Bone Healing Module
Diunggah oleh
IceKing233Deskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Bone Healing Module
Diunggah oleh
IceKing233Hak Cipta:
Format Tersedia
Bone Healing Module
1. Describe the normal sequence of bone healing
Fracture happens when continuity of bone is broken and blood supply
is interrupted
Happens when force applied to bone is greater than capability of bone
to maintain its intergrity, can also happen with lesser forces applied to
abnormal bone (pathological fracture), or repetitive sub-maximal
forces applied to normal bone (stress fracture)
Steps
I.
Inflammation
o Hematoma and local cell death where vessel disruption has
resulted in ischemia
o Area infiltrated by inflammatory cells local swelling and warmth.
o Inflammatory cells release lysosomal enzymes and other
mediators
o Fibroblasts, mesenchymal cells and osteoprogenitor cells
o Inflammation at peak 48 hours after fracture
o In this phase for several days
II.
Repair
o Begins few days after injury and persists a few months: two
phases
o Phase one = soft callus formation: lasts for six weeks after
injury. Bony fragments united by fibrinogous tissue = woven bone.
Fracture may still angulate if no external support takes at least
10 days so callus to become visual on radiograph
o Phase two = hard callus formation woven bone transformed to
lamellar bone takes ~3 months
III.
Remodeling
o Bone replaced 10-18% of skeleton replaced every year but
accelerated in children and fracture repair. Woven bone converted
to lamellar bone and medullary canal is reconstituted
2. Identify factors which influence the rate and success of bone healing
3. Recognize abnormal patterns of bone healing
Non-Union Fracture: delayed if union not seen at 6 month mark, described as
non-union. Two types
Atrophic: little callus formed, responds to bone grafting or
implementation of donor bone
Hypertrophic: obvious callus but continued instability often results
from increased motion at fracture site- do surgical stabilization
If non-union persists and remains mobile false joint or
pseudoarthrosis may form
Stress Fractures: imbalance of bone formation and healing, often seen in
young healthy individuals and repetitive physical activity
Common sites = tibea, metatarsal and femoral neck
Plain radiographs may be negative
Bone scans or MRI are diagnostic
Treat with immobilization
Textbook Page 232-249
Identify key features in the history of a patient with musculoskeletal
injury.
Identify key physical findings in a patient presenting with a
musculoskeletal injury
Select appropriate diagnostic tests in patients presenting with a
suspected musculoskeletal injury.
List factors which influence the rate and success of bone healing
Describe a general management protocol for patients with fractures or
dislocations
A. Fractures
Fracture is a break or loss of continuity in bone
Describe fractures according to the following
Type
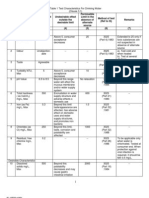
o Open: puncture through skin, need immediate treatment to
prevent infection
o Closed: overlying skin or mucosa is intact
o Stress fracture: repeated submaximal stress
o Pathologic fracture: Minimal trauma to abnormal bone (i.e.
osteoporosis)
Site: describe bone affected and specific location
o Epiphysis, metaphysis or diaphysis
o Diaphysis heals more slowly described in 1/3s (proximal, middle
or distal)
Pattern: suggests type and amount of kinetic energy
o Transverse = low energy, from direct blow or ligament avulsion.
Stress and pathological fractures often have this pattern
o Spiral or oblique = rotating/twisting injury
Comminuted/multifragmented = more than two fragments. If
middle fragment triangular called butterfly, if cylindrical called
segmental. Imply large forces and greater damage to blood
supply
o Impacted: seen in metaphyseal bone, low impact, two bone
fragments jammed together
o Compression: trabecular or cancellous bone is crushed
Displacement: fractured bone fragments may be displaced
o Anterior-posterior, medial-lateral, or length (shortening or
distraction)
o Position of distal fragment always named relative to proximal
o Angulation is relationship between long axis of distal fragment
to long axis of proximal. Described by two conventions
Direction to which distal fragment is inclined
Location of the fracture angle apex is described
o Varus: deformity apex away from midline
o Valgus: deformity apex towards midline
o Rotational deformity also expressed by identifying distal
fragment as related to proximal
o
Salter-Harris Classification of Growth Plate Fractures: in children growth plate
(physis) is between epiphysis and metaphysis
Type I: separation of epiphysis from metaphysis
Type II: passes through growth plate and exits metaphysis
Type III: extends from growth plate to epiphysis to enter the joint
Type IV: extends from metaphysis through growth plate to epiphysis
o Type III and IV are intra-articular and have highest incidence of
growth disturbance if not properly managed
Type V: crushing of epiphyseal growth plate
All growth plate fractures must be followed one year radiographically
post-surgery
Evaluation of Patients with MSK Trauma
Fracture suggested by history of injury, or in children limp or refusal to
use extremity
Symptoms: pain, swelling, deformity
Bony tenderness or crepitus suggests fracture
Assess vascular integrity and neurological status
2 MOST IMPORTANT clinical features of fracture (assessed before xray): open or closed, is neurovascular status compromised
Complete radiological exam includes
o Two views of infected bone at right angles
o Visualization of joint above and joint below injured area
o Radiological examination of known injury associations (e.g. knee
injury and hip dislocation)
o If not visualized radiographically but is clinically suspected,
reassess
Principles of Fracture Management
Treat life-threatening conditions first, then check integrity of neural and
vascular sites distal to fracture
MSK injuries must be splinted in field: splint stays on for transport and
must immobilize joint above and below fracture site
All open fractures treated as contaminated: do culture and cover with
sterile dressing, tetanus prophylaxis (if necessary) and antibiotic
treatment.
Patient prepared for surgery, necrotic tissue is debrided. 48-72 hours
later wound reopened for debridement of subsequently necrotic tissue
Two principles of fracture care:
Reduction: reduce deformity of fracture.
o Closed method: manipulation of fracture into functional position
o Open method: fracture is surgically exposed and manipulated
directly. When closed method fails or fracture is intra-articular
Maintenance of Reduction: maintain alignment until healing complete
o Facture immobilization: plaster or fibroglass cast
o Continuous traction applied through skin (foam rubber boot),
skeleton (pin inserted in bone distal to fracture site), or gravity
(activity through dependent extremity)
o Complications associated with casts and traction: circulatory
impairment, nonunion and peripheral nerve injury, ulcers, joint
stiffness and muscle atrophy
o Internal fixation devices: pins, screws, plates, etc. Enhances
early patient mobility but complications include surgical
exposure and refrature through screw holes after hardware is
removed
o External fixation: minimally invasive- threaded pins placed in
bone above and below fracture site and attached to external
frame. Complications = pin tract infection and delayed union
Rehabilitation of Function
Limb immobilized in position of max function use isometric exercises.
ROM exercise for adjacent joints. After cast removed active ROM and
resistive muscle strengthening
Speed of rehab depends on rate and quality of fracture healing.
Dependent on: amount of energy imparted to bone at time of injury,
type of bone, integrity of soft tissue envelope and patients general
health and age
Bone healing evaluated clinically (fracture no longer tender on
palpation) and radiologically (distinct bony trabeculae cross fracture
site)
Complications of Fracture Healing
I ) Local
Infection: higher incidence in open fractures
Delayed union: healing is slower than usual
Nonunion: incomplete healing, may form pseudoarthrosis (false joint)
Malunion: heals with deformity causes functional or cosmetic
impairment
Avascular necrosis: blood supply to bone injured by trauma e.g. head
of femur
Growth disturbances: children, growth may cease or continue
asymmetrically, do radiograph at one year anniversary
Post-traumatic arthritis: complication of displaced intra-articular
fractures and indirectly from severe angular deformity
II) Systemic Complications
Not common, usually result from trauma in general, include sepsis,
shock, tetanus, etc.
B. Joint Subluxation and Dislocation
Sublaxation: joints partially out of contact
Dislocation: joints completely out of contact
Diagnosis, evaluation & Treatment
Reluctance to move joint, held in typical posture, need to do
neurovascular evaluation, radiograph in dislocated position
Can be described as open or closed, distal head described in relation to
proximal
Realigned by traction
C. Common MSK Injuries
I) Upper Extremity
Carpal scaphoid fracture: most common of carpal bones, often after fall
on outstretched hand, if tenderness in anatomical snuff box treat (even
if radiograph negative), bone scan, CT or follow up radiograph at 7-14
days confirms. Cast for undisplaced and open reduction and internal
fixation for displaced
Distal radius fracture: also from falling on hand, transverse fracture of
distal radius proximal to wrist = Colles (common in elderly
osteoporotic patients), treated by longitudinal traction to hand,
manipulation into flexion and ulnar deviation, and splint from elbow to
palm. Do radiograph at 10 days. Evaluate median nerve. Should-hand
syndrome (shoulder and finger stiffness) common complication in
elderly
Olecranon fracture: direct blow to elbow, cannot extend it
Pulled Elbow: when child pulled forcibly by hand, impingement of
anular ligament on radial neck, treatment = flex elbow and supinate
hand
Supracondylar humerus fracture = fall on outstretched hand with
elbow extended, distal fragment displaced posteriorly, neurovascular
complications b/c brachial artery and medial/radial nerves become
entrapped, can cause compartment syndrome b/c of ischemia
Shoulder dislocation: humeral head anterior to fossa in 90%, axillary
nerve and artery can be hurt, test axillary nerve sensory over deltoid
patch and motor of deltoid. Reduction achieved by gradual shoulder
abduction with longitudinal traction. Posterior dislocation rare but
should be considered in all patients with shoulder symptoms after
electrocution or a seizure
2) Lower Extremity
Hip fractures: common in elderly. Common types are: i)femoral neck:
blood supply can be damaged, higher incidence of nonunion, treatment
by reduction or surgically fixed ii) intertrochanteric: outside hip joint,
good blood supply, reduced under radiographic guidance
Femoral shaft fractures: usually from high energy trauma and blood
loss is considerable, pelvis and hip must also be assessed, treat by
interlocked intermedullary nailing
Hip Dislocations: often occur in motor vehicle accidents when knee
strikes dashboard hip driven posteriorly out of acetabulum socket and
sciatic nerve may stretch, all patients assessed for foot drop and
reduced urgently risk of avascular necrosis of femoral head
Tibea and fibular shaft fractures: tibea fractures often opened and
contaminated, risk of compartment syndrome, key clinical sign in
unconscious patient is pain out of proportion to injury. Treat by closed
reduction and above-the-knee cast immobilization. Also external
fixation
Ankle injuries: mechanism of injury can be inferred from fracture line.
Transverse= pulling off force. Medial malleolus is transverse =
abduction, lateral malleolus = adduction. Spinal fracture is rotatory
force. Coronal plane spiral fracture = lateral malleolus pattern, foot
externally rotated on leg and body. Anatomic open reduction with
internal fixation
3) Spinal and Pelvic Fractures
Spinal fractures: spinal stability is critical concept in treatment. Also
perform neuro assessment
Pelvic fractures: high velocity trauma and can be associated with blood
loss and multi organ system injuries. Emergency pelvic stabilization
and external fixation essential. 2 goals are to stop bleeding and permit
sitting stability to facilitate pulmonary physiotherapy
D. Traumatic Amputations and Replantation
Completely severed digits and limbs can be re-attached
Children have better prognosis
Rule of thumb: greater the amount of muscle attached to the
amputated part, the poorer the prognosis
E. Compartment Syndrome
Bleeding and tissue swelling inside compartment- local acidosis, cell
injury and edema. Muscle and nerve necrosis can result. Classic signs
are 4 Ps: pain, parenthesia, paralysis, pallor. Do fasciotomy
Anda mungkin juga menyukai
- Seminar On Upper Limb FractureDokumen166 halamanSeminar On Upper Limb FractureArko dutta100% (1)
- Fractures: Pathophysiology and EtiologyDokumen5 halamanFractures: Pathophysiology and EtiologyHafid JuniorBelum ada peringkat
- Orthopaedic Surgery Fractures and Dislocations: Tomas Kurakovas MF LL Group 29Dokumen13 halamanOrthopaedic Surgery Fractures and Dislocations: Tomas Kurakovas MF LL Group 29Tomas Kurakovas100% (1)
- FracturesDokumen26 halamanFracturesMelinda MelinBelum ada peringkat
- EVALUATE AND TREAT ORTHOPEDIC INJURIESDokumen24 halamanEVALUATE AND TREAT ORTHOPEDIC INJURIESvikramBelum ada peringkat
- Trauma - Intertrochanteric Fracture - RustiniDokumen7 halamanTrauma - Intertrochanteric Fracture - Rustinidedyalkarni08Belum ada peringkat
- Classification of FracturesDokumen26 halamanClassification of FracturesHoney May Rollan VicenteBelum ada peringkat
- Lo MSK 2-3Dokumen6 halamanLo MSK 2-3FirmanHidayatBelum ada peringkat
- Orthopaedic EssaysDokumen139 halamanOrthopaedic EssaysDuncan Jackson100% (1)
- Orthopedic InjuriesDokumen27 halamanOrthopedic InjuriesvikramBelum ada peringkat
- تروما محاضرة 1Dokumen58 halamanتروما محاضرة 1202003339Belum ada peringkat
- Principles of Bone FracturesDokumen59 halamanPrinciples of Bone Fracturesanwar jabariBelum ada peringkat
- Fractures: Mary Grace B. Gutierrez Resti Mariano Ma. Cindy O. BautistaDokumen50 halamanFractures: Mary Grace B. Gutierrez Resti Mariano Ma. Cindy O. BautistaJustin Ahorro-DionisioBelum ada peringkat
- Dr. Chowdhury Iqbal Mahmud: MBBS, Frcs (Uk), MCH (Ortho, Uk)Dokumen48 halamanDr. Chowdhury Iqbal Mahmud: MBBS, Frcs (Uk), MCH (Ortho, Uk)Chowdhury Iqbal MahmudBelum ada peringkat
- General Principles of Fractures: Department of Orthopaedic Surgery Liu Xueyong (刘学勇)Dokumen82 halamanGeneral Principles of Fractures: Department of Orthopaedic Surgery Liu Xueyong (刘学勇)Banna Kiran KumarBelum ada peringkat
- MusculoskelealDokumen32 halamanMusculoskelealEbuka AniBelum ada peringkat
- Fracture Nursing Care Management: Study GuideDokumen5 halamanFracture Nursing Care Management: Study Guidezahwa ayundaBelum ada peringkat
- Introduction of FractureDokumen80 halamanIntroduction of Fracturealsead798Belum ada peringkat
- Common Orthopedic Emergency Conditions and Their ManagementDokumen6 halamanCommon Orthopedic Emergency Conditions and Their ManagementDhruva PatelBelum ada peringkat
- FRACTUREDokumen16 halamanFRACTUREPriyaBelum ada peringkat
- Types and Treatment of FracturesDokumen68 halamanTypes and Treatment of FracturesokaciaBelum ada peringkat
- Traumatic InjuryDokumen64 halamanTraumatic InjuryDYRAH GRACE COPAUSBelum ada peringkat
- Fractures: Types, Complications, and ManagementDokumen26 halamanFractures: Types, Complications, and Managementsm - kardmBelum ada peringkat
- Fracture: Suchithra.P.V 1 Year Msc. Nursing College of Nursing AlappuzhaDokumen96 halamanFracture: Suchithra.P.V 1 Year Msc. Nursing College of Nursing AlappuzhaAakash A. AgrawalBelum ada peringkat
- Fracture Types and ManagementDokumen53 halamanFracture Types and Managementrahul yadav100% (7)
- Tibial Plateau and Shaft Fractures GuideDokumen22 halamanTibial Plateau and Shaft Fractures GuidevadimmadanBelum ada peringkat
- Schwartz Ortho NotesDokumen16 halamanSchwartz Ortho Notesfsf50% (2)
- Fractures GuidelinesDokumen73 halamanFractures GuidelinesChester Abraham LongaBelum ada peringkat
- Principles of Fractures: (Continued)Dokumen44 halamanPrinciples of Fractures: (Continued)Abdi Ñãśìr Møhàmèď ŚàĺàhBelum ada peringkat
- Fracture 01Dokumen42 halamanFracture 01api-19916399Belum ada peringkat
- Ortho - Surgery PDFDokumen15 halamanOrtho - Surgery PDFIC BBelum ada peringkat
- Introduction To Fracture, Bone Healing and Complication: Prof - DR Jameel - Tahseen Mehsen Trauma and Orthopedics SurgeonDokumen20 halamanIntroduction To Fracture, Bone Healing and Complication: Prof - DR Jameel - Tahseen Mehsen Trauma and Orthopedics Surgeonحسين رسول ناجيBelum ada peringkat
- Skeletal Trauma-Plain Film Trauma Terminology ReviewDokumen35 halamanSkeletal Trauma-Plain Film Trauma Terminology Reviewbjpalmer100% (3)
- Types of Fractures and Healing StagesDokumen45 halamanTypes of Fractures and Healing Stagesanupama varghese100% (1)
- NCP: Nursing Care Plan For Bone FracturesDokumen8 halamanNCP: Nursing Care Plan For Bone FracturesElham TabaoBelum ada peringkat
- Management of Musculoskeletal InjuriesDokumen102 halamanManagement of Musculoskeletal InjuriesMaria Lynne Parambita100% (1)
- Fractures and Low Back Pain: Dr. Lubna DwerijDokumen49 halamanFractures and Low Back Pain: Dr. Lubna DwerijNoor MajaliBelum ada peringkat
- Fractures Diagnosis and TreatmentDokumen5 halamanFractures Diagnosis and TreatmentubaycentralBelum ada peringkat
- Percutaneous Osteosynthesis of The Distal Fractures of The Femur. Eladio Saura Mendoza e Eladio Saura SanchezDokumen12 halamanPercutaneous Osteosynthesis of The Distal Fractures of The Femur. Eladio Saura Mendoza e Eladio Saura SanchezNuno Craveiro LopesBelum ada peringkat
- ORIF Radius and Ulna ProcedureDokumen7 halamanORIF Radius and Ulna ProcedurealcojonicBelum ada peringkat
- Orthopedic: Dislocations of The Hip JointDokumen16 halamanOrthopedic: Dislocations of The Hip JointAnmarBelum ada peringkat
- FrakturDokumen188 halamanFrakturSiti RaihanatiBelum ada peringkat
- Fracturesgoutosteosprain 2Dokumen199 halamanFracturesgoutosteosprain 2Rose Cristille Yeso JocsonBelum ada peringkat
- Musculoskeletal Disorders FRACTURESDokumen10 halamanMusculoskeletal Disorders FRACTURESرافت العواضيBelum ada peringkat
- Pembahasan TTG FrakturDokumen48 halamanPembahasan TTG FrakturErik Ad'perdianBelum ada peringkat
- Orthopedic EmergenciesDokumen75 halamanOrthopedic EmergenciesAlex beharuBelum ada peringkat
- Understanding Intertrochanteric Fractures of the FemurDokumen12 halamanUnderstanding Intertrochanteric Fractures of the FemurEinz Nur Amalyah IdrusBelum ada peringkat
- Musculoskeletal Fractures GuideDokumen8 halamanMusculoskeletal Fractures GuideandreeaBelum ada peringkat
- 1 Classifications of FracturesDokumen33 halaman1 Classifications of Fracturesرغد شاكر محمود أحمدBelum ada peringkat
- General Principles of FractureDokumen31 halamanGeneral Principles of Fractureamel015Belum ada peringkat
- Comprehensive SummaryDokumen37 halamanComprehensive Summaryhrg79qzwc2Belum ada peringkat
- Types of Bone Fractures and Common Traction MethodsDokumen3 halamanTypes of Bone Fractures and Common Traction MethodsMarc AnchetaBelum ada peringkat
- Orthopedic NursingDokumen23 halamanOrthopedic Nursinggabrielle magdaraog100% (1)
- Orthopedic: Clinical Features of FracturesDokumen6 halamanOrthopedic: Clinical Features of FracturesDrAyyoub AbboodBelum ada peringkat
- Knee and Leg Injuries: Causes, Symptoms, TreatmentsDokumen14 halamanKnee and Leg Injuries: Causes, Symptoms, TreatmentsDrAyyoub AbboodBelum ada peringkat
- FIX - Fracture and DislocationDokumen80 halamanFIX - Fracture and DislocationWildan Hilmi AnsoriBelum ada peringkat
- Orthopedics Condensed MaterialDokumen13 halamanOrthopedics Condensed Materialhznknzbwk7Belum ada peringkat
- Comprehensive Guide to the General Approach and Management of Orthopedic Trauma and FracturesDokumen14 halamanComprehensive Guide to the General Approach and Management of Orthopedic Trauma and FracturesJeffrey Ariesta PutraBelum ada peringkat
- Distal Clavicle Osteolysis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandDistal Clavicle Osteolysis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- MSF - Financial - Report - 2021 - FINAL ProvisionalDokumen78 halamanMSF - Financial - Report - 2021 - FINAL ProvisionaldcgfdcBelum ada peringkat
- Drinking Water - Is 10500-1991 PDFDokumen3 halamanDrinking Water - Is 10500-1991 PDFearthanskyfriends100% (1)
- Legal and Policy Mechanisms for Urban Pollution ControlDokumen511 halamanLegal and Policy Mechanisms for Urban Pollution ControlPASTOR STARBelum ada peringkat
- Supervisory Relationship GuideDokumen4 halamanSupervisory Relationship GuideremamadhavaBelum ada peringkat
- Mobility - Nursing Test QuestionsDokumen91 halamanMobility - Nursing Test QuestionsRNStudent1100% (3)
- Financial Behavior of Millenial Genration On Investment DecisionDokumen8 halamanFinancial Behavior of Millenial Genration On Investment DecisionYuslia Nandha Anasta SariBelum ada peringkat
- Cancer FungusDokumen2 halamanCancer FungusRajesh KumarBelum ada peringkat
- Cyanotic Congenital Heart Disease With Decreased Pulmonary Blood FlowDokumen7 halamanCyanotic Congenital Heart Disease With Decreased Pulmonary Blood FlowdrhomiedanBelum ada peringkat
- IMer C Research CompetitionDokumen1 halamanIMer C Research CompetitiongabbynengBelum ada peringkat
- Hayrax Con Mascara Facial PDFDokumen8 halamanHayrax Con Mascara Facial PDFSantos LopBelum ada peringkat
- Law Oblicon :) )Dokumen9 halamanLaw Oblicon :) )Fiona MoralesBelum ada peringkat
- HSE L123 - 2016 - Health Care and First Aid On Offshore Installions and Pipeline WorksDokumen31 halamanHSE L123 - 2016 - Health Care and First Aid On Offshore Installions and Pipeline WorksKris WilochBelum ada peringkat
- The Centaur: Magazine From Centaur Services LimitedDokumen28 halamanThe Centaur: Magazine From Centaur Services LimitedStela SilvaBelum ada peringkat
- Trauma Copiilor AbandonatiDokumen132 halamanTrauma Copiilor AbandonatiPaula CelsieBelum ada peringkat
- King's Speech Speech Impediment OvercomeDokumen3 halamanKing's Speech Speech Impediment OvercomeMichael KesslerBelum ada peringkat
- IAEA SSR-3 - Safety of Research ReactorsDokumen152 halamanIAEA SSR-3 - Safety of Research Reactorsmadalina_troneaBelum ada peringkat
- Constructing Temporary Access Road for Geothermal PlantDokumen3 halamanConstructing Temporary Access Road for Geothermal PlantGad100% (6)
- Confined Space Rescue PlanDokumen10 halamanConfined Space Rescue PlanNick Shelley100% (2)
- Alternative Work Arrangement November 16-20, 2020Dokumen4 halamanAlternative Work Arrangement November 16-20, 2020Maria Kristel L PascualBelum ada peringkat
- Toronto Public Health Absenteeism Notification LetterDokumen2 halamanToronto Public Health Absenteeism Notification LetterToronto StarBelum ada peringkat
- NCP of MGH PatientDokumen2 halamanNCP of MGH PatientMaverick LimBelum ada peringkat
- Book Review: Mastery of Hand Strength (1st Edition) : Wednesday, February 11, 2009Dokumen8 halamanBook Review: Mastery of Hand Strength (1st Edition) : Wednesday, February 11, 2009Ernesto MoraBelum ada peringkat
- Aesthetic Management of Immediate Anterior Tooth Replacement With Ovate Pontic: A Case Report PDFDokumen5 halamanAesthetic Management of Immediate Anterior Tooth Replacement With Ovate Pontic: A Case Report PDFAnita PrastiwiBelum ada peringkat
- Level 2 Certificate in Understanding Behaviour That ChallengesDokumen26 halamanLevel 2 Certificate in Understanding Behaviour That Challenges0115Nurul Haque EmonBelum ada peringkat
- Adolescence: An Age of Storm and Stress: Saba HashmiDokumen15 halamanAdolescence: An Age of Storm and Stress: Saba HashmiVANDANA MISHRABelum ada peringkat
- Dent 336: Endodontics Course SyllabusDokumen9 halamanDent 336: Endodontics Course SyllabusFiru LgsBelum ada peringkat
- Ingredients:: The Lemonade Diet (Adapted From)Dokumen2 halamanIngredients:: The Lemonade Diet (Adapted From)test100% (2)
- Project Report On Herbal Extraction UnitDokumen17 halamanProject Report On Herbal Extraction UnitEIRI Board of Consultants and PublishersBelum ada peringkat
- Good Will HuntingDokumen2 halamanGood Will HuntingkyshbBelum ada peringkat
- Austin Kraft ResumeDokumen2 halamanAustin Kraft Resumeapi-384086145Belum ada peringkat