2D2016 3.4-2 Azotemia and Urinary Abnormalities (Harrison's)
Diunggah oleh
elleinasHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
2D2016 3.4-2 Azotemia and Urinary Abnormalities (Harrison's)
Diunggah oleh
elleinasHak Cipta:
Format Tersedia
Trans 3.
4-2
December 3, 2013
Harrisons
Azotemia and
Urinary Abnormalities
Believe you can and youre halfway there.
AZOTEMIA: INTRODUCTION
Renal syndromes may arise as a:
o Consequence of a systemic illness or
o Can occur as a primary renal disease
Nephrologic syndromes usually consist of several elements
that reflect the underlying pathologic processes
The duration and severity of the disease affect those
findings and typically include one or more of the following:
o Reduction
in
glomerular
filtration
rate
(GFR)
(azotemia)
o Abnormalities of urine sediment [red blood cells (RBC),
white blood cells, casts, and crystals]
o Abnormal excretion of serum proteins (proteinuria)
o Disturbances in urine volume (oliguria, anuria,
polyuria)
o Presence of hypertension and/or expanded total body
fluid volume (edema)
o Electrolyte abnormalities
o In some syndromes, fever/pain
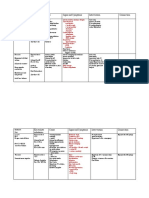
Initial Clinical And Laboratory Data Base For Defining
Major Syndromes In Nephrology
SYNDROMES
Acute or rapidly
progressive
renal failure
Acute nephritis
Chronic renal
failure
Nephrotic
syndrome
Asymptomatic
urinary
abnormalities
Urinary tract
infection/pyelon
ephritis
IMPORTANT CLUES
TO DIAGNOSIS
Anuria
Oliguria
Documented recent
decline in GFR
Hematuria, RBC
casts
Azotemia, oliguria
Edema,
hypertension
Azotemia for >3
months
Prolonged
symptoms or signs
of uremia
Symptoms or signs
of renal
osteodystrophy
Kidneys reduced in
size bilaterally
Broad casts in
urinary sediment
Proteinuria >3.5 g
per 1.73 m2 per
24h
Hypoalbuminemia
Edema
Hyperlipidemia
Hematuria
Proteinuria (below
nephrotic range)
Sterile pyuria, casts
Bacteriuria >105
colonies/ml
Other infectious
agent documented
in urine
Pyuria, leukocyte
casts
Binsol. Calagui. Disquitado. Perez.
COMMON
FINDINGS
Hypertension,
hematuria
Proteinuria,
pyuria
Casts, edema
Proteinuria
Pyuria
Circulatory
congestion
Proteinuria
Casts
Polyuria,
nocturia
Edema,
hypertension
Electrolyte
disorders
Casts
Lipiduria
Hematuria
Mild azotemia
Mild proteinuria
Fever
Renal tubule
defects
Hypertension
Nephrolithiasis
Urinary tract
obstruction
Frequency, urgency
Bladder tenderness,
flank tenderness
Electrolyte disorders
Polyuria, nocturia
Renal calcification
Large kidneys
Renal transport
defects
Systolic/diastolic
hypertension
Previous history of
stone passage or
removal
Previous history of
stone seen by x-ray
Renal colic
Azotemia, oliguria,
anuria
Polyuria, nocturia,
urinary retention
Slowing of urinary
stream
Large prostate,
large kidneys
Flank tenderness,
full bladder after
voiding
Hematuria
"Tubular"
proteinuria (<1
g/24h)
Enuresis
Proteinuria
Casts
Azotemia
Hematuria
Pyuria
Frequency,
urgency
Hematuria
Pyuria
Enuresis,
dysuria
AZOTEMIA
ASSESSMENT OF GLOMERULAR FILTRATION RATE
GLOMERULAR FILTRATION RATE (GFR)
Primary metric for kidney "function"
Direct
measurement
involves
administration
of
a
radioactive isotope (such as inulin or iothalamate) that is
filtered at the glomerulus but neither reabsorbed nor
secreted throughout the tubule
Clearance of inulin or iothalamate in milliliters per minute
equals the GFR and is calculated from the rate of removal
from the blood and appearance in the urine over several
hours
Direct measurements are frequently available through
nuclear radiology departments
SERUM CREATININE
Used as a surrogate to estimate when direct measurement
of GFR is not available
Most widely used marker for GFR
GFR is related directly to the urine creatinine excretion
and inversely to the serum creatinine (UCr/PCr)
In the outpatient setting, this serves as an estimate for GFR
(although much less accurate)
Signs and symptoms of uremia develop at significantly
different levels of serum creatinine, depending on
o The patient (size, age, and sex)
o The underlying renal disease
o The existence of concurrent diseases and true GFR
In general, patients do not develop symptomatic uremia
until renal insufficiency is quite severe (GFR <15 mL/min)
Page 1 of 7
Azotemia and Urinary Abnormalities
A significantly reduced GFR (either acute or chronic)
usually is reflected in a rise in serum creatinine and
leads to retention of nitrogenous waste products
(azotemia) such as urea.
Azotemia may result from:
o Reduced renal perfusion
o Intrinsic renal disease
o Postrenal processes (ureteral obstruction)
Precise determination of GFR is problematic as both
commonly measured indices (urea and creatinine) have
characteristics that affect their accuracy as markers of
clearance.
o Urea clearance may underestimate GFR significantly
because of urea reabsorption by the tubule
Creatinine is derived from muscle metabolism of creatine,
and its generation varies little from day to day
Creatinine clearance, an approximation of GFR, is
measured from plasma and urinary creatinine excretion
rates for a defined time period (usually 24 h) and is
expressed in milliliters per minute:
o Useful for estimating GFR because it is a small, freely
filtered solute that is not reabsorbed by the
tubules
o Levels can increase acutely from dietary ingestion of
cooked meat, however, and creatinine can be secreted
into the proximal tubule through an organic cation
pathway (especially in advanced progressive chronic
kidney disease), leading to overestimation of GFR
o When a timed collection for creatinine clearance is not
available, decisions about drug dosing must be based
on serum creatinine alone
o Two formulas are used widely to estimate kidney
function from serum creatinine:
More sensitive marker of early GFR decline than is
plasma creatinine
Influenced by age, race, and sex and additionally is
associated with diabetes, smoking, and markers of
inflammation.
APPROACH TO PATIENT
Established that GFR is reduced
Determine whether it is acute or chronic renal injury
through the clinical situation, history, and laboratory data
o However, the laboratory abnormalities characteristic of
chronic
renal
failure,
including
anemia,
hypocalcemia, and hyperphosphatemia, often are
also present in patients presenting with acute renal
failure
Radiographic evidence of renal osteodystrophy can be
seen only in chronic renal failure but is a very late
finding, and these patients are usually on dialysis
The urinalysis and renal ultrasound occasionally can
facilitate distinguishing acute from chronic renal failure
Advanced chronic renal insufficiency often have:
o Proteinuria
o Nonconcentrated urine (isosthenuria; isosmotic with
plasma)
o Small kidneys on ultrasound, characterized by
increased echogenicity and cortical thinning
Treatment should be directed toward slowing the
progression of renal disease and providing symptomatic
relief for edema, acidosis, anemia, and hyperphosphatemia
Acute renal failure can result from processes that affect:
o Renal blood flow (prerenal azotemia)
o Intrinsic renal diseases (affecting small vessels,
glomeruli, or tubules)
o Postrenal processes (obstruction to urine flow in
ureters, bladder, or urethra)
PRERENAL FAILURE
Cockcroft-Gault
Decreased renal perfusion accounts for 4080% of acute
renal failure and, if appropriately treated, is readily
reversible
MDRD (Modification of Diet in Renal Disease)
Several limitations of using serum creatininebased
estimating equations must be acknowledged
o Gradual loss of muscle from chronic illness, chronic use
of glucocorticoids, or malnutrition
Mask significant changes in GFR with small or
imperceptible
changes in serum
creatinine
concentration.
CYSTATIN C
Member of the cystatin superfamily of cysteineprotease
inhibitors
Produced at a relatively constant rate from all nucleated
cells
Binsol. Calagui. Disquitado. Perez.
Etiologies of prerenal azotemia:
o Decreased circulating blood volume
gastrointestinal haemorrhage
burns
diarrhea
diuretics
o Volume sequestration
pancreatitis
peritonitis
rhabdomyolysis
o Decreased effective arterial volume
cardiogenic shock
sepsis
Renal perfusion also can be affected by reductions in
cardiac output from:
o Peripheral vasodilation due to
Sepsis
Drugs
o Profound renal vasoconstriction
Severe heart failure
Page 2 of 7
Azotemia and Urinary Abnormalities
Hepatorenal syndrome
Drugs such as NSAIDs
True or "effective" arterial hypovolemia leads to a fall
in mean arterial pressure, which in turn triggers a series of
neural and humoral responses that include:
o Activation of the sympathetic nervous
o Renin-angiotensinaldosterone system
o Antidiuretic hormone (ADH) release
GFR
is
maintained
by
prostaglandin-mediated
relaxation of afferent arterioles and angiotensin II
mediated constriction of efferent arterioles.
Once the mean arterial pressure falls below 80 mmHg,
there is a steep decline in GFR.
Blockade of prostaglandin production by NSAIDs can
result in severe vasoconstriction and acute renal failure
Blocking
angiotensin
action
with
angiotensinconverting enzyme (ACE) inhibitors or angiotensin
receptor blockers (ARBs) decreases efferent arteriolar
tone and in turn decreases glomerular capillary perfusion
pressure
Patients on NSAIDs and/or ACE inhibitors/ARBs are most
susceptible to hemodynamically mediated acute renal
failure when blood volume is reduced for any reason
Patients with bilateral renal artery stenosis (or stenosis
in a solitary kidney) are dependent on efferent arteriolar
vasoconstriction for maintenance of glomerular filtration
pressure and are particularly susceptible to a precipitous
decline in GFR when given ACE inhibitors or ARBs
Prolonged renal hypoperfusion may lead to acute tubular
necrosis (ATN). Prerenal analysis and urinary electrolytes
can be useful in distinguishing prerenal azotemia from ATN
The urine of patients with prerenal azotemia can be
predicted from the stimulatory actions of norepinephrine,
angiotensin II, ADH, and low tubule fluid flow rate on salt
and water reabsorption
In prerenal conditions tubules are intact, leading to:
o Concentrated urine (>500 mosmol)
o Avid Na retention (urine Na concentration <20 mM/L,
fractional excretion of Na <1%)
o UCr/PCr >40
The prerenal urine sediment is usually normal or has
occasional hyaline and granular casts, whereas the
sediment of ATN usually is filled with cellular debris and
dark (muddy brown) granular casts
LABORATORY IN ACUTE RENAL FAILURE
PRERENAL
OLIGURIC
INDEX
AZOTEMIA
ACUTE RENAL
FAILURE
BUN/PCr ratio
>20:1
10-15:1
Urine sodium (UNa),
<20
>40
meq/L
Urine osmolality,
>500
<350
mosmol/L H2O
Fractional excretion of
<1%
>2%
sodium
Urine/plasma creatinine
(UCr/PCr)
>40
Binsol. Calagui. Disquitado. Perez.
<20
BUN, blood urea nitrogen; PCr, plasma creatinine; PNa,
plasma sodium concentration; UCr, urine creatinine
concentration; UNa, urine sodium concentration.
POSTRENAL FAILURE
Urinary tract obstruction
o Accounts for <5% of cases of acute renal failure
o Usually reversible and must be ruled out early in the
evaluation
o Diagnosed by the presence of ureteral and renal
pelvic dilation on renal ultrasound. However, early in
the course of obstruction or if the ureters are unable to
dilate (e.g., encasement by pelvic tumors or
periureteral), the ultrasound examination may be
negative
Note: Since a single kidney is capable of adequate clearance,
obstructive acute renal failure requires obstruction at the
urethra or bladder outlet, bilateral ureteral obstruction, or
unilateral obstruction in a patient with a single functioning
kidney.
INTRINSIC RENAL DISEASE
Entertained when prerenal and postrenal azotemia have
been excluded as etiologies of renal failure
Intrinsic renal disease can arise from:
o Processes involving large renal vessels
o Intrarenal microvasculature and glomeruli
o The tubulointerstitium
Ischemic ATN and toxic ATN account for 90% of cases of
acute intrinsic renal failure
The clinical setting and urinalysis are helpful in
separating the possible etiologies of acute intrinsic renal
failure.
Prerenal azotemia and ATN are part of a spectrum of
renal hypoperfusion
o Evidence of structural tubule injury is present in ATN,
whereas prompt reversibility occurs with prerenal
azotemia upon restoration of adequate renal perfusion
o ATN often can be distinguished from prerenal azotemia
by urinalysis and urine electrolyte composition
Ischemic ATN is observed most frequently in patients who
have
undergone
major
surgery,
trauma,
severe
hypovolemia, overwhelming sepsis, or extensive burns
Nephrotoxic ATN complicates the administration of many
common medications, usually by inducing a combination of
intrarenal vasoconstriction, direct tubule toxicity, and/or
tubule obstruction
The kidney is vulnerable to toxic injury by virtue of its rich
blood supply (25% of cardiac output) and its ability to
concentrate and metabolize toxins
o A diligent search for hypotension and nephrotoxins
usually will uncover the specific etiology of ATN
o Discontinuation of nephrotoxins and stabilization of
blood pressure often will suffice without the need for
dialysis while the tubules recover
Processes that involve the tubules and interstitium can lead
to acute kidney injury (AKI), a subtype of acute renal
failure. These processes include:
o Drug-induced
interstitial
nephritis
(especially
antibiotics, NSAIDs, and diuretics)
o Severe infections (both bacterial and viral),
o Systemic
diseases
(e.g.,
systemic
lupus
erythematosus)
Page 3 of 7
Azotemia and Urinary Abnormalities
o Infiltrative disorders (e.g., sarcoid, lymphoma, or
leukemia)
The urinalysis in 75% of cases usually shows:
o Mild to moderate proteinuria
o Hematuria
o Pyuria
o Occasionally white blood cell casts
o Finding of RBC casts in interstitial nephritis has been
reported but should prompt a search for glomerular
diseases
Occasionally, renal biopsy will be needed to distinguish
among these possibilities. The finding of eosinophils in
the urine is suggestive of allergic interstitial nephritis
or atheroembolic renal disease and is optimally
observed by using a Hansel stain.
o The absence of eosinophiluria, however, does not
exclude these etiologies
Occlusion of large renal vessels including arteries and
veins is an uncommon cause of acute renal failure. A
significant reduction in GFR by this mechanism suggests
bilateral processes or a unilateral process in a patient with a
single functioning kidney
Renal arteries can be occluded with:
o Atheroemboli
o Thromboemboli
o In situ thrombosis
o Aortic dissection
o Vasculitis
OLIGRIA AND ANURIA
UO: <400 mL/day
Can accompany any cause of acute renal
failure and carries a more serious prognosis
for renal recovery in all conditions except
prerenal azotemia
Anuria
UO: <100 mL/day
Is the complete absence of urine formation
Can be caused by total urinary tract
obstruction, total renal artery or vein
occlusion, and shock (manifested by
severe hypotension and intense renal
vasoconstriction)
Occasionally caused by cortical necrosis,
ATN,
and
rapidly
progressive
glomerulonephritis occasionally cause anuria
Nonoliguria UO: >400mL/day in patients with acute or
chronic azotemia
With nonoliguric ATN, disturbances of
potassium and hydrogen balance are less
severe than in oliguric patients, and recovery
to normal renal function is usually more
rapid
Oliguria
ATHEROEMBOLIC RENAL FAILURE
Can occur spontaneously but most often is associated
with recent aortic instrumentation
Emboli are cholesterol-rich and lodge in medium and small
renal arteries, leading to an eosinophil-rich inflammatory
reaction
Patients with atheroembolic acute renal failure often have a
normal urinalysis, but the urine may contain
eosinophils and casts
Diagnosis: renal biopsy, but this is often unnecessary
when other stigmata of atheroemboli are present (livedo
reticularis, distal peripheral infarcts, eosinophilia).
Renal artery thrombosis may lead to mild proteinuria
and hematuria, whereas renal vein thrombosis typically
induces heavy proteinuria and hematuria.
Diseases of the glomeruli (glomerulonephritis and
vasculitis) and the renal microvasculature (hemolyticuremic syndromes, thrombotic thrombocytopenic purpura,
and malignanthypertension) usually present with various
combinations of glomerular injury:
o Proteinuria
o Hematuria
o Reduced GFR
o Alterations of sodium excretion that lead to
hypertension, edema, and circulatory congestion (acute
nephritic syndrome)
These findings may occur as primary renal diseases or as
renal manifestations of systemic diseases. The clinical
setting and other laboratory data help distinguish primary
renal diseases from systemic diseases.
Binsol. Calagui. Disquitado. Perez.
Page 4 of 7
Azotemia and Urinary Abnormalities
The magnitude of proteinuria and the protein
composition of the urine depend on the mechanism of
renal injury that leads to protein losses
Both charge and size selectivity normally prevent virtually
all plasma albumin, globulins, and other high-molecularweight proteins from crossing the glomerular wall
o If this barrier is disrupted, plasma proteins may leak
into the urine (glomerular proteinuria)
o Smaller proteins (<20 kDa) are freely filtered but are
readily reabsorbed by the proximal tubule
FeNa, fractional excretion of sodium; GBM, glomerular
basement membrane; RBC, red blood cell; WBC, white blood
cell
ABNORMALITIES OF THE URINE
PROTEINURIA
Diagnosis:
DIPSTICK detects mostly albumin
Disadvantage:
False Positive: pH > 7.0 and concentrated or
contaminated
urine
which
obscure
significant
proteinuria in a much diluted urine
Designation
Trace
1+
2+
3+
4+
Approximate amount
Concentration
Daily
5-20 mg/dL
30 mg/dL
Less than 0.5
g/day
100 mg/dL
0.5-1 g/day
300 mg/dL
1-2 g/day
More than 2000
More than 2
mg/dL
g/day
Quantification of urinary albumin on a spot urine sample
(ideally from a first morning void) by measuring an
albumin-to-creatinine ratio (ACR) helpful in
approximating a 24-h albumin excretion rate (AER)
where ACR (mg/g) AER (mg/24 h).
Proteinuria that is not predominantly albumin will be missed
by dipstick screening. This is particularly important for the
detection of Bence Jones proteins in the urine of patients
with multiple myeloma.
Tests to measure total urine protein concentration
accurately rely on precipitation with sulfosalicylic or
trichloracetic acid.
Binsol. Calagui. Disquitado. Perez.
APPROACH TO PATIENT
Investigation of proteinuria is often initiated by a positive
dipstick on routine urinalysis.
Conventional dipsticks detect predominantly albumin and
provide a semiquantitative assessment (trace, 1+, 2+, or
3+), which is influenced by urinary concentration as
reflected by urine specific gravity (minimum <1.005,
maximum 1.030).
More exact determination of proteinuria should employ a
spot morning protein/creatinine ratio (mg/g) or a 24h urine collection (mg/24 h).
Traditionally, healthy individuals excrete <150 mg/d of
total protein and <30 mg/d of albumin.
However, even at albuminuria levels <30 mg/d, risk for
progression
to
overt
nephropathy
or
subsequent
cardiovascular disease is increased.
The remainder of the protein in the urine is secreted by the
tubules (Tamm-Horsfall, IgA, and urokinase) or
represents small amounts of filtered 2-microglobulin,
apoproteins, enzymes, and peptide hormones
Another mechanism of proteinuria occurs when there is
excessive production of an abnormal protein that
exceeds the capacity of the tubule for reabsorption.
This most commonly occurs with plasma cell
dyscrasias, such as multiple myeloma, amyloidosis,
and lymphomas.
Page 5 of 7
Azotemia and Urinary Abnormalities
The normal glomerular endothelial cell forms a barrier
composed of pores of 100 nm that retain blood cells but
offer little impediment to passage of most proteins.
The glomerular basement membrane traps most large
proteins (>100 kDa), and the foot processes of epithelial
cells (podocytes) cover the urinary side of the glomerular
basement membrane and produce a series of narrow
channels (slit diaphragms) to allow molecular passage of
small solutes and water but not proteins.
When the total daily excretion of protein is >3.5 g,
hypoalbuminemia,
hyperlipidemia,
and
edema
(nephrotic syndrome) are often present as well.
Renal failure occurs through a variety of mechanisms,
including tubule obstruction (cast nephropathy) and light
chain deposition.
Hypoalbuminemia in nephrotic syndrome occurs through
excessive urinary losses and increased proximal tubule
catabolism of filtered albumin.
Edema forms from renal sodium retention and reduced
plasma oncotic pressure, which favors fluid movement from
capillaries to interstitium.
To compensate for the perceived decrease in effective
intravascular volume, these occur (promote continued
renal salt and water reabsorption and progressive edema.):
o activation of the renin-angiotensin system
o stimulation of ADH
o activation of the sympathetic nervous system
A hypercoagulable state may arise from:
o urinary losses of antithrombin III
o reduced serum levels of proteins S and C
o hyperfibrinogenemia
o enhanced platelet aggregation
Hypercholesterolemia may be severe and results from
increased hepatic lipoprotein synthesis
HEMATURIA, PYURIA AND CASTS
Isolated hematuria without proteinuria, other cells, or casts
is often indicative of bleeding from the urinary tract.
HEMATURIA
Defined as two to five RBCs per high-power field (HPF)
and can be detected by dipstick.
A false positive dipstick for hematuria (where no RBCs are
seen on urine microscopy) may occur when myoglobinuria
is present, often in the setting of rhabdomyolysis.
Common causes of isolated hematuria: stones,
neoplasms, tuberculosis, trauma, and prostatitis.
Gross hematuria with blood clots is usually not an
intrinsic renal process; rather, it suggests a postrenal
source in the urinary collecting system.
A single urinalysis with hematuria is common and can
result from menstruation, viral illness, allergy, exercise, or
mild trauma.
Persistent or significant hematuria (>3 RBCs/HPF on
three urinalyses, a single urinalysis with >100 RBCs, or
gross hematuria) is associated with significant renal or
urologic lesions in 9.1% of cases.
Neoplasms are rare in the pediatric population, and isolated
hematuria is more likely to be "idiopathic" or associated
with a congenital anomaly.
Hematuria with pyuria and bacteriuria is typical of infection
and should be treated with antibiotics after appropriate
cultures.
Binsol. Calagui. Disquitado. Perez.
Acute cystitis or urethritis in women can cause gross
hematuria.
Hypercalciuria and hyperuricosuria are also risk factors for
unexplained isolated hematuria in both children and adults.
ISOLATED MICROSCOPIC HEMATURIA
Manifestation of glomerular diseases
RBCs of glomerular origin are often dysmorphic when
examined by phase-contrast microscopy
Irregular shapes of RBCs may also result from pH and
osmolarity changes produced along the distal nephron.
Common etiologies:
o IgA nephropathy (episodic gross hematuria)
o hereditary nephritis (episodic gross hematuria)
o thin basement membrane disease (family history of
renal failure is often present in patients with hereditary
nephritis, and patients with thin basement membrane
disease often have other family members with
microscopic hematuria)
Definitive diagnosis: renal biopsy
RBC CASTS
Hematuria with dysmorphic RBCs, RBC casts, and protein
excretion
>500
mg/d
is
virtually
diagnostic
of
glomerulonephritis.
Form as RBCs that enter the tubule fluid become
trapped in a cylindrical mold of gelled Tamm-Horsfall
protein
ISOLATED PYURIA
Unusual since inflammatory reactions in the kidney or
collecting system also are associated with hematuria
Presence of bacteria suggests infection, and white blood cell
casts with bacteria are indicative of pyelonephritis
White blood cells and/or white blood cell casts also may be
seen in acute glomerulonephritis as well as in
tubulointerstitial processes such as interstitial nephritis
and transplant rejection
In chronic renal diseases, degenerated cellular casts
called waxy casts can be seen in the urine.
Broad casts are thought to arise in the dilated tubules of
enlarged nephrons that have undergone compensatory
hypertrophy in response to reduced renal mass (i.e.,
chronic renal failure).
A mixture of broad casts typically seen with chronic renal
failure together with cellular casts and RBCs may be seen in
smoldering
processes
such
as
chronic
glomerulonephritis.
ABNORMALITIES OF THE URINE VOLUME
The volume of urine produced varies with the fluid intake,
renal function, and physiologic demands of the individual.
POLYURIA
True polyuria - (>3 L/d) in quantification of volume by
24-h urine collection
Polyuria results from two potential mechanisms:
o Solute diuresis: excretion of nonabsorbable solutes
(such as glucose)
urine volume is >3 L/d and urine osmolality is
>300 mosmol/L
search for the responsible solute(s) is mandatory
(glucose, mannitol, or urea)
o Water diuresis: excretion of water (usually from a
defect in ADH production or renal responsiveness).
Page 6 of 7
Azotemia and Urinary Abnormalities
urine output is >3 L/d and the urine is dilute
(<250 mosmol/L), total mosmol excretion is
normal and a water diuresis is present
could arise from polydipsia, inadequate secretion
of vasopressin (central diabetes insipidus), or
failure of renal tubules to respond to vasopressin
(nephrogenic diabetes insipidus)
The average person excretes between 600 and 800
mosmol of solutes per day, primarily as urea and
electrolytes.
Poorly controlled diabetes mellitus with glucosuria is
the most common cause of a solute diuresis, leading to
volume depletion and serum hypertonicity.
Since the urine sodium concentration is less than that of
blood, more water than sodium is lost, causing
hypernatremia and hypertonicity.
Common iatrogenic solute diuresis occurs from:
o mannitol administration
o radiocontrast media
o high-protein feedings (enterally or parenterally),
leading to increased urea production and excretion.
Less commonly, excessive sodium loss may result from
cystic renal diseases or Bartter's syndrome or during
the course of a tubulointerstitial process (such as resolving
ATN).
In these so-called salt-wasting disorders, the tubule
damage results in direct impairment of sodium reabsorption
and indirectly reduces the responsiveness of the tubule to
aldosterone.
Usually, the sodium losses are mild, and the obligatory
urine output is <2 L/d (resolving ATN and postobstructive
diuresis are exceptions and may be associated with
significant natriuresis and polyuria).
Formation of large volumes of dilute urine is usually due to
polydipsic states or diabetes insipidus.
Primary polydipsia can result from habit, psychiatric
disorders, neurologic lesions, or medications.
During deliberate polydipsia, extracellular fluid volume is
normal or expanded and plasma vasopressin levels are
reduced because serum osmolality tends to be near the
lower limits of normal.
ADH, antidiuretic hormone; ATN, acute tubular necrosis.
Urine osmolality should also be maximally dilute at 50
mosmol/L.
CENTRAL DIABETES INSIPIDUS
Etiology:
idiopathic in origin
secondary to a variety of hypothalamic conditions
o posthypophysectomy or trauma
o neoplastic, inflammatory, vascular or infectious
hypothalamic diseases
Idiopathic central diabetes insipidus is associated with
selective destruction of the vasopressin-secreting neurons
in the supraoptic and paraventricular nuclei and can be
inherited as an autosomal dominant trait or occur
spontaneously.
A plasma vasopressin level is recommended as the best
method
for
distinguishing
between
central
and
nephrogenic diabetes insipidus.
Alternatively, a water deprivation test plus exogenous
vasopressin may distinguish primary polydipsia from
central and nephrogenic diabetes insipidus
Binsol. Calagui. Disquitado. Perez.
Page 7 of 7
Anda mungkin juga menyukai
- Pathology+101 Complete)Dokumen147 halamanPathology+101 Complete)Goh Kah Yong100% (2)
- Cheat Sheet For Fluid Balance and ElectrolytesDokumen2 halamanCheat Sheet For Fluid Balance and ElectrolytesLiel TorresBelum ada peringkat
- Med 1.3 HeentDokumen13 halamanMed 1.3 Heentelleinas100% (3)
- Med 1.3 HeentDokumen13 halamanMed 1.3 Heentelleinas100% (3)
- MED 1.4 PE of The Chest, Lungs, Breast, and Axilla PDFDokumen16 halamanMED 1.4 PE of The Chest, Lungs, Breast, and Axilla PDFelleinasBelum ada peringkat
- MED 1.2 BP MeasurementDokumen4 halamanMED 1.2 BP MeasurementelleinasBelum ada peringkat
- 1.1 Bacterial Morphology PDFDokumen4 halaman1.1 Bacterial Morphology PDFelleinasBelum ada peringkat
- Pharm Fall Cardiovascular Pharmacology Study Guide-106Dokumen47 halamanPharm Fall Cardiovascular Pharmacology Study Guide-106sean liyanageBelum ada peringkat
- MED 1.1.1 History Taking and Clinical Decision Making PDFDokumen9 halamanMED 1.1.1 History Taking and Clinical Decision Making PDFelleinasBelum ada peringkat
- MED 1.1.1 History Taking and Clinical Decision Making PDFDokumen9 halamanMED 1.1.1 History Taking and Clinical Decision Making PDFelleinasBelum ada peringkat
- MED 1.1.1 History Taking and Clinical Decision Making PDFDokumen9 halamanMED 1.1.1 History Taking and Clinical Decision Making PDFelleinasBelum ada peringkat
- You Laugh You Drink Free Game Download by DSS Games-MinDokumen6 halamanYou Laugh You Drink Free Game Download by DSS Games-Minmartina325Belum ada peringkat
- Rhythm P Wave PR Interval QRS Rate Regularity Life Threatening CausesDokumen3 halamanRhythm P Wave PR Interval QRS Rate Regularity Life Threatening CausesLedio XhezairiBelum ada peringkat
- ND RDDokumen22 halamanND RDKatie Marie Wilson100% (1)
- MED 2.2 Examination of The Male GenitaliaDokumen7 halamanMED 2.2 Examination of The Male Genitaliaelleinas100% (1)
- MED 2.2 Examination of The Male GenitaliaDokumen7 halamanMED 2.2 Examination of The Male Genitaliaelleinas100% (1)
- MED 2.7 Gait and StationDokumen3 halamanMED 2.7 Gait and StationelleinasBelum ada peringkat
- Emergency Nursing Nclex ExamDokumen19 halamanEmergency Nursing Nclex ExamsjardioBelum ada peringkat
- Introduction To Acid Base Metabolic AcidosisDokumen12 halamanIntroduction To Acid Base Metabolic AcidosisKris Sharine Batalla OderoBelum ada peringkat
- NUR 317L Head-to-Toe Assessment 8 NUR 317L Head-to-Toe Assessment 8Dokumen4 halamanNUR 317L Head-to-Toe Assessment 8 NUR 317L Head-to-Toe Assessment 8Mary LowryBelum ada peringkat
- Nurs 604 Assignment 1 Critical Appraisal of An Advance Practice Role Final Copy For SubmissionDokumen12 halamanNurs 604 Assignment 1 Critical Appraisal of An Advance Practice Role Final Copy For Submissionapi-323169345Belum ada peringkat
- Diuretics For CardiacDokumen6 halamanDiuretics For CardiacBetsy Brown ByersmithBelum ada peringkat
- NCP Ineffective Gas ExchangeDokumen2 halamanNCP Ineffective Gas ExchangeRez ApegoBelum ada peringkat
- Fluid and Electrolyte Final OutputDokumen19 halamanFluid and Electrolyte Final OutputNatasha Alaine E. CayabyabBelum ada peringkat
- Medicine 2.3b Motor System ExaminationDokumen8 halamanMedicine 2.3b Motor System ExaminationelleinasBelum ada peringkat
- Chapter38 Assessment and Management of Patients With Rheumatic DisordersDokumen38 halamanChapter38 Assessment and Management of Patients With Rheumatic Disordersjericho dinglasanBelum ada peringkat
- Acetaminophen (Tylenol)Dokumen1 halamanAcetaminophen (Tylenol)Ciara GonzalezBelum ada peringkat
- HEAD TO TOE - Health Assessment in Nursing 5th Edition (Weber & Kelley)Dokumen20 halamanHEAD TO TOE - Health Assessment in Nursing 5th Edition (Weber & Kelley)folkloriantaro100% (1)
- Seeley's Chapter 8 Nervous SystemDokumen100 halamanSeeley's Chapter 8 Nervous SystemChristine Tapawan88% (8)
- Type 2 Diabetes: Annals of Internal MedicineDokumen17 halamanType 2 Diabetes: Annals of Internal MedicinenicoolBelum ada peringkat
- Diabetes and Complications: When Documenting Diabetes, It's Important To Note The FollowingDokumen2 halamanDiabetes and Complications: When Documenting Diabetes, It's Important To Note The Followingmeikaizen100% (1)
- Head Injury 1Dokumen33 halamanHead Injury 1drvishal bhattBelum ada peringkat
- Imaging Diagnosis of Pancreatic Cancer: A State-Of-The-Art ReviewDokumen15 halamanImaging Diagnosis of Pancreatic Cancer: A State-Of-The-Art ReviewTanwirul JojoBelum ada peringkat
- The Workings of The Brain Powers of The MindDokumen17 halamanThe Workings of The Brain Powers of The MindLovely ramirezBelum ada peringkat
- Air Layering Instructional SheetDokumen6 halamanAir Layering Instructional Sheetcandy_kb17Belum ada peringkat
- Neuro Notes #3Dokumen11 halamanNeuro Notes #3Monica JubaneBelum ada peringkat
- Medicine 2.3c Reflex TestingDokumen5 halamanMedicine 2.3c Reflex TestingelleinasBelum ada peringkat
- Hyponatremia: Presenter: DR Arun Karmakar Moderator: Prof. N. SharatkumarDokumen50 halamanHyponatremia: Presenter: DR Arun Karmakar Moderator: Prof. N. SharatkumarLyra FebriandaBelum ada peringkat
- Facial Nerve MCQDokumen4 halamanFacial Nerve MCQIqbal Syed100% (1)
- High Acuity Exam 1 Study Guide - 2Dokumen12 halamanHigh Acuity Exam 1 Study Guide - 2Angelica WilliamsBelum ada peringkat
- Diabetes Standards Primary Care 2022Dokumen29 halamanDiabetes Standards Primary Care 2022alialison7666Belum ada peringkat
- FOCUSED SOAP NOTE Health HX Tina JonesDokumen6 halamanFOCUSED SOAP NOTE Health HX Tina JonesMallory Zabor100% (1)
- AHP - Family Nurse PractitionerDokumen6 halamanAHP - Family Nurse PractitionerMaria Fudji HastutiBelum ada peringkat
- Tips For The Physicians Licenszcdcxure Examination1Dokumen7 halamanTips For The Physicians Licenszcdcxure Examination1filchibuff100% (2)
- Report of The Experimental Results of Drossinakis IAWG Korotkov 2012Dokumen21 halamanReport of The Experimental Results of Drossinakis IAWG Korotkov 2012magi44kenn100% (1)
- SyncopeDokumen10 halamanSyncopeHNINBelum ada peringkat
- Healthy People 2020Dokumen8 halamanHealthy People 2020Alex MungaiBelum ada peringkat
- System Disorder: Renal CalculiDokumen1 halamanSystem Disorder: Renal CalculiHolly DeckelmanBelum ada peringkat
- Spontaneous Regression of Pancreatic Cancer: A Case Report and Literature ReviewDokumen5 halamanSpontaneous Regression of Pancreatic Cancer: A Case Report and Literature ReviewHitomi-Belum ada peringkat
- Nurs 350 Pico Paper Phillips AaronDokumen7 halamanNurs 350 Pico Paper Phillips Aaronapi-240550685100% (1)
- General Principles of Disorders of Water Balance (Hyponatremia and Hypernatremia) and Sodium Balance (Hypovolemia and Edema)Dokumen31 halamanGeneral Principles of Disorders of Water Balance (Hyponatremia and Hypernatremia) and Sodium Balance (Hypovolemia and Edema)Juan InsignaresBelum ada peringkat
- Comprehensive Nursing Assessment For Care Plan: AllergiesDokumen14 halamanComprehensive Nursing Assessment For Care Plan: AllergiesBrittany ShrewsburyBelum ada peringkat
- Varices Esophagus PDFDokumen7 halamanVarices Esophagus PDFDimas ErlanggaBelum ada peringkat
- UTI & Pyelonephritis 1Dokumen1 halamanUTI & Pyelonephritis 1Hailey ReeseBelum ada peringkat
- Acute Myocardial InfarctionDokumen10 halamanAcute Myocardial InfarctionBianca Watanabe - RatillaBelum ada peringkat
- HyponatremiaDokumen19 halamanHyponatremiaapi-260357356Belum ada peringkat
- LasixDokumen1 halamanLasixKatie McPeek100% (2)
- Kidney Stones 1Dokumen4 halamanKidney Stones 1mynksharma100% (1)
- Case 27 (LC Fix)Dokumen14 halamanCase 27 (LC Fix)galih suharno0% (1)
- Toronto Notes Nephrology 2015 31Dokumen1 halamanToronto Notes Nephrology 2015 31JUSASBBelum ada peringkat
- FAELDONEA - B. Concept MapDokumen1 halamanFAELDONEA - B. Concept MapPatricia Jean FaeldoneaBelum ada peringkat
- Nephrology CritiquesDokumen18 halamanNephrology CritiquesYelle QuilatanBelum ada peringkat
- Case 36 AscitesDokumen4 halamanCase 36 AscitesMichaelBelum ada peringkat
- Sirs & ModsDokumen5 halamanSirs & Modsmarlou agananBelum ada peringkat
- Acute On Chronic Kidney DiseaseDokumen6 halamanAcute On Chronic Kidney DiseaseElizabeth LieBelum ada peringkat
- Electrolyte Imbalance Cause Signs and Symptoms Intervention ConnectionDokumen6 halamanElectrolyte Imbalance Cause Signs and Symptoms Intervention ConnectionmkninnyBelum ada peringkat
- Lab Values and Vital SignsDokumen4 halamanLab Values and Vital SignsWole Olaluwoye100% (1)
- 1538 Exam 4 Cell Reg & GriefDokumen35 halaman1538 Exam 4 Cell Reg & GriefJade EdanoBelum ada peringkat
- Urinary Incontinence and Chronic Kidney Disease - Important Points (1) - 2Dokumen4 halamanUrinary Incontinence and Chronic Kidney Disease - Important Points (1) - 2barbaraBelum ada peringkat
- SimulationDokumen5 halamanSimulationJessFriend100% (1)
- SBARQ FormDokumen1 halamanSBARQ FormTracy100% (5)
- CKD EsrdDokumen83 halamanCKD EsrdRita Lakhani100% (1)
- Cirrhosis and Its Complications Evidence Based TreatmentDokumen20 halamanCirrhosis and Its Complications Evidence Based TreatmentSucii Sekar NingrumBelum ada peringkat
- Travis: Blaser, RNDokumen1 halamanTravis: Blaser, RNapi-540097476Belum ada peringkat
- Ada 2023Dokumen294 halamanAda 2023Ahmed Ashab FerdousBelum ada peringkat
- KIDNEY INJURY/Renal Failure: Acute & Chronic: Prof Sampson Antwi Paediatric Nephrologist Sms-Knust/Kath October 2018Dokumen84 halamanKIDNEY INJURY/Renal Failure: Acute & Chronic: Prof Sampson Antwi Paediatric Nephrologist Sms-Knust/Kath October 2018Effah FestusBelum ada peringkat
- Cirrhosis Case StudyDokumen20 halamanCirrhosis Case StudyJodi Schaefer100% (1)
- Medicine 2.3d Sensory ExaminationDokumen4 halamanMedicine 2.3d Sensory ExaminationelleinasBelum ada peringkat
- Medicine 2.3a Gait and StationDokumen4 halamanMedicine 2.3a Gait and StationelleinasBelum ada peringkat
- MED 2.1c History Notes of The AbdomenDokumen2 halamanMED 2.1c History Notes of The AbdomenelleinasBelum ada peringkat
- MED 3.1 Renal Symptoms 1Dokumen6 halamanMED 3.1 Renal Symptoms 1elleinasBelum ada peringkat
- MED 2.6 Cranial NervesDokumen8 halamanMED 2.6 Cranial NerveselleinasBelum ada peringkat
- MED 1.1.2 Skin Assessment and LesionsDokumen4 halamanMED 1.1.2 Skin Assessment and LesionselleinasBelum ada peringkat
- Rula SheetDokumen2 halamanRula SheetCarl Christian CabelloBelum ada peringkat
- Tonsillectomy TechniquesDokumen11 halamanTonsillectomy TechniquesBrigita De VegaBelum ada peringkat
- Bones of The Axial SkeletonDokumen4 halamanBones of The Axial SkeletonJasminKate SutacioBelum ada peringkat
- Vedda+Blood+Sugar+Remedy+PDF+ +Book+Recipes+Free+Download+Michael+DempseyDokumen20 halamanVedda+Blood+Sugar+Remedy+PDF+ +Book+Recipes+Free+Download+Michael+DempseyBianca SmitheIncas AllenBelum ada peringkat
- A Single 10-Min Bout of Cold-Water Immersion Therapy After Strenuous Plyometric Exercise Has NoDokumen6 halamanA Single 10-Min Bout of Cold-Water Immersion Therapy After Strenuous Plyometric Exercise Has NoUmi RasyidahBelum ada peringkat
- Nano DentistryDokumen6 halamanNano DentistryanugrasBelum ada peringkat
- Lie Detection (Forensic 15) Module 9Dokumen3 halamanLie Detection (Forensic 15) Module 9Divina DugaoBelum ada peringkat
- 24 Cerebral Blood FlowDokumen31 halaman24 Cerebral Blood FlowZuhaib Ahmed100% (1)
- Medscape Imperforate AnusDokumen22 halamanMedscape Imperforate AnusVonny RiskaBelum ada peringkat
- Class XI Practicals Term2Dokumen5 halamanClass XI Practicals Term2Prince KBelum ada peringkat
- Client Screening Website FormDokumen2 halamanClient Screening Website FormBrett Whipp100% (2)
- 1987 Liophis - Green Species of South America - Dixon PDFDokumen20 halaman1987 Liophis - Green Species of South America - Dixon PDFLuis VillegasBelum ada peringkat
- Desolation - RL CaulderDokumen308 halamanDesolation - RL CaulderInes LagarrigueBelum ada peringkat
- Types of Burns ArticleDokumen7 halamanTypes of Burns ArticleSeltri 'ceti' SeptianiBelum ada peringkat
- Non-Pharmacological Treatment Options inDokumen9 halamanNon-Pharmacological Treatment Options inkemal ghazaliBelum ada peringkat
- Before Diving Make A Complete Dive Plan Together & Estimate Sea ConditionsDokumen8 halamanBefore Diving Make A Complete Dive Plan Together & Estimate Sea ConditionsMike LuckyBelum ada peringkat
- 6.1 Digestion BNDokumen24 halaman6.1 Digestion BNHana ElattarBelum ada peringkat
- Signal TransductionDokumen38 halamanSignal TransductionIndraPramanaIdaBagusBelum ada peringkat
- Unit 5.: Facultad de Medicina Humana "Daniel Alcides Carrión Garcia"Dokumen12 halamanUnit 5.: Facultad de Medicina Humana "Daniel Alcides Carrión Garcia"MARCOABADBelum ada peringkat
- Manage Chest TubesDokumen75 halamanManage Chest TubesWillington CuaresmaBelum ada peringkat
- Kreisberg-Zakarin Et Al IPNS Antonie Van Leeuwenhoek 1999Dokumen8 halamanKreisberg-Zakarin Et Al IPNS Antonie Van Leeuwenhoek 1999ElBelum ada peringkat
- VEALDokumen8 halamanVEALcutiepattotieBelum ada peringkat