TON Annual Meeting Silabus
Diunggah oleh
ansyemomoleHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
TON Annual Meeting Silabus
Diunggah oleh
ansyemomoleHak Cipta:
Format Tersedia
Traumatic Optic Neuropathy
Leonard Levin, MD, PhD
University of Wisconsin Medical School
Madison, WI
LEARNING OBJECTIVES
INTRODUCTION
1. The attendee should understand the typology of
traumatic optic neuropathy.
(Some of this syllabus is taken from Levin LA. Traumatic
Optic Neuropathy. In Roy And Fraunfelders Current
Ocular Therapy, 6th edition. Eds: Roy FH, Fraunfelder F.
Saunders, Philadelphia, 2007, which in turn was adapted
from the chapter of the same name by Neil Miller in the
5th edition.)
2. The attendee should know the evidence behind the
various treatment choices for traumatic optic
neuropathy.
3. The attendee should know the basis for future
treatments in traumatic optic neurpathy.
ANTERIOR VS. POSTERIOR TRAUMATIC OPTIC
NEUROPATHY
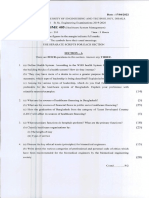
CME QUESTIONS
1. Treatment of indirect traumatic optic neuropathy with
megadose corticosteroids in a patient with significant
head injury is:
a) Recommended.
b) Not recommended because of lack of evidence.
c) Not recommended because of increased risk of
death.
2. Non-penetrating blunt head trauma with involvement
of the optic nerve canal is likely to result in which of
these fundus findings acutely?
a) Disk edema
b) Central retinal vein occlusion
c) Central retinal artery occlusion
d) Any of the above
e) None of the above
3. The absence of a canal bone fragment or sphenoid
sinus fluid essentially rules out:
a) Significant optic nerve injury
b) Any optic nerve injury
c) It does not rule out either.
KEYWORDS
Traumatic optic neuropathy is the name given to the
syndrome of an optic neuropathy after head or ocular
trauma in the absence of other causes. Like any other
optic neuropathy, there are variable degrees of visual
acuity and visual field loss, and an afferent pupillary
defect if unilateral or significantly asymmetric.
Traumatic optic neuropathy is either anterior or posterior,
and within each category, can either be direct or indirect.
Trauma to the anterior optic nerve usually injures the
central retinal artery and vein, which enter or exit the
nerve approximately 10 mm posterior to the globe.
This vascular injury often results in retinal infarct,
hemorrhages, and/or disk edema, manifestations of
central retinal or branch artery occlusion, central retinal
vein occlusion, or anterior ischemic optic neuropathy.
Trauma posterior to the entrance and exit of the central
retinal artery and vein from the optic nerve does not cause
retinal vascular changes unless those vessels are
simultaneously involved within the orbit. Axonal injury in
the posterior optic nerve does not cause any acute effects
on the disk, nerve fiber layer, or retinal ganglion cell
layers. Axonal transport abnormalities posteriorly do not
affect the more anterior nerve fibers, so disc edema is not
seen in posterior traumatic optic neuropathy. For these
reasons, isolated posterior traumatic optic neuropathy is
associated with a normal fundus examination at
presentation, and can be misdiagnosed, for example as
factitious visual loss. Only after a few weeks are the
structural signs of optic neuropathy evident, namely disk
pallor and thinning of the retinal nerve fiber layer.
1. Trauma
2. Optic neuropathy
3. Corticosteroids
4. Optic canal decompression
5. Neuroprotection
A particular type of posterior traumatic optic neuropathy
is when there is injury to the chiasm, in which case there
may be unilateral or bilateral temporal visual field defects
respecting the vertical meridian. Chiasmal injury can be
seen with posterior avulsion of the optic nerve, e.g.
traumatic enucleation, or penetration from a foreign body.
2009 Annual Meeting Syllabus | 75
DIRECT TRAUMATIC OPTIC NEUROPATHY
Direct traumatic optic neuropathy is defined when there is
penetration of the optic nerve by a foreign body or
projectile. Anterior direct optic nerve injuries result from
penetrating ocular or orbital trauma that damages the
anterior optic nerve, e.g. a knife transecting the optic
nerve just posterior to the globe. Posterior direct optic
nerve injuries result from penetrating orbital or head
trauma more posteriorly, e.g. a bullet that passes just
anterior to the chiasm.
Direct injuries tend to produce severe and immediate
visual loss, with little likelihood of recovery. The reason
for this presumably is that a major element in these
injuries is transection injury to retinal ganglion cell axons,
which causes instantaneous loss of axonal conduction and
an inability to regenerate axons later.
healing of the edema or other molecular events blocking
conduction, axonal function can return.
The severity of initial visual loss in patients with traumatic
optic neuropathy varies from no light perception to better
than 20/20, with sometimes only a visual field defect as
functional evidence of disease. Patients with very poor
vision (e.g. light perception only or no light perception)
are less likely to improve, regardless of therapy, than are
patients with vision better than light perception. The
reason is likely that severe injury causes either axonal
transection, membrane disruption, or cytoskeletal
disorganization, any of which can lead to axonal
dissolution and irreversible loss of conduction of visual
information.
In some cases the visual loss only begins several hours to
days after the injury. If this happens, the possibility of an
intrasheath hemorrhage should be entertained, and
neuroimaging repeated.
INDIRECT TRAUMATIC OPTIC NEUROPATHY
Indirect traumatic optic neuropathy is diagnosed when
there is traumatic optic neuropathy but no foreign body.
Indirect injuries are caused by forces transmitted at a
distance from the optic nerve, e.g. blunt head trauma
without penetration. The least common are anterior
indirect injuries, which often usually associated with
sudden rotation of the globe from blunt trauma. Examples
include a digit to the globe or falling and hitting the eye
on the corner of a table. Anterior indirect traumatic optic
neuropathy can cause partial or total avulsion of the optic
nerve, with associated hemorrhage and occlusion of the
central retinal artery and vein.
Posterior indirect injury is the most common cause of
traumatic optic neuropathy. Posterior indirect traumatic
optic neuropathy results from blunt head trauma that
transmits a concussive force to the optic nerve, resulting
in contusion or sometimes transection. There may be little
or no evidence of significant head trauma; a fall from a
bicycle may suffice. In other cases there is multisystem
trauma or significant brain injury. Loss of consciousness
occurs in 40% to 72% of patients with traumatic optic
neuropathy. Motor vehicle and bicycle accidents are the
most frequent causes of traumatic optic neuropathy,
accounting for 17% to 63% of cases. Traumatic optic
neuropathy may be iatrogenic, especially after
maxillofacial or endoscopic surgery as a result of
inadvertent direct injury to the optic nerve or transmitted
force fracturing the optic canal.
The most common site of posterior indirect optic nerve
injury is the optic canal; the intracranial optic nerve is the
next most common site of injury. There may or may not
be bone fractures. Despite being most common, posterior
indirect traumatic optic neuropathies fortunately
occasionally have the most favorable prognosis, with
spontaneous visual recovery sometimes occurring at
variable times after injury. Presumably, the injury causes
concussion and focal blockade of axonal conduction
without loss of its structural integrity. Once there is
76 | North American Neuro-Ophthalmology Society
NEUROIMAGING
Neuroimaging is important in the evaluation of a patient
with traumatic optic neuropathy not only for
demonstrating correlative signs of injury, but also
detection of pre-existing structural lesions and coincident
intracranial effects of trauma, e.g. hematomas or carotidcavernous fistulas. CT scanning is superior to magnetic
resonance imaging (MRI) in delineating fractures of bone.
It is critical that CT be performed with very thin sections,
and reconstructions performed, particularly in the coronal
plane. From 20% to 50% of patients with posterior
traumatic optic neuropathy have evidence of an optic
canal fracture by neuroimaging, and sometimes the clue is
a small loss of contour of bone. Although the
displacement on neuroimaging may be small, it is possible
that at the time of injury, there was a much larger
displacement of the bone into the canal. Even in the
absence of a fracture, blood in the sphenoid sinus should
raise suspicion for optic nerve injury.
MRI is better for imaging soft tissue, particularly the
intracranial optic nerve and chiasm, and may be useful for
delineating intrasheath hemorrhage or optic nerve
transection within intact meninges. It is critical that MRI
only be performed after a metallic intracranial,
intraorbital, or intraocular foreign body has been ruled out
by CT scanning or conventional radiography. If CT is used
for screening, care should be taken to use thin slices and
no interslice skip.
TREATMENT OF TRAUMATIC OPTIC NEUROPATHY
Anterior and Direct Traumatic Optic Neuropathy
There is no evidence that treatment of anterior optic
injuries or direct optic nerve injuries is efficacious. In the
former, the concurrent vascular injuries cause direct
ischemia and infarction to the neural retina and/or optic
nerve head, and the time until irreversible neuronal death
is measured in minutes to hours. In the latter, there is
often sufficient direct axonal trauma to disrupt the
integrity of the axon, up to and including its transection,
and in the central nervous system of mammals, this is a
point of no return for neuronal function.
An exception is anterior traumatic optic neuropathy
associated with neuroimaging evidence of an enlarged
optic nerve sheath. In these cases, an optic nerve sheath
fenestration should be performed in the hopes of
evacuating an intrasheath hematoma.1
Posterior Indirect Traumatic Optic Neuropathy
With respect to posterior indirect traumatic optic
neuropathy, the three commonly used approaches that
have been used are very high doses (megadoses) of
corticosteroids, decompression of the optic canal, and
observation alone.
Unfortunately, there is insufficient evidence from good
quality randomized trials to guide decision-making on
how to treat traumatic optic neuropathy. Because visual
function often spontaneously improves in this disease,
clinical trials are particularly necessary for physicians to
select therapies based on evidence. Some of the critical
issues are discussed below.
Megadose Corticosteroids
Experimental models of white matter trauma in animals
showed that doses of fifteen to thirty milligrams per
kilogram of intravenous methylprednisolone is protective
for injured neurons2. The NASCIS 2 and 3 studies found
that patients treated within 8 hours of spinal cord injury
with a loading dose of 30 milligrams per kilogram of
intravenous methylprednisolone load followed by 5.4
ml/kg/hr continuous infusion for 48 hours had a better
outcome than control patients3, 4. Extrapolating these
results to traumatic optic nerve injury, it was thought
reasonable to believe that similar doses should be used
for injury to this comparable central nervous system white
matter structure. However, over the years there has been
controversy about interpretation of the NASCIS data5, 6,
and its application to the treatment of spinal cord injury is
not uniform7, 8. Furthermore, animal and cell culture data
suggest that high doses of methylprednisolone may
actually be toxic for the retinal ganglion cell and/or its
axon9-11. Finally, the Corticosteroid Randomisation After
Significant Head Injury (CRASH) trial demonstrated that
48 hours of megadose methylprednisolone significant
increased the risk of death after head injury12, with a
hazard ratio at 6 months of 1.15 (95% CI 1.071.24)13.
The authors concluded:
these final results still provide clear evidence that
treatment with corticosteroids following head injury
affords no material benefit. The absence of evidence of
any neurological benefit from corticosteroid treatment
after head injury might also have implications for the
use of corticosteroids in spinal cord injury, which
should remain an area for debate.13
Not surprisingly, a recent Cochrane review on
corticosteroids in traumatic optic neuropathy concluded
that there was no insufficient evidence to support their
use, particularly more than 8 hours after injury.14
Optic Canal Decompression
Decompression of the optic canal is usually achieved
through the transethmoidal route, most commonly via an
external ethmoidectomy or endonasally.15,16 The canal is
then decompressed inferomedially from the superior
lateral wall of the sphenoid sinus, with care taken to avoid
the carotid artery. Although the canal can also be
decompressed through an intracranial approach, the
former is less invasive. However, if surgery in the area is
being performed for other reasons necessitating
unroofing of the canal, then an argument can be made
that decompression of the canal should be done through
this approach.
However, there is also no evidence that optic canal
decompression is efficacious. A recent Cochrane review
concluded that:
There is no conclusive evidence that any particular
form of surgical decompression improves the visual
outcome in TON. The decision to proceed with surgery
in TON remains controversial and each case needs to
be assessed on its own merits. The final decision will
inevitably reflect a combination of clinical judgement,
the availability of local surgical expertise and the
patients perception of the possible risks and
benefits.17
If surgery is to be considered, it should only be performed
in centers with experience with the procedure. Because of
the possibility that the carotid may be iatrogenically
injured, there should be informed consent regarding the
risk of death or stroke. Surgery should not be performed
on an unconscious patient because of the difficulty in
assessing visual function. A possible exception is when
the pupil in the affected eye is amaurotic, i.e. nonreactive
to light but reactive to light in the contralateral eye. The
presence of a relative afferent pupillary defect indicates
only that an optic neuropathy is present; it does not
indicate the severity. A patient with a relative afferent
pupillary defect may have 20/20 visual acuity.
Observation
Traumatic optic neuropathy may improve without any
treatment18. There are no convincing randomized control
trials to show a treatment benefit in traumatic optic
neuropathy, and a nonrandomized concurrent
comparative study did not demonstrate clear differences
between treatments and observation19. Therefore when a
patient cannot give informed consent for corticosteroid or
surgical therapy, some neuro-ophthalmologists may
simply observe the patient. This is especially reasonable
when it is difficult to assess the status of the afferent
visual system, e.g. in an unconscious or pediatric patient,
unless one eye is completely blind, as manifested by an
amaurotic pupil (one that does not react directly to light
but does react consensually).
2009 Annual Meeting Syllabus | 77
FUTURE TREATMENTS
CME ANSWERS
Neuroprotection has been a popular subject of research
for optic nerve disease, as a way of preventing the death
of retinal ganglion cells. Most studies of neuroprotection
in animals use as an outcome measure the number of
surviving retinal ganglion cells. However, treatments that
maintain retinal ganglion cell viability without taking into
account their ability to function are unlikely to be useful
clinically when translated to human use. For patients,
visual function is the critical endpoint, and the value of
neuroprotection directed at retinal ganglion cell soma
survival alone is questionable.
1. c
The questionable utility of somal neuroprotection is
especially true for traumatic optic neuropathy, which
occurs as a result of axonal damage. A treatment which
maintains the viability of the ganglion cell body but leaves
the axon injured is unlikely to be effective at maintaining
function. On the other hand, treatments that not only
keep the retinal ganglion cell from dying, but also
maintain its metabolic and biochemical functions, might
still be helpful because the invigorated cell body could
better maintain an injured axon. This would explain why
treatments which work at the cell body (e.g. NMDA
antagonists) help preserve visual function despite axonal
damage, e.g. in glaucoma20. In other words,
neuroprotective treatments for the cell body may be
helpful for marginally injured axons. Nonetheless, it
makes sense that treatments directed at preserving the
axon, i.e. axoprotection, would be a more useful strategy
for traumatic optic neuropathy.
As of yet, there is little known about how best to protect
an axon in traumatic optic neuropathy. Part of the reason
is that experimental models of traumatic optic neuropathy
use a direct axonal injury, while the clinical disease is
usually indirect, and probably a result of concussive injury
causing focal shearing, edema, and/or ischemia The most
investigated area for axoprotection is ischemia of the
isolated optic nerve, with work by Waxman and colleagues
dating back to the 1990s. They and others showed that
calcium and sodium influx mediate ischemic or anoxic
damage to retinal ganglion cell axons21, and that this can
be ameliorated by drugs that block sodium channels22, 23.
This area has been comprehensively reviewed24.
Another approach is based on the studies of the Wallerian
degeneration slow (WldS) strain of mice. WldS mice have a
mutation which results in delayed Wallerian degeneration
in both the peripheral and central nervous systems.
Axonal degeneration takes place in weeks instead of days
after injury or axonal disease. Although axonal
degeneration is delayed in these mice, death of the cell
soma by classic apoptosis occurs at the same rate as wild
type mice. Therefore, axonal degeneration and somal
apoptosis occur by different and autonomous molecular
mechanisms25, and it is likely that therapeutic approaches
aimed at the former may be of value for traumatic optic
neuropathy.
2. e
3. c
REFERENCES
1.
Mauriello JA, DeLuca J, Krieger A, et al. Management of
traumatic optic neuropathya study of 23 patients. Br J
Ophthalmol 76: 349; 1992.
2.
Hall ED. The neuroprotective pharmacology of
methylprednisolone. J Neurosurg 76: 13; 1992.
3.
Bracken MB, Shepard MJ, Collins WF, et al. A randomized,
controlled trial of methylprednisolone or naloxone in the
treatment of acute spinal-cord injury. Results of the Second
National Acute Spinal Cord Injury Study. N Engl J Med 322:
1405; 1990.
4.
Bracken MB, Shepard MJ, Holford TR, et al. Administration of
methylprednisolone for 24 or 48 hours or tirilazad mesylate
for 48 hours in the treatment of acute spinal cord injury.
Results of the Third National Acute Spinal Cord Injury
Randomized Controlled Trial. National Acute Spinal Cord
Injury Study. JAMA 277: 1597; 1997.
5.
Coleman WP, Benzel D, Cahill DW, et al. A critical appraisal of
the reporting of the National Acute Spinal Cord Injury Studies
(II and III) of methylprednisolone in acute spinal cord injury.
J Spinal Disord 13: 185; 2000.
6.
Levin LA, Baker RS. Management of traumatic optic
neuropathy. J Neuroophthalmol 23: 72; 2003.
7.
Hurlbert RJ, Moulton R. Why do you prescribe
methylprednisolone for acute spinal cord injury? A Canadian
perspective and a position statement. Can J Neurol Sci 29:
236; 2002.
8.
Molloy S, Price M, Casey AT. Questionnaire survey of the views
of the delegates at the European Cervical Spine Research
Society meeting on the administration of methylprednisolone
for acute traumatic spinal cord injury. Spine 26: E562; 2001.
9.
Ohlsson M, Westerlund U, Langmoen IA, et al.
Methylprednisolone treatment does not influence axonal
regeneration or degeneration following optic nerve injury in
the adult rat. J Neuro-Ophthalmol 24: 11; 2004.
10. Diem R, Hobom M, Maier K, et al. Methylprednisolone
increases neuronal apoptosis during autoimmune CNS
inflammation by inhibition of an endogenous neuroprotective
pathway. J Neurosci 23: 6993; 2003.
11. Steinsapir KD, Goldberg RA, Sinha S, et al. Methylprednisolone
exacerbates axonal loss following optic nerve trauma in rats.
Restor Neurol Neurosci 17: 157; 2000.
12. Roberts I, Yates D, Sandercock P, et al. Effect of intravenous
corticosteroids on death within 14 days in 10008 adults with
clinically significant head injury (MRC CRASH trial):
randomised placebo-controlled trial. Lancet 364: 1321; 2004.
13. Edwards P, Arango M, Balica L, et al. Final results of MRC
CRASH, a randomised placebo-controlled trial of intravenous
corticosteroid in adults with head injury-outcomes at 6
months. Lancet 365: 1957; 2005.
14. Yu-Wai-Man P, Griffiths PG. Steroids for traumatic optic
neuropathy. Cochrane Database Syst Rev: CD006032; 2007.
15. Levin LA, Joseph MP, Rizzo JF, 3rd, et al. Optic canal
decompression in indirect optic nerve trauma. Ophthalmology
101: 566; 1994.
78 | North American Neuro-Ophthalmology Society
16. Goldberg RA, Steinsapir KD. Extracranial optic canal
decompression: indications and technique. Ophthal Plast
Reconstr Surg 12: 163; 1996.
17. Yu Wai Man P, Griffiths PG. Surgery for traumatic optic
neuropathy. Cochrane Database Syst Rev: CD005024; 2005.
18. Wolin MJ, Lavin PJ. Spontaneous visual recovery from
traumatic optic neuropathy after blunt head injury. Am J
Ophthalmol 109: 430; 1990.
19. Levin LA, Beck RW, Joseph MP, et al. The treatment of
traumatic optic neuropathy: the International Optic Nerve
Trauma Study. Ophthalmology 106: 1268; 1999.
20. Hare WA, WoldeMussie E, Lai RK, et al. Efficacy and safety of
memantine treatment for reduction of changes associated
with experimental glaucoma in monkey, I: Functional
measures. Invest Ophthalmol Vis Sci 45: 2625; 2004.
21. Waxman SG, Black JA, Ransom BR, et al. Protection of the
axonal cytoskeleton in anoxic optic nerve by decreased
extracellular calcium. Brain Res 614: 137; 1993.
22. Garthwaite G, Goodwin DA, Neale S, et al. Soluble guanylyl
cyclase activator YC-1 protects white matter axons from nitric
oxide toxicity and metabolic stress, probably through Na(+)
channel inhibition. Mol Pharmacol 61: 97; 2002.
23. Fern R, Ransom BR, Stys PK, et al. Pharmacological protection
of CNS white matter during anoxia: actions of phenytoin,
carbamazepine and diazepam. J Pharmacol Exp Ther 266:
1549; 1993.
24. Stys PK. White matter injury mechanisms. Curr Mol Med 4:
113; 2004.
25. Raff MC, Whitmore AV, Finn JT. Axonal self-destruction and
neurodegeneration. Science 296: 868; 2002.
2009 Annual Meeting Syllabus | 79
Anda mungkin juga menyukai
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- CDC/NHSN Surveillance Definitions For Specific Types of InfectionsDokumen30 halamanCDC/NHSN Surveillance Definitions For Specific Types of InfectionssofiaBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- 10 Implant Imaging 1 by 1Dokumen8 halaman10 Implant Imaging 1 by 1bhupendraBelum ada peringkat
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Diagnostic Imaging Global Market-Forecast To 2022Dokumen4 halamanDiagnostic Imaging Global Market-Forecast To 2022VinayBelum ada peringkat
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Assignment # 5 CUDokumen3 halamanAssignment # 5 CUMaryamBelum ada peringkat
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Sports Injury Assessment PDFDokumen43 halamanSports Injury Assessment PDFPatricia Andrea Acevedo ArancibiaBelum ada peringkat
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- 3 Tesla MRI-1Dokumen57 halaman3 Tesla MRI-1LenchoGudinaBegnaBelum ada peringkat
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Diagnosis of Secondary Hypertension: An Age-Based Approach: Anthony J. Viera, MD, MPH, and Dana M. Neutze, MD, PHDDokumen8 halamanDiagnosis of Secondary Hypertension: An Age-Based Approach: Anthony J. Viera, MD, MPH, and Dana M. Neutze, MD, PHDmiguel ángelBelum ada peringkat
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- 10 1016@j Jor 2020 11 011Dokumen6 halaman10 1016@j Jor 2020 11 011Lee제노Belum ada peringkat
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Quiz (Lecture 5) : Date: 14/3/2018 (Wednesday) Time: 2.15 PM VenueDokumen50 halamanQuiz (Lecture 5) : Date: 14/3/2018 (Wednesday) Time: 2.15 PM VenueKoh Jiun AnBelum ada peringkat
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- DSP Microproject Bone PDFDokumen12 halamanDSP Microproject Bone PDFBusiness principlezBelum ada peringkat
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Australasian Health Facility Guidelines 2013Dokumen49 halamanAustralasian Health Facility Guidelines 2013aegysabetterwayBelum ada peringkat
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- L-4ff - 2/BME Date: 17/04/2022: Section-ADokumen13 halamanL-4ff - 2/BME Date: 17/04/2022: Section-AHumyra HossainBelum ada peringkat
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Test Bank For Human Diseases 8th Edition ZelmanDokumen18 halamanTest Bank For Human Diseases 8th Edition ZelmanJessica Charles100% (44)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- Fully Automated 3D Colon Segmentation and Volume Rendering in Virtual RealityDokumen9 halamanFully Automated 3D Colon Segmentation and Volume Rendering in Virtual RealityJamil Al-idrusBelum ada peringkat
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- Brainstem Stroke: Anatomy, Clinical and Radiological FindingsDokumen11 halamanBrainstem Stroke: Anatomy, Clinical and Radiological FindingsMetta WitariBelum ada peringkat
- 2020 - Sainson - UK - Reino Unido - Age and Sex References Interval VATDokumen26 halaman2020 - Sainson - UK - Reino Unido - Age and Sex References Interval VAT2192036250Belum ada peringkat
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- 00 Medical-Imaging-Preface-Waleed-AltalabiDokumen5 halaman00 Medical-Imaging-Preface-Waleed-Altalabiمحمدعبدالخالق العلوانيBelum ada peringkat
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- 1 Year of On-Demand Access!Dokumen32 halaman1 Year of On-Demand Access!azuma12345Belum ada peringkat
- RCR ProgrammeDokumen7 halamanRCR ProgrammeSafia RehmanBelum ada peringkat
- MR AbdDokumen14 halamanMR AbdKhairunNisaBelum ada peringkat
- Perinatal Asphyxia: Berhane G/her (MD, Ped.Y3R) Lecture Slides For C1 Medical Students of Adigrat UniversityDokumen80 halamanPerinatal Asphyxia: Berhane G/her (MD, Ped.Y3R) Lecture Slides For C1 Medical Students of Adigrat UniversityAlemuBelum ada peringkat
- Recent Advances in Applications of Multimodal Ultrasound-Guided Photoacoustic Imaging Technology-2020Dokumen12 halamanRecent Advances in Applications of Multimodal Ultrasound-Guided Photoacoustic Imaging Technology-2020Elizabeth EspitiaBelum ada peringkat
- Rush MD Ks Rewards RulebookDokumen2 halamanRush MD Ks Rewards RulebookKenar716Belum ada peringkat
- Pola 2017Dokumen10 halamanPola 2017RobertoBelum ada peringkat
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- 24315CE r4 1-synchronyImplantFS WEBDokumen4 halaman24315CE r4 1-synchronyImplantFS WEBLong An DoBelum ada peringkat
- Radiological Diagnostics of Respiratory SystemDokumen70 halamanRadiological Diagnostics of Respiratory SystemVAISHALI CHOUDHARYBelum ada peringkat
- Medical Image Processing Question PaperDokumen4 halamanMedical Image Processing Question Papersudhakar50% (2)
- bk978 1 6817 4068 3ch1Dokumen28 halamanbk978 1 6817 4068 3ch1fysmaBelum ada peringkat
- Superior Orbital Fissure Aka Tolosa Hunt SyndromeDokumen5 halamanSuperior Orbital Fissure Aka Tolosa Hunt SyndromeKalpana GunasekarBelum ada peringkat
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Medical Image Processing StudiesDokumen10 halamanMedical Image Processing Studieslovedeep161Belum ada peringkat
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)