Jurnal Epilepsi
Diunggah oleh
Farhan MarzukiJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Jurnal Epilepsi
Diunggah oleh
Farhan MarzukiHak Cipta:
Format Tersedia
Seizure 19 (2010) 455460
Contents lists available at ScienceDirect
Seizure
journal homepage: www.elsevier.com/locate/yseiz
Review
Cardiac changes in epilepsy
K. Jansen, L. Lagae *
University Hospitals Leuven, Herestraat 49, 3000 Leuven, Belgium
A R T I C L E I N F O
A B S T R A C T
Article history:
Received 5 January 2010
Received in revised form 5 July 2010
Accepted 9 July 2010
Epilepsy and seizures can have a dramatic effect on the autonomic nervous system by involvement of the
central autonomic control centers. The peri-ictal changes can lead to short-term alteration of cardiac
functions in patients with seizures, and are partially hemispheric specic. Changes in heart rhythm,
conduction and even subtle signs of ischemia have been reported. Ictal asystole and the lock-step
phenomenon during seizures play an important role in the pathophysiology of SUDEP. In patients with
longlasting epilepsy and multiple seizures, there are now convincing arguments for a chronic
dysfunction of the autonomic nervous system. In this sense, heart rate variability can be considered as a
biomarker of autonomic dysfunction in epilepsy. Early recognition of these short- and long-term cardiac
effects will become useful in predicting seizures and in guiding more individualized treatment in the
near future.
2010 British Epilepsy Association. Published by Elsevier Ltd. All rights reserved.
Keywords:
Autonomic
Heart
Childhood epilepsy
SUDEP
Nervus vagus
Contents
1.
2.
3.
4.
Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Acute cardiac changes and epilepsy . . . . . . . . . .
2.1.
Tachycardia . . . . . . . . . . . . . . . . . . . . . . . .
2.2.
Bradycardia and asystole . . . . . . . . . . . . .
2.3.
Conduction disorders . . . . . . . . . . . . . . . .
2.4.
SUDEP . . . . . . . . . . . . . . . . . . . . . . . . . . . .
2.5.
Syncope . . . . . . . . . . . . . . . . . . . . . . . . . . .
2.6.
Cardiac ischemia . . . . . . . . . . . . . . . . . . . .
Chronic cardiac changes in epilepsy . . . . . . . . . .
3.1.
Heart rate variability (HRV) . . . . . . . . . . .
3.2.
AED and HRV . . . . . . . . . . . . . . . . . . . . . .
3.3.
Chronic and refractory epilepsy and HRV
3.4.
Vagal nerve stimulation (VNS) and HRV .
Conclusion . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
1. Introduction
It has been shown that epilepsy and seizures can have a
profound effect on cardiac function. Subtle cardiac rhythm changes
in the preictal and ictal period are potential biomarkers and can be
used in algorithms to anticipate and detect seizures. The
phenomenon of SUDEP is closely linked to ictal cardiac changes.
* Corresponding author at: University Hospitals Leuven, Paediatric Neurology,
Herestraat 49, 3000 Leuven, Belgium. Tel.: +32 16343845; fax: +32 16343842.
E-mail address: Lieven.Lagae@uzleuven.be (L. Lagae).
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
455
456
456
457
457
457
458
458
458
458
458
458
459
459
459
In this short review, we describe the most frequent autonomic
cardiac changes seen during seizures and in epilepsy. Emphasis
will be put on the recent insights into the links between different
seizure types and cardiac changes.
In general, the autonomic nervous system is fundamental for
maintaining homeostasis in the body through regulation of heart
rate, respiration, micturition, digestion and reproduction. The
output from the autonomic nervous system is determined by a
balance of medullary reexes and inuences of the cerebral cortex.
The medulla integrates information from the respiratory, cardiovagal and vasomotor reex centers where a distinction can be
made between parasympathetic and sympathetic reex centers.
1059-1311/$ see front matter 2010 British Epilepsy Association. Published by Elsevier Ltd. All rights reserved.
doi:10.1016/j.seizure.2010.07.008
456
K. Jansen, L. Lagae / Seizure 19 (2010) 455460
In cardiac control the parasympathetic output to the heart is
mediated by the vagus nerve. The vagus nerve starts in the medulla
oblongata, where it originates from two separate nuclei, the dorsal
motor nucleus (DMN) and the more ventrally located nucleus
ambiguous (NA). These two brainstem centers are thought to have
a distinct evolutionary origin. In the polyvagal theory, the DMN
is considered the most primitive part of the vagus with a tonic
output on heart rate. The NA is the more recently developed or
smart vagus, responsible for phasic vagal output to the heart, as
reected by respiratory sinus arrhythmia or RSA.1
Increase in vagal efferent activity results in decrease of heart
rate, atrio-ventricular conduction and ventricular excitability.
There is a close coupling between the respiratory centers and the
cardiovascular system. The vagal efferents receive direct input
from the respiratory centers in the brainstem. The respiratory
centers get information from aortic receptors and lung stretch
receptors. Excitation exists during expiration by stimulation of the
chemo and baroreceptors in the lungs and aorta. Inhibition is
caused by lung ination through information from the lung stretch
receptors.
The sympathetic output to the heart is mediated by neurons
from the rostral ventrolateral medulla resulting in an increased
automatism of the sinus node, increase in atrio-ventricular
conduction and ventricular excitability and contractility.
Higher brain systems have a descending control on autonomic
outow from the brainstem to the heart. The output of the
medullary reexes is inuenced by the insular cortex, orbitofrontal cortex, cingulate, amygdala, hypothalamus and periaqueductal gray matter. The insula and prefrontal cortex are
thought to represent the autonomic nervous system at the
cortical level. During fetal development, the insula is the rst
cortical center of maturation and vascularisation, with a right
sided predominance.24 Input from the insula can give rise to an
excitatory pressor or inhibitory depressor response at the
cardiac level.5,6 There is evidence of a hemispheric specic
organisation of this response as shown in the depth electrode
studies by Oppenheimer et al.,7 with the pressor response
lateralized to the right and depressor response to the left
hemisphere.
2. Acute cardiac changes and epilepsy
Changes in cardiac function in epilepsy imply an activation of
the central autonomic network. In patients with seizures, epileptic
discharges are thought to propagate to the central autonomic
network and change or disturb normal autonomic control of vital
cardiac functions. This activation of central autonomic nervous
system is thought to be responsible for the peri-ictal autonomic
cardiac symptoms observed in epilepsy patients. The importance
of these autonomic features in the pathophysiology of epilepsy and
its complications has become more clear in the last years.811 Due
to the hemispheric specic organisation of the central autonomic
nervous system, autonomic symptoms in epileptic seizures can
provide lateralizing and localizing information. In return, better
recognition of clinical autonomic signs in epilepsy can provide
more information on the organisation of the central autonomic
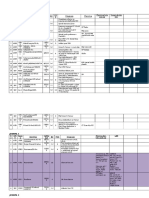
nervous system (Fig. 1).
2.1. Tachycardia
Ictal tachycardia has been reported in up to 100% of seizures.
Tachycardia can precede, coincide or follow ictal discharges.1214
As tachycardia may also precede the clinical and EEG onset of the
seizure it is not always considered secondary to the clonic phase.
The time lag between tachycardia and seizure onset varies
between 0.7 and 49.3 s. A possible mechanism is the propagation
of epileptic discharges to the right insular cortex.7 A predominance
for tachycardia in right sided temporal seizures can be expected
and is in some13,15 but not all16,17 studies conrmed, suggesting
inuence of other factors to explain the tachycardia. Ictal onset
tachycardia seems more prominent in TLE as compared with
extratemporal seizures (XTLE),18,19 supporting the hypothesis that
involvement of insular cortex is a key part of ictal tachycardia. The
duration of the tachycardia is also longer in patients with mesial
temporal lobe epilepsy compared to XTLE. It is possible that
epileptic discharges propagate towards the insular cortex more
easily and for a longer duration in TLE as compared to XTLE.
Tachycardia and development of tachyarrhythmia during
seizures is one of the possible causes of sudden unexplained
Fig. 1. Origin of autonomic symptoms in epilepsy.
K. Jansen, L. Lagae / Seizure 19 (2010) 455460
457
death in epilepsy patients (SUDEP). Tachycardia leading to malignant ventricular tachycardia and ventricular brillation has been
illustrated to be the cause of near SUDEP in a patient with TLE.20
peripheral autonomic nervous system and cardiopulmonary system
is assumed. There are three well recognized main pathophysiologic
mechanisms already known to trigger SUDEP3537:
2.2. Bradycardia and asystole
1. cardiovascular: ictal arrhythmias including ictal asytole and the
lock-step phenomenon;
2. neurogenic: neurogenic pulmonary edema;
3. respiratory: ictal respiratory suppression, central or obstructive
apnea.
Bradycardia and bradyarrhythmia are much less frequent and
are seen in seizures of various origins. A severe slowing of the heart
rate leading to asystole and syncope is referred to as the ictal
bradycardia syndrome.21
actors predisposing patients to ictal bradyarrhythmia remain
difcult to dene. The pathophysiology of bradyarrhythmia is
probably mediated through a complex cortical network. Cortical
stimulation of the left insular cortex and amygdalae have been noted
to elicit bradycardia.22,23 The left hemisphere appears to be the more
common site of origin, again supporting the hypothesis of
hemispheric specic organisation of cortical cardiac control.24,25
An atrio-ventricular block was noted in one patient during cortical
stimulation of the left temporal basal area.26 These results suggest a
higher risk of bradyarrythmia in epileptic seizures with seizure
spreading to the left insular cortex and amygdalae. The onset zone of
epileptic discharges in patients with ictal bradycardia is most
frequent temporal and less frontal, supporting the hypothesis of an
insular inuence.
Ictal bradycardia up to ictal asystole has been reported in
patients with refractory partial seizures and could be another
important link with SUDEP.27
2.3. Conduction disorders
Conduction disorders seem to be common during seizures in
intractable epilepsy. Nei et al.28 could demonstrate the presence of
arrhythmias or conduction disorders in seizures, particularly if
these are prolonged or generalized. They include atrial brillation,
supraventricular tachycardia and atrial and ventricular premature
depolarisation.
EKG changes, including T-wave inversion and ST-depression,
were more frequent and potentially more dangerous in patients
with generalized seizures.29
2.4. SUDEP
It is well known that people with epilepsy have an increased
risk for sudden unexpected death or SUDEP. SUDEP is dened as
the sudden unexpected non-traumatic and non-drowning death of
patients with epilepsy with or without evidence of a seizure,
excluding documented status epilepticus, and in whom postmortem examination does not reveal a structural or toxicological
cause for death.30 Opeskin and Berkovic looked at demographics
and risk factors among epilepsy patients. Their prole of patients at
risk for SUDEP are young persons with epilepsy. They are most
likely to die during sleep and seizure-related. Obstructive apnea
could be one explanation for sleep related death, but is not
supported by coroners ndings. The position of the patient,
together with lack of supervision of recovery from the seizure is
more likely.31,32 They found no correlation with seizure frequency
or particular epilepsy or number of AEDs.33 They did not nd a
difference in duration of epilepsy between SUDEP and control
groups. However, previous studies have shown that SUDEP
patients have earlier onset, longer duration of epilepsy and more
frequent seizures. There is evidence for an increase of cardiac
autonomic stimulation in patients with SUDEP, more pronounced
in epileptic seizures during sleep,34 compatible with the demographic ndings.
The exact mechanism of SUDEP remains an open question but is
probably multifactorial. An interaction between the central and
The rst possible mechanism underlying SUDEP are seizure
related cardiac arrhythmias with tachyarrhytmias, bradycardia
and ictal asystole as explained above. Tachyarrhythmias can evolve
to ventricular tachycardia and ultimately ventricular brillation. In
bradyarrhythmias, evolution to ictal asystole is observed in
patients with focal epilepsy. Both a sudden increase of vagal tone
or the effect of post-ganglionic epileptic discharges on the heart as
described below can be considered as an explanation for the
disturbed cardiac rhythm in epileptic seizures. Schuele reported a
series of 10 patients with focal epilepsy and ictal asystole, 8 with
TLE and 2 with XTLE.38,39 The loss of consciousness was observed
during video-electroencephalographic observation and occurred
late during the clinical event. Loss of postural tone was preceded by
8 s of asystole. In these patients activation leading to ictal asystole
is most likely mediated through an increased vagal tone. The
pattern of ictal asystole and the slowing EEG pattern of cerebral
hypoperfusion closely resembled the pattern seen in vasovagal
asystole. The underlying mechanism is most likely similar in both
conditions and assumes involvement of medullary reex centers
during epileptic discharges, responsible for the increase of vagal
tone. In the two patients with XTLE asystole could have been
triggered by hypoxia due to prolonged tonic muscle contraction
and respiratory arrest, and are not due to seizure propagation to
the medullary reex centers.
Another important neurophysiological phenomenon was described by Hilz et al.40 Seizure induced activation of the central
autonomic nervous system can cause a direct effect on postganglionic discharges on the heart. This results in a synchronisation of cardiac autonomic discharges with epileptogenic activity,
called the lock-step phenomenon and induces a lethal bradyarrythmia or asystole. Electrical stimulation of the insular cortex
results in a time-locked response on heart rhythm and can produce
different types of arrhythmia. In animal models electrical
microstimulation synchronised to the T wave of the ECG resulted
in increasing degrees of heart block and lead to escape rhythms and
ultimately asystole and dead.7 Secondary neurogenic pulmonary
edema is known as a rare life-threatening complication of central
nervous system injuries and epilepsy. Experimental studies have
postulated severe sympathetic discharge as the base of neurogenic
pulmonary edema. The cerebral sites regarded as trigger zones of
the sympathetic discharge are found in the posterior part of the
hypothalamus and in the ventral and dorsal medulla, comprising
the medial reticulated nucleus, dorsal motor vagus nucleus and
solitary tract.41 The sympathetic discharge causes systemic and
pulmonary vasoconstriction, resulting in increase in pulmonary
capillary hydrostatic pressure and shift of uid into the alveoli and
interstitium.42 A third possible mechanism in SUDEP is respiratory
suppression. Central respiratory depression can be the result of
epileptic discharges. Apnea is a rare clinical feature of seizures, but
laryngeal spasm and apnea have been reported as isolated epileptic
features or in complex partial seizures.43 The focal seizures
associated with apnea seem to originate mostly from the temporal
lobe.44 This observation together with the results of invasive EEG
monitoring in adults points to involvement of the limbic system in
seizures complicated by respiratory depression.45 Obstructive
458
K. Jansen, L. Lagae / Seizure 19 (2010) 455460
apnea and respiratory arrest have already been observed due to
tonic muscle contraction during seizures. This can lead to severe
hypoxia and trigger asystole.
Besides these three important triggers in the pathophysiology of
SUDEP, the evidence for individual predisposing risk factors is
growing. In some cases, these predisposing factors might be genetic.
Patients with an epilepsy syndrome caused by a mutation in the
sodium channel gene as in generalized epilepsy with febrile seizures
plus or severe myoclonic epilepsy of infancy seem to have a higher
risk for SUDEP.46 Chronic and refractory epilepsy and treatment of
epilepsy with anti-epileptic drugs have an inuence on the
autonomic balance, also predisposing patients for cardiovascular
complications. The latter will be discussed further in the text.
2.5. Syncope
The difference between syncope due to cardiac arrhythmia and
seizures in patients with established epilepsy remains clinically
challenging. In patients with epilepsy a distinction has to be made
between a cardiovascular or epileptic cause of loss of consciousness and syncope. Cardiovascular autonomic balance is determined by medullary reexes triggered by activation of
baroreceptors, cardiac receptors and chemoreceptors and inuences from the cerebral cortex, hypothalamus, amygdalae and
peri-aqueductal gray. As we mentioned earlier, patients with
epileptic seizures can develop various cardiovascular problems,
arrhythmias, ictal bradycardia and prolonged asystole caused by
epileptic discharges in higher autonomic control centers. These
cardiovascular problems can lead to ictal syncope as a result of
cerebral hypoperfusion. On the other hand, the sudden loss of tone
in patients with ictal asystole may be the result of ictal activation of
specic areas in the brain leading to loss of consciousness. Rapid
spread of ictal epileptic discharges with involvement of the
pontine reticular formation can lead to loss of consciousness and a
clinical syncope.5
2.6. Cardiac ischemia
As earlier mentioned, excessive autonomic stimulation may
result in cardiac arrhythmias. But repetitive autonomic stimulation can also lead to structural damage to the heart. This increases
the susceptibility to cardiac arrhythmias or ischemia. Myocardial
brosis has already been found in patients with SUDEP.47 Patients
with uncomplicated seizures do not seem to have postictal
troponin elevation, but signs of ischemia on EKG and elevated
cardiac enzymes in epileptic patients suggest secondary cardiac
damage.48,49 Alehan et al. could show presence of elevated BNP and
CK-MB in patients with seizures, the rst evidence of subtle cardiac
dysfunction in epilepsy patients.50
3. Chronic cardiac changes in epilepsy
3.1. Heart rate variability (HRV)
Heart rate variability can be used as a tool to show information on
the functional state of the autonomic nervous system. HRV is a
mirror of neuronal inuences on the cardiac pacemaker as one of the
important functions of the autonomic nervous system. Reduced HRV
has been established to be an increased risk of death in acute
myocardial infarction and in patients with diabetic neuropathy. But
various diseases are accompanied by a loss of ANS functionality and
therefore HRV can be used in health risk stratication.51
The physiologic uctuations of the heart rate are dened by
intrinsic oscillators at three different frequencies. These three main
frequency components in HRV reect the sympatho-vagal
balance.52
1. Respiratory sinus arrhythmia (RSA) is the most important high
frequency oscillator at 0.25 Hz. RSA is dened as the high
frequency (HF) spectral component and considered as a marker
of vagal modulation. RSA is heart rate variability in synchrony
with respiration. The RR interval is shortened during inspiration and prolonged during expiration. This is a biologic
phenomenon that is thought to have a positive inuence on
gas exchange by optimal ventilation/perfusion matching with
low energy expenditure.
2. In the medium frequency 0.1 Hz the Mayer waves are most
important. The rhythm corresponding to Mayer waves is dened
as the low frequency (LF) component and considered as an
indicator of sympathetic activation. This rhythm originates from
the baroreceptor loop.
3. The very low frequency (VLF) component at 0.05 Hz is dened
by thermoregulation, combined with humoral factors and other
slow components.
Heart rate variability was found to be lower in patients with
chronic refractory epilepsy, possibly resulting from parasympathetic or vagal reduction. This can make patients more susceptible
to tachycardia and brillation and possibly SUDEP.53,54
Impaired baroreex function was observed in a study of Dutsch
et al. in patients with temporal lobe epilepsy.55 The impaired
function can be another sign of autonomic instability in these
epileptic patients and a contributing factor in cardiac arrhythmias.
Serious heart rate oscillations in the postictal phase were noted
in a few patients.56 Although, they occur in a minority of patients,
they could be a potential risk factor for SUDEP.
3.2. AED and HRV
Heart rate variability seems to be different in treated patients
compared to untreated. It is possible that treatment of seizures
prevents detrimental effects on autonomic cardiac control.
Hallioglu et al. found a signicant difference in children treated
with valproic acid, oxcarbazepine or phenobarbital and children
without treatment. In the treated group better HRV was found.
These results indicate that patients without anti-epileptic drug
treatment have suppressed parasympathetic activity.57 But
treatment can also have a negative effect on HRV. A suppressive
effect of carbamazepine on both parasympathetic and sympathetic
cardiac functions was found in newly diagnosed epileptic
patients.58 Lossius et al. looked at autonomic parameters after
discontinuation of monotherapy, they found an increase of both
parasympathetic and sympathetic functions, demonstrated by
spectral analysis of HRV.59
3.3. Chronic and refractory epilepsy and HRV
Patients with longlasting and multiple seizures seem to be prone
to chronic dysfunction of autonomic cardiac control. In patients with
newly diagnosed (median time 27 months) and untreated epilepsy,
no difference was found in heart rate variability.60
Mukherjee et al.61 studied a cohort of well controlled and a
cohort of refractory patients and could show with a series of
autonomic tests that higher vasomotor tone, higher sympathetic
tone, lower parasympathetic tone and reactivity was found in the
group of refractory epilepsy patients. The observed dysautonomia
could be a predisposing factor to SUDEP. Chroni et al.62 could
demonstrate altered cardiovagal control in patients with chronic
epilepsy. They used simple neurophysiologic tests of the autonomic nervous system, Valsalva, Tilt-test, RR interval in normal
and deep breathing and sural nerve conductance to show a chronic
effect of epilepsy on the autonomous nervous system. Sathyaprabha et al.63 used heart rate and blood pressure measurements in
K. Jansen, L. Lagae / Seizure 19 (2010) 455460
rest, after Valsalva and postural change. Autonomic dysfunction
was found in 56.3% of the patients with chronic refractory epilepsy,
compared to a control group. In their study the dysfunction of the
autonomic system was more severe if the epilepsy was longer
lasting.
Ansakorpi et al.64,65 looked at refractory TLE patients to
demonstrate interictal autonomic dysfunction in response to
certain stimuli. He used newer analysis methods to demonstrate
altered complexity of heart rate in refractory epilepsy patients.
Ronkainen et al.66 found loss of HRV and suppressed circadian
dynamics in TLE, as well in controlled as in refractory patients.
In children with refractory epilepsy, the same arguments for a
chronic autonomic dysfunction are found. Heart rate abnormalities
were noted in children and adolescents with complex partial
seizures. The abnormalities were much more frequent compared
to adults and occurred in 98% of the complex partial seizures. Heart
rate variability also seems to be lower in children with chronic
refractory epilepsy, possibly resulting from parasympathetic or
vagal reduction. This can make patients more susceptible to
tachycardia and brillation54 (Harnod).
3.4. Vagal nerve stimulation (VNS) and HRV
The vagal nerve consists for 80% out of afferents and 20% of
efferents. Vagal efferents originate in the nucleus ambiguus and
DMN of the vagus. Cell bodies in the nucleus ambiguus send special
visceral efferent bers to the striated muscle bers of palate,
pharynx, larynx and esophagus. Cell bodies in the DMN send
general efferents to the heart, lungs and gastro-intestinal tract.
Afferent bers originate in the end organs: heart, lungs and gastrointestinal tract. These cells project axons to the nucleus tractus
solitaries (NTS), which then project to hypothalamus, amygdale,
dorsal raphe and thalamus. Vagal nerve stimulation produces
evoked potentials recorded from the cerebral cortex, the hippocampus, the thalamus, and the cerebellum. Most of the cardiovagal
bers run through the right vagus nerve, so stimulation of the left
vagus in the treatment of epilepsy is preferred to avoid potential
detrimental effects on heart rhythm.67 These structures in turn
synapse throughout the cerebral cortex and seem to have an
overall inhibitory effect. This was supported by the study of BenMenachem et al.68 who showed an increase of GABA in the CSF in
patients with VNS and a decrease of the excitatory aspartate.
For a long time, stimulation of the vagal nerve with VNS was
thought to have no effect on cardiac action. In contrast, Frei and
Osorio69 showed that left vagal nerve stimulation has complex
effects on instantaneous heart rate and heart rate variability with
large interindividual variability. They found different cardiac
chronotropic effects, either bradycardia or tachycardia, immediately followed by bradycardia during stimulation. HRV was found
to be increased or decreased.
The recent work of Stemper and Devinsky70 showed that VNS
inuences both sympathetic and parasympathetic cardiac regulations. The variability of the observed responses in patients treated
with VNS illustrates the interplay of divers afferent information
and central inuences.
4. Conclusion
There is growing evidence for the importance of the involvement of the central autonomic nervous system in epilepsy patients.
Short-term alteration of cardiac functions in patients with
seizures is caused by involvement of the central autonomic control
centers in seizure activity. Due to a hemispheric specic
localization of these control centers, the effect can give information
on lateralisation of the seizure. In return, autonomic symptoms in
seizure semeiology can give information on the localisation and
459
lateralisation of important autonomic centers in the central
nervous system as shown in the gure. Acute changes in cardiac
function during seizures include tachycardia, bradycardia up to
ictal asystole and more subtle conduction disorders. The pathophysiology of syncope in patients with epilepsy remains difcult.
Loss of consciousness can be due to cardiovascular complications
or involvement of the pontine reticular formation in seizure
propagation. Repetitive autonomic stimulation can lead to
structural damage of the heart. Cardiac ischemia as well as
myocardial brosis is already demonstrated in epilepsy patients.
The mechanism of SUDEP is multifactorial. We can identify three
different pathophysiologic triggers: acute cardiovascular changes
during seizures, tachyarrhythmias, bradyarrhythmias and ictal
asystole, neurogenic pulmonary edema and respiratory complications with central and obstructive apnea. Besides these triggers,
chronic epilepsy, drugs and genetics seem to be important
predisposing factors in patients with epilepsy.
In patients with longlasting epilepsy and multiple seizures,
there are arguments for a chronic dysfunction of the autonomic
nervous system. Heart rate variability is one of the markers used to
show information on the functional state of the autonomic nervous
system and is impaired in patients with longlasting epilepsy and
refractory seizures. Treatment of epilepsy with AED, not only VNS
can improve but also suppress heart rate variability. Early
recognition and possible prevention of these short- and longterm effects can prove to be of vital importance in the future.
References
1. Berntson GG, Cacioppo JT, Grossman P. Whither vagal tone. Biological Psychology
2007;74(December):295300.
2. Af A, Bouvier R, Buenerd A, Trouillas J, Mertens P. Development of the human
fetal insular cortex: study of the gyration from 13 to 28 gestational weeks. Brain
Structure & Function 2007;212:33546.
3. Benarroch EE. The central autonomic network: functional organisation, dysfunction, and perspective. Mayo Clinic Proceedings 1993;68:9881001.
4. Ostrowsky K, Maglin M, Ryvlin P, Isnard J, Guenot M, Mauguie`re F. Representation of pain and somatic sensation in the human insula: a study of responses to
direct electrical cortical stimulation. Cerebral Cortex 2002;12(April (4)):
37685.
5. Britton J, Bennaroch E. Seizures and syncope, anatomic basis and diagnostic
considerations. Clinical Autonomic Research 2006;16:1820.
6. Freeman R. Cardiovascular manifestations of autonomic epilepsy. Clinical Autonomic Research 2006;16:127.
7. Oppenheimer SM, Gelb A, Girvin JP, Hachinski VC. Cardiovascular effects of
human insular cortex stimulation. Neurology 1992;42(September (9)):1727
32.
8. Widdess-Walsh P, Kotagal P, Jeha L, Wu G, Burgess R. Multiple auras: clinical
signicance and pathophysiology. Neurology 2007;69:75561.
9. Janszky J, Fogarasi A, Toth V, Magalova V, Gyimesi C, Kovacs N, et al. Peri-ictal
vegetative symptoms in temporal lobe epilepsy. Epilepsy and Behavior
2007;11:1259.
10. Fogarasi A, Janszky J, Tuxhorn I. Autonomic symptoms during childhood partial
epileptic seizures. Epilepsia 2006;47:5848.
11. Baumgartner C, Lurger S, Leutmezer F. Autonomic symptoms during epileptic
seizures. Epileptic Disorders 2001;3:10316.
12. Mayer H, Benninger F, Urak L, Plattner B, Geldner J, Feucht M. EKG abnormalities
in children and adolescents with symptomatic temporal lobe epilepsy. Neurology 2004;63:3248.
13. Leutmezer F, Schernthaner C, Lurger S, Potzelberger K, Baumgartner C. Electrocardiographic changes at the onset of epileptic seizures. Epilepsia
2003;44(3):34854.
14. Di Gennaro G, Quarato P, Sebastiano F. Ictal heart rate increase precedes EEG
discharge in drug-resistant mesial temporal lobe seizures. Clinical Neurophysiology 2004;115:116977.
15. Massetani R, Strata G, Galli R, Gori S, Gneri C, Limbruno U, et al. Alteration of
cardiac function in patients with temporal lobe epilepsy: different roles of EEG
ECG monitoring and spectral analysis of RR variability. Epilepsia 1997;38:
3639.
16. Schernthaner C, Lindinger G, Potzelberger K, Zeiler K, Baumgartner C. Autonomic epilepsy, the inuence of epileptic discharges on heart rate and rhythm.
Wiener Klinische Wochenschrift 1999;111:392401.
17. Epstein MA, Sperling MR, OConnor MJ. Cardiac rhythm during temporal lobe
seizures. Neurology 1992;42(1):503.
18. Freeman R, Schachter SC. Autonomic epilepsy. Seminars in Neurology
1995;15:15866.
460
K. Jansen, L. Lagae / Seizure 19 (2010) 455460
19. Galimberti CA, Marchioni E, Barzizza F, Manni R, Sartori I, Tartara A. Partial
epileptic seizures of different origin variably affect cardiac rhythm. Epilepsia
1997;37:7427.
20. Espinoza PS, Lee JW, Tedrow UB, Bromeld EB, Dworetzky BA. Sudden unexpected near death in epilepsy: malignant arrhythmia from a partial seizure.
Neurology 2009;72(19):17023.
21. Britton JW, Ghearing GR, Benarroch EE, Cascino GD. The ictal bradycardia
syndrome: localization and lateralization. Epilepsia 2006;47:73744.
22. Healy B, Peck J. Bradycardia induced from stimulation of the left versus right
central nucleus of the amygdala. Epilepsy Research 1997;28:1014.
23. Oppenheimer SM, Wilson JX, Guiraudon C, Cechetto DF. Insular cortex stimulation produces lethal cardiac arrhythmias: a mechanism of sudden death?
Brain Research 1991;550(May (1)):11521.
24. Tinuper P, Bisulli F, Cerullo A, Carcangiu R, Marini C, Pierangeli G, et al. Ictal
bradycardia in partial epileptic seizures: autonomic investigation in three cases
and literature review. Brain 2001;124:236171.
25. Rocamora R, Kurthen M, Lickfett L, Von Oertzen J, Elger CE. Cardiac asystole in
epilepsy: clinical and neurophysiological features. Epilepsia 2003;44:17985.
26. Altenmuller DM, Zehender M, Schulze-Bonhage A. High grade atrioventricular
block triggered by spontaneous and stimulation induced epileptic activity in
the left temporal lobe. Epilepsia 2004;45:16404.
27. Rugg-Gunn FJ, Simister RJ, Squirrell M, Holdright DR, Duncan JS. Cardiac arrhythmias in focal epilepsy: a prospective long term study. Lancet 2004;364(December
(9452)):22129.
28. Nei M, Ho RT, Sperling R. EKG abnormalities during partial seizures in refractory
epilepsy. Epilepsia 2000;41(5):5428.
29. Opherc C, Coromilan J, Hirsch LJ. Heart rate and EKG changes in 102 seizures:
analysis of inuencing factors. Epilepsy Research 2002;52:11727.
30. Tomson T, Nashef L, Ryvlin P. Sudden unexpected death in epilepsy: current
knowledge and future directions. Lancet Neurology 2008;7:102131.
31. Nashef L, Fish DR, Garner S, Sander SW, Shorvon SD. Sudden death in epilepsy: a
study of incidence in a young cohort with epilepsy and learning difculty.
Epilepsia 1995;36:118794.
32. Langan Y, Nolan N, Hutchinson M. The incidence of sudden unexpected death in
epilepsy in South Dublin and Wicklow. Seizure 1998;7:33558.
33. Opeskin K, Berkovic S. Risk factors for sudden unexpected death in epilepsy: a
controlled prospective study based on coroners cases. Seizure 2003;12:45664.
34. Nei M, Ho RT, Abou-Khalil BW, Drislane FW, Liporace J, Romeo A, et al. EEG and
EKG in sudden unexplained death in epilepsy. Epilepsia 2004;45(4):33845.
35. Leung H, Kwan P, Elger CE. Finding the missing link between ictal bradyarrythmia, ictal asystole and sudden unexpected death in epilepsy. Epilepsy and
Behavior 2006;9:1930.
36. Nashef L, Garner S, Sander JW, Fish DR, Shorvon SD. Circumstances of death in
sudden death in epilepsy. Journal of Neurology Neurosurgery and Psychiatry
1998;64:34952.
37. Langan Y, Nashef L, Sander JW. Sudden unexpected death in epilepsy: a series of
witnessed deaths. Journal of Neurology Neurosurgery and Psychiatry
2000;68:2113.
38. Schuele S, Bermeo A, Locatelli ER, Burgess RC, Luders HO. Ictal asystole: a benign
condition? Epilepsia 2008;49:16871.
39. Schuele SU, Bermeo AC, Alexopoulos AV, Locatelli ER, Burgess RC, Dinner DS,
et al. Video-electrographic and clinical features in patients with ictal asystole.
Neurology 2007;69:43441.
0. Hilz MJ, Devinsky O, Doyle W, Mauerer A, Dutsch M. Decrease of sympathetic
cardiovascular modulation after temporal lobe epilepsy surgery. Brain
2002;125:98595.
41. Baumann A, Audibert G, McDonnell J, Mertes PM. Neurogenic pulmonary
edema. Acta Anaesthesiologica Scandinavica 2007;51:44755.
42. Sedy J, Zicha J, Kunes J, Jendelova P, Sykova E. Mechanisms of neurogenic
pulmonary edema development. Physiological Research 2008;57(4):499506.
43. Cohen HA, Ashkenazi H, Barzilai A, Lahat E. Acute nocturnal laryngospasm in
children: a possible epileptic phenomenon. Journal of Child Neurology
2000;15(3):2024.
44. Watanabe K, Hara K, Hakamada S, Negoro T, Sugiura M, Matsumoto A, et al.
Seizures with apnea in children. Pediatrics 1982;70:8790.
45. Nelson DA, Ray CD. Respiratory arrest from seizure discharges in limbic system.
Archives of Neurology 1986;19:199207.
46. Hindocha N, Nashef L, Elmslie F, Birch R, Zuberi S, Al-Chabali A, et al. Two cases
of sudden unexpected death in epilepsy in a GEFS+ family with an SCN1A
mutation. Epilepsia 2008;49:3605.
47. Natelson BH, Suarev RV, Terrence CF, Turizo R. Patients with epilepsy who die
suddenly have cardiac disease. Archives of Neurology 1998;55:85760.
48. Woodruff BK, Britton JW, Tigaran S, Cascino GD, Burritt MF, McConnell JP, et al.
Cardiac troponin levels following monitored epileptic seizures. Neurology
2003;60:16902.
49. Tigaran S, Molgaard H, McClelland R, Dam M, Jaffe AS. Evidence of cardiac
ischemia during seizures in drug refractory epilepsy patients. Neurology
2003;60:4925.
50. Alehan F, Erol I, Cemil T, Bayraktar N, Ogus E, Tokel K. Elevated CK-MB mass and
plasma brain-type natriuretic peptide concentrations following convulsive
seizures in children and adolescents: possible evidence of subtle cardiac
dysfunction. Epilepsia 2009;50(4):76075.
51. Task Force of The European Society of Cardiology and The North American
Society of Pacing and Electrophysiology. Heart rate variability: standards of
measurement, physiological interpretation and clinical use. European Heart
Journal 1996;17:35481.
52. Malik M, Camm AJ. Components of heart rate variability: what they really mean
and what we really measure. American Journal of Cardiology 1993;72:
8212.
53. Tomson T, Ericson M, Ihrman C, Lindblad LE. Heart rate variability in patients
with epilepsy. Epilepsy Research 1998;30(1):7783.
54. Harnod T, Yang CCH, Hsin YL, Shieh KR, Wang PJ, Kuo TB. Heart rate variability
in children with refractory generalized epilepsy. Seizure 2008;17(4):297301.
55. Dutsch M, Hilz M, Devinsky O. Impaired baroreex function in temporal lobe
epilepsy. Journal of Neurology 2006;253:13008.
56. Mayer H, Benninger F, Urak L, Plattner B, Geldner J, Feucht M. EKG abnormalities
in children and adolescents with symptomatic temporal lobe epilepsy. Neurology 2004;63:32432.
57. Hallioglu O, Okuyaz C, Mert E, Makharoblidze K. Effects of antiepileptic drug
therapy on heart rate variability in children with epilepsy. Epilepsy Research
2008;79:4954.
58. Persson H, Ericson M, Tomson T. Carbamazepine affects autonomic cardiac
control in patients with newly diagnosed epilepsy. Epilepsy Research
2003;57(1):6975.
59. Lossius M, Erikssen JE, Mowinckel P, Gulbrandsen P, Gierstad L. Changes in
autonomic cardiac control in patients with epilepsy after discontinuation of
antiepileptic drugs: a randomized controlled withdrawal study. European
Journal of Neurology 2007;14:10228.
60. Persson H, Ericson M, Tomson T. Heart rate variability in patients with untreated epilepsy. Seizure 2007;16:5048.
61. Mukherjee S, Tripathi M, Chandra PS, Yadav R, Choudhary N, Sagar R, et al.
Cardiovascular autonomic functions in well-controlled and intractable partial
epilepsies. Epilepsy Research 2009;85(August (23)):2619.
62. Chroni E, Sirrou V, Trachani E, Sakellaropoulos GC, Polychronopoulos P. Interictal alterations of cardiovagal function in chronic epilepsy. Epilepsy Research
2008;83(23):11723.
63. Sathyaprabha TN, Satishchandra P, Netravathi K, Sinha S, Thennarasu K, Raju TR.
Cardiac autonomic dysfunctions in chronic refractory epilepsy. Epilepsy Research 2006;72:4956.
64. Ansakorpi H, Korpelainen JT, Huikuri HV, Tolonen U, Myllyla VV, Isojarvi JI.
Heart rate dynamics in refractory and well controlled temporal lobe epilepsy.
Journal of Neurology Neurosurgery and Psychiatry 2002;72(1):2630.
65. Ansakorpi H, Korpelainen JT, Suominen K, Tolonen U, Myllyla VV, Isojarvi JI.
Interictal cardiovascular autonomic responses in patients with temporal lobe
epilepsy. Epilepsia 2000;41(1):427.
66. Ronkainen E, Ansakorpi H, Huikuri HV, Myllyla VV, Isojarvi JI, Korpelainen JT.
Suppressed circadian heart rate dynamics in temporal lobe epilepsy. Journal of
Neurology Neurosurgery and Psychiatry 2005;76(10):13826.
67. Rutecki P. Anatomical, physiological, and theoretical basis for the antiepileptic
effects of vagus nerve stimulation. Epilepsia 1990;31(Suppl. 2):S16.
68. Ben-Menachem E, Hamberger A, Hedner T, Hammond EJ, Uthman BM, Slater J,
et al. Effects of vagus nerve stimulation on amino acids in the CSF of patients
with partial seizures. Epilepsy Research 1995;20:2217.
69. Frei MG, Osorio I. Left vagus nerve stimulation with the neurocybernetic
prosthesis has complex effects on heart rate and on its variability in humans.
Epilepsia 2001;42(8):100716.
70. Stemper B, Devinsky O, Haendl T, Welsch G, Hilz MJ. Effects of vagus nerve
stimulation on cardiovascular regulation in patients with epilepsy. Acta Neurological Scandinavica 2008;117:2316.
Anda mungkin juga menyukai
- 323 Farhan Marzuki Ikatan Dokter Indonesia15673531235d6be923de939 PDFDokumen1 halaman323 Farhan Marzuki Ikatan Dokter Indonesia15673531235d6be923de939 PDFFarhan MarzukiBelum ada peringkat
- Farhan Marzuki: Replace With Occupation or Position HeldDokumen2 halamanFarhan Marzuki: Replace With Occupation or Position HeldFarhan MarzukiBelum ada peringkat
- Rekap Pasien Ortho 17 Agustus 2015Dokumen4 halamanRekap Pasien Ortho 17 Agustus 2015Farhan MarzukiBelum ada peringkat
- CV in EnglishDokumen5 halamanCV in EnglishAyah MochieBelum ada peringkat
- New PmiDokumen2 halamanNew PmiFarhan MarzukiBelum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5782)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (72)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Bacillus Clausii Is A RodDokumen9 halamanBacillus Clausii Is A RodGrax DeeBelum ada peringkat
- Tog Journal 2016 PDFDokumen61 halamanTog Journal 2016 PDFSai Khin Aung Tint100% (1)
- Do I Have Chronic Fatigue SyndromeDokumen10 halamanDo I Have Chronic Fatigue SyndromecassseaBelum ada peringkat
- Cape Biology 2014 U2 p1Dokumen12 halamanCape Biology 2014 U2 p1FiveLimaRomeo100% (4)
- 1 - MyopiaDokumen9 halaman1 - MyopiaSpislgal PhilipBelum ada peringkat
- ZVora Top 20 Inicet PDFDokumen26 halamanZVora Top 20 Inicet PDFThe Two Kids MomBelum ada peringkat
- Fluid & Electrolytes ManagementDokumen18 halamanFluid & Electrolytes ManagementSh ReyaBelum ada peringkat
- Prenatal Development and GeneticsDokumen23 halamanPrenatal Development and GeneticsJoseph Barnes100% (1)
- SB5 - Revision - Summary Filled inDokumen1 halamanSB5 - Revision - Summary Filled inSiaBelum ada peringkat
- Redox-Genome Interactions in Health and DiseaseDokumen650 halamanRedox-Genome Interactions in Health and Diseaseaurea_ramBelum ada peringkat
- Roles of Vitamins in Stem Cells: Cellular and Molecular Life Sciences May 2020Dokumen22 halamanRoles of Vitamins in Stem Cells: Cellular and Molecular Life Sciences May 2020Chanda DajaniBelum ada peringkat
- Time - Special Edition - The Future of Medicine, 2023Dokumen100 halamanTime - Special Edition - The Future of Medicine, 2023carlos samboniBelum ada peringkat
- Mi Rna Scope BrochureDokumen3 halamanMi Rna Scope BrochurewendyBelum ada peringkat
- GMO - Friend or Foe?Dokumen17 halamanGMO - Friend or Foe?jpfarreBelum ada peringkat
- EUROLINE Myositis Profi Le 3 (IgG) SummaryDokumen2 halamanEUROLINE Myositis Profi Le 3 (IgG) SummaryShahid Hussain100% (1)
- 5 Health As A Social InstitutionDokumen34 halaman5 Health As A Social InstitutionSze Yinn PikaaBelum ada peringkat
- Explore PharmacologyDokumen23 halamanExplore PharmacologyAndrea CarmenBelum ada peringkat
- Thromboxane A2Dokumen16 halamanThromboxane A2Concepcion R. Aquino0% (1)
- 4727 Whatman DNA - OmniSwab Appnote - v15Dokumen6 halaman4727 Whatman DNA - OmniSwab Appnote - v15Alejandra Torres100% (1)
- Inno-Lipa HBV Brochure 0Dokumen2 halamanInno-Lipa HBV Brochure 0yayladag1970Belum ada peringkat
- Physical and Occupational Therapy Licensure Exam ReviewDokumen7 halamanPhysical and Occupational Therapy Licensure Exam ReviewKennie Ramirez100% (2)
- EUA Roche Elecsys IfuDokumen5 halamanEUA Roche Elecsys IfuFadhila N HandayaniBelum ada peringkat
- 05-02-Genetika MikroorganismeDokumen48 halaman05-02-Genetika MikroorganismeKinad DanikBelum ada peringkat
- Clinical Success of Deproteinization in Hypocalcified Amelogenesis ImperfectaDokumen7 halamanClinical Success of Deproteinization in Hypocalcified Amelogenesis ImperfectaMelisa GuerraBelum ada peringkat
- Molecular and Cellular Endocrinology: Biff F. Palmer, Deborah J. CleggDokumen7 halamanMolecular and Cellular Endocrinology: Biff F. Palmer, Deborah J. CleggEgy SunandaBelum ada peringkat
- Mineralocorticoids: Shajeer. SDokumen42 halamanMineralocorticoids: Shajeer. SShajeer SalimBelum ada peringkat
- A Geroscience Perspective On Immune Resilience and Infectious Diseases - A Potential Case For MetforminDokumen20 halamanA Geroscience Perspective On Immune Resilience and Infectious Diseases - A Potential Case For MetforminAna Raquel Realista Coelho Dos Santos PedrosaBelum ada peringkat
- Thyrotoxicosis and Graves DiseaseDokumen25 halamanThyrotoxicosis and Graves DiseaseMeekel SusikuBelum ada peringkat
- Pathophysiology of Type 1 DiabetesDokumen14 halamanPathophysiology of Type 1 DiabetesBoBelum ada peringkat
- Dr. Daniel H. Bessesen: The Biology of ObesityDokumen58 halamanDr. Daniel H. Bessesen: The Biology of ObesityNational Press FoundationBelum ada peringkat