
forms a viscous gel which is the protective mechanism of
sperm cell to wait until the female immune response dies
down (since sperm cells are recognized as foreign cells)
melting of coagulum requires:
o fibrinolysin (from the Golgi)
o heparin (from female reproductive system)
Figure 15. Vas deferens cross section. mucosa (M), longitudinal
smooth muscle (L-SM), circular smooth muscle (C-SM)
Figure 16. Pseudostratified columnar epithelium of the vas deferens.
lamina propria (LP)
Figure 17. Seminal vesicle mucosa characterized of numerous folds
(arrows) giving the lumen (L) a distinctive appearance. smooth muscle
(SM)
Urethra
Membranous Urethra shortest and least dilatable
Prostatic Urethra most dilatable, usually 3 cm long
Penile Urethra (Spongy Urethra) longest, dilated at
the bulb and glans penis
ACCESSORY GLANDS
does not produce sperm
produces other secretions that contribute to the semen
Semen - the fluid expelled during ejaculation consisting
of seminal fluid and spermatozoa, including some
desquamated duct lining cells
Seminal Vesicles
a single, blind-ended, highly tortuous tube around 15 cm
in length, but does not serve any storage function
Castillo, Cerrillo, Chanyungco
Figure 18. Seminal vesicle mucosal folds contain smooth muscles (SM)
covered by a thin lamina propria (LP)
Page 5 / 7
Histology of the Male Reproductive System
Prostate
found under the bladder
a compound tubuloalveolar gland (30-50 branched
tubuloalveolar units) surrounded by a dense
fibromuscular stroma (important in pathology)
epithelium:
o 30-50 secretory alveoli (pseudostratified columnar)
secreting into 15-25 excretory ducts (transitional)
o the secretory and ductal portions are embedded in
the stroma
produces the first fraction of ejaculate (13-33%)
o help sperm survive in thefemale tract by
coagulating and de-coagulating on time
o citric acid
o fibrinolysin makes semen fluid-like in female
tract and helps activate the acrosomal cap
o acid phosphatase
o prostate-specific antigen (PSA)
o zinc to ensure the health of sperms
o fertilization-promoting peptide (FPP)
HD 201
Zones of the Prostate
all glands are lateral and posterior to the urethra
zones are not that appreciable in light microscopy
Anterior Fibromuscular Stroma (AFS)
no glands, non-secretory, mostly fibers
Transitional Zone
surrounds proximal urethra
5-10% of prostatic tissue
10-20% source of prostate cancer
origin of benign prostatic hypertrophy (BPH)
Central Zone
surrounds ejaculatory ducts
25% of volume
5% of prostate cancers (more aggressive due to
contiguous structures around it: seminal vesicle, vas
deferens, blood supply)
Peripheral Zone
posterolateral region
70% of volume
largest zone and occupies most of the prostate
65-80% source of prostate cancer
Figure 21. Organization of the prostate gland.
Clinical Correlates
Figure 19. Small tubuloalveolar glands (G) embedded within a dense
fibromuscular stroma (S).
Corpora Amylacea
small spherical concretions, often calcified
laminated amyloid structures
present as early as during fetal development
increases past 50 years old
higher occurrences in elderly
related to epithelialdegeneration
does not indicatehealth or age of the prostate
therefore, it has no clinical significance
Prostate Cancer
usually begins at the peripheral zone; more aggressive
forms of cancer arise from the smaller zones of the
prostate
treated differently depending on the site of malignancy
(either fibromuscular or secretory)
cancers within the core of the prostate are more
aggressive and deadlier
Benign Prostatic Hypertrophy
symptoms of (dysuria, nocturia, difficulty in initiating
streams, dribbling) is due to the hypertrophy of the
transitional zone which compresses the urethra.
Digital Rectal Exam
wear gloves, lubricate and after inserting, palpate
anteriorly to feel the prostate
o normal: small and soft
o tumor: hard
o benign hypertrophy: large and soft
in females, insert other finger through the vagina to
check if there are fistulas
Bulbourethral Glands (Cowpers Glands)
paired tubuloalveolar glands
epithelium: mucus-secreting simple columnar
epithelium
function: to make pre-ejaculate fluid, which lubricates
urethra forsperm; washes out urine (2-3%) which is
acidic
pre-ejaculate fluid may contain sperm, thus, it can get
a girl pregnant (why withdrawal method fails)
Figure 20. A prostate tubuloalveolar unit including a corpus amylaceum
(CA) concretion. smooth muscle (M), lamina propria (LP),
pseudostratified columnar epithelium (E)
Castillo, Cerrillo, Chanyungco
Page 6 / 7
Histology of the Male Reproductive System
HD 201
.
Baby you're all that I want, when you're lyin' here in my
arms, I findin' it hard to believe, we're IN HIBIN ...
Capacitance
initiated by FPP
Destabilization of Acrosomal Cap
so that genetic material of male can combine with that of
the female
removal of steroids and glycoproteins
more fluid membrane
Increased Calcium Permeability
increased cAMP, increased
forward
motility,
hypermotility
Decreased Level of FPP
overly high levels of FPP prevent capacitation sperms
cant swim
decreases within vaginal secretions
Male Fertility
Normal Semen and Sperm
20 million sperms per mL
2 mL total volume of semen
40 million sperms present per ejaculate
30% of the sperms should be mature and developed
75% of the sperms should be alive or viable
25% of the sperms should be swimming with rapid
forward movement
50% of the sperms should be swimming even if they
are sluggish
Causes of Male Infertility
Organic
Hypothyroidism high TSH might increase prolactin
hyperprolactinemia
conginetal adrenal hyperplasia too much androgens
panhypopituitarism lack of GH
hypogonadal hypopituitarism
varicocoele enlargement of pampiniform plexus
cryptorchidism undescended testis
testicular torsion
damaged ducts
infection (TB, mumps, typhoid, gonorrhea, syphilis)
Klinefelters syndrome extra X chromosome
Inorganic
smoking significantly decreases both sperm count and
sperm cell motility
prolonged use of marijuana and other recreational drugs
chronic alcohol abuse
anabolic steroid use causes testicular shrinkage
overly intense exercise produces high levels of adrenal
steroid hormones leading to testosterone deficiency
malnutrition and anemia including inadequate vitamin C
and zinc in the diet
tight underwear increases scrotal temperature
exposure to environmental hazards and toxins
pesticides, lead, paint, radiation, radioactive substances,
mercury, benzene, boron, heavy metals
excessive stress
Bryan Adams - Hibin
#3
Knock, knock!
.
Mitosis
.
.
MITOSIS, my knees, my shoulder, my head ...
#4
The Egg
.
.
.
Meaning: NALAMANGAN
Example: Wala ka pala eh! The egg na naman kita! Hahaha!
#5
Bakit malungkot ang mammalian embryo?
.
.
.
Kasi ALLANTOIS
#6
Anong TV programs and pinapanood ng mga mammalian
embryo?
.
.
.
E di CHORIONovelas
Carlos: Hello to my other anatomates (Anna x 2 and Earl)! Shoutout sa mga daga namin sa research, plz dont die. Congratulations
sa Medrhythmics sa MGMR, sobrang galing niyo! At siyempre,
hello kay Abby O.
Giselle: Ang tunay na lalaki, hindi nagsusuot ng skinny jeans.
Overly intense exercise is bad for your sperm kaya okay lang
maging chubby. :p
End of Transcript
#1
Knock, knock!
.
Inhibin
.
.
Would you know my name, if I saw you IN HIBIN ?..
Eric Clapton Tears in Hibin
#2
Knock, knock!
.
Inhibin (again)
.
Castillo, Cerrillo, Chanyungco
Page 7 / 7
Anda mungkin juga menyukai
- Histology Class Notes: The Big PictureDari EverandHistology Class Notes: The Big PicturePenilaian: 5 dari 5 bintang5/5 (1)
- Last Minute Embryology: Human embryology made easy and digestible for medical and nursing studentsDari EverandLast Minute Embryology: Human embryology made easy and digestible for medical and nursing studentsBelum ada peringkat
- Histology ImagesDokumen10 halamanHistology ImagesLilliana Beltran100% (1)
- Histology SlidesDokumen26 halamanHistology SlidesDhruvJaiswal100% (2)
- Histology: An IntroductionDokumen46 halamanHistology: An IntroductionSarah100% (2)
- Histology ExamsDokumen2 halamanHistology Examsqarafi4007Belum ada peringkat
- Histology Quiz 3Dokumen10 halamanHistology Quiz 3Nick JacobBelum ada peringkat
- HistologyDokumen6 halamanHistologyMikaela Joy Villaflores CortesBelum ada peringkat
- Histology UnkownsDokumen11 halamanHistology UnkownsBec Jeans100% (2)
- Histology Practice PracticalDokumen38 halamanHistology Practice PracticalDeep Patel88% (8)
- Histology: Lecture NotesDokumen97 halamanHistology: Lecture Notessky100% (4)
- Histology of Ear and EyeDokumen2 halamanHistology of Ear and EyeAnny Alvrz100% (1)
- GI Tract Histology SummaryDokumen5 halamanGI Tract Histology SummaryFluffy_iceBelum ada peringkat
- Connective TissueDokumen7 halamanConnective TissueSheena Pasion100% (1)
- Digestive HistologyDokumen11 halamanDigestive HistologyFahd Abdullah Al-refai100% (2)
- Histology NotesDokumen4 halamanHistology NotesThonieroce Apryle Jey Morelos100% (3)
- Epithelium and Connective Tissue NotesDokumen8 halamanEpithelium and Connective Tissue NotesMiguel Mansilla100% (1)
- Histology Test Bank PrelimsDokumen40 halamanHistology Test Bank Prelimsjed larsen capulong gavino100% (8)
- Embryology TimelineDokumen3 halamanEmbryology TimelineGillianWalcottBelum ada peringkat
- Histology of The Respiratory SystemDokumen62 halamanHistology of The Respiratory Systemmichelle100% (1)
- Human Physiology LecturesDokumen171 halamanHuman Physiology LecturesPhysiology by Dr Raghuveer57% (7)
- Histology PlacentaDokumen26 halamanHistology Placentakhiks34100% (2)
- Histology Notes (Edited)Dokumen10 halamanHistology Notes (Edited)Lo Jia HuiBelum ada peringkat
- Slide N Label HistologyDokumen35 halamanSlide N Label HistologyIsidore Patrick100% (2)
- Histology StainsDokumen7 halamanHistology StainsFrozenMan100% (2)
- Epithelial Tissue - Overview PDFDokumen9 halamanEpithelial Tissue - Overview PDFAslak TorgersenBelum ada peringkat
- Histology of The EAR Histology of The EARDokumen21 halamanHistology of The EAR Histology of The EARhendri67% (3)
- Histology, Lecture 6, Connective Tissues (Lecture Notes)Dokumen6 halamanHistology, Lecture 6, Connective Tissues (Lecture Notes)Ali Al-Qudsi100% (3)
- Characteristics of Histology SlidesDokumen4 halamanCharacteristics of Histology SlidesLaiq Khan100% (1)
- Histology of The Special SenseDokumen84 halamanHistology of The Special SenseRushda100% (1)
- Simple Squamous Epithelium: VRMM2023Dokumen5 halamanSimple Squamous Epithelium: VRMM2023VERONICA ROSE MAGPOCBelum ada peringkat
- Histology Slides EpitheliumDokumen3 halamanHistology Slides EpitheliumNourhan JamalBelum ada peringkat
- (HISTOLOGY) Endocrine SystemDokumen11 halaman(HISTOLOGY) Endocrine Systemwipi112Belum ada peringkat
- Histology Slide GuideDokumen50 halamanHistology Slide GuideEldar Sulejmanovic100% (2)
- Anatomy and Physiology Chapter 2 Test Flash CardsDokumen8 halamanAnatomy and Physiology Chapter 2 Test Flash Cardsmalenya1Belum ada peringkat
- Histology Practical Study GuideDokumen4 halamanHistology Practical Study GuideNewshaSajadi100% (1)
- AnatomyDokumen45 halamanAnatomyrkoppikarBelum ada peringkat
- Teach Yourself HistologyDokumen19 halamanTeach Yourself HistologySambili Tonny100% (1)
- 1st Year MBBS Histology Slides and Identification Points (FINAL)Dokumen57 halaman1st Year MBBS Histology Slides and Identification Points (FINAL)Lucas Victor Almeida50% (6)
- Blood Physiology Part 2 Dr. OlivarDokumen5 halamanBlood Physiology Part 2 Dr. OlivarJorelyn FriasBelum ada peringkat
- Respiratory System PhysiologyDokumen35 halamanRespiratory System PhysiologySherwan R Shal100% (2)
- Special Senses Hearing and EquilibriumDokumen17 halamanSpecial Senses Hearing and EquilibriumMompati Letsweletse100% (1)
- Histology of Female Reproductive System 2020Dokumen45 halamanHistology of Female Reproductive System 2020Devina Kriskineya100% (2)
- Cells and Tissues: Lecture Presentation by Patty Bostwick-Taylor Florence-Darlington Technical CollegeDokumen66 halamanCells and Tissues: Lecture Presentation by Patty Bostwick-Taylor Florence-Darlington Technical CollegeNishith100% (4)
- Connective Tissue TypesDokumen2 halamanConnective Tissue Typesraphael100% (2)
- Anatomy Physiology The Endocrine System MCQ ExamDokumen37 halamanAnatomy Physiology The Endocrine System MCQ Examaminata6100% (4)
- Reproductive SystemDokumen42 halamanReproductive SystemAileen Grace Delima100% (1)
- Pathology Lecture SeriesDokumen168 halamanPathology Lecture SeriesButch DumdumBelum ada peringkat
- Physiology of HomeostasisDokumen17 halamanPhysiology of HomeostasisRamadan PhysiologyBelum ada peringkat
- Histology of Digestive SystemDokumen100 halamanHistology of Digestive SystemFadhila Putri Palupi100% (3)
- Histology Questions QuizDokumen28 halamanHistology Questions QuizminervamoonBelum ada peringkat
- Module 4 - Tissues StudentDokumen40 halamanModule 4 - Tissues StudentYaemi Yormi100% (1)
- Histology Practical ExamDokumen7 halamanHistology Practical ExamMicky MoranteBelum ada peringkat
- Anatomy & Physiology - AllDokumen15 halamanAnatomy & Physiology - AllAnubhav ShuklaBelum ada peringkat
- Respiratorysystem 120105050542 Phpapp01Dokumen43 halamanRespiratorysystem 120105050542 Phpapp01Buuvee BeBelum ada peringkat
- Histology Notes 2Dokumen13 halamanHistology Notes 2Lukas BüchlerBelum ada peringkat
- Anatomy and Physiology of NoseDokumen32 halamanAnatomy and Physiology of NoseBinita ShakyaBelum ada peringkat
- Anatomy QuestionsDokumen133 halamanAnatomy QuestionsNatukunda DianahBelum ada peringkat
- Eng - PDF JsessionidDokumen2 halamanEng - PDF JsessionidMaxine AlbaBelum ada peringkat
- ER Monitoring SheetDokumen3 halamanER Monitoring SheetMaxine AlbaBelum ada peringkat
- Eng PDFDokumen34 halamanEng PDFAkbar RihansyahBelum ada peringkat
- Absite January2014 ReviewDokumen1.226 halamanAbsite January2014 ReviewAnnTran100% (12)
- Environmental EmbryologyDokumen22 halamanEnvironmental EmbryologyMaxine AlbaBelum ada peringkat
- Penicillins: Strep Pneumoniae S. AureusDokumen10 halamanPenicillins: Strep Pneumoniae S. AureusMaxine Alba100% (1)
- Third World - STSDokumen4 halamanThird World - STSMaxine AlbaBelum ada peringkat
- The Scientific Research CommunityDokumen6 halamanThe Scientific Research CommunityMaxine AlbaBelum ada peringkat
- MHEG 2 QuizDokumen2 halamanMHEG 2 QuizMaxine AlbaBelum ada peringkat
- Anatomy of The Gene: Promoters and Enhancers (Gilbert, p.39)Dokumen2 halamanAnatomy of The Gene: Promoters and Enhancers (Gilbert, p.39)Maxine AlbaBelum ada peringkat
- Human Sensory ReceptionDokumen55 halamanHuman Sensory ReceptionMaxine AlbaBelum ada peringkat
- Schematic DiagramDokumen4 halamanSchematic DiagramMaxine AlbaBelum ada peringkat
- Cell Transport: Diffusion in Colloidal MediumDokumen3 halamanCell Transport: Diffusion in Colloidal MediumMaxine AlbaBelum ada peringkat
- Note GuideDokumen2 halamanNote GuideDemetrius Hobgood0% (1)
- 144 Diagnosa FKTPDokumen5 halaman144 Diagnosa FKTPpuskesmas100% (1)
- Effect of Adding Different Levels of Olive Leaf Powder To The Diet On The Production Performance and Some Physiological Characteristics of BroilersDokumen9 halamanEffect of Adding Different Levels of Olive Leaf Powder To The Diet On The Production Performance and Some Physiological Characteristics of BroilersreviewjreBelum ada peringkat
- Annatomy Notes For Bpe StudDokumen14 halamanAnnatomy Notes For Bpe StudYoga KalyanamBelum ada peringkat
- Short Stories For KidsDokumen14 halamanShort Stories For KidsSherine Lois QuiambaoBelum ada peringkat
- Life Cycle of Leishmania SPDokumen3 halamanLife Cycle of Leishmania SPUttam Kr PatraBelum ada peringkat
- Airway Management 1Dokumen17 halamanAirway Management 1kamel6Belum ada peringkat
- DR FdarDokumen2 halamanDR FdarHenry Philip Sabado Presto0% (1)
- 9700 m16 Ms 42 PDFDokumen10 halaman9700 m16 Ms 42 PDFsamihaBelum ada peringkat
- Lecture Notes - BIOS1170B (Body Systems - (Structure and Function) ) (Sydney)Dokumen86 halamanLecture Notes - BIOS1170B (Body Systems - (Structure and Function) ) (Sydney)SK AuBelum ada peringkat
- Development of The Fetal Membranes and PlacentaDokumen4 halamanDevelopment of The Fetal Membranes and PlacentaBandula KusumsiriBelum ada peringkat
- What Is Tetralogy of FallotDokumen2 halamanWhat Is Tetralogy of FallotJamaica Cruz San Pedro100% (1)
- Petri DishDokumen7 halamanPetri DishMizzannul HalimBelum ada peringkat
- A To Z Orthodontics Vol 3 Malocclusion1Dokumen36 halamanA To Z Orthodontics Vol 3 Malocclusion1Ishtiaq HasanBelum ada peringkat
- Down SexDokumen14 halamanDown SexRuslan ZhuravskyBelum ada peringkat
- The Periodontal Ligament: A Unique, Multifunctional Connective TissueDokumen21 halamanThe Periodontal Ligament: A Unique, Multifunctional Connective TissueSamuel Flores CalderonBelum ada peringkat
- Blood DopingDokumen16 halamanBlood Dopingpriyanka lalwaniBelum ada peringkat
- Uterovaginal ProlapseDokumen16 halamanUterovaginal Prolapseapi-3705046100% (1)
- Nutrition: Important ConceptsDokumen12 halamanNutrition: Important ConceptshafizaqaiBelum ada peringkat
- Samphire2003 PDFDokumen9 halamanSamphire2003 PDFYacine Tarik AizelBelum ada peringkat
- Schirmer TestDokumen3 halamanSchirmer TestRisa UtamiBelum ada peringkat
- College Prep Main Ideas WorksheetDokumen10 halamanCollege Prep Main Ideas Worksheetlorrainecarrillo18Belum ada peringkat
- The Little Book of Sexual HappinessDokumen40 halamanThe Little Book of Sexual Happinesswolf4853100% (2)
- Top 93 Nursing Skills, Procedures and Normal Values - OkDokumen26 halamanTop 93 Nursing Skills, Procedures and Normal Values - OkWilmaBongotanPadawil100% (1)
- BSCI 4001 Transcript MidtermDokumen4 halamanBSCI 4001 Transcript MidtermLynell Caraang BarayugaBelum ada peringkat
- Ascaris Suum PDFDokumen6 halamanAscaris Suum PDFAdinda RahmaBelum ada peringkat
- Nur112: Anatomy and Physiology ISU Echague - College of NursingDokumen14 halamanNur112: Anatomy and Physiology ISU Echague - College of NursingWai KikiBelum ada peringkat
- Articulo 3Dokumen5 halamanArticulo 3Valeria Rodriguez GomezBelum ada peringkat
- Variability and Accuracy of Sahlis Method InEstimation of Haemoglobin ConcentrationDokumen8 halamanVariability and Accuracy of Sahlis Method InEstimation of Haemoglobin Concentrationastrii 08Belum ada peringkat
- EsquistocitosDokumen10 halamanEsquistocitoswillmedBelum ada peringkat