Jaad O: Nline
Diunggah oleh
punish0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
34 tayangan2 halamanljopikjg
Judul Asli
1-s2.0-S0190962214009992-main
Hak Cipta
© © All Rights Reserved
Format Tersedia
PDF, TXT atau baca online dari Scribd
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen Iniljopikjg
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PDF, TXT atau baca online dari Scribd
0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
34 tayangan2 halamanJaad O: Nline
Diunggah oleh
punishljopikjg
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PDF, TXT atau baca online dari Scribd
Anda di halaman 1dari 2
JAAD ONLINE
CASE
LETTERS
Ophthalmic cyclosporine for the treatment of
psoriatic conjunctivitis
To the Editor: A 54-year-old woman with a history of
moderate to severe psoriasis and psoriatic arthritis
presented with red scaly plaques on her knees,
elbows, and trunk affecting 8% of her total body
surface area. She reported contemporaneous onset
of her psoriasis and conjunctivitis. Bilateral conjunctival injection was noted with no exudates, photophobia, miosis, or eyelid edema (Fig 1). Physical
exam was otherwise normal. Past medical history
included hypertension, diabetes, and depression.
Medications included metformin, enalapril, and
amlodipine. The patient had failed treatment with
etanercept and adalimumab in the past. She was
started on a regimen of 5- to 10-mg/kg infliximab
intravenous (IV) infusion every 4 to 6 weeks. After 5
rounds of treatment, her conjunctival erythema had
cleared completely and her psoriasis had improved.
The infliximab was discontinued prematurely due to
a lapse in her insurance coverage. After 2 months
without systemic treatment, the conjunctival injection recurred bilaterally, at which time she was
started on cyclosporine ophthalmic emulsion
0.05%, 1 drop in each eye twice daily, and methotrexate 20 mg/week. On follow-up at 11 days, the
conjunctivitis had completely resolved (Fig 2).
Ocular involvement occurs in approximately 10%
of psoriasis patients and commonly includes
conjunctivitis, keratoconjunctivitis sicca, and uveitis.1,2 An ophthalmology referral at initial presentation is suggested to assess the degree of ocular
involvement and for ongoing monitoring. The prevalence of conjunctivitis in psoriasis patients has been
reported to be as high as 64.5%.1 Karabulut et al3
found that the conjunctival epithelial cells of psoriasis patients lacking clinical ocular disease demonstrated increased rates of squamous metaplasia
compared with controls, with no correlation between the presence of squamous metaplasia and
duration of skin disease. They also found increased
rates of neutrophil clumping in the conjunctival
tissue of these patients, reminiscent of the epidermal
microabscesses pathognomonic of psoriasis. Their
findings suggest a common underlying disease process, as in our patient, whose conjunctivitis responded independently to both IV infliximab and
ophthalmic cyclosporine. Her rapid response to
treatment after relapse is most likely attributable to
treatment with cyclosporine, which has a faster onset
J AM ACAD DERMATOL
Open access under CC BY-NC-ND license.
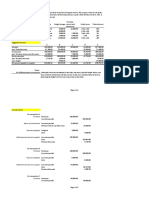
Fig 1. Psoriatic conjunctivitis at baseline.
Fig 2. Psoriatic conjunctivitis resolved after treatment with
ophthalmic cyclosporine.
of action than methotrexate. Her comorbid psoriatic
arthritis further supports the notion that the conjunctivitis was a manifestation of her underlying disease,
in that ocular inflammation is a common feature of
overlap among the seronegative arthritides.4
Ophthalmic cyclosporine has demonstrated an
excellent safety profile with minimal intraocular
penetration and absorption in the bloodstream and
has been successful for the treatment of several
inflammatory ocular surface disorders including
allergic conjunctivitis, vernal keratoconjunctivitis,
posterior blepharitis, and ocular rosacea.5 Our case
suggests that ophthalmic cyclosporine may also be a
treatment option for ocular psoriasis.
Kaiane A. Habeshian, BS,a and Jacob Oren Levitt,
MDb
Geisel School of Medicine at Dartmouth,a
Hanover, New Hampshire, and Department of
Dermatology,b Mount Sinai Hospital, New York
Funding sources: None.
Conflicts of interest: None declared.
Correspondence to: Jacob Oren Levitt, MD, 5 East
98th Street, 5th Floor, Box 1048, New York, NY,
10029
E-mail: jacoblevittmd@gmail.com
REFERENCES
1. Erbagci I, Erbagci Z, Gungor K, Berkir N. Ocular anterior
segment pathologies and tear film changes in patients with
psoriasis vulgaris. Acta Med Okayama 2003;57:299-303.
2. Au S, Yaniv S, Gottlieb AB. Psoriatic eye manifestations.
Psoriasis Forum 2011;17:169-79.
AUGUST 2014 e43
J AM ACAD DERMATOL
e44 Letters
AUGUST 2014
3. Karabulut AA, Yalvac IS, Vahaboglu H, Nurozler AB, Duman S.
Conjunctival impression cytology and tear-film changes in
patients with psoriasis. Cornea 1999;18:544-8.
4. Lambert JR, Wright V. Eye inflammation in psoriatic arthritis.
Ann Rheum Dis 1976;35:354-6.
5. Utine CA, Stern M, Akpek EK. Clinical review: topical
ophthalmic use of cyclosporine A. Ocular Immunol Inflamm
2010;18:352-61.
http://dx.doi.org/10.1016/j.jaad.2013.12.034
Chronic granulomatous disease presenting
with ecthyma gangrenosum in a neonate
To the Editor: While the primary immunodeficiency
chronic granulomatous disease (CGD) frequently
presents with cutaneous manifestations, associated
ecthyma gangrenosum (EG) has rarely been reported. EG is an ulcerative infection, typically caused
by Pseudomonas aeruginosa in immunocompromised patients. We report a 23-day-old male with
EG due to Klebsiella oxytoca, who was subsequently
diagnosed with CGD. This case emphasizes the
importance of initiating broad antibiotic coverage
and immunologic work-up in infants with EG.
A 23-day-old term male presented to our institution febrile with temperature up to 39.28C and a 1week history of erythema of the perineum that
progressed to pustules and ulcerations. Family and
social histories were noncontributory. Upon admission, vancomycin and acyclovir were initiated by the
pediatrics team.
Because the ulcerations were not improving, a
dermatology consult was initiated. Upon examination, irregularly shaped ulcerations were noted in the
perineum and buttocks (Fig 1). Given concern for
EG, ceftazidime was added. Wound care included
gentamicin ointment and white petrolatum. Work-up
was significant for leukocytosis and elevated band
count. Blood cultures, herpes simplex virus polymerase chain reaction, and lesional viral cultures
were negative. Bacterial wound cultures grew
Klebsiella oxytoca and Enterococcus faecium, confirming a diagnosis of EG. Klebsiella oxytoca was
thought to be the primary pathogen, but antibiotics
also covered Enterococcus faecium. The patients
ulcerations dramatically improved within 1 week of
antimicrobial therapy (Fig 2).
Diagnosis of EG prompted an immunologic
investigation that was remarkable for dihydrorhodamine 123 (DHR); flow cytometric analysis showed
no granulocyte oxidase activity. Work-up of the
patients mother showed oxidative abnormalities in
70% of granulocytes, confirming X-linked CGD in
our patient. After diagnosis, the patient was started
on prophylactic itraconazole, trimethoprim/sulfamethoxazole, and interferon-gamma.
Fig 1. Ecthyma gangrenosum in neonatal chronic granulomatous disease. Multiple deep ulcerations of the left
buttock, right perianal area, and perineum following 2
days of antibiotic therapy and wound care.
Fig 2. Ecthyma gangrenosum in neonatal chronic granulomatous disease. Dramatic healing of ulcerations
following 9 days of antibiotic therapy and wound care.
CGD is a rare primary immunodeficiency caused
by defective formation of the phagocyte respiratory
burst. It results in recurrent bacterial and fungal
infections, which can lead to granuloma formation.1-3 Cutaneous infections affect 60% to 70% of
patients with CGD.2 Inheritance of CGD is usually
X-linked, but can be autosomal recessive. DHR has
replaced nitroblue tetrazolium as the confirmatory
test given its ability to differentiate subtypes.
In our patient, EG was the presenting manifestation
of CGD. EG has been reported only once
previously with CGD; however, that pathogen
was Chromobacterium violaceum.1 EG is a rare infection, characteristically seen in immunocompromised
Anda mungkin juga menyukai
- Case Study CAPS PDFDokumen5 halamanCase Study CAPS PDFCitra KristiBelum ada peringkat
- Orbital Apex Syndrome Secondary To Herpes Zoster OphthalmicusDokumen4 halamanOrbital Apex Syndrome Secondary To Herpes Zoster OphthalmicusYosiita KartinaaBelum ada peringkat
- Haemophilus Influenzae Associated ScleritisDokumen4 halamanHaemophilus Influenzae Associated ScleritisHackerBelum ada peringkat
- 10 1016@j Jaad 2012 12 513Dokumen1 halaman10 1016@j Jaad 2012 12 513Kuro ChanBelum ada peringkat
- Zoster Sine HerpeteDokumen7 halamanZoster Sine HerpeteLalo RCBelum ada peringkat
- MUCORMYCOSISDokumen4 halamanMUCORMYCOSISipe.jacobBelum ada peringkat
- Jurnal 1Dokumen4 halamanJurnal 1tiara haprlBelum ada peringkat
- Tubercular Posterior SchleritisDokumen6 halamanTubercular Posterior SchleritisInayatul muthmainnahBelum ada peringkat
- MainDokumen3 halamanMainomidazadmehr1375Belum ada peringkat
- Laporan Kasus Ulkus Kornea Jamur Dengan Hipopion .Eva RiantiDokumen21 halamanLaporan Kasus Ulkus Kornea Jamur Dengan Hipopion .Eva RiantiBenk Setsuna F. SeieiBelum ada peringkat
- Imprimir 2Dokumen3 halamanImprimir 2Gino VitteriBelum ada peringkat
- Acute Necrotizing Panophthalmitis in Seropositive Case of ChikungunyaDokumen3 halamanAcute Necrotizing Panophthalmitis in Seropositive Case of ChikungunyaPratyushBelum ada peringkat
- The Kaohsiung J of Med Scie - 2013 - Tsai - Pyoderma Gangrenosum Intractable Leg Ulcers in Sjogren S SyndromeDokumen2 halamanThe Kaohsiung J of Med Scie - 2013 - Tsai - Pyoderma Gangrenosum Intractable Leg Ulcers in Sjogren S SyndromeAsad KakarBelum ada peringkat
- Staphylococcus Epidermidis End PDFDokumen4 halamanStaphylococcus Epidermidis End PDFNisaBelum ada peringkat
- 38surekha EtalDokumen3 halaman38surekha EtaleditorijmrhsBelum ada peringkat
- Cefixime Induced Stevens-Johnson Syndrome A Case Report and Review of LiteratureDokumen2 halamanCefixime Induced Stevens-Johnson Syndrome A Case Report and Review of LiteratureDorainne JohnsonBelum ada peringkat
- 7692-Article Text-30295-3-10-20200319 PDFDokumen4 halaman7692-Article Text-30295-3-10-20200319 PDFHata BotonjicBelum ada peringkat
- Conjunctivitis As A Manifestation of Wegener 'S GranulomatosisDokumen5 halamanConjunctivitis As A Manifestation of Wegener 'S GranulomatosisAsd DsaBelum ada peringkat
- JurnalDokumen3 halamanJurnalAulia Kamal Ansari PanggabeanBelum ada peringkat
- JurnalMata Pigrum Keratitis 1471-2415!13!31Dokumen4 halamanJurnalMata Pigrum Keratitis 1471-2415!13!31Alfrino Patriando AdamBelum ada peringkat
- Letter To The EditorsDokumen1 halamanLetter To The Editorsfelaxis fBelum ada peringkat
- Junal PyodermaDokumen6 halamanJunal PyodermaJares Clinton Saragih SimarmataBelum ada peringkat
- Tatalaksana Ulkus Kornea Yang Disebabkan Oleh Methycillin Resistant Staphylococcus Haemolyticus MRSH - Mia NursalamahDokumen14 halamanTatalaksana Ulkus Kornea Yang Disebabkan Oleh Methycillin Resistant Staphylococcus Haemolyticus MRSH - Mia NursalamahYA MAAPBelum ada peringkat
- Ocular Erythema Nodosum Leprosum An Immunohistochemical StudyDokumen3 halamanOcular Erythema Nodosum Leprosum An Immunohistochemical StudyRathinamBelum ada peringkat
- Chronic Bullous Disease of Childhood and Pneumonia in A Neonate With VATERL Association and Hypoplastic Paranasal SinusesDokumen2 halamanChronic Bullous Disease of Childhood and Pneumonia in A Neonate With VATERL Association and Hypoplastic Paranasal SinusesCharissa Mia D. Salud-GniloBelum ada peringkat
- Annals of Medicine and SurgeryDokumen3 halamanAnnals of Medicine and SurgeryAfifah Siti NurBelum ada peringkat
- Pustular Psoriasis Complicated With Acute Generalized Exanthematous Pustulosis.Dokumen4 halamanPustular Psoriasis Complicated With Acute Generalized Exanthematous Pustulosis.pancholarpancholarBelum ada peringkat
- Necrotisans Erythema Nodosum Leprosum With Systemic ManifestDokumen1 halamanNecrotisans Erythema Nodosum Leprosum With Systemic Manifestzak bearBelum ada peringkat
- BachmanDokumen1 halamanBachmanotheasBelum ada peringkat
- American Journal of Ophthalmology Case Reports: Yael Sharon, David S. Chu TDokumen5 halamanAmerican Journal of Ophthalmology Case Reports: Yael Sharon, David S. Chu TDaviel Quin DavBelum ada peringkat
- Rhinocerebral Mucormycosis Case ReportDokumen3 halamanRhinocerebral Mucormycosis Case ReportYani ManuelBelum ada peringkat
- Jurding Mata EndophthalamitisDokumen24 halamanJurding Mata EndophthalamitisBenk Setsuna F. SeieiBelum ada peringkat
- Penetrating Keratoplasty in Active Acanthamoeba KeratitisDokumen5 halamanPenetrating Keratoplasty in Active Acanthamoeba Keratitisdrvishalkulkarni2007Belum ada peringkat
- Crs LinDokumen4 halamanCrs LinPoolerErBelum ada peringkat
- Proptosis UnilateralDokumen5 halamanProptosis UnilateralCarlos NiveloBelum ada peringkat
- 2012 A Case Report of Mucormycosis of Faciotemporal Region Mimicking As Bacterial Necrotizing FasciitisDokumen5 halaman2012 A Case Report of Mucormycosis of Faciotemporal Region Mimicking As Bacterial Necrotizing FasciitisWaqar JeelaniBelum ada peringkat
- Amniotic Membrane Transplantation Combined With Antiviral and Steroid Therapy For Herpes Necrotizing Stromal KeratitisDokumen7 halamanAmniotic Membrane Transplantation Combined With Antiviral and Steroid Therapy For Herpes Necrotizing Stromal KeratitisnelyBelum ada peringkat
- 0034 7280 Rbof 76 04 0213Dokumen3 halaman0034 7280 Rbof 76 04 0213syramadhantiBelum ada peringkat
- Primary Conjunctival Tuberculosis-2Dokumen3 halamanPrimary Conjunctival Tuberculosis-2puutieBelum ada peringkat
- Argon Laser Phototherapy in The Treatment of Refractory Fungal Keratitis.Dokumen3 halamanArgon Laser Phototherapy in The Treatment of Refractory Fungal Keratitis.Rodrigo BarreraBelum ada peringkat
- Acute Necrotizing Sinusitis Caused by Staphylococcus Lugdunensis 2011Dokumen3 halamanAcute Necrotizing Sinusitis Caused by Staphylococcus Lugdunensis 2011J Sebastian PeinadoBelum ada peringkat
- Ulkus Kornea. Pendekatan Diagnostik .IndriyaniDokumen13 halamanUlkus Kornea. Pendekatan Diagnostik .IndriyaniAvabel Player 1Belum ada peringkat
- Challenging Treatment of Bilateral Multiple Infection Panuveitis in HIV/AIDS PatientsDokumen5 halamanChallenging Treatment of Bilateral Multiple Infection Panuveitis in HIV/AIDS PatientsRosyid PrasetyoBelum ada peringkat
- Tozinameran Induced AGEP-DRESSDokumen2 halamanTozinameran Induced AGEP-DRESSCHONG WEI SHENGBelum ada peringkat
- Ofy 038Dokumen5 halamanOfy 038Rosandi AdamBelum ada peringkat
- Ad 32 334Dokumen3 halamanAd 32 334Nurvia AndrianiBelum ada peringkat
- Reversal Reaction With Nodules That Initially Diagnosed As Erythema Nodosum Leprosum in Borderline Lepromatous LeprosyDokumen6 halamanReversal Reaction With Nodules That Initially Diagnosed As Erythema Nodosum Leprosum in Borderline Lepromatous Leprosysilvavitria mandenasBelum ada peringkat
- Observations On Time Course Changes of The CherryDokumen16 halamanObservations On Time Course Changes of The CherryAndi Tiara S. AdamBelum ada peringkat
- Soal IimDokumen16 halamanSoal IimramadhanihidayatdwiputraBelum ada peringkat
- Contact LensDokumen6 halamanContact LensReno Prananditya AshafBelum ada peringkat
- PIIS0008418219302121Dokumen4 halamanPIIS0008418219302121J MBelum ada peringkat
- Cutaneous Aspergilosis Caused by Aspergillus Flavus: A Case ReportDokumen6 halamanCutaneous Aspergilosis Caused by Aspergillus Flavus: A Case ReportAditya Yudha PratamaBelum ada peringkat
- Tatalaksana Ulkus Kornea Jamur Dematiaceae - Andivan RahmanDokumen12 halamanTatalaksana Ulkus Kornea Jamur Dematiaceae - Andivan RahmanazkaBelum ada peringkat
- Atypical Case of Presumed Ocular Tuberculosis Presenting As Unilateral Occlusive VasculitisDokumen4 halamanAtypical Case of Presumed Ocular Tuberculosis Presenting As Unilateral Occlusive VasculitisInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Conjunctivitis Due To Neisseria Sicca: A Case Report: ReferencesDokumen4 halamanConjunctivitis Due To Neisseria Sicca: A Case Report: ReferencesnidaBelum ada peringkat
- Rheumatoid Arthritis Associated Scleritis OPHTHALMOLOGY MCQSDokumen5 halamanRheumatoid Arthritis Associated Scleritis OPHTHALMOLOGY MCQSkishorechandraBelum ada peringkat
- Tubercular ScleritisDokumen5 halamanTubercular Scleritismutya yulindaBelum ada peringkat
- Acute Epiglottitis in The Immunocompromised Host: Case Report and Review of The LiteratureDokumen5 halamanAcute Epiglottitis in The Immunocompromised Host: Case Report and Review of The Literaturerosandi sabollaBelum ada peringkat
- Kel 6aDokumen11 halamanKel 6apunishBelum ada peringkat
- Jadwal Stase Divisi Dokter Muda IKA Apif AuliaDokumen9 halamanJadwal Stase Divisi Dokter Muda IKA Apif AuliapunishBelum ada peringkat
- 1768OCv1Dokumen27 halaman1768OCv1punishBelum ada peringkat
- Clin Infect Dis. 2010 Minion 997 9Dokumen3 halamanClin Infect Dis. 2010 Minion 997 9punishBelum ada peringkat
- Ibrt 06 I 4 P 232Dokumen2 halamanIbrt 06 I 4 P 232Aditia Nata KusumaBelum ada peringkat
- Ni Hms 142733Dokumen16 halamanNi Hms 142733punishBelum ada peringkat
- 2032Dokumen10 halaman2032punishBelum ada peringkat
- 1 s2.0 S1319453414000356 MainDokumen6 halaman1 s2.0 S1319453414000356 MainpunishBelum ada peringkat
- 1 s2.0 S1198743X14632353 MainDokumen3 halaman1 s2.0 S1198743X14632353 MainpunishBelum ada peringkat
- 355Dokumen6 halaman355punishBelum ada peringkat
- 1 s2.0 S1319453414000356 MainDokumen6 halaman1 s2.0 S1319453414000356 MainpunishBelum ada peringkat
- 1 s2.0 S0161642015007034 MainDokumen2 halaman1 s2.0 S0161642015007034 MainpunishBelum ada peringkat
- 1 s2.0 S1319453414000836 MainDokumen1 halaman1 s2.0 S1319453414000836 MainpunishBelum ada peringkat
- 1 s2.0 S1319453414000411 MainDokumen7 halaman1 s2.0 S1319453414000411 MainpunishBelum ada peringkat
- 1 s2.0 S0161642015007034 MainDokumen2 halaman1 s2.0 S0161642015007034 MainpunishBelum ada peringkat
- 1 s2.0 S0161642015005485 MainDokumen9 halaman1 s2.0 S0161642015005485 MainpunishBelum ada peringkat
- 1 s2.0 S1198743X14632353 MainDokumen3 halaman1 s2.0 S1198743X14632353 MainpunishBelum ada peringkat
- Classification of Hand Eczema Clinical and Aetiological TypesDokumen10 halamanClassification of Hand Eczema Clinical and Aetiological Typeswilliam28assholeBelum ada peringkat
- Features of Staphylococcus Aureus Colonization in Patients With NummularDokumen4 halamanFeatures of Staphylococcus Aureus Colonization in Patients With Nummularwilliam28assholeBelum ada peringkat
- Lecture 4 EMADokumen36 halamanLecture 4 EMAYai IbrahimBelum ada peringkat
- The Mystery of Putins DissertationDokumen16 halamanThe Mystery of Putins DissertationDoinaCebanuBelum ada peringkat
- 8 - Packed Tower Design-1Dokumen65 halaman8 - Packed Tower Design-1M.H vafaeiBelum ada peringkat
- Project Report - Performance Anaylysis of Mutual Funds in IndiaDokumen52 halamanProject Report - Performance Anaylysis of Mutual Funds in Indiapankaj100% (1)
- Preliminary Exam (Primark)Dokumen4 halamanPreliminary Exam (Primark)Zybel RosalesBelum ada peringkat
- Baptismal DelayDokumen20 halamanBaptismal DelayfiohdiohhodoBelum ada peringkat
- Unit 2: TransducerDokumen24 halamanUnit 2: TransducerROYAL GAMER YTBelum ada peringkat
- 31504647-Antenna System (On Tower) Installation Standard ModelDokumen27 halaman31504647-Antenna System (On Tower) Installation Standard ModelBadr AmerBelum ada peringkat
- D6 Gamemasters Aid Screen Weg51019eOGLDokumen40 halamanD6 Gamemasters Aid Screen Weg51019eOGLMr DM100% (1)
- Australia Harvesting Rainwater For Environment, Conservation & Education: Some Australian Case Studies - University of TechnologyDokumen8 halamanAustralia Harvesting Rainwater For Environment, Conservation & Education: Some Australian Case Studies - University of TechnologyFree Rain Garden ManualsBelum ada peringkat
- Defining The Christian Faith PaperDokumen8 halamanDefining The Christian Faith Paperlin tongBelum ada peringkat
- Handout No. 03 - Purchase TransactionsDokumen4 halamanHandout No. 03 - Purchase TransactionsApril SasamBelum ada peringkat
- B2 UNIT 6 Test StandardDokumen6 halamanB2 UNIT 6 Test StandardКоваленко КатяBelum ada peringkat
- Heat Cured ElastomersDokumen40 halamanHeat Cured ElastomerslberrierBelum ada peringkat
- Nemo Outdoor 8.40 User Guide PDFDokumen392 halamanNemo Outdoor 8.40 User Guide PDFXxbugmenotxXBelum ada peringkat
- 3.6 A 40Nm Cmos Highly Linear 0.4-To-6Ghz Receiver Resilient To 0Dbm Out-Of-Band BlockersDokumen3 halaman3.6 A 40Nm Cmos Highly Linear 0.4-To-6Ghz Receiver Resilient To 0Dbm Out-Of-Band Blockershaoyue huangBelum ada peringkat
- MBTI - 4 Temperaments: Guardians (SJ) Rationals (NT) Idealists (NF) Artisans (SP)Dokumen20 halamanMBTI - 4 Temperaments: Guardians (SJ) Rationals (NT) Idealists (NF) Artisans (SP)Muhammad Fauzan MauliawanBelum ada peringkat
- Final Project Part-3 Marketing PlanDokumen8 halamanFinal Project Part-3 Marketing PlanIam TwinStormsBelum ada peringkat
- Artikel 8 - (CURRICULUM EVALUATION)Dokumen12 halamanArtikel 8 - (CURRICULUM EVALUATION)Kikit8Belum ada peringkat
- Combustion FundamentalsDokumen30 halamanCombustion FundamentalsPrem SagarBelum ada peringkat
- Lac MapehDokumen4 halamanLac MapehChristina Yssabelle100% (1)
- 7th Nani Palkhiwala Research Paper CompetitionDokumen31 halaman7th Nani Palkhiwala Research Paper CompetitionhridhaykhuranaBelum ada peringkat
- Chemistry Module 3Dokumen14 halamanChemistry Module 3MASHBelum ada peringkat
- SIDPAC Standard Data Channels: Ch. No. Symbols Description UnitsDokumen2 halamanSIDPAC Standard Data Channels: Ch. No. Symbols Description UnitsRGFEBelum ada peringkat
- Ca Final Compiler Paper 5 Advanced Management Accounting PDFDokumen432 halamanCa Final Compiler Paper 5 Advanced Management Accounting PDFAnn SerratoBelum ada peringkat
- Working With Hierarchies External V08Dokumen9 halamanWorking With Hierarchies External V08Devesh ChangoiwalaBelum ada peringkat
- What Is E-CollaborationDokumen7 halamanWhat Is E-CollaborationToumba LimbreBelum ada peringkat
- Al Rafay ProfileDokumen8 halamanAl Rafay ProfileRana UsmanBelum ada peringkat
- Nur Syamimi - Noor Nasruddin - Presentation - 1002 - 1010 - 1024Dokumen14 halamanNur Syamimi - Noor Nasruddin - Presentation - 1002 - 1010 - 1024abdulhasnalBelum ada peringkat
- Service Instruction Selection of Suitable Operating Fluids For ROTAX Engine Type 916 I (Series), 915 I (Series), 912 I (Series), 912 and 914 (Series)Dokumen15 halamanService Instruction Selection of Suitable Operating Fluids For ROTAX Engine Type 916 I (Series), 915 I (Series), 912 I (Series), 912 and 914 (Series)Martin PilatiBelum ada peringkat