JPEN J Parenter Enteral Nutr-2011-Zamberlan-523-9 PDF
Diunggah oleh
arawindahaniastriJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
JPEN J Parenter Enteral Nutr-2011-Zamberlan-523-9 PDF
Diunggah oleh
arawindahaniastriHak Cipta:
Format Tersedia
Original Communication
Nutrition Therapy in a Pediatric
Intensive Care Unit: Indications,
Monitoring, and Complications
Journal of Parenteral and
Enteral Nutrition
Volume 35 Number 4
July 2011 523-529
2011 American Society for
Parenteral and Enteral Nutrition
10.1177/0148607110386610
http://jpen.sagepub.com
hosted at
http://online.sagepub.com
Patrcia Zamberlan, MSc1; Artur Figueiredo Delgado, MD2; Cludio Leone, PhD3;
Rubens Feferbaum, MD4; and Thelma Suely Okay, PhD4
Financial disclosure: None declared.
Background: Nutrition therapy (NT) is essential for the care of
critically ill children. Inadequate feeding leads to malnutrition
and may increase the patients risk of morbidity and mortality.
The aim of this study was to describe the NT used in a tertiary
pediatric intensive care unit (PICU). Methods: The authors
evaluated NT administered to 90 consecutive patients who
were hospitalized for 7 days in the PICU of Instituto da
Criana, Hospital das Clnicas, Universidade de So Paulo,
Brazil. NT was established according to the protocol provided
by the institutions NT team. NT provided a balance of fluids
and nutrients and was monitored with a weekly anthropometric nutrition assessment and an evaluation of complications.
Results: NT was initiated, on average, within 72 hours of hospitalization. Most children (80%) received enteral nutrition
(EN) therapy; of these, 35% were fed orally and the rest via
nasogastric or postpyloric tube. There were gastrointestinal
complications in patients (5%) who needed a postpyloric tube.
Parenteral nutrition (PN) was used in only 10% of the cases,
and the remaining 10% received mixed NT (EN + PN). The
average calorie and protein intake was 82 kcal/kg and 2.7 g/kg
per day. Arm circumference and triceps skinfold thickness
decreased. Conclusions: The use of EN was prevalent in the
tertiary PICU, and few clinical complications occurred. There
was no statistically significant change in most anthropometric
indicators evaluated during hospitalization, which suggests
that NT probably helped patients maintain their nutrition status. (JPEN J Parenter Enteral Nutr. 2011;35:523-529)
Clinical Relevancy Statement
Introduction
Undernutrition is highly prevalent in critically ill children
around the world, mainly in tertiary pediatric intensive care
units. Nutrition intervention with a focus on adequate
delivery of micro- and macronutrients guided by protocols
can improve the quality of treatment and aid in avoiding
further undernutrition. Knowledge of the sequential
anthropometric condition of admitted patients is essential
in providing early and sufficient nutrition support.
Despite technological advances, malnutrition is still widespread in pediatric intensive care units (PICUs). Studies
have shown that 24% to 55% of patients present with
acute or chronic malnutrition on admission and that
deterioration of nutrition status commonly occurs during
hospitalization.1-3
Critically ill children have a high risk of malnutrition because of stress-induced changes in intermediary
metabolism; these changes are characterized by an
increased basal metabolic rate and intensive protein
catabolism.4-6 In general, the development or perpetuation of malnutrition during hospitalization in the PICU
is due to illness, unknown nutrition condition, and an
inadequate supply of nutrients.7,8 In these patients, malnutrition is associated with physiologic instability. As a
result, more intensive clinical care is required, and the
mortality rate is high.6
Nutrition care studies have proposed that an early
intervention that targets nutrition assessment can prevent or minimize the complications of malnutrition.9,10
Nutrition therapy (NT) is indicated when a patient is
unable to receive calories and nutrients orally for a long
period of time. Enteral nutrition (EN) is preferred
Keywords: nutrition assessment; anthropometry; children;
nutrition therapy; enteral nutrition; parenteral nutrition
From the 1Division of Nutrition and 2Pediatric Intensive Care
Unit, Nutritional Team of Instituto da Criana do Hospital das
Clnicas da Faculdade de Medicina da Universidade de So
Paulo, So Paulo, Brazil; 3Department of Mother and Child
Health, Faculdade de Sade Pblica da Universidade de So
Paulo, So Paulo, Brazil; and 4Department of Pediatrics,
Faculdade de Medicina da Universidade de So Paulo, So
Paulo, Brazil.
Received for publication January 15, 2010; accepted for publication August 7, 2010.
Address correspondence to: Patrcia Zamberlan, Division of
Nutrition, Nutritional Team of Instituto da Criana do Hospital das
Clnicas da Faculdade de Medicina da Universidade de So Paulo,
So Paulo, Brazil; e-mail: pzamberlan@uol.com.br.
523
Downloaded from pen.sagepub.com by guest on June 7, 2015
524 Journal of Parenteral and Enteral Nutrition / Vol. 35, No. 4, July 2011
because it is more physiologic, promotes intestinal trophism, stimulates the immune system, and reduces the
incidence of bacterial translocation and sepsis; in addition, it presents fewer complications and costs less than
parenteral nutrition (PN).9,11,12 However, when it is
impossible to use the digestive tract, PN is the only
alternative for ensuring an adequate supply of nutrients
during hospitalization.13 The combination of PN and EN
may be useful for the first 72 hours of intensive clinical
care or when EN alone is not sufficient to meet the
nutrition demands of the patient.8,14-16
Although the consensus is that NT is essential in the
care of critically ill children, especially in the acute phase
of stress, its implementation remains the major challenge
in PICUs. Both PN and EN present risks. EN may be associated with gastric complications, which may affect tolerance and increase the risk of aspiration pneumonia. PN can
result in atrophy of the intestinal mucosa, liver abnormalities, hyperglycemia, and an increased risk of infectious complications.6,9
The main objective of this 1-year study was to
describe the restrictions, monitoring, and complications
associated with NT in a tertiary PICU.
Methods
Subjects
For this descriptive, prospective study, the participants
were selected from infants, preschool children, schoolchildren, and adolescents sequentially admitted to the
PICU of Instituto da Criana, Hospital das Clnicas da
Universidade de So Paulo, Brazil. This 15-bed, tertiary
ICU primarily attends to patients with chronic diseases,
according to the institutions specialties.
We studied 90 patients but did not include newborns,
those patients who stayed in the PICU for <7 days, and
children whose parents did not provide free and informed
consent.
This study was approved by the Research and Ethics
Committee of Instituto da Criana and the Commission
for Analysis of Research Projects, Faculty of Medicine,
Universidade de So Paulo.
Nutrition Therapy
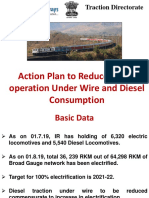
NT was initiated after hemodynamic stabilization and followed the approach determined by the NT team of
Instituto da Criana, summarized in Figure 1. The calories and nutrients (macronutrients and micronutrients)
required for parenteral or enteral feeding were calculated
daily. Increases were made according to feeding tolerance
and always aimed to meet the nutrition requirements of
each individual patient.
Monitoring of complications was performed during
the period of the NT, and nutrition status was evaluated
weekly.
Anthropometric Nutrition Assessment
Anthropometric nutrition assessment was carried out in
the first 24 hours of admission and repeated a week later.
To minimize the possibility of errors, all measurements
were carried out by the main author (PZ) of the study.
The assessment included weight (W), height (H) or
length (L), arm circumference (AC), and triceps skinfold
thickness (TST), according to the standards proposed by
Frisancho.17,18
We measured W with a scale that was calibrated for
accuracy before each use. Children who weighed >16 kg
were weighed standing, and infants were weighed using a
scale accurate to 5 g. Children who could not be weighed
independently were held by an adult (a parent or evaluator)
while being weighed. The childs weight was obtained by
subtracting the weight of the adult from the total weight of
the child and adult. L was measured in children aged 3 years
or younger using a pediatric anthropometer with an accuracy of 0.1 cm. Children were supine for the measurement.
In children older than 3 years, H was measured
using a wooden stadimeter with an accuracy of 0.1 cm.
In children whose condition prevented the use of conventional measuring techniques (eg, those patients who
were mechanically ventilated or taking vasoactive drugs),
H was predicted from measurements of the distance
between the knee and ankle with the child kept in the
supine position. The length between the heel and the
anterior surface of the leg at the knee (femoral condyle)
was measured with a pediatric anthropometer. There
were the following equations proposed by Chumlea
et al19 in 1994:
White girls = 43.21cm + (2.15cm distance knee / ankle)
Black girls = 46.59cm + (2.02cm distance knee / ankle)
White boys = 40.54cm + (2.22cm distance knee / ankle)
Black boys = 39.60cm + (2.18cm distance knee / ankle)
Using the data for W and H or L, we obtained the
following indices: W/age (A), H/A or L/A, W/H or W/L.
We calculated body mass index for age (BMI/A) with the
following equation: BMI/A = W (kg)/H2 (m).
AC was measured with a metric tape marked in 0.5cm increments. Measurements were taken at the midpoint of the distance between the acromion and the
olecranon with the arm extended along the body.
TST was obtained using a Lange skinfold caliper
(Cambridge Scientific Industries, Cambridge, MD) with
constant pressure of 10 g/mm2 on the contact surface.
The measurement was taken on the back of the arm,
Downloaded from pen.sagepub.com by guest on June 7, 2015
Nutrition Therapy in Pediatric Intensive Care / Zamberlan et al 525
Nutrition assessment
NT
Is gastrointestinal tract
functioning?
No?
Yes?
EN
EN + PN
PN
Complete polymeric diet by
polyurethane or silicone
NGT
Intermittently every 3 or 4
hours
Gastric residue
(>50% of the volume infused),
abdominal distension,
vomiting, diarrhea
Failure 3 consecutive
times?
Medical
assessment
Continuous infusion 18 or
24 hours
Failure with
continuous infusion?
Tube placed in postpyloric
position; complete oligomers
diet
Failure?
PN
Figure 1. NT flow chart of Instituto da Criana, Hospital das Clnicas, Universidade de So Paulo, Brazil. EN, enteral nutrition;
NGT, nasogastric tube; NT, nutrition therapy; PN, parenteral nutrition.
parallel to the longitudinal axis, at the midpoint between
the acromion and olecranon. We used the average of 3
consecutive measurements.
Arm muscle circumference (AMC) and arm muscle
area (AMA) were calculated from the values of AC and
TST with the following equations: AMC (cm) = AC
(TSTx); AMA (cm2) = AMC2/4.
Nutrition status was determined from the z score for the
following indices: W/A, H/A or L/A, W/H or W/L, BMI/A,
AC/A, and AC/H. We used reference values from the
National Center for Health Statistics (NCHS)20 for children
older than 5 years and from the World Health Organization
(WHO)21 for children younger than 5 years old. EPI
Info, 2000 and WHO Anthro, 2006 were used for the
Downloaded from pen.sagepub.com by guest on June 7, 2015
526 Journal of Parenteral and Enteral Nutrition / Vol. 35, No. 4, July 2011
13 (14%)
36 (41%)
Table 2. Frequency of Malnutrition on Admission to
the Pediatric Intensive Care Unit (n = 90)a
Indicator
20 (22%)
21 (23%)
<2 years
2 to <5 years
5 to <10 years
10 to 20 years
Figure 2. Distribution of children (n = 90) assessed in the
pediatric intensive care unit (by age).
H/A or L/A
W/A
W/H or W/L
BMI/A
AC/A
TST
AMC
AMA
Cutoff Point
- 2 dp
- 2 dp
- 2 dp
- 2 dp
- 2 dp
p5
p5
p5
% Patients
50.0
27.7
8.0
13.3
47.8
33.0
46.6
45.5
A, age; AC, arm circumference; AMA, arm muscle area; AMC,
arm muscle circumference; BMI, body mass index; H, height; L,
length; TST, triceps skinfold thickness; W, weight.
a
According to various anthropometric indicators used in the
screening.
Table 1. Reasons for Hospitalization
Cause
n (%)
Sepsis or septic shock
Infection without sepsis
Postliver transplant
Postoperative
Respiratory failure
Epilepsy
Other, eg, Oncologic disease and dialytic
severe renal dysfunction
Total
22
20
11
9
5
1
22
(24.5)
(22.2)
(12.2)
(10.0)
(5.5)
(1.1)
(24.5)
90 (100.0)
calculations. TST, AMC, and AMA were classified by percentiles, according to the method of Frisancho.18
Statistical Analysis
The results were tabulated in an Excel (v 6.0; Microsoft,
Redmond, Washington) spreadsheet. The mean and standard deviation (SD) z scores were obtained for all anthropometric indicators (W/A, H/A or L/A, W/H, BMI/A,
AC/A, AC/H or AC/L, TST, AMC, and AMA) and for calories and protein.
To identify changes in anthropometric indicators over
time, we used the paired Student t test to perform comparative analyses between admission and the seventh day
of hospitalization. Data were considered statistically significant at P < .05, and a 95% confidence interval was
used for measures of central tendency.
We used SPSS Statistical Software (version 12.01;
SPSS Inc, Chicago, IL) to perform the calculations.
Results
Subjects
The study population consisted of 90 patients whose
median age was 35.5 months (2.9 years). The majority of
Figure 3. Types of nutrition therapy (NT) used during hospitalization in the pediatric intensive care unit. EN, enteral nutrition; PN, parenteral nutrition.
Oral
Ngt
Postpyloric Tube
Figure 4. Routes of enteral nutrition administration during
hospitalization in the pediatric intensive care unit. NGT,
nasogastric tube.
patients were younger than 2 years (Figure 2). There were
no statistically significant differences regarding gender
(46 females, 44 males).
During hospitalization in the PICU, 18 deaths
occurred, which corresponded to 20% of the cases. The
Downloaded from pen.sagepub.com by guest on June 7, 2015
Nutrition Therapy in Pediatric Intensive Care / Zamberlan et al 527
Table 3. Anthropometric Indicators (Means) on
Admission and on Day 7 of Hospitalization
Indicator
Admission
z W/A
z BMI/A
z AC/H
TST, mm
AMC, cm
AMA, cm2
0.95
0.43
1.37
9.2
12.5
13.2
Day 7 of Hospitalization
1.12
0.26
1.89
8.0
12.3
13.0
P
.152
.310
<.001a
<.001a
.221
.352
A, age; AC, arm circumference; AMA, arm muscle area; AMC,
arm muscle circumference; BMI, body mass index; H, height;
TST, triceps skinfold thickness; W, weight; z, z score.
a
Statistically significant (p < .05).
reasons for hospitalization in the PICU are shown in
Table 1. Of the 90 patients, 81 (90%) had an ailment. The
median length of stay in the PICU was 11 days.
Table 2 shows the frequency of malnutrition in 90
children admitted to the PICU, as determined by the
anthropometric indicators used in the screening.
Nutrition Therapy
Following hospitalization NT was started an average of 72
hours after hemodynamic stabilization. The sequential
nutrition assessment occurred on the seventh day of hospitalization, and most children (80%) had received EN; in
>50% of the EN recipients, the gastric route was used,
(Figures 3 and 4). Intermittent administration predominated, and only 1 child received continuous infusion. In
5% of the patients, the enteral tube was placed in the
duodenum because of the persistence of gastric residue
and/or abdominal distension; this procedure followed the
protocol of the NT team of Instituto da Criana, as previously described.
Among children who were prescribed oral diets, more
than half received no dietary restriction of nutrients, and
35% received a sodium-restricted diet, which was used
before hospitalization. The vast majority of patients admitted
to this tertiary PICU presented with an underlying disease
that required dietary restriction of nutrients (eg, sodium).
We chose a complete polymeric diet appropriate for
each age group, as suggested by the Dietary Reference
Intake (DRI) guidelines22; we administered these formulas via nasogastric tube. For postpyloric feeding, we chose
a complete oligomeric diet with a caloric density of 0.7
kcal/mL and 2 to 3 g of protein per 100 mL.
The average calorie and protein supply, with a week
of admission and during the course of therapy, corresponded to 82 kcal/kg/d (47 kcal/kg/d) and 2.7 g/kg/d
(1.9 g/kg/d), respectively, and the ratio of protein nitrogen to calories was 1:160. PN was used for 10% of the
children. In general, the volume and composition of the
PN formula met the macronutrient and micronutrient
recommendations suggested by the DRI.22
Sequential Anthropometric Nutrition Assessment
The comparative analysis (paired t test) between the
initial assessment (admission) and the seventh day of
hospitalization shows that there was a statistically significant difference in the z score mean of AC/H and in
the absolute average of TST (Table 3).
Discussion
Having a greater need for nutrients and limited energy
reserves will increase a childs risk of developing nutrition
deficiencies. This risk is especially high in critically ill children. Metabolic stress and an inadequate supply of nutrients
can result in malnutrition.7,23 Thus, assessment, monitoring,
and NT are of utmost importance in caring for these patients.
When we analyzed the characteristics of our study
population, we found no differences in gender and a predominance of children younger than 2 years of age, with
a median age of 2.9 years. Most children and adolescents
presented with an ailment. The PICU of Instituto da
Criana is considered tertiary and cares for children aged
2 months to 18 years, mainly those who are followed at
specialty clinics. The heterogeneity of this study population in terms of age and medical condition was acknowledged in Delgado et al,3 who studied the same population,
and by Alievi et al,24 who studied children in a PICU tertiary in Porto Alegre, Brazil.
Several studies have reported ICU mortality rates
between 9% and 38%,25,26 which are consistent with our
observed mortality rate of 20%.
In a study of the nutrition status of children in a tertiary, pediatric, neonatal ICU in the Netherlands, Hulst
et al1 reported that the nutrition status of their study participants was worse than that of the general population.
In this study, 24% of children were malnourished, and the
authors concluded that a considerable number of patients
required specialized NT during hospitalization in the
ICU. These characteristics were similar to those found in
our study. The high prevalence of malnutrition (H/A or
L/A = 50%, W/A = 27.7%, BMI/A = 13.3%, AC/A =
47.8%) among children and adolescents admitted to the
PICU could be explained by the high incidence of ailments (90%). In studies conducted in the 1980s, Pollack
et al27,28 found malnutrition rates ranging from 32% to
37% in patients with acute and chronic illnesses. In addition, Leite et al29 found 65% of their patients were malnourished, most of whom were recovering from cardiac
surgery. By comparing our results with theirs, we concluded that malnutrition in the PICU, as assessed by
anthropometry, has been present for the last 20 years and
is still very prevalent in these units. It is known that in
Downloaded from pen.sagepub.com by guest on June 7, 2015
528 Journal of Parenteral and Enteral Nutrition / Vol. 35, No. 4, July 2011
critically ill patients, anthropometric assessment is difficult to interpret because the measurements may be influenced by factors caused by disease or trauma, (eg, fluid
retention and swelling). However, the consensus is that
this assessment is very important for the nutrition evaluation and monitoring of patients in the PICU.1,3
Nutrition depletion is associated with physiologic
instability and an increased need for care in critically ill
children, and it could have a negative impact on growth
and neurologic development, especially in younger children. NT in the PICU is a challenge because it is common
to restrict liquids and discontinue feeding for diagnostic
and therapeutic procedures and also because some patients
have digestive intolerance.30 Nutrition intervention is
essential, and most PICUs should develop their own protocols and multidisciplinary teams for providing nutrition
support. In 2002, the American Society for Parenteral and
Enteral Nutrition updated guidelines for EN and PN
therapy, including strategies for critically ill children, such
as the following recommendations: nutrition assessment,
indirect calorimetry, predictive equations to avoid overfeeding, and administration of EN and PN.
EN has been the method of choice for NT in critically
ill patients. EN maintains the integrity of the intestinal
mucosa, thereby limiting bacterial translocation and
reducing the risk of sepsis; in addition, EN improves protein metabolism and caloric deficit.7 In general, EN is
safe and well tolerated by critically ill children, even those
who receive vasoactive drugs, which can reduce intestinal
perfusion.32,33 In our study, 80% of the patients received
EN, which was administered according to the PICUs NT
protocol. Since 2005, this EN protocol has enforced the
early use of NT that is specific for the clinical condition
of the patient. Although most patients received NT within
72 hours of hospitalization, others were treated later.
For most critically ill patients who receive EN, the
stomach is a more physiologic route, and tube placement
is simple and fast.34 However, some authors have documented that a nasogastric tube is not tolerated as well as a
postpyloric tube, particularly in patients who are being
mechanically ventilated; these patients often have reduced
gastric motility secondary to the administration of drugs
and the accumulation of gastric residue.35,36 Thus, a high
percentage of these children cannot receive adequate
nutrition, especially as a result of the frequent interruptions in EN.34 Postpyloric EN is an alternative because it
reduces the volume of gastric residue and the number of
interruptions in feeding.36,37 Because transpyloric EN
reduces gastric residue, it should also reduce the risk of
pulmonary aspiration and aspiration pneumonia. However,
this effect has not been observed. Meert et al32 found that
children with transpyloric EN achieved a higher caloric
intake than did those with gastric EN, but the incidence of
complications from gastric and pulmonary aspiration was
similar in both groups. In our study, a nasogastric tube was
used in 60% of children who received EN. Although most
patients were fasting when admitted to the hospital, they
received adequate nutrition support at the end of first
week, with an average energy intake of 82 kcal/kg/d and an
average protein intake of 2.7 g/kg/d. The patients clinical
condition was decisive in determining caloric requirements; however, there is always concern regarding hospital
malnutrition, which is a very important aspect for the
recovery of the patients. Moreover, these patients generally
have a deficient diet at home; their intake is influenced by
the clinical and nutrition aspects of the disease.
Only 5% of the patients required postpyloric EN because
of persistent gastric residues and/or abdominal distension. A
large proportion of critically ill patients receive gastric EN by
continuous infusion; this form of administration improves
feeding tolerance, reduces the gastric residual volume, and
thereby reduces the risk of aspiration. However, a recent
study found the same incidence of complications in patients
with continuous and intermittent EN. We used a form of
intermittent administration in most cases.
Compared with EN, the main disadvantage of PN is
the risk of infectious complications. In a group of 500
critically ill children evaluated prospectively, PN was
associated with an increased risk of infections.38 However,
in PICU patients who are unable to receive or tolerate
EN, PN should be indicated.6 In our study, 10% of the
children were unable to tolerate EN, and PN was indicated. To improve nutrition support, a mixed NT was
prescribed for 10% of the patients.
NT monitoring was performed by a sequential anthropometric assessment. We found a statistically significant
difference in H/A during hospitalization, and we believe
that this finding was caused by a potential measurement
error when there was a higher technical difficulty in
obtaining the L/H.
Metabolic stress causes intense proteolysis that
involves a large loss of muscle. In anthropometry, measurements of the arm, including AMC and AMA, are able
to estimate changes in the bodys protein stores. It is possible that critically ill patients exhibit decreased values of
these indicators during hospitalization in an ICU. In this
study, there was a statistically significant change in absolute average of TST and z score mean of AC/H, but we did
not observe a significant change in the median AMC or
AMA. However, it is difficult to determine whether
changes in nutrition status have taken place, because
anthropometric measurements can be influenced by
many factors, (eg, fluid shifts) in addition, 1 week of hospitalization is not necessarily long enough for significant
alterations to occur. Even so, anthropometric evaluation,
including nutrition assessment, is still important for a
critically ill patient. Delgado et al39 obtained similar findings, also justified by the short hospitalization time
(around 7 days) of these patients in an ICU. Furthermore,
although our study was descriptive, we observed that early
administration of NT was appropriate and possibly helped
our study participants maintain their nutrition status.
Downloaded from pen.sagepub.com by guest on June 7, 2015
Nutrition Therapy in Pediatric Intensive Care / Zamberlan et al 529
In summary, our data show that malnutrition is
prevalent in critically ill children. Nutrition intervention
in children, guided by a multidisciplinary team and nutrition support protocols and monitored by anthropometric
assessment, may help reduce nutrition deficits during
hospitalization in the PICU. It is possible to introduce
early gastric EN, and PN should be indicated when the
digestive tract is not functioning or when EN alone is
unable to meet the nutrition demands of the patient.
References
1. Hulst J, Joosten K, Zimmermann L, Hop W, et al. Malnutrition in
critically ill children: from admission to 6 months after discharge.
Clin Nutr. 2004;23:223-232.
2. de Neef M, Geukers VG, Dral A, Lindeboom R, Sauerwein HP,
Bos AP. Nutritional goals, prescription and delivery in a pediatric
intensive care unit. Clin Nutr. 2008;27:65-71.
3. Delgado AF, Okay TS, Leone C, et al. Hospital malnutrition and
inflammatory response in critically ill children and adolescents
admitted to a tertiary intensive care unit. Clinics (Sao Paulo).
2008;63:357-362.
4. Lavery GG, Glover P. The metabolic and nutritional response to
critical illness. Curr Opin Crit Care. 2000;6:233-238.
5. Slone DS. Nutritional support of the critically ill and injured
patient. Crit Care Clin. 2004;20:135-157.
6. Skillman HE, Wischmeyer PE. Nutrition therapy in critically ill infants
and children. JPEN J Parenter Enteral Nutr. 2008;32:520-534.
7. Briassoulis G, Zavras N, Hatzis T. Malnutrition, nutritional indices, and early enteral feeding in critically ill children. Nutrition.
2001;17:548-557.
8. Ista E, Joosten K. Nutritional assessment and enteral support of
critically ill children. Crit Care Nurs Clin N Am. 2005;17:385-393.
9. Gramlich L, Kichian K, Pinilla J, Rodych NJ, Dhaliwal R, Heyland
DK. Does enteral nutrition compared to parenteral nutrition result
in better outcomes in critically ill adult patients? A systematic
review of the literature. Nutrition. 2004;20:843-848.
10. Stratton RJ, Elia M. Who benefits from nutritional support: what
is the evidence? Eur J Gastroenterol Hepatol. 2007;19:353-358.
11. Artinian V, Krayem H, DiGiovine B. Effects of early enteral feeding
on the outcome of critically ill mechanically ventilated medical
patients. Chest. 2006;129:960-967.
12. Mazuski JE. Feeding the injured intestine: enteral nutrition in the
critically ill patient. Curr Opin Crit Care. 2008;14:432-437.
13. Koletzko B, Goulet O, Hunt J, et al. Guidelines on paediatric
parenteral nutrition of the European Society of Paediatric
Gastroenterology, Hepatology and Nutrition (ESPGHAN) and the
European Society for Clinical Nutrition and Metabolism (ESPEN),
supported by the European Society of Paediatric Research (ESPR).
J Pediatr Gastroenterol Nutr. 2005;41(suppl 2):S1-S87.
14. Heidegger CP, Romand JA, Treggiari MM, Pichard C. Is it now
time to promote mixed enteral and parenteral nutrition for the
critically ill patient? Intensive Care Med. 2007;33:963-969.
15. Heidegger CP, Darmon P, Pichard C. Enteral vs parenteral nutrition for the critically ill patient: a combined support should be
preferred. Curr Opin Crit Care. 2008;14:408-414.
16. de Lorenzo AG, Grau T, Montejo JC, Leyba CO, Santana SR;
SENPE-Baxter. III working meeting SENPE-Baxter: complementary parenteral nutrition in the critically ill patient [in Spanish].
Nutr Hosp. 2008;23:203-205.
17. Frisancho AR. Triceps skin fold and upper arm muscle size
norms for assessment of nutritional status. Am J Clin Nutr. 1974;
27:1052-1058.
18. Frisancho AR. Anthropometric Standards for the Assessment of
Growth and Nutritional Status. Ann Arbor, MI: University of
Michigan Press; 1999.
19. Chumlea WC, Guo SS, Steinbaugh ML. Prediction of stature from
knee height for black and white adults and children with application to mobility-impaired or handicapped persons. J Am Diet Assoc.
1994;94:1385-1391.
20. NCHS (National Center for Health Statistic). Growth Curves
Children Birth18. Washington, DC: National Center for Health
Statistics; 2000.
21. World Health Organization Multicentre Growth Reference Study
Group. WHO child growth standards based on length/height,
weight and age. Acta Paediatr Suppl. 2006;450:76S-85S.
22. Institute of Medicine. Dietary Reference Intakes for Energy,
Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and
Amino Acids. Washington, DC: National Academies Press; 2002.
23. Joosten KF, Hulst JM. Prevalence of malnutrition in pediatric hospital patients. Curr Opin Pediatr. 2008;20:590-596.
24. Alievi PT, Carvalho PR, Trotta EA, Mombelli Filho R. The impact of
admission to a pediatric intensive care unit assessed by means of global
and cognitive performance scales. J Pediatr (Rio J). 2007;83:488-490.
25. Rocker G, Cook D, Sjokvist P, et al. Clinician predictions of intensive care unit mortality. Crit Care Med. 2004;32:1149-1154.
26. Colpan A, Akinci E, Erbay A, Balaban N, Bodur H. Evaluation of risk
factors for mortality in intensive care units: a prospective study from
a referral hospital in Turkey. Am J Infect Control. 2005;33:42-47.
27. Pollack MM, Wiley JS, Holbrook PR. Early nutritional depletion in
critically ill children. Crit Care Med. 1981;9:580-583.
28. Pollack MM, Wiley JS, Kanter R, Holbrook PR. Malnutrition in
critically ill infants and children. JPEN J Parenter Enteral Nutr.
1982;6:20-24.
29. Leite HP, Isatugo MK, Sawaki L, Fisberg M. Anthropometric
nutritional assessment of critically ill hospitalized children. Rev
Paul Med. 1993;111:309-313.
30. Lambe C, Hubert P, Jouvet P, Cosnes J, Colomb V. A nutritional
support team in the pediatric intensive care unit: changes and factors impeding appropriate nutrition. Clin Nutr. 2007;26:355-363.
31. ASPEN Board of Directors and the Clinical Guidelines Task Force.
Guidelines for the use of parenteral and enteral nutrition in adult
and pediatric patients. JPEN J Parenter Enteral Nutr.
2002;26(suppl):1SA-138SA.
32. Meert KL, Daphtary KM, Metheny NA. Gastric vs small-bowel
feeding in critically ill children receiving mechanical ventilation: a
randomized controlled trial. Chest. 2004;126;872-878.
33. Snchez C, Lpez-Herce J, Carrillo A, Menca S, Vigil D. Early
transpyloric enteral nutrition in critically ill children. Nutrition.
2007;23:16-22.
34. Lpez-Herce J. Gastrointestinal complications in critically ill
patients: what differs between adults and children? Curr Opin Clin
Nutr Metab Care. 2009;12:180-185.
35. Mentec H, Dupont H, Bocchetti M, Cani P, Ponche F, Bleichner
G. Upper digestive intolerance during enteral nutrition in critically
ill patients: frequency, risk factors, and complications. Crit Care
Med. 2001;29:1955-1961.
36. Montejo JC, Grau T, Acosta J, et al; Nutritional and Metabolic
Working Group of the Spanish Society of Intensive Care Medicine
and Coronary Units. Multicenter, prospective, randomized, singleblind study comparing the efficacy and gastrointestinal complications of early jejunal feeding with early gastric feeding in critically
ill patients. Crit Care Med. 2002;30:796-800.
37. Mesejo A, Juan M, Garca-Simn M. Enteral access and intestinal
function assessment in the critically ill patient [in Spanish]. Nutr
Hosp. 2007;22(suppl 2):37-49.
38. Gilio AE, Stape A, Pereira CR, Cardoso MF, Silva CV, Troster EJ.
Risk factors for nosocomial infections in a critically ill pediatric
population: a 25-month prospective cohort study. Infect Control
Hosp Epidemiol. 2000;21:340-342.
39. Delgado AF, Kimura HM, Cardoso AL, Uehara D, Carrazza FR.
Nutritional follow-up of critically ill infants receiving short term
parenteral nutrition. Rev Hosp Clin Fac Med Sao Paulo. 2000;55:
3-8.
Downloaded from pen.sagepub.com by guest on June 7, 2015
Anda mungkin juga menyukai
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Experiment No. 11 Fabricating Concrete Specimen For Tests: Referenced StandardDokumen5 halamanExperiment No. 11 Fabricating Concrete Specimen For Tests: Referenced StandardRenBelum ada peringkat
- Modern Slavery Unveiled Training in Manila 2022 PrimerDokumen13 halamanModern Slavery Unveiled Training in Manila 2022 PrimerRapplerBelum ada peringkat
- Sigmund Freud QuotesDokumen7 halamanSigmund Freud Quotesarbeta100% (2)
- DODAR Analyse DiagramDokumen2 halamanDODAR Analyse DiagramDavidBelum ada peringkat
- Das MarterkapitalDokumen22 halamanDas MarterkapitalMatthew Shen GoodmanBelum ada peringkat
- REMEDIOS NUGUID vs. FELIX NUGUIDDokumen1 halamanREMEDIOS NUGUID vs. FELIX NUGUIDDanyBelum ada peringkat
- Summer 2011 Redwood Coast Land Conservancy NewsletterDokumen6 halamanSummer 2011 Redwood Coast Land Conservancy NewsletterRedwood Coast Land ConservancyBelum ada peringkat
- Common Application FormDokumen5 halamanCommon Application FormKiranchand SamantarayBelum ada peringkat
- New U. 4. 2Dokumen6 halamanNew U. 4. 2Jerald Sagaya NathanBelum ada peringkat
- Simply Learn Hebrew! How To Lea - Gary Thaller PDFDokumen472 halamanSimply Learn Hebrew! How To Lea - Gary Thaller PDFsuper_gir95% (22)
- Diabetic Foot InfectionDokumen26 halamanDiabetic Foot InfectionAmanda Abdat100% (1)
- History of Philippine Sports PDFDokumen48 halamanHistory of Philippine Sports PDFGerlie SaripaBelum ada peringkat
- CARET Programme1 Bennett-1Dokumen10 halamanCARET Programme1 Bennett-1TerraVault100% (3)
- Robots Template 16x9Dokumen13 halamanRobots Template 16x9Danika Kaye GornesBelum ada peringkat
- Final DSL Under Wire - FinalDokumen44 halamanFinal DSL Under Wire - Finalelect trsBelum ada peringkat
- Balochistan Conservation Strategy VDokumen388 halamanBalochistan Conservation Strategy VHãšãñ Trq100% (1)
- Pembaruan Hukum Melalui Lembaga PraperadilanDokumen20 halamanPembaruan Hukum Melalui Lembaga PraperadilanBebekliarBelum ada peringkat
- Dues & Scholarship Section: NotificationDokumen6 halamanDues & Scholarship Section: NotificationMUNEEB WAHEEDBelum ada peringkat
- Learners' Activity Sheets: Homeroom Guidance 7 Quarter 3 - Week 1 My Duties For Myself and For OthersDokumen9 halamanLearners' Activity Sheets: Homeroom Guidance 7 Quarter 3 - Week 1 My Duties For Myself and For OthersEdelyn BuhaweBelum ada peringkat
- Training Material Operasional Mitsubishi UNEJDokumen35 halamanTraining Material Operasional Mitsubishi UNEJkhamid surajabBelum ada peringkat
- Research Methods LessonDokumen26 halamanResearch Methods LessonCarole Janne EndoyBelum ada peringkat
- Your Porsche CodeDokumen10 halamanYour Porsche Codemahmut ezikBelum ada peringkat
- A Study On Waves of FeminismDokumen3 halamanA Study On Waves of FeminismLusekero MwangondeBelum ada peringkat
- Factors Affecting Job Satisfaction of EngineersDokumen35 halamanFactors Affecting Job Satisfaction of Engineerslingg8850% (2)
- Dealer DirectoryDokumen83 halamanDealer DirectorySportivoBelum ada peringkat
- Statement of Purpose EitDokumen3 halamanStatement of Purpose EitSajith KvBelum ada peringkat
- Tomato & Tomato Products ManufacturingDokumen49 halamanTomato & Tomato Products ManufacturingAjjay Kumar Gupta100% (1)
- Corti Et Al., 2021Dokumen38 halamanCorti Et Al., 2021LunaBelum ada peringkat
- Zsoka PDFDokumen13 halamanZsoka PDFMasliana SahadBelum ada peringkat
- COVID 19 Private Hospitals in Bagalkot DistrictDokumen30 halamanCOVID 19 Private Hospitals in Bagalkot DistrictNaveen TextilesBelum ada peringkat