The Role of Hormones and Hormonal
Diunggah oleh
nikuHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
The Role of Hormones and Hormonal
Diunggah oleh
nikuHak Cipta:
Format Tersedia
REVIEW ARTICLE
CNS Drugs 2003; 17 (5): 325-342
1172-7047/03/0005-0325/$30.00/0
Adis Data Information BV 2003. All rights reserved.
The Role of Hormones and Hormonal
Treatments in Premenstrual Syndrome
Torbjorn Backstrom, Lotta Andreen, Vita Birzniece, Inger Bjorn, Inga-Maj Johansson,
Maud Nordenstam-Haghjo, Sigrid Nyberg, Inger Sundstrom-Poromaa,
Goran Wahlstrom, Mingde Wang and Di Zhu
Department of Clinical Sciences, Obstetrics and Gynecology, Umea University, Umea, Sweden
Contents
Abstract . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 325
1. Diagnostic Procedure and Criteria . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 326
2. Epidemiology . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 326
3. Aetiology . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 327
3.1 Ovarian Steroids and Symptoms . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 328
3.2 Indications of Different Sex Steroid Sensitivity . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 329
3.3 Neurosteroids . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 329
3.4 Pathogenesis Within the Brain . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 329
4. Treatment . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 330
4.1 SSRIs . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 331
4.2 Hormonal and Antihormonal Treatments . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 331
4.2.1 Induction of Anovulation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 331
4.2.2 Oral Contraceptives . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 334
4.3 Spironolactone . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 336
4.4 Progesterone . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 337
5. Conclusion . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 337
Abstract
Premenstrual syndrome (PMS) is a menstrual cycle-linked condition with both
mental and physical symptoms. Most women of fertile age experience cyclical
changes but consider them normal and not requiring treatment. Up to 30% of
women feel a need for treatment. The aetiology is still unclear, but sex steroids
produced by the corpus luteum of the ovary are thought to be symptom provoking,
as the cyclicity disappears in anovulatory cycles when a corpus luteum is not
formed. Progestogens and progesterone together with estrogen are able to induce
similar symptoms as seen in PMS. Symptom severity is sensitive to the dosage of
estrogen. The response systems within the brain known to be involved in PMS
symptoms are the serotonin and GABA systems. Progesterone metabolites, especially allopregnanolone, are neuroactive, acting via the GABA system in the
brain. Allopregnanolone has similar effects as benzodiazepines, barbiturates and
alcohol; all these substances are known to induce adverse mood effects at low
dosages in humans and animals. SSRIs and substances inhibiting ovulation, such
as gonadotrophin-releasing hormone (GnRH) agonists, have proven to be effective treatments. To avoid adverse effects when high dosages of GnRH agonists are
326
Backstrom et al.
used, add-back hormone replacement therapy is recommended. Spironolactone
also has a beneficial effect, although not as much as SSRIs and GnRH agonists.
The effect of ovarian hormones on mood and
CNS-related disorders is of great interest, especially
since the discovery that some ovarian hormones are
potent modulators of neurotransmitter systems in
the brain. Ovarian hormones have been discussed as
aetiological factors in premenstrual syndrome
(PMS) a menstrual cycle-linked, CNS-related condition since the syndrome was first described.
PMS has long been debated, but today increased
knowledge and agreement on diagnostic criteria
have helped to make PMS research more comparable.
Both patients and clinicians have been confused,
and often in disagreement, over whether PMS
should be considered a disease or merely a normal
phenomenon not requiring treatment. This is largely
because of a failure to appreciate that PMS severity
varies tremendously. Although most women experience mild mood and somatic symptoms premenstrually, a small but significant number are severely
disabled by the disorder.[1] Furthermore, scientists in
the field of PMS have not agreed on which terminology to use.[2] It was not until the publication of
diagnostic criteria for PMS in the American Psychiatric Associations DSM-IV[3] that a distinct diagnosis of a severe form of PMS with mood symptoms
premenstrual dysphoric disorder (PMDD) could
be made.
In this review, we discuss the hormonal background of and possible treatments for PMS.
1. Diagnostic Procedure and Criteria
The correct diagnosis of a disease is essential for
successful treatment. The diagnostic criteria for
PMS have until now been a long-standing problem.
Many diagnostic procedures have been developed.
All modern procedures have one common feature,
namely to establish the cyclical nature of the symptom variation during the menstrual cycle using daily
prospective self ratings of symptoms. A number of
rating scales have been developed, but the type of
Adis Data Information BV 2003. All rights reserved.
scale does not seem to be critical as long as the scale
contains an assessment of the most important symptoms in PMS.
To fulfil the criteria for PMDD (or severe PMS),
patients need to present with at least five of the
following specific symptoms during the premenstrual week: depression, irritability, anxiety/tension, affect lability, decreased interest, difficulty in concentrating, fatigue, feeling out of control, insomnia,
change in appetite, breast tenderness and breast
swelling. At least one of these symptoms must be a
mood symptom. The symptoms must be severe
enough to interfere with usual activities. Patients
must be devoid of symptoms in the follicular phase
to ensure that the premenstrual complaint is not
merely an exacerbation of an underlying mood disorder. The PMDD diagnosis must be confirmed by
prospective ratings for at least 2 months.[3] As none
of the symptoms of PMDD/PMS are unique to the
syndrome, patients need to keep a daily diary of
symptoms for at least 2 months to establish the
temporal relationship between the onset of symptoms and the premenstrual period. Furthermore,
ovulation should be diagnosed, for example by measuring luteal progesterone.
Among 82 consecutive patients seeking help for
cyclical mood changes at a PMS clinic, only 30%
were free of symptoms during the preovulatory
period and 14% did not show a significant mood
change between preovulatory and premenstrual periods.[4] The remaining 56% showed a significant
number of days with preovulatory symptoms
(premenstrual aggravation group). This shows the
need for more objective criteria for diagnosis than a
case history alone. We have found daily prospective
self ratings to be a great help in this respect.
2. Epidemiology
A higher prevalence of premenstrual changes is
reported in retrospective questionnaires compared
with prospective ratings. Up to 75% of fertile woCNS Drugs 2003; 17 (5)
The Role of Hormones and Hormonal Treatments in PMS
327
men retrospectively report changes in mental and
physical symptoms in the premenstrual week.[5]
Over 50% of the participants in community sample
studies report the presence of PMS, but only 26%
of them met the criteria for PMDD.[1,6] Most women
consider PMS to be a normal phenomenon and not a
disease state. This implies that when women say
they have PMS, they are usually not referring to a
medical condition. Rather, they refer to various
changes during the premenstrual phase in some
menstrual cycles, changes most women can manage
by themselves. It is possible that women attach a
different meaning to the construct PMS than researchers and clinicians do. This might partially
explain the discrepancy between studies assessing
the prevalence of PMS using prospective versus
retrospective methods.[7-9]
In community samples, severe and uncomfortable premenstrual symptoms are found in 217% of
fertile women.[1,5,6,10-12] These figures are somewhat
higher than the estimated prevalence of PMDD of
17%, reported in studies using prospective daily
ratings, with recurrent occupational impairment and
conforming to the DSM-IV criteria.[1,6,13-17] From
studies in community samples, 614% of fertile
women state that they wish to consult a physician
regarding their premenstrual symptoms.[1,5,12] In USbased reports, approximately 1030% of the respondents took prescription or over-the-counter medications to relieve premenstrual symptoms.[6,18]
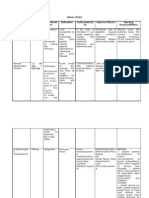
(see figure 1).[19] The severity of symptoms of irritability and depression gradually increased during the
luteal phase in parallel with the rise in serum progesterone levels, beginning shortly after ovulation. The
maximum symptom severity occurred 35 days after the progesterone peak in the luteal phase. The
highest severity occurred during the last 5 premenstrual days or the first day of menstruation. The
symptoms disappeared totally a few days after the
onset of menstrual bleeding, when gonadal hormone
levels had declined. During the preovulatory phase,
there was a period of well-being closely related to
Depression score
Irritability score
40
50
20
3. Aetiology
Adis Data Information BV 2003. All rights reserved.
Progesterone (nmol/L)
60
The temporal symptom variations experienced
during the menstrual cycle and the close link to the
luteal phase indicate that a factor produced by the
corpus luteum of the ovary is involved in provoking
premenstrual symptoms.
One study analysed the relationship between
symptom development and hormonal variations during the menstrual cycle. Women with a history of
cyclical mood changes were asked, during one menstrual cycle, to rate their adverse mood symptoms
daily using a visual analogue scale and give blood
samples for plasma allopregnanolone, estradiol, progesterone and luteinising hormone determinations
Luteinising hormone (U/L)
100
600
40
300
20
Estradiol (pmol/L)
Allopregnanolone (nmol/L)
60
0
1
Postmenstrual
Periovulatory
Premenstrual
Time (days)
Fig. 1. The relationship between premenstrual syndrome (PMS)
symptom development and variations in plasma hormone concentrations during menstrual cycles in women with PMS.
CNS Drugs 2003; 17 (5)
328
Backstrom et al.
the estradiol peak. PMS symptoms had already started to worsen prior to the premenstrual decrease in
the luteal hormones, meaning that a withdrawal
effect of these hormones cannot alone provoke the
symptoms.[19]
This is further supported by the discovery that a
truncation of the late luteal phase of the menstrual
cycle by giving the antiprogestogen mifepristone
does not remove premenstrual symptoms. This suggests that the endocrine events during the late luteal
phase do not directly generate the symptoms of PMS
and that the events provoking the symptoms occur
earlier in the luteal phase.[20]
Despite numerous efforts to identify endocrine
disturbances in patients with PMS, there are very
few consistent endocrine findings. The relationship
between symptom development and the progesterone peak in the luteal phase is obvious, but apart
from that there is a general agreement on the absence of peripheral markers of hypothalamus-pituitary-gonadal axis dysfunction in PMS.[2,21,22] The
most important finding by far is the necessity of
ovulation and corpus luteum formation for PMS
development. During anovulatory cycles, spontaneous or induced, when a corpus luteum is not formed,
the cyclicity in symptoms disappears.[23-27] The effect of induced anovulation as a treatment for PMS
is discussed further in section 4.2.1.
3.1 Ovarian Steroids and Symptoms
Although no differences in progesterone and estradiol plasma levels have been shown between patients with PMS and control individuals, these sex
steroids appear to have an impact on symptom development and severity within patients. Particular
attention has been paid to estradiol, progesterone
and progesterone metabolites active on the GABAA
receptor in the brain. Evidence to substantiate this
assumption is found through sequential hormone
replacement therapy (HRT) in postmenopausal women. Estrogen/progestogen sequential replacement
therapy resembles the hormonal variations of an
ovulatory menstrual cycle, and estrogen-only treatment is similar to an anovulatory cycle. Women
receiving sequential HRT respond with a significant
Adis Data Information BV 2003. All rights reserved.
deterioration in their mood and physical signs when
progestogen is given during the final part of the
treatment cycle, whereas those receiving estrogen
alone do not show any deterioration in mood at the
end of the treatment cycle.[28-30] Estrogen + progestogen add-back therapy during gonadotrophin-releasing hormone (GnRH) agonist treatment in PMS
(to relieve hypoestrogenic symptoms) induces
progestogenic adverse effects similar to the symptoms in PMS, although the efficacy of the GnRH
treatment on mood symptoms is still evident.[27]
Both estradiol and progesterone seem to be of
importance, as symptoms were induced with both
estrogen and progesterone in women with PMS in
whom the ovarian function had been interrupted
with GnRH agonists.[31] Increased estradiol and progesterone plasma levels during the luteal phase were
found to be related to more severe symptoms when
compared with cycles in the same individuals with
lower luteal phase estradiol and progesterone levels.
The symptom severity was in particular related to
the luteal estradiol levels.[32] In addition, a subgroup
of patients with higher luteal phase estradiol levels
showed more severe symptoms compared with patients with lower luteal phase estradiol.[33] Moreover, estradiol treatment during the luteal phase
induced more negative symptoms than placebo in a
group of patients with PMS.[34] Postmenopausal women receiving HRT and with higher plasma estradiol levels during the progestogen period experienced
more symptoms than women with lower levels.[35]
Together with the progestogen, a higher dosage of
estrogen (3 mg/day compared with 2 mg/day)
caused significantly more negative mood and physical symptoms than the lower dosage in the same
patients in a double-blind study. However, a higher
estrogen dosage by itself without progestogen did
not induce more symptoms. The conclusion is that
an increase in the estrogen dose accentuates negative mood and physical symptoms during the
progestogen phase of sequential HRT but not in the
absence of a progestogen.[36]
This finding is consistent with the follicular
phase of the menstrual cycle, when estrogen dominates and reaches its highest levels. At the preovuCNS Drugs 2003; 17 (5)
The Role of Hormones and Hormonal Treatments in PMS
329
latory phase, women with PMS feel at their best and
estradiol does not seem to provoke symptoms. Obviously, estradiol and progesterone acting together
seem to induce a different response in the CNS than
when they act separately.
tolerance for GABAA receptor allosteric agonists.[40-42]
3.2 Indications of Different Sex
Steroid Sensitivity
If there is no difference in sex steroid levels
between patients with PMS and control individuals,
some other difference must exist, as not all women
react to the substances produced by the corpus luteum. At least two other possibilities exist, namely
that an as yet unknown provoking factor is produced
from the corpus luteum in women with PMS, or that
the sensitivity in the brain to the steroids differs
between patients and control individuals.
There exists some evidence for the latter hypothesis. In a double-blind study of the effect of oral
contraceptives on mood, it was found that it was
mainly women with PMS who reacted with negative
mood changes while receiving oral contraceptives.[37] Women who had difficulty tolerating oral
contraceptives reported a greater number of moderate/severe premenstrual changes.[38] In women with
PMS who were given a GnRH agonist to inhibit
ovarian hormone production, add-back therapy of
estradiol or progesterone resulted in a significant
recurrence of symptoms; women without PMS who
received the same regimen and women with PMS
who were given placebo during continued GnRH
agonist administration experienced no changes in
mood.[31] Postmenopausal women with a history of
PMS responded with more negative symptoms
while receiving progestogens than women without a
PMS history.[30] The sedative response to intravenous pregnanolone, a progesterone metabolite and
GABAA receptor agonist) was reduced in the luteal
phase in patients with PMS compared with control
individuals.[39] In addition, patients with severe
symptoms were less sensitive to the given pregnanolone than patients with more moderate symptoms.[39] Similar results were obtained with alcohol
and benzodiazepines given intravenously, suggesting that patients with PMS have developed a
Adis Data Information BV 2003. All rights reserved.
3.3 Neurosteroids
The progesterone metabolites allopregnanolone
and pregnanolone, which have benzodiazepine-like
effects, have been analysed in serum with contradictory results. Some studies have detected significantly lower plasma levels of allopregnanolone in the
late luteal phase in PMS patients compared with
control individuals, while other studies have
not.[43-47] In a study comparing two cycles in the
same women, worse symptoms were seen during
cycles with high levels of estradiol, pregnenolone
and pregnenolone sulphate, whereas cycles with increased levels of allopregnanolone were associated
with a better well-being.[44] Although plasma levels
of neuroactive steroids may or may not differ between PMS patients and control individuals,
neuroactive steroids might still play a role in the
symptom provocation of PMS if the differences
between women with and without PMS are based on
neuroactivity within the brain.
3.4 Pathogenesis Within the Brain
As discussed in sections 3.13.3, there are strong
indications that the steroids from the corpus luteum
are the provoking factor. However, there must exist
a response system within the brain where the action
takes place. The classical hormonal receptors for
estradiol and progesterone exist in the brain and are
specifically distributed to certain areas.[48] Some
authors claim that central progesterone receptors are
not involved in PMS pathophysiology.[49] Treatment
with mifepristone, a progesterone receptor antagonist that provides effective blockade of the progesterone receptors, did not alleviate premenstrual symptoms.[49] More research needs to be conducted
before this issue can be resolved.
The serotonin and GABA systems are considered
the two transmitter systems most involved in PMS
aetiology. The serotonin system is considered mainly because SSRIs are effective treatments for PMS
and PMDD. The direct mechanism by which they
work is unknown, but many studies indicate a conCNS Drugs 2003; 17 (5)
330
nection between the serotonin system and PMS.[50]
Challenge studies have shown blunted responses to
serotonergic interventions, but as the results are
found during the entire cycle, it has been suggested
that the change in the serotonin system is a vulnerability trait rather than a state marker of PMS.[50]
Tryptophan depletion causes a significant aggravation of premenstrual symptoms compared with a
sham procedure, and symptom magnitude correlates
with tryptophan decrease.[51] Altered platelet paroxetine binding in the follicular phase has been found
in women with PMDD but not in control individuals. Furthermore, paroxetine binding was normalised by successful treatment of PMDD with a low
dose of the GnRH agonist buserelin (see section
4.2.1). The results are consistent with the hypothesis
that changes in serotonergic transmission could be a
feature of PMDD.[52] However, steroid hormone
fluctuations across the menstrual cycle alter binding
for the serotonin 5-HT2A receptor and serotonin
transporter. Progesterone appears to be the major
determinant for these changes.[53]
Direct connections between the serotonin and
GABA systems have also been shown, as the
GABAA receptor subunit composition changes in
knockout mice without the 5-HT1A receptor.[54] Also, when PMDD patients were treated with SSRIs,
the decreased sensitivity towards pregnanolone in
the luteal phase normalised in parallel with the improvement of symptoms.[55]
The GABA transmitter system is the major inhibitory system in the mammalian CNS. The progesterone metabolite allopregnanolone is a GABAA receptor positive modulator and a potent neurosteroid
with behavioural and biochemical characteristics
similar to ethanol, barbiturates and benzodiazepines.
Another potent progesterone metabolite is pregnanolone, also naturally produced during the menstrual cycle.[22,39,56] Benzodiazepines, barbiturates, alcohol and allopregnanolone have been shown to exert
a bimodal action on negative mood symptoms. At
high dosages they have anxiolytic, antiaggressive,
sedative/anaesthetic and antiepileptic effects in both
animals and humans.[22,56,57] However, in low concentrations or doses, severe adverse emotional reac Adis Data Information BV 2003. All rights reserved.
Backstrom et al.
tions are induced in approximately 23% of individuals and moderate emotional reactions in up to 20%
of individuals.[58-67] These GABAA receptor-active
drugs induce negative mood, irritability and aggression.
A bimodal effect has also been noted with different dosages of medroxyprogesterone and natural
progesterone in postmenopausal women.[68,69] Postmenopausal women taking HRT felt worse in terms
of irritability and negative mood effects while taking
medroxyprogesterone 10mg than medroxyprogesterone 20mg[68] and worse while taking vaginal progesterone 400mg than vaginal progesterone
800mg.[69]
As another indication that a low concentration of
allopregnanolone is involved in negative mood induction, female rats exhibit increased anxiety behaviour during low-dose and short-term progesterone
treatment.[70] This is due to an allopregnanolone
effect and occurs in parallel with an upregulation of
the hippocampal 4 subunit of the GABAA receptor
and decreased benzodiazepine sensitivity.[70] This
effect corresponds with a reduction in benzodiazepine sensitivity in women with PMDD.[40,41]
This decreased sensitivity is an indication of a tolerance development to allopregnanolone that is
known to occur.[71] Another indication of the involvement of allopregnanolone in menstrual cyclelinked, CNS-related changes is that in women with
petit mal epilepsy, the absence seizure frequency
has a similar pattern during the menstrual cycle as
the mood changes in PMS.[72] Allopregnanolone and
progesterone are known to exacerbate petit mal epilepsy.[72-74]
4. Treatment
There are two main principles for the treatment of
PMS. One treatment strategy focuses on hormonal
treatments of different types, mainly by inducing an
anovulatory state. The other treatment strategy focuses on effects within the CNS that ameliorate or
block the effects of the provoking factor; this latter
strategy is related to the similarities and interactions
between PMS and major depression and aims at
modulating serotonergic neurotransmission. The
CNS Drugs 2003; 17 (5)
The Role of Hormones and Hormonal Treatments in PMS
treatments that have shown benefit over placebo
treatments are SSRIs; treatments that induce anovulation, such as GnRH agonists, high dosages of
estrogen, low dosages of danazol (an antigonadotrophin) and surgical oophorectomy; and spironolactone (an aldosterone, androgen and progesterone
antagonist).
4.1 SSRIs
The SSRI treatments are beyond the scope of this
paper, but it should be noted that they are effective
treatments for PMS, as shown in a meta-analysis
recently completed.[75]
The effectiveness of tricyclic antidepressants
with a serotonergic profile[76] and SSRIs[75,77] in the
treatment of PMS has been confirmed in several
clinical trials. Most studies have evaluated continuous treatment, but cyclic treatment (during the last
14 days of the menstrual cycle) has also been proven
effective.[78] Long-term studies using SSRIs are as
yet scarce, but one study evaluated the use of fluoxetine for a mean of 18 months and concluded that it
was effective and well tolerated.[79] Approximately
half of the subjects achieved complete remission of
symptoms, while the others experienced significant
improvement. Sexual dysfunction was the most
common adverse effect, occurring in 17% of women.[79,80]
4.2 Hormonal and Antihormonal Treatments
4.2.1 Induction of Anovulation
By inducing anovulation, premenstrual symptom
cyclicity disappears. Induction of anovulation can
be accomplished by the use of GnRH analogues, but
other methods are also possible. Estradiol implants
in high enough doses cause anovulation; medroxyprogesterone in high dosages and danazol are also
able to inhibit ovulation and consequently have an
effect on the cyclicity of symptoms.[81,82] Oophorectomy, the first described treatment for PMS, has a
marked effect on PMS symptoms. However, hysterectomy while leaving the ovaries intact does not
relieve PMS.[83]
Adis Data Information BV 2003. All rights reserved.
331
High-Dosage Gonadotrophin-Releasing Hormone
(GnRH) Agonists
Anovulation and amenorrhoea can be achieved
using either a depot injection or nasal spray in high
dosages similar to those used for endometriosis
treatment. The treatment is hormonally similar to a
medical reversal oophorectomy. The use of GnRH
agonists depends on their ability to cause pituitary
desensitisation to GnRH through downregulation of
the GnRH receptor. During downregulation, luteinising hormone and follicle-stimulating hormone secretion by the pituitary is substantially reduced. As a
consequence, normal sex steroid production is interrupted and anovulation and amenorrhoea are obtained. Several studies have evaluated high-dosage
GnRH agonist treatment in PMS and, although these
drugs are difficult to blind, most studies have used
placebo comparisons and reported a marked positive
effect on the premenstrual symptoms.[24-27,84-91]
Symptom relief occurs in both psychoemotional
and physical symptoms with high-dosage GnRH
agonist treatment in PMS.[24-27,84-91] There are, however, women who cannot tolerate the adverse effects
of climacteric symptoms. Also, women who experience a premenstrual aggravation of symptoms that
occur throughout their cycle especially depression
do not experience full relief with the treatment.[25,26,31,85,89] In addition, one study did not show
high-dosage GnRH agonist treatment to be effective
when compared with placebo, but this study did not
use the common DSM-IV criteria for the diagnosis
of PMS.[92] Long-term treatment has also shown
relief of symptoms for the duration of the treatment.[85,88]
The main drawback to GnRH agonist treatment
at high dosages is the hypoestrogenism and its consequences for bone mineral density, postmenopausal symptoms and perhaps also cognitive function.
Given the deteriorating effect on bone mass, GnRH
agonist treatment cannot be used in clinical practice
for more than 69 months without adding back
estradiol and progestogen. To avoid the adverse
effects of treatment, add-back therapy using estrogen/progestogen HRT has been tried. Since all of
the short- and long-term adverse effects of GnRH
agonist therapy are the result of hypoestrogenism,
CNS Drugs 2003; 17 (5)
332
Backstrom et al.
this is based on sound rationale. However, some of
the PMS symptoms return during add-back therapy
as progestogenic adverse effects. Despite this, the
efficacy of the GnRH agonist treatment on mood
symptoms compared with placebo was still evident,
even when combined with the estrogen/progestogens add-back therapy.[26,27,31,90,91,93] In one study,
tibolone was used as add-back therapy and, in combination with GnRH agonist therapy, was found to
be superior to placebo.[91] There are now randomised, placebo-controlled studies showing a beneficial effect with GnRH agonists plus add-back therapy.[26,27,31,90,91,93] With this regimen, the risks and
adverse effects of the treatment are limited.
Lower-Dosage GnRH Agonists
If the GnRH agonist is used at a lower dosage, the
downregulation of the follicle-stimulating hormone
and luteinising hormone production from the pituitary will not be complete. Ovulation will then be
inhibited, but estradiol production will continue.
With this treatment, patients will not experience
climacteric vasomotor symptoms as adverse effects.
The risk with lower-dosage GnRH agonists is
that endometrial hyperplasia develops with longterm treatment. In a double-blind, placebo-controlled, crossover study, 23 patients with PMS received nasal buserelin 400g once a day for 3
months. Twenty-one of the patients became anovulatory on that dosage, and two became amenorrhoeic. During the anovulatory cycles with buserelin
treatment, cyclical mood changes had disappeared.
However, during treatment with placebo, patients
still showed cyclical mood changes. In addition,
patients felt significantly better during the anovulatory cycles with buserelin treatment than with
placebo treatment.[24] If this type of treatment is to
be used long term, progestogens must be given at
regular intervals to properly protect the endometrium. Negative progestogenic adverse effects may
then occur, possibly lessening the benefit of the
treatment.
Ultra-Low Dosage GnRH Agonists
In one double-blind, placebo-controlled crossover study, 27 women with severe PMS/PMDD
were treated with nasal spray buserelin 100g once
Adis Data Information BV 2003. All rights reserved.
a day for 2 months.[94] With this ultra-low dosage,
women still ovulate, but steroid production during
the luteal phase from the corpus luteum is decreased.
The primary outcome measure consisted of daily
ratings by the patients for mood and physical symptoms throughout the study. The results showed that
the low-dose GnRH agonist, compared with placebo, significantly relieved premenstrual irritability
and depression. Also, positive symptoms such as
friendliness and cheerfulness were improved during
the premenstrual week. Likewise, physical symptoms of swelling and headache were significantly
improved during buserelin treatment, though breast
tenderness scores were unaffected.
As mentioned in section 3.4, some indicators of a
disturbed serotonin system in patients with PMDD
were normalised during treatment with ultra-low
doses of buserelin.[52] However, the ultra-low dose
GnRH agonist treatment regimen induced anovulation in as many as 56% of patients, though these
patients were significantly older (>35 years) than
those women who maintained ovulatory cycles
throughout the study.[94] The advantage with this
regimen is that ovulatory women continue to have
regular menstrual cycles, and the adverse effects are
therefore minimal. The disadvantage is that some of
the older women became anovulatory, therefore experiencing the disadvantages of anovulation described above. Further studies are needed before this
type of treatment can be widely used.
Other Methods for Induction of Anovulation
A high dosage of estradiol in the form of subcutaneous pellets or transdermal estradiol patches (2
100g) has been given to suppress ovulation in
controlled studies.[81,95-97] Both routes of administering estradiol were effective for treating mental and
physical symptoms of PMS. To hinder endometrial
hyperplasia, cyclical progestogens were given to
ensure a regular withdrawal bleed. Although progestogenic adverse effects occurred, the net improvement was greater than with placebo.[81,95-97]
A randomised, prospective trial comparing estradiol patches in dosages of 100 and 200g twice
weekly combined with cyclical progestogens showed no difference in the effectiveness of these two
CNS Drugs 2003; 17 (5)
The Role of Hormones and Hormonal Treatments in PMS
333
dosages. However, a greater dropout rate and a
greater incidence of adverse effects attributed to
estrogen was noted in the higher dosage group.[97]
ies. Danazol is known to have androgenic adverse
effects on lipids and to cause acne, vocal changes
and negative mood at the higher dosage used for
endometriosis. However, these symptoms were not
observed with the dosages used in the six aforementioned studies. Despite this, the study withdrawal
rates were higher in these studies (32.5%) than those
seen in other PMS studies (11.5%).[24,101]
Progestogens including medroxyprogesterone
are known to increase appetite and weight. With the
aim to reduce the risk of potential adverse effects,
danazol 200 mg/day was given only in the luteal
phase of the menstrual cycle in a randomised, double-blind, placebo-controlled study over 3
months.[104] The study enrolled 100 women with
PMS and mastalgia. Significant improvement was
seen for mastalgia, but no improvement was seen for
any other symptom or for the global PMS score.
A long-term follow-up study of 50 patients who
had used estradiol implants for PMS for a mean of
5.6 years (range 28 years) was conducted.[98] There
was a continued beneficial response to treatment for
all symptoms, varying from 74% for bloating to
96% for depression. Cyclical progestogenic symptoms occurred in 58% of patients. These were partially relieved by alterations in dose, type and duration of progestogen treatment, but in seven patients
the symptoms remained severe. Attempts to reduce
the dose of progestogen led to cystic hyperplasia in
four patients. There were no complications from
venous thrombosis, pulmonary embolus, breast disease or atypical endometrial hyperplasia.
A high dosage of progestogens alone has also
been used to inhibit ovulation. In a placebo-controlled, double-blind, crossover study, an oral dosage of 15 mg/day for 21 days each cycle of either
medroxyprogesterone or norethisterone suppressed
ovulation.[99] Both progestogens significantly reduced breast discomfort compared with placebo.
Medroxyprogesterone also significantly improved
individual psychological symptom scores by the
second active treatment cycle and total psychological symptom scores in both active cycles; however,
norethisterone was no more effective than placebo.
A rather high dropout rate (27%) was evident in this
study, with menstrual disturbances as the main adverse effect.
Danazol, a progestogen with some androgen
properties, given for the treatment of endometriosis,
has also been used in the treatment of PMS. The
dosages used in PMS treatment 100mg twice a day
or 200mg once a day are lower than the dosages
used for endometriosis. At these dosages, ovulation
inhibition occurs in the majority of cases.[82,100-103]
Five placebo-controlled, double-blind studies and
one open-label study compared danazol 200 mg/day
with placebo.[82,100-103] In each study, danazol had a
beneficial effect on PMS symptoms compared with
placebo in cycles where anovulation was obtained,
despite the relatively small sample sizes of the stud Adis Data Information BV 2003. All rights reserved.
Surgical Oophorectomy
Surgical oophorectomy is a dramatic way of interrupting ovulation and is, of course, impossible to
assess in randomised, placebo-controlled studies.
However, the two reports below describe substantial
effects consistent with the results from other methods of inhibiting ovulation. This approach cannot be
recommended except in well informed patients with
extremely severe PMS who have failed to benefit
from previous medical treatments.
In the first study, 14 women with severe PMS
were first successfully treated with danazol to suppress cyclic ovarian steroidogenesis.[105] Following
this, a bilateral ovariectomy and concomitant hysterectomy were performed. Both medical ovarian suppression and ovariectomy with low-dose estrogen
add-back therapy afforded lasting relief from cyclic
symptoms of PMS.
In another study, 14 women with severe,
debilitating PMS underwent a hysterectomy and
oophorectomy and were given continuous estrogen
replacement.[106] All patients had clear cyclic symptoms and psychological scores consistent with a
major disruption of their lives before surgery. All
previous medical treatments had failed to benefit
these patients. The diagnosis and severity of PMS
were assessed by means of prospective charting and
CNS Drugs 2003; 17 (5)
334
Backstrom et al.
psychological evaluation. Six months after surgery,
PMS symptom charting revealed complete disappearance of a cyclic pattern, with scores equivalent
to those of a healthy population. Psychological measures 6 months after the operation showed a dramatic improvement in mood, general affect, well-being,
life satisfaction and overall quality of life.
4.2.2 Oral Contraceptives
In general, oral contraceptives are not known to
have as beneficial an effect on mood symptoms. In
fact, negative mood symptoms are a well known
adverse effect of oral contraceptive use in women of
fertile age. Approximately 3050% of women state
adverse mood effects as a reason for interrupting or
changing oral contraceptive use.[107,108] Several studies have investigated oral contraceptives and their
relation to PMS in both clinical trials and naturalistic settings.
In a double-blind study, Cullberg[37] investigated
whether oral contraceptives with three different
norgestrel dosages would produce negative mood
symptoms in a group of women recruited from the
general Swedish population. The majority of women
did not react to any of the dosages, but women with
a history of PMS experienced negative mood symptoms while taking the ethinylestradiol/norgestrel
combination at the lowest dosage. This suggests that
women with PMS are more sensitive to hormonal
provocation than women without PMS.
A few studies have suggested that there is a
similarity in the adverse mood effects experienced
with oral contraceptives and the symptoms experienced in PMS.[109,110] Women taking oral contraceptives continued to show cyclical mood changes,
but these changes tended to be of a different pattern
during the treatment cycle than those observed when
they were not taking oral contraceptives.[109,110]
In a retrospective, community-based prevalence
study, PMS symptoms were reported by a significantly higher proportion of women who did not
receive oral contraceptives compared with those
who did receive oral contraceptives.[5] In a casecontrol questionnaire study, premenstrual changes
were assessed in 101 women using oral contraceptives and 149 not using oral contraceptives.[38] Wo Adis Data Information BV 2003. All rights reserved.
men using oral contraceptives had lower severity
scores on the subscales of premenstrual anxiety,
fatigue, negative mood, water retention and impaired social functioning than those not using oral
contraceptives. Women who had experienced difficulty tolerating oral contraceptives reported a
greater number of moderate/severe premenstrual
changes. In women who were recruited from the
general Icelandic population, daily prospective
symptom ratings revealed that users and non-users
of oral contraceptives reported similar frequencies
of cyclical symptom changes.[1]
The interpretation of the above studies is not
easy, but it appears that women with a history of
PMS are less likely to take oral contraceptives than
women without a history of PMS. This may explain
the lower prevalence of PMS symptoms in women
taking oral contraceptives, as women with PMS
react badly to oral contraceptives and stop taking
them. Another interpretation may be that oral contraceptives do actually have a treatment effect on
PMS symptoms. However, given the negative findings from studies assessing the use of oral contraceptives in the treatment of women with PMS (discussed in the following section), this seems unlikely.
Oral Contraceptive Treatment Studies
The rationale for using oral contraceptives as
PMS treatment is that they inhibit ovulation. However, clinical trials assessing the use of oral contraceptives as possible therapeutics for PMS have
yielded disappointing results; the treatment effect of
oral contraceptives on mood changes has not exceeded that of placebo in controlled studies.[111]
In one study, 82 women with moderate to severe
premenstrual symptoms were enrolled in a doubleblind, placebo-controlled trial of a triphasic oral
contraceptive over 3 months.[111] Forty-five women
with confirmed premenstrual changes completed the
study. Physical symptoms significantly improved
with active treatment compared with placebo, but
there were no beneficial effects over placebo for any
of the mood symptoms. In fact, sexual interest decreased in women taking oral contraceptives, an
effect that was independent of any adverse influence
on mood.
CNS Drugs 2003; 17 (5)
The Role of Hormones and Hormonal Treatments in PMS
335
In another study, 276 oral contraceptive users
(171 combined and 105 triphasic) were compared
with 276 non-users.[112] All women regarded themselves as having PMS, and the groups were matched
for age, parity and marital status. The oral contraceptive users reported significantly less menstrual
pain and premenstrual breast tenderness, but there
were no differences in negative mood symptoms.
When controlling for the severity of menstrual pain,
women using oral contraceptives showed significantly less improvement in negative mood symptoms compared with non-users.
Women with PMDD were treated with a combination of drospirenone 3mg and ethinylestradiol
30g in a double-blind, randomised, placebo-controlled trial.[113] Drospirenone is a spironolactonelike progestogen with antiandrogenic and antimineralocorticoid activity. However, the results were disappointing, as appetite, acne and food cravings were
the only measures to reach statistically significant
improvement. The primary outcome measure was
daily symptom scores as assessed on the Calendar of
Premenstrual Experiences scale.
Given the lack of benefits discussed in this section, it seems that oral contraceptives should not be
used as a treatment specifically for PMS, particularly not for the treatment of mood-associated symptoms. However, it is important to address the issue
of whether certain oral contraceptives aggravate
PMS symptoms to a lesser extent than others (see
the following section).
either only in the premenstrual phase (pure PMS)
or during the entire cycle with premenstrual aggravation were recruited.[110] Three oral contraceptives were used: monophasic ethinylestradiol/
desogestrel, a monophasic combined oral contraceptive containing levonorgestrel and a triphasic
combined oral contraceptive containing levonorgestrel. Pretreatment cycles were followed for two cycles on each oral contraceptive. All oral contraceptives had a beneficial effect on PMS symptoms
compared with the pretreatment period. Cyclical
symptom changes were noted during all oral contraceptive treatments with a similar pattern as in ovulatory cycles of patients with PMS. Oral monophasic ethinylestradiol/desogestrel was associated with
fewer changes in mood parameters than the monophasic and triphasic levonorgestrel oral contraceptives. Physical complaints were less frequent with
the triphasic levonorgestrel preparation than with
the monophasic desogestrel preparation. The effects
of the three oral contraceptives were more consistent
in women with pure PMS compared with those who
had PMS with premenstrual aggravation.
Comparisons of Progestogens Used in
Oral Contraceptives
All progestogens seem to induce negative mood
changes. However, few comparative studies have
been reported. The influence of different progestogens in oral contraceptives on premenstrual complaints has been examined in three studies.[110,114,115]
In a retrospective questionnaire study, premenstrual depression and abdominal swelling were significantly more common in women taking oral contraceptives containing lynestrenol compared with
norgestrel.[114]
In a randomised, blinded, prospective, crossover
clinical trial, 37 women with cyclical mood changes
Adis Data Information BV 2003. All rights reserved.
The incidence of premenstrual symptoms were
investigated in a study comparing two oral contraceptives, one containing 30g ethinylestradiol and
3mg drospirenone and the other containing 30g
ethinylestradiol combined with 150g desogestrel.[115] Before the onset of treatment, the incidence
of premenstrual symptoms was higher in the
ethinylestradiol/drospirenone group than in the
ethinylestradiol/desogestrel group. During the treatment period, however, the incidence of premenstrual symptoms was lower with ethinylestradiol/drospirenone compared with ethinylestradiol/desogestrel.
Different Oral Contraceptive Dosages and
Treatment Regimens
In a population-based study, Cullberg[37] showed
that women with a history of PMS experienced the
most adverse effects with oral contraceptive preparations containing the lowest dosage of norgestrel
(60 g/day) compared with placebo. However, with
the highest dosage (1.0 and 0.5 mg/day), there were
CNS Drugs 2003; 17 (5)
336
no differences in negative mood when compared
with placebo.
Bancroft et al.[116] showed that negative mood
symptoms were greater in women receiving triphasic oral contraceptives containing levonorgestrel than
those receiving monophasic oral contraceptives containing levonorgestrel. In another study, patterns of
menstrual cycle-related changes were compared between three different contraceptive groups: monophasic low-dose oral contraceptives (n = 35), triphasic oral contraceptives (n = 30) and a control
group receiving nonsteroidal contraception (n =
57).[109] The women in each group were matched for
age, occupation and parity. Each woman recorded
daily ratings of mood, physical signs and sexual
interest for two or three cycles. Cyclicity was evident in all variables assessed for all groups. Breast
tenderness was less severe in patients in the monophasic group compared with patients in both the
triphasic and non-oral contraceptive groups. No other differences between the groups were evident.
Changes in mood symptoms have been reported
with other types of hormonal contraceptives (e.g.
implantable and intrauterine systems).[117,118] For example, in a study assessing the effect of a levonorgestrel-releasing intrauterine system in the management of menorrhagia, it was reported that 56% of
patients noticed considerable improvement or cure
of their PMS symptoms.[117] In contrast, Wagner and
Berenson[118] described two women, aged 18 and 29
years, who developed both major depression and
panic disorder while using levonorgestrel implants.
These women, who had no prior psychiatric history,
developed major depression and panic disorder 12
months after insertion of levonorgestrel capsule implants. The symptoms worsened over the course of a
year. Following the removal of the implants, symptoms of depression and anxiety resolved within 1
month. Despite such results, these studies reporting
mood changes with intrauterine and implant contraceptives were designed for reasons other than investigating mood changes, and therefore the validity of
these reports is questionable.
Adis Data Information BV 2003. All rights reserved.
Backstrom et al.
4.3 Spironolactone
Spironolactone is an aldosterone receptor antagonist used as a diuretic and antihypertensive. Perhaps less well known is that spironolactone is also
an androgen antagonist, can antagonise progesterone-induced anaesthesia and has been shown to
antagonise the anaesthetic and sedative effects of
pentobarbital and neurosteroid anaesthetics.[119]
This effect of resistance to neurosteroid anaesthesia
is not related to its antimineralocorticoid activity
and is independent of the other known pharmacological actions of spironolactone. The exact mechanism
is not known.[120]
In a placebo-controlled, double-blind study, the
treatment effect of spironolactone seemed to be
greater on physical symptoms, but mood symptoms
also improved with active treatment compared with
placebo.[121] Women with pure PMS and who met
the DSM-IV criteria for PMDD were found to respond better to spironolactone than women with
premenstrual aggravation of PMS symptoms that
were present during the entire cycle. In women with
pure PMS, significantly greater improvements were
evident in symptoms of irritability, fatigue, wellbeing and energy levels, compared with somatic
symptoms.
In an open-label trial, OBrien et al.[122] found
that more than 80% of patients with PMS reported
experiencing a relief in PMS symptoms. Hendler[123]
also reported success with spironolactone in the
treatment of PMS in an uncontrolled trial. Recently,
Hellberg et al.[124] reported that spironolactone was
significantly better than placebo in relieving mood
symptoms. In contrast, Vellacott et al.[125] reported
that mood symptoms were not significantly improved with spirolactone compared with placebo. In
this double-blind study, spirolactone was significantly superior to placebo only in the treatment of
swelling and breast tenderness. Moreover, Burnet et
al.[126] found no significant differences in mood
symptoms in patients receiving spironolactone or
placebo, with the exception of a subgroup of patients. In this subgroup, spironolactone had a significantly beneficial effect on mood in patients who had
significantly higher androgen levels during the folCNS Drugs 2003; 17 (5)
The Role of Hormones and Hormonal Treatments in PMS
337
licular phase compared with the luteal phase of the
menstrual cycle. Some controversy thus still exists
over spironolactone as a treatment for PMS, but the
evidence from these studies suggests that spironolactone may have a role in the management of PMS
symptoms.[127]
mifepristone, however, no effect over placebo was
seen.[20,49] In one of these studies, a 6-month, randomised, double-blind, crossover design, a low dose
of mifepristone (5mg on alternate days for four
doses, beginning 3 days after the urinary luteinising
hormone surge) or placebo was given.[49] Symptoms
of PMS were similar during mifepristone and placebo treatments. In another study, 14 women with
PMS were given oral mifepristone (12.5 or 25 mg/
kg of bodyweight) on the seventh day after the surge
of luteinising hormone.[20] On the sixth through the
eighth day after the surge, they also received injections of either placebo or human chorionic gonadotropin (2000IU). Seven additional women with PMS
received only placebo during the study. The degree
and pattern of symptom severity were similar in all
treatment groups.
Given the anxiolytic actions demonstrated in laboratory animals during administration of high dosages of the progesterone metabolites allopregnanolone[137] and pregnanolone,[138] one would expect
that allopregnanolone and pregnanolone in high
dosages would have beneficial effects on PMS.
These compounds have not been assessed in clinical
trials, but oral micronised progesterone treatment
resulting in supraphysiological levels of allopregnanolone and pregnanolone has been investigated in
placebo-controlled studies.[139-142] These placebocontrolled trials have, however, produced contradictory results, with some showing that progesterone
treatment does not always alleviate overall premenstrual distress.[139] In one study, oral micronised
progesterone showed a beneficial effect over placebo,[140] whereas another study conducted by some of
the same authors was prematurely terminated because of the lack of effect from micronised progesterone.[141] Other studies have not been able to correlate concentrations of allopregnanolone with mood
symptoms.[142]
4.4 Progesterone
Ever since Katrina Daltons description of PMS
and menstrual cycle-linked symptoms, she has advocated a progesterone deficiency as the cause of
the condition.[128] If this hypothesis had been correct, treatment with progesterone would have been
logical. A number of placebo-controlled studies investigating the effect of progesterone have been
conducted. Unfortunately, the majority of these
have not produced promising results, finding only a
placebo effect.
The route of administration, vaginal or oral, is of
importance. In the vaginal treatments, progesterone
itself is the dominating steroid in the blood, and very
low concentrations of metabolites are formed. With
the oral route, the steroids pass through the liver
before they enter general circulation within the
body. In the liver, a large concentration of 3hydroxy-5/ metabolites are formed. These metabolites have benzodiazepine-like effects and might
therefore be suitable for PMS treatment.[129] The
studies with vaginal progesterone have used pessaries in dosages of 100800mg twice a day. The
studies reported here are all double-blind, randomised studies using reasonable criteria and workup for
the diagnosis of PMS. Five studies showed that
vaginal progesterone, in dosages from 100800mg
twice a day, had no beneficial effect on mood or
physical symptoms.[130-134] Two studies have shown
some beneficial effect on mood symptoms compared with placebo.[135,136]
Although the exact mechanism via which progesterone acts on PMS symptoms is not known, one
possibility is that the progesterone effect is mediated
via the classical hormonal receptor. If this were the
case, a blockage of this receptor using mifepristone,
a progesterone receptor antagonist, would have a
beneficial effect on symptoms. In two studies of
Adis Data Information BV 2003. All rights reserved.
5. Conclusion
Despite the significant understanding now held
regarding hormones and CNS function, more research into the pathogenesis behind menstrual
cycle-linked mood changes is needed. A consensus
CNS Drugs 2003; 17 (5)
338
Backstrom et al.
on how to define the condition, diagnostic criteria
and diagnostic procedure has been reached. Good
clinical trials show some treatments to be effective.
With a deeper knowledge of the pathogenesis, new
treatments, especially those that block symptomprovoking factors, will appear.
Sound diagnostic procedures are compulsory prior to the administration of treatment. A significant
number of women at a fertile age are severely burdened by menstrual cycle-linked symptoms. Ovulation is needed for the symptoms to develop. Progestogens given alone or in combination with estrogen
can induce symptoms similar to those seen in PMS
and are therefore suspected as symptom-provoking
factors. The response systems within the brain that
are known to be involved include serotonin and
GABA. Certain progesterone metabolites, such as
allopregnanolone, are allosteric agonists to the
GABAA receptor with a similar action as benzodiazepines, barbiturates and alcohol. Patients with
PMS have a decreased sensitivity to GABAA receptor active substances compared with control individuals. These substances, including allopregnanolone,
at low dosages are known to induce adverse mood
effects in some humans and animals. Well designed
clinical trials show that SSRI preparations have positive effects on PMS symptoms. Substances inhibiting ovulation, such as GnRH agonists, have proven
to be effective treatments. To avoid adverse effects
when high dosages of GnRH agonists are used, addback HRT is recommended. Oral contraceptives
have no treatment effect over placebo. Spironolactone has a mild effect and may be an alternative if
the patient cannot take any of the previously mentioned treatments.
Acknowledgements
This work has been supported by the Swedish Research
Council, Medicine (Proj 4X11198), EU Regional Fund, Objective 1 and Umea University research funds. The authors
have no commercial interest in the paper or other conflicts of
interest that are relevant to the content of this paper.
References
1. Sveindottir H, Backstrom T. Prevalence of menstrual cycle
symptom cyclicity and premenstrual dysphoric disorder in a
Adis Data Information BV 2003. All rights reserved.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
random sample of women using and not using oral contraceptives. Acta Obstet Gynecol Scand 2000; 79: 405-13
Halbreich U, Bancroft J, Dennerstein L, et al. Menstrually
related disorders: points of consensus, debate, and disagreement. Neuropsychopharmacology 1993; 9: 13-5
American Psychiatric Association. Diagnostic and statistical
manual of mental disorders. 4th ed. Washington, DC: American Psychiatric Association, 1994: 714-8
Hammarback S, Backstrom T, MacGibbon-Taylor B. Diagnosis
of premenstrual syndrome: description and evaluation of a
procedure for diagnosis and differential diagnosis. J Psychosom Obstet Gynaecol 1989; 10: 25-42
Andersch B, Wendestam C, Hahn L, et al. Premenstrual complaints. I: prevalence of premenstrual symptoms in a Swedish
urban population. J Psychosom Obset Gynaecol 1986; 5: 39-49
Sternfeld B, Swindle R, Chawla A, et al. Severity of premenstrual symptoms in a health maintenance organization population. Obstet Gynecol 2002; 99: 1014-24
Sveinsdottir H, Marteinsdottir G. Retrospective assessment of
premenstrual changes in Icelandic women. Health Care Women Int 1991; 12: 303-15
Sveinsdottir H, Lundman B, Norberg A. Womens perceptions
of phenomena they label premenstrual tension: normal experiences reflecting ordinary behaviour. J Adv Nurs 1999; 30:
916-25
Marvan ML, Cortes-Iniestra S. Womens beliefs about the prevalence of premenstrual syndrome and biases in recall of
premenstrual changes. Health Psychol 2001; 20: 276-80
Johnson SR, McChesney C, Bean JA. Epidemiology of premenstrual symptoms in a nonclinical sample. I: prevalence, natural
history and help-seeking behavior. J Reprod Med 1988; 33:
340-6
Ramcharan S, Love EJ, Fick GH, et al. The epidemiology of
premenstrual symptoms in a population-based sample of 2650
urban women: attributable risk and risk factors. J Clin
Epidemiol 1992; 45: 377-92
Angst J, Sellaro R, Merikangas KR, et al. The epidemiology of
perimenstrual psychological symptoms. Acta Psychiatr Scand
2001; 104: 110-6
Rivera-Tovar AD, Frank E. Late luteal phase dysphoric disorder
in young women. Am J Psychiatry 1990; 147: 1634-3
Hardie EA. Prevalence and predictors of cyclic and noncyclic
affective change. Psychol Women Q 1997; 21: 229-314
Gehlert S, Hartlage S. A design for studying the DSM-IV
research criteria of premenstrual dysphoric disorder. J Psychosom Obstet Gynaecol 1997; 18: 36-44
Banerjee N, Roy KK, Takkar D. Premenstrual dysphoric disorder: a study from India. Int J Fertil Womens Med 2000; 45:
342-4
Wittchen HU, Becker E, Lieb R, et al. Prevalence, incidence
and stability of premenstrual dysphoric disorder in the community. Psychol Med 2002; 32: 119-32
Singh BB, Berman BM, Simpson RL, et al. Incidence of
premenstrual syndrome and remedy usage: a national
probability sample study. Altern Ther Health Med 1998; 4:
75-9
Backstrom T, Sanders D, Leask RM, et al. Mood, sexuality,
hormones and the menstrual cycle. II: hormone levels and their
relationship to premenstrual syndrome. Psychsom Med 1983;
45: 503-7
Schmidt PJ, Nieman LK, Grover GN, et al. Lack of effect of
induced menses on symptoms in women with premenstrual
syndrome. N Engl J Med 1991; 324: 1174-9
CNS Drugs 2003; 17 (5)
The Role of Hormones and Hormonal Treatments in PMS
339
21. Rubinow DR, Hoban MC, Grover GN, et al. Changes in plasma
hormones across the menstrual cycle in patients with menstrually related mood disorder and in control subjects. Am J Obstet
Gynecol 1988; 158: 5-11
22. Wang M, Backstrom T, Sundstrom I, et al. Neuroactive steroids
and central nervous system disorders. Int Rev Neurobiol 2001;
46: 421-59
23. Hammarback S, Ekholm UB, Backstrom T. Spontaneous anovulation causing disappearance of cyclical symptoms in women
with the premenstrual syndrome. Acta Endocrinol (Copenh)
1991; 125: 132-7
24. Hamarback S, Backstrom T. Induced anovulation as treatment
of premenstrual tension syndrome: a double-blind cross-over
study with GnRH-agonist versus placebo. Acta Obstet
Gynecol Scand 1988; 67: 159-66
25. Brown CS, Ling FW, Andersen RN, et al. Efficacy of depot
leuprolide in premenstrual syndrome: effect of symptom severity and type in a controlled trial. Obstet Gynecol 1994; 84:
779-86
26. Mezrow G, Shoupe D, Spicer D, et al. Depot leuprolide acetate
with estrogen and progestin add-back for long-term treatment
of premenstrual syndrome. Fertil Steril 1994; 62: 932-7
27. Mortola JF, Girton L, Fischer U. Successful treatment of severe
premenstrual syndrome by combined use of gonadotropinreleasing hormone agonist and estrogen/progestin. J Clin Endocrinol Metab 1991; 72: 252A-F
28. Hammarback S, Backstrom T, Holst J, et al. Cyclical mood
changes as in the premenstrual tension syndrome during sequential estrogen-progestogen postmenopausal replacement
treatment. Acta Obstet Gynecol Scand 1985; 64: 393-7
29. Magos AL, Brewster E, Sing R, et al. The effect of norethisterone in postmenopausal women on oestrogen therapy: a model
for the premenstrual syndrome. Br J Obstet Gynaecol 1986;
93: 1290-6
30. Bjorn I, Bixo M, Strandberg-Nojd K, et al. Negative mood
changes during hormone replacement therapy: a comparison
between two progestogens. Am J Obstet Gynecol 2000; 183:
1419-26
31. Schmidt PJ, Nieman LK, Danaceau MA, et al. Differential
behavioral effects of gonadal steroids in women with and in
those without premenstrual syndrome. N Engl J Med 1998;
338: 209-16
32. Hammarback S, Damber JE, Backstrom T. Relationship between symptom severity and hormone changes in women with
premenstrual syndrome. J Clin Endocrinol Metab 1989; 68:
125-30
33. Seippel L, Backstrom T. Luteal phase estradiol relates to symptom severity between patients with premenstrual syndrome. J
Clin Endocrinol Metab 1998; 83: 1988-92
34. Dhar V, Murphy BE. Double-blind randomized crossover trial
of luteal phase estrogens (Premarin) in the premenstrual syndrome (PMS). Psychoneuroendocrinology 1990; 15: 489-93
35. Klaiber EL, Broverman DM, Vogel W, et al. Relationships of
serum estradiol levels, menopausal duration and mood during
hormonal replacement therapy. Psychoneuroendocrinology
1997; 22: 549-58
36. Bjorn I, Sundsrom-Poromaa I, Bixo M, et al. Increase of estrogen dose deteriorates mood during progestin phase in sequential hormonal therapy. J Clin Endocr Metab. In press
37. Cullberg J. Mood changes and menstrual symptoms with different gestagen/estrogen combinations: a double blind comparison with placebo. Acta Psychiatr Scand Suppl 1972; 236: 1-84
38. Graham CA, Sherwin BB. The relationship between retrospective premenstrual symptom reporting and present oral contraceptive use. J Psychosom Res 1987; 31: 45-53
39. Sundstrom I, Andersson A, Nyberg S, et al. Patients with
premenstrual syndrome have a different sensitivity to a
neuroactive steroid during the menstrual cycle compared to
control subjects. Neuroendocrinology 1998; 67: 126-38
40. Sundstrom I, Ashbrook D, Backstrom T. Reduced benzodiazepine sensitivity in patients with premenstrual syndrome: a pilot study. Psychoneuroendocrinology 1997; 22:
25-38
41. Sundstrom I, Nyberg S, Backstrom T. Patients with premenstrual syndrome have reduced sensitivity to midazolam compared
to control subjects. Neuropsychopharmacology 1997; 17:
370-81
42. Nyberg S, Sundstrom Poromaa I, Backstrom T. Patients with
premenstrual dysphoric disorder have a decreased sensitivity
to alcohol in the luteal phase [abstract no. 187]. Nordic Federation of Societies of Obstetricians and Gynecologists (NFOG)
XXXIII Congress; 2002 Jun 1-4; Umea. Umea: Nordic Federation of Societies of Obstetricians and Gynecologists, 2002
43. Schmidt PJ, Purdy RH, Moore PH, et al. Circulating levels of
anxiolytic steroids in the luteal phase in women with premenstrual syndrome and in control subjects. J Clin Endocrinol
Metab 1994; 79: 1256-60
44. Wang MD, Seippel L, Purdy RH, et al. Relationship between
symptom severity and steroid variation in women with
premenstrual syndrome: study on serum pregnenolone,
pregnenolone sulfate, 5-pregnan-3,20-dione and 3-hydroxy-5-pregnan-20-one. J Clin Endocrinol Metab 1996; 81:
1076-82
45. Sundstrom I, Backstrom T. Patients with premenstrual syndrome have decreased saccadic eye velocity compared to
control subjects. Biol Psychiatry 1998; 44: 755-64
46. Rapkin AJ, Morgan M, Goldman L, et al. Progesterone metabolite allopregnanolone in women with premenstrual syndrome.
Obstet Gynecol 1997; 90: 709-14
47. Monteleone P, Luisi S, Tonetti A, et al. Allopregnanolone
concentrations and premenstrual syndrome. Eur J Endocrinol
2000; 142: 269-73
48. McEwen BS, Coirini H, Schumacher M. Steroid effects on
neuronal activity: when is the genome involved? Ciba Found
Symp 1990; 153: 3-12
49. Chan AF, Mortola JF, Wood SH, et al. Persistence of premenstrual syndrome during low-dose administration of the progesterone antagonist RU 486. Obstet Gynecol 1994; 84: 1001-5
50. Kouri EM, Halbreich U. State and trait serotonergic abnormalities in women with dysphoric premenstrual syndromes.
Psychopharmacol Bull 1997; 33: 767-70
51. Menkes DB, Coates DC, Fawcett JP. Acute tryptophan depletion aggravates premenstrual syndrome. J Affect Disord 1994;
32: 37-44
52. Bixo M, Allard P, Backstrom T, et al. Binding of [3H]paroxetine to serotonin uptake sites and of [3H]lysergic acid diethylamide to 5-HT2A receptors in platelets from women with
premenstrual dysphoric disorder during gonadotropin releasing hormone treatment. Psychoneuroendocrinology 2001; 26:
551-64
53. Sundstrom Poromaa I, Wihlback A-C, Bixo M, et al. Influence
of menstrual cycle on platelet serotonin uptake site and
5-HT2A receptor binding [abstract no. 32]. Nordic Federation
of Societies of Obstetricians and Gynecologists (NFOG) XXXIII Congress; 2002 Jun 1-4; Umea. Umea: Nordic Federation
of Societies of Obstetricians and Gynecologists, 2002
Adis Data Information BV 2003. All rights reserved.
CNS Drugs 2003; 17 (5)
340
54. Sibille E, Pavlides C, Benke D, et al. Genetic inactivation of the
serotonin1a receptor in mice results in downregulation of
major GABAA receptor a subunits, reduction of GABAA
receptor binding, and benzodiazepine-resistant anxiety. J
Neurosci 2000; 20: 2758-65
55. Sundstrom I, Backstrom T. Citalopram increases pregnanolone
sensitivity in patients with premenstrual syndrome: an open
trial. Psychoneuroendocrinology 1998; 23: 73-88
56. Paul SM, Purdy RH. Neuroactive steroids. FASEB J 1992; 6:
2311-22
57. Backstrom T, Gee KW, Lan N, et al. Steroids in relation to
epilepsy and anaesthesia. Ciba Found Symp 1990; 153: 225-30
58. Beauchamp MH, Ormerod BK, Jhamandas K, et al. Neurosteroids and reward: allopregnanolone produces a conditioned
place aversion in rats. Pharmacol Biochem Behav 2000; 67:
29-35
59. Fish EW, Faccidomo S, DeBold JF, et al. Alcohol, allopregnanolone and aggression in mice. Psychopharmacology (Berl)
2001; 153: 473-83
60. Lee GP, Loring DW, Meador KJ, et al. Severe behavioral
complications following intracarotid sodium amobarbital injection: implications for hemispheric asymmetry of emotion.
Neurology 1988; 38: 1233-6
61. Kurthen M, Linke DB, Reuter BM, et al. Severe negative
emotional reactions in intracarotid sodium amytal procedures:
further evidence for hemispheric asymmetries? Cortex 1991;
27: 333-7
62. Masia SL, Perrine K, Westbrook L, et al. Emotional outbursts
and post-traumatic stress disorder during intracarotid
amobarbital procedure. Neurology 2000; 54: 1691-3
63. Miczek KA, ODonnell JM. Alcohol and chlordiazepoxide increase suppressed aggression in mice. Psychopharmacology
1980; 69: 39-44
64. Miczek KA, Weerts EM, DeBold JF. Alcohol, benzodiazepineGABAA receptor complex and aggression: ethological analysis of individual differences in rodents and primates. J Stud
Alcohol Suppl 1993; 11: 170179
65. Yoshimura H, Ogawa N. Acute and chronic effects of psychotropic drugs on maternal aggression in mice. Psychopharmacology 1989; 97: 339-42
66. Ferrari PF, Parmigiani S, Rodgers RJ, et al. Differential effects
of chlordiazepoxide on aggressive behavior in male mice: the
influence of social factors. Psychopharmacology (Berl) 1997;
134: 258-65
67. Miczek KA, DeBold JF, van Erp AM, et al. Alcohol, GABAAbenzodiazepine receptor complex, and aggression. Recent Dev
Alcohol 1997; 13: 139-71
68. Bjorn I, Bixo M, Nojd K, et al. The impact of different doses of
medroxyprogesterone acetate on mood symptoms in sequential
hormonal therapy. Gynecol Endocrinol 2002; 16: 1-8
69. Andreen L, Bixo M, Nyberg S, et al. Progesterone effects during
sequential hormone replacement therapy. Eur J Endocrinology. In press
70. Gulinello M, Gong QH, Li X, et al. Short-term exposure to a
neuroactive steroid increases alpha4 GABA(A) receptor
subunit levels in association with increased anxiety in the
female rat. Brain Res 2001; 910: 55-66
71. Birzniece V, Zhu D, Lindblad C, et al. Acute allopregnanolone
tolerance [abstract no. 186]. Nordic Federation of Societies of
Obstetricians and Gynecologists (NFOG) XXXIII Congress;
2002 Jun 1-4; Umea. Umea: Nordic Federation of Societies of
Obstetricians and Gynecologists, 2002
Adis Data Information BV 2003. All rights reserved.
Backstrom et al.
72. Backstrom T, Baird DT, Bancroft J, et al. Endocrinological
aspects of cyclical mood changes during the menstrual cycle or
the premenstrual syndrome. J Psychosom Obstet Gynaecol
1983; 2: 8-20
73. Banerjee PK, Snead III OC. Neuroactive steroids exacerbate
gamma-hydroxybutyric acid-induced absence seizures in rats.
Eur J Pharmacol 1998; 359: 41-8
74. Grunewald RA, Aliberti V, Panayiotopoulos CP. Exacerbation
of typical absence seizures by progesterone. Seizure 1992; 1:
137-8
75. Dimmock PW, Wyatt KM, Jones PW, et al. Efficacy of selective serotonin-reuptake inhibitors in premenstrual syndrome: a
systematic review. Lancet 2000; 356: 1131-6
76. Eriksson E, Hedberg MA, Andersch B, et al. The serotonin
reuptake inhibitor paroxetine is superior to the noradrenaline
reuptake inhibitor maprotiline in the treatment of premenstrual
syndrome. Neuropsychopharmacology 1995; 12: 167-76
77. Steiner M, Steinberg S, Stewart S, et al. Fluoxetine in the
treatment of premenstrual dysphoria. N Engl J Med 1995; 332:
1529-34
78. Sundblad C, Hedberg MA, Eriksson E. Clomipramine administered during the luteal phase reduces the symptoms of premenstrual syndrome: a placebo-controlled trial. Neuropsychopharmacology 1993; 9: 133-45
79. Pearlstein TB, Stone AB. Long-term fluoxetine treatment of late
luteal phase dysphoric disorder. J Clin Psychiatry 1994; 55:
332-5
80. Sundstrom-Poromaa I, Bixo M, Bjorn I, et al. Compliance to
antidepressant drug therapy for treatment of premenstrual syndrome. Psychosom Obstet Gynecol 2000; 21: 205-11
81. Magos AL, Brincat M, Studd JW. Treatment of the premenstrual syndrome by subcutaneous estradiol implants and cyclical
oral norethisterone: placebo controlled study. BMJ 1986; 292:
1629-33
82. Hahn PM, Van Vugt DA, Reid RL. A randomized, placebocontrolled, crossover trial of danazol for the treatment of
premenstrual syndrome. Psychoneuroendocrinology 1995; 20:
193-209
83. Backstrom CT, Boyle H, Baird DT. Persistence of symptoms of
premenstrual tension in hysterectomized women. Br J Obstet
Gynaecol 1981; 88: 530-6
84. Muse KN, Cetel NS, Futterman LA, et al. The premenstrual
syndrome: effects of "medical ovariectomy". N Engl J Med
1984; 311: 1345-9
85. Bancroft J, Boyle H, Warner P, et al. The use of an LHRH
agonist, buserelin, in the long-term management of premenstrual syndromes. Clin Endocrinol (Oxf) 1987; 27: 171-82
86. Hussain SY, Massil JH, Matta WH, et al. Buserelin in premenstrual syndrome. Gynecol Endocrinol 1992; 6: 57-64
87. Freeman EW, Sondheimer SJ, Rickels K, et al. Gonadotropinreleasing hormone agonist in treatment of premenstrual symptoms with and without comorbidity of depression: a pilot
study. J Clin Psychiatry 1993; 54: 192-5
88. West CP, Hillier H. Ovarian suppression with the gonadotrophin-releasing hormone agonist goserelin (Zoladex) in management of the premenstrual tension syndrome. Hum Reprod
1994; 9: 1058-63
89. Freeman EW, Sondheimer SJ, Rickels K. Gonadotropin-releasing hormone agonist in the treatment of premenstrual symptoms with and without ongoing dysphoria: a controlled study.
Psychopharmacol Bull 1997; 33: 303-9
90. Leather AT, Stud JW, Watson NR, et al. The treatment of
severe premenstrual syndrome with goserelin with and without
CNS Drugs 2003; 17 (5)
The Role of Hormones and Hormonal Treatments in PMS
341
"add-back" estrogen therapy: a placebo-controlled study.
Gynecol Endocrinol 1999; 13: 48-55
Di Carlo C, Palomba S, Tommaselli GA, et al. Use of leuprolide
acetate plus tibolone in the treatment of severe premenstrual
syndrome. Fertil Steril 2001; 75: 380-4
Helvacioglu A, Yeoman RR, Hazelton JM, et al. Premenstrual
syndrome and related hormonal changes: long-acting gonadotropin releasing hormone agonist treatment. J Reprod Med
1993; 38: 864-70
Studd J, Leather AT. The need for add-back with a gonadotropin-releasing hormone agonist therapy. Br J Obstet
Gynaecol 1996; 103: 1-4
Sundstrom I, Nyberg S, Bixo M, et al. Treatment of premenstrual syndrome with gonadotropin-releasing hormone agonist in a
low dose regimen. Acta Obstet Gynecol Scand 1999; 78: 891-9
Magos AL, Collins WP, Studd JW. Management of the premenstrual syndrome by subcutaneous implants of oestradiol. J
Psychosom Obstet Gynaecol 1984; 3: 93-9
Watson NR, Studd JW, Savvas M, et al. Treatment of severe
premenstrual syndrome with oestradiol patches and cyclical
oral norethisterone. Lancet 1989; II: 730-2
Smith RN, Studd JW, Zamblera D, et al. A randomised comparison over 8 months of 100 micrograms and 200 micrograms
twice weekly doses of transdermal oestradiol in the treatment
of severe premenstrual syndrome. Br J Obstet Gynaecol 1995;
102: 475-84
Watson NR, Studd JW, Savvas M, et al. The long-term effects
of estradiol implant therapy for the treatment of premenstrual
syndrome. Gynecol Endocrinol 1990; 4: 99-107
West CP. Inhibition of ovulation with oral progestins: effectiveness in premenstrual syndrome. Eur J Obstet Gynecol Reprod
Biol 1990; 34: 119-28
Gilmore DH, Hawthorn RJ, Hart DM. Danol for premenstrual
syndrome: a preliminary report of a placebo-controlled double-blind study. J Int Med Res 1985; 13: 129-30
Watts JF, Edwards RL, Butt WR. Treatment of premenstrual
syndrome using danazol: preliminary report of a placebocontrolled, double-blind, dose ranging study. J Int Med Res
1985; 13: 127-8
Deeny M, Hawthorn R, McKay Hart D. Low dose danazol in the
treatment of the premenstrual syndrome. Postgrad Med J 1991;
67: 450-4
Halbreich U, Rojansky N, Palter S. Elimination of ovulation and
menstrual cyclicity (with danazol) improves dysphoric
premenstrual syndromes. Fertil Steril 1991; 56: 1066-9
OBrien PM, Abukhalil IE. Randomized controlled trial of the
management of premenstrual syndrome and premenstrual mastalgia using luteal phase-only danazol. Am J Obstet Gynecol
1999; 180: 18-23
Casson P, Hahn PM, Van Vugt DA, et al. Lasting response to
ovariectomy in severe intractable premenstrual syndrome. Am
J Obstet Gynecol 1990; 162: 99-105
Casper RF, Hearn MT. The effect of hysterectomy and bilateral
oophorectomy in women with severe premenstrual syndrome.
Am J Obstet Gynecol 1990; 162: 105-9
Milsom I, Sundell G, Andersch B. A longitudinal study of
contraception and pregnancy outcome in a representative sample of young Swedish women. Contraception 1991; 43: 111-9
Sanders SA, Graham CA, Bass JL, et al. A prospective study of
the effects of oral contraceptives on sexuality and well-being
and their relationship to discontinuation. Contraception 2001;
64: 51-8
109. Walker A, Bancroft J. Relationship between premenstrual
symptoms and oral contraceptive use: a controlled study. Psychosom Med 1990; 52: 86-96
Cavalli-Bjorkman B, et al. Effects of
110. Backstrom T, Lindhe BA,
oral contraceptives on mood: a randomized comparison of
three phasic and monophasic preparations. Contraception
1992; 46: 253-68
111. Graham CA, Sherwin BB. A prospective treatment study of
premenstrual symptoms using a triphasic oral contraceptive. J
Psychosom Res 1992; 36: 257-66
112. Bancroft J, Rennie D. The impact of oral contraceptives on the
experience of perimenstrual mood, clumsiness, food craving
and other symptoms. J Psychosom Res 1993; 37: 195-202
113. Freeman EW, Kroll R, Rapkin A, et al. Evaluation of a unique
oral contraceptive in the treatment of premenstrual dysphoric
disorder. J Womens Health Gend Based Med 2001; 10: 561-9
114. Andersch B. The effect of various oral contraceptive combinations on premenstrual symptoms. Int J Gynaecol Obstet 1982;
20: 463-9
115. Foidart JM, Wuttke W, Bouw GM, et al. A comparative
investigation of contraceptive reliability, cycle control and
tolerance of two monophasic oral contraceptives containing
either drospirenone or desogestrel. Eur J Contracept Reprod
Health Care 2000; 5: 124-34
116. Bancroft J, Sanders D, Warner P, et al. The effects of oral
contraceptives on mood and sexuality: comparison of triphasic
and combined preparations. J Psychosom Obstet and Gynaecol
1987; 7: 1-8
117. Barrington JW, Bowen Simpkins P. The levonorgestrel intrauterine system in the management of menorrhagia. Br J
Obstet Gynaecol 1997; 104: 614-6
118. Wagner KD, Berenson AB. Norplant-associated major depression and panic disorder. J Clin Psychiatry 1994; 55: 478-80
119. Selye H, Mecs I, Savoie L. Inhibition of anesthetics and sedative
actions by spironolactone. Anesthesiology 1969; 31: 261-4
120. Selye H. Spironolactone actions, independent of mineralocorticoid blockade. Steroids 1969; 13: 803-8
121. Wang M, Hamarback S, Lindhe BA, et al. Treatment of
premenstrual syndrome by spironolactone: a double-blind, placebo-controlled study. Acta Obstet Gynecol Scand 1995; 74:
803-8
122. OBrien PMS, Craven D, Selby C, et al. Treatment of premenstrual syndrome by spironolactone. Br J Obstet Gynecol 1979;
86: 142-7
123. Hendler NH. Spironolactone for premenstrual syndrome. Female Patient 1980; 5: 17-20
124. Hellberg D, Claesson B, Nilsson S. Premenstrual tension: a
placebo-controlled efficacy study with spironolactone and
medroxyprogesterone acetate. Int J Gynaecol Obstet 1991; 34:
243-8
125. Vellacott ID, Shroff NE, Pearce MY, et al. A double-blind,
placebo-controlled evaluation of spironolactone in the premenstrual syndrome. Curr Med Res Opin 1987; 10: 450-6
126. Burnet RB, Radden HS, Easterbrook EG, et al. Premenstrual
syndrome and spironolactone. Aust N Z J Obstet Gynaecol
1991; 31: 366-8
127. Vellacott I. D, OBrien PM. Effect of spironolactone on
premenstrual syndrome symptoms. J Reprod Med 1987; 32:
429-34
128. Dalton K. The premenstrual syndrome and progesterone therapy. London: William Heineman, 1984
91.
92.
93.
94.
95.
96.
97.
98.
99.
100.
101.
102.
103.
104.
105.
106.
107.
108.
Adis Data Information BV 2003. All rights reserved.
CNS Drugs 2003; 17 (5)
342
129. De Lignieres B, Dennerstein L, Backstrom T. Influence of route
of administration on progesterone metabolism. Maturitas
1995; 21: 251-7
130. Maddocks S, Hahn P, Moller F, et al. A double-blind placebocontrolled trial of progesterone vaginal suppositories in the
treatment of premenstrual syndrome. Am J Obstet Gynecol
1986; 154: 573-81
131. Andersch B, Hahn L. Progesterone treatment of premenstrual
tension: a double blind study. J Psychosom Res 1985; 29:
489-93
132. Freeman E, Rickels K, Sondheimer SJ, et al. Ineffectiveness of
progesterone suppository treatment for premenstrual syndrome. JAMA 1990; 264: 349-53
133. Sampson GA. Premenstrual syndrome: a double-blind controlled trial of progesterone and placebo. Br J Psychiatry 1979;
135: 209-15
134. Magos A, Studd J. Progesterone and the premenstrual syndrome: a double blind crossover trial. BMJ (Clin Res Ed)
1985; 291: 213-4
135. Magill PJ. Investigation of the efficacy of progesterone pessaries in the relief of symptoms of premenstrual syndrome:
Progesterone Study Group. Br J Gen Pract 1995; 45: 589-93
136. Baker ER, Best RG, Manfredi RL, et al. Efficacy of progesterone vaginal suppositories in alleviation of nervous symptoms
in patients with premenstrual syndrome. J Assist Reprod Genet
1995; 12: 205-9
137. Bitran D, Hilvers RJ, Kellogg CK. Anxiolytic effects of 3 alphahydroxy-5 alpha[beta]-pregnan-20-one: endogenous metabo-
Adis Data Information BV 2003. All rights reserved.
Backstrom et al.
lites of progesterone that are active at the GABAA receptor.
Brain Res 1991; 561: 157-61
138. Wieland S, Lan NC, Mirasedeghi S, et al. Anxiolytic activity of
the progesterone metabolite 5 alpha-pregnan-3 alphao1-20-one. Brain Res 1991; 565: 263-8
139. Freeman EW, Rickels K, Sondheimer SJ, et al. A double-blind
trial of oral progesterone, alprazolam, and placebo in treatment
of severe premenstrual syndrome. JAMA 1995; 274: 51-7
140. Dennerstein L, Spencer-Gardner L, Gotts C, et al. Progesterone
and the premenstrual syndrome: a double blind crossover trial.
BMJ 1985; 290: 1617-21
141. Vanselow W, Dennerstein L, Greenwood KM, et al. Effect of
progesterone and its 5- and 5-metabolites on symptoms of
premenstrual syndrome according to route of administration. J
Psychosom Obstet Gynaecol 1996; 17: 29-38
142. Freeman EW, Purdy RH, Coutifaris C, et al. Anxiolytic metabolites of progesterone: correlation with mood and performance
measures following oral progesterone administration to
healthy female volunteers. Neuroendocrinology 1993; 58:
478-84
Correspondence and offprints: Dr Torbjorn Backstrom, Department of Clinical Sciences, Obstetrics and Gynecology,
University Hospital, SE 901 85 Umea, Sweden.
E-mail: Torbjorn.Backstrom@obgyn.umu.se
CNS Drugs 2003; 17 (5)
Anda mungkin juga menyukai
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Neurotransmitter Cheat Sheet AP ReviewDokumen2 halamanNeurotransmitter Cheat Sheet AP ReviewNathania DawitBelum ada peringkat
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Steroids QuizDokumen3 halamanSteroids Quizfaqed ilzakiraBelum ada peringkat
- Elsharnoby Pediatric Made EasyDokumen160 halamanElsharnoby Pediatric Made Easyelmaadawy20020% (1)
- Farid Pharmacology FinalDokumen12 halamanFarid Pharmacology FinalFariedfrd0% (1)
- SCOPE OF CLINICAL PHARMACYDokumen13 halamanSCOPE OF CLINICAL PHARMACYkeerthanaBelum ada peringkat
- Useful Medications For Oral Conditions: AnalgesicsDokumen7 halamanUseful Medications For Oral Conditions: AnalgesicsAswathyBelum ada peringkat
- Following OvulationDokumen1 halamanFollowing OvulationnikuBelum ada peringkat
- Hyperalgesia in The Setting of AnxietyDokumen1 halamanHyperalgesia in The Setting of AnxietynikuBelum ada peringkat
- Curriculum Vitae: ExperienceDokumen2 halamanCurriculum Vitae: ExperiencenikuBelum ada peringkat
- Balram Jadhav CVDokumen3 halamanBalram Jadhav CVnikuBelum ada peringkat
- Synopsis EditedDokumen8 halamanSynopsis EditednikilBelum ada peringkat
- J Infect Dis. 1999 Dinarello S294 304Dokumen11 halamanJ Infect Dis. 1999 Dinarello S294 304nikuBelum ada peringkat
- PKCDokumen52 halamanPKCnikuBelum ada peringkat
- Sunita Apticon15Dokumen3 halamanSunita Apticon15nikuBelum ada peringkat
- Genome Mapping: Paul H DearDokumen7 halamanGenome Mapping: Paul H DearvidpoohBelum ada peringkat
- Scott Reuschel TANDEM LABS - Regulated Bioanlysis For The Pharmaceutical IndustryDokumen33 halamanScott Reuschel TANDEM LABS - Regulated Bioanlysis For The Pharmaceutical IndustrynikuBelum ada peringkat
- NeuropeptidesDokumen36 halamanNeuropeptidesnikuBelum ada peringkat
- Overdose Dan ToxikasiDokumen44 halamanOverdose Dan ToxikasiRandi N. FarizaBelum ada peringkat
- ELSI Working Group 1st ReportDokumen9 halamanELSI Working Group 1st ReportnikuBelum ada peringkat
- Chrono 2Dokumen5 halamanChrono 2nikuBelum ada peringkat
- Chrono 4Dokumen27 halamanChrono 4nikuBelum ada peringkat
- Chrono 3Dokumen9 halamanChrono 3nikuBelum ada peringkat
- Us 20100323011Dokumen15 halamanUs 20100323011nikuBelum ada peringkat
- CytokininDokumen7 halamanCytokininPablo AlbanBelum ada peringkat
- Pro Kinase CDokumen9 halamanPro Kinase CnikuBelum ada peringkat
- Pharmacologic Activity of Phosphodiesterases and Their InhibitorsDokumen15 halamanPharmacologic Activity of Phosphodiesterases and Their InhibitorsnikuBelum ada peringkat
- Management PoisoningDokumen6 halamanManagement PoisoningatifdocBelum ada peringkat
- Hyperalgesia in The Setting of AnxietyDokumen1 halamanHyperalgesia in The Setting of AnxietynikuBelum ada peringkat
- United States: (12) Patent Application Publication (10) Pub. No.: US 2011/0206766 A1Dokumen20 halamanUnited States: (12) Patent Application Publication (10) Pub. No.: US 2011/0206766 A1nikuBelum ada peringkat
- Teach Tox SlidesDokumen23 halamanTeach Tox SlidesnikuBelum ada peringkat
- Systemic Target Single ExposureDokumen10 halamanSystemic Target Single ExposurenikuBelum ada peringkat
- Week2PostHoc 03Dokumen22 halamanWeek2PostHoc 03nikuBelum ada peringkat
- Systemin Target Repeated ExposureDokumen11 halamanSystemin Target Repeated ExposurenikuBelum ada peringkat
- United States: (12) Patent Application Publication (10) Pub. No.: US 2013/0052239 A1Dokumen22 halamanUnited States: (12) Patent Application Publication (10) Pub. No.: US 2013/0052239 A1nikuBelum ada peringkat
- NPP 2009222 ADokumen12 halamanNPP 2009222 AnikuBelum ada peringkat
- NIH Public Access: Author ManuscriptDokumen24 halamanNIH Public Access: Author ManuscriptnikuBelum ada peringkat
- Mapeh 6: Quarter 4 - Module 1Dokumen10 halamanMapeh 6: Quarter 4 - Module 1ALEX CORPORALBelum ada peringkat
- Cefuroxime, Celecoxib, ChloridineDokumen2 halamanCefuroxime, Celecoxib, ChloridinekrizzywhizzyBelum ada peringkat
- Pha ProfilesDokumen5.178 halamanPha ProfilesSDBelum ada peringkat
- TRAMADOLDokumen4 halamanTRAMADOLRudie Lee PascualBelum ada peringkat
- GuideDokumen24 halamanGuideBenjamin TantiansuBelum ada peringkat
- Dosage CalculationsDokumen8 halamanDosage CalculationsReinna Angel CampoBelum ada peringkat
- Previous Year Board Exam Questions (2007-2016) : Chemistry in Everyday LifeDokumen6 halamanPrevious Year Board Exam Questions (2007-2016) : Chemistry in Everyday Lifehoney1002Belum ada peringkat
- Pharma 9Dokumen4 halamanPharma 9Uday kumarBelum ada peringkat
- Moderna and Spikevax COVID-19 Vaccines Fact SheetDokumen8 halamanModerna and Spikevax COVID-19 Vaccines Fact SheetRebeca CervantesBelum ada peringkat
- DilutionDokumen12 halamanDilutioncristina tina100% (1)
- Pharmacology Unit 3Dokumen8 halamanPharmacology Unit 3Anvesh SkBelum ada peringkat
- Respiratory Drugs for Cough & Asthma ReliefDokumen5 halamanRespiratory Drugs for Cough & Asthma ReliefHamad AlshabiBelum ada peringkat
- BIOAVAILABILITY AND BIOEQUIVALANCE STUDIES Final - PPTX'Dokumen32 halamanBIOAVAILABILITY AND BIOEQUIVALANCE STUDIES Final - PPTX'Md TayfuzzamanBelum ada peringkat
- Drug Study - SenkotDokumen2 halamanDrug Study - SenkotiamthueyBelum ada peringkat
- Amiodarone IV Administration 1.0Dokumen5 halamanAmiodarone IV Administration 1.0Ari BinkosimBelum ada peringkat
- Dose Response RelationshipDokumen24 halamanDose Response RelationshipPoonam RaiBelum ada peringkat
- Antiepileptic Drugs: Dr. M.T.Madhushika Lecturer Department of Pharmacology Faculty of MedicineDokumen68 halamanAntiepileptic Drugs: Dr. M.T.Madhushika Lecturer Department of Pharmacology Faculty of MedicineThilini PrasanthikaBelum ada peringkat
- Ondansetron 4Mg Tablets (Ondansetron Hydrochloride) PL 04543/0509 Ondansetron 8Mg Tablets (Ondansetron Hydrochloride) PL 04543/0510Dokumen47 halamanOndansetron 4Mg Tablets (Ondansetron Hydrochloride) PL 04543/0509 Ondansetron 8Mg Tablets (Ondansetron Hydrochloride) PL 04543/0510Santosh VarmaBelum ada peringkat
- Evaluation of Poisoning and Drug Overdose Among Cases Presented To Poison Control Centre, Ain Shams University Hospital During The Year 2015Dokumen13 halamanEvaluation of Poisoning and Drug Overdose Among Cases Presented To Poison Control Centre, Ain Shams University Hospital During The Year 2015Hany TawfikBelum ada peringkat
- Drug Study ArraDokumen5 halamanDrug Study ArraPaul ManaloBelum ada peringkat
- Case Study: Betty SueDokumen15 halamanCase Study: Betty SueamitBelum ada peringkat
- Aroosa Qamar PharmacologyDokumen17 halamanAroosa Qamar PharmacologyAdan IsrarBelum ada peringkat
- 11.BMD 308 - Adrenergic PharmacologyDokumen29 halaman11.BMD 308 - Adrenergic PharmacologyMega XtericsBelum ada peringkat
- 3 Carbamates InsecticidesDokumen13 halaman3 Carbamates InsecticidesAmit SharmaBelum ada peringkat