Pseudocyst of Pancreas: A Clinical Study
Diunggah oleh
IOSRjournalHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Pseudocyst of Pancreas: A Clinical Study
Diunggah oleh
IOSRjournalHak Cipta:
Format Tersedia
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS)
e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 14, Issue 10 Ver. VI (Oct. 2015), PP 101-105
www.iosrjournals.org
Pseudocyst of Pancreas: A Clinical Study
Varun Laddha1, Prashant Tubachi2, K. Rajgopal Shenoy3
1,2,3
(Department of Surgery KMC Manipal, India)
Abstract:
Introduction:Pancreatic pseudocysts belong to a large and heterogeneous group of cystic pancreatic lesions
and represent a complication of acute or chronic pancreatitis. The objective of this observational study was to
study the different etiologies, clinical features, investigations and management of pseudocyst of pancrease in
patients being treated at KMC hospital Manipal.
Methodology:A prospective observational study was carried out on patients diagnosed with a pancreatic
pseudocyst in the Department of Surgery/Medicine/Gastroenterology in Kasturba hospital, Manipal. The study
was conducted over a period of 2 years from 1st September 2012 to 31st August 2014. A total of 50 patients
were included in the study.
Results:The majority of patients belonged to the age group of 30-39 yrs(40%) and showed a predisposition
towards males (96%). Abdominal pain was the presenting symptom (98%) and abdominal tenderness was
present in 62% of patients. Majority of the patients had history of alcohol abuse (47%). CECT abdomen was
more useful for details of pseudocyst. The mean size of pseudocyst was 9.62 cms. Most common site for
pseudocyst was body and tail (24%). The major complication seen was hemorrhage in cyst (8%).The most
commonly done procedure was cystogastrostomy (18%).
Conclusion: Surgery is the traditional modality for treating pancreatic pseudocysts, with high success rates and
low morbidity and mortality, and it still plays an important role in therapy. Laparoscopic management has
been reported with very encouraging results, but long-term follow-up has still to show equivalence to open
surgery. Endoscopic therapy is a reasonable alternative to surgery, particularly for chronic pseudocysts, and is
increasingly being used.
Keywords: Alcohol abuse, Cystogastrostomy, Cystic neoplasm of pancrease, Pancreatitis, Pancreatic
pseudocyst.
I.
Introduction
A pseudocyst presents as a cystic cavity connected to the pancreatic duct system, either directly or via
the pancreatic inflammatory tissue. Pancreatic pseudocysts may occur as a consequence of both acute and
chronic pancreatitis. It contains a collection of pancreatic juice, usually sterile, is rich in pancreatic enzymes,
and enclosed by a well-defined non-epithelialized wall of fibrous or granulation tissue.
Pancreatic pseudocysts are caused by pancreatic ductal disruption following increased pancreatic
ductal pressure, either due to stenosis, protein plugs or calculi obstructing the main pancreatic ductal system, or
as a consequence of pancreatic necrosis following an attack of acute pancreatitis[1, 2].Formation of a pancreatic
pseudocyst requires four or more weeks from the onset of acute pancreatitis. Acute fluid collections are not
surrounded by a wall, andoccur early after acute pancreatitis.
Classification of pancreatic pseudocysts based on the underlying aetiology of pancreatitis (acute or
chronic) and the ductal anatomy, and the presence of communication between the cyst and the pancreatic duct,
was published in 1991 and is still valid [3].
The pseudocyst size ranges from very small to more than 25 cm in diameter[4, 5].Most commonly only
one pseudocyst is present after acute pancreatitis. The symptoms depend on the size and location of the
pseudocyst and may include pain, nausea and vomiting. Less frequent are gastric outlet and/or bile duct
obstruction, bleeding andrupture [6]. Occasionally, the pseudocyst is palpable.
Pancreatic pseudocysts are diagnosed in 10-15% of patients after acute pancreatitis [7,8]. Even if no
comprehensive cohort study has been conducted to evaluate the true incidence of pseudocysts, it is
approximated to be 0.5-1 per 100 000 adults annually [9].
The occurrence of pseudocyst parallels that of pancreatitis and the etiology of pseudocysts resembles
the causes of pancreatitis closely, and it is more common after alcohol-induced than after non-alcohol-related
pancreatitis. Alcohol-related pancreatitis appears to be the major cause in studies from countries where alcohol
consumption is high and accounts for 59%-78% of all pseudocysts [10].
Sensitivity rates for USG in the detection of pancreatic pseudocysts are 75% to 90%. Therefore, USG is
inferior to CT, which has a sensitivity of 90% to 100%. USG has several limitations and examinations are
highly operator dependent [10].In addition, CT scans provide more detailed information regarding the
DOI: 10.9790/0853-14106101105
www.iosrjournals.org
101 | Page
Pseudocyst of Pancreas: A Clinical Study
surrounding anatomy and can demonstrate additional pathology, including pancreatic duct dilatation and
calcifications, common bile duct dilatation, and extension of the pseudocyst outside the lesser sac.
MRI is generally not routinely used. However, the pancreatic duct and biliary systems are easily
visualized in detail, although interpreting the status of pancreatic duct integrity may be difficult[11].EUS is
usually used as a secondary test to further evaluate pancreatic cyst detected by other imaging modality (USG,
CT or MRI). Cyst fluid aspiration can be done for analysis.
Percutaneous drainage, endoscopic drainage and surgery are the available treatment strategies[12].
Treatment forpseudocyst includes Conservative treatment, meaning observation, based on the knowledge that
spontaneous resolution can occur [13]. It is suitable in patients without symptoms, with unaltered or diminishing
pseudocyst size. Percutaneous puncture with USG or CT guidance can give instant pain relief and the possibility
to fluid bacterial culture, but the recurrence rate is high.
Endoscopic transpapillary drainage with ERCP is suitable in pseudocystsdue to chronic pancreatitis,
which communicate with the ductal system [14]. The potential complications are severe bleeding and
perforation [15]. Endoscopic treatment has been shown to be as equally effective as open surgery [16]. Even if
the trend is towards primary minimally invasive treatment, open surgery with internal drainage to the
gastrointestinal tract is a well-established and safe choice with good results, but also associated with significant
morbidity and mortality in some cases [17,18].The complications of pancreatic pseudocyst include splenic
complications, rupture, hemorrhage, infection, biliary complications and portal hypertension.
The present study was carried out to evaluate the various etiologies, clinical presentations, investigative
procedures, treatment modalities and complications of pseudocyst of pancreas.
II.
Methodology
A prospective observational study was carried out on patients diagnosed with a pancreatic pseudocyst
in the Department of Surgery/Medicine/Gastroenterology in Kasturba hospital, Manipal. The study was
conducted over a period of 2 years from 1st September 2012 to 31st August 2014. A total of 50 patients were
included in the study.All patients >16 yrs of age admitted in Kasturba hospital, Manipal, diagnosed as pancreatic
pseudocyst were included in the study. Patients < 16yrs and with other cystic lesions of pancreas, viz., cystic
neoplasm of pancreas, etc. were excluded.Patients presenting with pancreatic pseudocysts were clinically
examined and subjected to a proforma in accordance with the inclusion and exclusion criteria of the study.The
results obtained were statistically analyzed using SPSS 21.0 software.
III. Results
The present study which was conducted on a group of 50 patients, revealed the following observations.
These cases were all either hithero untreated cases or those referred from a primary or a secondary centre for
tertiary care, owing to complications, at Kasturba Hospital, Manipal.
The majority of patients belonged to the age group of 30-39 years which accounted for 40% of the total
number of patients.The mean age was 38.52 years with standard deviation of 11.213 yrs.The sex distribution in
this study showed a predisposition towards males, 48 patients (96%), as compared to females 2 patients (4%).
Abdominal pain was the presenting symptom in 49(98%) in majority of patients. Radiation to the back
was seen in 30(60%). Diarrhea and breathlessness were seen in least of the cases i.e in 2(4%) cases. Abdominal
tenderness was present in 31 (62%) of patients. A palpable mass was present in 23 (46%). 6 (12%) patients had
ascites on examination.
37 (74%) patients had history of alcohol abuse. Biliary disease was present in 9 (18%) patients. 2
patients had history of laparoscopic cholecystectomy. 1 (2%) patient had hypertriglyceridemia as a cause on
evaluation (Table 1).
21 (42%) patients had acute pancreatitis, and 29 (58%) patients had chronic pancreatitis. Leucocytosis
was found in 16 (32%) patients. 7 (14%) patients had hemoglobin less than 10 gm/dl. 10 (20%) patients were
diabetic. Direct bilirubin was raised in 7 (14%) patients. Serum ALP was elevated in 12 (24%) patients. Serum
amylase was elevated in 36 (72%) patients. 32 (64%) patients had raised serum lipase.
Chest X-ray showedpleural effusion in 11 (22%) patients. Ultrasonography was performed in 37 (74%)
patients, of which pseudocyst was not clearly visualized in 2 cases and became evident on CECT abdomen.
USG abdomen was very useful in visualizing pancreatic duct and biliary tree abnormality.CECT abdomen was
done in 39 (78%) patients, and was useful for details of pseudocyst viz., site, size, adjacent organs, presence of
hemorrhage, etc.
The mean size of pseudocyst was 9.62 cms. The standard deviation was 4.499 cms. The smallest
pseudocyst was 1.9 cms. The largest was 20 cms.Most common site for pseudocyst was body and tail, 12 (24%)
patients and least common was uncinate process, 1 (2%) patients.13 (23%) patients had multiple pseudocysts.
DOI: 10.9790/0853-14106101105
www.iosrjournals.org
102 | Page
Pseudocyst of Pancreas: A Clinical Study
5 (10%) patients had gall stones. 1 (2%) had CBD dilatation. Pancreatic duct calculi were found in 3 (6%)
patients and 13 (26%) patients showed pancreatic duct dilatation.4(8%) of the cases presented with the
complication of hemorrhage in cyst. Pancreato-pleural fistula was seen in 3(6%) of the patients (Table 2).
15 (30%) patients were managed conservatively as most of them had lesion less than 6 cms in diameter and did
not have a mature cyst wall. These patients were followed up regularly. 7 (14%) patients underwent
percutaneous USG guided aspiration. ERCP and pancreatic duct stenting was done in 7(14%) patients. 6 (12%)
patients underwent EUS guided cystogastrostomy. 15 patients were treated surgically. Most commonly done
procedure was cystogastrostomy, in 9 (18%) patients. 3 (6%) patients underwent roux-en-y cystojejunostomy
and external drainage was done in another 3 (6%) patients. 1 patient underwent laparoscopic cystogastrostomy
with cholecystectomy. Cystogastrostomy with cystojejunostomy was done in same setting in 1 patient (Table 3).
The cases were followed up for 6 months.In the conservative group, of the 15 patients, 9 patients had on
and off recurrent abdominal pain. In 3 patients the cyst had disappeared. The cyst had increased in 3 of the
patients. All were managed conservatively. Among the 7 patients who underwent USG guided aspiration,
complete resolution was seen in 1 patient. In 5 out of 7 patients treated by ERCP and pancreatic duct stenting,
complete resolution was achieved. EUS guided cystogastrostomy was done in 6 patients out of which in 5
patients cyst had disappeared. Cystogastrostomy was done in 9 patients, of which, 4 showed complete
resolution. In all the 3 cases treated by roux-en-y cystojejunostomy, cyst disappeared completely. 2 of 3 cases
who underwent external drainage showed complete resolution (Table 4).
Thepost operative complications include infection of residual cavity which was seen in1 patient
developed and was managed conservatively. Patient improved on conservative management. The post
procedural complication included infection of residual cavity following ERCP and pancreatic duct stenting in 1
patient and was managed by pigtail drainage. The patient expired due to bleeding.1 patient developed bleeding
in residual cavity, post EUS guided cystogastrostomy and was managed with blood transfusions.In the study,
out of 50 patients, 2 were lost on follow up (they were on conservative management). 2 patients had discharged
themselves against medical advice (1 had USG guided drainage and other was on conservative management). 2
patients died due to pseudoaneurysmal bleed (had USG guided drainage).
IV. Tables
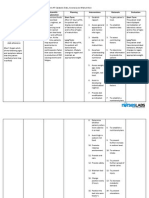
Table 1: Etiology
Etiology
Alcoholism only
Gallstones disease only
Both gall stones and alcoholism
Hypertriglyceridemia
Idiopathic
TOTAL
Frequency
34
6
3
1
6
50
Percent
68%
12%
6%
2%
12%
100%
Table 2: Complications
Hemorrhage in cyst
Pancreato-pleural fistula
Rupture in peritoneal cavity
Pseudoaneurysmal bleed
Pancreato-gastric fistula
Infection of cyst
TOTAL
Frequency
4
3
2
2
1
1
13
Percent
8%
6%
4%
4%
2%
2%
26%
Table 3: Management
Management modality
Conservative
USG guided pigtail drainage
ERCP and pancreatic duct stenting
EUS guided cystogastrostomy
Surgical cystogastrostomy
Surgical roux-en-y cystojejunostomy
Surgical external drainage
Total
DOI: 10.9790/0853-14106101105
Frequency
15
7
7
6
9
3
3
50
Percent
30
14%
14%
12%
18%
6%
6%
100%
www.iosrjournals.org
103 | Page
Pseudocyst of Pancreas: A Clinical Study
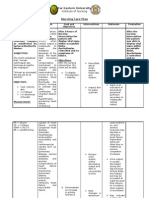
Table 4: 6 Month Follow Up
Conservative
USG Guided Pigtail Drainage
Ercp And Pancreatic Duct Stenting
Eus Guided Cystogastrostomy
Surgical Cystogastrostomy
Surgical
Roux-En-Y
Cystojejunostomy
Surgical External Drainage
Total
Cyst
Decreased
5
2
2
1
2
0
Cyst
Disappeared
3
1
5
5
4
3
Cyst
Increased
3
1
0
0
1
0
No
Change
1
0
0
0
0
0
Not
Done
3
3
0
0
2
0
Total
1
13
2
23
0
5
0
1
0
8
3
50
V.
15
7
7
6
9
3
Discussion
In most of the series,Bodker et al., 1980 [19], Bodil Anderson, 2010, pseudocysts were seenin 4th and
th
5 decades, and the mean age was around 40-47 yrs. In our present series, majority of patients belonged to the
age group of 30-40 yrs and the mean age was 38.52 yrs.
As compared to other studiesBodil Anderson, 2010, Varadarajulu et al., 2013[20], marked male
predominance was seen in our study, in the ratio of 24:1 (male:female) and may be attributed to the fact that
alcoholism is less common in females in India.
Abdominal pain is a consistent finding and is usually located in the epigastrium and upper abdominal
quadrants often associated with radiation to back. Frequently patients present with mass abdomen or sometimes
with nausea, vomiting, anorexia, jaundice. Weight loss is a common feature but is more marked in neoplastic
cysts [21]. In our present study also pain abdomen was the commonest complaint being present in 98%, with
radiation to back in 60%. Other symptoms like vomiting, anorexia, weight loss were also present in a significant
number of patients.Physical examination in our study revealed abdominal tenderness in 62% of patients and a
palpable mass in 46% of patients. Fever, ascites and jaundice were present in some patients. In many other
series, tenderness was not a very common clinical finding, whereas a palpable mass was reported in 75% of
cases [21].
Various western countries revealed alcoholism as the commonest cause of pancreatits leading to
pseudocyst formation (65-80%), by biliary tract disease in about (6-20%) cases and trauma as the cause in (310%). Others were classified as idiopathic cases (6-20%)[20, 22, 23, 24].Our present study shows alcohol intake
as the commonest etiology (68%)
Amylase and lipase levels are often elevated, but may be within reference ranges. Some laboratory tests
may provide clues to the underlying etiology of pancreatitis (e.g. elevated triglycerides or calcium level).
Elevated liver chemistries raise the suspicion for biliary pancreatitis [12].In our present study, serum amylase
was raised in 72% patients with 8% of patients having serum amylase more than 1000 u/l. Serum lipase was
elevated in 64% of patients.Leucocytosis was present in 32% patients. Hemoglobin of less than 10gm/dl was
found in 14% patients. Raised direct bilirubin was seen in 14% patients and raised serum alkaline phosphatase
was seen in 24% patients.20% cases were diabetic, signifying pancreatic destruction.
Radiological studies are extremely helpful in making the diagnosis. Chest x-ray may show the evidence
of pleural effusion. Our study revealed pleural effusion in 22% of patients.In our study, Ultrasonography was
performed in 37 (74%) patients and CECT abdomen was done in 39 (78%) patients.
In a series at John Hopkins and Mayo Clinic, infection of the pseudocyst was reported in 4% and 1% respectively
[8]. In our study infection of the pseudocyst was seen in 2% cases.Rupture of the pseudocyst may be seen as a surgical
emergency with severe acute abdominal pain. It occurs in less than 3% of cases[25]. In our study, rupture with peritonitis
was seen in 4% cases.
Several studies have indicated that the size of the cyst and the length of time the cyst has been present are poor
predictors of potential for pseudocyst resolution or complications, but in general, larger cysts are more likely to become
symptomatic or cause complications[26]. However, some patients with larger collections do well; therefore, size of the
pseudocyst alone is not an indication for drainage [13, 27]. The two main indications for invasive intervention are the
presence of symptoms or the presence of complications (infection, bleeding, gastric outlet or biliary obstruction).
In our study, conservative management was done for 15 patients with spontaneous regression in 3
patients (20%). The largest pseudocyst which disappeared after conservative management in the study was of
12.7 cms.
The reported long-term success rate for pseudocyst resolution for USG-guided pseudocyst drainage is
around 50%. Unsuccessful drainages are usually caused by large ductal leaks or obstruction of the main
pancreatic duct[26]. In a small series, the EUS approach has resulted in a success rate of more than 90% in
patients with chronic pseudocysts[27]. The recurrence rate after endoscopic drainage is low, 4%, and the
complication rate is less than 16% [26].In our study, 77% of patients undergoing EUS guided drainage (83.3%)
or ERCP and pancreatic stenting (71.4%) had complete resolution.
DOI: 10.9790/0853-14106101105
www.iosrjournals.org
104 | Page
Pseudocyst of Pancreas: A Clinical Study
A significantly higher mortality rate is associated with surgical therapy (9%) [12]In our study, there
was no mortality associated with surgical therapy. 58.33% patients showed complete resolution (44.44% of
patients undergoing cystogastrostomy and 100% of patients undergoing roux-en-y cystojejunostomy).
VI.
Conclusions
The most common age group in which pseudocysts of pancreas occur is 4 th and 5th decades with
marked male predominance. Alcohol abuse is the most common etiological factor for
pseudocystformation.Abdominal pain is the most common presenting complaint and is usually physical
examination usually reveals abdominal tenderness and/or a palpable mass, most commonly in
epigastrium.Amylase and lipase levels are often elevated, but may be within reference ranges.
USG has several limitations, as compared with CT, in the initial diagnosis of a pseudocyst, but is still
the most commonly used procedure as it is relatively more feasible and cheaper.Endoscopic retrograde
cholangiopancreatography (ERCP) is quite accurate in identifying pseudocysts and pancreatic ductal anomalies
and can be used for therapeutic purposes also.
Surgery is the traditional modality for treating pancreatic pseudocysts, with high success rates and low
morbidity and mortality, and it still plays an important role in therapy. Laparoscopic management has been
reported with very encouraging results, but long-term follow-up has still to show equivalence to open surgery.
Endoscopic therapy is a reasonable alternative to surgery, particularly for chronic pseudocysts, and is
increasingly being used.
References
[1].
[2].
[3].
[4].
[5].
[6].
[7].
[8].
[9].
[10].
[11].
[12].
[13].
[14].
[15].
[16].
[17].
[18].
[19].
[20].
[21].
[22].
[23].
[24].
[25].
[26].
[27].
Gumaste VV, Pitchumoni CS. Pancreatic pseudocyst. Gastroenterologist. 1996;4:33-43.
Sanfey H, Aguilar M, Jones RS. Pseudocysts of the pancreas, a review of 97 cases.Am Surg. 1994;60:661-668.
D'Egidio A, Schein M. Pancreatic pseudocysts: a proposed classification and its management implications. Br J Surg. 1991;78:981984.
D'Egidio A, Schein M. Percutaneous drainage of pancreatic pseudocysts: a prospective study. World J Surg. 1992;16:141-145;
discussion 145-146.
Vitas GJ, Sarr MG. Selected management of pancreatic pseudocysts: operative versus expectant management. Surgery.
1992;111:123-130.
Yeo CJ, Bastidas JA, Lynch-Nyhan A, Fishman EK, Zinner MJ, Cameron JL. The natural history of pancreatic pseudocysts
documented by computed tomography. SurgGynecol Obstet. 1990;170:411-417.
Bradley EL, Clements JL, Jr., Gonzalez AC. The natural history of pancreatic pseudocysts: a unified concept of management. Am J
Surg. 1979;137:135-141.
O'Malley VP, Cannon JP, Postier RG. Pancreatic pseudocysts: cause, therapy, and results. Am J Surg. 1985;150:680-682.
Wade JW. Twenty-five year experience with pancreatic pseudocysts. Are we making progress? Am J Surg. 1985;149:705-708.
Pitchumoni CS, Agarwal N. Pancreatic pseudocysts. When and how should drainage be performed? GastroenterolClin North Am
1999; 28: 615-639
Morgan DE, Baron TH, Smith JK, Robbin ML, Kenney PJ. Pancreatic fluid collections prior to intervention: evaluation with MR
imaging compared with CT and US. Radiology 1997; 203: 773-778
Habashi S, Draganov PV. Pancreatic pseudocyst.World J Gastroenterol. 2009;15:38-47.
Cheruvu CV, Clarke MG, Prentice M, Eyre-Brook IA. Conservative treatment as an option in the management of pancreatic
pseudocyst.Ann R CollSurg Engl. 2003;85:313-316.
Catalano MF, Geenen JE, Schmalz MJ, Johnson GK, Dean RS, Hogan WJ. Treatment of pancreatic pseudocysts with ductal
communication by transpapillary pancreatic duct endoprosthesis.GastrointestEndosc. 1995;42:214-218.
Seewald S, Ang TL, Teng KC, Soehendra N. EUS-guided drainage of pancreatic pseudocysts, abscesses and infected necrosis. Dig
Endosc. 2009;21Suppl 1:S61-65.
Barthet M, Bugallo M, Moreira LS, Bastid C, Sastre B, Sahel J. Management of cysts and pseudocysts complicating chronic
pancreatitis. A retrospective study of 143 patients.GastroenterolClin Biol. 1993;17:270-276.
Johnson LB, Rattner DW, Warshaw AL. The effect of size of giant pancreatic pseudocysts on the outcome of internal drainage
procedures.SurgGynecol Obstet. 1991;173:171-174.
Frey CF. Pancreatic pseudocyst--operative strategy. Ann Surg. 1978;188:652-662.
Bodker A, Kjaergaard J, Schmidt A, Tilma A. Pancreatic pseudocysts: a follow-up study. Ann. Surg. 1981; 194: 80
Varadarajulu S, Bang J, Sutton B, Trevino J, Christein J, Wilcox C. Equal efficacy of endoscopic and surgical cystogastrostomy for
pancreatic pseudocyst drainage in a randomized trial. Gastroenterology 2013;145:583590
Anderson MC, Chapman WC. Pseudocysts of the pancreas. In: Howard JM, Jordan GL, Reber HA, eds. Surgical Diseases of the
Pancreas. Philadelphia: Lea &Febiger, 1987: 564590.
Walt AJ, Bouwman DL, Weaver DW, Sachs RJ.The impact of technology on the management of pancreatic pseudocyst.5th annual
Samuel Jason MixterLecture.ArchSurg 1990; 125: 759-763.
Usatoff V, Brancatisano R, Williamson RC. Operative treatment of pseudocysts in patients with chronic pancreatitis.Br J Surg2000;
87: 1494-1499.
Yin W, Chen H, Huang S, Lin C, Lin S, Shyu D, Wei C, Lee M, Chou A, Tseng K, Chang Y. The role of surgery in pancreatic
pseudocyst. Tzu Chi Med J 2004; 16:359-369
Bradley EL. A clinically based classification system for acute pancreatitis.Summary of the International Symposium on Acute
Pancreatitis, Atlanta, GA, September 11 through 13, 1992.Arch Surg 1993; 128: 586-90.
Yeo CJ, Bastidas JA, Lynch-Nyhan A, Fishman EK, Zinner MJ, Cameron JL. The natural history of pancreatic pseudocysts
documented by computed tomography. SurgGynecolObstet 1990; 170: 411-417
Andersson B, Nilsson E, Willner J, Andersson R. Treatment and outcome in pancreatic pseudocysts. Scand J Gastroenterol2006; 41:
751-756
DOI: 10.9790/0853-14106101105
www.iosrjournals.org
105 | Page
Anda mungkin juga menyukai
- "I Am Not Gay Says A Gay Christian." A Qualitative Study On Beliefs and Prejudices of Christians Towards Homosexuality in ZimbabweDokumen5 halaman"I Am Not Gay Says A Gay Christian." A Qualitative Study On Beliefs and Prejudices of Christians Towards Homosexuality in ZimbabweInternational Organization of Scientific Research (IOSR)Belum ada peringkat
- Attitude and Perceptions of University Students in Zimbabwe Towards HomosexualityDokumen5 halamanAttitude and Perceptions of University Students in Zimbabwe Towards HomosexualityInternational Organization of Scientific Research (IOSR)Belum ada peringkat
- Socio-Ethical Impact of Turkish Dramas On Educated Females of Gujranwala-PakistanDokumen7 halamanSocio-Ethical Impact of Turkish Dramas On Educated Females of Gujranwala-PakistanInternational Organization of Scientific Research (IOSR)Belum ada peringkat
- The Role of Extrovert and Introvert Personality in Second Language AcquisitionDokumen6 halamanThe Role of Extrovert and Introvert Personality in Second Language AcquisitionInternational Organization of Scientific Research (IOSR)Belum ada peringkat
- A Review of Rural Local Government System in Zimbabwe From 1980 To 2014Dokumen15 halamanA Review of Rural Local Government System in Zimbabwe From 1980 To 2014International Organization of Scientific Research (IOSR)Belum ada peringkat
- The Impact of Technologies On Society: A ReviewDokumen5 halamanThe Impact of Technologies On Society: A ReviewInternational Organization of Scientific Research (IOSR)100% (1)
- A Proposed Framework On Working With Parents of Children With Special Needs in SingaporeDokumen7 halamanA Proposed Framework On Working With Parents of Children With Special Needs in SingaporeInternational Organization of Scientific Research (IOSR)Belum ada peringkat
- Relationship Between Social Support and Self-Esteem of Adolescent GirlsDokumen5 halamanRelationship Between Social Support and Self-Esteem of Adolescent GirlsInternational Organization of Scientific Research (IOSR)Belum ada peringkat
- Assessment of The Implementation of Federal Character in Nigeria.Dokumen5 halamanAssessment of The Implementation of Federal Character in Nigeria.International Organization of Scientific Research (IOSR)Belum ada peringkat
- Investigation of Unbelief and Faith in The Islam According To The Statement, Mr. Ahmed MoftizadehDokumen4 halamanInvestigation of Unbelief and Faith in The Islam According To The Statement, Mr. Ahmed MoftizadehInternational Organization of Scientific Research (IOSR)Belum ada peringkat
- Comparative Visual Analysis of Symbolic and Illegible Indus Valley Script With Other LanguagesDokumen7 halamanComparative Visual Analysis of Symbolic and Illegible Indus Valley Script With Other LanguagesInternational Organization of Scientific Research (IOSR)Belum ada peringkat
- An Evaluation of Lowell's Poem "The Quaker Graveyard in Nantucket" As A Pastoral ElegyDokumen14 halamanAn Evaluation of Lowell's Poem "The Quaker Graveyard in Nantucket" As A Pastoral ElegyInternational Organization of Scientific Research (IOSR)Belum ada peringkat
- Edward Albee and His Mother Characters: An Analysis of Selected PlaysDokumen5 halamanEdward Albee and His Mother Characters: An Analysis of Selected PlaysInternational Organization of Scientific Research (IOSR)Belum ada peringkat
- Importance of Mass Media in Communicating Health Messages: An AnalysisDokumen6 halamanImportance of Mass Media in Communicating Health Messages: An AnalysisInternational Organization of Scientific Research (IOSR)Belum ada peringkat
- Topic: Using Wiki To Improve Students' Academic Writing in English Collaboratively: A Case Study On Undergraduate Students in BangladeshDokumen7 halamanTopic: Using Wiki To Improve Students' Academic Writing in English Collaboratively: A Case Study On Undergraduate Students in BangladeshInternational Organization of Scientific Research (IOSR)Belum ada peringkat
- Role of Madarsa Education in Empowerment of Muslims in IndiaDokumen6 halamanRole of Madarsa Education in Empowerment of Muslims in IndiaInternational Organization of Scientific Research (IOSR)Belum ada peringkat
- Designing of Indo-Western Garments Influenced From Different Indian Classical Dance CostumesDokumen5 halamanDesigning of Indo-Western Garments Influenced From Different Indian Classical Dance CostumesIOSRjournalBelum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5795)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Illizarov and Principle of Distraction OsteogenesisDokumen7 halamanIllizarov and Principle of Distraction OsteogenesisThiru MuruganBelum ada peringkat
- Substance Abuse and Traumatic Brain Injury: John D. Corrigan, PHDDokumen50 halamanSubstance Abuse and Traumatic Brain Injury: John D. Corrigan, PHDSilvanaPutriBelum ada peringkat
- Supine Versus Prone Position For Percutaneous Nephrolit - 2019 - International JDokumen10 halamanSupine Versus Prone Position For Percutaneous Nephrolit - 2019 - International JFelicia JesslynBelum ada peringkat
- 27Dokumen2 halaman27Helen UgochukwuBelum ada peringkat
- GlioblastomaDokumen2 halamanGlioblastomaDaniela BulmagăBelum ada peringkat
- 65 Interview Questions For Nurses.13Dokumen3 halaman65 Interview Questions For Nurses.13natalieshirleyBelum ada peringkat
- Cystic Fibrosis: Meet The Client: Debbie BakerDokumen8 halamanCystic Fibrosis: Meet The Client: Debbie BakerJasjit Singh100% (1)
- ProRoot MTA BrochureDokumen12 halamanProRoot MTA BrochureAdela FechetaBelum ada peringkat
- Acutrak2 Radial Head Case StudyDokumen2 halamanAcutrak2 Radial Head Case StudyDinesh KumarBelum ada peringkat
- EclampsiaDokumen14 halamanEclampsiaUmi PulunganBelum ada peringkat
- Great Critical Care ReliefDokumen9 halamanGreat Critical Care ReliefBenedict FongBelum ada peringkat
- 10th Monthly Compliance Report On Parkland Memorial HospitalDokumen92 halaman10th Monthly Compliance Report On Parkland Memorial HospitalmilesmoffeitBelum ada peringkat
- Oral Probiotic Treatment of Lactobacillus Rhamnosus Lcr35® Prevents Visceral Hypersensitivity To A Colonic Inflammation and An Acute Psychological StressDokumen13 halamanOral Probiotic Treatment of Lactobacillus Rhamnosus Lcr35® Prevents Visceral Hypersensitivity To A Colonic Inflammation and An Acute Psychological StressMaria TejedaBelum ada peringkat
- Remifentanil Versus Propofol/Fentanyl Combination in Procedural Sedation For Dislocated Shoulder Reduction A Clinical TrialDokumen5 halamanRemifentanil Versus Propofol/Fentanyl Combination in Procedural Sedation For Dislocated Shoulder Reduction A Clinical TrialerinBelum ada peringkat
- Juvenile Idiopathic Arthritis in A Premature Baby: Rare Case ReportDokumen3 halamanJuvenile Idiopathic Arthritis in A Premature Baby: Rare Case ReportKevin Wladimir ChanchicochaBelum ada peringkat
- Intake and Output PPT - 1Dokumen44 halamanIntake and Output PPT - 1Prajna TiwariBelum ada peringkat
- Irda Non Payable ListDokumen21 halamanIrda Non Payable ListMUKESH SINGHBelum ada peringkat
- Praposal DM-1Dokumen117 halamanPraposal DM-1sanjay sabdeBelum ada peringkat
- Keith R Poskitt - Chronic Ulceration of The LegDokumen5 halamanKeith R Poskitt - Chronic Ulceration of The LegKovoor LedchumananBelum ada peringkat
- 5 Altered Nutrition Less Than Body Requirements Chronic Renal Failure Nursing Care PlansDokumen3 halaman5 Altered Nutrition Less Than Body Requirements Chronic Renal Failure Nursing Care Plansjustin_sane40% (5)
- Heidi Agustin Joseph Azevedo Alternative Nutrition CounselingDokumen16 halamanHeidi Agustin Joseph Azevedo Alternative Nutrition Counselingapi-242435158Belum ada peringkat
- Institute of Nursing: Far Eastern UniversityDokumen3 halamanInstitute of Nursing: Far Eastern UniversityaleccespirituBelum ada peringkat
- Selective Awareness TherapyDokumen10 halamanSelective Awareness TherapyHashem Al AttasBelum ada peringkat
- Case Analysis 13 - Hirschsprungs DiseaseDokumen5 halamanCase Analysis 13 - Hirschsprungs DiseaseAHOUR PANGILAYANBelum ada peringkat
- AgonistsDokumen25 halamanAgonistsOfficially RandomBelum ada peringkat
- Dilation and CurettageDokumen15 halamanDilation and Curettagenautilus81Belum ada peringkat
- Skradski Jaclyn CVDokumen6 halamanSkradski Jaclyn CVapi-293245490Belum ada peringkat
- Dr.H.O.GUNEWARDENE (Folder)Dokumen38 halamanDr.H.O.GUNEWARDENE (Folder)Ian GardnerBelum ada peringkat
- Histotechnologist, ImmunohistochemistDokumen3 halamanHistotechnologist, Immunohistochemistapi-78178945Belum ada peringkat
- A Clinical Success in The Management of Kotha (Digital Gangrene) by Leech Therapyandpanchtiktaghritaguggulu - A Single Case StudyDokumen5 halamanA Clinical Success in The Management of Kotha (Digital Gangrene) by Leech Therapyandpanchtiktaghritaguggulu - A Single Case StudyIJAR JOURNALBelum ada peringkat