(OS 213) LEC 20 Congestive Heart Failure in Children
Diunggah oleh
nilsJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
(OS 213) LEC 20 Congestive Heart Failure in Children
Diunggah oleh
nilsHak Cipta:
Format Tersedia
OS 213: Circulation and Respiration
LEC 20: CONGESTIVE HEART FAILURE IN CHILDREN
Exam # 1 | Dr. Connie Sison | August 1, 2012
OUTLINE
I. Introduction
II. Pathophysiology of Heart Failure
A. Dangerous Compensatory Mechanisms
III. Clinical Manifestations
IV. Diagnosing Heart Failure in Children
A. History of Newborn and Infants
B. History of Children and Young Adults
C. Physical Examination
D. Heart Failure Classification in Children
E. Causes of Heart Failure in Children
V. Management and Treatment
A. Non-Pharmacologic
B. Surgical
C. Pharmacologic
VI. Summary
Note: We did not include the x-ray frames and pictures shown in the lecture
since they were the same as those used in lecture 09 (Overview of Heart
Diseases in Children). Please refer to the pictures under the Congestive Heart
Failure section of the said transcription. Thank you.
o Nice to know: Cardiovascular disease can be associated with
increased CO as occurs during infection and sepsis, or
decreased CO, as in cardiomyopathy and heart failure (2014)
A. Dangerous compensatory mechanisms
When there is a decrease in the oxygen delivery by the heart
(CO), PHYSIOLOGIC COMPENSATORY MECHANISMS come into
play to make sure that vital organs get enough oxygen (i.e.
augment O2 delivery).
o Neurohumoral responses
Sympathetic Nervous System Stimulation causing increased cardiac
rate and contractility
Renin-angiotensin-aldosterone system: can be activated by beta-1
receptors to produce Angiotensin II
Other Mediators; Arginine Vasopressin (AVP) = antidiuretic hormone
(ADH)
I. INTRODUCTION
Congestive Heart Failure
ULTIMATE GOAL: RECOGNIZE and initially treat a CHILD in
HEART FAILURE (HF)
A clinical syndrome in which the heart is unable to pump enough
blood to meet its needs, to dispose of venous return adequately,
or a combination of the two
Definition: inadequate oxygen delivery by the heart or circulatory
system to meet the demands of the body
II. PATHOPHYSIOLOGY OF HEART FAILURE
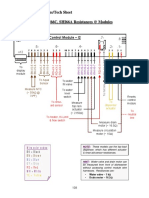
Figure 1. Factors affecting Oxygen delivery. Hb = hemoglobin,
CO = cardiac ouput, HR = heart rate
Recall: Cardiac output (CO) is the volume of blood being pumped
by the heart, in particular by a left (LV) or right ventricle (RV) in 1
min.; also, CO is the combined sum of output from the RV and the
output from LV during systole. (on the average, CO for male =
5 L/min, CO for female = 4.5 L/min) . (2014)
Supposing Cardiac output okay but child anemic, oxygen delivery
still inadequate High Output Cardiac Failure
CO depends on Heart Rate (HR) and Stroke Volume (CO = HR x
SV). Stroke volume (SV), which is the volume of blood pumped
from one ventricle of the heart with each beat, depends on
preload, contractility and afterload.
o Preload end-diastolic volume (EDV) - degree to which the
ventricles are stretched prior to contracting
o Contractility (especially of the LV) inotropy - intrinsic ability
of the heart to contract independent of preload and afterload;
how intense the ventricle can propel blood
o Afterload - resistance to which the LV contracts; measure the
tension produced by LV in order to contract lower afterload
higher stroke vol higher CO; reflection of PVR
o SV = EDV ESV [ESV = end-systolic volume]
o Ejection fraction = SV/EDV; Ejection fraction is the fraction of
blood pumped out of ventricles with each heartbeat.
In heart failure, the problem lies in the cardiac output. If CO is
compromised (i.e. when there is a shunt), heart may fail to deliver
enough blood.
MARKY, JAMES, ALLIE
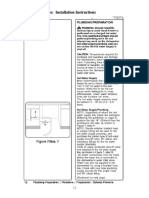
Figure 2. Neurohormonal Responses w/c compensate for
decreased CO.
overcompensations; may not be good for the heart and may
lead to heart failure
Increased Preload (remember Frank-Starling mechanism)
o Salt and water retention (expansion of extracellular volume)
o Redistribution of renal flow
o Sympathetic stimulation
o Aldosterone
o AVP/ADH
o possibly, heart will dilate
Increased Cardiac Rate and Contractility
o By means of sympathetic Stimulation
o alpha-1 receptor activation peripheral vasoconstrict
o beta -1 tachycardia, arrhythmia, salt and water retention (Via
Juxtaglomerular (JG) cells)
Increased Afterload
o Increased in peripheral vascular resistance
o Sympathetic stimulation
o Angiotensin II (potent vasoconstrictor)
o AVP/ADH
Myocardial hypertrophy/LV remodeling: ultimately associated w/
alterations in cellular & subcellular phenotype (necrosis, fibrosis)
reducing contractility
o Increased in peripheral vascular resistance
Catecholamine
Aldosterone
Angiotensin II
III. CLINICAL MANIFESTATIONS
Increased Preload (and inability of heart to deal with increased
preload)
o Pulmonary Congestion
Tachypnea, Dyspnea, Orthopnea
o Systemic Congestion heart cannot dispose of venous return
properly
Hepatomegaly (chronic passive congestion), Bipedal Edema
o Pallor
Increased Sympathetic Stimulation
UPCM 2016 B: XVI, Walang Kapantay!
1 of 4
OS 213
LEC 0X: CONGESTIVE HEART FAILURE IN CHILDREN
o Tachycardia
o Diaphoresis (excessive sweating)
o Arrhythmia
Increased Afterload
o Vasoconstriction cold extremities because of peripheral
vasoconstriction brain heart kidney priority, warmth means
good perfusion less severe heart failure
To perfuse distal organs
o Cold extremities (due to peripheral vasoconstriction)
o Pallor
Hallmark of Heart Failure
Decreased O2 delivery (signs and symptoms) EASY
FATIGABILITY (intermittency of feeding) SHOCK death
Feed hingal tigil 1-2 hours before volume of milk is consumed
sign of easy fatigueability
IV. DIAGNOSING HEART FAILURE IN CHILDREN
A. History Taking in Newborn and Infants
Birth and Maternal History
o possible predisposition to congenital causes of HF
Intermittent feeding
o feeding may be labored or impossible due to rapid breathing
(i.e. in pulmonary congestion)
o slow or poor feeding
Normally, an infant can consume milk equivalent to [age of
baby in months + 1] ounces of milk in less than 30 minutes
every 2 to 3 hours) [1 oz = 30 ml]
o Easy fatigability (poor eating less energy)
Diaphoresis
o Due to the stimulation of sympathetic NS
o Can be observed especially during feeding
o Excessive sweating even on cool and temperate environments
(confirm this with the childs parents; environment might just
really be warm)
o More evident on the forehead
Poor weight gain or weight loss
o body needs more energy to enhance cardiac output
Relative to the other child in the same stage of development
o Refer to growth charts
Repeated respiratory tract infection/chronic cough
o More than 8 instances per year sign of HF
o possible compression of lymphatic drainage bronchial airways
due to enlarged PA
Agitation & unusual irritability
o Perfusion of the brain is compromised
o Irritability due to organic cause: rapid breathing; childs does
not feed not well
B. History Taking in Children and Young Adults
Exercise intolerance/easy fatigability (hallmark of CHF)
o ask the usual activities, compare it to his/her peers
Tachypnea, shortness of breath, Dyspnea pulmonary
congestions
Abdominal pain or distention (e.g. Hepatomegaly, Splenomegaly)
Orthopnea & Paroxysmal Nocturnal Dyspnea (in older children)
o Venous return higher in supine position
o (heart cannot cope with increased preload) pressure
reflected back to lungs pulmonary congestion
Chronic cough
Puffy eyelids, swollen feet
o not as common in children (but note that edema in infants is
mostly in the back due to supine position) as in older adults
o points to renal in etiology especially in children (2014)
C. Physical Examination
General Survey
Failure to thrive (FTT)
o Evaluated either by a low weight for the child's age, or by a low
rate of increase in the weight
Wasting or acute malnutrition
o Caused by an extremely low energy intake, nutrient losses due
toinfection, or a combination of the two
Chromosomal syndromes
o In infants w/ Downs Syndrome, 50% may have cardiac
problems, most of w/c have CAVSD (Complete Atrio-Ventricular
Septal Defect)
o Edwards syndrome (Trisomy 18) 98% will have congenital
heart disease
o So due to such statistics, it is recommended to have a 2D echo
in such cases even if no abnormalities were heard in
ausculation
Color: pale, cyanotic (can help narrow down possible CHDs),
jaundiced (i.e. in liver congestion)
Anxious/irritable compromised oxygen to the brain
Signs Diaphoresis - sweat on the forehead sympathetic
activation
Signs of Cardiorespiratory distress
o Dyspnea, Shortness of breath, Tachypnea
o Subcostal Retractions = Harrisons groove (make sure to note
its presence or absence in routine PE) which indicates poor lung
compliance. But this can also be sings of asthma and
pneumonia
Vital Signs
Sinus tachycardia results in decreased cardiac output
o Sustained CR > 220 /min infants
o Sustained CR > 150/min older children
CR = cardiac rate
Consider Supraventricular Tachycardia
o Abnormal increase in HR HF
o There are instances when tachycardia is the cause of HF
arryhtmia causing HF
o Results in decreased cardiac output
Diastolic filling time decreased in tachycardia decreased stroke
volume
Decreased preload
Hypotension
o May lead to shock
Tachypnea
o Pediatric Respiratory Rates (RR)
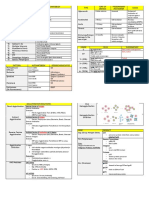
Table 1. Normal breath rates per pediatric age group
Age
Rate (breaths/min)
Infant (birth1 yr)
3060
Toddler (13 yrs)
Preschooler (36 yrs)
2440
2234
School-age (612 yrs)
2440
Adolescent (1218 yrs)
1216
o It is normal for infant to have a RR of 60 breaths/min. Adults
with the same RR are already tachypneic.
Cardiac Examination
Precordial activity (possible LVH)
Prominent S3 poor ventricular compliance (Kentucky gallop
vs. S4 Tennessee)
Heart murmurs
Lung Examination
Look for signs of pulmonary congestion
oxygenation and ventilation)
o Tachypnea and subcostal retractions
o Labored respiratory effort
o Nasal flaring
(compromised
use of accessory muscles of respiration
MARKY, JAMES, ALLIE
UPCM 2016 B: XVI, Walang Kapantay!
2 of 4
OS 213
LEC 0X: CONGESTIVE HEART FAILURE IN CHILDREN
o Grunting
infants; Dyspnea on exertion in older children
(relative to his/her peers) NO Growth failure;
in an attempt to keep the alveoli open (2014)
increase end alveolar pressure
o Hacking cough
bronchial mucosal edema
CLASS III
Marked tachypnea or diaphoresis with feeds or
exertion; Prolonged feeding times
Growth failure from CHF;
Symptoms in mild activities combing hair,
taking a bath*
CLASS IV
Symptoms at rest with tachypnea, retractions,
grunting or diaphoresis
o Rales or crackles
clicking, rattling, or crackling noises
unusual in infants;
may suggest concurrent pneumonia
(bibasal rales because of gravity)
o Wheezing
continuous, coarse, whistling sound
congestion of airway due to pulmonary edema
not exclusive to asthma; can be also cardiac in etiology; but all who
have asthma have wheezing
wheezing despite giving beta-agonists = most probably cardiac in
origin
Abdominal Examination
Hepatomegaly
Ascites (accumulation of fluid in the peritoneal cavity)
Splenomegaly
o PE: dullness to percussion over Traube's space
o NOT associated with CHF but due to hematologic disorders like
beta-thalassemia and leukemia
Examination of the Extremities
Cool extremities:
o warm extremities = well-perfused; most probably, heart does
well
Peripheral pulse
Capillary refill;
o While legs are raised the legs, blood flow should return in < 2
seconds after blanching
Peripheral edema
o Extremely rare in infants; edema found only in dependent area
o Edema usually due to presence of TR (Tricuspid Regurgitation)
o Systemic congestion-dependent edema in adults
HEENT (Head-Eye-Ear-Nose-Throat) Examination
Neck vein distention/engorgement
Difficult to evaluate, small in children; not too common in infants;
in acquired heart disease
o Constrictive pericarditis
o Pericardial effusion
Facial edema/Puffy eyelids
o Again, usually point to a renal etiology in infants
The three-minute examination for CHF (from 2013)
Take sleeping or resting respiratory rate for ONE FULL MINUTE.
Note the patients general appearance - distress, color, perfusion
Palpate forehead for diaphoresis.
Check capillary refill.
Examine tibial and other areas for edema.
Palpate precordium and assess its activity.
Examine the abdomen for hepatomegaly.
Palpate the pulses right arm and leg pulse simultaneously;
carotid pulses
Auscultation:
o Head and abdomen bruits
o Heart murmurs or gallops
o Lungs rales or rhonchi
D. Heart Failure Classification in Children
Difficult
Range of ages and developmental stages
Variety of etiology (myocardial dysfunction, left to right shunt)
Table 2. Ross Classification of Heart Failure in Infants
CLASS I
Presence of structural heart disease but NO
limitations or symptoms
CLASS II
Mild tachypnea or diaphoresis with feeding in
MARKY, JAMES, ALLIE
Evaluation of CHF in Children
o Medical history
o Physical examination
o CXR (Chest X-Ray); Echocardiography (2D-Echo); ECG
(Electrocardiography)
Heart size ct ratio > 0.55
Cephalization vessels at upper lung recruited to aid
circulation and become more evident
o ABG (Arterial blood Gas) when patient is in respiratory
diseases; how much ventilation is needed
o Low bicarb low pH metabolic acidosis pO2 pCO2
o CBC (Complete Blood Count); RBS (Random Blood Sugar);
Electrolytes
Associated and aggravating factors in CHF in children
o Fever*
o Infection*
o Fluid losses*
o Electrolyte imbalance
o Anemia
o Dysrhythmia/Arrhythmia
*will also manifest tachycardia (HR); address or control these
first before addressing HF
E. Causes of Heart Failure in Children
At Birth
Structural abnormalities
o Hypoplastic Left Heart Syndrome (HLHS)
o Volume overload lesions
Tricuspid Regurgitation
Pulmonary Regurgitation
Systemic Arteriovenous Fistula
Heart rate abnormalities
o Supraventricular Tachycardia
o Congenital Complete Heart Block
Myocarditis
1st Week of Life
Structural abnormalities
o TGA
o PDA (premature infants)
o HLHS
o TAPVR (Total Anomalous Pulmonary Venous Return; w/
obstruction)
o Critical AS (Aortic Stenosis), Coarctation of Aorta, Interrupted
Aortic Arch
o Critical PS (Pulmonary Stenosis)
1st Two Months of Life
Decreased pulmonary vascular resistance (due to increased flow
of blood to the lungs) compared to the first weeks of life)
Structural abnormalities
o Left to Right Shunts
Aortic level shunt (e.g. PDA)
Ventricular level shunt (e.g. VSD)
Atrial level shunt (e.g. TAPVR)
o Left-sided obstructive lesions
o Others: Anomalous origin of LCA (Left Coronary Artery) from PA
(Pulmonary Artery)
UPCM 2016 B: XVI, Walang Kapantay!
3 of 4
OS 213
LEC 0X: CONGESTIVE HEART FAILURE IN CHILDREN
Pulmonary Abnormalities/Chronic Hypoxia (Right-Heart Failure)
o Increase pulmonary artery pressure; pose a higher resistance to
right ventricle
o CNS Hypoventilation
o Upper Airway Obstruction
o Broncho-Pulmonary Dysplasia
Heart Muscle Abnormalities
o Cardiomyopathy/EFE (Endocardial Fibroelastosis)
o Myocarditis
o Pompes diseases
Older Children
Acquired Heart Diseases
o Infective endocarditis
o Rheumatic fever & heart disease (5-15 y.o.)
o Myocarditis
o Cardiomyopathy
o Pericarditis
o Cor pulmonale
Congenital Heart Disease
o Unoperated end stage
o Pulmonary hypertension
o Post-operative heart failure
Others
o Infective endocarditis
o Dysrhythmias
o Systemic hypertension
Anemia
o Decrease Catecholamine/Sympathetic Effects
-BLOCKERS: Carvedilol
Prevent progressive cell death and structural deterioration
o ALDOSTERONE ANTAGONISTS
o -BLOCKERS
o ACE INHIBITORS
o ARBs (Angiotensin II Receptor Blockers)
o Substances which cause LV Remodeling and deterioration of
the heart
Sympathetic s
Aldosterone
Angiotensin II
VI. SUMMARY
Pathophysiology is basically similar to adult CHF.
Clinical manifestations and treatment are grounded on the same
principles as adult CHF.
Diagnosis of CHF is based on History and PE
Diagnosis of cause is based on presentation & age group
Chest x-ray, ECG, & echocardiogram are essential in diagnosis
and treatment of CHF.
Medical treatment is geared towards augmenting oxygen
delivery, decreasing oxygen demand, and tempering
compensatory mechanisms.
Surgery and/or cardiac catherization intervention is often
necessary for definitive treatment.
END OF TRANSCRIPTION
V. MANAGEMENT AND TREATMENT
GOALS:
o Augment oxygen delivery
o Temper physiologic (over)compensations
TYPES:
o Non-Pharmacologic
o Surgical
o Pharmacologic
A. Non-Pharmacologic
Bed rest; use high back-rest (or just carry the baby on its back);
use cardiac chair
O2; ventilatory support; pulmophysiotherapy
Thermoregulation
Appropriate fluid therapy
Nutritional support calories and K+ supplement
Treat associated problems first: anemia and infection (because
these may aggravate the manifestations of Heart Failure and
Heart Failure itself)
James: Kung may game manuod ng cinemalaya sa Diliman, sabihan
niyo ko! Tara, punta tayo!
Marky: Omg, Im scared that Nico will okray our formatting.
HEEHEE! AND TO THE TRANS COMM HEAD: HELLO, Queen Elizabeth
shall bear down the Hand of Justice. CHOS. :))
Allie: Trese Pwede, halloo. May alam ba kayong pwedeng pagpaprint-an ng t-shirt natin? Lampas isang taon na eh. Jejeje. Shameless
recommendation, ba: My Body is a Cage Peter Gabriel. Or the
Arcade Fire version.
B. Surgical
Definitive depends on the type of CHD (e.g. VSD closure, PDA
transection/ligation, arterial switch operation)
Palliative done to postpone surgery for 6 months until definitive
surgery can be done; a usual occurrence in PGH due to high costs
of definitive surgery; usually costs around 20k only (e.g.
pulmonary artery banding, man-made pulmonic valve stenosis)
C. Pharmacologic
Enhance Oxygen Delivery/Increase Cardiac Output
o Augment Myocardial Contractility (for acute HF)
DIGOXIN/LANOXIN
-AGONISTS: Dobutamine, Dopamine
BIPYRIDINES: Milrinone (an inotrope vasodilator)
Tempre compensatory mechanisms
o Decrease Preload/ Volume Overload
DIURETICS: Furosemide, Spirinolactone
VENOUS DILATORS: Nitroglycerin
o Decrease Afterload
ACE INHIBITORS: Captopril, Enalapril
BIPYRIDINES: Milrinone
ARTERIAL VASODILATORS: Nitroglycerin
MARKY, JAMES, ALLIE
UPCM 2016 B: XVI, Walang Kapantay!
4 of 4
Anda mungkin juga menyukai
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Segment2 - ZRYOBI R18MT Multiverktyg ManualDokumen3 halamanSegment2 - ZRYOBI R18MT Multiverktyg ManualnilsBelum ada peringkat
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Viii. Troubleshooting Circulation Pump - Water Switch Pump Nuisance TrippingDokumen4 halamanViii. Troubleshooting Circulation Pump - Water Switch Pump Nuisance TrippingnilsBelum ada peringkat
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- Beginners Python Cheat Sheet PCC AllDokumen26 halamanBeginners Python Cheat Sheet PCC Alljuan ruiz100% (2)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Segment44 - ZRYOBI R18MT Multiverktyg Manual PDFDokumen1 halamanSegment44 - ZRYOBI R18MT Multiverktyg Manual PDFnilsBelum ada peringkat
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Bosch Dishwasher Service Training Manual - Part7Dokumen4 halamanBosch Dishwasher Service Training Manual - Part7nilsBelum ada peringkat
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- IX. Wiring Diagrams/Tech Sheet Measuring SHU66C, SHI66A Resistances at ModulesDokumen4 halamanIX. Wiring Diagrams/Tech Sheet Measuring SHU66C, SHI66A Resistances at ModulesnilsBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Bosch Dishwasher Service Training Manual - Part1 PDFDokumen4 halamanBosch Dishwasher Service Training Manual - Part1 PDFnilsBelum ada peringkat
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Anvandarmanual Elektroniskt Kodlas Part15Dokumen2 halamanAnvandarmanual Elektroniskt Kodlas Part15nilsBelum ada peringkat
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Bosch Dishwasher Service Training Manual - Part6 PDFDokumen4 halamanBosch Dishwasher Service Training Manual - Part6 PDFnilsBelum ada peringkat
- Viii. Troubleshooting Door Latch - Miswired LatchesDokumen4 halamanViii. Troubleshooting Door Latch - Miswired LatchesnilsBelum ada peringkat
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Bosch Dishwasher Service Training Manual - Part13 PDFDokumen4 halamanBosch Dishwasher Service Training Manual - Part13 PDFnilsBelum ada peringkat
- Troubleshooting water leaks and circulation pump issuesDokumen4 halamanTroubleshooting water leaks and circulation pump issuesnilsBelum ada peringkat
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Bosch Dishwasher Service Training Manual - Part3 PDFDokumen4 halamanBosch Dishwasher Service Training Manual - Part3 PDFnilsBelum ada peringkat
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Bosch Dishwasher Service Training Manual - Part5 PDFDokumen4 halamanBosch Dishwasher Service Training Manual - Part5 PDFnilsBelum ada peringkat
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- IX. Wiring Diagrams/Tech Sheet Measuring SHU995X, SHV68 GM276, GI 976/966 Resistances at ModulesDokumen4 halamanIX. Wiring Diagrams/Tech Sheet Measuring SHU995X, SHV68 GM276, GI 976/966 Resistances at ModulesnilsBelum ada peringkat
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Troubleshooting and repair instructions for Frigidaire dishwasher control modules and heatersDokumen4 halamanTroubleshooting and repair instructions for Frigidaire dishwasher control modules and heatersnilsBelum ada peringkat
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- VI. Component Access/Replacement Control Modules - Apexx Control Module DisassemblyDokumen4 halamanVI. Component Access/Replacement Control Modules - Apexx Control Module DisassemblynilsBelum ada peringkat
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- Bosch Dishwasher Service Training Manual - Part14Dokumen4 halamanBosch Dishwasher Service Training Manual - Part14nilsBelum ada peringkat
- VIII. Troubleshooting Basic Dishwasher TroubleshootingDokumen4 halamanVIII. Troubleshooting Basic Dishwasher TroubleshootingnilsBelum ada peringkat
- IV. Installation Issues: Installation InstructionsDokumen4 halamanIV. Installation Issues: Installation InstructionsnilsBelum ada peringkat
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- VI. Component Access/Replacement Water ValvesDokumen4 halamanVI. Component Access/Replacement Water ValvesnilsBelum ada peringkat
- IX. Wiring Diagrams/Tech Sheet Measuring SHU303x/313x/33/430x/432x/53/68/88/99, SHV43/48 Circulation Pump Resistances at ModulesDokumen3 halamanIX. Wiring Diagrams/Tech Sheet Measuring SHU303x/313x/33/430x/432x/53/68/88/99, SHV43/48 Circulation Pump Resistances at ModulesnilsBelum ada peringkat
- Viii. Troubleshooting Circulation Pump - Service Index UC/06, UC/11 & UC/12 Parts ChangesDokumen4 halamanViii. Troubleshooting Circulation Pump - Service Index UC/06, UC/11 & UC/12 Parts ChangesnilsBelum ada peringkat
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- VI. Component Access/Replacement Door Latches - Removal & InstallationDokumen4 halamanVI. Component Access/Replacement Door Latches - Removal & InstallationnilsBelum ada peringkat
- VII. Component Testing/Test Procedures Using Test ProgramsDokumen4 halamanVII. Component Testing/Test Procedures Using Test ProgramsnilsBelum ada peringkat
- IX. Wiring Diagrams/Tech Sheet Measuring SHU43C/53A UC/14 Resistances at ModulesDokumen4 halamanIX. Wiring Diagrams/Tech Sheet Measuring SHU43C/53A UC/14 Resistances at ModulesnilsBelum ada peringkat
- Bosch Dishwasher Service Training Manual - Part6 PDFDokumen4 halamanBosch Dishwasher Service Training Manual - Part6 PDFnilsBelum ada peringkat
- Viii. Troubleshooting Dispenser - Top Load DispenserDokumen4 halamanViii. Troubleshooting Dispenser - Top Load DispensernilsBelum ada peringkat
- Bosch Dishwasher Service Training Manual - Part22Dokumen4 halamanBosch Dishwasher Service Training Manual - Part22nilsBelum ada peringkat
- Bosch Dishwasher Service Training Manual - Part18Dokumen4 halamanBosch Dishwasher Service Training Manual - Part18nilsBelum ada peringkat
- Best Practice Diagnostic Guidelines For Patients Presenting With Breast Symptoms PDFDokumen60 halamanBest Practice Diagnostic Guidelines For Patients Presenting With Breast Symptoms PDFfauziafahmi95Belum ada peringkat
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Sample Medical Specialty QuestionsDokumen58 halamanSample Medical Specialty Questionsplayuhz100% (1)
- BioPsych Handout 4 RESTRUCTUREDDokumen7 halamanBioPsych Handout 4 RESTRUCTUREDMarial JavierBelum ada peringkat
- Nursing Health History Format (Used For Client Care Plan)Dokumen2 halamanNursing Health History Format (Used For Client Care Plan)Hamid Colangcag AmborBelum ada peringkat
- Relationship Between Cigarette Smoking and Novel Risk Factors For Cardiovascular DiseaseDokumen4 halamanRelationship Between Cigarette Smoking and Novel Risk Factors For Cardiovascular DiseaseInternational Medical PublisherBelum ada peringkat
- Carte SemioDokumen279 halamanCarte SemioJoão Vitor LacerdaBelum ada peringkat
- Ezolvin Syrup Patient Information Leaflet PDFDokumen1 halamanEzolvin Syrup Patient Information Leaflet PDFSameer SamouaBelum ada peringkat
- Fact File Gastro Intestinal HormonesDokumen2 halamanFact File Gastro Intestinal HormonesSudip DevadasBelum ada peringkat
- Grannys List July 2010Dokumen423 halamanGrannys List July 2010ElectroPig Von FökkenGrüüvenBelum ada peringkat
- Assessment Exam in Cc2and3Dokumen7 halamanAssessment Exam in Cc2and3mika de guzmanBelum ada peringkat
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- OaDokumen6 halamanOafidatahir93Belum ada peringkat
- The Female Athlete Triad - Literature ReviewDokumen10 halamanThe Female Athlete Triad - Literature Reviewapi-340298177Belum ada peringkat
- Elder Abuse and Neglect: Brenda Holmes MSN/Ed, RNDokumen25 halamanElder Abuse and Neglect: Brenda Holmes MSN/Ed, RNSonia SinghBelum ada peringkat
- Tugas 1 Reading IIIDokumen7 halamanTugas 1 Reading IIIeva desmaliaBelum ada peringkat
- Maintain Acid-Base BalanceDokumen34 halamanMaintain Acid-Base BalanceAnnie GeorgeBelum ada peringkat
- Diabetes Mellitus (Etiology, Classification, and Diagnosis)Dokumen6 halamanDiabetes Mellitus (Etiology, Classification, and Diagnosis)ayu permata dewiBelum ada peringkat
- Allergic RhinitisDokumen31 halamanAllergic RhinitisJayR.Chauhan100% (1)
- ANTHROPOMETRY: MEASURING THE HUMAN BODYDokumen32 halamanANTHROPOMETRY: MEASURING THE HUMAN BODYRoshni AgarwalBelum ada peringkat
- Nephrotic syndrome: Causes, clinical presentations and histopathologyDokumen53 halamanNephrotic syndrome: Causes, clinical presentations and histopathologyAnna Althafunnisa100% (1)
- Chapter 004Dokumen10 halamanChapter 004Erika Midkiff100% (2)
- RTP RLSSampleUTMCR2CarePlanSnapshotDokumen3 halamanRTP RLSSampleUTMCR2CarePlanSnapshotHendry HuangBelum ada peringkat
- Foundation of Professional Nursing Practice Review (40Dokumen25 halamanFoundation of Professional Nursing Practice Review (40Sittie Haya LazimBelum ada peringkat
- Post Test NUR 219Dokumen3 halamanPost Test NUR 219Naomi VirtudazoBelum ada peringkat
- Berginia Ciliata (Haw.) Sternb: A Miracle in Between The Stone Menace To Kidney Stone Its Vital Uses and Important Chemicals-A ReviewDokumen7 halamanBerginia Ciliata (Haw.) Sternb: A Miracle in Between The Stone Menace To Kidney Stone Its Vital Uses and Important Chemicals-A ReviewJiwan PaudelBelum ada peringkat
- AUTOIMMUNE DISEASES AND ASSOCIATED AUTOANTIBODIESDokumen8 halamanAUTOIMMUNE DISEASES AND ASSOCIATED AUTOANTIBODIESLynx EemanBelum ada peringkat
- The Child With A Cardiovascular/Hematologic DisorderDokumen23 halamanThe Child With A Cardiovascular/Hematologic DisorderHannaBelum ada peringkat
- DM Final PDFDokumen15 halamanDM Final PDFgiftyBelum ada peringkat
- BMI PresentationDokumen25 halamanBMI PresentationJenny Bolesa BarrerasBelum ada peringkat
- Nephrotic Syndrome (Nephrosis)Dokumen9 halamanNephrotic Syndrome (Nephrosis)Radit Radovzky MayangkaraBelum ada peringkat
- Female Sterilisation: Presented by Group 4Dokumen23 halamanFemale Sterilisation: Presented by Group 4IbrahimWagesBelum ada peringkat
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDari EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionPenilaian: 4 dari 5 bintang4/5 (402)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessDari EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessPenilaian: 4.5 dari 5 bintang4.5/5 (327)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDari EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityPenilaian: 4 dari 5 bintang4/5 (13)
- The Ultimate Guide To Memory Improvement TechniquesDari EverandThe Ultimate Guide To Memory Improvement TechniquesPenilaian: 5 dari 5 bintang5/5 (34)
- Techniques Exercises And Tricks For Memory ImprovementDari EverandTechniques Exercises And Tricks For Memory ImprovementPenilaian: 4.5 dari 5 bintang4.5/5 (40)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDari EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsPenilaian: 3.5 dari 5 bintang3.5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDari EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeBelum ada peringkat