Bernardo Morne
Diunggah oleh
CohenHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Bernardo Morne
Diunggah oleh
CohenHak Cipta:
Format Tersedia
Version
2011.11.03.22
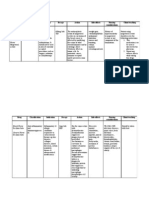
2011 Medical Scheme Quotation
RESOLUTION
Foundation 5501-7500
M Bernardo
2011/07/07
Quote Ref : 496317 Pay 3 children
SCHEME OPTION:
Description of Cover:
Principal Member
Adult Dependant no. 1
Discovery
Keycare Plus
3901-6250
MEDIHELP
Necesse
0 - 7500
Pay 3 Children
Pay 4 Children
TOPMED
Network 3501-7500
Pay 4 children
H1
G2
D1
B1
(Income R5 501 - R7 500)
(Income R3 901 - R6 250)
(Income 0 - 7500)
(Income R3 501 - R7 500)
Capitation
Capitation
Capitation
(Private Network)
Capitation
(CareCross)
Risk Contribution
Risk Contribution
Risk Contribution
Risk Contribution
R 670
R 512
R 533
R 533
R 684
R 540
R 763
R 763
Risk Only
Risk Only
Risk Only
Risk Only
R 45
R 45
R 45
R 45
R 1,227
R 1,111
R 1,269
R 1,571
R 60
R 53
R 62
R 77
R 1,287
R 1,164
R 1,331
R 1,648
Zurreal4Life Platinum - R145 per family
KeyFIT R33/Vitality R145 (Both R158)
N/A
Multiply - R146
Various products available
ranging from R80 - R95
Various products available
ranging from R80 - R95
Various products available
ranging from R80 - R95
Various products available
ranging from R80 - R95
Service Fee: A fee is included in the total for assisting members with: claims /
query resolution, annual personal assistance at option renewal, quartely news
letter etc.
Total Monthly Contribution
(Including R45 Service Fee)
Late Joiner Penalty
(This penalty will be added to your premium every month)
Total Monthly Contribution with Late Joiner Penalty
Optional Loyalty Club
Gap Cover:
Optional Insurance product that provides cover for specialist's fee's whilst
hospitalised, above 100% of Scheme Tariff up to 400% of Scheme Tariff.
Terms will apply.
This summary is for information purposes only and does not supersede the Rules of a Scheme. In the event of any discrepancy between the summary and the Rules of a Scheme, the Rules will prevail.
Underwriting that can be applied to your membership:
3 Month general waiting period
12 month exclusion on pre-existing condition
Late joiner penalty
Advice Provided by:
Optivest - a licensed financial services provider: FSB 13475
Optivest in an Independent healthcare consultancy organisation that strives to present
clients with the highest level of service and does not have shareholding or direct interest
in any medical scheme or medical scheme administrator.
Jackie Verster
Marketing Consultant
OPTIVEST HEALTH SERVICES
Tel: 021 970 6897
Fax: 0866 875 501
Email: jverster@optivest.co.za
FSB license: 13475
Page 1 (of 3)
SCHEME OPTION:
H1
G2
D1
B1
(Income R5 501 - R7 500)
(Income R3 901 - R6 250)
(Income 0 - 7500)
(Income R3 501 - R7 500)
100% of Scheme Tariff
100% of Scheme Tariff
100% of Scheme Tariff
100% of Scheme Tariff
Network Hospitals
Network
Any Hospital
Any Hospital
None
(co-payments apply)
None
IN HOSPITAL BENEFITS:
Rate of Cover for Specialist fees during hospitalisation
Hospitals that may be utilized
(Pre-authorisation is required before treatment starts, or in case of an emergency
within the next two business days)
Overall limits & Deductibles
Listed Procedures: Procedures normally performed in hospital, performed in
Doctor's room/Day Ward e.g.Gastroscopy, etc.
R800 000 Per Family
Unlimited - Subject to pre-authorisation. R1000
In Hospital: Unlimited at Network Hospitals. *CoCovered in Network of Day-Case facilities within
payments apply - see below
co-payment unauthorised non-emercency
50km radius, otherwise Keycare Network hospital
Out of Hospital: Unlimited at Network Provider
admission
None
Colonoscopy, Endoscopy, Gastroscopy in doctor's
rooms/as day case in hospital under concious
sedation, unless clinically appropriate for general
anaestetic - req pre-auth at 100% of Scheme Tariff
In Hospital: Normal delivery: 3 days & 2 nights.
Caesar: 4 days & 3 nights
Out of Hospital: 2 x 2D scans
In Hospital: Unlimited
Out of Hospital: 4 Antenatal visits, 1 Scan and
selected blood test - referred by KeyCare
Network doctor
In Hospital: R16 000 per confinement, subject to
OAL. Out of Hospital: Ltd to 2 Sonars & 2
Specialist consultations per pregnancy, within
Network.
In Hospital: Unlimited (limited to 1 birth per family
per year). Out of Hospital: Pre & postnatal care
provided by Carecross provider,up to 20 weeks,
2 Ultrasound Scans
Covered at Network Provider. Subject to PMB
21 Days per beneficiary
Prescribed Minimum Benefits
Prescribed Mininum Benefits only
Covered at Network Provider. Subject to PMB
In Hospital: Unlimited if related to approved
hospital event (back & neck not covered)
Out of Hospital: Ltd to R2100 per beneficiary
(paid from Specialist benefit)
In and out of Hospital: R10 000 per family per
year
In Hospital: Unlimited - subject to preauthorisation
Out of Hospital: No Benefit
Unlimited through ICON Network. Protocols apply
Cover PMB at cancer specialist in the ICON
network. Register on the Oncology Programme
Subject to ICON Oncology management program Limited to R200 000 pbpa.
protocols - PMB Only
Treatment limited to Tier 1 protocols.
HIV Programme (Network Hospitals). Subject to
Scheme Protocols and PMB. Covered at
provincial facility if not registered
Unlimited if registered on HIVCare Programme R12 000 if not registered
Unlimited, subject to Disease Mangement
Programme and protocols
Subject to registration on the CareWorks
program
ER24
Discovery 911
Netcare 911
ER 24 - Unlimited.
Non-Prefered Provider: Ltd to R1600 per family
7 Days supply
R100 per beneficiary per admission
R240 per beneficiary per admission
No Benefit
Emergency Ward Treatment which does not result in
Hospitalisation
R1 115 per family
Preferred Casualty units in Keycare Network of
hospitals, only pay R110 of consultation. Other
casualty units will pay R250 for consultation
Covered only if indicated as Emergency (PMB)
by treating doctor
No Benefit
International Medical Travel Assistance
No Benefit
No Benefit
No Benefit
No Benefit
No Benefit
No Benefit
R13 500 per family for sub-acute & private
nursing facilities. Subject to pre-authorisation &
case management.
Limited to PMB treatment only
Prescribed Minimum Benefits
Subject to PMB treatment
Prescribed Minimum Benefits
Unlimited to PMB
Prescribed Minimum Benefits
Prescribed Minimum Benefits and 8 additional
conditions covered
Maternity Benefits
(In & Out of Hospital)
Psychiatric & Psychological Treatment
MRI & CAT Scans
(In & Out of Hospital)
Oncology/Cancer (In & Out of Hospital)
(Comprehensive Oncology benefits per scheme available on request)
HIV/Aids - Sub limits on Medicine might apply
Ambulances Services/Administrators used by the Scheme (In case
of an Emergency any service can be used)
Discharge Medicine (Take Home Medicine)
Post Hospitalisation Benefit (Treatment after discharge pertaining to
hospitalisation paid from Risk benefits)
Internally Implanted Prostheses
(Limits apply only on Prostheses)
Dialysis
Joint replacements, including but not limited to
R30 600 per family, subject to Prosthesis specific hips, knees, shoulders and elbows will be
limit
excluded.
No cover for elective hip & knee replacements
Cover for PMB Emergencies only
Covered at Network hospitals and subject to
PMB. Protocols apply
Covered up to maximum of 100% of Scheme
Tariff at a network provider only
Chronic Benefits:
All Schemes provide unlimited Prescribed Minimum Benefits (PMB) for the
Prescribed Minimum Benefits
treatment of Conditions (Chronic Disease List) e.g. Diabetes, Asthma, Cholesterol,
Hypertension, etc. Benefits are Subject to a Scheme treatment plan, formulary, Subject to Network formulary
registration, pre-authorisation and a Designated Service Provider (DSP) to avoid a
co-payment. Benefits will be paid first from stipulated (if any) available Chronic
Designated Service Provider: Network Provider
Benefits, thereafter unlimited at DSP. Non-PMB conditions will be paid from
Acute/Savings benefits if Chronic Benefits are not available/depleted.
Page 2 (of 3)
Prescribed Minimum Benefits
Designated Service Provider: Chosen primary
dispensing GP, Optipharm, DisChem or Clicks
If the designated service provider is not used, a
40% co-payment will apply
Designated Service Provider: Medihelp
Pharmacy Network
Designated Service Provider: CareCross
SCHEME OPTION:
OUT OF HOSPITAL BENEFITS:
*Day-to-Day Benefits, or **Savings, which is included
in the Total Monthly Premium to make provision for
medical expenses that does not require hospitalisation
e.g. GP visits & Dentistry is displayed on this page.
H1
G2
D1
B1
(Income R5 501 - R7 500)
(Income R3 901 - R6 250)
(Income 0 - 7500)
(Income R3 501 - R7 500)
Limited Primary Health Care available through
Network Providers
No Benefit for Wisdom teeth removal
Unlimited Primary Health Care Benefits available
through chosen KeyCare Network Doctor
(No Benefits for Wisdom teeth removal)
Screening Benefit
Guardian Benefit covers certain preventative
screening tests at Network Providers.
Trauma Recovery Extended Benefit
Includes Pharmacist Benefit of R283 per family
for over the counter medication
Mobility Devices Benefit
Unlimited Primary Health Care Benefits available Unlimited Primary Health Care available through
through the Medihelp Preferred Provider Network your chosen CareCross Provider
Dental covered at 100% of Scheme dental tariff - (Impacted Wisdom teeth - no cover, except in
Subject to DENIS limits, protocols & pre-auth
trauma cases)
TOTAL *In-Scheme Day-to-Day Benefits(if applicable) & or **Savings:
Annual Threshold/Safety Net limit to be reached:
N/A
N/A
N/A
N/A
Estimated Self Payment Gap:
N/A
N/A
N/A
N/A
General Practitioner Visits
Unlimited at Network Provider
Unlimited at chosen KeyCare Network doctor
Second GP can be nominated
Unlimited at Medihelp Network provider. Out of
network visits ltd to R700 single member,
R1 400 per family with 20% co-payment
Unlimited-at Primary CareCross GP. Non-Primary
ltd to 3 visits per family to max of R1000 per
family per year
Specialist Visits
4 network visits per family to a max of R1 000.
Subject to pre-authorisation.
R2100 per beneficiary-must be referred by GPonly at doctor working at a network hospital.
Subject to pre-authorisation.
R2000 per beneficiary, to maximum of R2 800
per family. Subject to pre-authorisation.
Limited to R2 100 per family per year. Subject to
referral by Carecross GP and pre-authorisation.
Prescribed/ Acute Medicine
Subject to Network accute formulary.
Pharmacist Benefit R283 per family
Unlimited Subject to the KeyCare Acute Medicine Subject to overall annual limit. Must be
Formulary prescribed by network General
prescribed by network GP and obtained from
Practioner
dispensing GP or network pharmacy
(Consultations, Oral hygiene, Extractions & Fillings)
2 annual check ups per beneficiary covered at
Network Providers
Unlimited at chosen KeyCare Dentist Network
Subject to DENIS protocols, e.g. 1 routine
checkup, 1 oral hygiene visit, 4 fillings pbpa
Unlimited - Subject to CareCross Dentist.
Dentures ltd to 1 set per 24-month cycle per
family. 20% co-pay
Specialised/Advanced Dentistry
No Benefit
No Benefit
No Benefit
No Benefit
No Benefit
No Benefit
Occupational Therapists & Physiotherapy
R1 300 per beneficiary to a maximum of
R2 000 per family
No Benefit
Mental Health
No Benefit
No Benefit
Prescribed Minimum Benefits
Psychiatry limited to PMB
Optical
1 Consultation per beneficiary per 24-month
cycle covered at Network Provider, including
single mono or bifocal prescription.
One eye test, 1 pair of clear single-vision, bifocal
or multi-focal lenses with basic frame or basic set
of contact lenses every 2 years per beneficiary from Keycare Optometry Network
PPN Network. 1 eye test, 1 pair clear single
vision or bifocal glasses per beneficiary in 24month cycle. R150 towards frames. R395
towards contact lenses (PPN only).
Subject to CareCross Optometrist. Benefits per
beneficiary per 24 month cycle: 1 consultation, 1
pair of white single and/or bifocal lenses and
choice of selected frames or contact lenses limit
R350 per beneficiary
Radiology & Pathology
Limited to Network Provider
Pathology: Unlimited - only if required by KeyCare
Network doctor
Radiology: Selected basic x-rays at a radiology
facility in the Network, if required by Network GP
Subject to overall annual limit. Subject to referral
Basic radiology and pathology unlimited - Subject
by network GP, preferred providers Lancet and
to CareCross Doctor/Facility
Pathcare and clinical protocols
Copyright reserved by Optivest Health Services
*Co-payments apply:
*Funeral Benefit: R5 000 benefit to Principal
R1 000 on Circumcision, Colonoscopy, Sigmoidoscopy, member for R1. Maximum age 65 next birthday.
Proctoscopy, Excision nailbed, Myringotomy (grommets);
R1 250 on Gastroscopy, Skin lesions; R2 000 on
Arthroscopy; R2 250 on Hysteroscopy; R2 500 on
Conservative Back treatment, Joint replacements; R3
000 on Functional nasal surgery,
HysterectomyLaparoscopic procedure, Reflux surgery;
R4 000 on Spinal Surgery
Basic Dentistry
Auxiliary Services (Homeopaths, Dieticians, Clinical psychologists, Speech
therapists, Physiotherapy, Chiropractors & Occupational therapists)
*In Scheme Day-to-Day Benefits:
Benefits that are part of Risk Cover, unused benefits will not carry over to next year.
**Savings:
Fixed Rand Amount for Day-to-Day Benefits upfronted annually. Savings that are not used for be
carried over to next year.
All Day-to-Day Benefits and Savings is calculated pro-rata per annum .
Co-payments will not apply for procedures performed out of
hospital or for PMB.
Optional Co-Pay Cover
Page 3 (of 3)
Children regarded as child dependants up to 21st Birthday
Unlimited - Subject to CareCross Formulary
Anda mungkin juga menyukai
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- FacilitiesDokumen19 halamanFacilitiesJeffs9430Belum ada peringkat
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Intraoral RadiographicDokumen62 halamanIntraoral RadiographicEuginiaBelum ada peringkat
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- AssertivenessDokumen4 halamanAssertivenessDamir MujagicBelum ada peringkat
- Grant ProposalDokumen16 halamanGrant Proposalapi-392153225Belum ada peringkat
- WHO-GMP Guidlines For Pharmaceutical IndustriesDokumen148 halamanWHO-GMP Guidlines For Pharmaceutical Industriesmoo78100% (5)
- What Are Coping Mechanisms?Dokumen7 halamanWhat Are Coping Mechanisms?Blaze QuibanBelum ada peringkat
- Aaron Beck On Cognitive Therapy: Instructor's ManualDokumen46 halamanAaron Beck On Cognitive Therapy: Instructor's ManualNarendra100% (3)
- Pulmonary RehabilitationDokumen412 halamanPulmonary Rehabilitationhuxley237860% (5)
- Hendrix PDFDokumen2 halamanHendrix PDFgeorgiana vasileBelum ada peringkat
- CSA11 CholelithiasisDokumen3 halamanCSA11 CholelithiasisBerlon LacsonBelum ada peringkat
- Artificial LiverDokumen1 halamanArtificial LiverPradeep MahalikBelum ada peringkat
- Renal Diseases " Review "Dokumen22 halamanRenal Diseases " Review "api-3827876Belum ada peringkat
- In Vivo Dosimetry in BrachytherapyDokumen17 halamanIn Vivo Dosimetry in BrachytherapySUBHABelum ada peringkat
- Measles (Campak, Rubeola, Gabak, Kerumut)Dokumen20 halamanMeasles (Campak, Rubeola, Gabak, Kerumut)Ami UtamiatiBelum ada peringkat
- Chapter 1. Introduction To PsychiatryDokumen11 halamanChapter 1. Introduction To PsychiatryDiego Francesco MacaliBelum ada peringkat
- Endoscopy and Microendoscopy of The Lacrimal Drainage SystemDokumen60 halamanEndoscopy and Microendoscopy of The Lacrimal Drainage SystemhwalijeeBelum ada peringkat
- Drug Study - CaDokumen3 halamanDrug Study - Casaint_ronald8Belum ada peringkat
- Occular Drug Delivery System - Vinod SijuDokumen120 halamanOccular Drug Delivery System - Vinod Sijuvinsijuvin555Belum ada peringkat
- Folding and Unfolding Manual WheelchairsDokumen9 halamanFolding and Unfolding Manual WheelchairsprkranjithkumarBelum ada peringkat
- DOI Bienestar, Autoeficacia e Independencia en Adultos Mayores Un Ensayo Aleatorizado de Terapia OcupacionalDokumen8 halamanDOI Bienestar, Autoeficacia e Independencia en Adultos Mayores Un Ensayo Aleatorizado de Terapia OcupacionalJhon MillerBelum ada peringkat
- Bourdin, D. (2003) - La Pensée Clinique Clinical Thinking André GreenDokumen4 halamanBourdin, D. (2003) - La Pensée Clinique Clinical Thinking André GreenofanimenochBelum ada peringkat
- Resorption of A Calcium Hydroxide/iodoform Paste (Vitapex) in Root Canal Therapy For Primary Teeth: A Case ReportDokumen4 halamanResorption of A Calcium Hydroxide/iodoform Paste (Vitapex) in Root Canal Therapy For Primary Teeth: A Case ReportHasbi Brilian KumaraBelum ada peringkat
- Grand Case Presentation FormatDokumen7 halamanGrand Case Presentation FormatRENEROSE TORRESBelum ada peringkat
- AtosPharma Intro PDFDokumen33 halamanAtosPharma Intro PDFmohalaaBelum ada peringkat
- Assessment of Development and GrowthDokumen21 halamanAssessment of Development and Growthdrng48Belum ada peringkat
- EMIMAc MSDSDokumen6 halamanEMIMAc MSDSalvaro_cruzBelum ada peringkat
- Application of CTASDokumen32 halamanApplication of CTASsidekick941Belum ada peringkat
- Pathophysiology of Congenital Heart Disease in The Adult: Special ReportDokumen11 halamanPathophysiology of Congenital Heart Disease in The Adult: Special ReportResiden KardiologiBelum ada peringkat
- Document 105Dokumen14 halamanDocument 105Marie JhoanaBelum ada peringkat
- Ashley's TreatmentDokumen3 halamanAshley's TreatmentBrandon M. DennisBelum ada peringkat