Hospitalization Policy
Diunggah oleh
Sudheer ChDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Hospitalization Policy
Diunggah oleh
Sudheer ChHak Cipta:
Format Tersedia
You and IBM: Hospitalization Policy India
You and IBM - India
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Health
Life
Career
Tools
Health benefits
India
[Profiled for India]
Hospitalization Policy
Effective: 01 January 2015 till 31st December 2015
OBJECTIVE
To provide employees and their immediate dependents an opportunity to avail insurance coverage
for hospitalization and Domiciliary hospitalization expenses incurred on account of their medical
needs.
ELIGIBILITY
Employee, Spouse and Children Policy (ESC Policy)
All IBM India regular (full time and part time) employees and their immediate dependents (spouse
and up to 4 children).
The Primary Insureds male and female children aged between 0 days and 24 years irrespective of
gender can be enrolled as long as they are unmarried, still financially dependent on him/her and
have not established their own independent households.
Regular (full time and part time) employees who are covered under the Employee State Insurance
Coverage (ESIC) Act will also be covered under this policy.
If an employee opts out of this policy, none of the benefits in this policy shall apply. However, the
employee shall continue to be eligible for benefits required under law.
Parents Policy
Employees can insure their dependent parents by paying the premium applicable.
The maximum age up to which parents can be insured is 90 years.
SCOPE
The policy coverage is limited to expenses incurred within India.
GENERAL INFORMATION
Insurance Company - Apollo Munich Health Insurance Company Ltd.
Apollo Munich Health Insurance Company Ltd will continue as the insurer for the Group Health
insurance Policy of IBM India for the calendar year 2015.
Apollo Munich Health Insurance (AMHI) is one of the leading insurers in India providing health
insurance. AMHI is a joint venture between Apollo Hospitals group, the leading corporate hospital
group in Asia and Munich Health, an entity of Munich Re, one of the largest re-insurers in the world.
TPA (Third Party Administrator) - Medi Assist India TPA Pvt Ltd
Medi Assist India TPA Pvt Ltd will be the Third Party Administrator (TPA) and will facilitate
administration of Group Hospitalization Policy for IBM India Regular Employees for the calendar
year 2015.
1 of 33
05/06/2015 10:15 PM
You and IBM: Hospitalization Policy India
You and IBM - India
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Health
Life
Career
Tools
All IBM India regular employees may avail coverage.
The base sum insured under this policy is INR 300,000. Employees have the option of increasing
the sum insured by opting for additional cover, the premium for which is payable by the employee.
This is a family floater plan, provided for the nuclear family (nuclear family is defined as employee,
spouse and up to 4 dependent children) i.e. there is no restriction on the amount available for each
member as long as the family does not exceed the limit of INR 300,000 or the enhanced cover in
case additional cover is opted.
All existing employees as of December 31, 2014 may avail coverage from January 1, 2015, by
default.
Spouse & Children insured as of December 31, 2014 may avail coverage from January 1, 2015.
Validation and updation of dependents details (spouse and children) of existing employees will be
possible on or before February 14, 2015.
New employee may avail coverage from their date of joining IBM India.
New employees can enroll their dependents, enhance the family floater cover, enroll parent/s and
opt for parent coverage within 45 days of joining.
New dependents are to be insured within 45 days of eligibility
From date of marriage
From date of birth of a baby
From date of legal adoption of a child
It is the responsibility of the employee to declare correct and accurate information regarding the
name and date of birth as declared in Medi Assist Website. If any information provided by an
employee is found to be incorrect or false this would result in BCG violation.
Claims submitted for dependents whose name has not been enrolled in the website will not be
processed by Medi Assist. Further, the claim will not be paid if such a claim is in any manner
fraudulent or supported by any fraudulent means or devices whether by the insured person or by
any other person acting on his behalf.
Employees share in the Premium (ESC Policy)
The premium for the base sum insured is shared between the employee and IBM.
If an employee avails of the insurance coverage, there would be a deduction of INR 1463 per
annum from the employees salary.
Unless an employee chooses to opt out of the policy, the premium, for this coverage will be
deducted from the employees salary in the month of March 2015 for employees who were on the
rolls of the company on December 31 of the previous year.
For new employees the premium will be deducted in the succeeding month after completing 45
days from enrollment start date.
This premium is eligible for deduction from the taxable income within the defined limits under
Section 80 D of the Income Tax Act.
This premium deduction does not require a declaration in the investment module of You and IBM
tool, as the deduction will happen automatically from the employees salary.
Premium amounts for primary coverage and enhanced coverage for employee and nuclear family
will be deducted from the employee's payroll without any prior intimation. The deduction will be
done within 90 days of the employee having enrolled his/her dependents on the Medi Assist
website.
For onsite employees, the deduction will be done from the onsite payroll.
2 of 33
05/06/2015 10:15 PM
You and IBM: Hospitalization Policy India
You and IBM - India
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Health
Life
Career
Tools
In case, an employee does not wish to be part of the ESC policy, he/she has an option to opt out of
the policy within 45 days of enrollment start date. Once an employee has opted for the ESC policy,
he/she will not be able to opt out of the policy mid -year
The employee can log in to Medi Assist website to opt out.
Once the employee opts out of the scheme, they and their immediate family are not eligible for any
benefits as specified in this policy.
The employee would only be eligible for hospitalization benefits on account of accident during the
course of employment and for treatment of occupational diseases, as required under applicable
law.
Once an employee has opted out of the policy, they may rejoin the policy only next year as midterm
inclusion is not allowed.
In case employee opts out the employee would only be eligible for hospitalization benefits on
account of accident during the course of employment and for treatment of occupational diseases,
as required under applicable law for a sum insured of INR 200,000
DOMICILIARY EXPENSES ON OUTPATIENT CARE
This benefit is extended only to the employee. It is not applicable to the Parents Policy.
Domiciliary expenses on outpatient care for employee is up to a sum insured of INR 10,000 and
with a co-payment of 50% applicable on each & every claim (i.e., actual cost maximum of INR
20,000 at 50% co pay). This INR 10, 000 as a sublimit of the basic in patient sum insured and
balance cannot be carried forward to subsequent year(s). There is no minimum amount for
claim.
This benefit would be available only for specialist consultations and investigations prescribed by
a specialist and not for the treatment taken. Please note that routine health checkups do not fall
under the category of domiciliary benefit and such claims will not be admitted by the insurer.
Charges towards specialist consultation and investigations prescribed by the specialist are
covered.
A specialist is defined as a Physician (M.B.B.S.) whose practice is limited to a particular branch
of medicine or surgery, especially one who is certified by a board of physicians and should hold
an additional degree of MD or MS, DM, MCH, DGO, DNB, FRCS, MRCP, FRCSC and FRCAS.
Some common specialists include
Cardiologist
ENT Specialist
Neurologist
Oncologist
Gastroenterologist
Pediatrician
Gynecologist & obstetrics
Orthopedics
Nephrologists
Urologist
Ophthalmologist
Endocrinologist
Psychiatric/ Behavioral consultation by a Psychiatrist (MD Psychiatry, or similar degree) is
covered. (Psychologist consultation not covered)
3 of 33
05/06/2015 10:15 PM
You and IBM: Hospitalization Policy India
You and IBM - India
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Health
Life
Career
Tools
routine blood work, x ray, ECG, MRI, CT scans etc.
Non Allopathic/Non Specialists consultation; investigation/Medicines & consumables/Routine
Checks ups etc are not covered whether prescribed by an allopathic doctor or not.
Copayment Applicable on Domiciliary Outpatient care
A copayment of 50% on the admissible claim amount shall apply on each and every claim by the
employee and dependents ( Spouse and children)
Special provision under Domiciliary Outpatient care
In event of any incident identified as a workplace incident and if recommended by IBM
The co-payment (50%) applicable under the benefit shall be waived for the claim and
100% of the eligible expenses under consultation, investigation and treatment / medication
would be covered upto the sum insured (INR 10,000) under the benefit
All other terms, conditions under the benefit would remain unchanged
Additional coverage under family floater (ESC Policy)
An employee availing the policy has the option of buying additional coverage for his/her family in
excess of INR 300,000 up to a maximum of INR 700,000 (a total sum insured of maximum of INR
1,000,000 for family).
The incremental premium incurred due to additional coverage will be deducted from the
employees salary. There would be an additional service tax levied on the insurance premium.
Please refer Medi Assist portal for rate chart of premiums applicable
(https://www.mediassistindia.net/IWP).
Employees will need to make a fresh enrollment if they intend to take an additional cover for 2015
for self and dependents (spouse and children).
Please note if the employee had enrolled for an additional cover last year (2014), they would still
need to enroll afresh on or before February 14, 2015.
In case, the employee does not enroll afresh for 2015, the additional coverage would not be carried
forward from 2014 by default.
Any ailment diagnosed / treated during coverage/enrollment window period under the lower sum
insured will continue to have the lower sum insured as the maximum cover (for that ailment and all
related ailments). This is applicable when the sum insured has been increased during enrollment
period.
Coverage at any point for any person under the ESC policy will not exceed INR 10 Lacs even
if both employee and the spouse are employees of IBM. The policy sub-limits for maternity,
domiciliary expenses, etc would apply.
Addition of Dependents (ESC Policy)
Existing employees availing the policy can add dependents at the time of renewal of the insurance
policy once a year and on or before February 14, 2015. They have to log on to the Medi Assist
website and add dependent details. Coverage will be effective from the starting date of the new
policy.
New employees availing the policy can add dependent details within 45 days of joining by logging
on to the Medi Assist website. Coverage will be effective from the date of joining.
Newly married employees availing the policy can add spouse details by logging on to the Medi
Assist website within 45 days of the date of marriage. Coverage will be effective for the spouse
from the date of marriage.
Employees availing the policy who have a new born child can add him/her within 45 days of the
4 of 33
05/06/2015 10:15 PM
You and IBM: Hospitalization Policy India
You and IBM - India
child from the date of birth.
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Health
Life
Career
Tools
Employees availing the policy who have adopted a child can add him/her within 45 days of the date
of legal adoption by logging on to the Medi Assist website. Coverage will be effective from the date
of adoption.
Mid Term Inclusion (ESC Policy)
Mid Term Inclusions will be allowed only as an exception for employees availing the policy who
missed adding the newly married spouse, new born child and adopted child details due to some
valid reasons. Some of the reasons for which midterm inclusion can be allowed are
New addition in family (spouse or child) while employee was on international assignment and
looking for enrollment soon after his/her return to home country (IBM India).
New hire who could not attend the benefits session as part of "New Hire Induction" or "RBA
program" and hence did not have access to IBM India email to refer welcome email from RBA
and action accordingly, as the employee was operating from the client location since date of
joining.
Employee was on LOA or on long leave for the complete allowed window period. (45 days from
the policy start date or marriage/childbirth, whichever is applicable)
Any request for Midterm Inclusions for spouse and children has to have approvals from the HR
Partner/Advisor along with the IST Benefits Lead. The employee would need to submit proof
of marriage or birth certificate whichever is applicable. The coverage date will be effective from
the date the inclusion is endorsed by the insurer.
There is no mid- term enhancement of sum insured with respect to existing members under both
the policies viz., Employee, Spouse & Children and Parents.
Removal of Dependents (ESC Policy)
Dependents cannot be removed during a policy period except under the following circumstances
Divorce
Death of a dependent
Resignation of the employee
The company at its sole discretion can ask for supporting documents for addition or removal of
dependents from the coverage.
Benefits Covered under ESC Policy: For details please refer to the relevant section.
Inpatient Hospitalization
30 days pre hospitalization
60 days post hospitalization
Day care procedures covered specified list
Waiver of Pre-existing disease exclusion
No 30 days and two/one year waiting period
No room rent or type restriction
Copayment 5% for employee and 20% for dependents. In case of death of an employee the
copay would be waived for the claim
Congenital internal diseases are covered.
Congenital external diseases are covered
5 of 33
05/06/2015 10:15 PM
You and IBM: Hospitalization Policy India
You and IBM - India
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Health
Life
Career
Tools
Exclusions under this benefit are
De- addiction program
Admission for primary purpose of confinement
Complications from family planning devices where Hospitalization is required (eg: Impacted IUCD)
Ambulance Limit at INR 1,500 per hospitalization- covers charges from the place of incidence to
the hospital.
Orthopedic appliances up to 5% of the eligible hospitalization expenses or actuals whichever is
lower - Artificial limbs, crutches or any other external appliance and/or device used for diagnosis or
treatment.
Laser treatment for correction of eye due to refractive error greater than or equal to 7.5D is
covered. The procedure would be covered even if the refractive error is less than 7.5D if the
surgery is performed for therapeutic reasons like erosions, non-healing ulcers, recurrent corneal
erosions, nebular opacities, etc.
Domiciliary Hospitalization Benefit
Maternity benefits
Domiciliary expenses on outpatient care
Cancer screening tests
Critical Illness Buffer:
Additional sum insured Benefits (Top-up)
Value Added Services
PARENTS POLICY
The maximum age up to which a member can be enrolled is 90 years.The coverage is on individual
basis i.e. this is not a family floater.
Employees availing the policy can choose to cover their dependent parents each, for a sum insured
of either INR 50,000, INR 100,000, INR 200,000, INR 300,000, INR 400,000 or INR 500,000.
The premium for covering parents will be deducted from the employee's salary. There would be an
additional service tax levied on the insurance premium. This amount will be eligible for deduction
from taxable income within the defined limits under Section 80 D of the Income Tax Act. This
premium deduction doesnt require declaration in the investment module of You and IBM tool as
the deduction will happen automatically from the employees salary.
The Parent Policy also attracts an additional Third Party Administrator (TPA) charge of INR 71 per
parent per year and an additional service tax on the same which will also be deducted from the
employees salary. Please refer Medi Assist portal for rate chart of premiums applicable
(https://www.mediassistindia.net/IWP).
It is the responsibility of the employee to declare correct and accurate information regarding the
name and date of birth in the Medi Assist website. Any information provided by an employee is
found to be incorrect or false would result in BCG Violation.
Employees who intend to enroll their parent/s have to make fresh enrollment of parent/s for 2015
and choose coverage for parent/s. Please note if you had enrolled your parent/s in 2014 and if you
want to enroll them in 2015 as well, you are required to enroll them afresh and opt for the specified
coverage in 2015. In case, you dont enroll afresh for 2015, the enrollment and coverage for
parents would not be carried forward from 2014 by default.
Enrollment and coverage for parents for existing employees can only be done at the time of
renewal of the policy i.e., till February 14, 2015.
Enrollment and coverage for parents for new employees can only be done within 45 days from the
6 of 33
05/06/2015 10:15 PM
You and IBM: Hospitalization Policy India
You and IBM - India
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Health
Life
Career
Tools
Please note that parents declaration made in 2015 is subject to two year lock-in period. The
credentials and sum insured declared in 2015 will be freezed for 2015 & 2016. The employee does
not have an option to opt out of the policy in 2016. However new joiners will need to make the
enrollment decision at the time of joining.
Premium for parents however is payable on annual basis only i.e two years premium is not
payable at one go
No member can be covered twice in the policy even if he/she is a dependent of more than
one employee.
Claims submitted for dependents whose name has not been enrolled in the website will not be
processed by the TPA. Further, the claim will not be paid if such claim be in any manner is
fraudulent or supported by any fraudulent means or devise whether by the insured person or by
any other person acting on his behalf.
Any ailment diagnosed / treated during coverage/enrollment window period under the lower sum
insured will continue to have the lower sum insured as the maximum cover (for that ailment and all
related ailments). This is applicable when the sum insured has been increased during enrollment
window period.
Employees share in the Premium (Parents Policy)
The premium for insuring the parents will be completely borne by the employee.
Premium for parents however is payable on annual basis only i.e two years premium is not
payable at one go
Premium amount for coverage of employee's parents will be deducted from the employee's payroll
without any prior intimation.
The deduction will be done within 90 days of the employee having enrolled his/her dependents on
the Medi Assist website.
For onsite employees, the deduction will be done from the onsite payroll.
Addition of Dependent parents (Parents Policy)
Existing employees availing the policy can opt for parents coverage at the time of renewal of the
insurance policy once a year and on or before February 14, 2015. They have to log on to the Medi
Assist website and add dependent details. Coverage will be effective from the starting date of the
new policy.
New employees availing the policy can opt for parents coverage within 45 days of joining by
logging on to the Medi Assist website. Coverage will be effective from the date of joining.
Mid Term Inclusion (Parents Policy)
There is no mid-term inclusion process for parents.
There is no mid- term enhancement of sum insured in respect of existing members under both the
policies viz., Employee, Spouse & Children and Parents.
Removal of Dependents (Parents Policy)
Dependents cannot be removed during a policy period except under the following circumstances
Divorce
Death of a dependent
Resignation of the employee
The Insurance Company at its sole discretion can ask for supporting documents for addition or
7 of 33
05/06/2015 10:15 PM
You and IBM: Hospitalization Policy India
You and IBM - India
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Health
Life
Career
Tools
Benefits Covered under the Parents Policy: For details please refer to the relevant section.
Hospitalization Expenses
Domiciliary Hospitalization Benefit
Additional Benefits
Value Added Services
HOSPITALISATION EXPENSES
All pre-existing diseases are covered; Hospitalization on account of only investigation, tests and diagnosis is not covered. In case there is
an active treatment of the disease following the investigation, tests and diagnosis, the expenses of
investigation, tests and diagnosis will be covered.
Pre hospitalization expenses incurred 30 days prior to hospitalization and post hospitalization
expenses incurred up to 60 days after hospitalization relating to the illness is covered to the extent
of insurance coverage available; provided that the ailment is covered under the policy. This is
applicable for all eligible treatments other than maternity.
NO CREDIT WILL BE OFFERED FOR THESE EXPENSES. All pre hospitalization claims should
be submitted only with / after the main hospitalization claim is submitted. Reimbursement of these
expenses (both pre and post hospitalization) is possible only on production of complete and
detailed bills and documents relating to the same along with a signed claim form.
Copayment Applicable on Hospitalization Expenses.
A co-payment of 5% on the admissible claim amount shall apply on each and every claim by the
employee.
A co-payment of 20% on the admissible claim amount shall apply on each and every claim by
the dependents (Spouse, children and parents).
The co-payment on admissible claim amount shall not apply in case of death of the employee
during hospitalization.
DOMICILIARY HOSPITALISATION BENEFIT
Domiciliary Hospitalization refers to medical treatment for a period exceeding three days for such
illness/disease/injury which in the normal course would require care and treatment at a
hospital/nursing home but is actually taken whilst confined at home in India under any of the
following circumstances namely:
The condition of the patient is such that he/she cannot be moved to the Hospital/Nursing Home, or
Patient cannot be moved to the Hospital/Nursing Home for lack of accommodation therein.
However, the Domiciliary Hospitalization benefits shall NOT cover:
1. Expenses incurred for pre and post hospitalization treatment.
2. Expenses incurred for the treatment of any of the following diseases:
Asthma
Bronchitis
Chronic Nephritis and Nephritic Syndrome
Diarrhea and all types of Dysenteries including Gastroenteritis
Diabetes Mellitus and Insidious
8 of 33
05/06/2015 10:15 PM
You and IBM: Hospitalization Policy India
You and IBM - India
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Health
Life
Career
Tools
Hypertension
Influenza, Cough, and Cold
All Psychiatric and Psychosomatic disorders
Pyrexia of unknown origins for less than ten days
Tonsillitis and Upper Respiratory Tract infections including Laryngitis
Pharyngitis
Arthritis, Gout, and Rheumatism
Note: When treatment such as Dialysis, Chemotherapy, Radiotherapy, Eye Surgery, Lithotripsy
(Kidney stone removal), D&C and Tonsillectomy are taken in the Hospital/Nursing Home and the
insured is discharged the same day, the treatment will be taken under the Hospitalization Benefit
Section.
This benefit is within the overall inpatient cover i.e. there is no additional sum insured OR sub limit
applicable on this benefit.
Copayment Applicable on Domiciliary Hospitalization Expenses.
A copayment of 5% on the admissible claim amount shall apply on each and every claim by the
employee.
A copayment of 20% on the admissible claim amount shall apply on each and every claim by the
dependents (Spouse, children and parents).
The copayment on admissible claim amount shall not apply in case of death of the employee
during hospitalization.
IN PATIENT TREATMENT FOR PSYCHIATRIC AND BEHAVIORAL CONDITIONS
This benefit is extended only to the employee, spouse, and dependent children. It is not applicable
to the Parents Policy.
This benefit is unique considering that health insurance products in India typically exclude
coverage of psychiatric conditions.
The benefit shall pay for all eligible expenses incurred of inpatient treatment for any psychiatric and
behavioral condition.
This benefit is within the overall inpatient cover i.e. there is no additional sum insured OR sub limit
applicable on this benefit.
Some exclusions for this benefit are:
1. De addiction programs
2. Admission for primary purpose of confinement
Copayment Applicable Inpatient Psychiatric and Behavioral Expenses.
A copayment of 5% on the admissible claim amount shall apply on each and every claim by the
employee.
A copayment of 20% on the admissible claim amount shall apply on each and every claim by the
dependents (Spouse, children).
The copayment on admissible claim amount shall not apply in case of death of the employee
during hospitalization.
9 of 33
05/06/2015 10:15 PM
You and IBM: Hospitalization Policy India
You and IBM - India
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Health
Life
Career
Tools
This benefit is extended only to the employee, spouse, and dependent children. It is not applicable
to the Parents Policy.
Domiciliary expenses on outpatient care for employee, spouse and dependent children is up to a
sum insured of INR 10,000 and with a co-payment of 50% applicable on each & every claim (i.e.,
actual cost maximum of INR 20,000 at 50% co pay). This INR10, 000 is a sublimit of the basic in
patient sum insured and balance cannot be carried forward to subsequent year(s). There is no
minimum amount for claim.
This benefit would be available only for specialist consultations and investigations prescribed by a
specialist and not for the treatment taken. Please note that routine health checkups do not fall
under the category of domiciliary benefit and such claims will not be admitted by the insurer.
Charges towards specialist consultation and investigations prescribed by the specialist are
covered.
A specialist is defined as a Physician (M.B.B.S.) whose practice is limited to a particular branch of
medicine or surgery, especially one who is certified by a board of physicians and should hold an
additional degree of MD or MS, DM, MCH, DGO, DNB, FRCS, MRCP, FRCSC and FRCAS. Some
common specialists include
Cardiologist
ENT Specialist
Neurologist
Oncologist
Gastroenterologist
Pediatrician
Gynecologist & obstetrics
Orthopedics
Nephrologists
Urologist
Ophthalmologist
Endocrinologist
Psychiatric/ Behavioral consultation by a Psychiatrist (MD Psychiatry, or similar degree) is
covered. (Psychologist consultation not covered)
Any investigation prescribed by a specialist would be admissible under the Domiciliary Plan. i.e.
routine blood work, x ray, ECG, MRI, CT scans etc.
Non Allopathic/Non Specialists consultation; investigation/Medicines & consumables/Routine
Checks ups etc are not covered whether prescribed by an allopathic doctor or not.
Copayment Applicable on Domiciliary Outpatient care
A copayment of 50% on the admissible claim amount shall apply on each and every claim by the
employee and dependents ( Spouse and children)
Special provision under Domiciliary Outpatient care
In event of any incident identified as a workplace incident and if recommended by IBM
The co-payment (50%) applicable under the benefit shall be waived for the claim and
100% of the eligible expenses under consultation, investigation and treatment / medication
would be covered upto the sum insured (INR 10,000) under the benefit
10 of 33
05/06/2015 10:15 PM
You and IBM: Hospitalization Policy India
You and IBM - India
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Health
Life
Career
Tools
MATERNITY BENEFIT
This benefit is extended only to the employee, spouse, and dependent children policy. It is not
applicable to the Parents Policy.
The limit for maternity benefit for employees availing the policy is up to a maximum of INR 50,000
within the overall inpatient cover. If both Husband & wife are employees of IBM even then the
maximum of INR 50,000 only be applicable for maternity claim.
Hospitalization for maternity benefit can be availed up to 4 children.
The insurance plan also provides for pre and post natal expenses as a part of the maternity benefit.
The benefit will include consultations, prescribed medications and prescribed investigations up to a
maximum of INR 10,000 per maternity event. This benefit is a sub limit of the maternity benefit of
INR 50,000.
Pre Natal expenses prior to hospitalization and post hospitalization expenses incurred up to 60
days after maternity are covered to the extent of maternity sublimit of INR 10,000.
The pre natal claims should be submitted only with / after the main claim. Reimbursement of these
expenses (both pre and post natal) is possible only on production of complete and detailed bills
and documents relating to the same along with a signed claim form.
In case of any active treatment given to the new born baby, the expenses will be treated as child
expenses (immunization expenses excluded).
Copayment Applicable on Maternity Expenses
A copayment of 5% on the admissible claim amount shall apply on each and every claim by the
employee maternity and related claims up to 4 deliveries. A copayment of 20% on the admissible
claim amount shall apply on each and every claim by the dependents for maternity and related
claims up to 4 deliveries. The copayment on admissible claim amount shall not apply in case of
death of the employee during hospitalization.
HEALTH SCREENING BENEFIT
I.Health screening benefit is available to eligible members on an annual basis unless otherwise
specified
II.Biometric Screening
Combination of Onsite & offsite mode will be used
Onsite here means IBM Campus and Offsite means identified network hospitals / diagnostic
centres
Employees who are not able to participate in the onsite biometric screening camps have a choice
to get the screening done at identified network diagnostic centres/hospitals and file a
reimbursement claim
BMI, BP, Random blood glucose, total cholesterol, Hb%, peak flow test, manual short HRA from
wellness checkpoint will be offered for all employees through onsite biometrics screening camps
III. his benefit is extended only under the employee, spouse, and children (ESC) Policy. This benefit
is not applicable to the Parents Policy. This benefit is applicable to employees only except for
Sections H,I & J where children are eligible.
IV. This benefit is within the overall Sum Insured as a sub limit i.e. there is no additional sum
insured. Any Claim will be paid from main sum insured.
V. The benefit can be claimed as a reimbursement. No cashless is available for this benefit.
11 of 33
05/06/2015 10:15 PM
You and IBM: Hospitalization Policy India
You and IBM - India
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Health
Life
Career
Tools
VII. The benefit would cover tests for specific screening of conditions only and not for
diagnostic purposes, existing medical conditions, treatment or follow-up treatment
VIII. Following screening tests are also covered (in addition to biometric screening): Depending on
the age / gender & risk factor(s), screening may be suggested.
A. Risk factor screening:
Service
Smoking Use Screening
Alcohol Abuse Screening
Depression Screening
Family History of cancer, premature
cardiovascular disease, and other
significant illness
Frequency
Questions and Counselling by Healthcare Professional
on every screening visit starting at age 12 or as clinically
appropriate
Questions and Counselling by Healthcare Professional
on every screening visit starting at age 12 or as clinically
appropriate
Questions and Counselling by Healthcare Professional
on every screening visit starting at age 12 or as clinically
appropriate
On every screening visit
B. Physical Exam:
Service
Height, Weight, Body mass index (BMI),
Waist circumference
Blood pressure measurement
Vision screening
Recommendation
Measurement on every screening visit
Measurement on every screening visit
Measurement on every visit (Snellen chart
recommended) on every visit
C. Blood Tests:
Service
Total-cholesterol and HDL-cholesterol
measurement (Full lipid profile including
fasting Total-cholesterol, LDL-cholesterol,
HDL-cholesterol and Triglyceride
measurement is also acceptable)
Fasting blood glucose measurement
Recommendation
Check in men 35 years old and above and women 45
years old and above. Start earlier for any adult with any
risk factors for cardiovascular disease. Repeat testing
every 5 years if normal or more frequent if elevated.
Measure in adults 40 years old and above or earlier if
tobacco use, obesity, family history of diabetes or large
for gestational age baby, hypertension or dyslipidemia
present. If normal repeat every 5 years; more frequent
screening is appropriate based on risk factors.
D. Other tests
One time HIV
Screening (Rapid HIV
Test by Blood or Saliva)
One time Hepatitis B
Screening
Test individuals at increased risk or upon request by patient. May repeat
based on risk factors.
Test the following individuals:
Persons born in geographic regions with HBsAg prevalence of 2%
Unvaccinated persons whose parents were persons not vaccinated as
infants whose parents were born in geographic regions with HBsAg
prevalence of 8%
Injection-drug users
12 of 33
05/06/2015 10:15 PM
You and IBM: Hospitalization Policy India
You and IBM - India
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Health
Life
Career
Tools
Persons with elevated ALT/AST of unknown etiology
Persons with medical conditions that require immunosuppressive therapy
Infants born to HBsAg-positive mothers
Household contacts and sex partners of HBV-infected persons
Persons who are the source of blood or body fluid exposures that might
warrant post exposure prophylaxis (e.g., needle stick injury to a health
care worker)
Persons infected with HIV
One time Hepatitis C
Screening
HCV-testing is recommended for those who:
Currently inject drugs
Ever injected drugs, including those who injected once or a few times
many years ago
Have certain medical conditions, including persons:
who received clotting factor concentrates produced before 1987
who were ever on long-term hemodialysis
with persistently abnormal alanine aminotransferase levels (ALT)
who have HIV infection
Were prior recipients of transfusions or organ transplants, including
persons who:
were notified that they received blood from a donor who later tested
positive for HCV infection
received a transfusion of blood, blood components or an organ
transplant before July 1992
HCV- testing based on a recognized exposure is recommended for:
Healthcare, emergency medical, and public safety workers after needle
sticks, sharps, or mucosal exposures to HCV-positive blood
Children born to HCV-positive women
Note: For persons who might have been exposed to HCV within the past 6
months, testing for HCV RNA or follow-up testing for HCV antibody is
recommended.
Tuberculosis screening Screening is recommended for:
Household contacts and other close contacts of patients with active TB
People living with HIV
Current and former workers in workplaces with silica exposure
TB should be considered in people with an untreated fibrotic chest X-ray
lesion
In settings where the TB prevalence in the general population is
124/100,000 population or higher
Osteoporosis screening Preferred screening test is dual-energy x-ray absorptiometry (DEXA scan).
Screen women age 65 or older. Screening in men and in women under
age 65 based on risk factors. Repeat testing should be based on risk
factors and findings of previous test.
13 of 33
05/06/2015 10:15 PM
You and IBM: Hospitalization Policy India
You and IBM - India
Service
Cervical cancer
screening
Breast cancer
screening
Colon cancer
screening
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Health
Life
Career
Tools
Recommendation
Preferred screening test is the Papanicolau (Pap) smear. Screen women ages
21 to 65 years, every 3 years.
Preferred screening test is mammography. Screen women ages 50 to 75 years
every two years.
Screen all adults ages 50 to 75 by:
Fecal occult blood testing on 3 consecutive stool samples annually
Flexible Sigmoidoscopy every 5 years, with fecal occult blood testing every 3
years
Or Colonoscopy every 10 years
G. Vaccination
Service
Hepatitis B Vaccine
Recommendation
All doses + booster dose
H. Consultation fee for children
Service
Well child visit for ages 0-3
Recommendation
at the following ages:
3 to 5 days
1 month
2 months
4 months
6 months
9 months
12 months
15 months
18 months
24 months
30 months
Ages 3-18
Every year
I. Risk factor screening for children:
Smoking Use
Screening
Alcohol Abuse
Screening
Depression
Screening
Questions and Counseling by Healthcare Professional) on every screening visit
starting at age 12 or as clinically appropriate
Questions and Counseling by Healthcare Professional on every screening visit
starting at age 12 or as clinically appropriate
Questions and Counseling by Healthcare Professional on every screening visit
starting at age 12 or as clinically appropriate
J. Physical Exam for children
Service
Height, Weight, and Body mass index (BMI),
waist circumference
Blood pressure measurement
Vision screening
Recommendation
Measurement on every screening visit
Measurement on every screening visit
Measurement on every visit (Snellen chart
recommended) on every visit
ADDITIONAL BENEFITS
14 of 33
05/06/2015 10:15 PM
You and IBM: Hospitalization Policy India
You and IBM - India
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Health
Life
Career
Tools
The insurance plan will cover ambulance expenses for all emergency hospitalizations. The limit for
the ambulance charge is INR 1,500. Employees can claim ambulance charges only from the place
of incidence/home of the patient to the hospital and not the return trip. Ambulance usage on the
return trip will be at the cost of the employee.
Expenses towards Appliances:
The insurance plan will cover the cost of appliances as a part of orthopedic treatment. These include
but are not restricted to braces, splints, crutches, wheel chairs, artificial limb etc. These expenses
are a part of the hospitalization benefit and are reimbursable up to a maximum of 5% of the total
eligible claim amount or actual expense of the appliance whichever is lower.
CRITICAL ILLNESS BUFFER
This benefit is extended only to the employee, spouse, and dependent children. This benefit is not
applicable to the Parents Policy.
IBM shall extend support of an additional INR 700,000 per policy year for the treatment of the
following critical illnesses.
The Critical Illness Buffer can only be used once the family floater amount and the additional
coverage if any taken by the employee have been exhausted and only for the following diseases
1. Blindness
2. Cancer
3. Coronary artery surgery
4. Heart valve replacement
5. Kidney failure
6. Major organ transplant
7. Multiple sclerosis
8. Myocardial infarction
9. Paralysis
10. Stroke
11. Surgery of Aorta
12. Treatment of any injury arising out of road accidents to employees
13. Coma of specified severity
14. Motor Neuron Disease
15. Complications for a Preterm Baby
Coverage of HIV / AIDS through Critical Illness Buffer: HIV/AIDS is included in the critical
illness list for critical illness buffer. However unlike other critical illnesses mentioned above, this is
not covered under the family floater cover.
Apart from this list of illnesses, the buffer amount of INR 700,000 can be utilized for the treatment
of any injury arising out of road accidents to employees.
In case of any exception to the policy terms on critical illness, employee would require approval
from IBM Global Health design team and is subject to the availability of funds in the Corporate
Buffer of IBM India.
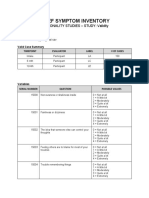
Copayment Applicable: The critical illness is linked with the additional coverage taken by the
employee. The eligibility for critical illness buffer will be determined as per the table below.
Additional coverage Amount opted for self
and Family
5 lakhs to 7 lakhs
3 lakhs to 4 lakhs
1 lakh to 2 lakhs
15 of 33
Copayment
(%)
0%
10%
20%
Total Sum Insured
(Base+Additional)
8 to10 Lakh
6 to 7 Lakh
4 to 5 Lakh
05/06/2015 10:15 PM
You and IBM: Hospitalization Policy India
You and IBM - India
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Health
Life
Career
Tools
VALUE ADDED SERVICES
Apollo Munich Health Insurance is providing a host of value added services as listed below
exclusive for IBMers
Discounts on Master Health Checkup
You can get discounts up to 20% for a master health checkup for yourself and your immediate
family (enrolled in the IBM medical insurance policy). You can reach out to Apollo Munich on the
toll free number 1800 102 0333 or write to customerservice@apollomunichinsurance.com.
The Apollo team will help you locate the nearest pharmacy / clinic / hospital. Please show your
Medi Assist Health id card (E card) with Apollo Munich logo or IBM Id card to avail these benefits.
Incase you have any concerns, do escalate by calling on the Toll free number and an Apollo team
member will address it on priority.
Discounts on diagnostics, consultation and medicines at Apollo Clinics and Apollo
Pharmacies
You can also avail discounts on diagnostics, consultation and medicines at Apollo Clinics. This
discount will differ from one clinic to another. The Apollo team will help you locate the nearest
pharmacy / clinic / hospital. Please show your Medi Assist Health id card (E card) with Apollo
Munich logo or IBM Id card to avail these benefits. Incase you have any concerns, do escalate by
calling on the Toll free number and an Apollo team member will address it on priority.
There is 11.5% discount offered to IBMers on medicines, 5% discount on purchase of non pharma
(FMCG) item and 15% discount on Apollo private labels products from Apollo Pharmacies. This
discount is not available at pharmacies located in the Apollo Hospitals and Apollo Clinics.
Process of registration
1. Log into apollopharmacy.info/IBM
2. Click on enrollment
3. Provide personal details as requested
4. Click Submit
5. Apollo advantage E card will appear
6. Take a printout of the E card
7. Show this card to Apollo Pharmacy for availing discounts
Healthline
Apollo Munich Health insurance has set up a dedicated health line especially for IBMers. Managed
by qualified doctors, the health line will provide:
Advice on self-care and symptom management
Advice on the prevention of illness
Health information on common illnesses
The employee can avail this service by calling the toll free number 1800 102 0099 between 09.00
18.00 hours, Monday to Friday (except on holidays).
Disclaimer: This service is not a substitute to consultation with physician and employees
need to discuss with their personal Physicians before going ahead with clinical support
services.
Health Tool
Log onto http://www.letsstayhealthy.com/login.aspx to educate yourself on common / chronic
16 of 33
05/06/2015 10:15 PM
You and IBM: Hospitalization Policy India
You and IBM - India
ways of improving your diet and overall wellbeing.
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Health
Life
Career
Tools
EXCLUSIONS UNDER THE POLICY:
The Insurer will not make any payment for any claim in respect of any Insured Person directly or
indirectly for, caused by, arising from or in any way attributable to any of the following unless
expressly stated to the contrary in this Policy:
i. Invasion, act of foreign enemy, civil war, public defense, rebellion, revolution, insurrection,
military or usurped acts, chemical and biological weapons
ii. Any Insured Person committing or attempting to commit a criminal or illegal act, or intentional
self-injury or attempted suicide while sane or insane.
iii. Any Insured Persons participation or involvement in naval, military or air force operation, racing,
diving, aviation, scuba diving, parachuting, hang gliding, rock or mountain climbing.
iv. The abuse or the consequences of the abuse of intoxicants or hallucinogenic substances such
as drugs and alcohol, including smoking cessation programs and the treatment of nicotine addiction
or any other substance abuse treatment or services, or supplies.
v. Obesity or morbid obesity or any weight control program, where obesity means a condition in
which the Body Mass Index (BMI) is above 29 and morbid obesity means a condition where the BMI
is above 37.
vi. Alzheimers disease; general debility or exhaustion (run down condition); genetic disorders;
stem cell implantation or surgery; or growth hormone therapy; sleep apnea
vii. Venereal disease, sexually transmitted disease or illness;
viii. Sterility, treatment whether to effect or to treat infertility, any fertility, sub fertility or assisted
conception procedure, surrogate or vicarious pregnancy, birth control, contraceptive supplies or
services and complications arising therefrom.
ix. Dental treatment and surgery of any kind, unless requiring Hospitalisation.
x. Treatment and supplies for analysis and adjustments of spinal subluxation, diagnosis and
treatment by manipulation of the skeletal structure or for muscle stimulation by any means (except
treatment of fractures and dislocations of the extremities).
xi. Circumcision (not if required as a part of treatment of or for a disease or due to injury).
xii. Laser treatment for correction of eye due to refractive error less than 7.5; if the procedure is
performed only to get rid of spectacles or contact lenses the claim is not payable; if the Lasik
Surgery is performed for therapeutic reasons like erosions, non-healing ulcers, recurrent corneal
erosions, nebular opacities, etc it is payable.
xiii. Aesthetic or change of life treatments of any description such as sex transformation operations,
treatments to do or undo changes in appearance or carried out in childhood or at any other times
driven by cultural habits, fashion or the like or any procedures which improve physical appearance.
xiv. Plastic surgery or cosmetic surgery unless necessary as a part of medically necessary treatment
certified by the attending Medical Practitioner for reconstruction following an Accident or Illness.
xv. Experimental, investigational or unproven treatment, devices and pharmacological regimens, or
measures primarily for diagnostic, X ray or laboratory examinations or other diagnostic studies
which are not consistent with or incidental to the diagnosis and treatment of the positive existence or
presence of any Illness for which confinement is required at a Hospital.
xvi. Convalescence, cure, rest cure, sanatorium treatment, rehabilitation measures, private duty
nursing, respite care, long term nursing care or custodial care.
xvii. Any non-allopathic treatment. Except Ayush Benefit Expenses incurred on treatment taken
under Ayurveda, Unani, Sidha and Homeopathy subject to amounts specified in the Schedule of
Benefits.
xviii. All preventive care, vaccination including inoculation and immunisations, any physical,
psychiatric or psychological examinations or testing during these examinations; enteral feedings
(infusion formulas via a tube into the upper gastrointestinal tract) and other nutritional and electrolyte
supplements, unless certified to be required by the attending Medical Practitioner as a direct
consequence of an otherwise covered claim.
xix. Charges related to a Hospital stay not expressly mentioned as being covered, including but not
limited to charges for admission, discharge, administration, registration, documentation and filing.
xx. Items of personal comfort and convenience including but not limited to television, telephone,
17 of 33
05/06/2015 10:15 PM
You and IBM: Hospitalization Policy India
You and IBM - India
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Health
Life
Career
Tools
services, guest services as well as similar incidental services and supplies, and vitamins and tonics
unless vitamins and tonics are certified to be required by the attending Medical Practitioner as a
direct consequence of an otherwise covered claim.
xxi. Treatment rendered by a Medical Practitioner which is outside his discipline or the discipline for
which he is licensed; referral fees or out station consultations; treatments rendered by a Medical
Practitioner who shares the same residence as an Insured Person or who is a member of an
Insured Person's family, however proven material costs are eligible for reimbursement in
accordance with the applicable cover.
xxii. The provision or fitting of hearing aids, spectacles or contact lenses including optometric
therapy, any treatment and associated expenses for alopecia, baldness, wigs, or toupees, medical
supplies including elastic stockings, diabetic test strips, and similar products.
xxiii. Any treatment or part of a treatment that is not of a reasonable cost, not medically necessary;
nonprescription drugs or treatments.
xxiv. Artificial limbs, crutches or any other external appliance and/or device used for diagnosis or
treatment.
xxv. Vaccination / Immunization.
xxvi. Stem cell Therapy/replacement.
xxvii. Treatment for ARMD Age Related Macular Degeneration with Avastin/ Macugen/ Lucentis
etc. C3R (CORNEAL COLLAGEN CROSSLINKING WITH RIBOFLAVIN) and INTACS are not
payable. Treatment related to ROP (retinopathy of prematurity) and RFL (Retrolental Fibroplasia) is
not payable.
xxviii. Treatment of Seronegative Spondyloarthritis/ Ankylosing Spondylitis, Crohns disease,
Psoriasis etc with biological agents like Remicade, Infliximab, Adalimumab, Rituximab etc.
xxix. Quantum Magnetic Resonance Therapy or RFQMR (Cytotron) treatments are not admissible
under the policy.
NOTE : All types of non-medical expenses (refer the next question for details of the same) incurred
during the course of hospitalization are not covered and have to be paid to the hospital before
discharge
USER GUIDANCE
Medi Assist HELPDESK
The TPA (Medi Assist) will be setting up helpdesks for IBM employees at various locations
supported by Apollo Munich client relationship personnel. Please refer to the communications by
Team Benefits in this regard.
This help desk facility is an attempt to help the employees in putting forward any queries that they
may have regarding the health benefits and the policy provided by IBM.
In case of any queries/suggestions, please feel free to get in touch with or write to
ibmcare@mediassistindia.com or iqueries@in.ibm.com
Frequently Asked Questions (General):
Q. What is a family floater?
A. There is no restriction on the size of the individual claim in a year as long as the family does not
exceed the limit of INR 300,000 or the enhanced cover in case you have opted for the enhanced
cover.
Q. Who is Medi Assist India TPA Private Limited?
A. Medi Assist India TPA Private Limited is your service provider who will facilitate administration of
IBM India Limited Group Health insurance Policy (GHI) on behalf of Apollo Munich health Insurance
company ltd and assist you in accessing quality health care. It is not an insurance company; it acts
18 of 33
05/06/2015 10:15 PM
You and IBM: Hospitalization Policy India
You and IBM - India
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Health
Life
Career
Tools
Q. What are the services available to me through Apollo Munich health Insurance/Medi Assist
India TPA Private Limited?
A. The following services are available to employees
Online Enrollment System: For self and dependents
Electronic id cards: For self and dependents
Network Hospital: The largest network of hospitals in the country
Preferred Network Hospital : Discounted package rates on treatments
Cashless hospitalization facility: For treatment at network hospitals for ailments covered under the
Group Mediclaim Policy
Claims administration services: Registration of each claim
Assessment of each claim for eligibility under the plan
Recovery of missing documents if required
Submission of claim to the TPA and follow up for speedy reimbursement
Dedicated Helpline Both Voice and mail based services
Help desks at designated places
Q. Who can be covered under the policy and for what amount?
A. You and your nominated dependents (spouse and children*) are eligible under a family floater
cover of INR 300,000 unless you have opted out of the policy. If you wish to enhance the coverage
beyond the family floater of INR 300,000 (up to INR 1,000,000 in total), the incremental premium
has to be borne by yourself**.
You have the option of covering your parents under the parents' policy, but the premium, TPA
charges and the service tax would have to be borne by yourself.
NOTE: No other dependents can be insured under this health plan.
* 4 number of children are covered upto to age of 24.
** Premium chart is available on the site https://www.mediassistindia.net/IWP
Q. Do I have an option of opt out of the policy?
A. Yes, you can opt out of the policy by submitting your intent in the Medi Assist website before 14th
February 2015 or 45 days from the date of joining, whichever is earlier. The premium will not be
deducted from your salary. In this case, you and your immediate family will not be covered. You will
be provided only coverage for hospitalization on account of accident during the course of
employment and treatment of occupational diseases, to the extent you are entitled to such benefits
under any statute or law.
Q. How does the coverage take place for a new joiner?
A. Your coverage will begin from the date you have joined IBM, unless you have opted out of the
policy. But for your dependents, you need to visit the website https://www.mediassistindia.net/IWP
and complete your online enrollment procedure by submitting your dependents' details within 45
days from the date of your joining. Please use your employeeID@IBM as the username. An initial
password has been set up for you using a combination of your date of birth and your employee id.
For example, if your employee id is 123456, your username would be 123456@IBM and if your date
of birth is 30-November-2014, your initial password would be 30112014123456. Please change your
password after you log in for the first time.
Claims submitted for dependents whose name has not been enrolled in the website will not be
processed by the TPA.
19 of 33
05/06/2015 10:15 PM
You and IBM: Hospitalization Policy India
You and IBM - India
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Health
Life
Career
Tools
A. Newly married employees can add spouse details within 45 days of the date of marriage.
Coverage will be effective for the spouse from the date of marriage.
Employees who have a new born child can add them within 45 days of the date of birth. Coverage
will be effective for the new born child from the date of birth.
Mid Term Inclusions (after 45 days period) will be allowed only as an exception for employees who
missed adding the spouse details and new born child details due to some valid reasons Any request
for Midterm Inclusions for spouse and children has to have approvals from the HR Partner/Advisor
along with the IST Benefits Lead. The employee would need to submit proof of marriage or birth
certificate whichever is applicable. The coverage date will be effective from the date the inclusion is
endorsed by the TPA on behalf of the insurer.
There is no mid term inclusion process for parents.
There is no mid term enhancement of sum insured in respect of existing members under both the
policies viz., Employee, Spouse & Children and Parents
Claims submitted for dependents whose name has not been enrolled in the website will not be
processed by the TPA.
In case of a divorce/demise in the family, please inform Team Benefits/India/Contr/IBM, as soon as
possible.
Q. 'I am a newly hired employee. My wife has a preexisting health condition. How is this
handled/covered?'
A. Your wife's condition will be covered; there is a 9 month (waiver) period.
Q. How do I complete Online Enrollment procedure?
A. Here are the steps given below for enrolling
Step 1: Click on the link https://www.mediassistindia.net/IWP
Step 2: Enter your User ID and Password
Step 3: Its mandatory to change your password, before you can access any details.
Please call the support team at 1-800-425-5860 if you face any difficulties in logging in or accessing
the portal
i. It is mandatory to review and update Self and dependent details
1. Go to Beneficiary
2. Click on Online Enrollment
3. If any details need to be edited please click the Edit button highlighted against each
member.
4. Click Confirm
ii. Update bank detail to be used for reimbursement
1. Go to Beneficiary
2. Click on Online Enrollment
3. Enter Bank details under the "Bank Details" section
Q. What is an electronic ID card?
A. All employees and the insured members (provided they have not opted out), under this plan, are
entitled for an e ID card. This ID card will identify them for admission into the network hospitals and
to allow access to credit facilities at preferred hospitals around the country. This e ID card is non
transferable.
20 of 33
05/06/2015 10:15 PM
You and IBM: Hospitalization Policy India
You and IBM - India
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Health
Life
Career
Tools
returned upon request or in the event of separation from the Company's services.
Q. How do I get an electronic ID card?
A. You can and need to print the electronic ID card online. Follow the below mentioned steps to print
the ID card:
Complete the online enrollment process by adding self and dependent details by visiting
https://www.mediassistindia.net/IWP (Refer to steps for online enrollment).
It is advisable to take a print of the ID cards after completing the enrollment. These ID cards will be
useful at the time of hospitalization.
Step 1: Log on to https://www.mediassistindia.net/IWP
Step 2: Enter your User ID and Password
Step 3: You can download your e-cards anytime from the "E-cards" section of the portal
Q. What happens if I lose the ID card?
A. If you lose the ID card, you may print another copy of the card online. Follow the above
mentioned steps to print copies of the ID Card.
Frequently Asked Questions (ENROLLMENT):
Q. How do I know my balance Sum Insured?
A. Please mail Medi Assist at ibmcare@mediassistindia.com with details about your complete
name, employee id, Card number.
Q. What do I do when I do not receive any revert on enrollment related queries from Medi
Assist?
A. Please mail your query to ibm@apollomunichinsurance.com, you shall receive revert within 48
working hours.
Q. Can I club my group insurance with my personal insurance?
A. This cannot be done as both are different plans with different coverage.
Q. Can I increase my coverage (sum insured) by paying extra premium?
A. This can be done only during the declaration period.
Q. After quitting IBM, can I continue availing the benefits of this policy by paying extra
premium?
A. Once you leave IBM your coverage under the group policy would cease. You can choose to buy
a retail policy with Apollo Munich but it would be subject underwriting with the portability guidelines.
Q. Can I enroll my brother/sister/uncle/ aunt by paying additional premium?
A. No, this cannot be done as family definition is limited to self, spouse and 4 living children.
Q. If I declare my parents in 2015, can I remove them from insurance coverage next year?
A. Parents declaration made in 2015 is subject to two year lock-in period. The credentials and sum
insured declared in 2015 will be freezed for 2015 & 2016. The employee do not have an option to
opt out of the policy in 2016.
Q.I have opted for 50,000 sum insured in 2015 for my mother. Can I enhance the sum insured
in 2016?
A. Parents declaration made in 2015 is subject to two year lock-in period. The credentials and sum
insured declared in 2015 will be freezed for 2015 & 2016.
21 of 33
05/06/2015 10:15 PM
You and IBM: Hospitalization Policy India
You and IBM - India
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Health
Life
Career
Tools
A. No. The parents coverage should start either at the beginning of policy 2015 for exisiting
employees or along with new employee joining. If employee is covered in ESC or optout policy in
2015 he cannot declare the dependents in 2016 policy.
Q. Will I be insured in the policy even If I have not got my electronic id card?
A. You and your nominated dependents will be insured from the day you join IBM/date of renewal of
policy, whichever is later, provided you complete the online enrollment at
https://www.mediassistindia.net/IWP within the specified timeline.
Q. What do I do if I decide to leave the services of IBM?
A. You need to inform and submit the claim (if any) to Medi Assist before your Last working day.
This is very important because once you are deleted from the policy you will not be eligible to claim
reimbursement for any expenses incurred.
Employees, who have resigned from IBM, are required to respond to Shortfall raised by Medi Assist
within 5 working days failing which the claim will be rejected and prorated premium refund will be
advised in FFS.
In case, there is no claim made (processed & amount settled) by you for self and nuclear family,
prorata premium paid for coverage and/or additional coverage will be refunded back to you for the
period the coverage cease to exist. In case of any claim is made (Processed & amount settled) for
any one/all of the insured person, there will not be any refund of premium.
In case, there is no claim made (Processed & amount settled) for the parent, prorata premium paid
for the concerned parent will be refunded back to you for the period the coverage cease to exist. In
case of any claim is made (Processed & amount settled), there will not be any refund of premium.
Frequently Asked Questions (CLAIMS):
Q. Medi Assist Call Centre not giving correct update on my claim status, what should I do?
A. Please write to ibmcare@mediassistindia.com and seek for your claim status, in case there is no
revert within 48 hrs, please mail ibm@apollomunichinsurance.com.
Q. What do I do in case of a hospitalization in my family?
A. In case of planned hospitalization, call on the helpline numbers of Medi Assist India TPA
Private Limited to inform them when you or your nominated dependent needs hospitalization. This
should be done at least 48 hours prior to the date of admission.
Fill the Pre Authorization form, available with the Network Hospitals upon showing the Medi Assist
ID card or by mentioning your IBM employee id. This can also be obtained from the Medi Assist
helpline or can be downloaded from the Medi Assist website.
Submit/Fax the Pre Authorization Form to our toll free fax numbers at Bangalore 48 hours in
advance.
The advance intimation to Medi Assist will help you to avoid payment of advance amount to some
hospitals.
Sign the relevant documents including discharge summary before leaving the hospital/getting
discharged. If your hospitalization is authorized, then ensure you pay for non-medical expenses and
copayment charges for the dependents and parents, if enrolled.
For a non-network hospital, employee has to arrange to fax the complete pre authorization to Medi
Assist.
22 of 33
05/06/2015 10:15 PM
You and IBM: Hospitalization Policy India
You and IBM - India
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Health
Life
Career
Tools
authorization is complete and eligibility is determined. Medi Assist will then send an authorization
letter to the hospital.
Emergency Cashless Hospitalization:
Pre Auth Emergency Contact Numbers for IBM Employees.
Pre Auth IBM 1: 8880798041
Pre Auth IBM 2: 8088033184
When you have an emergency hospitalization and get admitted into a network hospital, please
inform your family member/relative/friend to contact the billing dept in the hospital with Medi Assist
ID or IBM employee id to send Pre authorization form to Medi Assist. If your hospitalization is
authorized, then ensure you pay for non-medical expenses and copayment charges for the
dependents and parents, if enrolled. Kindly sign the relevant documents before leaving the
hospital/getting discharged.
Cashless claims
Q What is Pre Authorization?
A. Pre authorization is a process that necessarily needs to be completed prior to hospitalization. The
forms for the same can be obtained by calling Medi Assists Telephone Help Lines or downloaded
directly from the Medi Assist web site (Home Page). The form needs to be filled with the help of the
treating doctor. This form contains details like details of treating physician and hospital*, details of
diagnosis*, treatment proposed*, past history, estimate expenses*, signature of the treating
physician*, etc. Medi Assists medical team will then evaluate the same based on medical and policy
grounds. The advance intimation to Medi Assist will help you to avoid payment of advance amount
to some hospitals.
* If complete details are not provided in the form, then credit (in the case of a network hospital) or
claim eligibility (in the case of an out of network hospital) cannot be provided.
Q. What is an Authorization letter?
A. On approval of pre authorization, an authorization letter will be sent to the hospital (only if it is on
Apollo Munich network). The letter authorizes the hospital to extend credit for all medical expenses
during hospitalization. Therefore to use Apollo Munich cashless hospitalization service it is very
important for you to follow the pre authorization process.
Q. My Pre Authorization request has been rejected. What could be the reasons?
A. Pre authorization may be declined under the following circumstances 1) Information provided was
inadequate 2) Disease is not covered by policy 3) Sum insured is exhausted
Q. How to know whether a particular treatment or hospital is covered or not under
insurance?
A. For list of network hospitals, please visit https://www.mediassistindia.net/IWP. In order to know
whether a particular treatment is covered or not please send a pre auth request to Medi Assist.
Q. During my last hospitalization, I was asked for a deposit / advance. Why?
A. Network & non-network hospitals request for deposit, same is adjusted with the final bill.
Q. What do I do incase a network hospital does not accept my Medi Assist Card?
A. In case there is an issue with a network hospital not accepting your card, then please get in touch
with the people mentioned in the escalation matrix (detailed below) or call the toll free number of
Medi Assist 1800 425 5860.
Q. What is a Network Provider and how do I identify them?
A. Based on Apollo Munichs experience and expertise they have tied up with hospitals across the
23 of 33
05/06/2015 10:15 PM
You and IBM: Hospitalization Policy India
You and IBM - India
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Network Hospitals is available on Medi Assist website.
Health
Life
Career
Tools
Q. Does it mean that I cannot get treated in a hospital of my choice?
A. You can get treated in any hospital within the country but the cashless facility will be available
only at the network hospitals. Moreover, the collection of bills and related documents in case of a
network hospital will be done by Medi Assist, whereas in case of a hospital outside of network, you
will have to collect all the documents at the time of discharge and send it to Medi Assist along with a
signed claim form.
Important: Please note that any hospital/nursing home you choose has to be registered and/or
have minimum 15 beds.
Q. Do I need to pay any money at the time of discharge?
A. In case of Non Network Hospitals - You will have to make all payments yourself and then forward
the claim (all the hospital documents and signed claim form in original) to Medi Assist in order to get
claim reimbursed from Insurance Company.
In case of Network Hospitals - Depending upon eligibility, Medi Assist will extend credit for all the
medical expenses billed by the Network hospital for the treatment of your illness only. All
non-medical expenses (described above) and any amount exceeding the credit limit will have to be
paid by you to the hospital at the time of discharge. In case if the patient admitted is a dependent,
80% of the medical expenses will be paid for and you will have to pay the balance 20% along with
all the non-medical expenses (described above) and any amount exceeding the credit limit will have
to be paid by you to the hospital at the time of discharge. The advance intimation to Medi Assist will
help you to avoid payment of advance amount to some hospitals.
Reimbursement claims
Q. How do I get a fresh cheque as my cheque has gone stale?
A. Please handover the stale cheque to the helpdesk executive of Medi Assist, fresh cheque will be
issued within 15 working days.
Q. What is the process of getting rejected cases reviewed?
A. Please mail Medi Assist at ibmcare@mediassistindia.com with details about your rejected claim.
Q. Incase my cashless request is rejected, what should I do?
A. If your cashless is rejected due to some reason, please make the payment and submit the bills
for reimbursement, case will be reviewed as per policy terms & conditions.
Q. How do I submit my claim documents for reimbursement?
A. Please handover your claim documents to the executive conducting Helpdesk in your location or
you can courier the documents to Medi Assist. Address for couriering the claim documents is:
Medi Assist India TPA Pvt Ltd; III Floor, Green Arch, Ist Main Road, J P Nagar,3rd Phase,
Bengaluru, 560078
Please specify Employee Name, Employee ID and Medi Assist Health card number on the
envelope.
Q. As per the doctor, admission was mandatory, then why did Medi Assist reject my claim
stating as Treatment possible on OPD basis?
A. Claim is processed as per policy terms & conditions, after assessing the claim if it is found that
admission was not required then decision will be considered accordingly.
Q. If my claim is rejected, can I ask Medi Assist to return my claim documents?
A. In case your claim is rejected for some reason; you can request Medi Assist for the original claim
24 of 33
05/06/2015 10:15 PM
You and IBM: Hospitalization Policy India
You and IBM - India
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Health
Life
Career
Tools
Q. Hospital says all documents are given, but Medi Assist says documents not provided.
What to do in such case?
A. Please check with Medi Assist what exactly are they asking for, approach the hospital with the
specific requirement.
Q. What is the process of availing corporate buffer?
A. In case of specified critical illnesses the employee is eligible for the buffer utilization as per limits
specified.
Q. What do I do in case I misplace my cheque?
A. Immediately inform your HR team and send an intimation mail to ibmcare@mediassistindia.com
with your complete details.
Q. Can my claim reimbursement be credited through direct bank transfer?
A. Yes, if you declare your bank account details on the Medi Assist portal, same will be considered
for direct fund transferred.
Q. What do I do incase my original claim documents are misplaced by me? Can I submit
photo copies?
A. Claim will not be processed on photocopies as originals are mandatory. Depending upon the
nature and amount of the misplaced bill, deductions will be done. However final decision vests with
the insurer.
Q. If both husband and wife are working with IBM and both have enrolled each other as
dependents, in that case if the maternity amount exceeds the limit, then can both claim the
maternity amount?
A. Maternity amount will be restricted to maternity limit; either of them can claim this amount.
Q. What is the maximum number of claims allowed in a year?
A. There is no limit on the number of claims in a years, claim amount will be limited to Sum Insured.
Q. Can I seek treatment at home and later claim it?
A. Please refer to terms and conditions under domiciliary hospitalization (detailed above).
Q. On receiving the claim settlement cheque, I notice an error in my name. How do I rectify
the same?
A. Please get in touch with your HR team with the cheque, generally the name provided during
enrollment is captured, but if there is any discrepancy kindly get the same clarified with your HR
team.
Q. My claim has been settled but I see some deductions. What can these be?
A. Deductions can pertain to non medical expenses, non submission of bills, co pay deductions.
General
Q. Can I claim health checkup charges?
A. Yes, if covered as per policy T&C
Q. Is there any minimum time limit for stay in the hospital?
A. Yes. Stay in the hospital should be for minimum of 24 hours. However, there are a few specific
ailments like Dialysis, Chemotherapy, Radiotherapy, Eye Surgery, Lithotripsy (Kidney stone
removal), D&C, and Tonsillectomy which can be covered even though the period of hospitalization is
less than 24 hours. For details on the same, please write to ibmcare@mediassistindia.com
Even if the stay is more than 24 hrs and there is no active line of treatment (only investigations,
25 of 33
05/06/2015 10:15 PM
You and IBM: Hospitalization Policy India
You and IBM - India
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Health
Life
Career
Tools
Q. What is a Claim Form?
A. A claim form is an important document which is essential for claim assessment. This form is
provided on request by Medi Assist help desk or can be downloaded from
https://www.mediassistindia.net/IWP. This form is to be signed by the member while availing the
credit facility or before submission of a claim.
Please go through the reference document for claims submission published in Medi Assist micro
site for IBM employees (https://www.mediassistindia.net/IWP) to minimize errors at the time of filling
the form.
NOTE: We will not be able to assess your claim (credit or non credit) without a signed claim form.
Q. What are considered Non-Medical Expenses?
A. Following are few of examples of Non-Medical expenses:
ADMINISTRATIVE EXPENSES
APPLIANCES
Admission charges
Water bed / Air cushion
Registration charges
Alpha bed
Medical Records/Medico legal charges
Hot water bag
Attendant stay charges
Bed pan / Kidney tray / Sputum cup
Relative stay charges
Crutches / Walker
Additional stay
Braces / Cervical collar
Gate pass / Attendant pass
Slings / Splints
Overhead charges
Knee caps
Establishment charges
Abdominal belt / LS belt
Tax
Nebuliser / Steam inhaler / Humidifier
Surcharge
Thermometer
Incidental charge
Chest binder
Waste disposal charges
Spirometer
DOCUMENTATION EXPENSES
Spacer
Glasses / lenses / goggles / Frames
Documentation charges
Discharge summary
Medical records charges
Birth certificate
Death certificate
Medical certificate
SERVICES
Private nurse charges
Telephone charges
Fax charges
Food / beverages
26 of 33
Dentures/dental braces/tooth implants
Hearing aids
Glucometer
B.P. Monitoring device
Other monitoring devices
Feeding Bottle
Cradle charges
Nipple shield / Breast reliever
Baby ID band
CONSUMABLES
Antiseptic/disinfectant solutions Soap
05/06/2015 10:15 PM
You and IBM: Hospitalization Policy India
You and IBM - India
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Health
Life
Career
Electricity charges
Oil /Cream
Water charges
Cream
T.V. / internet charges
Sanitary pads / Diapers
Newspaper / magazines
Cassette / CD / Film charges
A/c charges
Oxygen cylinder
Stationery charges
Health Foods
Tools
Linen / laundry charges
Mortuary / coffin charges
Ambulance charges
Before a hospitalization, it is absolutely essential to follow the pre authorization procedure which will
help Medi Assist to determine if the event will be covered under the policy. We understand that it
would not be possible for you to remember the above mentioned exclusions and hence the pre
authorization procedure will also help in determining the same.
Q. Will I be covered for pre hospitalization and post hospitalization expenses?
A. Yes, you will be covered for pre hospitalization expenses incurred 30 days prior to hospitalization
and post hospitalization expenses incurred up to 60 days after hospitalization relating to the illness
for which you have been hospitalized; provided that the ailment is covered under the policy. This is
applicable for all eligible treatments other than maternity. NO CREDIT WILL BE OFFERED FOR
THESE EXPENSES. Reimbursement of these expenses is possible only on production of complete
and detailed bills and documents relating to the same along with a signed claim form.
Q. What expenses are payable as a part of pre hospitalization and post hospitalization
expenses?
A. Consultation charges prescribed medicines and prescribed investigations.
Q. What are details to be included in the discharge summary?
A. This is a very important document; it will mention the Date of Admission and Date of Discharge,
Past History, details of treatment given, and requirement of medication post hospitalization, if any
and doctors signature. This will be on the letter head of the hospital.
Q. In how many days are claims to be submitted to Medi Assist?
A. Claim papers are to be submitted to Medi Assist Help desk representative or couriered to Medi
Assist within 30 days from the date of discharge. If any further documents (information) are required
then Medi Assist will send a shortfall of document intimation through email, and the same should
be requested to hospital and submitted back to Medi Assist for further processing of the claim. In
case, one does not submit the document within 3 Shortfall reminders (sent every 15 days), the case
will be closed and the case cannot be processed further.
Employees, who have resigned from IBM, are required to respond to Shortfall raised by Medi Assist
within 5 working days failing which the claim will be rejected and prorated premium refund will be
advised in FFS.
Q. What if the cost exceeds the level of hospitalization insurance cover?
A. In such a situation you will be liable to pay the differential amount. We will inform the hospital
about your eligible amount and they will recover the amount over and above the credit amount from
you directly.
Q. In a year how many times can I avail treatment in a hospital?
A. There is no limit on the number of times one can take treatment, however insurance company will
27 of 33
05/06/2015 10:15 PM
You and IBM: Hospitalization Policy India
You and IBM - India
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Health
Life
Career
Tools
Q. What is the definition of a Hospital/Nursing Home?
A. Hospital/Nursing home means any institution in India established for indoor care and treatment of
sickness and injuries and which
a. has been registered as a Hospital or Nursing Home with the local authorities and is under the
supervision of a registered and qualified medical practitioner
b. Should comply with minimum criteria as under
1. It should have at least 15 inpatient beds
2. Fully equipped operation theatre of its own wherever surgical operations are carried out
3. Fully qualified Nursing staff under its employment round the clock
4. Fully Qualified doctors should be in charge round the clock.
N.B In class C towns, condition of number of beds is reduced to 10.
Q. What does Ayurvedic treatment not cover?
A. Ayurvedic treatment on Out Patient basis, will not be payable. An admission for routine
panchakarma treatment without establishing diagnosis is not payable. Most of the ayurvedic
procedures require 1 to 2 hrs, which does not warrant hospitalization. In the absence of previous
consultations, confirming Investigation reports admission for planned panchakarma and related
ayurvedic treatment expenses are not payable.
Admissions at Non-registered hospitals, treatment availed in SPAs and resorts will not be payable.
Q. Can I claim for Abortion bills including pre and post hospitalization expenses?
A. Miscarriage / threatened abortions / medically indicated termination of pregnancy are payable.
Voluntary termination of pregnancy /infertility treatment related abortions / multifetal pregnancy
reductions (eg: triplet to twin) is not payable under policy.
Termination of pregnancy less than 12 weeks gestation is not payable.
Pre and post hospitalization expenses related to abortions / abortive outcomes are not payable
under policy.
Q. Infertility treatment is covered or not?
A. Infertility / secondary fertility /family planning (tubectomy, vasectomy) sterility related
consultations; treatments are not payable under policy. It will however cover complications from
Family Planning Devices where Hospitalization is required.
Q. ARMD, ROP, keratoconus eye complaints is payable under policy?
A. The treatment for ARMD (Age related Macular Degeneration) with Injections like Avastin /
Lucentis / Macugen is not payable. C3R (CORNEAL COLLAGEN CROSSLINKING WITH
RIBOFLAVIN) and INTACS are not payable. Treatment related to ROP (retinopathy of prematurity)
and RFL (retrolental fibroplasia) is not payable.
Q. Lasik surgery for Eye correction is covered?
A. Lasik surgery is covered if power exceeds >7.5. But surgeries indicated in view of cosmetic
/removing contact lens / spectacles are not payable. Surgeries related to implantable contact lens
not payable.
Q. Hospitalization for Investigations and evaluation is covered or not?
A. As per policy, admission into hospital for medically necessary treatment as an inpatient is
payable.
The claim is not admissible as the hospitalization was primarily for the purpose of investigation &
evaluation and oral medication.
28 of 33
05/06/2015 10:15 PM
You and IBM: Hospitalization Policy India
You and IBM - India
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Health
Life
Career
Tools
a) General checkups / routine health check investigations, dental consultations, physiotherapy are
not payable under Domiciliary OPD benefit.
b) Consultations, investigations prescribed by a specialist and treatment for road traffic accident
shall be reimbursed up to 50% of the eligible expense subject to a maximum of Rs. 10,000.
c) Specialist includes MD, MS, DM, MCH, DGO, and DNB.
d) Non Allopathic/Non Specialists consultation; investigation/Medicines & consumables/Routine
Checks ups etc is not covered whether prescribed by an allopathic doctor or not.
Q. What expenses are not payable under OPD benefit?
A. Expenses not payable under OPD benefit are:
a. Physiotherapy charges
b. Dental treatment related medical expenses
c. Maternity / infertility / miscarriage / pre conception related investigation / consultations
d. Vaccination expenses / doctor visits for vaccination consultations
e. Routine checkups / health checkups
f. Procedure charges except road traffic accidental injuries
g. Non allopathic treatments / medical expenses
h. Pharmacy / medicines / consumables & disposables
i. Bills without respective consultation letters / prescriptions
j. Consultation Bills other than specialist
k. Consultation fees details mentioned on letter head / bills which are not in preprinted bill
formats
Q.Maternity consultations are payable under OPD benefit?
A. Not payable. Please refer Pre natal and postnatal benefit.
Q. What do you mean by pre and post natal expenses will it be covered under policy?
A. From the date of conception to delivery the expenses related to scannings/ consultations are
payable under pre natal, after the delivery consultation expenses related to Mother will be paid upto
60 days under post natal benefit. Pre natal and post natal benefit will be payable upto Rs. 10000/under the limit of maternity sub limit.
In case of abortions / abortive out comes, pre and post natal is not payable / not applicable.
Q. Chemo therapy, dialysis is payable or not?
A. Payable under day care benefit. Employee has to submit Chemo / dialysis bills along with
Chemotherapy chart or Dialysis chart (which explains treatment summary along treatment dates).
Expenses related to CAPD (continuous ambulatory peritoneal dialysis) NOT payable.
Q. What are the benefits which can be availed under Domiciliary outpatient?
A. Domiciliary expenses under OPD care payable for Employee, spouse, and children.
Not applicable for parents. All domiciliary claims incurred by any family member (employee, spouse,
and dependent children) will be borne by the insurer and employee on a 50%: 50% basis.
Annual limit is INR 10,000 per family (i.e., actual cost maximum of INR 20,000 at 50% copay) and
balance cannot be carried forward to subsequent year(s). No minimum amount for claim.
Q. Are there any Specific criteria under domiciliary outpatient benefits?
A. Specialist consultations and investigations advised by specialist will be payable under the policy
with 50% copay on actual up to 10000 INR per family. Specialist includes MD, MS, DM, MCH, DGO,
DNB, FRCS, MRCP, FRCSC, FRCAS..
B. Dental / physiotherapy / maternity related expenses are not payable under domiciliary benefit.
29 of 33
05/06/2015 10:15 PM
You and IBM: Hospitalization Policy India
You and IBM - India
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Health
Life
Career
Tools
A. As per policy Inj. Remicade administration / IV infusion is not payable under hospitalization policy.
Q. RFQMR is payable or not?
A. Rotational Field Quantum Magnetic Resonance is not payable as per policy.
Q. What are the mandatory documents required for claim submission?
A. Checklist for employee reference:
1.Apollo Munich claim form duly filled and signed
2.Photocopy of Ecard
3.Original medicine bills and Doctors payment receipts with corresponding prescriptions. Doctor
name and specialization should be visible in prescriptions / consultation letters.
4.Lab reports
Note: Employees do not need to submit original Xray films, ultrasound films, scans, etc.
However, the employee may be asked to submit original lab reports/scans for further investigation, if
required.
Additionally, based on the claim type, the employee will be required to submit the following
documents:
S. Activity
No.
Claim Type
1 OPD / domiciliary claims
2 Cancer Screening Tests
3 Inpatient / Day care claims
30 of 33
Details
Mandatory documents for claim
submission Checklist For
employee reference
1. Treating Dr specialization details
(provided on prescription / letter head),
diagnosis along with Dr sign and seal
on claim form / prescriptions for all
OPD claims
1. Requisition letter (Doctor's
prescription on advising specific test )
2. Original bill with details of procedure
expenses
3. Investigation report (photocopy
attested by the doctor)
4. Investigation bill in original
1. Photocopy of detailed discharge
summary / day care summary with
signature & seal from hospital where
treatment is taken
2. Original consolidated hospital main
bill with break ups of each items duly
signed by insured
3. Original payment receipt of the
hospital bills
4. Original lab investigation bills with
original payment receipts (if any)
5. Original invoice bills for implants
(ex: stents / IOL /mesh etc) with
original payment receipts along with
stickers
6. In case of maternity, a certificate
from treating doctor stating obstetric
history with GPLA (Gravida, Para
Living & Abortion) details
05/06/2015 10:15 PM
You and IBM: Hospitalization Policy India
You and IBM - India
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Health
Life
Career
Tools
hospital bills
2. Original lab investigation bills with
original payment receipts (if any)
3. Photocopy of discharge summary of
the main claim with signature & seal
from hospital where treatment is taken
5 KYC/ AML documents if claim amount exceeds >
Documents for ID proof
1lakh; one ID proof ad one address proof has to be i. Pan Card
given mandatorily
ii. If Pan Card is not available please
submit any of the documents
mentioned below stating reason for not
having Pan Card.
a) Passport
b) Voters Identity Card
c) Driving License
d) Personal Identification and
Certification of the employees for your
identity.
e) Letter issued by Unique
identification Authority of India
containing details of name address
and Aadhar
f) Number
g) Job Card issued by NREGA duly
signed by an officer of the State
Government
Documents for address proof
I. Electricity Bill not older than 6
months from the date of Insurance
Contract
II. Telephone Bill pertaining to any kind
of telephone connection like mobile,
landline, wireless etc. Provided it is not
older than 6 months from the date of
claim submission
III. Ration Card
IV. Valid lease agreement along with
rent receipts which is not more than 3
months old as a residence proof
V. Saving Bank Passbook with details
of permanent/ present residence
address ( updated upto 1 month prior
to claim submission document)
VI. Statement of saving bank account
with details of present/ present
address ( updated upto 1 month prior
to claim submission document)
6 Contribution clause (If an employee is claiming from 1. Photocopy of mandatory documents
more than one insurer, the total claim expense is
(including additional documents
shared by the insurers proportionately. Each insurer specified in S. No. 2) along with
contributes towards the claim payment in proportion settlement note from other TPA /
to the sum insured limited opted.)
Insurer
2. Employee declaration on claimed
amount from AMHIC and settled
31 of 33
05/06/2015 10:15 PM
You and IBM: Hospitalization Policy India
You and IBM - India
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Health
Life
Career
balance cash paid receipts
Tools
Please go through the reference document for claims submission published in Medi Assist site for
IBM employees (https://www.mediassistindia.net/IWP) to minimize errors at the time of filling the
form.
Q. BPAP, CPAP is payable or not?
A. As per policy External appliances are not payable.
Q. Water, electricity, linen, AC charges are payable under room rent?
A. If those components are charged separately, then not payable as per policy.
Q. Ive got settlement for maternity claim under my Spouses insurance policy. Now I would
like to claim for Well baby expenses and pre and post natal expenses under policy?
A. Yes. You can claim well baby expenses upto Rs.10000 within the sublimit of maternity. Pre and
post natal can be payable upto Rs. 10000 within the sublimit of Maternity
Q. Congenital external ailments are payable under policy?
A. Cover for congenital external diseases irrespective of age is payable under policy.
Q. Hospitalization for CT scan or MRI scans is covered under policy?
A. As per policy admission for investigations & evaluation and oral medication is not payable.
Q. Why should I submit cash paid receipts?
A. As per original policy cash paid receipt along with original bills are mandatory requirement s for
claim process.
Frequently Asked Questions (MISCELLANEOUS):
Q. What are the Help Line Numbers?
A. For IBM employees, the exclusive help line number is 1800 425 5860.
You can also connect at the following toll free nos given below:
For Pre Auth Emergency Contact Numbers for IBM Employees are :
Pre Auth IBM 1: 8880798041
Pre Auth IBM 2: 8088033184
Q. Can I email my queries to Medi Assist India TPA Private Limited?
A. Yes, there is a dedicated email id for IBM. Please send your queries to
ibmcare@mediassistindia.com
Q. What is the escalation matrix followed in Medi Assist?
A. Below mentioned are the contact numbers and mail ids for any Queries.
1. Please contact IBM Priority number 1800 425 5860.
2. Please write to ibmcare@mediassistindia.com on any unanswered Queries by call centre for
more than 2 working days You may also mark the copy of the mail to Team Benefits/India/Contr/IBM
If you are not satisfied by the response received from the above mentioned ibmcare id, please write
to ibm@apollomunichinsurance.com
We request you to follow the below mentioned escalation matrix ONLY if your queries are not
replied by above mentioned contact points
32 of 33
05/06/2015 10:15 PM
You and IBM: Hospitalization Policy India
You and IBM - India
http://w3-01.ibm.com/hr/web/in/health/hb01-hip0...
Money
Health
Life
Career
Tools
Please write to ibm.escalation@mediassistindia.com
Turn around Time: 2 working days
Mark a copy to Parimala Dintakurthi (Dintakurthi Parimala/India/IBM)
If you are not satisfied by the response received from the above mentioned id, please write to
ibm@apollomunichinsurance.com
Escalation Level 2
Please call the CRM assigned to your location or nearest location
City
Delhi
Hyderabad
Bangalore
Pune
Kolkata
Mumbai
Chennai
CRM
Ankit Pandey
Lalit Neelkanth
Mr. Madhu
Prabir Mahato
Subir Chowdhary
Mangeshwari Reddy
S Karthikeyan
Mobile
8800098355
9959801888
9740081374
9970004199
9007003379
7738008635
8056014379
Alternatively you can also write to ibm@apollomunichinsurance.com
Turn around Time: 2 working days
Mark a copy to Devi Dharmalingam (devi.dharma@in.ibm.com)
Escalation Level 3
Please write to Aniket J Joshi (Aniket J Joshi/India/IBM)
Escalation Level 4
Please write to George Avery (George Avery/Singapore/IBM)
Note: Please write to each escalation level separately according to the timelines. Do not mark
a combined mail to all the escalation points.
Equal Opportunity:
http://w3.ibm.com/hr/ap/in/yourlife/en-us/dai01-eop01.html
POLICY MANAGEMENT
Change Management
The policies are owned by AP Compensation & Benefits Director. All changes made to the policy
should be approved by the policy owner.
Violations and Exceptions
All violations are to be brought to the attention of AP Compensation & Benefits Director. Exceptions
if any, if not specified, will be approved by AP Compensation & Benefits Director.
Updated on 19 January 2015
33 of 33
05/06/2015 10:15 PM
Anda mungkin juga menyukai
- Created by Jose Garcia Luz Maria LavalleDokumen29 halamanCreated by Jose Garcia Luz Maria LavalleLuz Maria LavalleBelum ada peringkat
- Parents Guide To ADHD v1Dokumen12 halamanParents Guide To ADHD v1Oktavianus Misro AdriantoBelum ada peringkat
- BPD MagazineDokumen92 halamanBPD Magazinetan hangBelum ada peringkat
- Ego Defense MechanismDokumen5 halamanEgo Defense Mechanismmarie100% (24)
- Comparație Între SCID 5 RV Și SCID 5 CVDokumen3 halamanComparație Între SCID 5 RV Și SCID 5 CVAdrianBelean100% (1)
- OfferLetter PDFDokumen11 halamanOfferLetter PDFNaveen GaneshBelum ada peringkat
- Medical BooksDokumen20 halamanMedical Booksapi-385347264% (14)
- Unani PsychiatryDokumen6 halamanUnani PsychiatryashfaqamarBelum ada peringkat
- TCS - OfferLetterDokumen11 halamanTCS - OfferLetterSai KrishnaBelum ada peringkat
- Psychoanalytic TheoryDokumen5 halamanPsychoanalytic TheoryKhalid Saeed50% (2)
- Kayla Bourque Citation and Report (First User To Put It On Scribd!)Dokumen19 halamanKayla Bourque Citation and Report (First User To Put It On Scribd!)raynmike100% (1)
- David WebbDokumen5 halamanDavid WebbKatherine JacksonBelum ada peringkat
- 508 Suicide Prevention Paper FinalDokumen46 halaman508 Suicide Prevention Paper FinalMaria Magdalena DumitruBelum ada peringkat
- ESICDokumen30 halamanESICpraveen singh BhimBelum ada peringkat
- Importance of Health InsuranceDokumen110 halamanImportance of Health InsuranceArnav Sharma100% (1)
- Symptoms and Signs - Dany NobusDokumen13 halamanSymptoms and Signs - Dany NobusSandra Carolina Viveros MontañoBelum ada peringkat
- Process Recording BlankDokumen14 halamanProcess Recording BlankJoric Magusara100% (1)
- HCL Offer LetterDokumen14 halamanHCL Offer LetterAbisheik SBelum ada peringkat
- Compensation Meezan WordDokumen9 halamanCompensation Meezan WordUsman Aziz0% (1)
- Dell Hospitalization Insurance PolicyDokumen7 halamanDell Hospitalization Insurance Policymohitg85Belum ada peringkat
- Health Insurance Ebook PDFDokumen29 halamanHealth Insurance Ebook PDFPrashant Pote100% (1)
- ESC H BAND FAQsDokumen8 halamanESC H BAND FAQsRamesh DeshpandeBelum ada peringkat
- TCS India FAQs - Health Insurance SchemeDokumen7 halamanTCS India FAQs - Health Insurance SchemeVipul KulshreshthaBelum ada peringkat
- Lecture 3 - The Employee's State Insurance Act, 1948Dokumen8 halamanLecture 3 - The Employee's State Insurance Act, 1948rishapBelum ada peringkat
- Benefits 187Dokumen2 halamanBenefits 187Naimi SmithBelum ada peringkat
- TCS India FAQsDokumen8 halamanTCS India FAQsRaj kishan ShawBelum ada peringkat
- SBI General's Health Insurance Policy - Retail: Take Control of Your Family's Health. and Happiness TooDokumen2 halamanSBI General's Health Insurance Policy - Retail: Take Control of Your Family's Health. and Happiness ToobpshuBelum ada peringkat
- Types of Medical BenefitsDokumen2 halamanTypes of Medical Benefitspriya6batra-2Belum ada peringkat
- Employees' State Insurance Scheme: Citizen'S CharterDokumen21 halamanEmployees' State Insurance Scheme: Citizen'S CharterBhawzBelum ada peringkat
- Reports Webdocs A1243 Assistive Devices Autism Benefit Persons With DisabilitiesDokumen1 halamanReports Webdocs A1243 Assistive Devices Autism Benefit Persons With DisabilitiesHari ShankarBelum ada peringkat
- Dear All Abmers, Circular: Abm'S Group Mediclaim Insurance Policy - 2019-20Dokumen8 halamanDear All Abmers, Circular: Abm'S Group Mediclaim Insurance Policy - 2019-20DudhmogreBelum ada peringkat
- Esi Act 1948Dokumen11 halamanEsi Act 1948vinodkumarsajjanBelum ada peringkat
- InfteatrcvseDokumen12 halamanInfteatrcvseJitendra BhatewaraBelum ada peringkat
- Esi PDFDokumen29 halamanEsi PDFParameshwara AcharyaBelum ada peringkat
- GMC Fte FTC Ind enDokumen15 halamanGMC Fte FTC Ind enMuaz AzizBelum ada peringkat
- Features At-A-Glance : 205-206, C-Wing, Crystal Plaza, New Link Road, Sample Report For Demonstration Purpose OnlyDokumen3 halamanFeatures At-A-Glance : 205-206, C-Wing, Crystal Plaza, New Link Road, Sample Report For Demonstration Purpose OnlySubhodeep NandiBelum ada peringkat
- FAQ Group Life InsuranceDokumen5 halamanFAQ Group Life InsuranceMuhammad Yousuf FazalBelum ada peringkat
- Kpit BenefitsDokumen12 halamanKpit BenefitsRAHUL DAM100% (1)
- Section 80d of Income TaxDokumen7 halamanSection 80d of Income TaxBAJRANG LAL AgrawalBelum ada peringkat
- 80D DeductionDokumen6 halaman80D DeductionsedunairBelum ada peringkat
- Health InsuranceDokumen11 halamanHealth InsurancedishaBelum ada peringkat
- Reports Webdocs W0215 FAQ ESC V2Dokumen12 halamanReports Webdocs W0215 FAQ ESC V2Mythily RBelum ada peringkat
- Act Labour Employees StateinsuranceDokumen15 halamanAct Labour Employees StateinsuranceShivam KumarBelum ada peringkat
- Mediclassic NewDokumen2 halamanMediclassic NewPiyush KantBelum ada peringkat
- Esi Act 1948Dokumen16 halamanEsi Act 1948Ravi NarayanaBelum ada peringkat
- Ab Arogyadaan SchemeDokumen11 halamanAb Arogyadaan SchemeSrinivas Kumar KBelum ada peringkat
- What Is Corporate Health Insurance?Dokumen4 halamanWhat Is Corporate Health Insurance?Muhammad RamzanBelum ada peringkat
- Module 1 - Statutory and Legal Compliance - HR Generalist CourseDokumen32 halamanModule 1 - Statutory and Legal Compliance - HR Generalist Coursesaptaksamadder4Belum ada peringkat
- Associate Welfare Trust Faqs - Version 5Dokumen9 halamanAssociate Welfare Trust Faqs - Version 5Bhabesh Kumar PandaBelum ada peringkat
- Apollo Munich Optima Restore BrochureDokumen2 halamanApollo Munich Optima Restore BrochureAmit SawantBelum ada peringkat
- Employees' State Insurance Act, 1948Dokumen6 halamanEmployees' State Insurance Act, 1948Ronan GomezBelum ada peringkat
- TMB UNI Family Health Care PolicyDokumen24 halamanTMB UNI Family Health Care Policysubu_devasena6782100% (1)
- Group Personal Accident (GPA) & Group Term Life (GTL)Dokumen6 halamanGroup Personal Accident (GPA) & Group Term Life (GTL)RajasekharBelum ada peringkat
- Policy Terms and Conditions FAQDokumen5 halamanPolicy Terms and Conditions FAQRahul SaswadkarBelum ada peringkat
- ESIC IntroductionDokumen10 halamanESIC IntroductionBHAVIK MODIBelum ada peringkat
- Flexi Medical Plan BrochureDokumen28 halamanFlexi Medical Plan BrochurewoodksdBelum ada peringkat
- Health InsuranceDokumen27 halamanHealth Insurancelittlemaster1982Belum ada peringkat
- Types of Esi BenefitsDokumen8 halamanTypes of Esi Benefitsbruce1990batmanBelum ada peringkat
- On "Employee's State Insurance Act 1948" of India.Dokumen20 halamanOn "Employee's State Insurance Act 1948" of India.Anshu Shekhar SinghBelum ada peringkat
- Assignment On: Study of The Employment Benefit Market of The CHINA and Comparing The Same With INDIAN MarketDokumen9 halamanAssignment On: Study of The Employment Benefit Market of The CHINA and Comparing The Same With INDIAN MarketSAURABH CHAUHANBelum ada peringkat
- Apollo Munich Optima Restore BrochureDokumen8 halamanApollo Munich Optima Restore BrochureSumit BhandariBelum ada peringkat
- Family Floater Health Insurance: Key BenefitDokumen4 halamanFamily Floater Health Insurance: Key BenefitPiku SBelum ada peringkat
- SBI PolicyDokumen9 halamanSBI Policyaharish_iitkBelum ada peringkat
- Retail Health BrochureDokumen2 halamanRetail Health BrochurejoinmeifyoucanBelum ada peringkat
- Vaccination For Covid-19Dokumen8 halamanVaccination For Covid-19Ravinda YadavBelum ada peringkat
- Health Insurance Marketplace Notice - Rev 2020Dokumen3 halamanHealth Insurance Marketplace Notice - Rev 2020andre krysaBelum ada peringkat
- Statutory BenefitsDokumen6 halamanStatutory BenefitsManishBelum ada peringkat
- Group Saving Linked Insurance SchemeDokumen14 halamanGroup Saving Linked Insurance SchemeSam DavidBelum ada peringkat
- Assignment On LL IDokumen8 halamanAssignment On LL Itanmaya_purohitBelum ada peringkat
- Employees State Insurance Act - Mod 6Dokumen10 halamanEmployees State Insurance Act - Mod 6ISHAAN MICHAELBelum ada peringkat
- Silver Health: Get Yourself and Your Family Covered by Silver Health Today and Sleep EasyDokumen2 halamanSilver Health: Get Yourself and Your Family Covered by Silver Health Today and Sleep EasyKumud GandhiBelum ada peringkat
- Teen Stress StatisticsDokumen5 halamanTeen Stress StatisticsAj BrarBelum ada peringkat
- English SbaDokumen16 halamanEnglish SbaSatyanand Loutan100% (3)
- Reflection On Bipolar DisorderDokumen2 halamanReflection On Bipolar DisorderLaila GabrielBelum ada peringkat
- Somatic Symptom Disorders and Personality DisordersDokumen15 halamanSomatic Symptom Disorders and Personality Disordersapi-287575009Belum ada peringkat
- Preventing and Managing Aggressive Behavior, Chapter 28Dokumen22 halamanPreventing and Managing Aggressive Behavior, Chapter 28Fadia AlramahiBelum ada peringkat
- Psychological Bulletin: A Brief History of Clinical PsychologyDokumen26 halamanPsychological Bulletin: A Brief History of Clinical PsychologyStiven GonzalezBelum ada peringkat
- Tustin (1994) - Perpetuation of An Error. Journal of Child Psychotherapy.20 (1), Pp.3-23Dokumen22 halamanTustin (1994) - Perpetuation of An Error. Journal of Child Psychotherapy.20 (1), Pp.3-23Lucia SalasBelum ada peringkat
- Diagnosis and Management of Post-Traumatic Stress DisorderDokumen6 halamanDiagnosis and Management of Post-Traumatic Stress DisorderGeorge PruteanuBelum ada peringkat
- CPG RESTRAIN GuidelinesDokumen8 halamanCPG RESTRAIN GuidelinesaartiBelum ada peringkat
- Tim Burton's Parent PredicamentDokumen8 halamanTim Burton's Parent PredicamentEleanor 'Nelly' LuckettBelum ada peringkat
- Hypnosis or HypnotherapyDokumen5 halamanHypnosis or HypnotherapyNadeem IqbalBelum ada peringkat
- Essay About Depression - 1628 Words 123 Help MeDokumen1 halamanEssay About Depression - 1628 Words 123 Help MeFahad AhmoodBelum ada peringkat
- ASD EtiologyDokumen21 halamanASD EtiologyJulia HartBelum ada peringkat
- Brief Symptom Inventory: Personality Studies - Study: ValidityDokumen7 halamanBrief Symptom Inventory: Personality Studies - Study: ValidityKeen ZeahBelum ada peringkat
- Pervasive Developmental DisordersDokumen11 halamanPervasive Developmental Disordersapi-3797941Belum ada peringkat
- Barabasz, A, F., Olness, K., Boland, R and Kahn, S. (2010) Medical Hypnosis Primer: Clinical and Research EvidenceDokumen3 halamanBarabasz, A, F., Olness, K., Boland, R and Kahn, S. (2010) Medical Hypnosis Primer: Clinical and Research EvidenceEdwardGardnerBelum ada peringkat
- Case Study JmeDokumen9 halamanCase Study Jmeapi-356829966100% (1)