Jurnal Cefamandol 1 PDF
Diunggah oleh
Twiin Roffie QlleeDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Jurnal Cefamandol 1 PDF
Diunggah oleh
Twiin Roffie QlleeHak Cipta:
Format Tersedia
ANTIMICROBIAL AGENTS
AND
Vol. 31, No. 6
CHEMOTHERAPY, June 1987, p. 876-882
0066-4804/87/060876-07$02.O0/O
Copyright C 1987, American Society for Microbiology
Ampicillin versus Cefamandole as Initial Therapy for
Community-Acquired Pneumonia
DAVID J. WEBER,lt* STEPHEN B. CALDERWOOD,' ADOLF W. KARCHMER,' AND JAMES E. PENNINGTON3
Infectious Disease Units, Massachusetts General Hospital, Boston, Massachusetts 02114,1 and New England Deaconess
Hospital' and Brigham and Women's Hospital,3 Boston, Massachusetts 02115
Received 14 October 1986/Accepted 27 February 1987
One hundred seven patients with community-acquired pneumonia thought to be of bacterial etiology by the
admitting physician but whose initial sputum Gram stain was inadequate to direct specific therapy were
randomized to receive either intravenous ampicillin or cefamandole as empiric therapy. Patients were excluded
if the initial sputum Gram stain was highly suggestive of infection with Streptococcus pneumoniae, Staphylococcus aureus, or an enteric gram-negative bacillus. The two study groups had comparable demographic and
presenting clinical features. The mean age of the patients evaluable for determination of clinical efficacy was
69 years, and >75% had at least one serious underlying medical disorder. In the 90 evaluable patients, there
were 11 therapeutic failures (12%), including 5 deaths (5%). Cefamandole, a broad-spectrum antibiotic, was
not more efficacious than ampiciHlin in producing a satisfactory clinical response or in shortening the duration
of parenteral therapy. Patients received an average of only 4 days of intravenous antibiotics before changeover
to oral therapy and were hospitalized for a mean of 7 days. No patient experienced a relapse of pneumonia
following successful completion of parenteral drug therapy. We conclude that cefamandole is not a more
effective agent than ampicillin for empiric therapy of community-acquired bacterial pneumonia of uncertain
etiology.
interest in using a broader-spectrum agent, such as cefamandole. Since broad-spectrum agents are more expensive than
ampicillin, it would be useful to document the clinical value
of using a broader-spectrum agent during empiric therapy of
pneumonia. Accordingly, this study was undertaken to compare the safety and efficacy of ampicillin versus cefamandole
in a prospective double-blind fashion as empiric therapy for
patients hospitalized for treatment of community-acquired
presumed bacterial pneumonia.
(This research was presented at the 25th Interscience
Conference on Antimicrobial Agents and Chemotherapy
[D. J. Weber, S. B. Calderwood, A. W. Karchmer, and
J. E. Pennington, Program Abstr. 25th Intersci. Conf. Antimicrob. Agents Chemother., abstr. no. 893, 1985].)
Pneumonia is the sixth leading cause of death in the
United States and is the fourth leading cause of death for
persons over the age of 65 (49). Traditional treatment guidelines for community-acquired bacterial pneumonia have
been based on knowledge of the causative agent (12, 13).
Definitive diagnosis, however, must await results of a culture of properly obtained sputum, blood, or transtracheal
aspirate. In some cases, a presumptive diagnosis may be
based on the analysis of a Gram stain of expectorated
sputum or a transtracheal aspirate (4, 29, 47, 57, 62).
However, sputum smears rmay be difficult to interpret due to
contamination with oral flora or the presence of more than
one potential pathogen or may be unavailable due to dehydration or the inability of the patient to cooperate. Likewise,
transtracheal aspiration is not without hazard and may be
contraindicated in certain patients (13, 28).
Since there is usually a sense of urgency to begin therapy
for pneumonia, initial treatment for many patients must be
selected empirically based on the clinical impression of
whether the most likely etiologic agent is bacterial or one of
the "atypical" pathogens (i.e., viruses, mycoplasmas, or
Legionella sp.) (12, 22, 34, 37, 43). For community-acquired
pteumonia of presumed bacterial etiology, ampicillin has
been a common empiric choice because Streptococcus pneumoniae and Haemophilus influenzae have been the most
frequently reported etiologic agents (5, 9, 14, 18, 19, 33, 36,
40, 46, 56, 61, 66). A number of reports, however, have
stressed the etiologic importance of Staphylococcus aureus,
Klebsiella sp., and other gram-negative bacilli, especially
among high-risk patient groups (3, 8, 14, 15, 21, 30, 38, 60,
63). In addition, the increasing prevalence of beta-lactamaseproducing H. influenzae has led to concern over possible
resistance to ampicillin. Thus, there has been considerable
MATERIALS AND METHODS
Study group. Between February 1983 and September 1984,
patients entering the Massachusetts General Hospital, New
England Deaconess Hospital, and Brigham and Woman's
Hospital with a primary diagnosis of community-acquiired
bacterial pneumonia were eligible for inclusion in this study.
Inclusion requirements included the following: age 18 years
or older; an admitting diagnosis of suspected communityacquired bacterial pneumonia; a new pulmonary infiltrate
demonstrated radiographically; and approval of the admitting physician. The diagnosis of suspected bacterial pneumonia was made by the admitting physician based on the
presence of clinical and laboratory findings (fever, cough,
pleuritic pain, auscultatory lung abnormalities, leukocytosis,
purulent sputum), Gram stain of sputum, if available on
admission, and a compatible radiographic abnormality. Patients were not included in the study if the admitting physician thought the pneumonia was likely due to a viral agent,
mycoplasma, or Legionella sp.
Exclusion criteria included the following: known allergy to
penicillins or cephalosporins; treatment with ampicillin,
amoxicillin, or a cephalosporin within the preceding 3 days;
*
Corresponding author.
t Present address: Infectious Disease Division 229H, University
of North Carolina at Chapel Hill, Chapel Hill, NC 27514.
876
VOL. 31, 1987
AMPICILLIN VERSUS CEFAMANDOLE FOR PNEUMONIA THERAPY
prior antibiotic therapy for the pneumonia to which there
appeared to have been a response; discharge from a hospital
within the preceding 2 weeks; drug-induced immunosuppression or neutropenia; lung cancer with postobstructive pneumonia; concomitant nonpulmonary infections; patients who
were moribund or had pneumonia severe enough to require
assisted ventilation on admission; the presence of empyema;
and serum creatinine over 4 mg/dl. Patients were also
excluded if, in the opinion of the admitting physician, the
initial sputum Gram stain was highly suggestive of infection
due to Streptococcus pneumoniae, Staphylococcus aureus,
or an enteric gram-negative bacillus; these patients were not
thought to require an empiric choice of antibiotics but rather
received specific therapy directed at the presumed pathogen.
Underlying diseases such as diabetes mellitus, alcoholism,
congestive heart failure, cancer, or chronic obstructive
pulmonary disease were not exclusion criteria.
Data obtained at study entry included complete blood
count and differential, platelet count, prothrombin time,
blood urea nitrogen, creatinine, serum glutamic oxalacetic
transaminase, bilirubin, alkaline phosphatase, blood sugar,
urinalysis, chest radiograph, and blood culture. Vigorous
attempts were made to obtain a deep sputum sample for
Gram stain and culture in all cases prior to study inclusion,
but invasive procedures such as transtracheal aspiration
were not performed.
Informed written consent, approved by the Human Studies Committees of the participating institutions, was obtained for all patients.
Parenteral therapy. The pharmacies of each institution,
using a separate computer-generated list of random assignments, allocated patients to receive either intravenous
ampicillin or cefamandole in a double-blind manner. Two
grams of the assigned antibiotic, mixed in one-half normal
saline, was administered intravenously over 30 min every 6
h. Vitamin C and B complex was added to the antibiotic
solutions so that they were of identical color. No other
antibiotics were administered to patients during receipt of
the study drug, but all other forms of therapy were at the
discretion of the primary physician. In cases of adverse
reaction to the study drug or failure of therapy, the study
antibiotic could be identified at the request of the primary
physician, but only after the patients' therapy had been
coded as successful, unsuccessful, or unevaluable.
Bacteriology. Routine cultures were performed in the
clinical microbiology laboratories of the participating institutions. Bacteria were isolated from the sputum by standard
methods and considered potential pathogens only if moderate or abundant growth occurred from a purulent specimen
(17, 27, 32, 45). All Gram stains of sputum samples were
reviewed by one of the investigators to allow correlation
with culture results. Antibiotic susceptibilities of isolated
pathogens were determined by using standard techniques (2,
23, 50, 51). All H. influenzae strains were tested for production of beta-lactamase with nitrocefin-impregnated disks (1).
Determination of response to parenteral therapy. Review of
each patient's clinical progress was conducted in a doubleblind manner until the response to parenteral therapy was
determined to be successful, unsuccessful, or unevaluable.
The response to therapy was considered unevaluable in 17
patients for one of the following reasons: the pulmonary
process on the initial radiograph was subsequently shown to
antedate this illness (nine patients); a noninfectious pulmonary process was documented (two patients); the patient left
the hospital against medical advice (two patients); the patient was withdrawn from the study by the primary physician
for
reasons
877
unrelated to therapeutic response (three pa-
tients); or an adverse drug reaction occurred prior to meeting
the criteria for determination of clinical success or failure
(one patient).
The criteria for a successful clinical response included the
following: improvement in clinical signs and symptoms as
determined by the primary physician, disappearance of fever
(temperature of -380C) for at least 48 h, and stability or
improvement in the chest radiograph. The response was
deemed unsuccessful if any of the following occurred while
the patients were receiving the study drug: death, progressive pulmonary infection, failure to improve after prolonged
antibiotic
administration (>10 days), or development of
metastatic infection due to the initial pulmonary pathogen. If
the response to treatment with the study drug was unsuccessful, antibiotic therapy was changed under the direction
of the primary physician.
Laboratory studies during treatment with the study drug
were performed as deemed necessary by the primary physician. A follow-up chest radiograph was obtained on all
patients prior to discontinuing the study drug. An attempt
was made to obtain sputum for culture from all patients prior
to changing to oral therapy.
Change to oral antibiotic therapy and subsequent follow-up.
Patients meeting the criteria for successful response to the
intravenous study drug were then eligible to receive oral
antibiotic therapy. Oral antimicrobial therapy was not determined by protocol; rather the time when oral therapy was
initiated, the duration of oral treatment, and the oral agent
used were determined by the primary physician, based on
results of sputum culture and clinical course. However,
physicians could elect to treat patients with the oral equivalent (amoxicillin or cefaclor) of the parenteral study drug
without unblinding the study if a satisfactory response to
initial parenteral therapy had occurred. All patients were
requested to return for a follow-up visit and chest radiograph
following completion of oral antibiotic therapy. Patients
developing new pulmonary infiltrates while on oral antibiotics or within 2 weeks of cessation of antibiotic therapy were
classified as follows: a relapse if the same pathogen was
isolated or if the infiltrate recurred in the same location but
no pathogen was isolated; a superinfection if a new pathogen
was isolated or an infiltrate developed in a new location but
no pathogen was isolated.
Patients were considered to be evaluable for assessment of
drug toxicity if they received three or more doses of parenteral study drug.
Discrete data were analyzed for significance by the chisquare test or two-tailed Fisher exact test. Ordinal data were
evaluated by the two-tailed Student t test for comparison of
independent samples.
RESULTS
Characteristics of study group and bacteriologic evaluation.
One hundred seven patients were randomized to receive
either intravenous ampicillin or cefamandole; 90 patients
were evaluable for clinical efficacy (Table 1). Evaluable
patients in the ampicillin and cefamandole groups were
comparable in demographic features and presenting clinical
and laboratory findings.
An initial expectorated sputum sample was obtained in 85
evaluable patients (94%) (Table 1). A potential bacterial
pathogen was identified in purulent sputum from 40 of these
85 patients (47%). In the remainder, only normal respiratory
flora were recovered by culture; while some of this latter
878
ANTIMICROB. AGENTS CHEMOTHER.
WEBER ET AL.
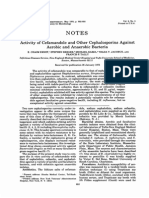
TABLE 1. Characteristics and presenting features of patients evaluable for clinical efficacy
Cefamandole
Ampicillin
Characteristic/feature
54
53
Total patients randomized
6
11
Unevaluable for clinical efficacy
48
42
Evaluable for clinical efficacy
Significancea
NS
Demographics
Male: female (no.)
Age (yr)
Wt (kg)
30:12
68.8 16.9
65.3 11.8
29:19
68.9 + 15.3
69.1 t 20.0
NS
NS
NS
Presentation
Days symptomatic, median (first, third quartile)
Admission temp (C)
5.0 (2.6, 7.1)
38.5 + 1.1
5.1 (2.7, 8.5)
38.4 0.9
NS
Underlying diseases
Patients with pulmonary diseases (no.)b
Asthma
Chronic obstructive lung disease
Restrictive lung disease
Patients with other disorders (no.)b
Ethanol abuse
Congestive heart failure
Diabetes mellitus
Cancer in remission
Neurologic impairmentc
Patients with at least one underlying disease (no.)
18 (43%)
5
15
2
25 (60%)
5
6
5
6
10
33 (77%)
17 (35%)
3
15
1
24 (57%)
7
4
8
4
8
36 (75%)
NS
34:8
15.0 5.9
32:9
1.3 0.6
41:7
13.3 5.1
36:9
1.3 0.5
NS
NS
NS
NS
8
7
1
1
4
19
2
11
8
0
0
0
26
3
Laboratory findings
Chest radiograph, infiltrate-one lobe: multilobar
Leukocyte count (1,000/mm3)
Bands, <15%.: >15%d
Creatinine (mg/dl)
Initial sputum culture (no. of patients)
Streptococcus pneumoniae
Haemophilus influenzae
Staphylococcus aureus
Escherichia coli
Mixed pathogens
Normal flora only
Sputum not obtained
NS
NS
NS, Not significant; P > 0.10.
Some patients had more than one underlying condition.
c Includes history of cerebrovascular accident, Alzheimer's disease, seizure disorder, or swallowing disorder.
d Differential leukocyte count unavailable for four patients.
group had purulent specimens by Gram stain, many had
specimens too contaminated by oral secretions for reliable
interpretation. Of the patients from whom a pathogen was
identified in sputum, 36 of 40 (90%) had a single pathogen
isolated. Multiple pathogens were isolated from four patients: Enterobacter cloacae and Acinetobacter calcoaceticus; H. influenzae and Streptococcus pneumoniae; H.
influenzae and Klebsiella pneumoniae; and Escherichia coli,
Enterobacter aerogenes, and Staphylococcus aureus. The
distribution of pathogens was similar in the two study
groups.
Two of the 90 evaluable patients had positive blood
cultures. Both patients had Streptococcus pneumoniae cultured from both sputum and blood and were randomized to
therapy with ampicillin. Both recovered uneventfully.
One of 17 strains (6%) of H. influenzae was ampicillin
resistant and cefamandole susceptible and produced betalactamase. The other gram-negative pathogens isolated were
resistant to ampicillin but susceptible to cefamandole except
for a single strain of A. calcoaceticus, which was resistant to
both antibiotics.
Response to initial parenteral therapy. Overall, the re-
sponse to therapy was unsuccessful in 11 patients (12%),
including 5 (5%) who died (Table 2). Five treatment failures
occurred in the ampicillin group, and six occurred in the
cefamandole group (P > 0.10). Two patients in the ampicillin
group developed progressive pneumonia; in one patient,
ampicillin-resistant Escherichia coli was isolated, while in
the other an etiology was not determined despite
bronchoscopy and open lung biospy. Three patients receiving ampicillin therapy died. One patient suffered a myocardial infarction on day 3 of therapy, a second patient suffered
a cardiac arrest from unknown causes on day 3 of therapy,
and the third patient, an insulin-dependent diabetic, died
following an episode of hypoglycemia and subsequent aspiration. When the randomization code was broken it was
learned that the single patient from whom a beta-lactamaseproducing H. influenzae had been isolated improved while
on ampicillin and was discharged on oral cefaclor.
The response to cefamandole was unsuccessful in six
patients. Three patients had progressive pulmonary infection. No etiology was defined in two patients despite invasive procedures; in a third patient, mycoplasma pneumonia
was documented serologically, and the patient improved on
VOL. 31, 1987
AMPICILLIN VERSUS CEFAMANDOLE FOR PNEUMONIA THERAPY
879
TABLE 2. Results of initial parenteral therapy
Parameter
Ampicillin
Cefamandole
Significancea
Evaluable patients (no.)
Therapeutic success: failure
Reasons for treatment failure (no. of patients)
Progressive pulmonary infection
Death
Meningitis
Total doses (no.) of parenteral study drug'
Days of parenteral drug therapyb
Doses (no.) of study drug until afebrile, median (first, third quartile)b
Days of hospitalization (median)b
42
37:5
48
42:6
NS
2
3
0
14.9 + 5.4
3.7 1.4
1 (<1, 2)
7.1 + 6.2 (5)
3
2
1
17.0 8.8
4.2 2.2
2 (<1, 3)
7.4 + 4.2 (6)
NS
NS
NS
NS, Not significant; P > 0.10.
b Excludes treatment failures.
a
erythromycin. One patient with pneumococcal pneumonia
developed meningitis after 2 days of cefamandole but responded to intravenous ampicillin. Two patients died while
on cefamandole. One patient with extrahepatic biliary obstruction from a presumed tumor died with progressive
respiratory failure and pneumonia of uncertain etiology. The
final patient became hypotensive with a marked left shift in
the leukocyte count (76% band forms) after three doses of
cefamandole; empiric therapy with nafcillin and gentamicin
was instituted, but the patient died. Her sputum grew
abundant Streptococcus pneumoniae susceptible to both
study drugs.
Patients classified as responding successfully received a
mean of 16.0
7.5 doses of intravenous antibiotic and were
hospitalized for 2 to 38 days (mean, 7.3
5.2 days).
Successful therapy produced rapid defervescence (median,
one dose of study drug). For several patients whose response was successful, hospitalization was prolonged not by
the pneumonia but by unrelated surgery or by a delay in
finding a chronic care bed. There were no significant differences in the length of study drug therapy or duration of
hospitalization between the ampicillin and cefamandole
groups (Table 2).
Colonization of the respiratory tract with potential bacterial pathogens occurred in 9 of 22 patients (41%) who had a
successful clinical response to ampicillin and follow-up
sputum cultures. Colonizing pathogens included the following: Klebsiella sp., 5; Enterobacter sp., 3; Serratia sp., 2;
Staphylococcus aureus, 2; and enterococci, 1. All of the
gram-negative isolates were ampicillin resistant. Five strains
of Klebsiella sp. and two strains of Enterobacter sp. were
susceptible to cefamandole. One Serratia strain showed
intermediate susceptibility to cefamandole. None of 21 patients who successfully completed a course of cefamandole
and had follow-up sputum cultures developed colonization
during the short period of study drug therapy. The rate of
colonization was lower in the cefamandole group than in the
ampicillin group (P < 0.01).
Toxicity of parenteral study drugs. One hundred three
patients received three or more doses of intravenous study
drug and were evaluated for side effects. Sequential monitoring of hematologic and chemistry data was not conducted
routinely. Four patients in the ampicillin group (8%) experienced side effects, which included phlebitis (one patient),
diarrhea (one patient), fever with drug rash (one patient),
and neutropenia (one patient). Three patients receiving
cefamandole (6%) experienced side effects, including phlebitis (one patient), drug rash (one patient), and fever with
leukocytosis and nephritis (one patient). Drug toxicity re
sulted in the discontinuation of study drug therapy in two
patients, one in the ampicillin group and one in the cefamandole group. One death resulted from drug toxicity; a patient
receiving ampicillin developed neutropenia shortly after a
change to oral amoxicillin and then went on to develop a
fatal pulmonary superinfection. There was no statistical
difference in the toxicity of intravenous ampicillin compared
with cefamandole (P > 0.10).
Follow-up after cessation of parenteral therapy. Patients
successfully completing parenteral therapy received an additional 8.7 + 3.1 days of oral antibiotics (Table 3). A variety
of oral antibiotics were used based on the pathogen isolated
and the preference of the primary physician. Amoxicillin and
cefaclor were not always used in sequence with the equivalent parenteral study drugs; thus, there is a difference in the
distribution of these oral drugs between the ampicillin and
cefamandole study groups.
Follow-up clinical information was obtained for 35 of 37
patients (95%) successfully completing a course of ampicillin
and 41 of 42 patients (98%) successfully completing a course
of cefamandole 2 to 10 weeks post-hospital discharge (Table
3). In the ampicillin group 34 patients (97%) were either well
TABLE 3. Oral therapy and clinical follow-up of patients
successfully treated with parenteral study drugs
Parameter
Days of oral antibiotic therapya
Ampicillin
8.8
2.7
Cefamandole
8.6
Oral therapy used (no. of patients)
Ampicillin or amoxicillin
Cefaclor
Penicillin
Other
27
4
3
3
20
13
3
6
Symptoms/signs at follow-up (no. of
patients)
None or minimal
Improved
Late superinfection
Unavailable
34
1
0
2
36
2
3
1
Chest radiograph at follow-up (no.
of patients)
Normal or base line
28
Improved
Unavailable
Late superinfection
a Not significant; P > 0.10.
33
0
6
3.5
880
WEBER ET AL.
or had minimal residual symptoms or signs of infection,
compared with 36 patients in the cefamandole group (88%)
(P > 0.10). Three patients, all in the cefamandole group,
presented with superinfection 2 to 3 days following completion of their oral antibiotics. One patient presented with H.
influenzae (beta-lactamase negative) tracheobronchitis, one
presented with a Pseudomonas maltophilia (ampicillin and
cefamandole resistant) pneumonia, and the final patient, who
had received only 5 days of antibiotics, developed a new
pulmonary infiltrate of unknown etiology.
DISCUSSION
Our study group was not designed to evaluate the etiology
of community-acquired pneumonia but rather to compare
two antibiotic regimens for empiric therapy of suspected
bacterial pneumonia. We excluded patients in whom the
Gram stain of initial sputum was thought by the admitting
physician to be highly suggestive of infection due to Streptococcus pneumoniae, Staphylococcus aureus, or an enteric
gram-negative bacillus since these patients should receive
specific antimicrobial therapy. We focused instead on the
large group of patients admitted to a hospital for antibiotic
therapy of presumed bacterial pneumonia of uncertain etiology. We also included patients in whom initial sputum Gram
stains suggested infection with H. influenzae, as either
ampicillin or cefamandole is commonly used in this situation.
The demographic makeup and presenting clinical and
laboratory features of our study group were similar to
previous reports of patients hospitalized with pneumonia,
except that our patients were somewhat older (5, 9, 14, 15,
18, 36, 40, 46, 56, 61). Of note was a 75% overall frequency
of underlying diseases known to predispose to pneumonia.
Thus, our study group may be considered a high-risk patient
population.
The etiology of pneumonia remained uncertain in over
one-half of the patients in our study. These were the patients
who were unable to produce an adequate sputum sample
uncontaminated with oral secretions, a common problem in
clinical practice. All of these patients, however, were felt to
have acute bacterial pneumonia by the admitting physician
and to require empiric antibiotic therapy. Of the patients in
this group who failed therapy with one of the study drugs,
only one was subsequently discovered to have an atypical
pneumonia, mycoplasma, despite extensive serologic and
invasive workup. In 40 patients, a presumed bacterial pathogen was isolated from sputum culture that correlated with
interpretation of sputum Gram stains when reviewed by one
of the investigators. In most of these patients, reading of the
initial sputum Gram stain by the admitting physician was
confounded by small amounts of contamination with respiratory tract flora, inability to obtain sputum during the first
several hours of hospitalization, or misinterpretation of the
organisms present. As in similar series, the most common
pathogens isolated were Streptococcus pneumoniae and H.
influenzae.
Although H. influenzae was isolated in 17 patients, only 1
of these strains (6%) produced beta-lactamase. We did not
identify any strains of H. influenzae that were beta-
lactamase negative and ampicillin resistant. Up to 50% of H.
influenzae strains isolated from the blood or cerebrospinal
fluid of pediatric patients have been reported to be ampicillin
resistant (7). However, our low rate of isolation of ampicil-
lin-resistant H. influenzae is similar to that in previous
reports of isolates from adult blood or sputum cultures (11,
48, 59, 64).
ANTIMICROB. AGENTS CHEMOTHER.
Six percent of our patients died, often from causes unrelated to respiratory insufficiency or sepsis. Several other
antibiotic trials of patients hospitalized with communityacquired respiratory infections have reported mortality rates
ranging from 4 to 11% and have noted that most deaths
resulted from the patients' underlying disorders (10, 20, 22,
25, 26, 31, 53, 58). The mortality rate for our patients is lower
than the 8 to 24% reported for patients hospitalized with
community-acquired pneumonia but not specifically entered
in a therapeutic trial (14, 15, 21, 40, 46, 61, 66). This
difference may reflect the fact that antibiotic trials, including
ours, often exclude patients with immunosuppression or
neutropenia or those who are severely ill and unable to give
informed consent. Our overall response rate of 88% is
similar to that reported in previous trials that used cefamandole alone for the treatment of lower respiratory tract
infections (26, 41, 42, 44, 53) or in comparison with cefotiam
(6), ceftizoxime (25, 35, 39, 58), cefonicid (24, 65), ceftazidime (16, 31), or cefoperazone (20).
The patient groups randomized to ampicillin and cefamandole therapy were comparable with regard to demographic,
clinical, laboratory, and radiographic characteristics on admission. Despite the inclusion of numerous elderly and
high-risk patients, cefamandole did not prove more efficacious than ampicillin when used as empiric therapy for
patients hospitalized with presumed bacterial pneumonia.
Side effects and superinfections were infrequent, and their
incidence did not differ between the ampicillin and cefamandole groups. Previous antibiotic trials have demonstrated
that cefamandole is as efficacious as penicillin for pneumococcal pneumonia (54, 55) and as efficacious as ampicillin for
lower respiratory infection due to H. influenzae (10). Further, broad-spectrum cephalosporins have not been shown
to be more efficacious than cefamandole for communityacquired pneumonia (6, 16, 20, 24, 25, 31, 35, 39, 58, 65).
Thus, cost considerations appear to favor the empiric use of
ampicillin over cefamandole for the majority of patients
hospitalized with presumed bacterial pneumonia of uncertain etiology. However, cefamandole or another broadspectrum antibiotic may be desirable as an initial empiric
agent in patient subgroups known to be at high risk for
infection due to Staphylococcus aureus or gram-negative
bacilli. These groups might include presumed bacterial pneumonia following viral influenza, patients cared for in extended-care facilities, neutropenic or immunosuppressed patients, or patients readmitted after recent hospitalization.
The rapid defervescence noted in our patients and the
relatively short duration of intravenous antibiotics used for
adequate clinical response (4 days) are worthy of comment.
Despite the older age of our patients and the high frequency
of concurrent serious medical and pulmonary disorders,
patients were hospitalized an average of only 7 days. No
patient who met our criteria for a successful response to
parenteral study drug subsequently developed a relapse of
pneumonia after a change to oral antibiotic or in the follow-up period. Only three patients, all in the cefamandole
group, developed superinfection following combined intravenous and oral antibiotic therapy.
We conclude that (i) cefamandole is not more effective
than ampicillin as initial empiric therapy in patients hospitalized with presumed bacterial pneumonia whose Gramstained sputum smear is inadequate to direct specific therapy
and (ii) patients who respond promptly to treatment with
intravenous antibiotics may often be switched to oral antibiotic therapy as early as 3 to 4 days after admission, without
significant risk of relapse of their pneumonia. Treatment of
VOL. 31, 1987
AMPICILLIN VERSUS CEFAMANDOLE FOR PNEUMONIA THERAPY
the majority of patients with uncomplicated communityacquired bacterial pneumonia does not require an extended
period of intravenous antibiotics.
ACKNOWLEDGMENTS
We gratefully acknowledge the assistance of the houie staff and
private physicians at the participating institutions in identifying and
entering patients into this study. Ronald Romnard of Massachusetts
General Hospital, Paul Sesin of New England Deaconess Hospital,
and Kathleen Benfell of Brigham and Women's Hospital provided
expert help in carrying out the double-blind randomization protocol.
Linda Krilov assisted in data collection.
This work was supported by Eli Lilly & Co., Indianapolis, Ind.
LITERATURE CITED
1. Anhalt, J. P., L. D. Sabath, and A. L. Barry. 1980. Special tests:
bactericidal activity, activity of antimicrobials in combinations,
and detection of beta-lactamase production, p. 478-484. In
E. H. Lennette, A. Balows, W. J. Hausler, Jr., and J. P. Truant
(ed.), Manual of clinical microbiology, 3rd ed. American Society for Microbiology, Washington, D.C.
2. Barry, A. L., and C. Thornsberry. 1980. Susceptibility testing:
diffusion test procedures, p. 463-474. In E. H. Lennette, A.
Balows, W. J. Hausler, Jr., and J. P. Truant (ed.), Manual of
clinical microbiology, 3rd ed. American Society for Microbiology, Washington, D.C.
3. Bentley, D. W. 1984. Bacterial pneumonia in the elderly: clinical
features, diagnosis, etiology, and treatment. Gerontology 30:
297-307.
4. Berk, S. L., S. A. Holtsclaw, A. Kahn, and J. K. Smith. 1981.
Transtracheal aspiration in the severely ill elderly patient with
bacterial pneumonia. J. Am. Geriatr. Soc. 29:228-231.
5. Berntsson, E., J. Blomberg, T. Lagergard, and B. Trollfors.
1985. Etiology of community-acquired pneumonia in patients
requiring hospitalization. Eur. J. Clin. Microbiol. 4:268-272.
6. Beumer, H. M., W. P. Olislagers, M. Kahn, and J. D. van
Hamersveld. 1985. Clinical evaluation of cefotiam and cefamandole in respiratory tract infections. Int. J. Clin. Pharmacol.
Ther. Toxicol. 23:105-108.
7. Campos, J., S. Garcia-Tornel, and I. Sanfeliu. 1984. Susceptibility studies of multiply resistant Haemophilus influentzae isolated from pediatric patients and contacts. Antimicrob. Agents
Chemother. 25:706-709.
8. Crane, L. R., and A. M. Lerner. 1983. Gram-negative bacillary
pneumonia, p. 227-250. In J. E. Pennington (ed.), Respiratory
infections: diagnosis and management. Raven Press, New York.
9. Crofton, J. 1970. The chemotherapy of bacterial respiratory
infections. Am. Rev. Respir. Dis. 101:841-859.
10. Delgado, D. G., C. J. Brau, C. G. Cobbs, and W. E. Dismukes.
1979. Clinical and laboratory evaluation of cefamandole in the
therapy of Haemophilus spp. bronchopulmonary infections.
Antimicrob. Agents Chemother. 15:807-812.
11. Doern, G. V., J. H. Jorgensen, C. Thornsberry, D. A. Preston,
and the Haemophilus influenzae Surveillance Group. 1986. Prevalence of antimicrobial resistance among clinical isolates of
Haemophilus influenzae: a collaborative study. Diagn. Microbiol. Infect. Dis. 4:95-107.
12. Donowitz, G. R., and G. L. Mandell. 1983. Empiric therapy for
pneumonia. Rev. Infect. Dis. 5(Suppl.):40-51.
13. Donowitz, G. R., and G. L. Mandeil. 1985. Acute pneumonia, p.
394-404. In G. L. Mandell, R. G. Douglas, Jr., and J. E.
Bennett (ed.), Principles and practices of infectious diseases.
John Wiley & Sons, Inc., New York.
14. Dorff, G. J., M. W. Rytel, S. G. Farmer, and G. Scanlon. 1973.
Etiologies and characteristic features of pneumonias in a municipal hospital. Am. J. Med. Sci. 266:349-358.
15. Ebright, J. R., and M. W. Rytel. 1980. Bacterial pneumonia in
the elderly. J. Am. Geriatr. Soc. 28:220-223.
16. Engle, J. C., P. W. Lifland, and C. J. Schleupner. 1985.
Comparison of ceftazidime with cefamandole for therapy of
community-acquired pneumonia. Antimicrob. Agents Chemother. 28:146-148.
881
17. Facklam, R. A. 1980. Streptococci and aerococci, p. 88-110. In
E. H. Lennette, A. Balows, W. J. Hausler, Jr., and J. P. Truant
(ed.), Manual of clinical microbiology, 3rd ed. American Society for Microbiology, Washington, D.C.
18. Fekety, F. R., Jr., J. Caldweli, D. Gump, J. E. Johnson, W.
Maxson, J. Mulholland, and R. Thoburn. 1971. Bacteria, viruses, and mycoplasmas in acute pneumonia in adults. Am.
Rev. Respir. Dis. 104:499-507.
19. Fiala, M. 1969. A study of the combined role of viruses,
mycoplasmas and bacteria in adult pneumonia. Am. J. Med.
Sci. 257:44-51.
20. File, T. M., and J. S. Tan. 1983. Cefoperazone versus cefamandole in the treatment of acute bacterial lower respiratory tract
infections. J. Antimicrob. Chemother. 11:75-82.
21. Garb, J. L., R. B. Brown, J. R. Garb, and R. W. Tuthill. 1978.
Differences in etiology of pneumonias in nursing homes and
community patients. J. Am. Med. Assoc. 240:2169-2172.
22. Garibaldi, R. A. 1985. Epidemiology of community-acquired
respiratory tract infections in adults. Am. J. Med. 78(Suppl.
6B):32-37.
23. Gavan, T. L., and A. L. Barry. 1980. Microdilution test procedures, p. 459-462. In E. H. Lennette, A. Balows, W. J.
Hausler, Jr., and J. P. Truant (ed.), Manual of clinical microbiology, 3rd ed. American Society for Microbiology, Washington,
D.C.
24. Geckler, R. W., G. D. McCormack, and J. S. Goodman. 1984.
Comparison of cefonicid and cefamandole for the treatment of
community-acquired infections of the lower respiratory tract.
Rev. Infect. Dis. 6(Suppl. 4):847-852.
25. Grieco, M. M., M. Lange, J. A. Daniels, M. Den, N. Atnaram,
and H. Kornfeld. 1982. Single-blind controlled study of
ceftizoxime and cefamandole in the treatment of communityacquired pneumonia. J. Antimicrob. Chemother. 10(Suppl.
C):223-225.
26. Hoverman, I. V., and L. 0. Gentry. 1978. Cefamandole nafate in
the treatment of acute bacterial pneumonia. Curr. Ther. Res.
24:622-629.
27. Isenberg, H. D., J. A. Washington II, A. Balows, and A. C.
Sonnenwirth. 1980. Collection, handling, and processing of
specimens, p. 52-82. In E. H. Lennette, A. Balows, W. J.
Hausler, Jr., and J. P. Truant (ed.), Manual of clinical microbiology, 3rd ed. American Society for Microbiology, Washington,
D.C.
28. Joyce, S. M. 1985. Transtracheal aspiration, p. 80-83. In J. R.
Roberts and J. R. Hedges (ed.), Clinical procedures in emergency medicine. The W. B. Saunders Co., Philadelphia.
29. Kalinske, R. W., R. H. Parker, D. Brandt, and P. D. Hoeprich.
1967. Diagnostic usefulness and safety of transtracheal aspiration. N. Engl. J. Med. 276:604-608.
30. Karnad, A., A. Salvador, and S. L. Berk. 1985. Pneumonia
caused by gram-negative bacilli. Am. J. Med. 79(Suppl.
1A):61-67.
31. Keeton, G. R., B. Kehoe, S. W. Phillips, and H. Daya. 1983.
Ceftazidime and cefamandole in the treatment of pneumonia. J.
Antimicrob. Chemother. 12(Suppl. A):27-30.
32. Kilian, M. 1980. Haemophilus, p. 330-336. In E. H. Lennette,
A. Balows, W. J. Hausler, Jr., and J. P. Truant (ed.), Manual of
clinical microbiology, 3rd ed. American Society for Microbiology, Washington, D.C.
33. Klimek, J. J., E. Ajemian, S. Fontecchio, J. Gracewski, B.
Klemas, and L. Jimenez. 1983. Community-acquired pneumonia
requiring admission to hospital. Am. J. Infect. Control 11:79-82.
34. La Force, F. M. 1985. Community-acquired lower respiratory
tract infections. Am. J. Med. 78(Suppl. 6B):52-57.
35. LaFrock, J. L., A. Molavi, A. L. Lentnek, K. V. I. Rolston, P. H.
Chandrasekar, B. R. Smith, W. Kannangara, R. F. Schell, S. S.
Oakes, and B. B. Carr. 1982. Comparative study of ceftizoxime
and cefamandole in the treatment of bronchopulmonary infections. J. Antimicrob. Chemother. 10(Suppl. C):215-221.
36. Larsen, R. A., and J. A. Jacobson. 1984. Diagnosis of community-acquired pneumonia: experience of a community hospital.
Compr. Ther. 10:20-25.
37. Lode, H. 1986. Initial therapy of pneumonia. Am. J. Med.
882
WEBER ET AL.
80(Suppl. 5C):70-74.
38. Louria, D. B., H. L. Blumenfeld, J. T. Ellis, E. D. Kilbourne, and
D. E. Rogers. 1959. Studies on influenza in the pandemic of
1957-1958. II. Pulmonary complications of influenza. J. Clin.
Invest. 38:213-265.
39. Lyons, R. W., S. M. Brock, and B. Lahiri. 1982. Ceftizoxime
and cefamandole in adult patients with acute respiratory failure.
J. Antimicrob. Chemother. 10(Suppl. C):227-228.
40. MacFaIrlane, J. T., R. G. Finch, M. J. Ward, and A. D. MacRae.
1982. Hospital study of adult community-acquired pneumonia.
Lancet ii:255-258.
41. Mandell, G. L. 1980. Cefamandole treatment of pulmonary
infection caused by gram-negative rods. Scand. J. Infect. Dis.
Suppl. 25:107-111.
42. Mattson, K., O.-V. Renkonen, A. Kohvakka, and H. Kikitalo.
1980. Clinical experience with cefamandole in pneumonia.
Scand. J. Infect. Dis. Suppl. 25:103-106.
43. McKellar, P. P. 1985. Treatment of community-acquired pneumonia. Am. J. Med. 79(Suppl. 2A):25-31.
44. Meyers, B. R., G. Wormser, G. Gartenberg, P. Nicholas, and
S. Z. Hirschman. 1978. Cefamandole: a new cephalosporin for
therapy of hospitalized patients with infection. Mt. Sinai J.
Med. 45:722-728.
45. Morella, J. A., and M. Bohnhoff. 1980. Neisseria and
Branhamella, p. 111-130. In E. H. Lennette, A. Balows, W. J.
Hausler, Jr., and J. P. Truant (ed.), Manual of clinical microbiology, 3rd ed. American Society for Microbiology, Washington,
D.C.
46. Mufson, M. A., V. Chang, V. Gill, S. C. Wood, M. J. Romansky,
and R, M. Chanock. 1967. The roles of viruses, mycoplasmas
and bacteria in acute pneumonia in civilian adults. Am. J.
Epidemiol. 86:526-544.
47. Murray, P. R., and J. A. Washington II. 1975. Microscopic and
bacteriologic analysis of expectorated sputum. Mayo Clin.
Proc. 50:339-344.
48. Musher, D. M., K. R. Kubitschek, J. Crennan, and R. E.
Baughn. 1983. Pneumonia and acute febrile tracheobronchitis
due to Haemophilus influenzae. Ann. Intern. Med. 99:444 450.
49. National Center for Health Statistics. 1984. Vital statistics of
United States. 1979. National. Center for Health Statistics,
Hyattsville, Md.
50. National Committee for Clinical Laboratory Standards. 1972.
Performance standards for clinical laboratory standards. Approved standard. National Committee for Clinical Laboratory
Standards, Villanova, Pa.
51. National Committee for Clinical Laboratory Standards. 1981.
Performance standards for antimicrobial disc susceptibility
tests. Approved standard ASM-2, vol. 2, no. 2. National Committee for Clinical Laboratory Standards, Villanova, Pa.
52. Pennington, J. E. 1983. Community-acquired pneumonia and
ANTIMICROB. AGENTS CHEMOTHER.
53.
54.
55.
56.
57.
58.
59.
60.
61.
62.
63.
64.
65.
66.
acute bronchitis, p. 125-134. In J. E. Pennington (ed.), Respiratory infections: diagnosis and management. Raven Press,
New York.
Perlino, C. A., and M. E. Plaut. 1977. Cefamandole treatment of
bacterial pneumonia. Curr. Ther. Res. 22:807-813.
Petty, B. G., C. R. Smith, J. C. Wade, G. L. Conrad, J. J.
Lipsky, J. J. Ellner, and P. S. Lietman. 1978. Double-blind
comparison of cefamandole and penicillin in pneumococcak
pneumonia. Antimicrob. Agents Chemother. 14:13-16.
Plaut, M. E., and C. A. Perlino. 1978. Cefamandole vs. procaine
penicillin for treatment of pneumonia due to Streptococcus
pneumoniae: a random trial. J. Infect. Dis. 117(Suppl.):133-138.
Prout, S., P. D. Potgieter, A. A. Forder, J. W. Moodie, and J.
Matthews. 1983. Acute community-acquired pneumonia. S. Afr.
Med. J. 64:443-446.
Rein, M. F., J. M. Gwaltney, W. M. O'Brien, R. H. Jennings,
and G. L. Mandell. 1978. Accuracy of Gram's stain in identifying pneumococci in sputum. J. Am. Med. Assoc. 239:26712673.
Rodriguez, J., G. J. Vazquez, R. H. Bermudez, A. Luina, and
C. H. R. Ronda. 1982. A randomnized clinical trial of ceftizoxime
and cefamandole in the treatment of serious lower respiratory
tract infections. J. Antimicrob. Chemother. 10(Suppl. C):
209-213.
Saginur, R., and J. G. Bartlett. 1980. Antimicrobial drug susceptibility of respiratory isolates of Hemophilus influenzae from
adults. Am. Rev. Respir. Dis. 122:61-63.
Schwartzmann, S. W., J. L. Adler, R. J. Sullivan, and W. M.
Marine. 1971. Bacterial pneumonia during the Hong Kong
influenza epidemic of 1968-1969. Experience in a city-county
hospital. Arch. Intern. Med. 127:1037-1041.
Sullivan, R. J., W. B. Dowdle, W. M. Marine, and J. C.
Hierholzer. 1972. Adult pneumonia in a general hospital. Arch.
Intern. Med. 129:935-942.
Thorsteinsson, S. B., D. M. Musher, and T. Fagan. 1975. The
diagnostic value of sputum culture in acute pneumonia. J. Am.
Med. Assoc. 233:894-895.
Verghese, A., and S. Berk. 1983. Bacterial pneumonia in the
elderly. Medicine (Baltimore) 62:271-285.
Wallace, R. J., Jr., D. M. Musher, and R. R. Martin. 1978.
Haemophilus influenzae pneumonia in adults. Am. J. Med.
64:87-93.
Wallace, R. J., Jr., S. L. Niefield, S. Waters, B. Waters, R. J.
Awe, K. Wiss, R. R. Martin, and S. B. Greenberg. 1982. Comparative trial of cefonicid and cefamandole in the therapy of
community-acquired pneumonia. Antimicrob. Agents Chemother. 21:231-235.
White, R. J., A. D. Blainey, K. J. Harrison, and S. K. R. Clarke.
1982. Causes of pneumonia presenting to a district general
hospital. Thorax 36:566-570.
Anda mungkin juga menyukai
- Jurnal Cefamandol 2 PDFDokumen4 halamanJurnal Cefamandol 2 PDFTwiin Roffie QlleeBelum ada peringkat
- 92 173 1 SM PDFDokumen9 halaman92 173 1 SM PDFMeri Novita SariBelum ada peringkat
- 92 173 1 SM PDFDokumen9 halaman92 173 1 SM PDFMeri Novita SariBelum ada peringkat
- Studi Geseran Spektrum UV Senyawa Asam Barbiturat Pada Plat Al-TLC Si G 60 F254 Akibat Pengaruh Perbedaan PH Pengeluen Untuk Keperluan Uji KonfirmasiDokumen4 halamanStudi Geseran Spektrum UV Senyawa Asam Barbiturat Pada Plat Al-TLC Si G 60 F254 Akibat Pengaruh Perbedaan PH Pengeluen Untuk Keperluan Uji KonfirmasiTwiin Roffie QlleeBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Differences in Housemen Performance from CUCMS and Other Medical SchoolsDokumen10 halamanDifferences in Housemen Performance from CUCMS and Other Medical SchoolsAfif AizatBelum ada peringkat
- Vaccination ScheduleDokumen1 halamanVaccination ScheduleAmanda KamienBelum ada peringkat
- Prevalence of Soil Transmitted Helminths infection in adults in North SulawesiDokumen4 halamanPrevalence of Soil Transmitted Helminths infection in adults in North SulawesiSahrul hamidBelum ada peringkat
- Olivia Millsop - Case Study Docx 1202Dokumen11 halamanOlivia Millsop - Case Study Docx 1202api-345759649Belum ada peringkat
- Eliminate Papillomas and Warts at Home in 1 Treatment Course - PapiSTOP® PHDokumen9 halamanEliminate Papillomas and Warts at Home in 1 Treatment Course - PapiSTOP® PHkiratuz1998Belum ada peringkat
- Nursing Management of Nephrotic SyndromeDokumen2 halamanNursing Management of Nephrotic SyndromeMARYAM AL-KADHIMBelum ada peringkat
- NCP Impaired Skin IntegrityDokumen3 halamanNCP Impaired Skin IntegrityMiar QuestBelum ada peringkat
- Research EssayDokumen12 halamanResearch Essayapi-608972617Belum ada peringkat
- Atrial Fibrillation - Diagnosis and Treatment - AAFP PDFDokumen8 halamanAtrial Fibrillation - Diagnosis and Treatment - AAFP PDFNaufal AmanullahBelum ada peringkat
- Medicinal ChemistryDokumen8 halamanMedicinal ChemistryLokesh BanthiaBelum ada peringkat
- U.S. clinical observerships help IMGs gain experienceDokumen8 halamanU.S. clinical observerships help IMGs gain experienceAkshit ChitkaraBelum ada peringkat
- Cutaneous MelanomaDokumen226 halamanCutaneous MelanomaGriskalia ChristineBelum ada peringkat
- Juvenile Idiopathic Arthritis (Jia) : IAP UG Teaching Slides 2015-16Dokumen15 halamanJuvenile Idiopathic Arthritis (Jia) : IAP UG Teaching Slides 2015-16KathirBelum ada peringkat
- US vs. Barium for Pediatric GERDDokumen6 halamanUS vs. Barium for Pediatric GERDAndreea KBelum ada peringkat
- Apollo Hospitals: Porters Generic FrameworkDokumen6 halamanApollo Hospitals: Porters Generic FrameworkVaibhav AroraBelum ada peringkat
- Cannabis-An IntroductionDokumen5 halamanCannabis-An IntroductionSaleha TariqBelum ada peringkat
- Sush Unity Haemotology-1700Dokumen51 halamanSush Unity Haemotology-1700Dr-Jahanzaib GondalBelum ada peringkat
- Acute Rheumatic FeverDokumen20 halamanAcute Rheumatic Feverfaizal samadBelum ada peringkat
- Lincomycin: Drug Information: ALERT: US Boxed WarningDokumen12 halamanLincomycin: Drug Information: ALERT: US Boxed WarningsadiaBelum ada peringkat
- Tugas AdmissionDokumen9 halamanTugas Admissionputri rahayuBelum ada peringkat
- Surgery and Surgical NursingDokumen193 halamanSurgery and Surgical NursingFan Eli100% (4)
- Microchem Non GLP ASTM E1052 Study Report NG14797Dokumen6 halamanMicrochem Non GLP ASTM E1052 Study Report NG14797MaryDianne RamosBelum ada peringkat
- UabDokumen20 halamanUabAnonymous n7RT07fzUdBelum ada peringkat
- Coliform BacteriaDokumen4 halamanColiform BacteriaLalu Novan SatriaBelum ada peringkat
- Fact Sheet 1 - Addiction OverviewDokumen5 halamanFact Sheet 1 - Addiction Overviewgoldbergleah100% (1)
- Therapeutically Aspects in Esophageal Atresia: RI Spataru, Niculina Bratu, A NicaDokumen4 halamanTherapeutically Aspects in Esophageal Atresia: RI Spataru, Niculina Bratu, A Nicanatacha479Belum ada peringkat
- Cerebral Concussion - PresentationDokumen19 halamanCerebral Concussion - PresentationAira AlaroBelum ada peringkat
- SickLeaveCertificate With and Without Diagnosis 20240227 144109Dokumen2 halamanSickLeaveCertificate With and Without Diagnosis 20240227 144109Sawad SawaBelum ada peringkat
- Immediate Dental Implant Placement Into Infected vs. Non-Infected Sockets: A Meta-AnalysisDokumen7 halamanImmediate Dental Implant Placement Into Infected vs. Non-Infected Sockets: A Meta-Analysismarlene tamayoBelum ada peringkat
- Cardiac Assessment Cheat SheetDokumen7 halamanCardiac Assessment Cheat Sheetpattie29Belum ada peringkat