Pyogenic Liver Abscess Mimicking Pleural Effusion: Case Study
Diunggah oleh
dm40Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Pyogenic Liver Abscess Mimicking Pleural Effusion: Case Study
Diunggah oleh
dm40Hak Cipta:
Format Tersedia
Case Study: Pyogenic liver abscess mimicking pleural effusion
Pyogenic liver abscess mimicking pleural effusion
Abiodun M, MBBS(Benin), Senior Registrar
Osarogiagbon W, MBBS, FWACP, Consultant Paediatrician
Oviawe O, MBBS, FWACP, FMCP, Professor of Child Health, Consultant Pulmonologist
Director, Institute of Child Health, University of Benin Teaching Hospital
Correspondence to: Moses Abiodun, e-mail: biodunmt@yahoo.com
Keywords: pyogenic liver abscess, pleural effusion, ultrasound-guided percutaneous drainage
Abstract
Pyogenic liver abscess is a major visceral abscess that may pose a diagnostic dilemma in a febrile child with prominent
extra-abdominal symptoms. We present a case of a well-nourished, immunocompetent four-year-old girl who had none of
the common predispositions to a liver abscess. Hence, in this unusual setting, pyogenic liver abscess was not considered
at the initial assessment, until closer evaluation and futile efforts to drain a seemingly large pleural effusion eventually
revealed the diagnosis, which was confirmed by imaging. She underwent ultrasound-guided percutaneous drainage of the
pyogenic liver abscess to avert the sequelae of this potentially fatal disorder. This underscores the need to think laterally
when considering differential diagnoses for the sick child.
Peer reviewed. (Submitted: 2011-07-02. Accepted: 2011-11-04.) SAAFP
Introduction
intrathoracic involvement due to sympathetic pleural
effusion or pneumonia. Rarely, pyogenic liver abscess may
present with thoracic empyema or pericardiac tamponade,
due to rupture of an abscess in the left lobe of the liver.8
Other metastatic complications of pyogenic liver abscess
include peritonitis, pericarditis, splenic abscess, necrotising
fasciitis, endophthalmitis, and brain abscesses, occurring
more commonly with Klebsiella pneumoniae than with other
bacteria (14.6 vs. 3.8%).9 The diagnosis of a liver abscess is
usually confirmed by imaging studies.2
Pyogenic liver abscess can present both diagnostic and
therapeutic challenges to healthcare providers. Based on
aetiology, liver abscesses can be classified as pyogenic,
which accounts for about 80% of cases; amoebic, which
constitutes 10% of cases; and fungal (Candida species),
which accounts for less than 10% of cases.1 A liver abscess
is twice as common in the right lobe than in the left lobe of
the liver.2 The annual incidence of liver abscess in children
varies widely in different regions of the world, occurring more
commonly in developing countries.2 The incidence ranges
from 28 per 100 000 in South African children, to more
than 79 per 100 000 paediatric admissions in India.3,4 Risk
factors for liver abscesses in children include malnutrition,
sickle cell disease, acquired immunodeficiency syndrome
and congenital immunodeficiencies, such as chronic
granulomatous disease.2,5
The treatment of a liver abscess can be medical, surgical,
or a combination of both. Currently, ultrasound-guided
percutaneous drainage is the treatment option of choice.2
Prognosis depends on the underlying pathology and
complications. With appropriate culture-sensitive antibiotics
and drainage, the mortality rate is less than 15% in children
with uncomplicated pyogenic liver abscess, but as high as
40% in complicated cases.2-4
Liver abscesses can result from local spread via the portal
circulation of an intra-abdominal infection focus (such as
appendicitis), or from an ascending biliary infection.6 It may
also be due to the haematogenous spread of a systemic
infection via the hepatic artery. Other potential sources of
infection include surgical wounds or penetrating injuries,
while about 15% of cases are cryptogenic.1,2
We managed a child with a liver abscess who presented
in an atypical manner, which led to treatment by pleural
aspiration and chest tube insertion. Important lessons,
in both the diagnosis and management of this important
condition, are presented in the case study.
Case study
Clinical features of liver abscesses in children include fever
and right hypochondrial tenderness in about 100% of cases,
hepatomegaly in 85%, and vomiting in 25%.7 Symptoms
such as cough, dyspnoea and severe chest pain suggest
S Afr Fam Pract 2012
S Afr Fam Pract 2012;54(5):459-462
A four-year-old girl was admitted to the paediatric ward
of University of Benin Teaching Hospital, Nigeria, on 29
December 2010. She was the youngest of three children,
459
Vol 54 No 5
Case Study: Pyogenic liver abscess mimicking pleural effusion
and lived with their parents in a three-bedroom flat. She
presented with high-grade fever that had lasted five weeks,
with associated chills and rigors, a cough of four-week
duration and right lower chest pain. She had had difficulty
breathing for a week. She also complained of appetite loss.
There was no history of trauma, and a systematic review of
the other systems was not contributory.
supradiaphragmatic, or pleural fluid collections (Figure
2). Liver function tests were essentially normal: alkaline
phosphatase (ALP) 25 IU/l, aspartate aminotransferase
(AST) 36 IU/l, alanine aminotransferase (ALT) 17 IU/l, total
bilirubin 0.4 mg/dl, conjugated bilirubin 0.3 mg/dl, total
protein 5.7 g/dl, albumin 3.4 g/dl, and globulin 2.3 g/dl.
Ultrasound-guided percutaneous drainage was performed,
and 280ml of cream-coloured purulent fluid was aspirated
(Figure 3). The cavity was irrigated with metronidazole and
gentamicin, and intravenous metronidazole was added to
her treatment. Post-aspiration, the cavity decreased to 4.3
x 4.7cm. A two-week post-aspiration chest X-ray showed
considerable descent of the elevated right hemidiaphragm.
The liver abscess aspirate showed both Gram-negative
On examination, she looked acutely ill, febrile (39C),
dyspnoeic, tachypnoeic, not pale, and not jaundiced.
She was well nourished. Her weight was 15 kg (> 50th
percentile), height 104cm (75th percentile), and mid-upper
arm circumference (MUAC) 15 cm. Her body mass index
(BMI) was 14kg/m2. Her chest was asymmetrical, with slight
bulging of the right hemithorax. The trachea was deviated
to the left, and the apex beat was displaced 3cm lateral to
the left mid-clavicular line. On percussion, there was stony
dullness and reduced breathing sounds in the right middle
and lower lung zones. The abdomen was flat and soft. There
was a 4 cm hepatomegaly below the right costal margin,
which was tender. There was no ascites, and all other organ
systems were normal.
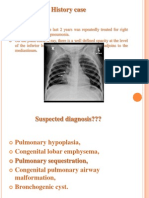
Initial assessment was for community-acquired lobar
pneumonia with a right-sided pleural effusion. Pulmonary
tuberculosis was considered to form part of the differential
diagnosis. A chest X-ray showed a homogenous opacity in
the right middle and lower lung zones, with mediastinal shift
(Figure 1a).
This was reported as a right-sided pleural effusion.
Diagnostic thoracocentesis yielded 3 ml of serous fluid.
A chest tube was successfully inserted, but had to be
removed, because it was not draining any fluid. Postextubation chest X-ray did not show any improvement.
Pleural fluid microscopy revealed the absence of acidfast bacilli (AFB). Gastric aspirate was also negative for
AFBs, and the Mantoux test was negative. A full blood
count showed the following: white blood count 12.4 x
103/l, neutrophil 7.6 x 103/l (61.2%), lymphocytes 3.4 x
103/l (27.2%), monocytes 0.9 x 103/l(7.6%), eosinophil
0.5 x 103/l (4.0%). The erythrocyte sedimentation
rate (ESR) was 18 mm/hour. Retroviral screen results
were negative, haemoglobin genotype was AA, a stool
microscopy showed no ova or parasite, and the blood
culture yielded no growth.
Despite treatment with intravenous cefuroxime (100mg/kg/
day), she continued to deteriorate, and by day three postadmission, the liver was markedly tender and 6cm below
the right costal margin. A review of the chest X-ray showed
a clear costophrenic angle without a meniscus sign (Figures
1a and 1b).
Figure 1a: Chest radiograph showing homogenous opacity in the
right hemithorax, a clear right costophrenic angle, and absence of
meniscus sign. Figure 1b: A sketch of Figure 1a, highlighting the
elevated right hemidiaphragm a, normal left hemidiaphragm b,
clear costophrenic angles, and mediastinal shift to the left.
Immediate abdominal and pleural ultrasonography revealed
a solitary liver abscess (13.4cm x 9.03cm) in the posterosuperior aspect of the right lobe of the liver, with no
evidence of biliary system dilatation, subdiaphragmatic,
S Afr Fam Pract 2012
460
Vol 54 No 5
Case Study: Pyogenic liver abscess mimicking pleural effusion
with prominent extra-abdominal symptoms and no risk
factors for liver abscess, such as malnutrition, sickle cell
disease, hepatobiliary disease, or immunosuppression.5
The prominent respiratory features in our patient resulted
from the pressure effect of the liver abscess on the right
hemidiaphragm causing pulmonary compression and
cardiomediastinal shift (Figures 1a and 1b). In this case, the
solitary right lobe abscess that was found is the usual trend.
Zibari et al reported 95% right lobe involvement, and 70%
of liver abscesses being solitary, in a large case series.10
Similarly, in a meta-analysis, Mishra et al reported that
approximately two-thirds of liver abscesses occur in the
right lobe of the liver, the majority of which are solitary.2 The
predilection for abscesses to occur in the right hepatic lobe
could be due to the fact that it has a larger blood supply
than the left and caudate lobes. Also, unlike the left portal
vein which branches at an angle, the right portal vein follows
a straight course in the direction of the common portal vein,
encouraging direct spread of infection from pylephlebitis.2
Figure 2: A well-defined, rounded area of mixed echogenicity,
measuring 13.4 x 9.03 cm in the posterosuperior aspect of the right
lobe, in keeping with a liver abscess
The most common organism isolated from pyogenic
liver abscess in children is Staphylococcus aureus, both
in developed and developing countries.2 Other species
implicated in pyogenic liver abscess are E. coli, Klebsiella,
Enterobacter and anaerobes.2 In this case, liver aspirate
microscopy showed both Gram-positive cocci and Gramnegative bacilli, but culture yielded no growth. Polymicrobial
aetiology is common, and blood culture may be negative
in about half of cases.7,11 Eosinophilia, found in this case,
may be due to previous helminthic infestation. Helminthiasis
has been implicated in pyogenic liver abscess in children
without pre-existing liver lesions, by inducing eosinophilia
and granulomatous changes while passing through the
liver.12
Clinical manifestations and sonographic findings of pyogenic
liver abscess, as found in our patient, are often distinct from
those of other cystic lesions of the liver, such as a simple
cyst, cystadenoma, echinococcal cyst, liver metastasis and
polycystic liver disease.12,13 On ultrasonography, simple
cysts appear as an anechoic unilocular fluid-filled space
with an imperceptible wall; cystadenoma as an hypoechoic
loculated lesion with thickened irregular walls; and an
echinococcal cyst as an anechoic smooth, round lesion
with calcification.12,13 The unifocal nature of the pyogenic
liver abscess, and the absence of a debilitating underlying
disease, are good prognostic factors in our patient.
Figure 3: Purulent aspirate (280 ml) obtained from the liver abscess
via ultrasound-guided percutaneous drainage
bacilli and Gram-positive cocci following Gram stain, but
culture (both aerobic and anaerobic) yielded no growth.
An acid-fast smear of the liver aspirate was also negative.
Neither fungal hyphae, nor yeast cells, were seen on
microscopy. Specimens from the abscess wall was negative
for Entamoeba histolytica. The patient recovered fully, and
was discharged with oral cefixime and metronidazole,
which she had to take for four weeks. She is being followed
up in our clinic.
As illustrated in this case report, thorough evaluation of
children without obvious risk factors for a liver abscess,
and a high index of suspicion, are crucial to enable prompt
diagnosis and management of this potentially fatal disease.
Discussion
Acknowledgements
Pyogenic liver abscess is a major visceral abscess that may
pose a diagnostic dilemma in a febrile child who presents
We thank Drs Iseh, Venn and Olaiya, who participated in the
management of this patient.
S Afr Fam Pract 2012
461
Vol 54 No 5
Case Study: Pyogenic liver abscess mimicking pleural effusion
References
7. Bari S, Sheikh KA, Malik AA, et al. Percutaneous aspiration versus open drainage
1. Krige JEJ. Pyogenic liver abscess. In: Kirsch R, Robson S, Trey C, editors.
8. Vong SC, Guo HR, Lin HJ, Foo NP. Cardiac tamponade secondary to pyogenic
of liver abscess in children. Pediatr Surg Int. 2007;23(1):69-74.
Diagnosis and management of liver disease. London: Chapman and Hall, 1995; p.
liver abscess. J Clin Gastroenterol. 2007;41(6):635-636.
196-202.
9. Yang CC, Yen CH, Ho MW, Wang JH .Comparison of pyogenic liver abscess
2. Mishra K, Basu S, Roychoudhury S, Kumar P. Liver abscess in children: an
caused by non-Klebsiella pneumoniae and Klebsiella pneumoniae. J Microbiol
overview. World J Pediatr. 2010;6(3):210-216.
Immunol Infect. 2004;37(3):176-184.
3. Hendricks MK, Moore SW, Millar AJ. Epidemiological aspects of liver abscesses
10. Zibari GB, Maguire S, Aultman DF, et al. Pyogenic liver abscess. Surg Infect.
in children in the Western Cape Province of South Africa. J Trop Pediatr.
2000;1(1):15-21.
1997;43(2):103-105.
11. Chemaly RF, Hall GS, Keys TF, Procop GW. Microbiology of liver abscesses
4. Kumar A, Srinivasan S, Sharma AK. Pyogenic liver abscess in children: South
gram stain and associated blood cultures. Diagn Microbial Infect Dis.
Indian experiences. J Pediatr Surg. 1998;33(3):417-421.
2003;46(4):245-248.
5. Lublin M, Bartlett DL, Danforth DN, et al. Hepatic abscess in patients with chronic
12. Pereira FE, Musso C, Castelo JC. Pathology of pyogenic liver abscess in children.
granulomatous disease. Ann Surg. 2002;235(3):383-391.
Pediatr Dev Pathol. 1999;2(6):537-543.
6. Rahimian J, Wilson T, Oram V, Holzman RS. Pyogenic liver abscess: Recent trends
13. Nisenbaum HL, Rowling SE. Ultrasound of focal hepatic lesions. Semin
in etiology and mortality. Clin Infect Dis. 2004;39(11):1654-1659.
Roentgenol. 1995;30(4):324-346.
Press Release
Rabies: 100% Fatal, 100% Preventable
Jean-Antoine Zinsou continues, If not treated immediately
- before the virus reaches the central nervous system and
the symptoms of the disease appear - rabies is fatal to both
animals and humans. The symptoms in humans include
headaches, fever, anxiety, muscle pains, vomiting, paralysis
and hydrophobia (fear of water). The symptoms of rabies in
animals include behavioural changes such as restlessness,
irritability, excitability and shyness.
In a bid to save thousands of lives, the Department of Health
(DoH),Sanofi Pasteur (the vaccines division of Sanofi), and
Merial South Africa (the animal Health Division of Sanofi),
have partnered with numerous human and animal health
organisations worldwide to support World Rabies Day on
28 September, creating awareness that rabies is 100%
preventable.
World Rabies Day, the single largest rabies education
and outreach initiative, is observed each year in about
135 countries. It aims to educate people about the risk of
rabies, to promote global awareness of its prevention, and
to mobilise resources to support local rabies prevention
programmes. Rabies is a viral disease that attacks the
central nervous system. It can be transmitted to animals
and humans mainly through a bite, but also through
contamination of broken skin or mucous membranes with
saliva from an infected animal. Rabies has been reported
throughout South Africa and in almost all types of domestic
animals and a number of wild animals. However, 99% of
cases are transmitted through contact with infected dogs.
Prevention is better than cure; rabies prevention starts with
the animal owner notes Theunis de Bruyn, Business Unit
Manager, Merial South Africa. We recommend that people
vaccinate dogs, cats and any other animal that has regular
contact with humans, such as horses.
Vaccination remains the only effective treatment against
rabies and acts by neutralising the virus before it actually
reaches the central nervous system.The vaccine can be
administered before exposure to the virus (pre-exposure
prophylaxis), or immediately after contact with an infected
animal (post-exposure prophylaxis). The World Health
Organization recommends that pre-exposure vaccination
should be promoted for children living in areas where
canine rabies is endemic, including South Africa. It is
also recommended for people who face increased risk of
exposure, such as laboratory staff, vets, animal handlers,
game rangers and travellers to high risk areas.
The WHO estimates that more than 55 000 people die each
year, more than half of them in Africa, with the most vulnerable
being children. Children are likely to suffer multiple bites and
scratches due to them being in close contact with dogs and
cats, which carry a higher risk of contracting rabies, and are
less likely to tell their parents when a bite, lick, or scratch
has occurred says Jean-Antoine Zinsou, Country Manager,
Sanofi Pasteur.
S Afr Fam Pract 2012
462
Vol 54 No 5
Anda mungkin juga menyukai
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Cervicothoracic Sign - Print Friendly - STATdxDokumen3 halamanCervicothoracic Sign - Print Friendly - STATdxmihaelaBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5795)
- X Thorax BeoordelenDokumen135 halamanX Thorax BeoordelenmtescasuraBelum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Basic Chest RadDokumen112 halamanBasic Chest Radtesfayegermame95.tgBelum ada peringkat
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Cyst and Cystlike Lung LesionsDokumen57 halamanCyst and Cystlike Lung LesionsAna StankovicBelum ada peringkat
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Lec2 X-Rays and FluorosDokumen39 halamanLec2 X-Rays and Fluorossana mumtazBelum ada peringkat
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- Underwriting GuideDokumen100 halamanUnderwriting GuideDaven TanBelum ada peringkat
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Makalah Bahasa Inggris NewDokumen25 halamanMakalah Bahasa Inggris Newmei diana sara'isBelum ada peringkat
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Evaluation of Compliance With Standard Criteria For Postero-Anterior (Pa) Chest Radiographs in Parklane Hospital EnuguDokumen37 halamanEvaluation of Compliance With Standard Criteria For Postero-Anterior (Pa) Chest Radiographs in Parklane Hospital EnuguLavinia VictorBelum ada peringkat
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Viva in Anaesthesiology: Questions and Answers On Abg, Drugs, Ecg, X-Ray&OthersDokumen121 halamanViva in Anaesthesiology: Questions and Answers On Abg, Drugs, Ecg, X-Ray&OthersAnish H DaveBelum ada peringkat
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Previous Years Question PapersDokumen19 halamanPrevious Years Question PapersViraj ShahBelum ada peringkat
- Case Series - CapDokumen162 halamanCase Series - CapMichael LinebargerBelum ada peringkat
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- Pleural EffusionDokumen72 halamanPleural Effusionmaeliszxc kimBelum ada peringkat
- Nhsbi FormDokumen1 halamanNhsbi FormClark Jayden JacobBelum ada peringkat
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Chest XrayDokumen6 halamanChest XrayAjit KumarBelum ada peringkat
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Note On Cardiopulmonary Physiotherapy PDFDokumen16 halamanNote On Cardiopulmonary Physiotherapy PDFTsz Kwan CheungBelum ada peringkat
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- 13-10 Topic 4. Chest X-Ray Anak IDAIDokumen20 halaman13-10 Topic 4. Chest X-Ray Anak IDAIReza Ervanda ZilmiBelum ada peringkat
- Chest X Ray BasicsDokumen99 halamanChest X Ray BasicsHarshaWakodkarBelum ada peringkat
- Labortory Test or ManeuverDokumen2 halamanLabortory Test or ManeuverJeno Luis J. ACUBBelum ada peringkat
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- Case Study-Breast CADokumen11 halamanCase Study-Breast CAJoanna Cabildo83% (6)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- TB PolicyDokumen33 halamanTB Policyyam kuan100% (1)
- AtelectasisDokumen15 halamanAtelectasisAmit Kumar RanoBelum ada peringkat
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- CT Features of Rounded Atelectasis: Findings Were Analyzed and ComparedDokumen4 halamanCT Features of Rounded Atelectasis: Findings Were Analyzed and ComparedSandara ParkBelum ada peringkat
- CXR Lecture DR Lenora FernandezDokumen70 halamanCXR Lecture DR Lenora Fernandezapi-19431894100% (1)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- DifdgDokumen54 halamanDifdgMarina Ivosevic MilosavljevicBelum ada peringkat
- Ajr 10 7226Dokumen9 halamanAjr 10 7226cuenta de gmailBelum ada peringkat
- Congenital Lung MalformationsDokumen115 halamanCongenital Lung MalformationsAhmad Abu KushBelum ada peringkat
- Chest CT Signs in Pulmonary Disease PDFDokumen19 halamanChest CT Signs in Pulmonary Disease PDFpvs5155Belum ada peringkat
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Laporan Kasus Efusi PleuraDokumen23 halamanLaporan Kasus Efusi PleuraReza RestuBelum ada peringkat
- GFHDFGHDokumen1.211 halamanGFHDFGHheetoothBelum ada peringkat
- Chest XDokumen8 halamanChest XAnnandra RahmanBelum ada peringkat
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)